ValueBased Care Volume to Value Lecture a Introduction
Value-Based Care Volume to Value Lecture a – Introduction to Volume to Value This material (Comp 23 Unit 6) was developed by Normandale Community College, funded by the Department of Health and Human Services, Office of the National Coordinator for Health Information Technology under Award Number 90 WT 0003. This work is licensed under the Creative Commons Attribution-Noncommercial-Share Alike 4. 0 International License. To view a copy of this license, visit http: //creativecommons. org/licenses/by-nc-sa/4. 0/.
Volume to Value Learning Objectives • List the major payers of health care in the U. S. • Define the broad strategies of volume to value and shared risk • Describe alternative payment models 2

Volume to Value Overview • Restructure care delivery through new payment models • Shift from fee-for-service to value-based • Use Health IT as a foundation for the shift from volume to value 3
Value in Health Care • Definition of value: • Equates to the relationship between health outcomes and dollars spent to achieve them. – “Health care outcomes per dollar spent” – Outcomes = Lower mortality and morbidity Source: Porter, M. E. , December 23, 2010 4
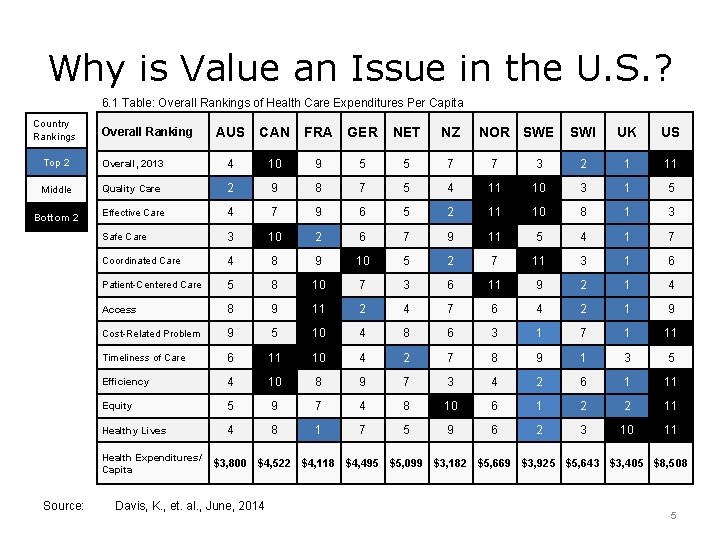
Why is Value an Issue in the U. S. ? 6. 1 Table: Overall Rankings of Health Care Expenditures Per Capita Country Rankings Overall Ranking AUS CAN FRA GER NET NZ NOR SWE SWI UK US Top 2 Overall, 2013 4 10 9 5 5 7 7 3 2 1 11 Middle Quality Care 2 9 8 7 5 4 11 10 3 1 5 Effective Care 4 7 9 6 5 2 11 10 8 1 3 Safe Care 3 10 2 6 7 9 11 5 4 1 7 Coordinated Care 4 8 9 10 5 2 7 11 3 1 6 Patient-Centered Care 5 8 10 7 3 6 11 9 2 1 4 Access 8 9 11 2 4 7 6 4 2 1 9 Cost-Related Problem 9 5 10 4 8 6 3 1 7 1 11 Timeliness of Care 6 11 10 4 2 7 8 9 1 3 5 Efficiency 4 10 8 9 7 3 4 2 6 1 11 Equity 5 9 7 4 8 10 6 1 2 2 11 Healthy Lives 4 8 1 7 5 9 6 2 3 10 11 Bottom 2 Health Expenditures/ Capita Source: $3, 800 $4, 522 $4, 118 $4, 495 $5, 099 $3, 182 $5, 669 $3, 925 $5, 643 $3, 405 $8, 508 Davis, K. , et. al. , June, 2014 5
Definition of Bad Value • Paying a lot more than someone else • Getting a lot less than someone else • Example: You go to the dealership and pay for a Lamborghini, but they give you a Chevy. Images: Lamborghini, Chevy Cruze CC BY-NC-SA 4. 0 6

Health Care Payers in the U. S. Image: CMS, Office of the Actuary, National Health Statistics Group 7
A Closer Look at Health Care Payers 6. 2 Chart: Who Paid for Health Care in 2014? [CATEGORY NAME], [VALUE] Source: National Health Expenditure 2014 Highlights [CATEGORY NAME], [VALUE] 8
How We Pay Health Care Providers in the U. S. • Fee-for-Service (FFS) – “Payment for specific health care services provided to a patient” (as opposed to payments received for the number of patients seen, the number of hours worked, or the number of patients enrolled in a health care panel) Source: Farlex and Partners, 2009 9
Proposed Payment Model Changes • From the 1980 s, when fee schedules were established, until 2011, when the Affordable Care Act introduced changes, the great majority of health care providers were paid under FFS contracts Sources: Bottles, 2012; CMS Fact Sheet, 2015 10
Benefits of the Fee-for-Service Model • Fee-for-service pays health care providers for activity, creating an incentive to work hard • The more you do, the more you’re paid • There is no incentive under Fee-for. Service for providers to withhold health care 11
Drawbacks of the Fee-for-Service Model • Fee-for-Service can result in unnecessary tests, procedures, visits, etc. , because the provider is paid based on activity • The biggest problem from a value perspective is that traditional Fee-for. Service is not linked to outcomes: the provider is paid whether or not your health improves 12
![Not a New Problem • “I find [medicine] the best of trades; for, whether Not a New Problem • “I find [medicine] the best of trades; for, whether](http://slidetodoc.com/presentation_image/09b19df2ea409740577cb19d1c7b0734/image-13.jpg)
Not a New Problem • “I find [medicine] the best of trades; for, whether we are right or wrong, we are paid equally well. We are never responsible for the bad work, and we cut away as we please in the stuff we work on. A shoemaker in making shoes can’t spoil a scrap of leather without having to pay for it, but we can spoil a man without paying one farthing for the damage done. ” Source: Moliere, The Doctor in Spite of Himself 13
The Story of Mc. Allen Texas • Mc. Allen had the second-highest per capita cost for Medicare spending by city in the U. S. • Patients there weren’t any sicker than patients in similar cities. • “The primary cause of Mc. Allen’s extreme costs was, very simply, the across-theboard overuse of medicine. ” Source: Gawande, A. 2009 14
Broad Strategy to Increase Value • Volume to Value, according to CMS, means “moving away from rewarding volume in order to shape the way health care is delivered to patients, and to improve the quality of care system-wide, while helping to reduce the growth of health care costs. ” Source: CMS Fact Sheet, 2015 15
Value-Based Payments • The payer rewards providers for desirable activities • Payment models share these aspects: – Quality/performance-based contract – Performance measures reports – Incentive or penalty 16
What is Measured • Examples of measures include: – Performance – Quality – Consumer satisfaction – Cost measures 17
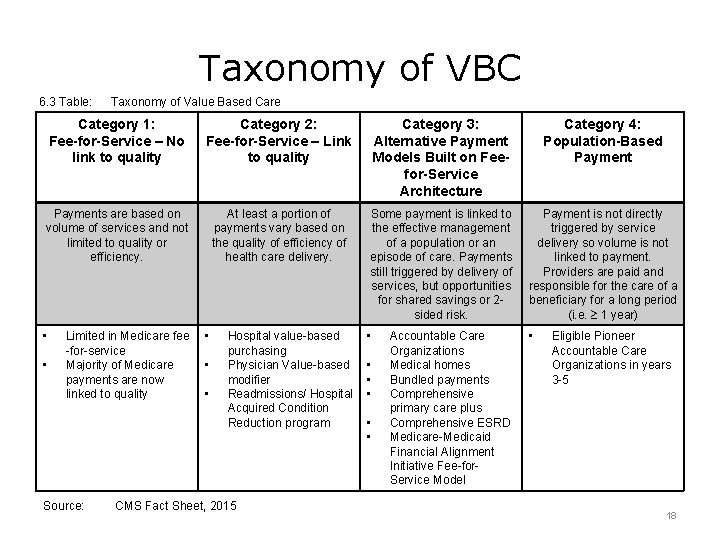
Taxonomy of VBC 6. 3 Table: Taxonomy of Value Based Care Category 1: Fee-for-Service – No link to quality Category 2: Fee-for-Service – Link to quality Category 3: Alternative Payment Models Built on Feefor-Service Architecture Category 4: Population-Based Payments are based on volume of services and not limited to quality or efficiency. At least a portion of payments vary based on the quality of efficiency of health care delivery. Some payment is linked to the effective management of a population or an episode of care. Payments still triggered by delivery of services, but opportunities for shared savings or 2 sided risk. Payment is not directly triggered by service delivery so volume is not linked to payment. Providers are paid and responsible for the care of a beneficiary for a long period (i. e. 1 year) • • Limited in Medicare fee -for-service Majority of Medicare payments are now linked to quality Source: • • • Hospital value-based purchasing Physician Value-based modifier Readmissions/ Hospital Acquired Condition Reduction program CMS Fact Sheet, 2015 • • • Accountable Care Organizations Medical homes Bundled payments Comprehensive primary care plus Comprehensive ESRD Medicare-Medicaid Financial Alignment Initiative Fee-for. Service Model Eligible Pioneer Accountable Care Organizations in years 3 -5 18
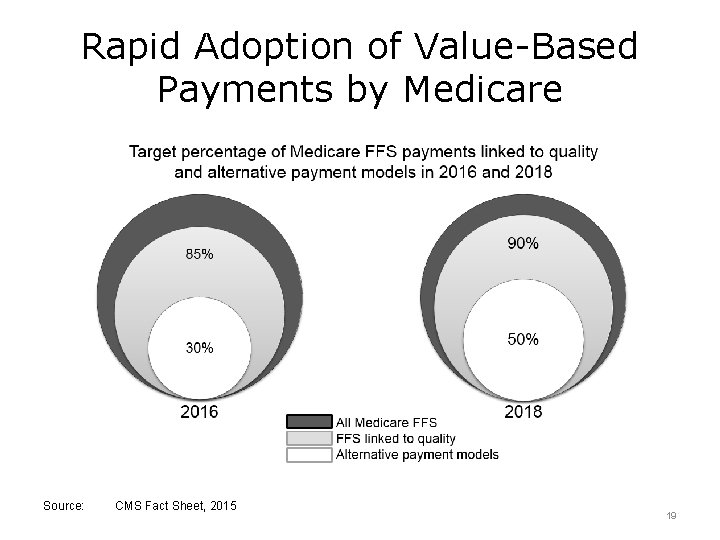
Rapid Adoption of Value-Based Payments by Medicare Source: CMS Fact Sheet, 2015 19
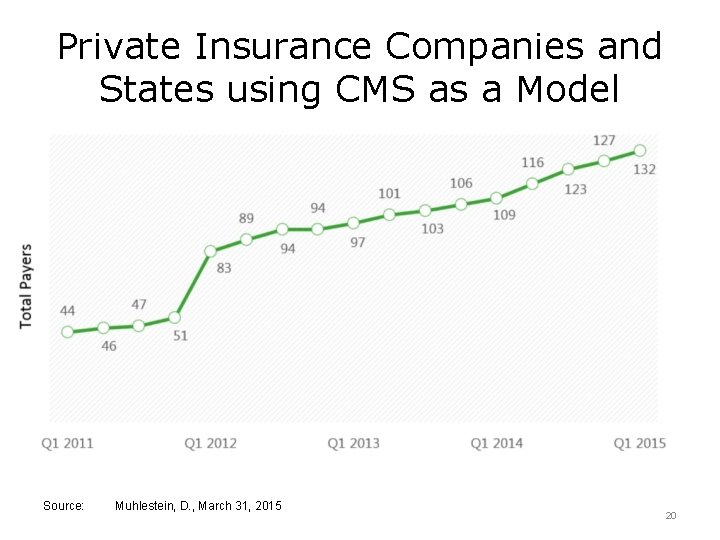
Private Insurance Companies and States using CMS as a Model Source: Muhlestein, D. , March 31, 2015 20
Health IT Essential to Measuring Outcomes • Value-based care is based on a foundation of measurement and reporting – providers enter into contracts that pay or penalize them based on goals • Measurement of the goals requires accurate statistical calculations. 21
Health IT Essential to Improving Processes • Improvement on the measured goals requires rapid feedback • Manual processes from paper records are not sufficient to run a national program with nearly 1. 2 million physicians Source: CMS, February 2016 22
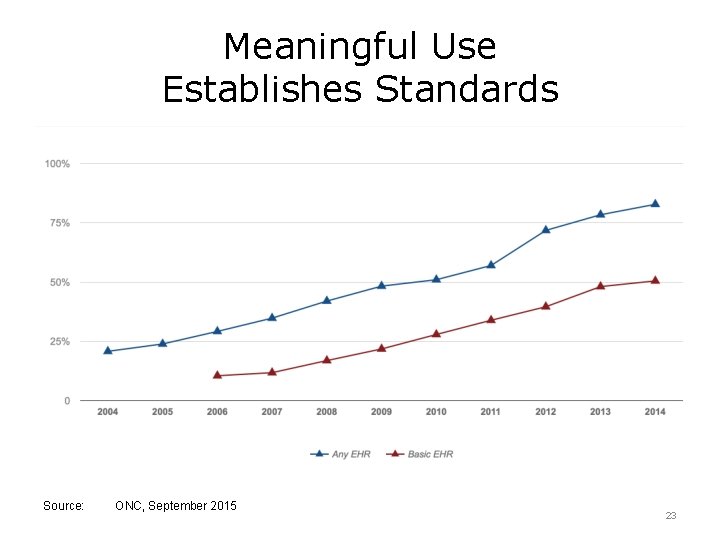
Meaningful Use Establishes Standards Source: ONC, September 2015 23
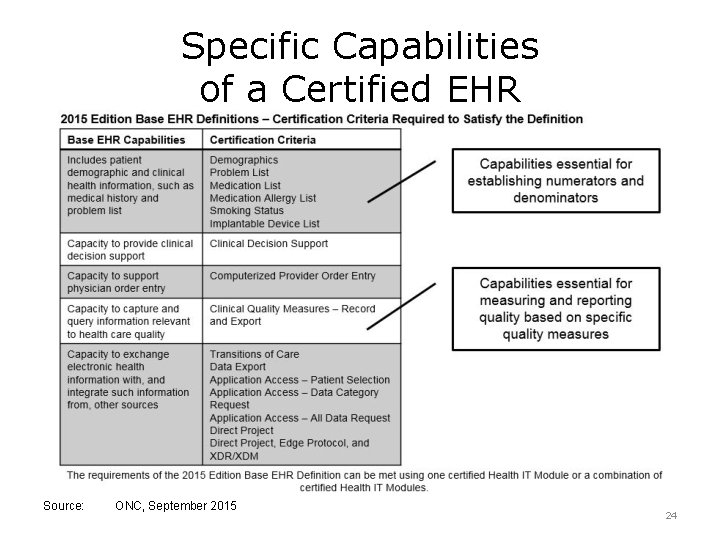
Specific Capabilities of a Certified EHR Source: ONC, September 2015 24
Evolution of Meaningful Use • The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) integrates some existing incentive programs, including Meaningful Use and the Physician Quality Reporting System (PQRS) into new Medicare payment models. Source: The CMS Blog, January 11, 2016 25
Volume to Value Lecture a Summary • As we have seen, the push for valuebased care and payment is growing rapidly • The strategy to move away from fee-forservice is being led by CMS • EHRs and other Health IT play essential roles in the measurement and reporting needed to support value-based payments 26
Volume to Value Lecture a – References 1 References: Better Care. Smarter Spending. Healthier People: Paying Providers for Value, Not Volume (January 26, 2015). CMS Fact Sheet. Retrieved from htpps: //www. cms. gov Bottles, K. M. D. (December 12, 2012). Is Fee-for-Service Really Dead? Really? The Health Care Blog. Retrieved from: http: //www. thehealthcareblog. com Comments of CMS Acting Administrator Andy Slavitt at the J. P. Morgan Annual Health Care Conference, Jan. 11, 2016. The CMS Blog. Retrieved from: https: //www. blog. cms. gov/ Farlex and Partners (2009). Medical Dictionary Gawande, A. (June 1, 2009). The Cost Conundrum: What a Texas town can teach us about health care. The New Yorker, Annals of Medicine. Retrieved from: http: www. thenewyorker. com Halamka, J. (November 11, 2015). The Path Forward for Meaningful Use. Life as a Healthcare CIO. Retrieved from: http: //www. geekdoctor. blogspot. com Mc. Knight, W. (January 12, 2016). CMS: End of meaningful use imminent in 2016. Internal Medicine News Digital Network. Retrieved from: http: //www. internalmedicinenews. com 27
Volume to Value Lecture a – References 2 References Porter, M. E. (December 23, 2010). What Is Value in Health Care? N Engl J Med; 363: 2477 -2481 DOI: 10. 1056/NE JMp 1011024 What is a MAC? (February 5, 2016). CMS. Retrieved from: https: //www. cms. gov Charts, Tables, Graphs 6. 1 Table: Davis, K. , Stremikis, K. , Squires, D. and Schoen, C. (June 2014). Mirror, Mirror on the Wall: How Performance of the U. S. Health Care System Compares Internationally, 2014 Update. The Commonwealth Fund. Retrieved from: http: //www. commonwealthfund. org 6. 2 Chart: National Health Expenditure 2014 Highlights (2014) CMS. gov Retrieved from: https: //www. cms. gov 6. 3 Table: Better Care. Smarter Spending. Healthier People: Paying Providers for Value, Not Volume (January 26, 2015). CMS Fact Sheet. Retrieved from htpps: //www. cms. gov 28
Volume to Value Lecture a – References 3 Images Slide 6: Lamborghini, Chevy Cruze CC BY-NC-SA 4. 0 Slide 7: Nation’s health dollar – where it came from, where it went (2014). [PDF] Retrieved from: https: //www. cms. gov/ Slide 19: Better Care. Smarter Spending. Healthier People: Paying Providers for Value, Not Volume (January 26, 2015). CMS Fact Sheet. Retrieved from htpps: //www. cms. gov Slide 20: Muhlestein, D. (March 31, 2015). Growth and Dispersion of Accountable Care Organizations in 2015. Health Affairs Blog. Retrieved from: http: //www. healthaffairsorg. blog/ Slide 23: Office of the National Coordinator for Health Information Technology. (September 2015). Office-based Physician Electronic Health Record Adoption: 20042014, Health IT Quick-Stat #50. Slide 24: Office of the National Coordinator for Health Information Technology. (2015). 2015 Edition Base EHR Definition – Certification Criteria Required to Satisfy Definition. 29
Volume to Value Lecture a This material was developed by Normandale Community College, funded by the Department of Health and Human Services, Office of the National Coordinator for Health Information Technology under Award Number 90 WT 0003. 30
- Slides: 30