Valvular Heart Disease Valves Mitral valve Aortic valve

- Slides: 26
Valvular Heart Disease
Valves • • Mitral valve Aortic valve Tricuspid valve Pulmonary valve
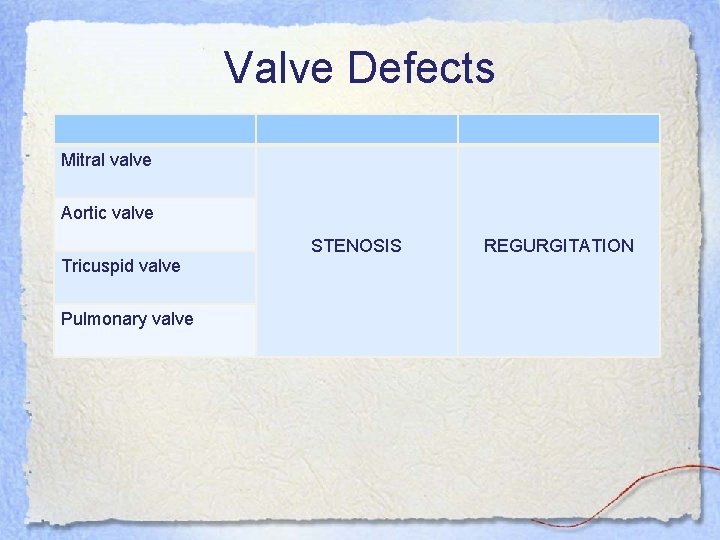
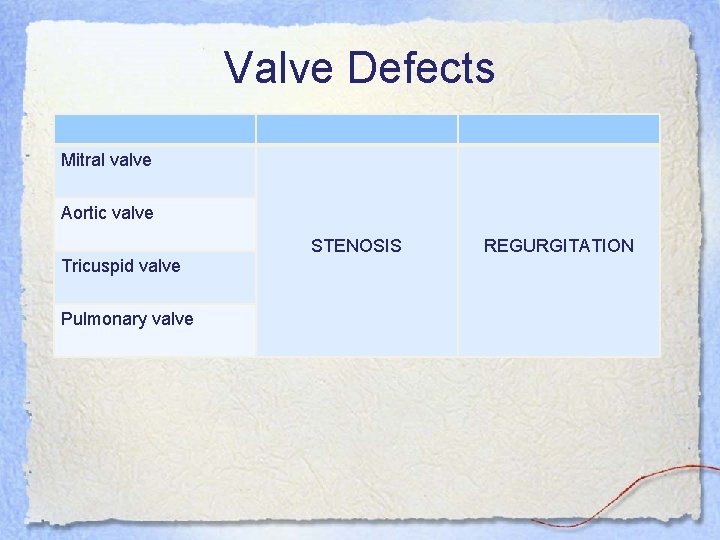
Valve Defects Mitral valve Aortic valve Tricuspid valve Pulmonary valve STENOSIS REGURGITATION
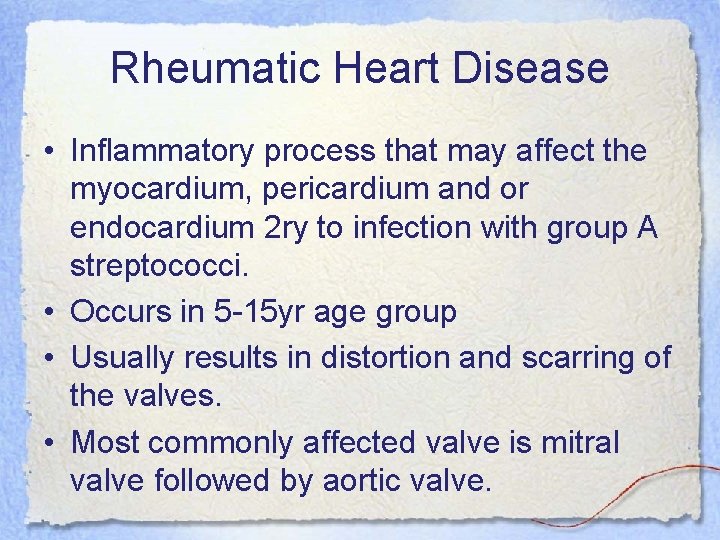
Rheumatic Heart Disease • Inflammatory process that may affect the myocardium, pericardium and or endocardium 2 ry to infection with group A streptococci. • Occurs in 5 -15 yr age group • Usually results in distortion and scarring of the valves. • Most commonly affected valve is mitral valve followed by aortic valve.
Pathology • Abs produced against streptococci cross react with cardiac myosin, sarcolemmal membrane protein. • Inflammation occurs in joints and skin in addition to heart.
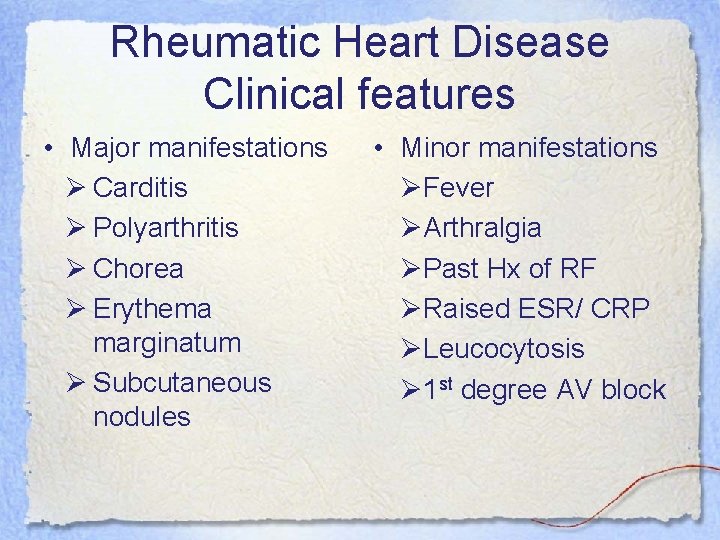
Rheumatic Heart Disease Clinical features • Major manifestations Ø Carditis Ø Polyarthritis Ø Chorea Ø Erythema marginatum Ø Subcutaneous nodules • Minor manifestations ØFever ØArthralgia ØPast Hx of RF ØRaised ESR/ CRP ØLeucocytosis Ø 1 st degree AV block
Rheumatic Heart Disease • Diagnosis is done according to Jones criteria. ü 2 or more major manifestations ü 1 major + 2 or more minor manifestations
Rheumatic Heart Disease Treatment • • • Penicillin Bed rest Aspirin Corticosteroid Secondary prevention with monthly benzathine penicillin injections.
Mitral Stenosis • • Usually results from rheumatic carditis Is a thickening by fibrosis or calcification Can be caused by tumors, calcium and thrombus Valve leaflets fuse and become stiff and the cordae tendineae contract These narrows the opening and prevents normal blood flow from the LA to the LV LA pressure increases, left atrium dilates, PAP increases, and the RV hypertrophies Pulmonary congestion and right sided heart failure occurs Followed by decreased preload and CO decreases
Mitral Stenosis, cont. • Mild – asymptomatic • With progression – dyspnea, orthopneas, dry cough, hemoptysis, and pulmonary edema may appear as hypertension and congestion progresses • Right sided heart failure symptoms occur later • S/S – Pulse may be normal to A-Fib – Apical diastolic murmur is heard
Mitral Regurgitation • Primarily caused by rheumatic heart disease, but may be caused by papillary muscle rupture form congenital, infective endocarditis or ischemic heart disease • Abnormality prevents the valve from closing • Blood flows back into the right atrium during systole • During diastole the regurg output flows into the LV with the normal blood flow and increases the volume into the LV • Progression is slowly – fatigue, chronic weakness, dyspnea, anxiety, palpitations • May have A-fib and changes of LV failure • May develop right sided failure as well
Mitral Valve Prolapse • Cause is variable and may be associated with congenital defects • More common in women • Valvular leaflets enlarge and prolapse into the LA during systole • Most are asymptomatic • Some may report chest pain, palpitations or exercise intolerance • May have dizziness, syncope and palpitations associated with dysrhythmias • May have audible click and murmur
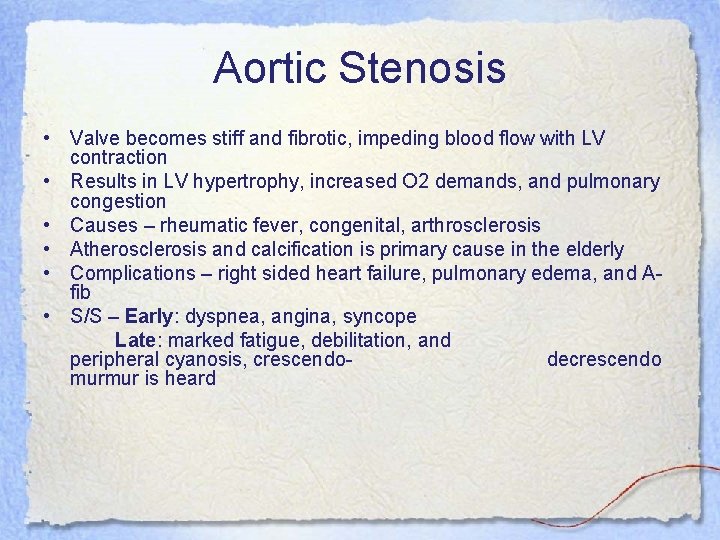
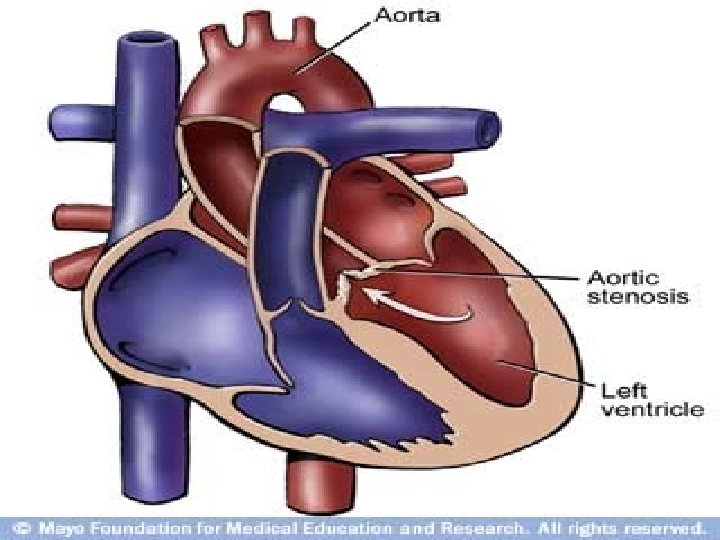
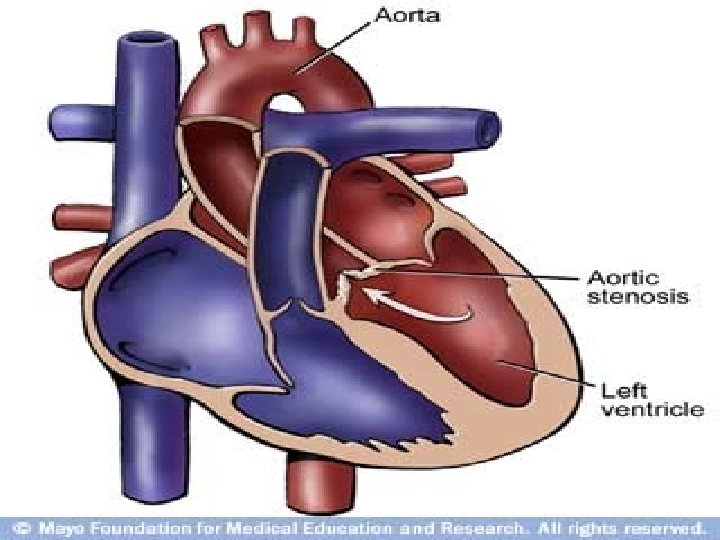
Aortic Stenosis • Valve becomes stiff and fibrotic, impeding blood flow with LV contraction • Results in LV hypertrophy, increased O 2 demands, and pulmonary congestion • Causes – rheumatic fever, congenital, arthrosclerosis • Atherosclerosis and calcification is primary cause in the elderly • Complications – right sided heart failure, pulmonary edema, and Afib • S/S – Early: dyspnea, angina, syncope Late: marked fatigue, debilitation, and peripheral cyanosis, crescendodecrescendo murmur is heard
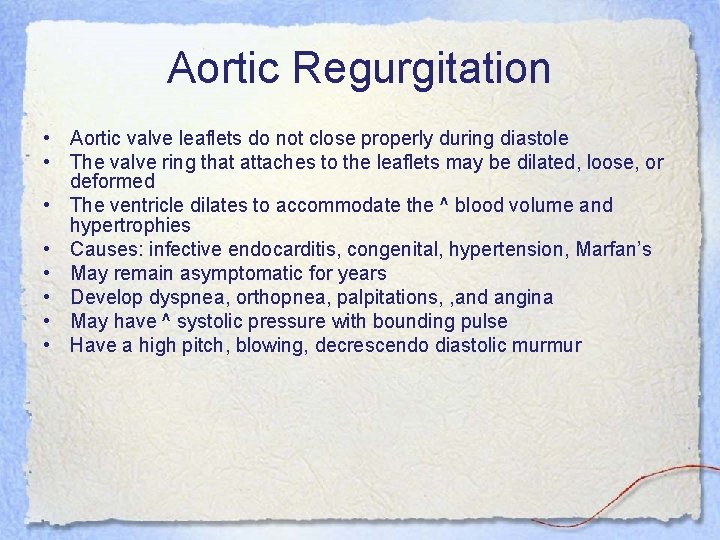
Aortic Regurgitation • Aortic valve leaflets do not close properly during diastole • The valve ring that attaches to the leaflets may be dilated, loose, or deformed • The ventricle dilates to accommodate the ^ blood volume and hypertrophies • Causes: infective endocarditis, congenital, hypertension, Marfan’s • May remain asymptomatic for years • Develop dyspnea, orthopnea, palpitations, , and angina • May have ^ systolic pressure with bounding pulse • Have a high pitch, blowing, decrescendo diastolic murmur
Assessment for Valve Dysfunction • Subjective symptoms – Fatigue – Weakness – General malaise – Dyspnea on exertion – Dizziness – Chest pain or discomfort – Weight gain – Prior history of rheumatic heart disease
Assessment, cont. • Objective symptoms – – – – – Orthopnea Dyspnea, rales Pink-tinged sputum Murmurs Palpitations Cyanosis, delayed capillary refill Edema Dysrhythmias Restlessness
Diagnosis • • • History and physical findings ECG Chest x-ray Cardiac catheterization Echocardiogram
Medial Treatment • Nonsurgical management focuses on drug therapy and rest • Diuretic, beta blockers, digoxin, O 2, vasodilators, prophylactic antibiotic therapy • Manage A-fib, if develops, with conversion if possible, and use of anticoagulation
Interventions • • Assess vitals, heart sounds, breath sounds O 2 as prescribed Emotional support Give medications I/O Weight Check for edema Explain disease process, provide for home care with O 2, medications
Surgical Management of Valve Disease • Mitral Valve – Commissurotomy – Mitral Valve Replacement – Balloon Valvuloplasty • Aortic Valve Replacement
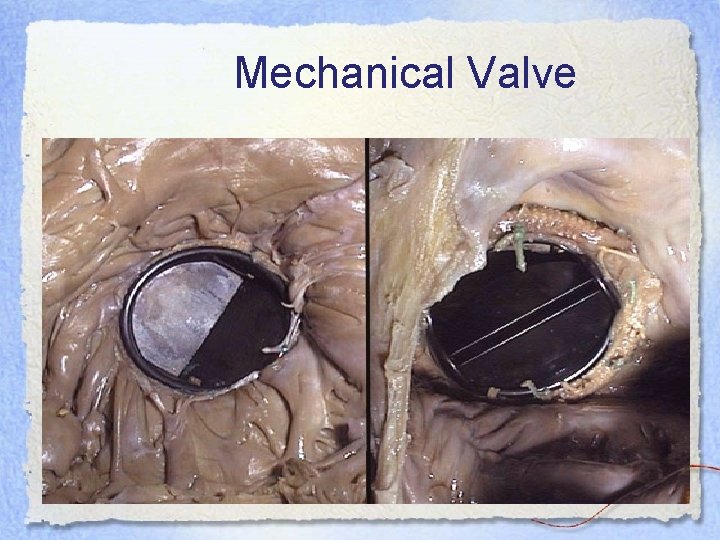
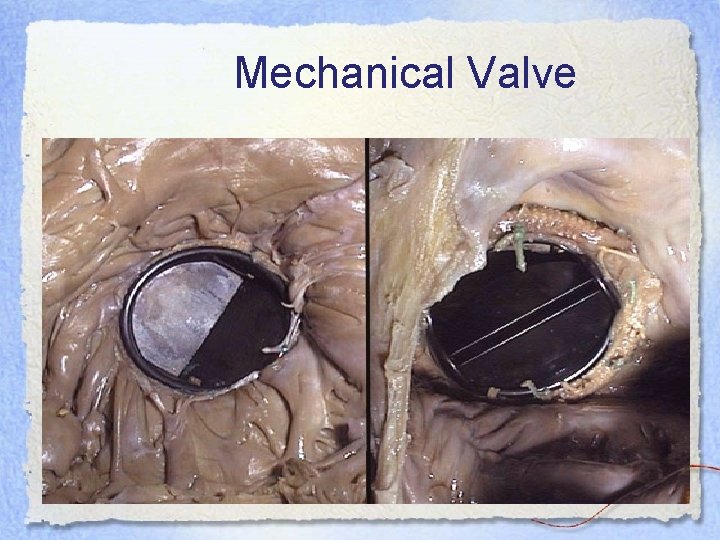
Mechanical Valve
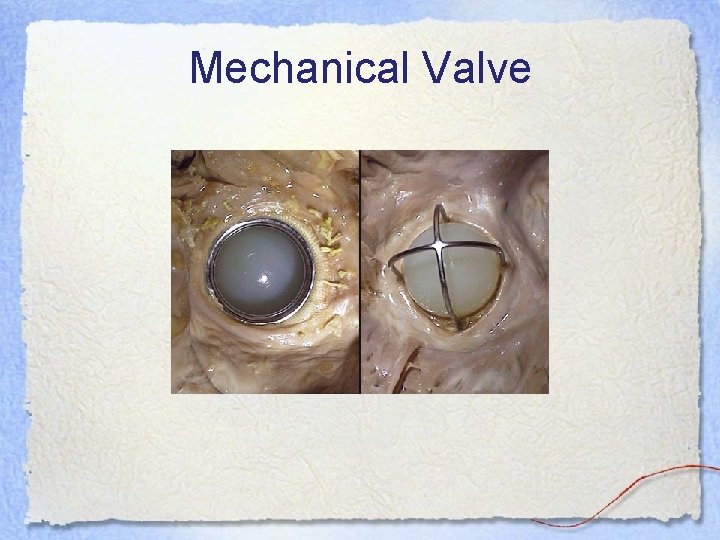
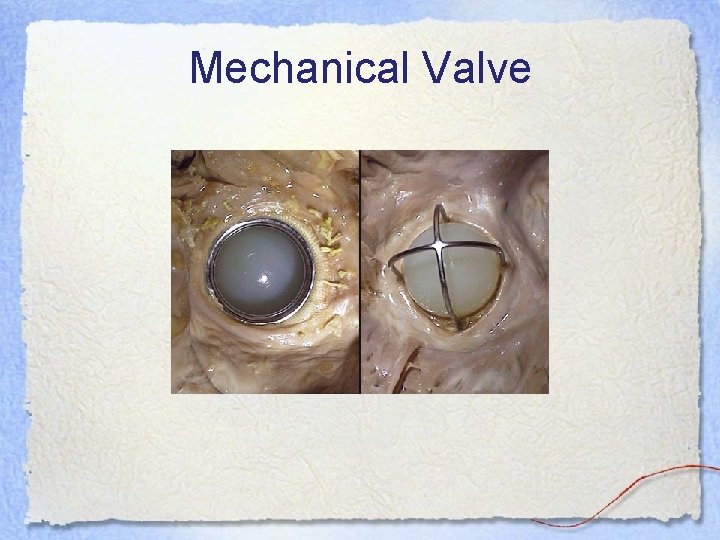
Mechanical Valve

Porcine Valve
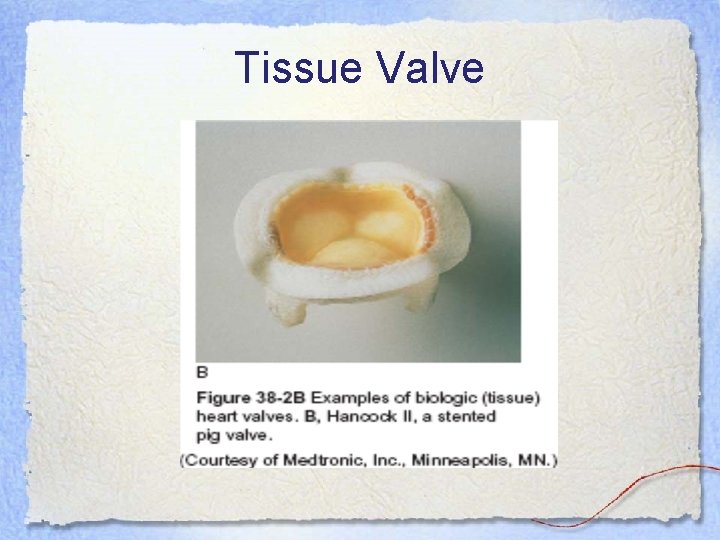
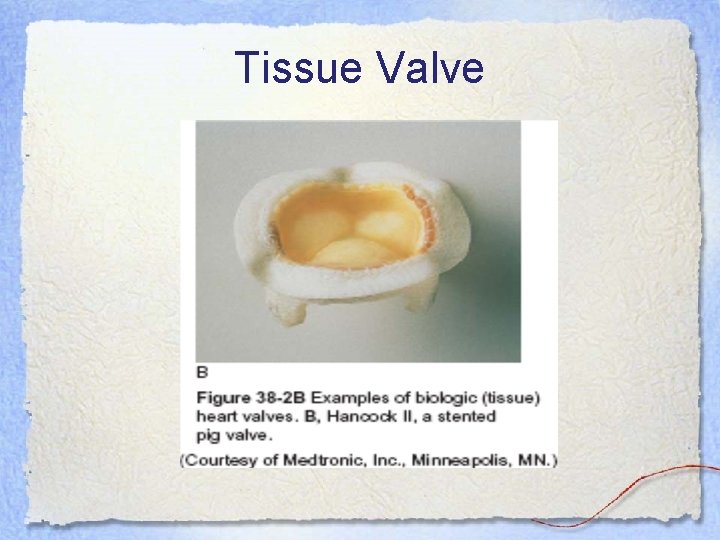
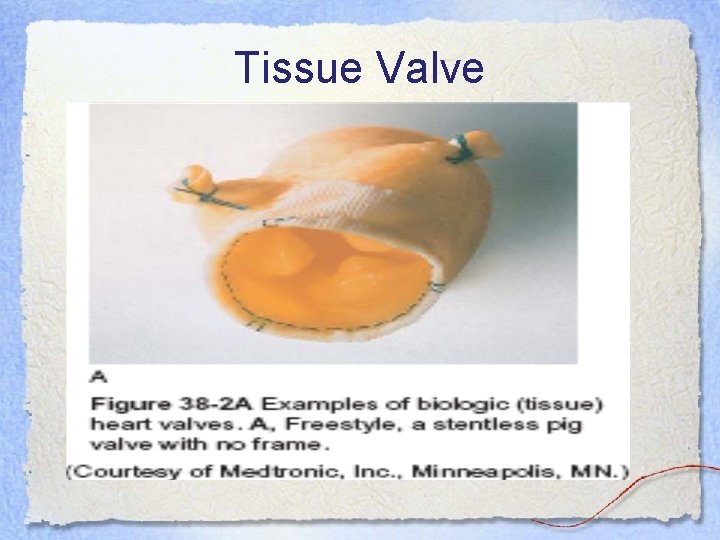
Tissue Valve
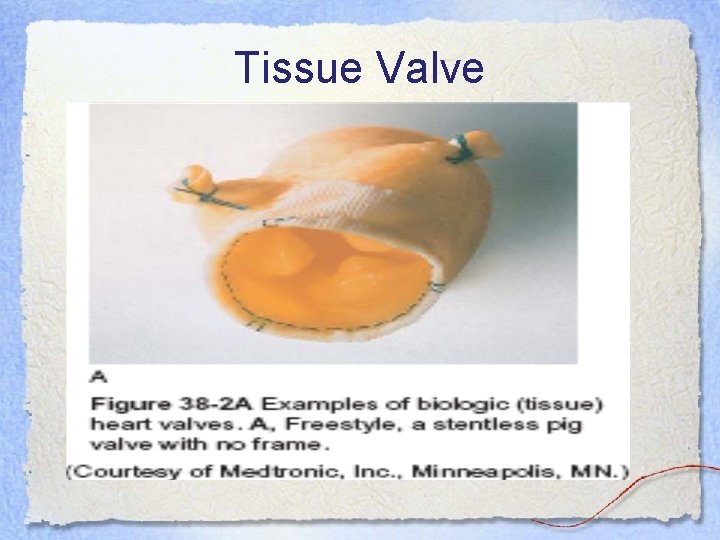
Tissue Valve