Valvular Heart Disease and the Cardiac Exam 2009













- Slides: 42
Valvular Heart Disease and the Cardiac Exam 2009

Overview n n n Clinical syndromes Overview of cardiac murmurs and maneuvers Left sided valvular lesions – Aortic stenosis and sclerosis – Mitral stenosis § Rheumatic fever prophylaxis – Acute and chronic aortic regurgitation – Acute and chronic mitral regurgitation n Right sided valvular lesions n n n Prosthetic valves Endocarditis prophylaxis Questions – Tricuspid valve disease
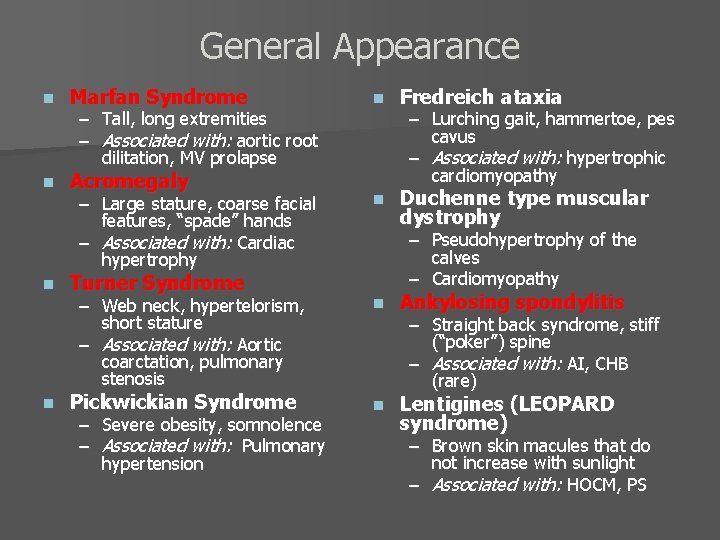
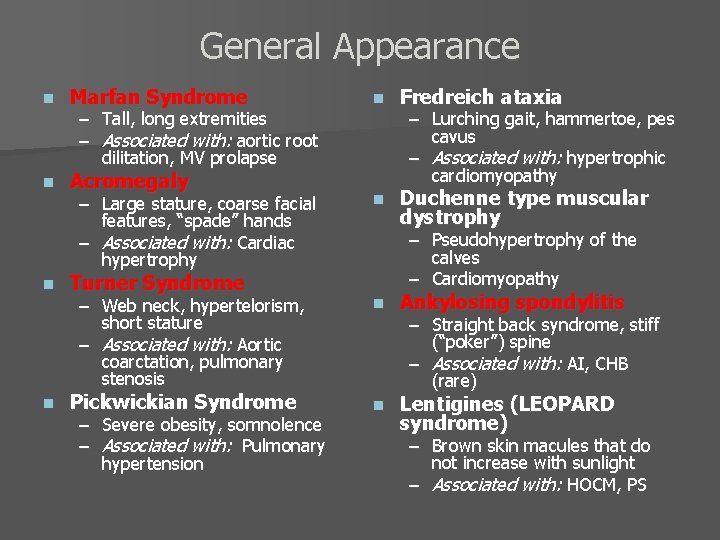
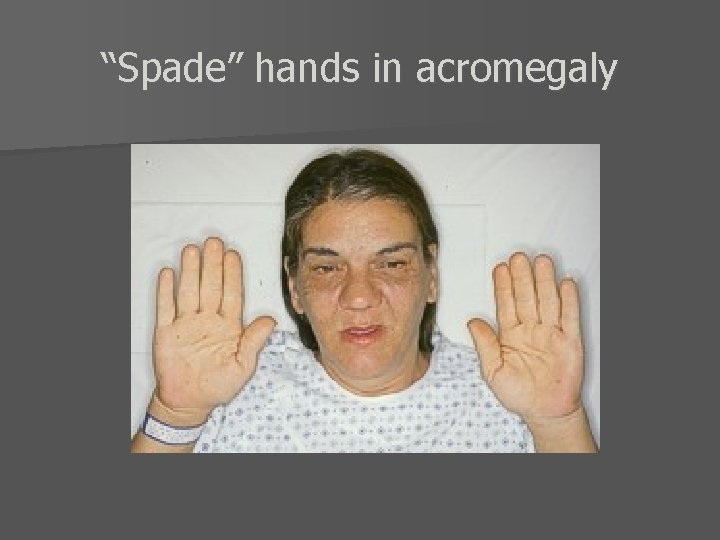
General Appearance n Marfan Syndrome n Acromegaly n n n Fredreich ataxia – Large stature, coarse facial features, “spade” hands – Associated with: Cardiac hypertrophy n Duchenne type muscular dystrophy – Web neck, hypertelorism, short stature – Associated with: Aortic coarctation, pulmonary stenosis n Ankylosing spondylitis n Lentigines (LEOPARD syndrome) – Tall, long extremities – Associated with: aortic root dilitation, MV prolapse Turner Syndrome Pickwickian Syndrome – Severe obesity, somnolence – Associated with: Pulmonary hypertension – Lurching gait, hammertoe, pes cavus – Associated with: hypertrophic cardiomyopathy – Pseudohypertrophy of the calves – Cardiomyopathy – Straight back syndrome, stiff (“poker”) spine – Associated with: AI, CHB (rare) – Brown skin macules that do not increase with sunlight – Associated with: HOCM, PS
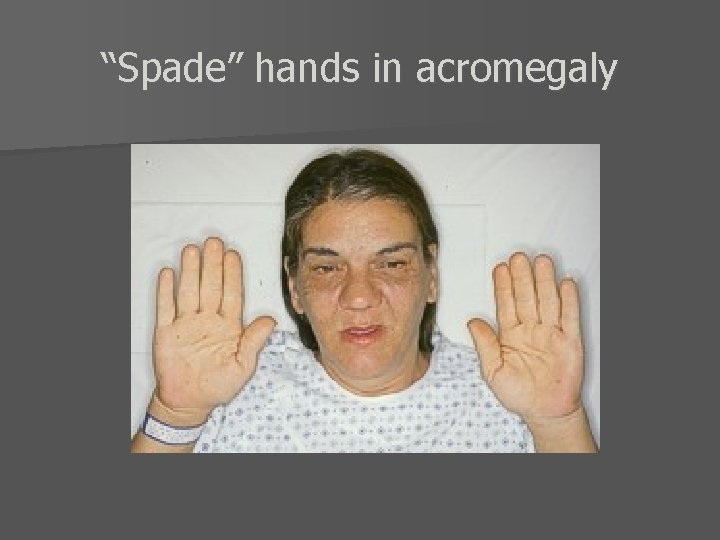
“Spade” hands in acromegaly

General Appearance- 2 n Hereditary hemorrhagic telangiectasia (Osler. Weber-Rendu) – Small capillary hemangiomas on the face or mouth – Associated with: Pulmonary arteriovenous fistula n n n Sarcoidosis n Tuberous Sclerosis n Myxedema Lupus – Butterfly rash on face, Raynaud phenomenon- hands, Livedo reticularis – Associated with: Verrucous endocarditis, Myocarditis, Pericarditis Pheochromocytoma – Pale diaphoretic skin, neurofibromatosis- café-au-lait spots – Associated with: Catecholamine-induced secondary dilated CM – Cutaneous nodules, erythema nodosum – Associated with: Secondary cardiomyopathy, heart block – Angiofibromas (face; adenoma sebaceum) – Associated with: Rhabdomyoma – Coarse, dry skin, thinning of lateral eyebrows, hoarseness of voice – Associated with: Pericardial effusion, LV dysfunction
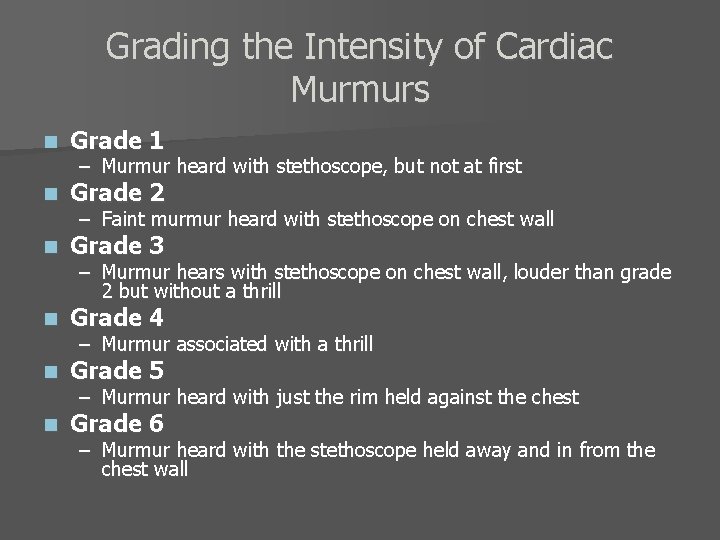
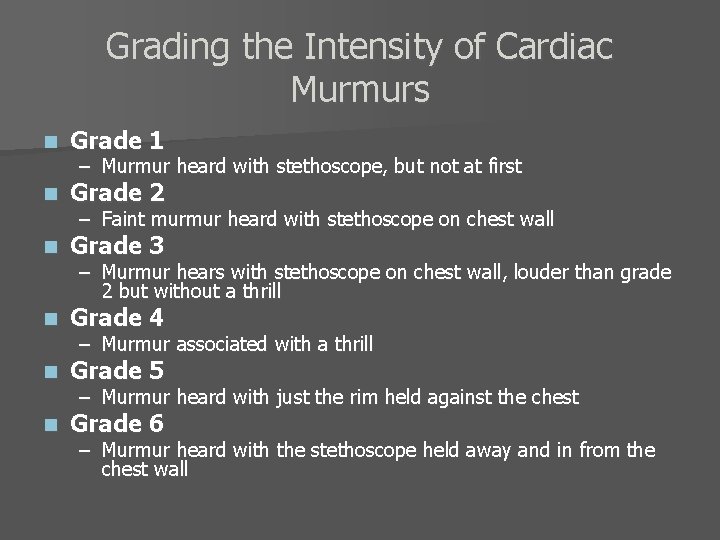
Grading the Intensity of Cardiac Murmurs n Grade 1 n Grade 2 n Grade 3 n Grade 4 n Grade 5 n Grade 6 – Murmur heard with stethoscope, but not at first – Faint murmur heard with stethoscope on chest wall – Murmur hears with stethoscope on chest wall, louder than grade 2 but without a thrill – Murmur associated with a thrill – Murmur heard with just the rim held against the chest – Murmur heard with the stethoscope held away and in from the chest wall

Cardiac Murmurs n Most mid systolic murmurs of grade 2/6 intensity or less are benign – Associated with physiologic increases in blood velocity: § Pregnancy § Elderly n In contrast, the following murmurs are usually pathologic: – Systolic murmurs grade 3/6 or greater in intensity – Continuous murmurs – Any diastolic murmur
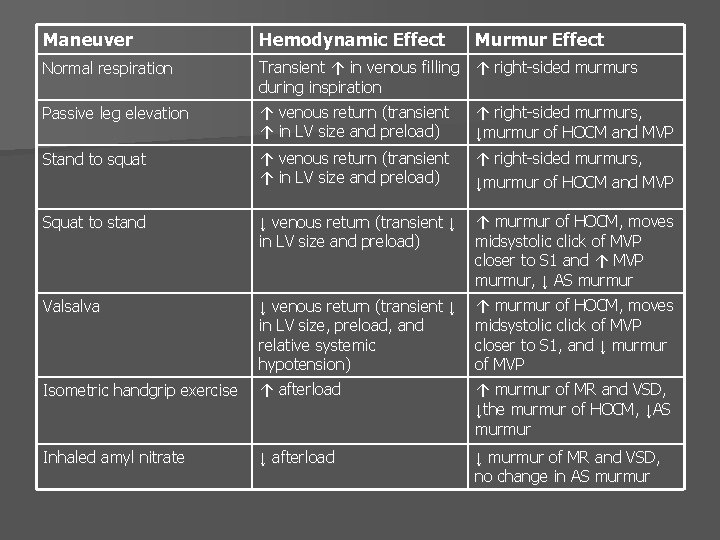
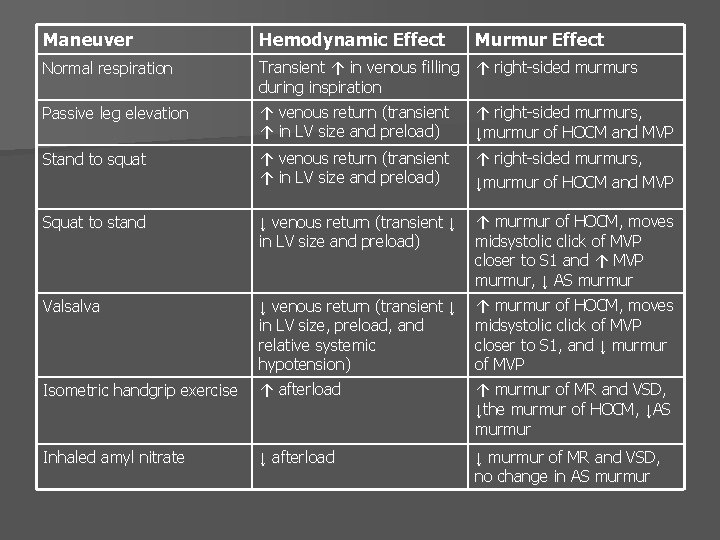
Maneuver Hemodynamic Effect Murmur Effect Normal respiration Transient ↑ in venous filling ↑ right-sided murmurs during inspiration Passive leg elevation ↑ venous return (transient ↑ in LV size and preload) ↑ right-sided murmurs, ↓murmur of HOCM and MVP Stand to squat ↑ venous return (transient ↑ in LV size and preload) ↑ right-sided murmurs, ↓murmur of HOCM and MVP Squat to stand ↓ venous return (transient ↓ in LV size and preload) ↑ murmur of HOCM, moves midsystolic click of MVP closer to S 1 and ↑ MVP murmur, ↓ AS murmur Valsalva ↓ venous return (transient ↓ in LV size, preload, and relative systemic hypotension) ↑ murmur of HOCM, moves midsystolic click of MVP closer to S 1, and ↓ murmur of MVP Isometric handgrip exercise ↑ afterload ↑ murmur of MR and VSD, ↓the murmur of HOCM, ↓AS murmur Inhaled amyl nitrate ↓ afterload ↓ murmur of MR and VSD, no change in AS murmur
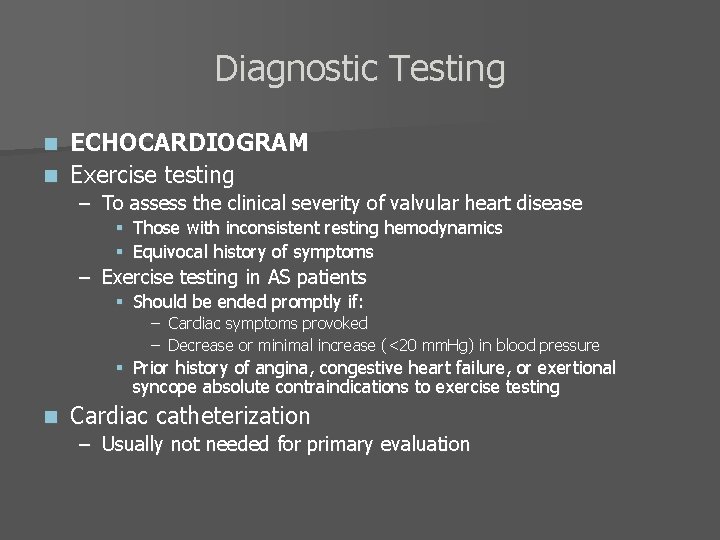
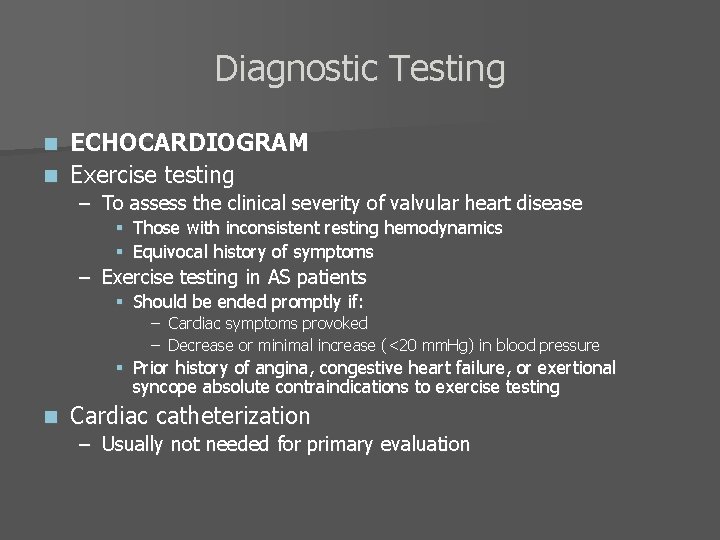
Diagnostic Testing ECHOCARDIOGRAM n Exercise testing n – To assess the clinical severity of valvular heart disease § Those with inconsistent resting hemodynamics § Equivocal history of symptoms – Exercise testing in AS patients § Should be ended promptly if: – Cardiac symptoms provoked – Decrease or minimal increase (<20 mm. Hg) in blood pressure § Prior history of angina, congestive heart failure, or exertional syncope absolute contraindications to exercise testing n Cardiac catheterization – Usually not needed for primary evaluation
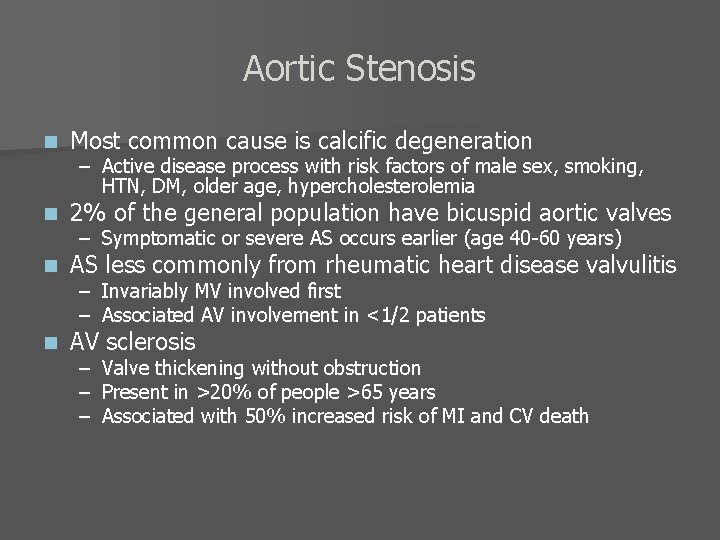
Aortic Stenosis n Most common cause is calcific degeneration n 2% of the general population have bicuspid aortic valves n AS less commonly from rheumatic heart disease valvulitis n AV sclerosis – Active disease process with risk factors of male sex, smoking, HTN, DM, older age, hypercholesterolemia – Symptomatic or severe AS occurs earlier (age 40 -60 years) – Invariably MV involved first – Associated AV involvement in <1/2 patients – Valve thickening without obstruction – Present in >20% of people >65 years – Associated with 50% increased risk of MI and CV death
Progression of Aortic Sclerosis n Hemodynamic progression usually slow – Average rate of increase in aortic jet velocity of 0. 3 m/s per year – Increase in mean transaortic gradient of 7 mm. Hg – Decrease in AVA of 0. 1 cm 2 per year n Severe AS – Aortic jet velocity > 4 m/s – Mean transvalvular pressure gradient > 50 mm. Hg – AVA < 1. 0 cm 2
Pathophysiology of Aortic Stenosis Obstruction of LV outflow increases intracavitary systolic pressures and leads to LV pressure overload n Initial compensatory mechanism is myocardial hypertrophy with preservation of systolic function n Diastolic function impaired as a consequence of increased wall thickness and abnormal myocardial relaxation n Increased wall stress and afterload causes eventual decrease in ejection fraction n
Pseudostenosis n Occurs in patients with impaired systolic function and aortic stenosis – Unable to generate transvalvular gradient Careful diagnostic testing with dobutamine infusion protocols can aid in differentiating between true AS and pseudostenosis n If the calculated AVA increases with augmentation of cardiac output, then pseudostenosis present n If AVA does not increase with dobutamine, then obstruction fixed and true AS present n

Clinical Presentation of Aortic Stenosis n Cardinal symptoms: – Angina § Occurs in >50% of patients, not sensitive due to prevalence of CAD – Syncope – CHF n n Sudden cardiac death rare, <1% per year In earlier stages, AS presentation more subtle n Rarely, AS diagnosed in the setting of GI bleeding – Dyspnea – Decreased exercise tolerance – Heyde’s syndrome § Bleeding caused by AVM § Concurrent AS occurs at prevalence rate of 15 -25% § Associated with an acquired von Willebrand syndrome due to disruption of v. W multimers through a diseased AV
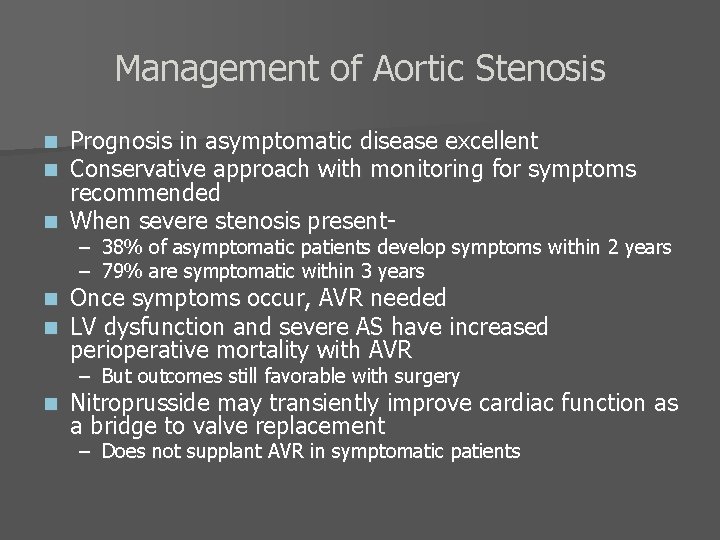
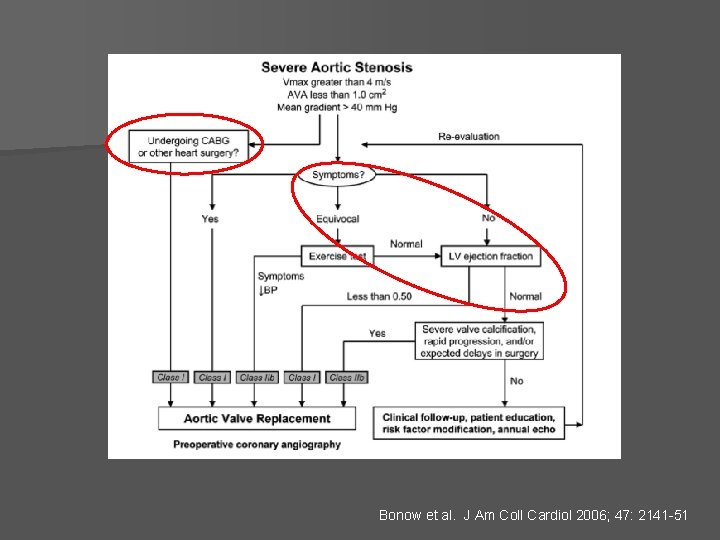
Management of Aortic Stenosis Prognosis in asymptomatic disease excellent Conservative approach with monitoring for symptoms recommended n When severe stenosis presentn n – 38% of asymptomatic patients develop symptoms within 2 years – 79% are symptomatic within 3 years n n Once symptoms occur, AVR needed LV dysfunction and severe AS have increased perioperative mortality with AVR – But outcomes still favorable with surgery n Nitroprusside may transiently improve cardiac function as a bridge to valve replacement – Does not supplant AVR in symptomatic patients
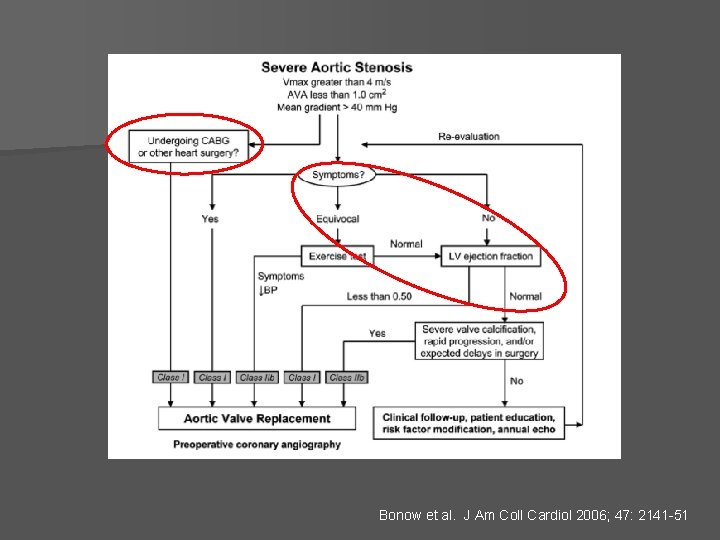
Bonow et al. J Am Coll Cardiol 2006; 47: 2141 -51
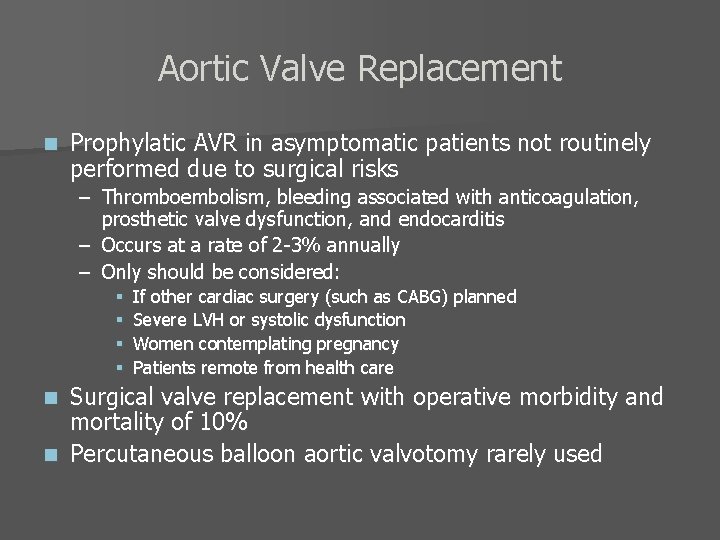
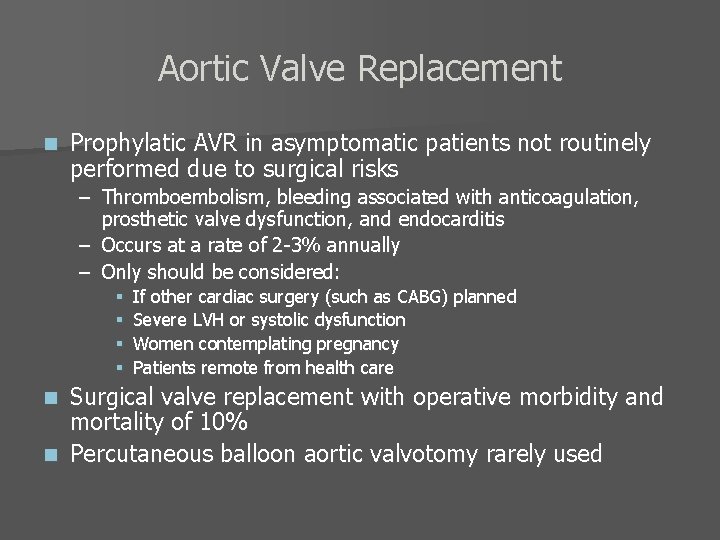
Aortic Valve Replacement n Prophylatic AVR in asymptomatic patients not routinely performed due to surgical risks – Thromboembolism, bleeding associated with anticoagulation, prosthetic valve dysfunction, and endocarditis – Occurs at a rate of 2 -3% annually – Only should be considered: § § If other cardiac surgery (such as CABG) planned Severe LVH or systolic dysfunction Women contemplating pregnancy Patients remote from health care Surgical valve replacement with operative morbidity and mortality of 10% n Percutaneous balloon aortic valvotomy rarely used n
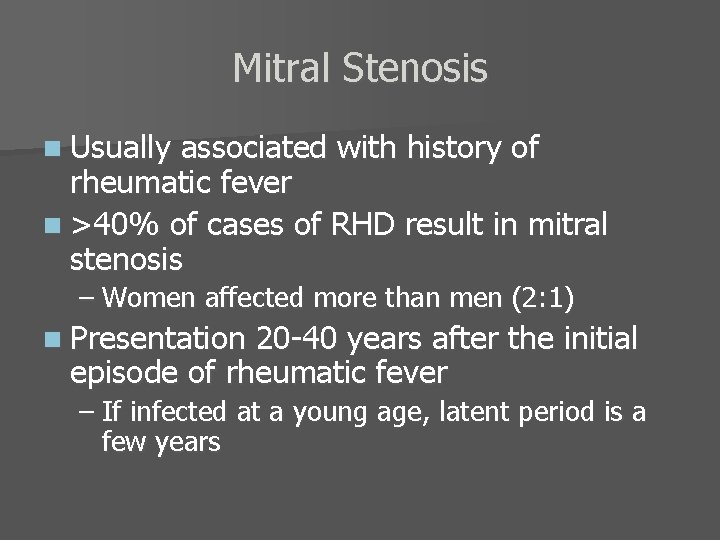
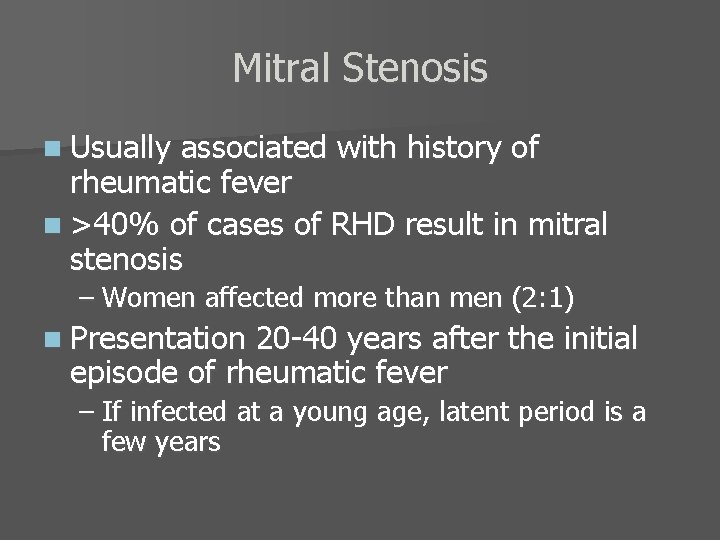
Mitral Stenosis n Usually associated with history of rheumatic fever n >40% of cases of RHD result in mitral stenosis – Women affected more than men (2: 1) n Presentation 20 -40 years after the initial episode of rheumatic fever – If infected at a young age, latent period is a few years

Clinical Presentation of Mitral Stenosis Significant MS leads to ↑LA pressure and pulm HTN n Symptoms include dyspnea with ↑ cardiac demand n – Exercise – Pregnancy n Survival excellent with asymptomatic or minimally symptomatic patients – >80% survival at 10 years n Survival in symptomatic patients much worse – 10 year survival drops to 15% or lower (if pulm HTN present) n Findings consistent with severe MS: – – – Transvalvular diastolic pressure gradient >10 mm. Hg MVA <1. 0 cm 2 Severe pulmonary hypertension (>60 mm. Hg)
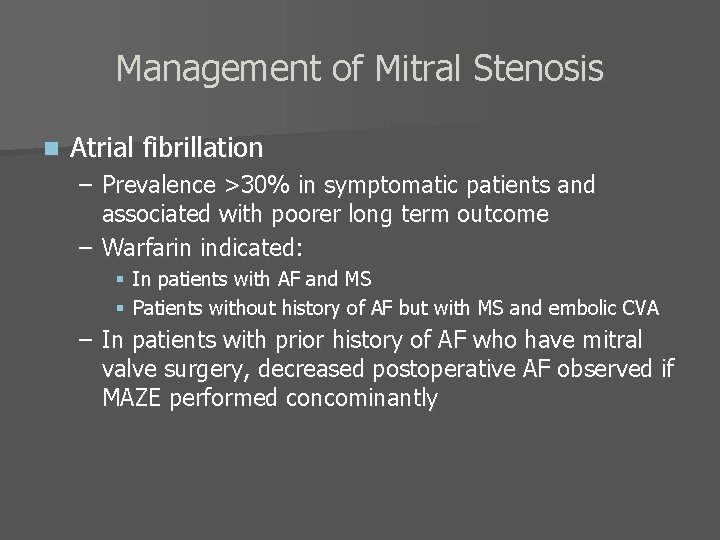
Management of Mitral Stenosis n Atrial fibrillation – Prevalence >30% in symptomatic patients and associated with poorer long term outcome – Warfarin indicated: § In patients with AF and MS § Patients without history of AF but with MS and embolic CVA – In patients with prior history of AF who have mitral valve surgery, decreased postoperative AF observed if MAZE performed concominantly

Mitral Valve Repair n Percutaneous valvotomy – Therapeutic intervention of choice if: § § § LAA thrombus excluded MR less than moderate Valvular characteristics favorable – Pliable leaflets, minimal commisural fusion, minimal valvular or subvalvular calcification – Pulmonary HTN not contraindication to valvotomy – Major complications include: severe MR (1 -8%), systemic embolization (1 -3%), and tamponade (12%) § Periprocedural mortality- 1% n Surgical commissurotomy or MVR can be performed in unfavorable anatomy

Bonow et al. J Am Coll Cardiol 2006; 47: 2141 -51
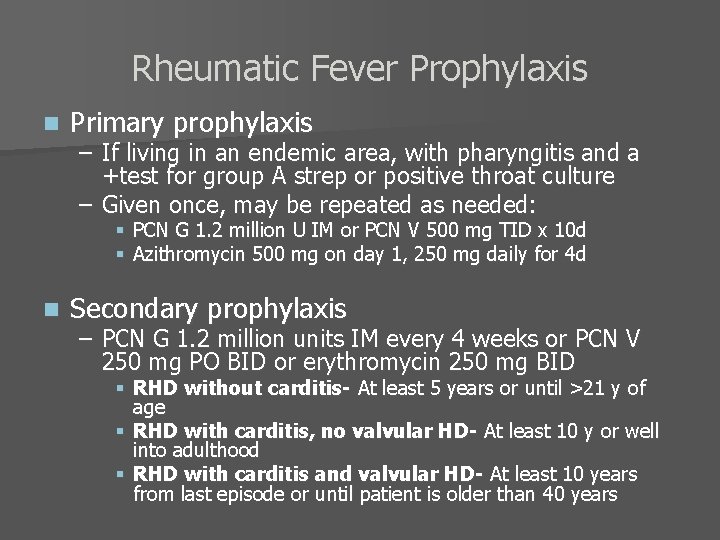
Rheumatic Fever Prophylaxis n Primary prophylaxis – If living in an endemic area, with pharyngitis and a +test for group A strep or positive throat culture – Given once, may be repeated as needed: § PCN G 1. 2 million U IM or PCN V 500 mg TID x 10 d § Azithromycin 500 mg on day 1, 250 mg daily for 4 d n Secondary prophylaxis – PCN G 1. 2 million units IM every 4 weeks or PCN V 250 mg PO BID or erythromycin 250 mg BID § RHD without carditis- At least 5 years or until >21 y of age § RHD with carditis, no valvular HD- At least 10 y or well into adulthood § RHD with carditis and valvular HD- At least 10 years from last episode or until patient is older than 40 years
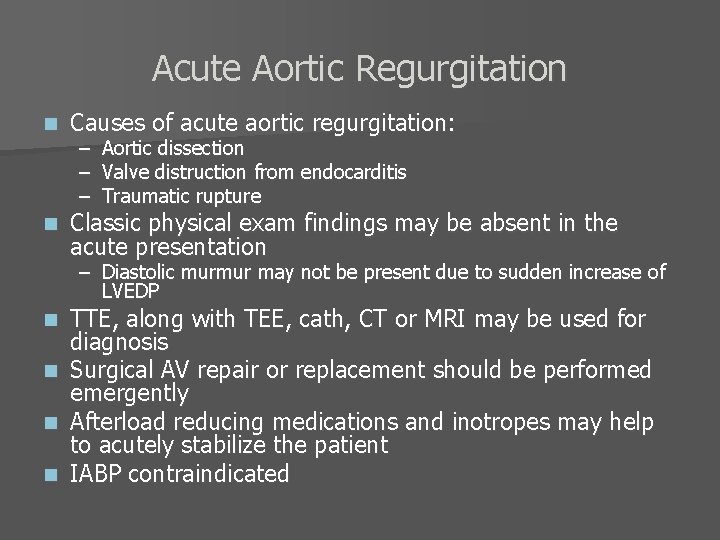
Acute Aortic Regurgitation n Causes of acute aortic regurgitation: n Classic physical exam findings may be absent in the acute presentation – – – Aortic dissection Valve distruction from endocarditis Traumatic rupture – Diastolic murmur may not be present due to sudden increase of LVEDP TTE, along with TEE, cath, CT or MRI may be used for diagnosis n Surgical AV repair or replacement should be performed emergently n Afterload reducing medications and inotropes may help to acutely stabilize the patient n IABP contraindicated n

Acute Mitral Regurgitation n Most often occurs in: n Symptoms almost always occur – Chordae tendineae rupture due to myxomatous valve disease or endocarditis – Myocardial infarction with papillary muscle dysfunction or rupture – Dyspnea and pulmonary edema Systolic function may occur normal or hyperdynamic n IABP or afterload reducing drugs to temporize n Surgical intervention for treatment n
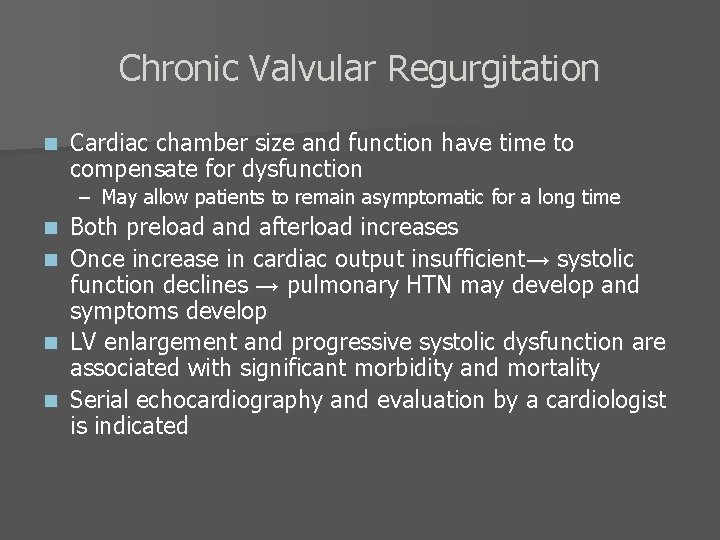
Chronic Valvular Regurgitation n Cardiac chamber size and function have time to compensate for dysfunction – May allow patients to remain asymptomatic for a long time n n Both preload and afterload increases Once increase in cardiac output insufficient→ systolic function declines → pulmonary HTN may develop and symptoms develop LV enlargement and progressive systolic dysfunction are associated with significant morbidity and mortality Serial echocardiography and evaluation by a cardiologist is indicated
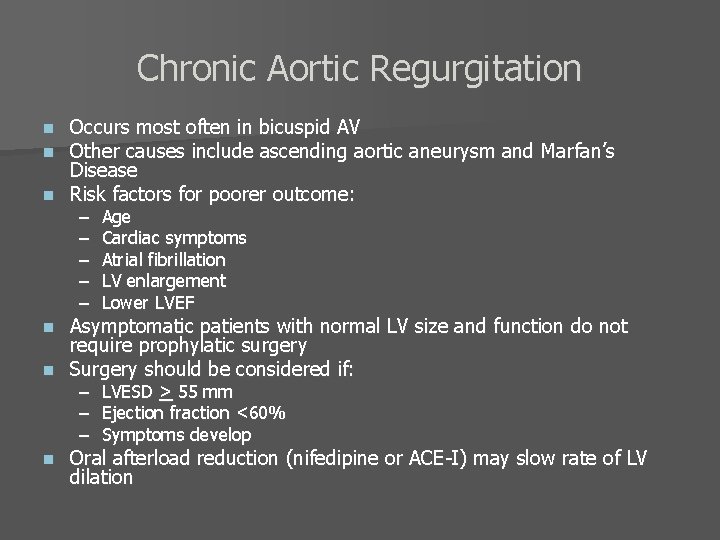
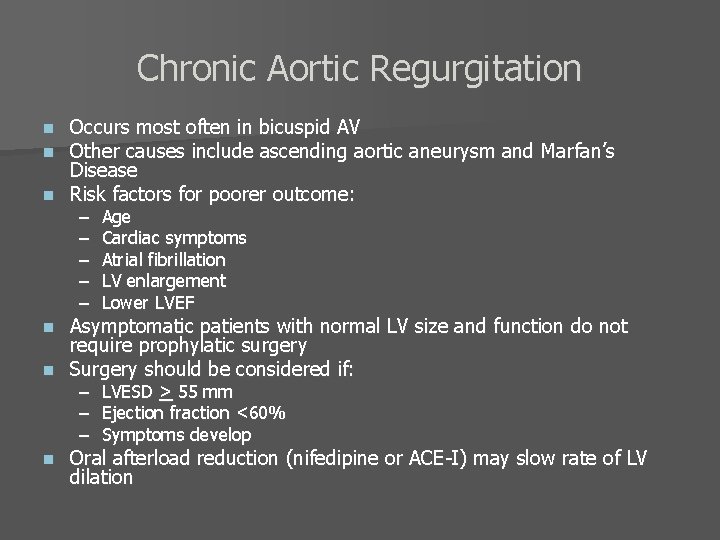
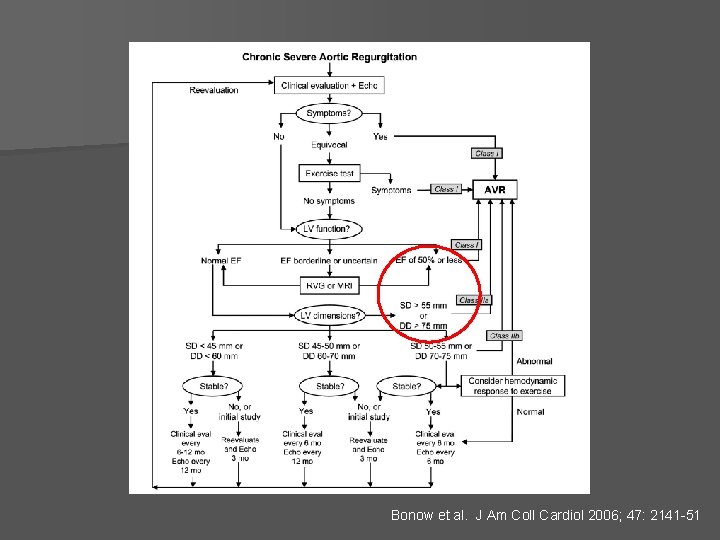
Chronic Aortic Regurgitation Occurs most often in bicuspid AV Other causes include ascending aortic aneurysm and Marfan’s Disease n Risk factors for poorer outcome: n n – – – Age Cardiac symptoms Atrial fibrillation LV enlargement Lower LVEF – – – LVESD > 55 mm Ejection fraction <60% Symptoms develop Asymptomatic patients with normal LV size and function do not require prophylatic surgery n Surgery should be considered if: n n Oral afterload reduction (nifedipine or ACE-I) may slow rate of LV dilation
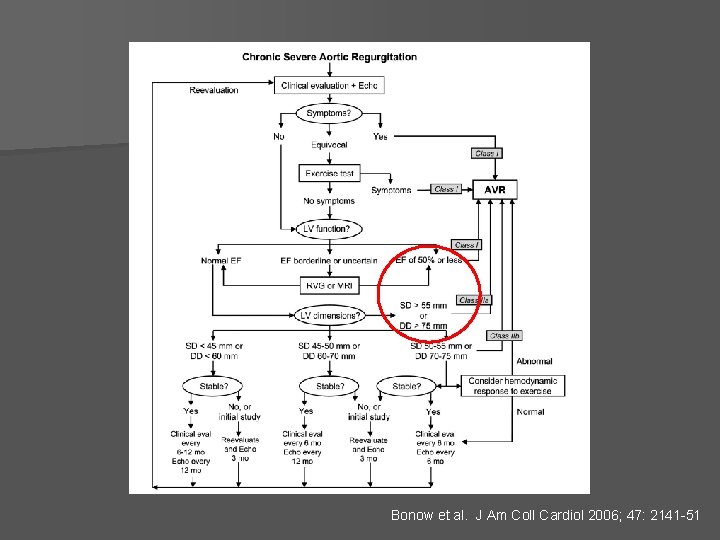
Bonow et al. J Am Coll Cardiol 2006; 47: 2141 -51

Chronic Mitral Regurgitation n Often caused by myxomatous disease or MVP – Myxomatous mitral valve disease with progressive MR associated with poor long term outcome § Higher risk of arrhythmias and sudden cardiac death – Mitral valve prolapse occurs in ~2% of the general population § Consists of the buckling of the mid portion of the valve leaflets into the LA § Usually asymptomatic, but may be associated with palpitations or chest discomfort § Prognosis usually benign § Antibiotic prophylaxis now not indicated
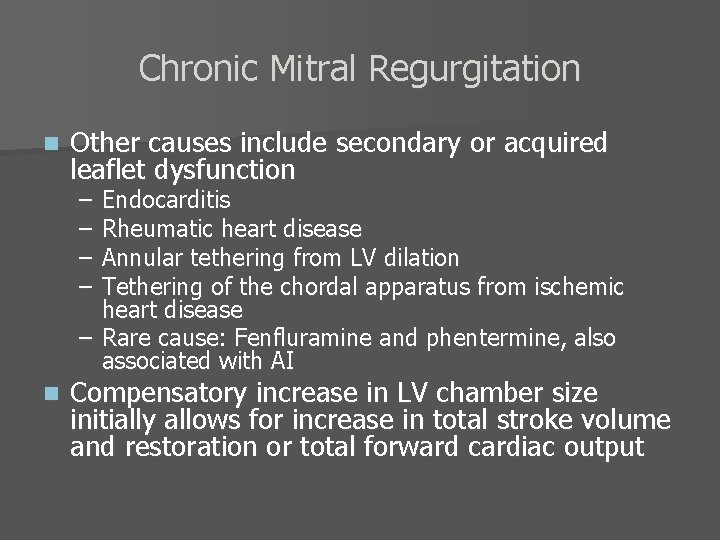
Chronic Mitral Regurgitation n Other causes include secondary or acquired leaflet dysfunction – – Endocarditis Rheumatic heart disease Annular tethering from LV dilation Tethering of the chordal apparatus from ischemic heart disease – Rare cause: Fenfluramine and phentermine, also associated with AI n Compensatory increase in LV chamber size initially allows for increase in total stroke volume and restoration or total forward cardiac output
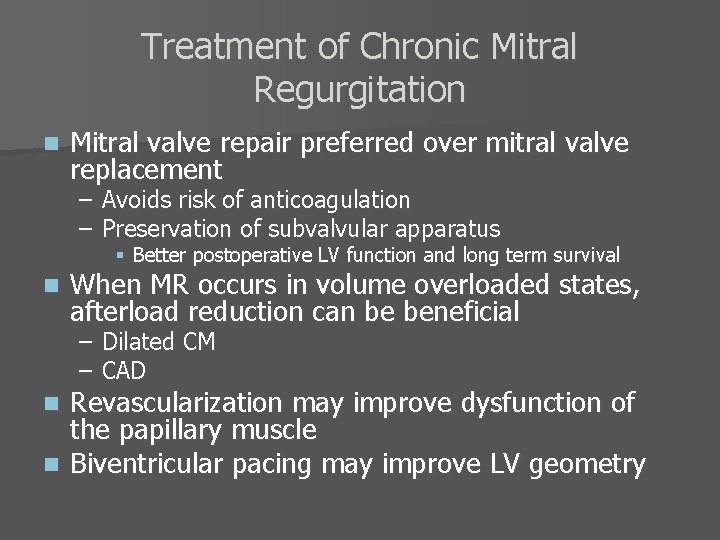
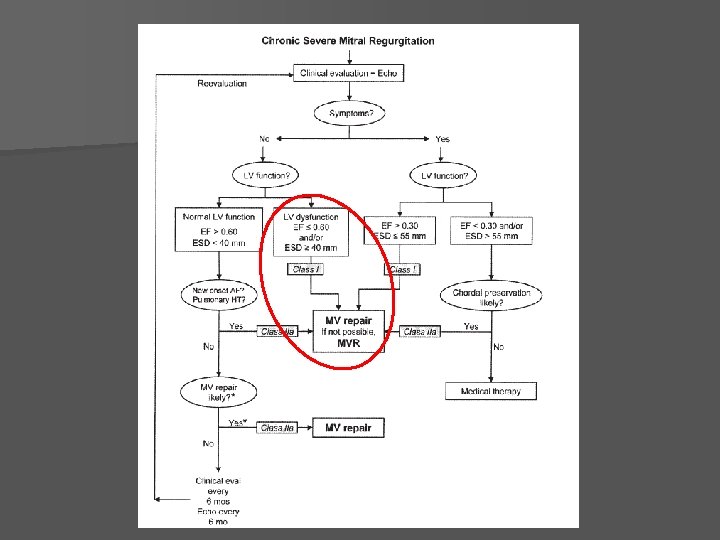
Treatment of Chronic Mitral Regurgitation n Mitral valve repair preferred over mitral valve replacement – Avoids risk of anticoagulation – Preservation of subvalvular apparatus § Better postoperative LV function and long term survival n When MR occurs in volume overloaded states, afterload reduction can be beneficial – Dilated CM – CAD Revascularization may improve dysfunction of the papillary muscle n Biventricular pacing may improve LV geometry n
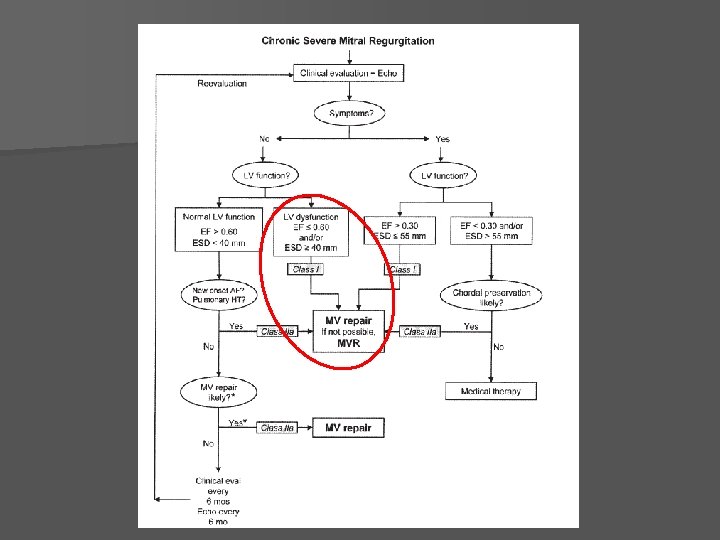

Timing of Intervention for Left-Sided Valvular Conditions Aortic Stenosis Mitral Stenosis Chronic Severe AR Chronic Severe MR Intervention: AVR Intervention: Percutaneous valvotomy if anatomy amenable and <moderate MR, and no LAA clot. Otherwise, open commissurotomy or MVR Intervention: Surgical AVR with aortic root replacement if needed Intervention: Surgical mitral valve repair if anatomy amenable. Otherwise, MVR IF: Patient is symptomatic (NYHA class II or greater, angina due to AS, or syncope) OR Patient has symptomatic severe AS and needs other cardiothoracic surgery (i. e. CABG) IF: Patient has moderate or more severe MS (MVA < 1. 5 cm 2) OR Pulmonary hypertrension at rest (PAP > 60 mm. Hg) OR Abnormal hemodynamic response to exercise: PAP > 60 mm. Hg Mean gradient > 15 mm. Hg IF: Patient is symptomatic (NYHA class II or greater) OR EF <60% OR ESD > 55 mm OR Abnormal hemodynamic response to exercise PAP increase by 25 mm. Hg IF: Patient is symptomatic (NYHA class II or greater) OR EF <60% OR ESD > 45 mm OR Pulmonary hypertension or atrial fibrillation OTHERWISE Depending on the severity of AS, at least annual clinical evaluation with TTE to monitor for symptom onset OTHERWISE Clinical evaluation at least annually, depending on the severity of the mitral stenosis OTHERWISE Repeat TTE at least yearly, repeat clinical evaluation at least biannually depending on the severity of the LV dilitiation OTHERWISE Repeat TTE yearly, repeat clinical evaluation biannually
Tricuspid Valve Disease n Tricuspid stenosis is rare n TR usually occurs secondary to: – Associated with rheumatic heart disease – – Pulmonary hypertension RV chamber enlargement with annular dilatation Endocarditis (associated with IV drug use) Injury following pacer lead placement Other secondary causes: carcinoid, radiation therapy, anorectic drug use, and trauma n Primary causes: Marfan’s syndrome and congenital disorders such as Ebstein’s anomaly and AV canal malformation n Echo is diagnostic in most cases n
Tricuspid Regurgitation Severe tricuspid regurgitation is difficult to treat and carries a poor overall clinical outcome n Symptoms are manifestations of systemic venous congestion n – Ascites – Pedal edema Surgical intervention usually considered if other cardiac surgery planned n Surgical options include valvular annuloplasty or replacement n – If replacement planned, bioprosthetic valve preferred

Prosthetic Valves- Mechanical n Three types: n n Durable but require life long anticoagulation For operative procedures, warfarin typically is discontinued for 48 -72 hours and restarted postop as soon as possible, except for: – Ball-cage valve – Single tilting disk valve – Bileaflet valve – Mechanical mitral prosthesis – Atrial fibrillation – Prior thromboembolic events

Ball-cage valve Single tilting disk valve Bileaflet valve
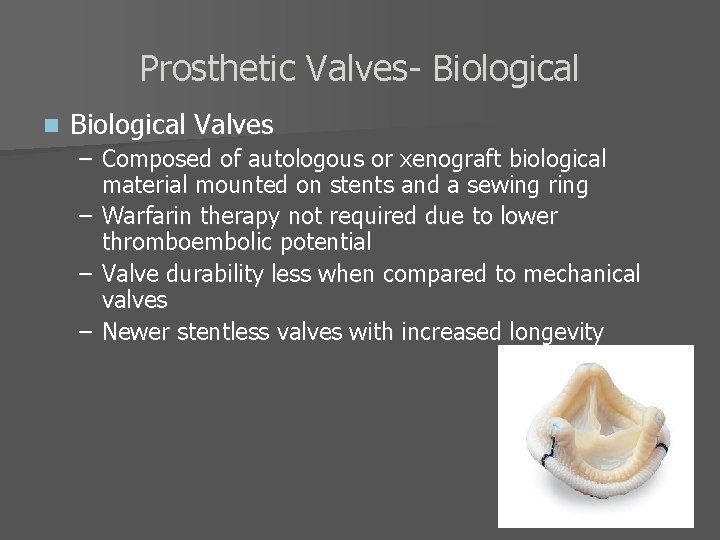
Prosthetic Valves- Biological n Biological Valves – Composed of autologous or xenograft biological material mounted on stents and a sewing ring – Warfarin therapy not required due to lower thromboembolic potential – Valve durability less when compared to mechanical valves – Newer stentless valves with increased longevity
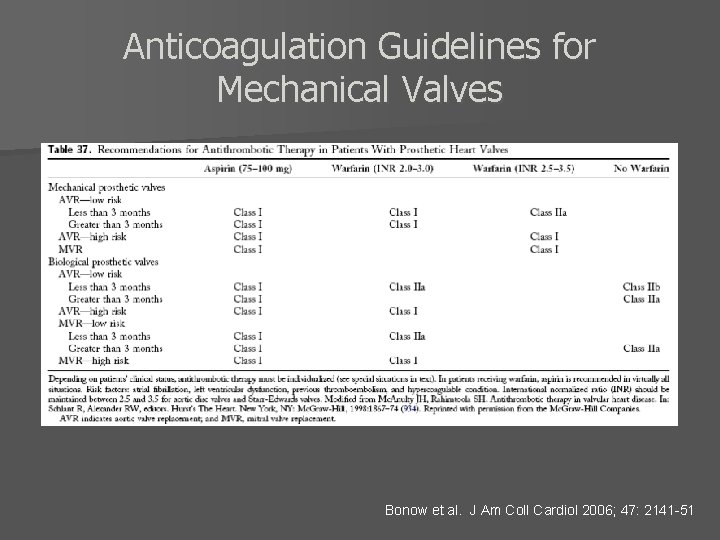
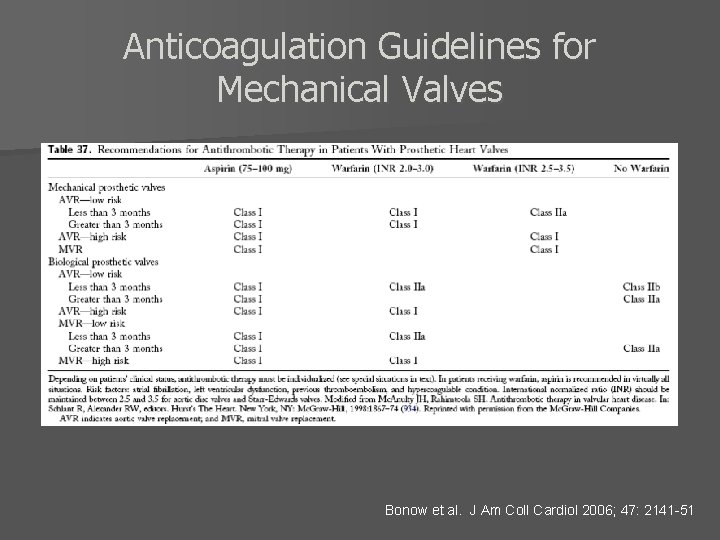
Anticoagulation Guidelines for Mechanical Valves Bonow et al. J Am Coll Cardiol 2006; 47: 2141 -51
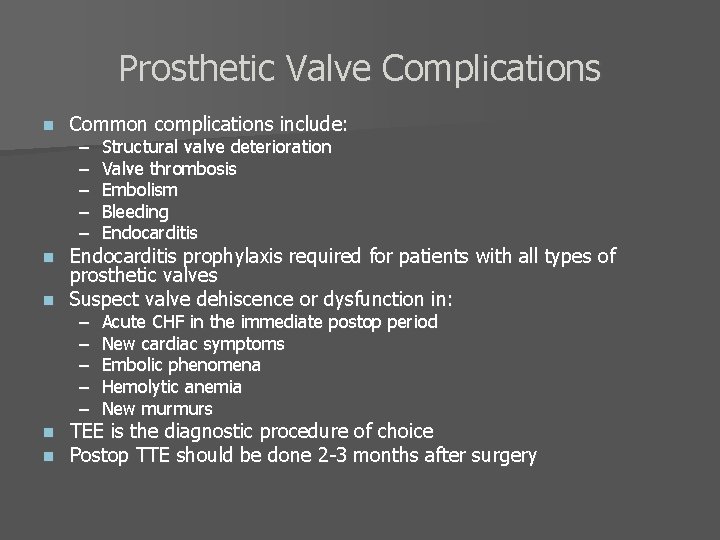
Prosthetic Valve Complications n Common complications include: – – – Structural valve deterioration Valve thrombosis Embolism Bleeding Endocarditis – – – Acute CHF in the immediate postop period New cardiac symptoms Embolic phenomena Hemolytic anemia New murmurs Endocarditis prophylaxis required for patients with all types of prosthetic valves n Suspect valve dehiscence or dysfunction in: n n n TEE is the diagnostic procedure of choice Postop TTE should be done 2 -3 months after surgery
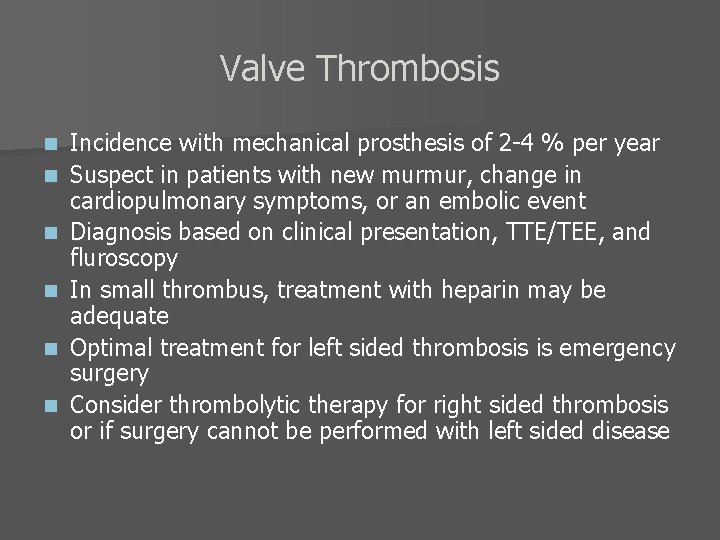
Valve Thrombosis n n n Incidence with mechanical prosthesis of 2 -4 % per year Suspect in patients with new murmur, change in cardiopulmonary symptoms, or an embolic event Diagnosis based on clinical presentation, TTE/TEE, and fluroscopy In small thrombus, treatment with heparin may be adequate Optimal treatment for left sided thrombosis is emergency surgery Consider thrombolytic therapy for right sided thrombosis or if surgery cannot be performed with left sided disease

Endocarditis Prophylaxis 2007 AHA Prevention of Infective Endocarditis Guidelines
 Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Mitral stenosis severity
Mitral stenosis severity Upper lobe diversion cxr
Upper lobe diversion cxr Dopamine uses
Dopamine uses Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Right sided heart failure
Right sided heart failure Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Causes of valvular heart disease
Causes of valvular heart disease Site:slidetodoc.com
Site:slidetodoc.com Traslape valvular
Traslape valvular Events of cardiac cycle class 11
Events of cardiac cycle class 11 Cardiac output and heart rate
Cardiac output and heart rate Bharathi viswanathan
Bharathi viswanathan Eisenmenger syndrome
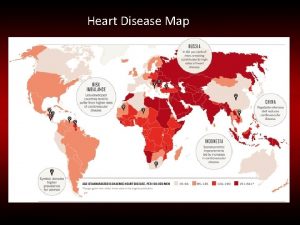
Eisenmenger syndrome Heart disease and stroke are the world's biggest killers
Heart disease and stroke are the world's biggest killers Modern treatment of heart disease
Modern treatment of heart disease Pico question examples heart disease
Pico question examples heart disease Ronaldo pictures
Ronaldo pictures Asd vs pulmonary stenosis murmur
Asd vs pulmonary stenosis murmur Pediatric knee chest position
Pediatric knee chest position Heart disease cat
Heart disease cat Heart disease data
Heart disease data Ie
Ie Terrible t's cyanotic heart disease
Terrible t's cyanotic heart disease Pathophysiology of ischemic heart disease
Pathophysiology of ischemic heart disease Rheumatic heart disease
Rheumatic heart disease Farah garmany
Farah garmany Heart disease
Heart disease Rhuematic fever
Rhuematic fever Coronary heart disease
Coronary heart disease Chronic coronary syndrome
Chronic coronary syndrome Rheumatic heart disease
Rheumatic heart disease Rheumatic heart disease causes
Rheumatic heart disease causes Ischemic heart disease
Ischemic heart disease Youtube
Youtube Nyha classification of heart disease
Nyha classification of heart disease Vijaya's echo criteria
Vijaya's echo criteria Right border of the relative cardiac dullness is formed by
Right border of the relative cardiac dullness is formed by Sheep heart diagram
Sheep heart diagram Heart to heart merrylands
Heart to heart merrylands Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Slidetodoc
Slidetodoc Bổ thể
Bổ thể