VALVULAR HEART DISEASE MUDr Jan Tomis 52016 Normal









- Slides: 63
VALVULAR HEART DISEASE MUDr. Jan Tomis 5/2016
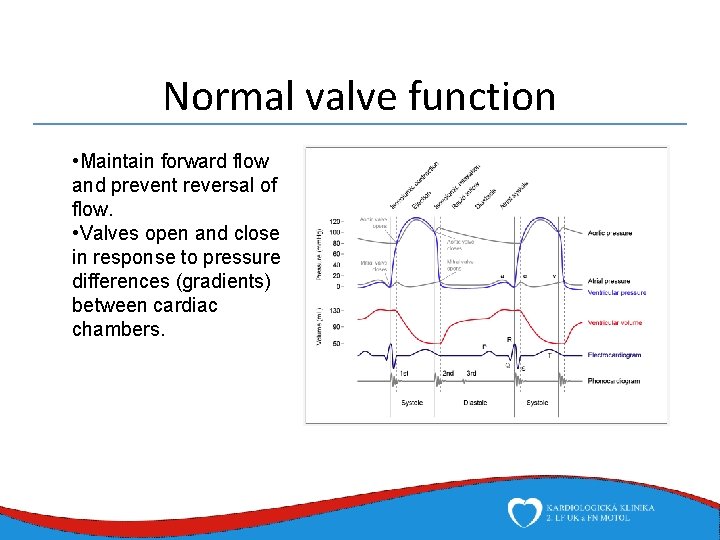
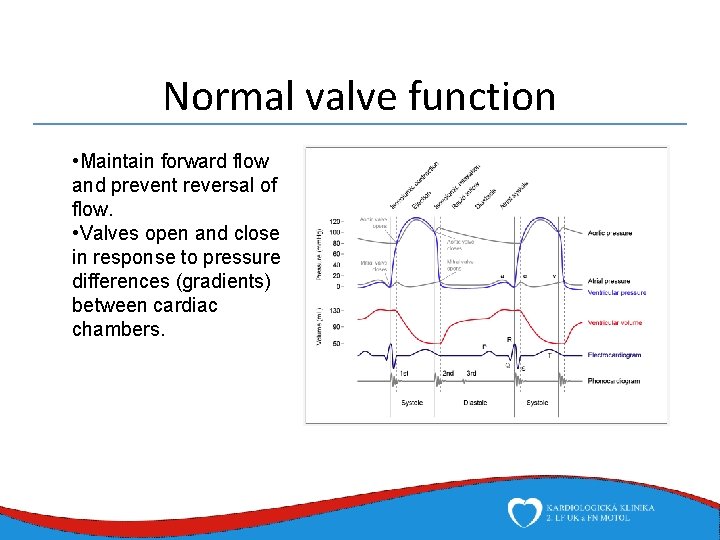
Normal valve function • Maintain forward flow and prevent reversal of flow. • Valves open and close in response to pressure differences (gradients) between cardiac chambers.
Abnormal valve function • Valve Stenosis • Obstruction to valve flow during that phase of the cardiac cycle when the valve is normally open. • Hemodynamic hallmark -“pressure gradient” • Valve Regurgitation, insufficiency, incompetence • Inadequate valve closure → reverse flow of the blood, back leakage • Combined – a single valve can be both stenotic and regurgitant; combinations of valve lesions can coexist • Single disease process • Different disease processes • One valve lesion may cause another • Certain combinations are particularly common(AS & MR, MS & TR)
Valvular heart disease • Common cause of cardiovascular morbidity, 2 nd most common indication for heart surgery (after ischemic heart disease) • In the Czech Republic (2012): 8644 heart surgeries, about 46% involved valve intervention • Combined myocardial revascularisation and valve surgery particularly common for some diagnosis – CABG + AVR (common risk factor), CABG + MRV (in ischemic mitral regurgitation)
Diagnosis • • • History Physical examination ECG Chest x-ray Echocardiography Invasive evaluation, CT, MRI
Diagnosis • • • History Physical examination ECG Chest x-ray Echocardiography Invasive evaluation, CT, MRI

History • Other known heart diseses • Congenital heart disease, bicuspid aortic valve • Ischemic heart disease • Rheumatic fever • Hypertrophic/dilated cardiomyopathy • Aortic diseases – Marfans, Ehlers-Danlos
History • Generally: symptoms of heart failure and low cardiac output • Breathlessness • Chest pain or dyscomfort • Syncope • Fatigue • Periferal or pulmonary oedema • Palpitations
Diagnosis • • • History Physical examination ECG Chest x-ray Echocardiography Invasive evaluation, CT, MRI
Physical examination
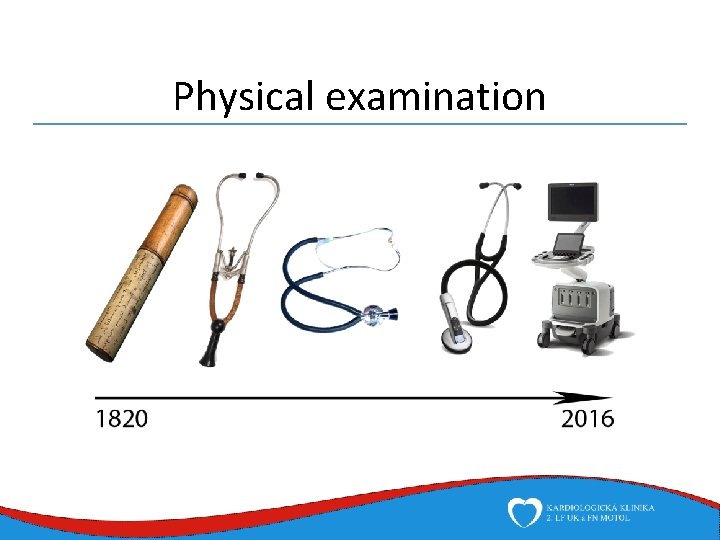
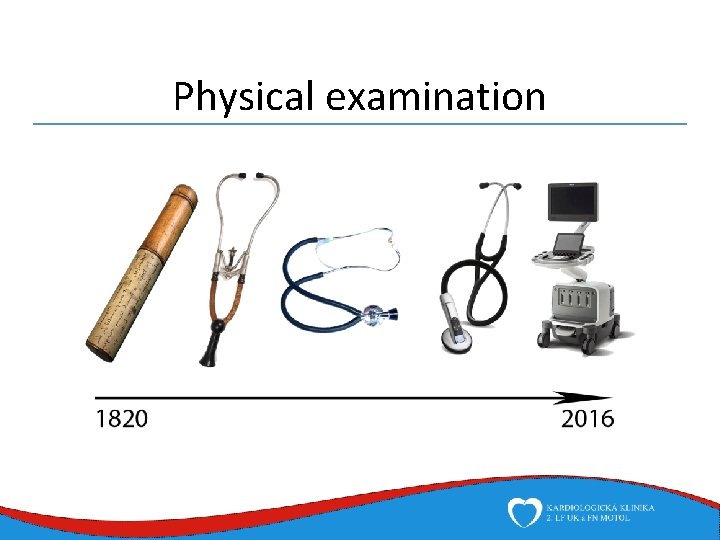
Physical examination
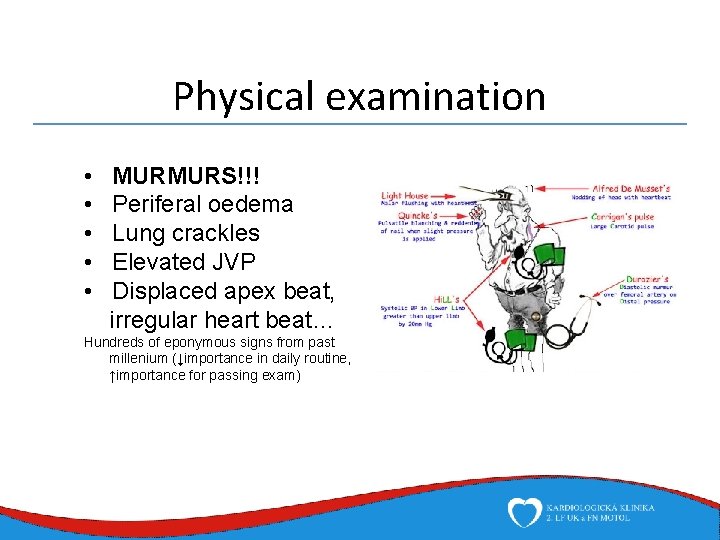
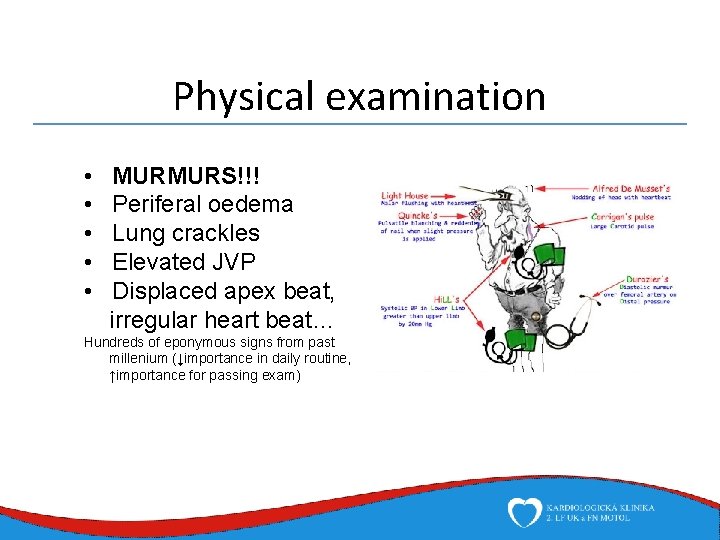
Physical examination • • • MURMURS!!! Periferal oedema Lung crackles Elevated JVP Displaced apex beat, irregular heart beat… Hundreds of eponymous signs from past millenium (↓importance in daily routine, ↑importance for passing exam)
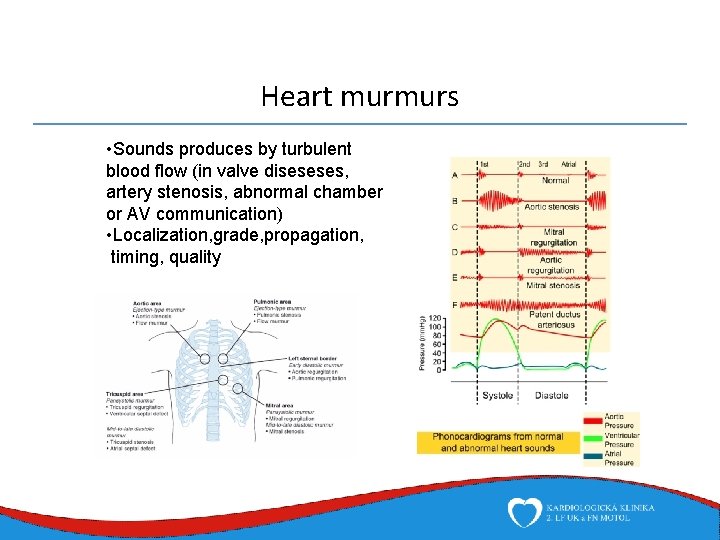
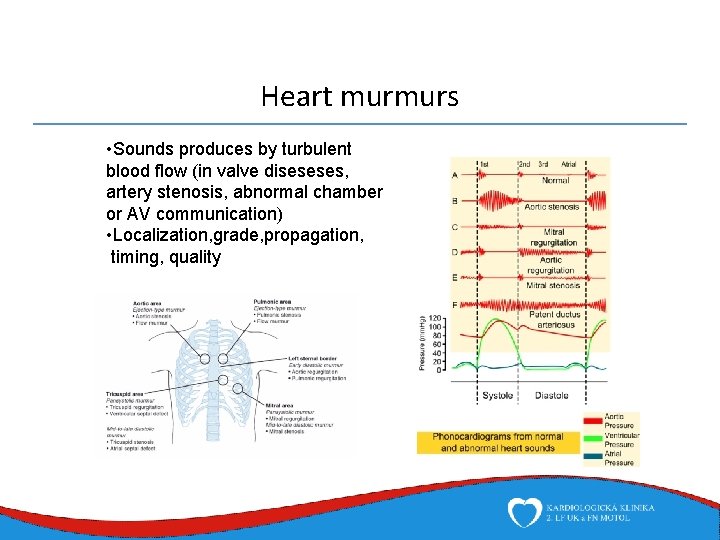
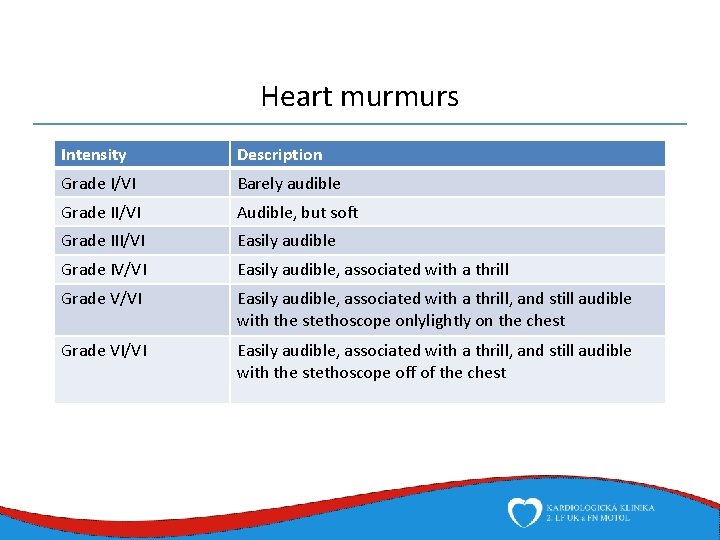
Heart murmurs • Sounds produces by turbulent blood flow (in valve diseseses, artery stenosis, abnormal chamber or AV communication) • Localization, grade, propagation, timing, quality
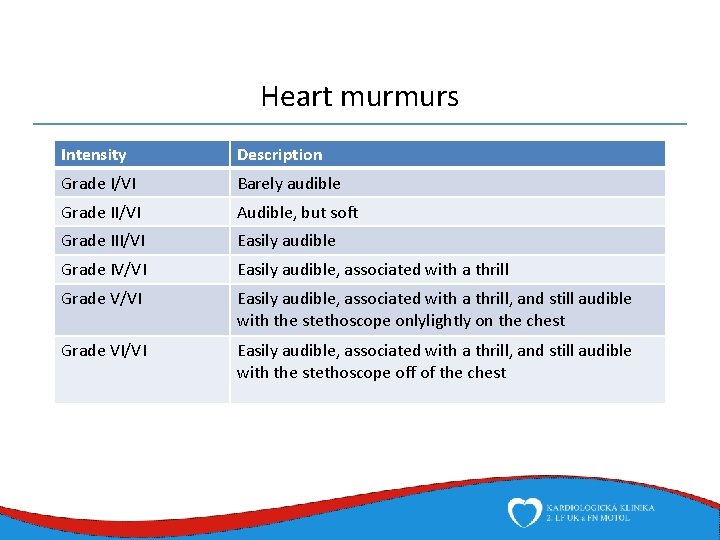
Heart murmurs Intensity Description Grade I/VI Barely audible Grade II/VI Audible, but soft Grade III/VI Easily audible Grade IV/VI Easily audible, associated with a thrill Grade V/VI Easily audible, associated with a thrill, and still audible with the stethoscope onlylightly on the chest Grade VI/VI Easily audible, associated with a thrill, and still audible with the stethoscope off of the chest
Diagnosis • • • History Physical examination ECG Chest x-ray Echocardiography Invasive evaluation, CT, MRI
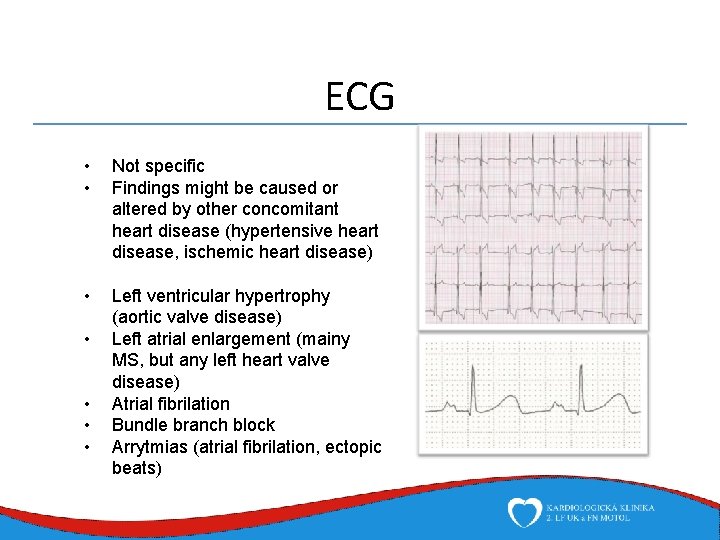
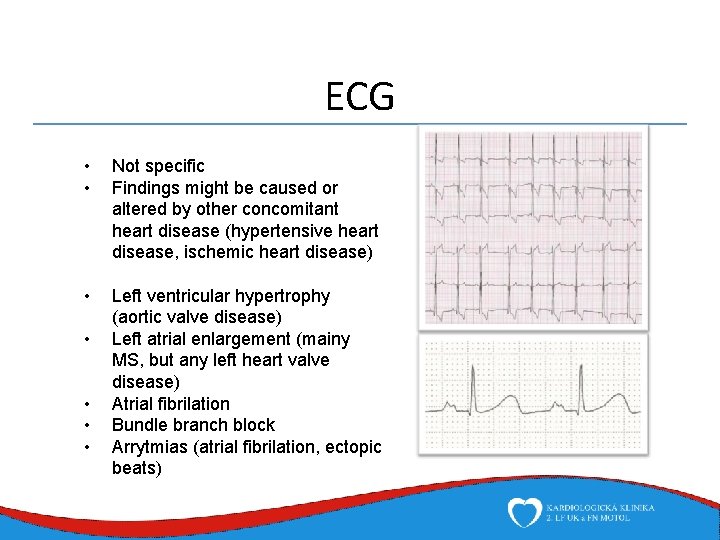
ECG • • Not specific Findings might be caused or altered by other concomitant heart disease (hypertensive heart disease, ischemic heart disease) • Left ventricular hypertrophy (aortic valve disease) Left atrial enlargement (mainy MS, but any left heart valve disease) Atrial fibrilation Bundle branch block Arrytmias (atrial fibrilation, ectopic beats) • •
Diagnosis • • • History Physical examination ECG Chest x-ray Echocardiography Invasive evaluation, CT, MRI
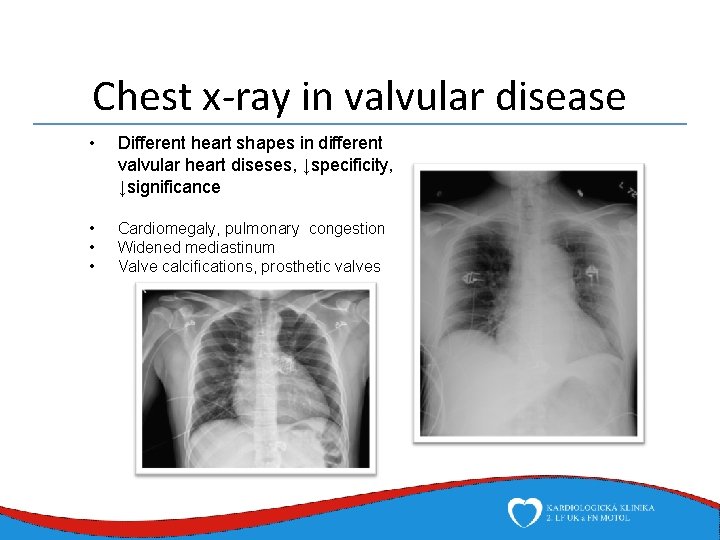
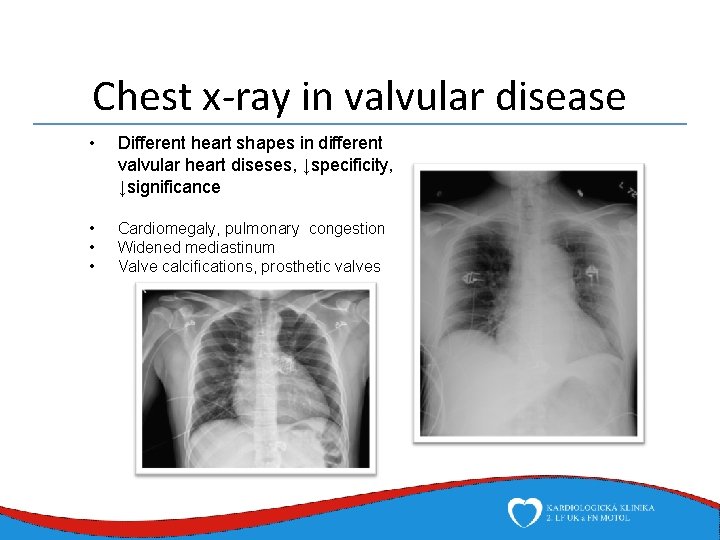
Chest x-ray in valvular disease • Different heart shapes in different valvular heart diseses, ↓specificity, ↓significance • • • Cardiomegaly, pulmonary congestion Widened mediastinum Valve calcifications, prosthetic valves

Diagnosis • • • History Physical examination ECG Chest x-ray Echocardiography Invasive evaluation, CT, MRI
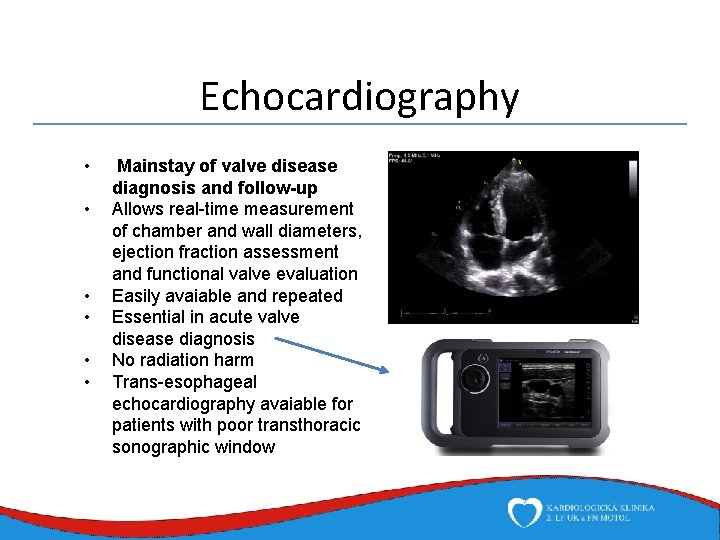
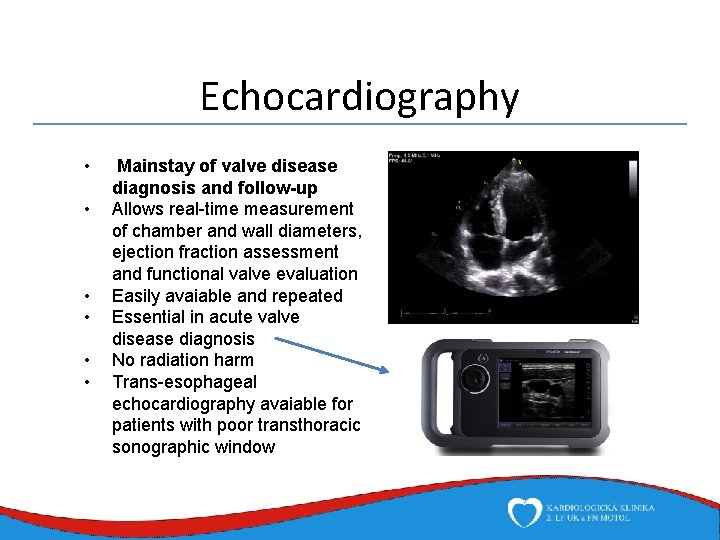
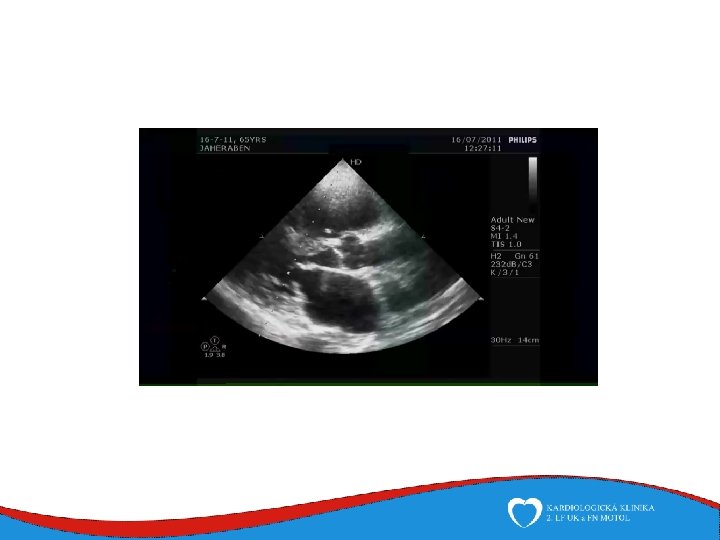
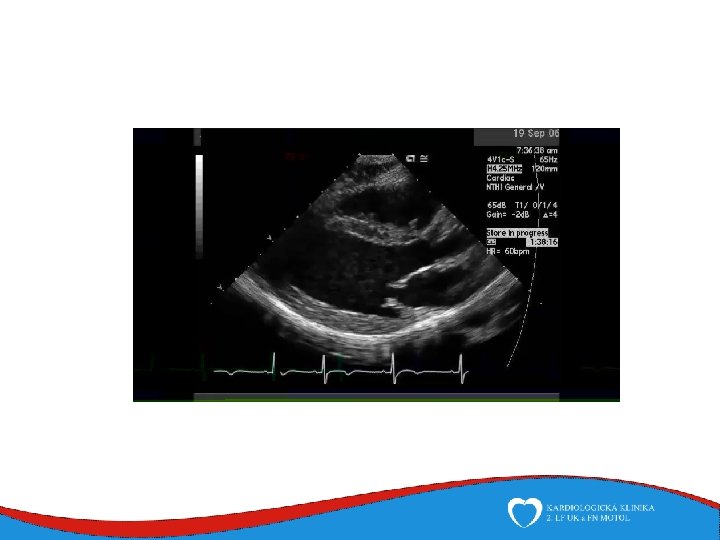
Echocardiography • • • Mainstay of valve disease diagnosis and follow-up Allows real-time measurement of chamber and wall diameters, ejection fraction assessment and functional valve evaluation Easily avaiable and repeated Essential in acute valve disease diagnosis No radiation harm Trans-esophageal echocardiography avaiable for patients with poor transthoracic sonographic window
Diagnosis • • • History Physical examination ECG Chest x-ray Echocardiography Invasive evaluation, CT, MRI
Invasive evaluation, CT, MRI • Methods usualy used for uncertain cases or repeat cardiac surgery / percutaneous inteventions planning • Angiography to assess regurgitation severity – direct transcatheter contrast medium administration into heart chambers – aortography, ventriculography Hemodynamic measurment – measuring of intracardial pressures and gradients CT aortography – method of choice in aortic dissection diagnosis CMRI – very precise evaluation of cardiac tissues and function, but expensive, low avaiability, long examination time • • •

Aortic stenosis • Most common indication for valve intervention • Causes • Degenerative aortic stenosis • Bicuspid aortic valve • Congenital aortic stenosis, unicuspid aortic valve • Rheumatic disease (always with mitral valve involvement) • Infective endocarditis (but severe stenosis due to massive vegetations is extremely rare) • Other rare causes – post radiation, associated with systemic disease
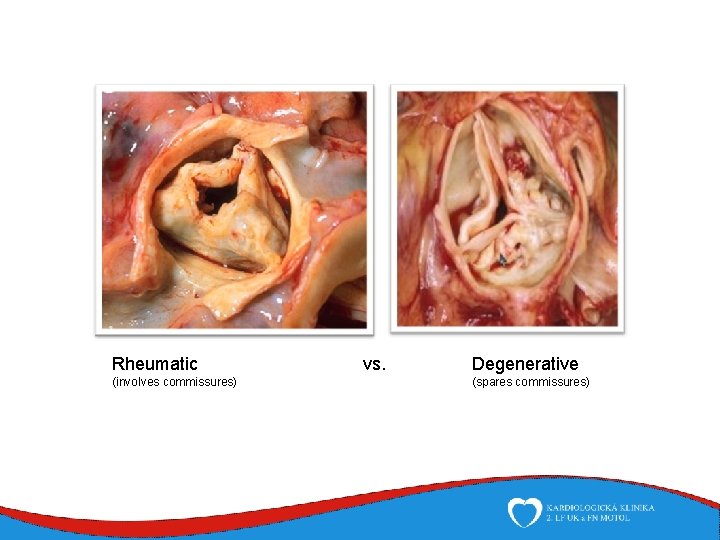
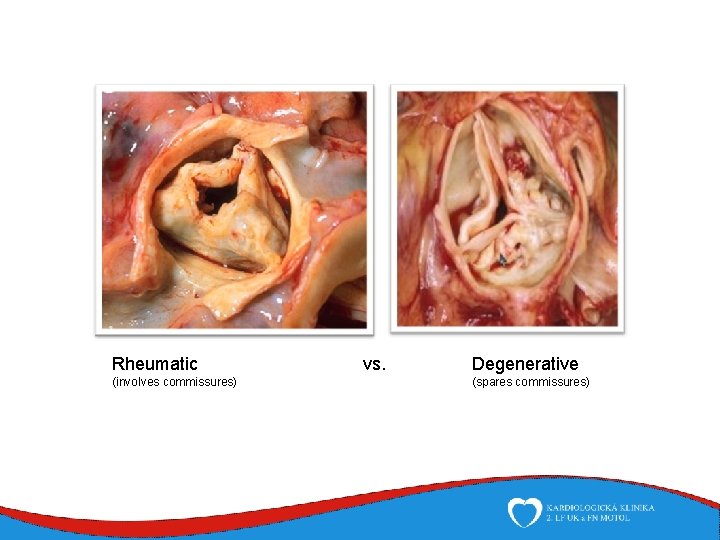
Rheumatic (involves commissures) vs. Degenerative (spares commissures)
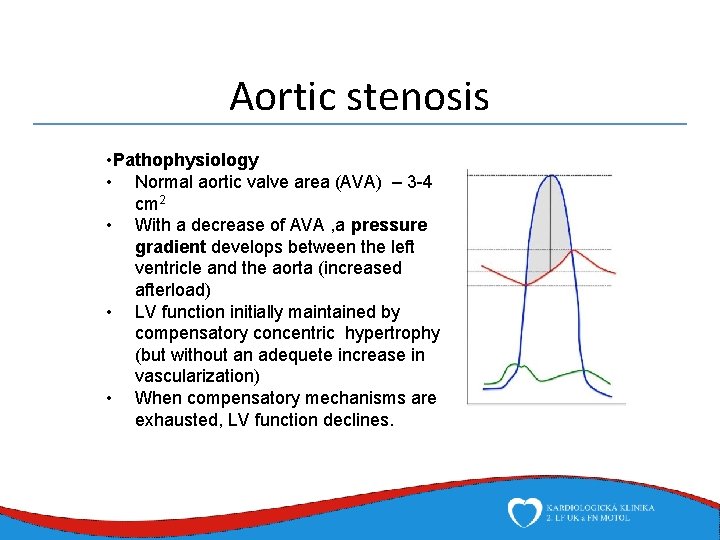
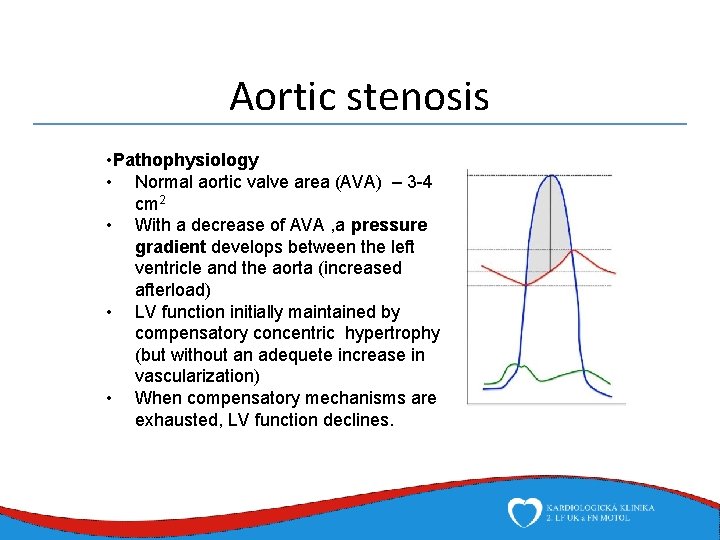
Aortic stenosis • Pathophysiology • Normal aortic valve area (AVA) – 3 -4 cm 2 • With a decrease of AVA , a pressure gradient develops between the left ventricle and the aorta (increased afterload) • LV function initially maintained by compensatory concentric hypertrophy (but without an adequete increase in vascularization) • When compensatory mechanisms are exhausted, LV function declines.
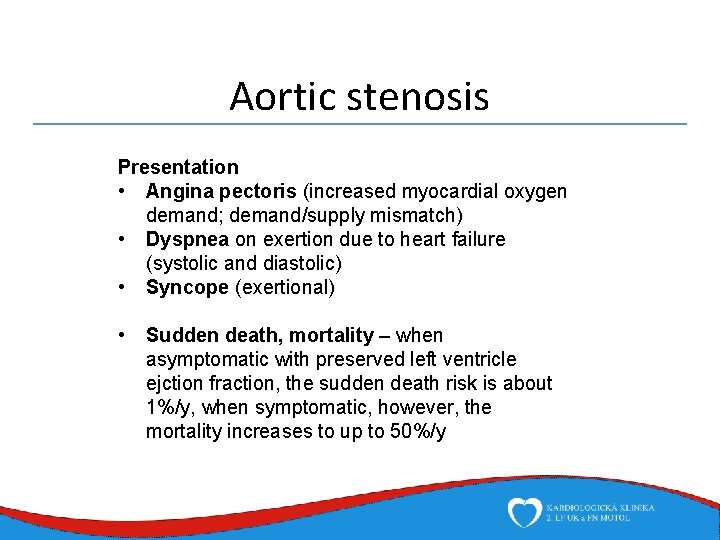
Aortic stenosis Presentation • Angina pectoris (increased myocardial oxygen demand; demand/supply mismatch) • Dyspnea on exertion due to heart failure (systolic and diastolic) • Syncope (exertional) • Sudden death, mortality – when asymptomatic with preserved left ventricle ejction fraction, the sudden death risk is about 1%/y, when symptomatic, however, the mortality increases to up to 50%/y
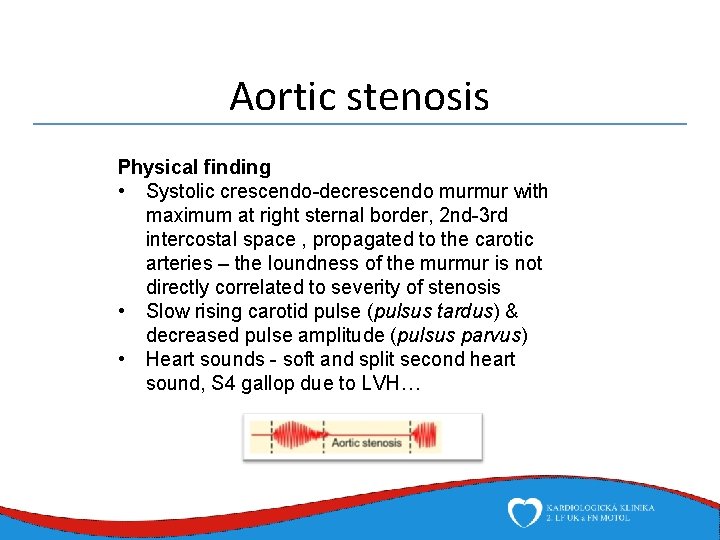
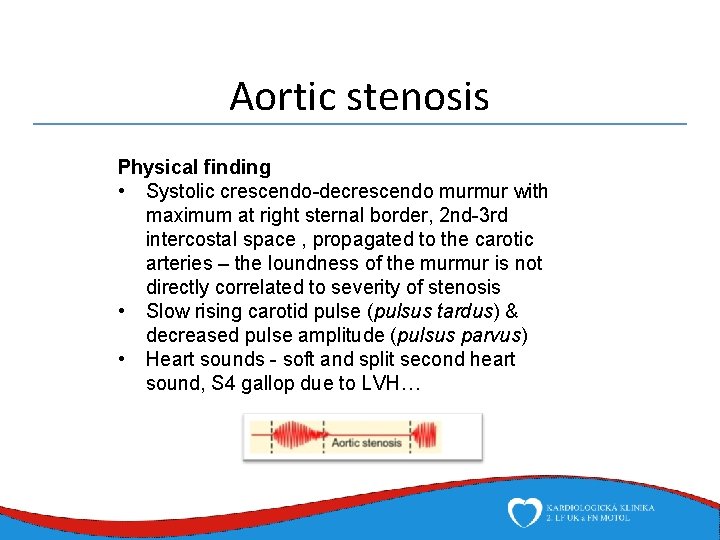
Aortic stenosis Physical finding • Systolic crescendo-decrescendo murmur with maximum at right sternal border, 2 nd-3 rd intercostal space , propagated to the carotic arteries – the loundness of the murmur is not directly correlated to severity of stenosis • Slow rising carotid pulse (pulsus tardus) & decreased pulse amplitude (pulsus parvus) • Heart sounds - soft and split second heart sound, S 4 gallop due to LVH…
Aortic stenosis Therapy – medical therapy has no prognostic effect • Aortic valve replacement • Standard therapy for patients with low surgical risk or with indication for other procedure • Mechanical/biological prosthesis • TAVI (transcatheter aortic valve implantation) – patiens at unaccaptable surgical risk (elderly, comorbid) • Percutaneous aortic balloon valvuloplasty (for congenital stenosis, or as a bridging therapy for unstable patients)
Aortic stenosis Indication for replacement • Severe aortic stenosis (AVA <1 cm 2, mean PG > 40 mm. Hg) • Symptomatic • LV function decreases • Other indication for surgery • Moderate stenosis (AVA 1, 5 -1 cm 2 ) • With other indication for surgery
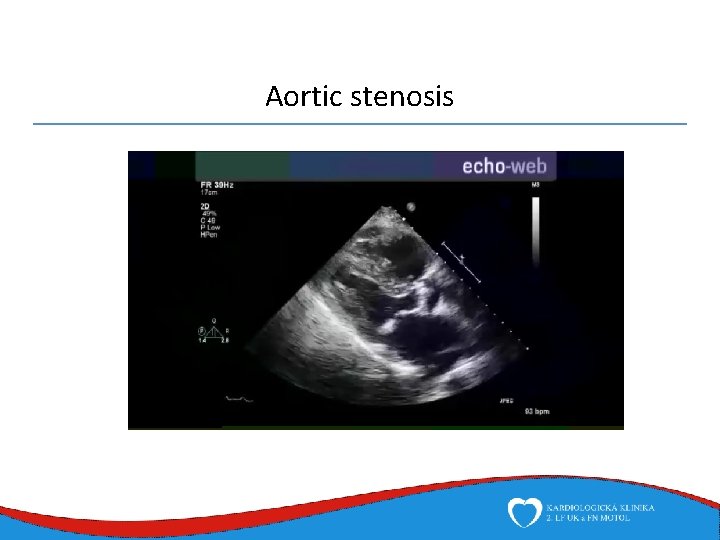
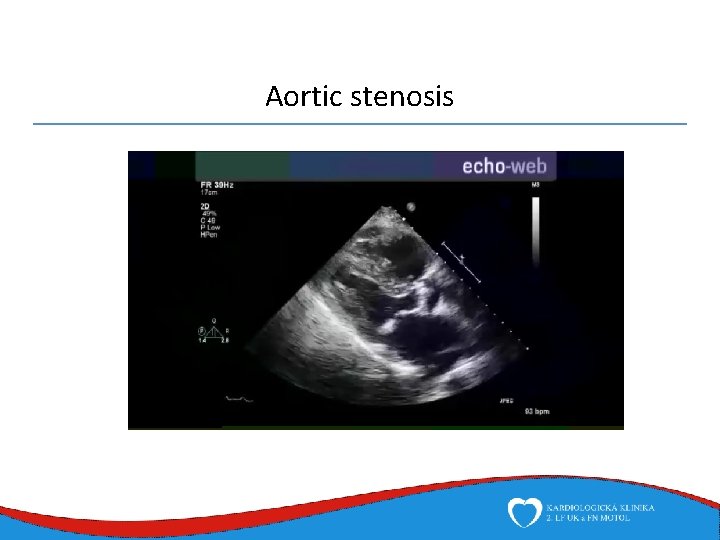
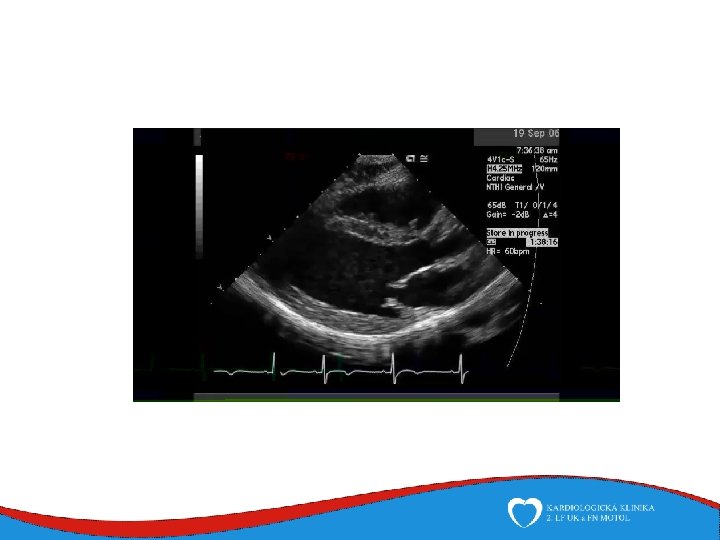
Aortic stenosis
Aortic regurgitation • Causes • Chronic aortic regurgitation • Bicuspid aortic valve • Rheumatic and degenerative – always with some degree of stenosis • Aortic root dilation (hypertension, Marfan’s, Ehlers. Danlos, syphylitic aortopathy) • Other rare causes (SLE, RA) • Acute aortic regurgiation • Infective endocarditis • Aortic regurgitation
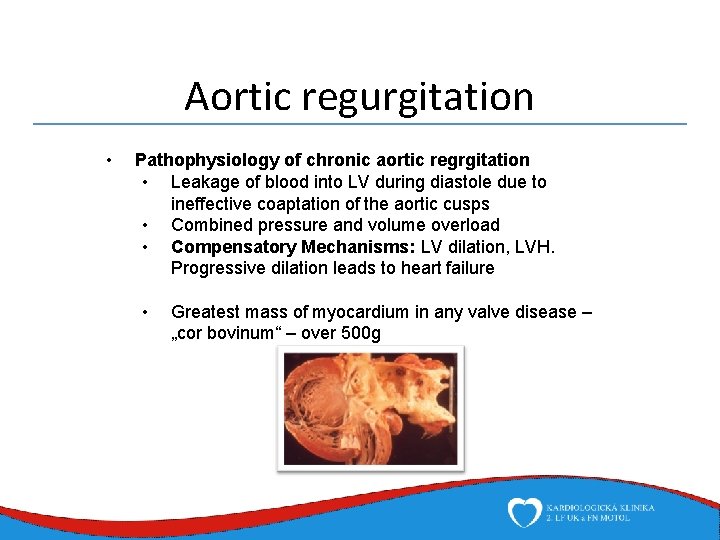
Aortic regurgitation • Pathophysiology of chronic aortic regrgitation • Leakage of blood into LV during diastole due to ineffective coaptation of the aortic cusps • Combined pressure and volume overload • Compensatory Mechanisms: LV dilation, LVH. Progressive dilation leads to heart failure • Greatest mass of myocardium in any valve disease – „cor bovinum“ – over 500 g
Aortic regurgitation • Presentation • Dyspnea: exertional, orthopnea, and paroxsymal nocturnal dyspnea • Chest pain • Fatigue • Palpitations: due to increased force of contraction or arrytmias
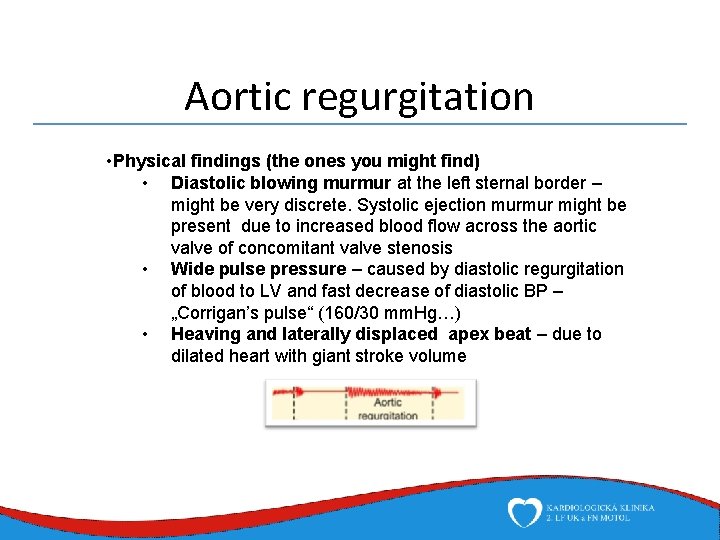
Aortic regurgitation • Physical findings (the ones you might find) • Diastolic blowing murmur at the left sternal border – might be very discrete. Systolic ejection murmur might be present due to increased blood flow across the aortic valve of concomitant valve stenosis • Wide pulse pressure – caused by diastolic regurgitation of blood to LV and fast decrease of diastolic BP – „Corrigan’s pulse“ (160/30 mm. Hg…) • Heaving and laterally displaced apex beat – due to dilated heart with giant stroke volume
Aortic regurgitation • Physical findings (the ones you might not find…) • Quincke’s sign - pulsations of nail bed • Muller’s sign - pulsation of uvula • De Musset sign - (head nodding in time with the heart beat) • Duroziez sign (systolic and diastolic murmurs heard over the femoral artery when it is gradually compressed with the stethoscope) • Austin Flint murmur (apex): Regurgitant jet impinges on anterior MVL causing it to vibrate

Aortic regurgitation • Acute aortic regurgitation • Caused by a leaflet perforation in infective endocarditis • In aortic dissection due to a change in aortic root geometry – dilation, extensive intimal tear with prolapse into LVOT and coaptation impairment • Presentation of acute aortic regurgitation itself is usually a pulmonary oedema accompanied by symptoms of the causing pathology • True emergency – mostly requires immediate cardiac surgery
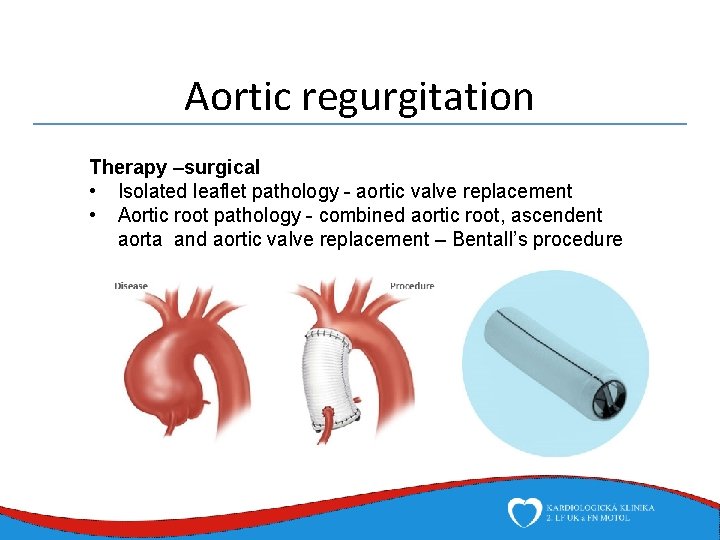
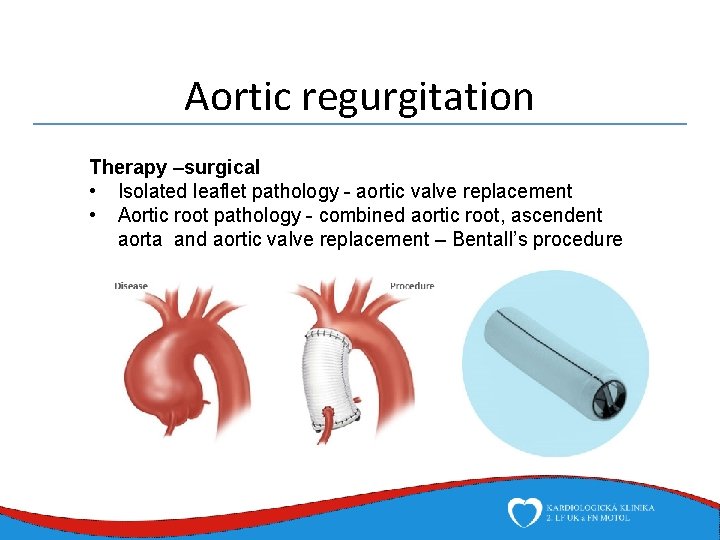
Aortic regurgitation Therapy –surgical • Isolated leaflet pathology - aortic valve replacement • Aortic root pathology - combined aortic root, ascendent aorta and aortic valve replacement – Bentall’s procedure
Aortic regurgitation Indication for replacement • Severe aortic regurgitation (EROA – effective regurgitant orifice area >0, 3 cm 2) • Symptomatic • LV dilates (over 50 mm EDD) or function decreases (EF < 55%) • Other indication for surgery • Acute • Moderate regurgitation (AVA 1, 5 -1 cm 2 ) • With other indication for surgery
Mitral stenosis • Causes • Rheumatic heart disease in up to 99% of all cases • Other causes are rare - mitral annular calcification, obstruction with massive endocarditis vegetations, left atrial myxoma, post radiation • Nowadays rare in developed countries, still prevalent in developing countries due to rheumatic fever
Mitral stenosis • Pathophysiology: • Normal mitral valve area 4 -6 cm 2 – stenosis becomes severe with MVA < 1 cm 2 • Increased transmitral pressure gradient: leads to left atrial pressure increase, enlargement and atrial fibrillation → • Development of postcapillary pulmonary hypertension (there is no valve to isolate the increased left atrial pressure from pulmonary veins) → • Right heart failure symptoms - due to pulmonary HT, secondary right ventricle dilation and tricuspid regurgitation
Mitral stenosis Presentation • Dyspnea • Syncope • Palpitations (atrial fibrilation is common) • In advanced cases - right heart failure symptoms – periferal oedema, increased JVP, hepatomegaly, ascites…
Mitral stenosis Physical finding • Diastolic murmur • Low-pitched diastolic rumble most prominent at the apex. • Heard best with the patient lying on the left side in held expiration • Intensity of the diastolic murmur does not correlate with the severity of the stenosis • Lung crackles • Pleural effusion • Facies mitralis: When MS is severe and the cardiac output is diminished, there is vasoconstriction, resulting in pinkishpurple patches on the cheeks (might be seen in terminal heart failure of any cause)

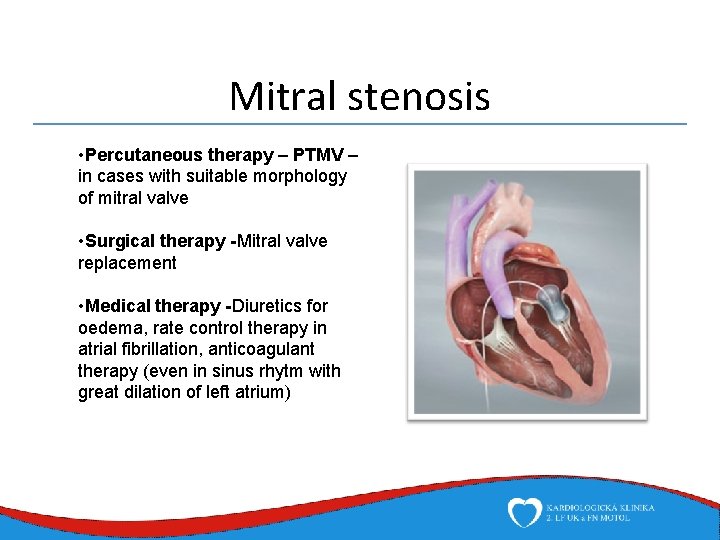
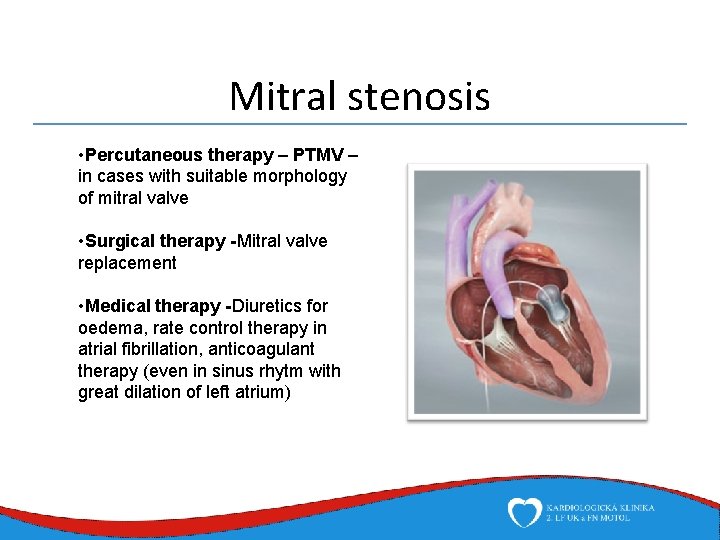
Mitral stenosis • Percutaneous therapy – PTMV – in cases with suitable morphology of mitral valve • Surgical therapy -Mitral valve replacement • Medical therapy -Diuretics for oedema, rate control therapy in atrial fibrillation, anticoagulant therapy (even in sinus rhytm with great dilation of left atrium)



Mitral regurgitation Causes • Primary mitral regurgitation („valve is the pathology“) impairment of the valve itself, the cords or the papilary muscles • Myxomatous degeneration (Barlow valve disease) • Leaflet prolapse (in Barlow disease or in normal valve with cord rupture) • Infective endocarditis • Rheumatic valve disease • Secondary mitral regurgitation („left ventricle it the pathology“) – impairment of left ventricle function and geometry • Ischemic heart disease • Dilated cardiomyopathy • Hypertrophic cardiomyopathy • Aortic valve disease
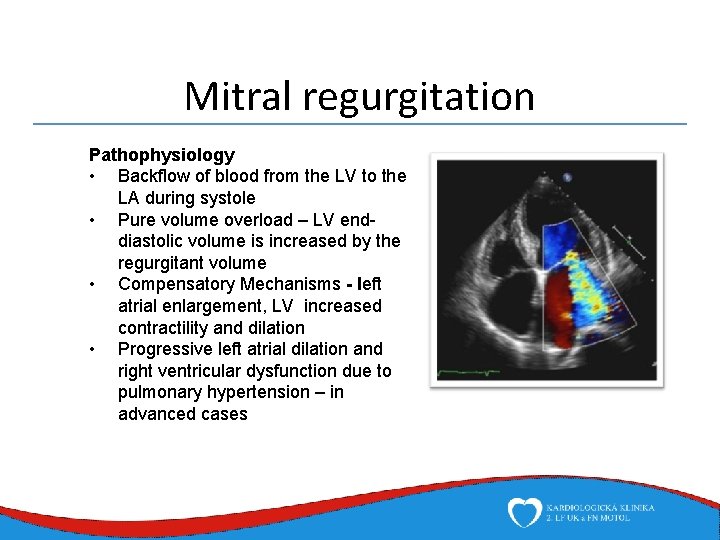
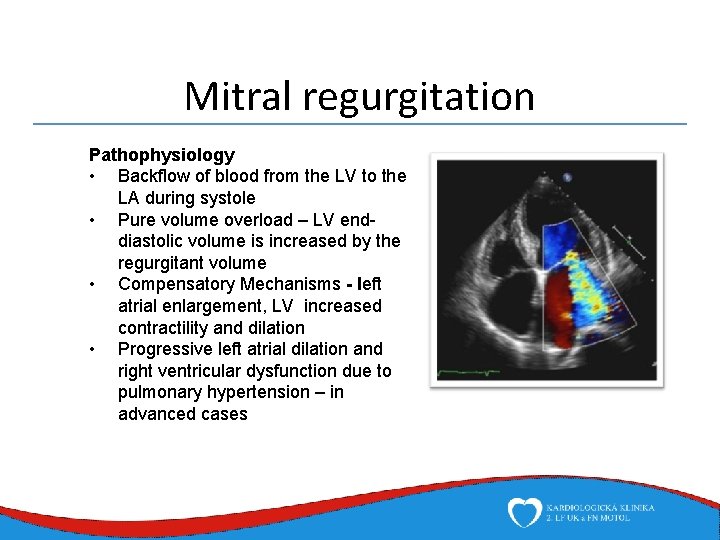
Mitral regurgitation Pathophysiology • Backflow of blood from the LV to the LA during systole • Pure volume overload – LV enddiastolic volume is increased by the regurgitant volume • Compensatory Mechanisms - left atrial enlargement, LV increased contractility and dilation • Progressive left atrial dilation and right ventricular dysfunction due to pulmonary hypertension – in advanced cases
Mitral regurgitation Presentation • Very long period of asymptomatic progresion • Exertional dyspnea, fatigue Physical finding • Holosystolic murmur best heard at heart apex with propagation to axilla • In case of mitral leaflet prolaps, a systolic click might be heard
Mitral regurgitation Therapy • Difers greatly according to the cause • Primary • Mitral valve repair – preserving the valve with surgically correcting the cause of regurgitation – ruptured cords replaced with artificial (Gore Tex) cords, resection of redundant leaflet tissue • Mitral valve replacement • Secondary • Treating the cause of ventricular dysfunction • Medical, device therapy - in dilated CMP, revascularization with annuloplasty in ischemic heart disease
Mitral regurgitation Acute mitral regurgitation • Causes • Cord rupture • Infective endocarditis – leaflet perforation, cord rupture, perivalvular fistula, absces • Papillary muscle rupture (mechanical complication of myocardial infarction, high force chest trauma) • Presentation • Acute heart failure – cardiogenic shock, pulmonary oedema • Management • Diuretics, nitrates, IABC → emergency surgery
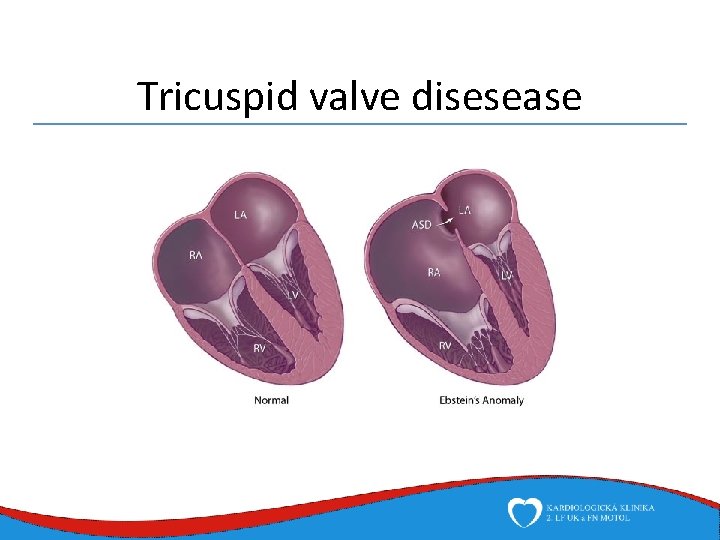
Tricuspid valve disesease • Tricuspid regurgitation • Is usually secondary – due to right ventricle dilation and failure as a result of pumonary hypertension (the most common cause of right heart failure is left heart failure) or volume overload (left-right shunt abnormalities) • Cor pulmonale – right ventricle failure in pulmonary disease • Primary: • Infective endocarditis – in i. v. abusers • Other are rare - Carcinoid, rheumatic, Ebstein anomaly – apical displacement of septal and posterior leaflet of tricuspid valve → „atrialization“ of a portion of the morphologic right ventricle • Symptoms of right heart failure – periferal oedema, elevated JVP, hepatomegaly, ascites… • Symptoms treated by diuretics, surgical treatment is only indicated in case of left sided valve intervention
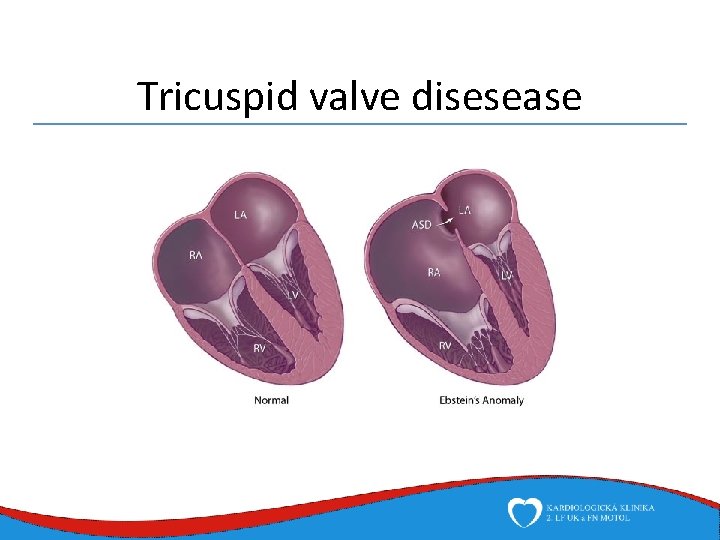
Tricuspid valve disesease
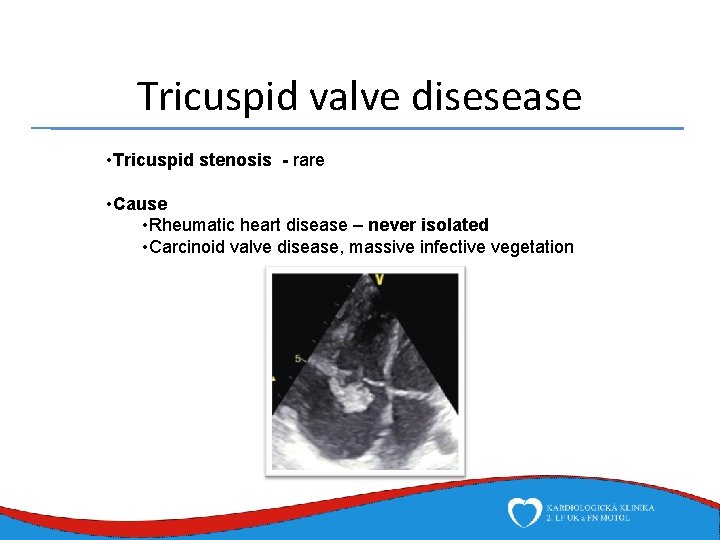
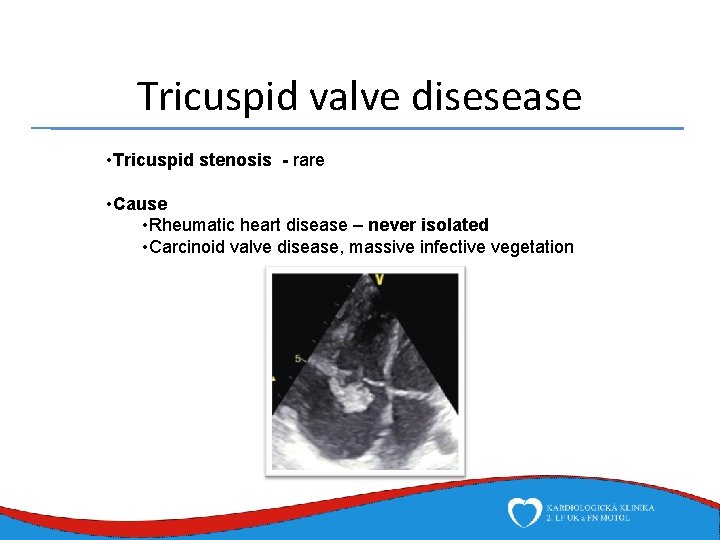
Tricuspid valve disesease • Tricuspid stenosis - rare • Cause • Rheumatic heart disease – never isolated • Carcinoid valve disease, massive infective vegetation
Pulmonic valve disesease • Isolated severe pulmonic valve diseases are extremely rare • Pulmonic stenosis – congenital • Systolic murmur at left sternal border, with possible interscapulary propagation • Pulmonic regurgitation – might be a result of pulmonary hypertension, usually no treatment
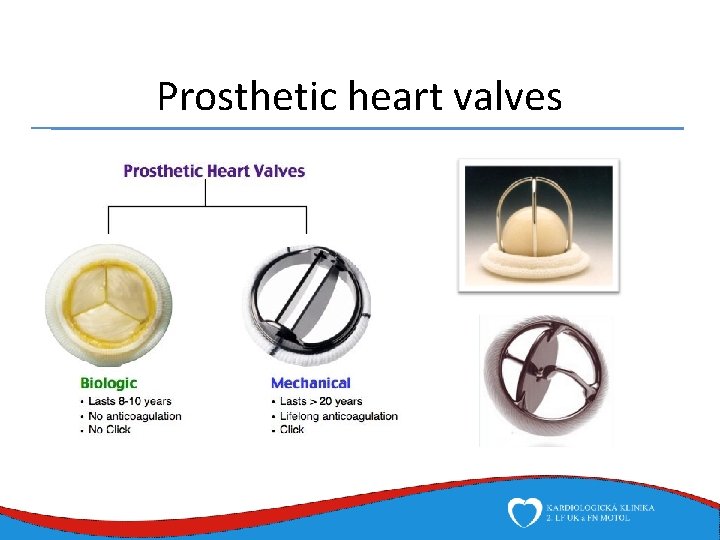
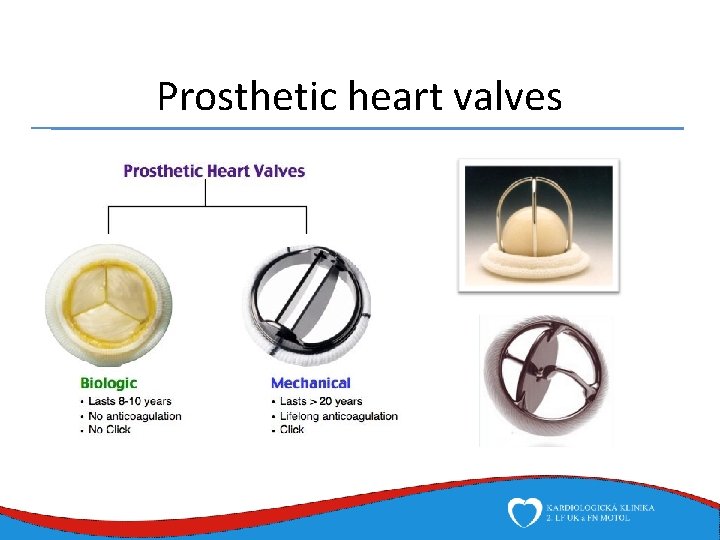
Prosthetic heart valves
