Values Ethics and Legal Issues Pam Llana MSN













- Slides: 47
Values, Ethics and Legal Issues Pam Llana, MSN, RN NUR 1117
� Nurses are obligated to provide ethical and legal client care � May need to resolve problems based on knowledge and skills � May be faced with difficult situations - what you think is RIGHT vs. RESPECT for the client’s rights / values � Legal practice of nursing is based on: �Standards of care �Nurse Practice Act (NPA) in your state of licensure

Values � Standards for decision-making that develop in the course of living � Truth � Honesty � Loyalty � Love � Care � Duty � Responsibility � Wisdom

Personal Values � Personal values - ideas or beliefs a person considers highly important � Value system – learned set of principles & rules - yours may differ from the client’s � Attitudes, beliefs & behaviors – related, but not the same as values � Behaviors - actions that demonstrate beliefs or values � Values are learned/influenced by: � Age � Developmental stage � Social influences � Family � Peers � School � Religion � Workplace � Culture

Cultural Competence �Everyone has a cultural identity which helps define expected behavior �Involves adjustment or recognition of one’s own culture in order to understand culture of client �Valuing client’s culture beliefs and recognizing need to bridge language barriers are essential Boyd, M. A. (2015). Psychiatric Nursing. Wolters Kluwer
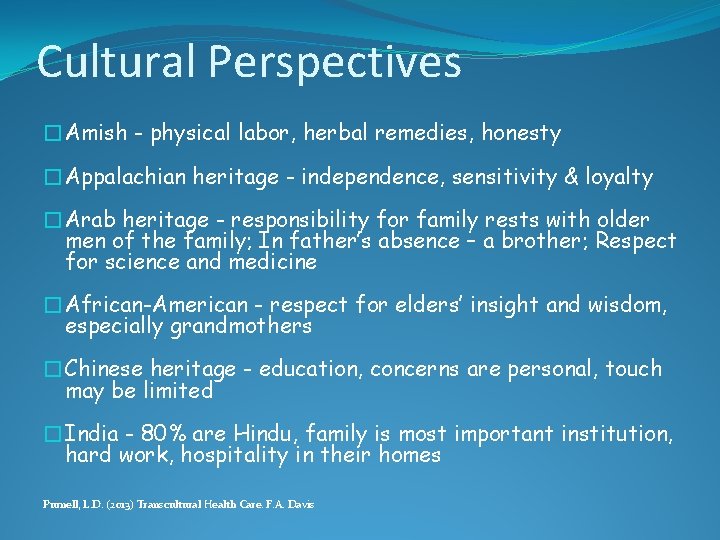
Cultural Perspectives �Amish - physical labor, herbal remedies, honesty �Appalachian heritage - independence, sensitivity & loyalty �Arab heritage - responsibility for family rests with older men of the family; In father’s absence – a brother; Respect for science and medicine �African-American - respect for elders’ insight and wisdom, especially grandmothers �Chinese heritage - education, concerns are personal, touch may be limited �India - 80% are Hindu, family is most important institution, hard work, hospitality in their homes Purnell, L. D. (2013) Transcultural Health Care. F. A. Davis
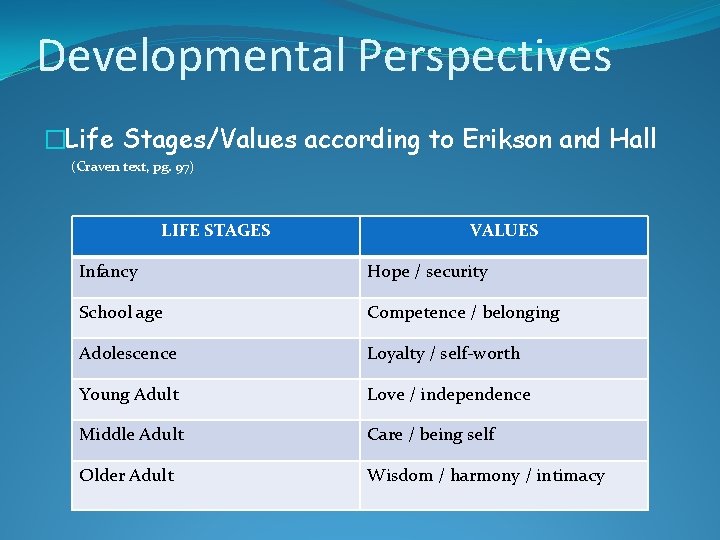
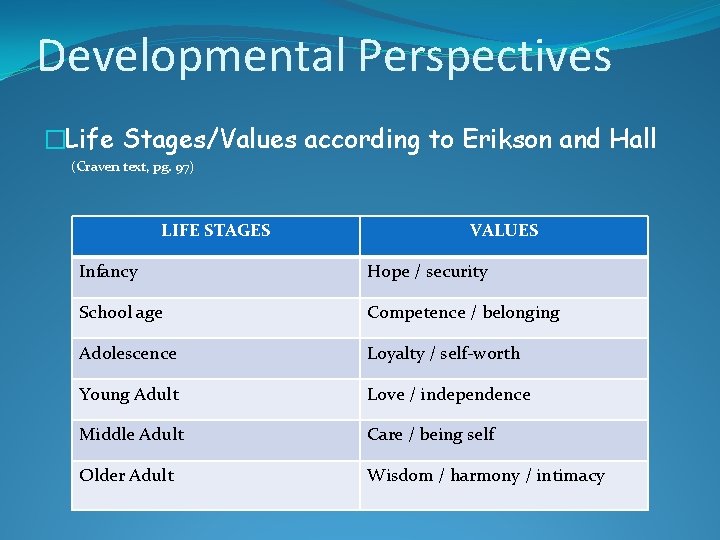
Developmental Perspectives �Life Stages/Values according to Erikson and Hall (Craven text, pg. 97) LIFE STAGES VALUES Infancy Hope / security School age Competence / belonging Adolescence Loyalty / self-worth Young Adult Love / independence Middle Adult Care / being self Older Adult Wisdom / harmony / intimacy

Value Conflicts: Resolutions in Nursing Care Situations �Between clients and healthcare providers: � Children at death bed �Between family members: �Refusing care vs. Advocating rights
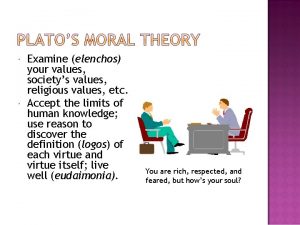
Ethics �Ethics Branch of philosophy dealing with standards of conduct and moral judgment �Professional ethics Standards of conduct to be upheld in all situations for a group

�International Council of Nurses (ICN, 2006) Code of Ethics for Nurses (p. 102) �American Nurses Association (ANA, 2011) Code of Ethics (p. 101) Common Codes • Compassion, respect • Responsible/accountable • Commitment to the patient - advocate for health, safety, confidentiality and rights of the client • Maintain competence/continue professional growth • Develop research-based professional knowledge • Personal conduct that reflects well on the profession to enhance public confidence
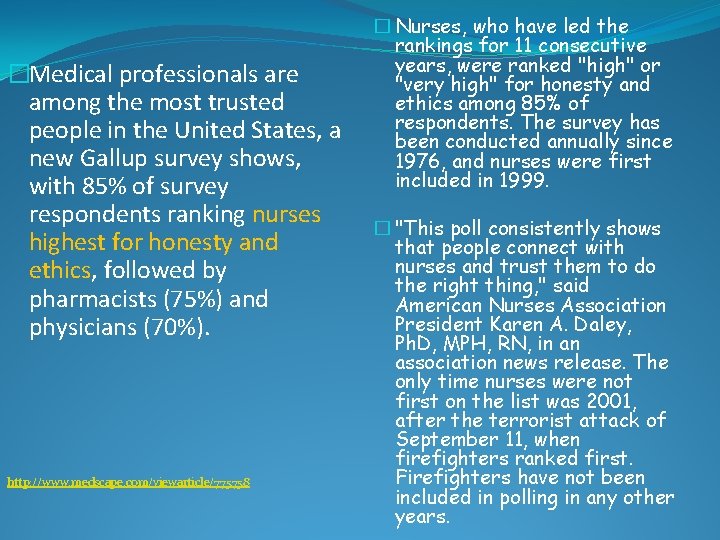
�Medical professionals are among the most trusted people in the United States, a new Gallup survey shows, with 85% of survey respondents ranking nurses highest for honesty and ethics, followed by pharmacists (75%) and physicians (70%). http: //www. medscape. com/viewarticle/775758 � Nurses, who have led the rankings for 11 consecutive years, were ranked "high" or "very high" for honesty and ethics among 85% of respondents. The survey has been conducted annually since 1976, and nurses were first included in 1999. � "This poll consistently shows that people connect with nurses and trust them to do the right thing, " said American Nurses Association President Karen A. Daley, Ph. D, MPH, RN, in an association news release. The only time nurses were not first on the list was 2001, after the terrorist attack of September 11, when firefighters ranked first. Firefighters have not been included in polling in any other years.



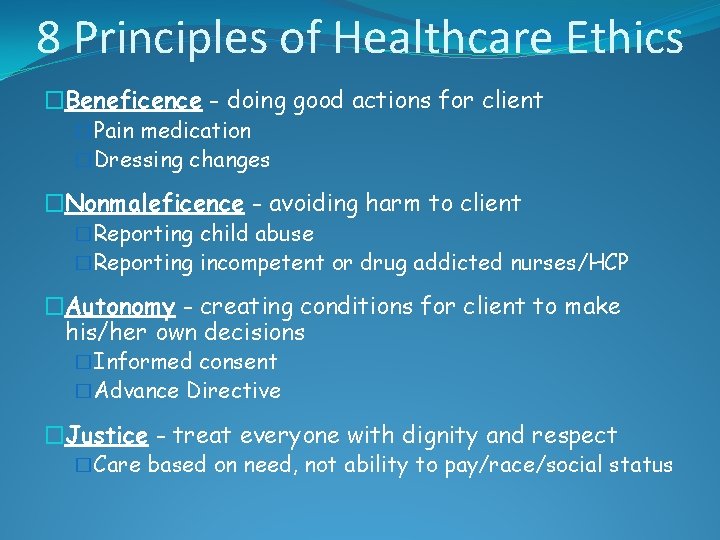
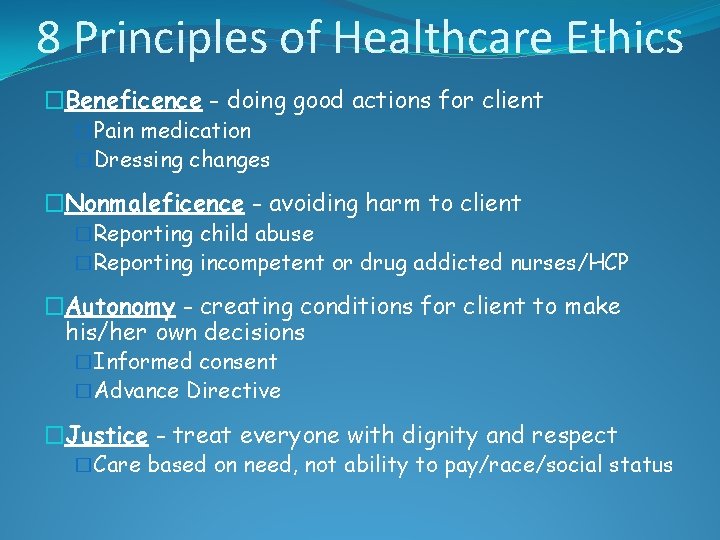
8 Principles of Healthcare Ethics �Beneficence - doing good actions for client �Pain medication �Dressing changes �Nonmaleficence - avoiding harm to client �Reporting child abuse �Reporting incompetent or drug addicted nurses/HCP �Autonomy - creating conditions for client to make his/her own decisions �Informed consent �Advance Directive �Justice - treat everyone with dignity and respect �Care based on need, not ability to pay/race/social status
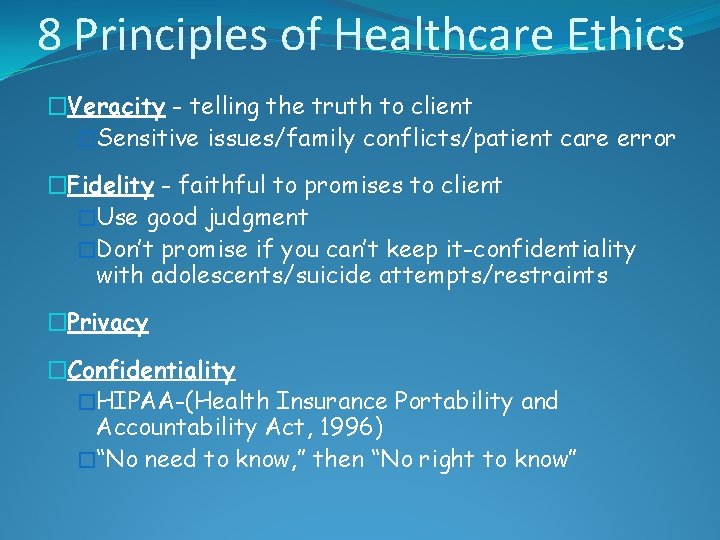
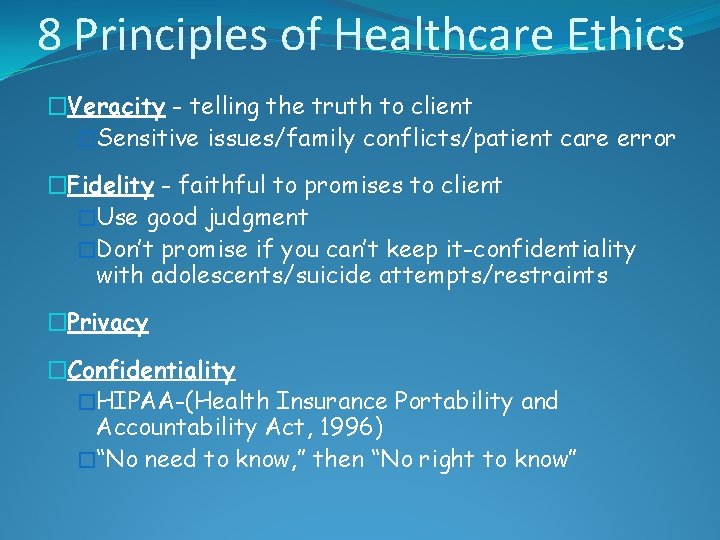
8 Principles of Healthcare Ethics �Veracity - telling the truth to client �Sensitive issues/family conflicts/patient care error �Fidelity - faithful to promises to client �Use good judgment �Don’t promise if you can’t keep it-confidentiality with adolescents/suicide attempts/restraints �Privacy �Confidentiality �HIPAA-(Health Insurance Portability and Accountability Act, 1996) �“No need to know, ” then “No right to know”

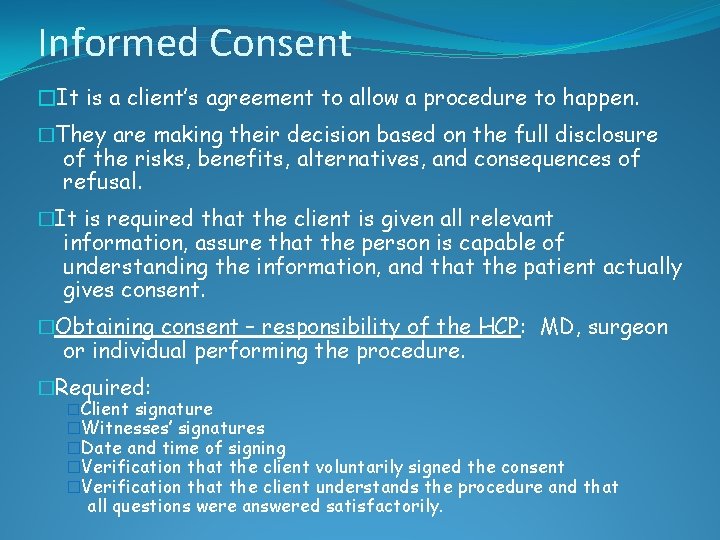
Consent �A signed consent form is necessary for all routine treatment, hazardous procedures such as surgery, chemo, and participation in research studies. �A client signs a general consent form when admitted to the hospital. �A different consent is needed for any specialized procedure. �Take into account a patient that is deaf, illiterate, or speaks a foreign language. �You must take steps to assure the patient understands what they are signing.
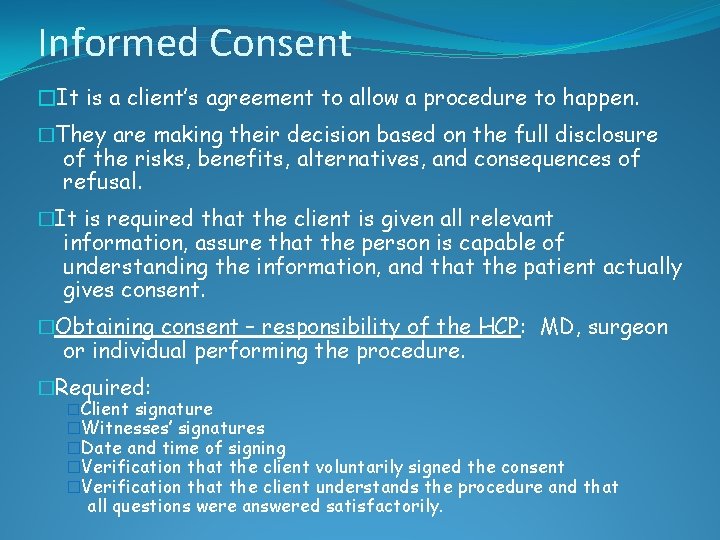
Informed Consent �It is a client’s agreement to allow a procedure to happen. �They are making their decision based on the full disclosure of the risks, benefits, alternatives, and consequences of refusal. �It is required that the client is given all relevant information, assure that the person is capable of understanding the information, and that the patient actually gives consent. �Obtaining consent – responsibility of the HCP: MD, surgeon or individual performing the procedure. �Required: �Client signature �Witnesses’ signatures �Date and time of signing �Verification that the client voluntarily signed the consent �Verification that the client understands the procedure and that all questions were answered satisfactorily.
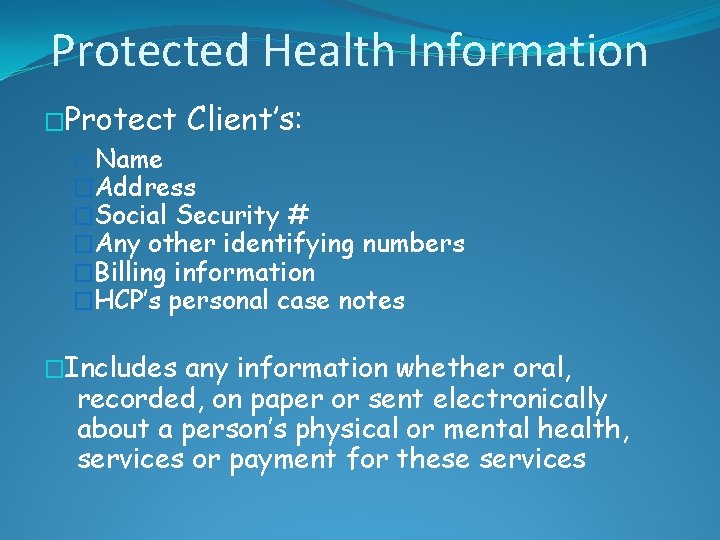
Protected Health Information �Protect Client’s: Name �Address �Social Security # �Any other identifying numbers �Billing information �HCP’s personal case notes � �Includes any information whether oral, recorded, on paper or sent electronically about a person’s physical or mental health, services or payment for these services
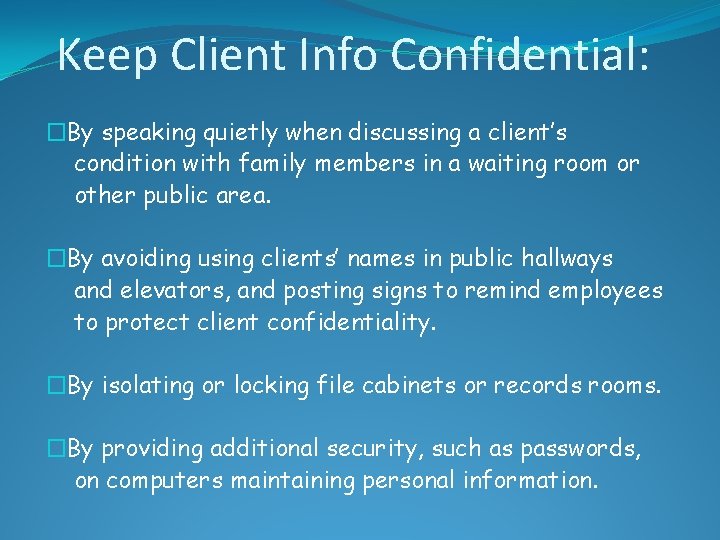
Keep Client Info Confidential: �By speaking quietly when discussing a client’s condition with family members in a waiting room or other public area. �By avoiding using clients’ names in public hallways and elevators, and posting signs to remind employees to protect client confidentiality. �By isolating or locking file cabinets or records rooms. �By providing additional security, such as passwords, on computers maintaining personal information.
Be careful with. . . �Student chart information: Do not take anything home that has any identifiable info on it. �Assure that faxing is secure; use cover sheet. �When calling in medication, do not disclose the reason for medication. �Healthcare personnel are on a “need to know” basis.

Be careful with. . . �Sign-in sheets require only the client’s name and NOT the reason for the visit. �Ask the client if you may call their home, may you leave a message on machine, or leave messages with other family members? �When leaving a message, only leave minimum amount of information that is necessary.
Be careful with. . . �No client information shared on Facebook or other social media! No comments or pictures! Even with patient’s permission! No, No ! ! ! �Destroy any identification materials in a shredder or incinerator. �Avoid identifying clients with communicable diseases, but prevent others from exposure.

The Client Care Partnership �American Hospital Association (AHA) �Formerly called “Patient’s Bill of Rights” � 6 basic treatment expectations during their hospital stay (Box 6 -3 on page 104): �High-quality hospital care �Clean and safe environment �Involvement in your care (Know 5 Rights) �Protection of your privacy �Preparing you and your family for when you leave hospital �Help with your bill and filing insurance claims
Client Bill of Rights �Mississippi Client Bill of Rights: http: //billstatus. ls. state. ms. us/documents/2013 /html/HB/1300 -1399/HB 1349 IN. htm
Mental Health �Voluntary admission / commitment �Individual voluntarily hospitalized for treatment �Individual maintains full legal and civil rights �Individual is free to leave at any time even against medical advice (AMA) �Involuntary commitment �Confined hospitalization of a person without the person’s consent but with a court order �Right to refuse treatment whether competent or incompetent �Each state has separate commitment statutes; 3 common elements: 1)mental disorder, 2)danger to self or others, 3)gravely disabled
Resolving Ethical Dilemmas �Ethical dilemmas: � 2 or more choices available �Difficult to determine best choice �Alternatives do not solve all needs for all involved �Each alternative has pros and cons �Strategies to prevent and resolve: �Validate feelings �Case analysis �Identify outcomes �Identify short and long-term goals �Clarify accountabilities �Follow through �Resolve reactions
Ethics Committee �Include nurses, physicians, administration personnel, clergy, social worker, attorney, and others �Required by The Joint Commission (TJC) � 3 Primary functions: �Policy development �Education �Consultation

Laws and Nursing
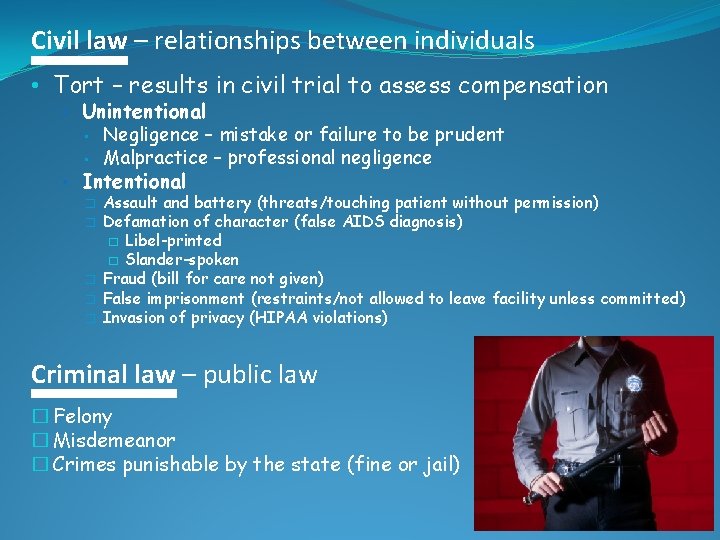
Civil law – relationships between individuals • Tort – results in civil trial to assess compensation • Unintentional • • Negligence – mistake or failure to be prudent Malpractice – professional negligence • Intentional � � � Assault and battery (threats/touching patient without permission) Defamation of character (false AIDS diagnosis) � Libel-printed � Slander-spoken Fraud (bill for care not given) False imprisonment (restraints/not allowed to leave facility unless committed) Invasion of privacy (HIPAA violations) Criminal law – public law � Felony � Misdemeanor � Crimes punishable by the state (fine or jail)
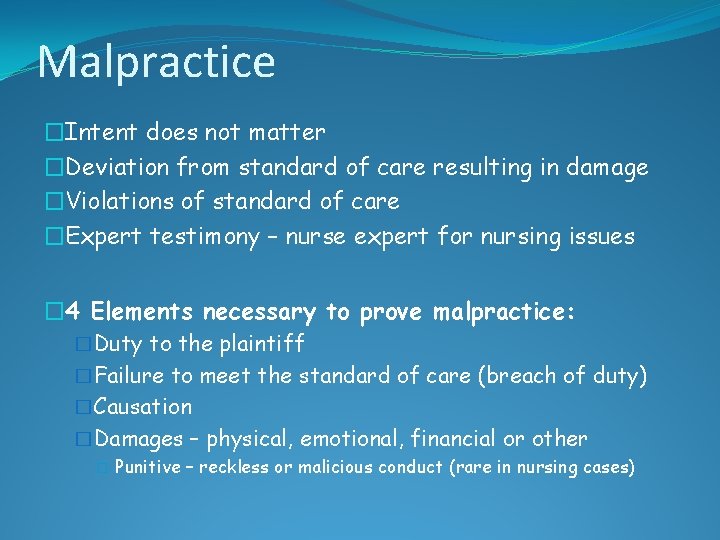
Malpractice �Intent does not matter �Deviation from standard of care resulting in damage �Violations of standard of care �Expert testimony – nurse expert for nursing issues � 4 Elements necessary to prove malpractice: �Duty to the plaintiff �Failure to meet the standard of care (breach of duty) �Causation �Damages – physical, emotional, financial or other � Punitive – reckless or malicious conduct (rare in nursing cases)
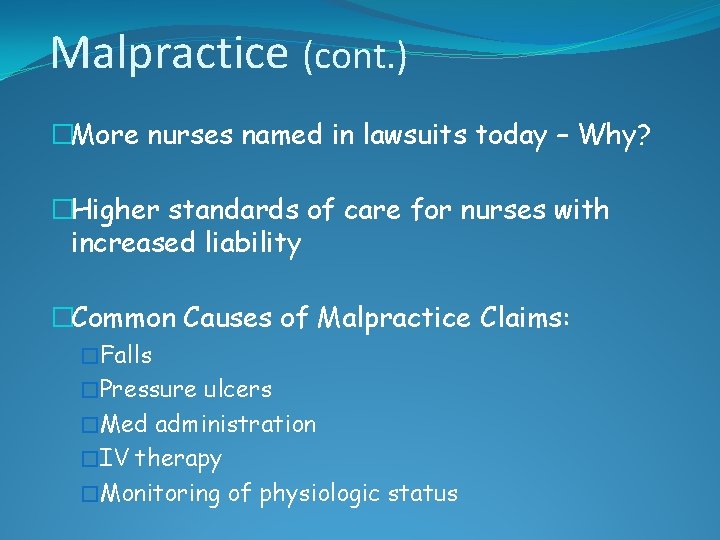
Malpractice (cont. ) �More nurses named in lawsuits today – Why? �Higher standards of care for nurses with increased liability �Common Causes of Malpractice Claims: �Falls �Pressure ulcers �Med administration �IV therapy �Monitoring of physiologic status
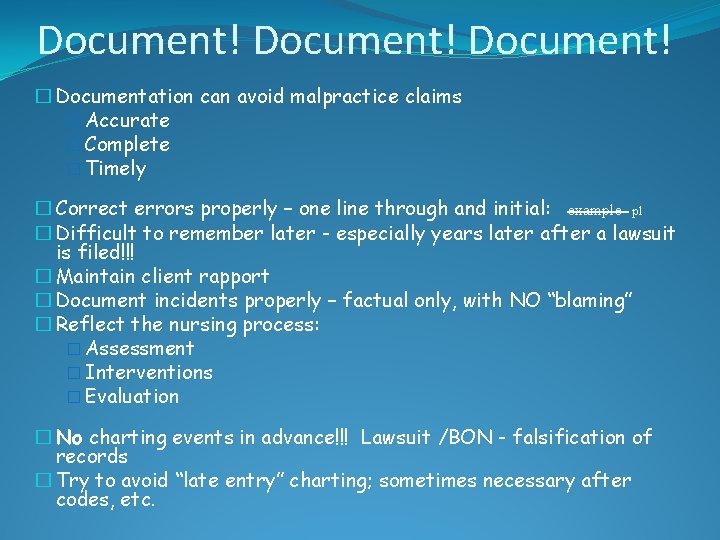
Document! � Documentation can avoid malpractice claims � Accurate � Complete � Timely � Correct errors properly – one line through and initial: example pl � Difficult to remember later - especially years later after a lawsuit is filed!!! � Maintain client rapport � Document incidents properly – factual only, with NO “blaming” � Reflect the nursing process: � Assessment � Interventions � Evaluation � No charting events in advance!!! Lawsuit /BON - falsification of records � Try to avoid “late entry” charting; sometimes necessary after codes, etc.
Allegations in paid claims (NSO 2006 -2010) �Delayed or failure to properly assess client or document assessment �Failure to: � assess need for medical intervention � assess client’s expressed complaints � monitor and report blood test results or vital signs � implement HCP orders, treatment protocols � supervise � identify or manage transfusion reaction �Equipment- malfunction, response to warning alarms, equipment not available, user error �Abandonment of client �Improper management of aging or behavioral health client �Medication errors �Nurse substance abuse, violation of rights, client abuse

Nursing Licensure �To practice as a nurse, one must be licensed in State where they reside. �Nurse Practice Act – BON in each State: �Define nursing �Scope of practice �Expectations �Government of nursing �Criteria for education �Advanced practice nurses
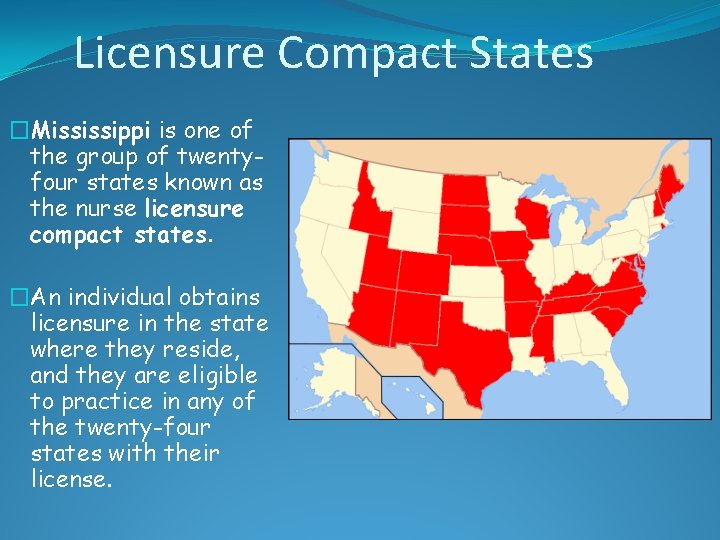
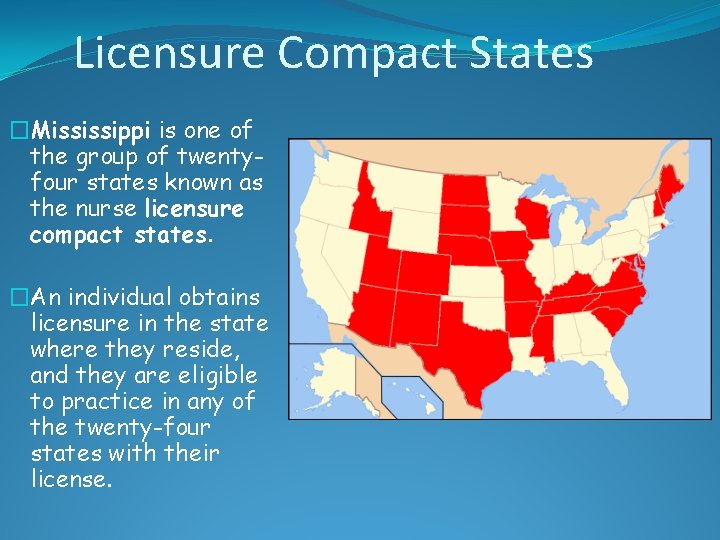
Licensure Compact States �Mississippi is one of the group of twentyfour states known as the nurse licensure compact states. �An individual obtains licensure in the state where they reside, and they are eligible to practice in any of the twenty-four states with their license.
Mississippi Board of Nursing �Website: http: //www. msbn. ms. gov/Pages/Home. aspx �Nurse Practice Act �Licensing Exam (NCLEX) �FAQ �License Verification �Position Statements �Disciplinary Actions: � Substance abuse � Falsification of application/documents � Misappropriation of drugs, supplies, or equipment
Standards of Care �Expected level of performance or practice as established by: � Guidelines � Authority � Custom �Nurse Practice Act (NPA) – Mississippi BON �ANA – American Nurses Association �Specialty Organizations (Critical Care, OR Nursing, etc. ) �TJC - The Joint Commission (safety & documentation) �CDC - Centers for Disease Control �Institutional/agency policies and procedures (WILL NOT override NPA) �Must be familiar with regulations regarding nursing care
Legal Protection for Nurses �Professional practice – stay within scope of practice �Follow chain of command to advocate for clients �Liability insurance (p. 113) recommended – provides for defense if you are sued Employer may state nurse was not acting within the scope of employment � Volunteer work � • Student nurse coverage?
Student nurses are responsible for own actions. Students must be prepared and supervised by their instructor or a designated preceptor. Nursing faculty are covered by the health care facility and the college. Students employed must follow their job descriptions. “Do Not Perform Task Outside your Scope of Practice. ” Telephone orders (T. O. s) are discouraged, but sometimes are necessary. Student nurses do NOT take T. O. s Always sign, date and time orders and all documentation.
HCP Prescriptions (Orders) �It is your responsibility as the nurse to make sure the HCP’s orders are followed through. �If you think the order is incorrect, you can’t read the writing, or you are just not sure what the HCP means, CALL HCP to clarify the order. �You have the authority and the obligation to question an order that may cause the client harm. Do not follow the order if it will harm the client. Clarify the order!
Sensitive Issues �Controlled substances �Do not resuscitate (DNR) �Code limitations �Must know code status of client �Advance Directive(AD): Living Will � Durable Power of Attorney for Healthcare (Healthcare proxy) � �Sample AD on pg. 103 Psychiatric Advance Directive (PAD) Allows client, while competent, to make choices in treatment and care. HCP can override when client’s decision-making capacity is clearly distorted because of mental illness.
Advance Directive �Documents that state your choices about medical treatment and/or name someone who may make those decisions for your medical treatment should you become unable to make those decisions. �Make sure these are signed in advance to let your doctor know what your wishes are. �AD allows you to be able to make legally valid decisions about your medical care. �Health care facilities are required to ask if the patient has an advance directive.
Living Will �This document is going to inform health care providers to withhold or withdraw life sustaining procedures in a client in which death is imminent. �Will need 2 witnesses that are not relatives when the person signs the document; Against agency policies for nurses to witness client signing legal documents. �Only a competent client is able to make or revoke a living will. �Nurse can be subject to liability if he/she ignores the wishes of the client.
Power of Attorney �Power of Attorney enables the Agent to act for the Principal even after the Principal is not mentally competent or physically able to make decisions. �Durable Power of Attorney – can make both business and health care decisions �Power of Attorney for Healthcare (also called Healthcare proxy) – can make only healthcare decisions
Good Samaritan Law • Legal immunity for healthcare professionals who assist in emergencies • No compensation accepted • Provide reasonable care • Obligated to stay until official rescue personnel arrive
EMTALA � Congress enacted the Emergency Medical Treatment & Labor Act (EMTALA) to ensure public access to emergency services regardless of ability to pay �EMTALA – prevents “patient dumping”
 Msn legal nurse consultant programs
Msn legal nurse consultant programs Bury pam pam
Bury pam pam Legal ethical and societal issues in media and information
Legal ethical and societal issues in media and information Professional issues ethics and computer law
Professional issues ethics and computer law Legal and ethical issues in use of ict
Legal and ethical issues in use of ict Ethical and legal issues in e-business
Ethical and legal issues in e-business Legal and ethical issues in computer security
Legal and ethical issues in computer security Professional and ethical issues during internship
Professional and ethical issues during internship Chapter 2 ethical and legal issues
Chapter 2 ethical and legal issues Medical legal and ethical issues chapter 3
Medical legal and ethical issues chapter 3 Chapter 3 ethical and legal issues
Chapter 3 ethical and legal issues Attack sophistication vs intruder technical knowledge
Attack sophistication vs intruder technical knowledge Legal and ethical issues chapter 5
Legal and ethical issues chapter 5 Legal and ethical issues chapter 3
Legal and ethical issues chapter 3 Reward system and legal issues
Reward system and legal issues Chapter 6 legal and ethical issues
Chapter 6 legal and ethical issues Chapter 5 legal and ethical issues
Chapter 5 legal and ethical issues Nflpn code of ethics
Nflpn code of ethics Chapter 2 ethical and legal issues
Chapter 2 ethical and legal issues Chapter 2 ethical and legal issues
Chapter 2 ethical and legal issues Chapter 5 legal and ethical responsibilities
Chapter 5 legal and ethical responsibilities Ethical and legal issues affecting the nursing assistant
Ethical and legal issues affecting the nursing assistant What is the difference between ethical and legal issues
What is the difference between ethical and legal issues Ethical and legal issues in community health nursing
Ethical and legal issues in community health nursing Legal and ethical issues chapter 5
Legal and ethical issues chapter 5 Chapter 2 ethical and legal issues
Chapter 2 ethical and legal issues Legal regulatory and political issues
Legal regulatory and political issues Legal and ethical issues in information security
Legal and ethical issues in information security Legal issues in psychiatric nursing
Legal issues in psychiatric nursing Chapter 6 legal and ethical issues
Chapter 6 legal and ethical issues Chapter 6 legal and ethical issues
Chapter 6 legal and ethical issues Chapter 3 legal and ethical issues
Chapter 3 legal and ethical issues Bruce maglino workplace values
Bruce maglino workplace values Instrumental values
Instrumental values Macro and micro ethics
Macro and micro ethics Environmental ethics issues and possible solutions
Environmental ethics issues and possible solutions Issues and ethics in the helping professions 9th edition
Issues and ethics in the helping professions 9th edition Issues and ethics in the helping profession
Issues and ethics in the helping profession If a nurse decides to withhold a medication
If a nurse decides to withhold a medication Cbsa values and ethics
Cbsa values and ethics Romantic transcendental conservation ethic
Romantic transcendental conservation ethic A foundation course in human values and professional ethics
A foundation course in human values and professional ethics Legal issues in performance appraisal
Legal issues in performance appraisal Legal issues in hrm
Legal issues in hrm Legal issues in sport/event marketing match-up
Legal issues in sport/event marketing match-up Legal issues in nursing practice
Legal issues in nursing practice Ethical issues in computer science
Ethical issues in computer science Legal issues in special education
Legal issues in special education