Validating the MMS An MH referral screen for
- Slides: 29
Validating the MMS: An MH referral screen for public assistance recipients in NYS Mary Jane Alexander, Ph. D. Deborah Layman, MA Gary Haugland, MA Nathan Kline Institute for Psychiatric Research APHA 141 st Annual Conference November 4, 2013
Presenter Disclosures Mary Jane Alexander The following personal financial relationships with commercial interests relevant to this presentation existed during the past 12 months: No relationships to disclose
Funding NYS Office of Temporary Disability Assistance NYS Office of Mental Health MH 078188 to Dr. Alexander
OUTLINE Why an MH screen – and why the MMS in Local Social Service Settings? MMS Study in NYS Local Social Service Departments Policy considerations
Why an MH screen – and why the MMS - in Local Social Service Settings?
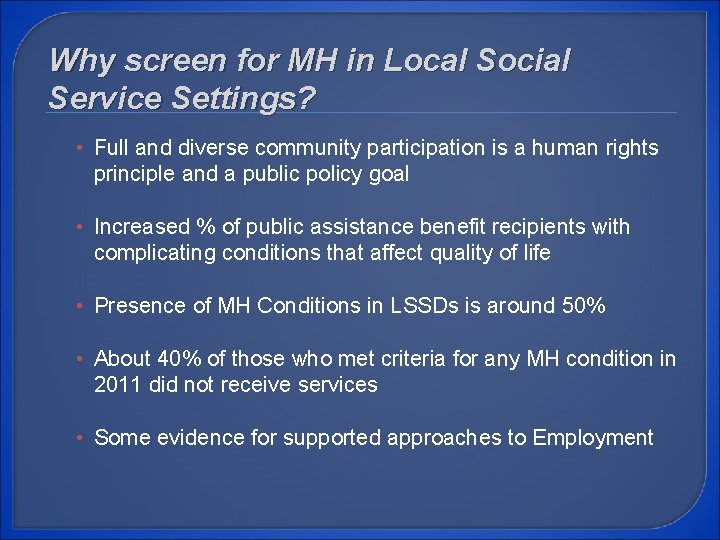
Why screen for MH in Local Social Service Settings? • Full and diverse community participation is a human rights principle and a public policy goal • Increased % of public assistance benefit recipients with complicating conditions that affect quality of life • Presence of MH Conditions in LSSDs is around 50% • About 40% of those who met criteria for any MH condition in 2011 did not receive services • Some evidence for supported approaches to Employment
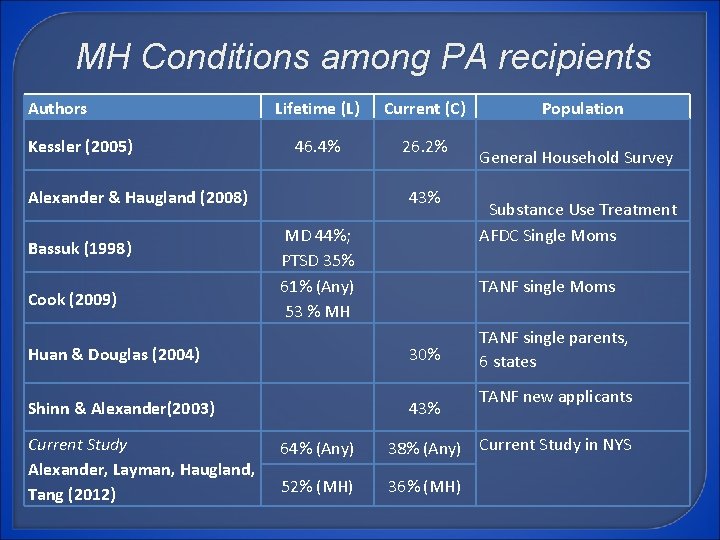
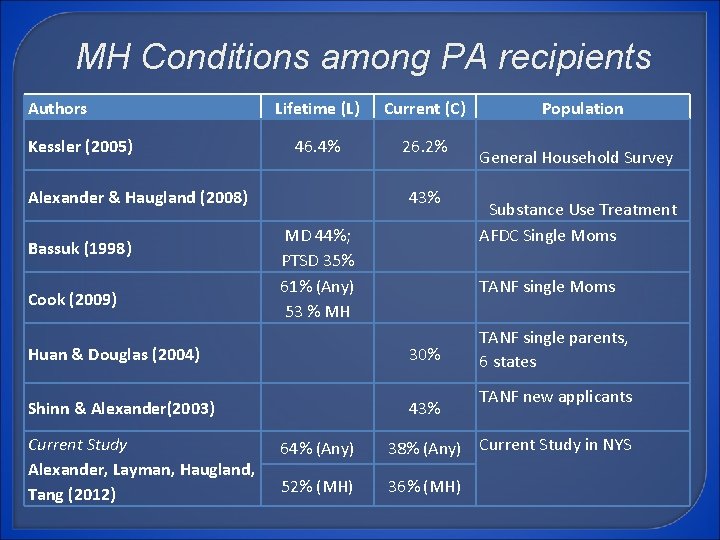
MH Conditions among PA recipients Authors Kessler (2005) Lifetime (L) Current (C) 46. 4% 26. 2% Alexander & Haugland (2008) Bassuk (1998) Cook (2009) 43% MD 44%; PTSD 35% 61% (Any) 53 % MH General Household Survey Substance Use Treatment AFDC Single Moms TANF single Moms Huan & Douglas (2004) 30% Shinn & Alexander(2003) 43% Current Study Alexander, Layman, Haugland, Tang (2012) Population TANF single parents, 6 states TANF new applicants 64% (Any) 38% (Any) Current Study in NYS 52% (MH) 36% (MH)
Why the MMS? Free Brief (22 items) Easy to use and score Computer based administration and scoring available Comprehensive (mood, anxiety, and psychosis) Excludes substance use (already screened by OTDA) Validated in NYS in Chemical Dependency OP & residential settings, street outreach programs, jails and shelters and now in local social service departments.
MMS Study in NYS Local Social Service Departments
Validation Study: Goals 1. Understand the extent of MH conditions and functioning among NYS beneficiaries 2. Validate the Modified Mini Screen (MMS) using the SCID 3. Develop decision rules for MH referrals
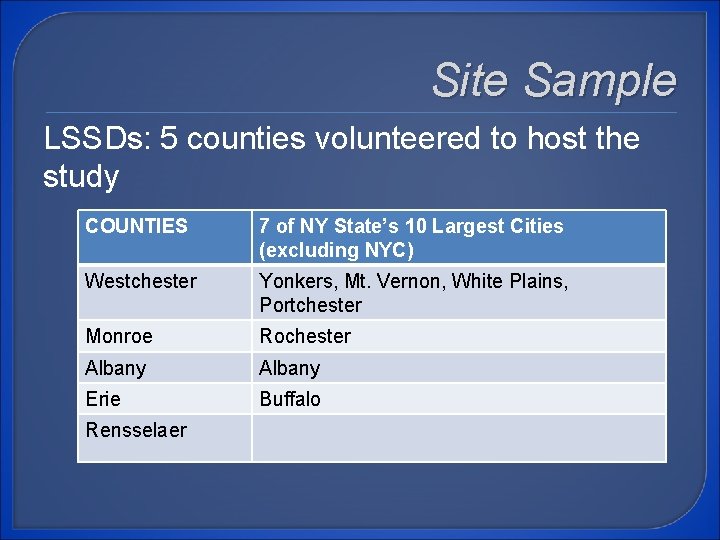
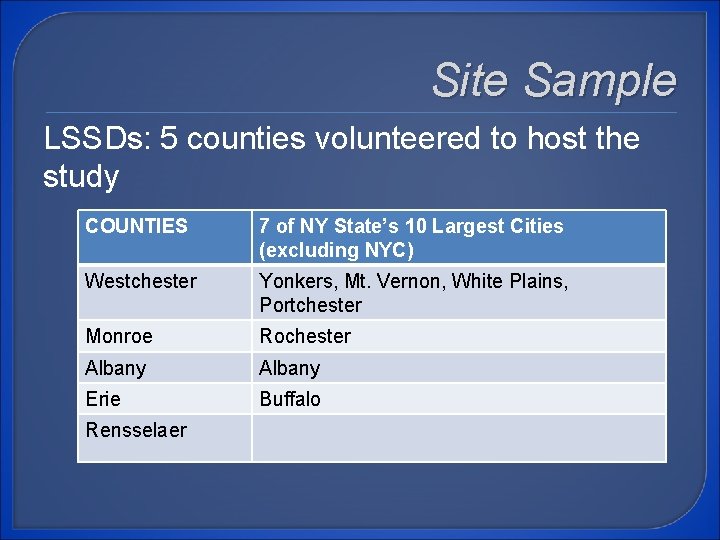
Site Sample LSSDs: 5 counties volunteered to host the study COUNTIES 7 of NY State’s 10 Largest Cities (excluding NYC) Westchester Yonkers, Mt. Vernon, White Plains, Portchester Monroe Rochester Albany Erie Buffalo Rensselaer
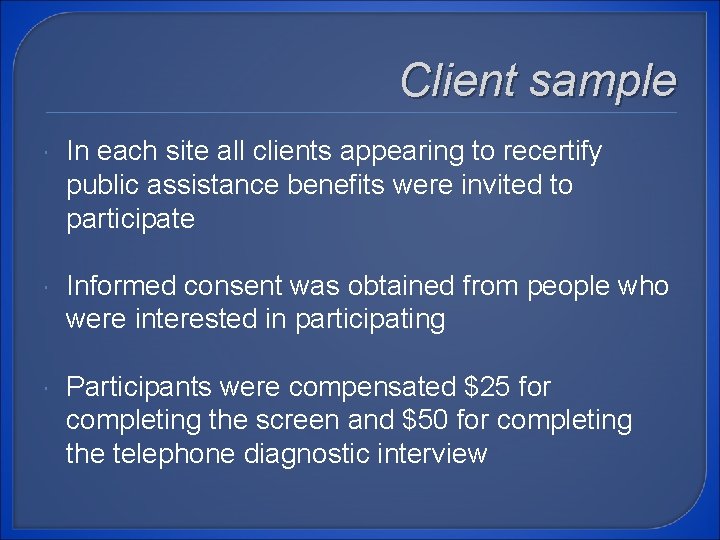
Client sample In each site all clients appearing to recertify public assistance benefits were invited to participate Informed consent was obtained from people who were interested in participating Participants were compensated $25 for completing the screen and $50 for completing the telephone diagnostic interview
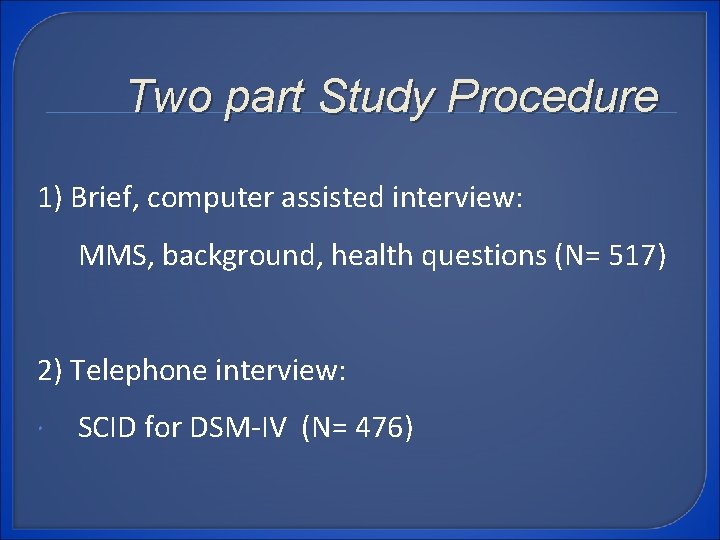
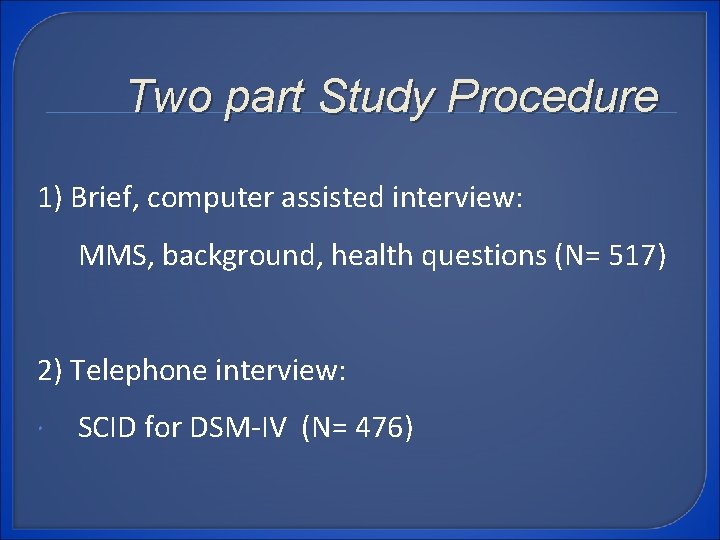
Two part Study Procedure 1) Brief, computer assisted interview: MMS, background, health questions (N= 517) 2) Telephone interview: SCID for DSM-IV (N= 476)
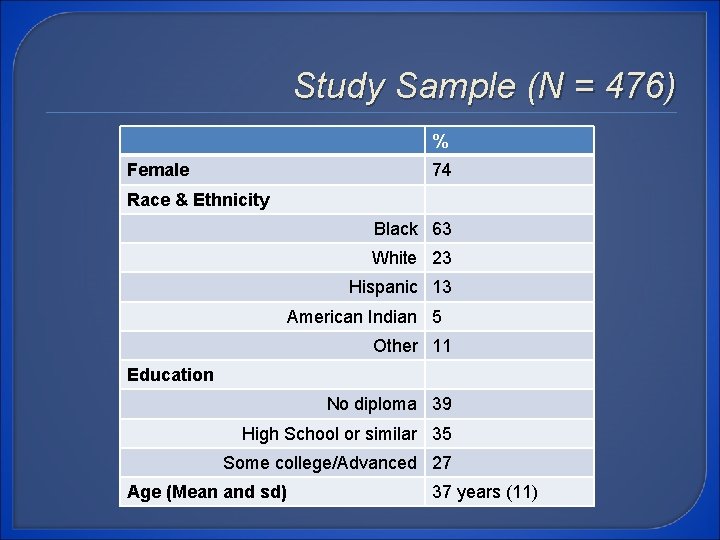
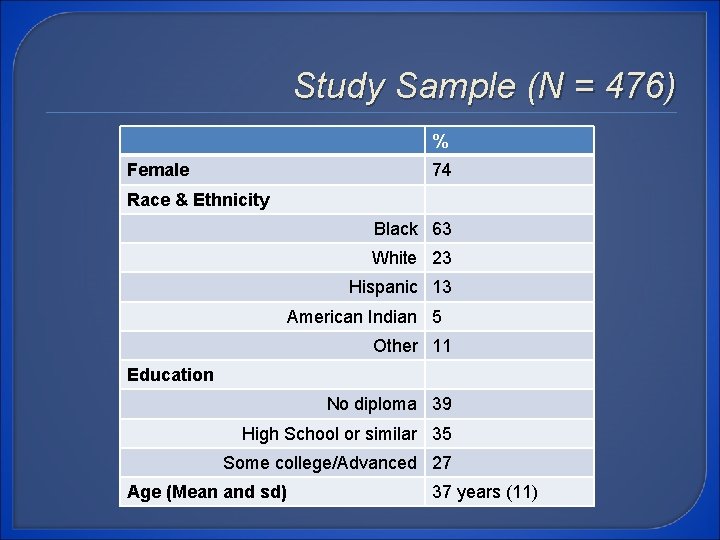
Study Sample (N = 476) % Female 74 Race & Ethnicity Black 63 White 23 Hispanic 13 American Indian 5 Other 11 Education No diploma 39 High School or similar 35 Some college/Advanced 27 Age (Mean and sd) 37 years (11)
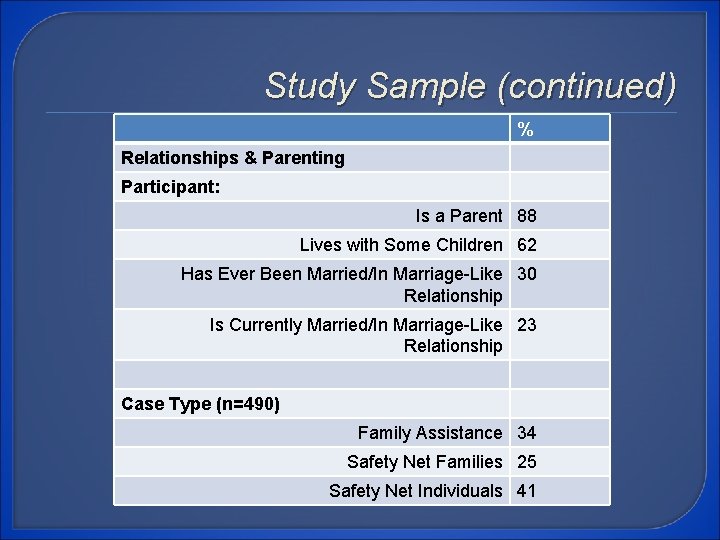
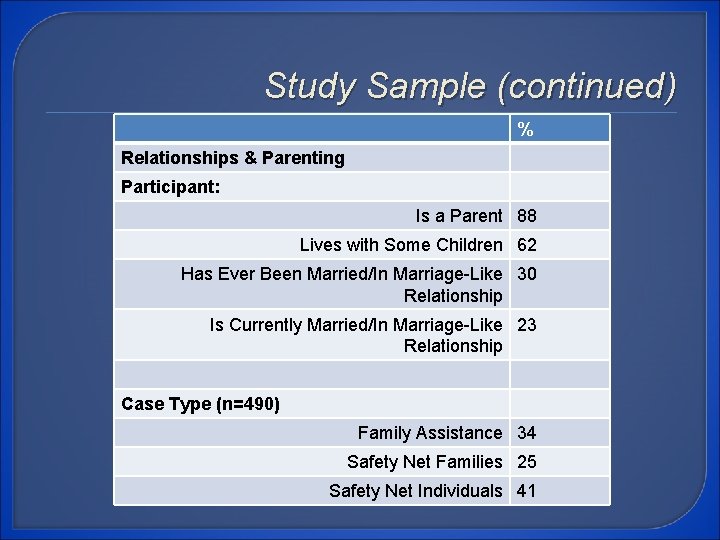
Study Sample (continued) % Relationships & Parenting Participant: Is a Parent 88 Lives with Some Children 62 Has Ever Been Married/In Marriage-Like 30 Relationship Is Currently Married/In Marriage-Like 23 Relationship Case Type (n=490) Family Assistance 34 Safety Net Families 25 Safety Net Individuals 41
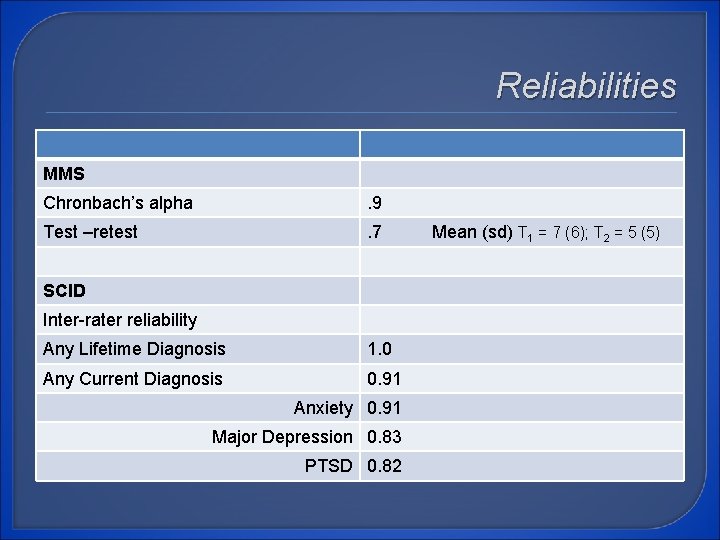
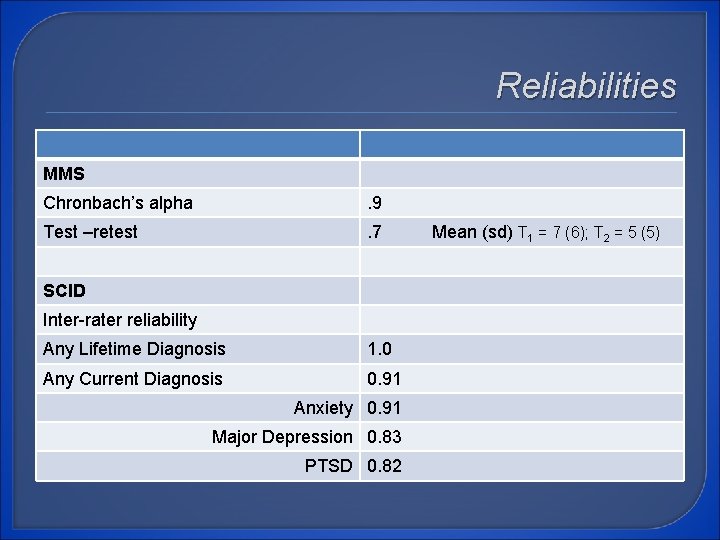
Reliabilities MMS Chronbach’s alpha . 9 Test –retest . 7 SCID Inter-rater reliability Any Lifetime Diagnosis 1. 0 Any Current Diagnosis 0. 91 Anxiety 0. 91 Major Depression 0. 83 PTSD 0. 82 Mean (sd) T 1 = 7 (6); T 2 = 5 (5)
What we learned about Mental Health, Health & Functioning
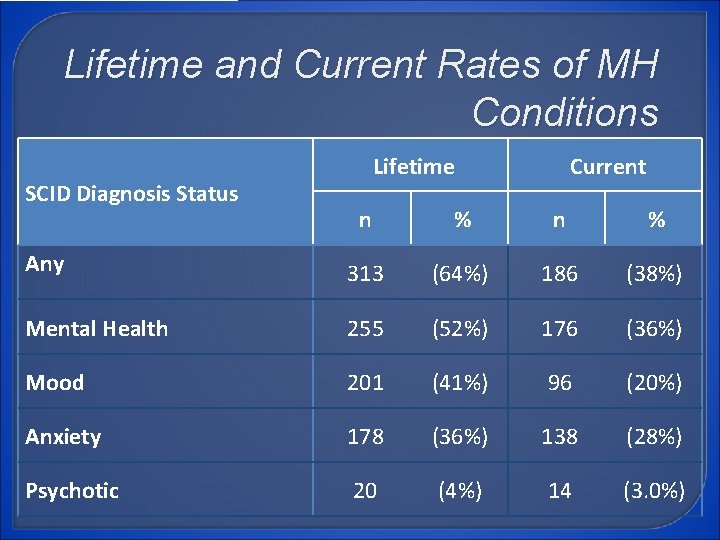
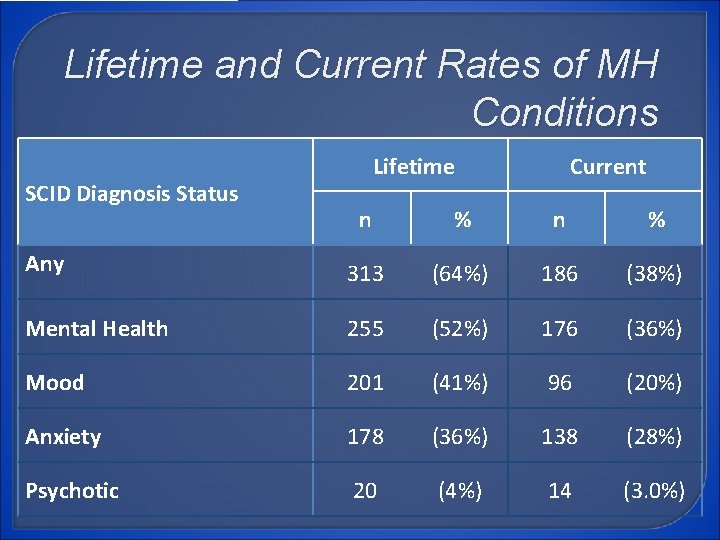
Lifetime and Current Rates of MH Conditions SCID Diagnosis Status Lifetime Current n % Any 313 (64%) 186 (38%) Mental Health 255 (52%) 176 (36%) Mood 201 (41%) 96 (20%) Anxiety 178 (36%) 138 (28%) Psychotic 20 (4%) 14 (3. 0%)
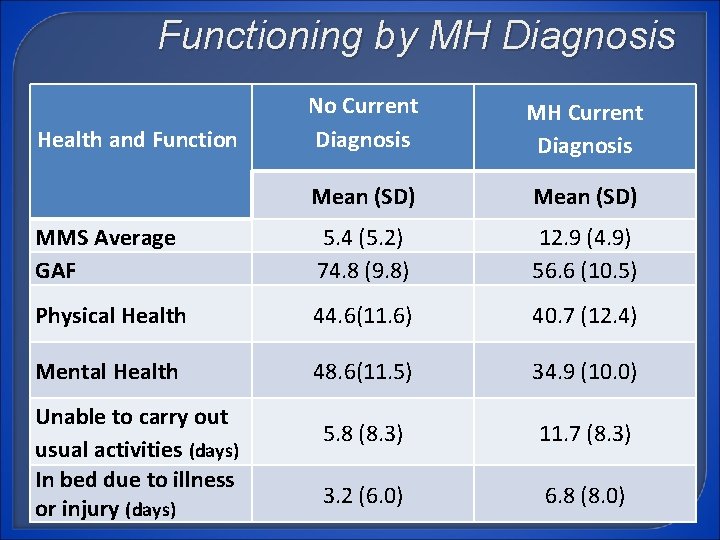
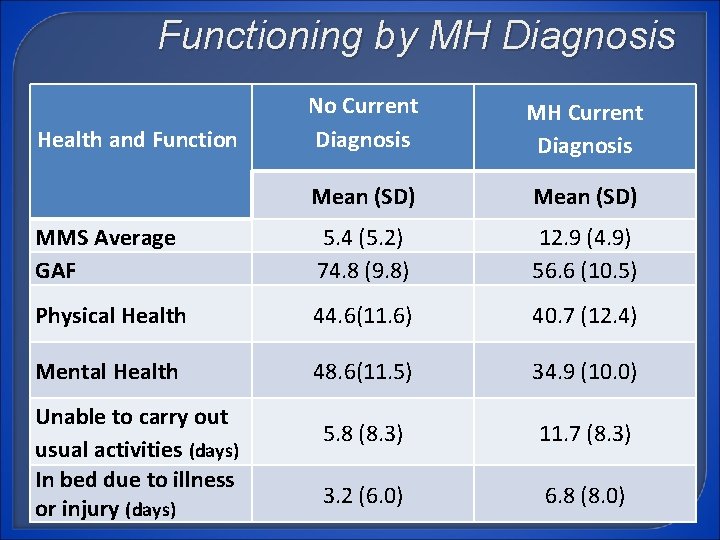
Functioning by MH Diagnosis No Current Diagnosis MH Current Diagnosis Mean (SD) MMS Average GAF 5. 4 (5. 2) 74. 8 (9. 8) 12. 9 (4. 9) 56. 6 (10. 5) Physical Health 44. 6(11. 6) 40. 7 (12. 4) Mental Health 48. 6(11. 5) 34. 9 (10. 0) 5. 8 (8. 3) 11. 7 (8. 3) 3. 2 (6. 0) 6. 8 (8. 0) Health and Function Unable to carry out usual activities (days) In bed due to illness or injury (days)
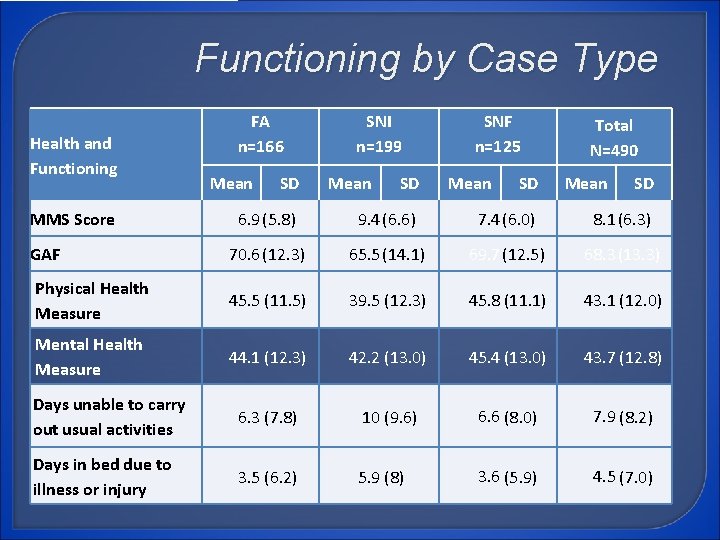
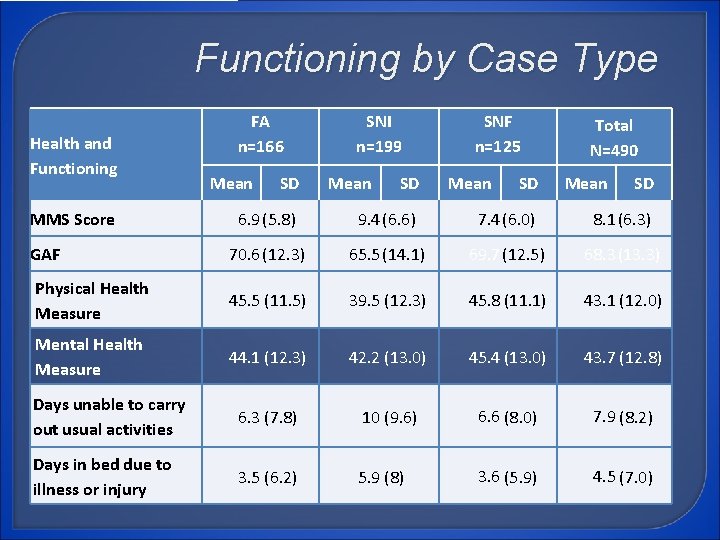
Functioning by Case Type Health and Functioning MMS Score FA n=166 Mean SD SNI n=199 Mean SD SNF n=125 Mean SD Total N=490 Mean SD 6. 9(5. 8) 9. 4(6. 6) 7. 4(6. 0) 8. 1(6. 3) GAF 70. 6 (12. 3) 65. 5 (14. 1) 69. 7 (12. 5) 68. 3 (13. 3) Physical Health Measure 45. 5 (11. 5) 39. 5 (12. 3) 45. 8 (11. 1) 43. 1 (12. 0) Mental Health Measure 44. 1 (12. 3) 42. 2 (13. 0) 45. 4 (13. 0) 43. 7 (12. 8) Days unable to carry out usual activities 6. 3 (7. 8) 10 (9. 6) 6. 6 (8. 0) 7. 9 (8. 2) Days in bed due to illness or injury 3. 5 (6. 2) 5. 9 (8) 3. 6 (5. 9) 4. 5 (7. 0)
What did we learn about MH? Over 1/3 rd of our sample met criteria for Current MH condition Over 60% of our sample met criteria for Lifetime MH condition All participants reported lower levels of functioning than the general population Participants with a Current MH condition reported poorer health and functioning than participants with No MH condition Safety Net Individuals and older participants reported poorer health and functioning and higher rates of all MH conditions than TANF and Safety Net Families
What did we learn about MH? Over a lifetime, mood disorders were most common (41% of all participants) In the past month, anxiety disorders were the most common (28% of all participants) 269 (55%) participants experienced a traumatic event in their lifetime 65 (13%) percent met criteria for PTSD in their lifetime
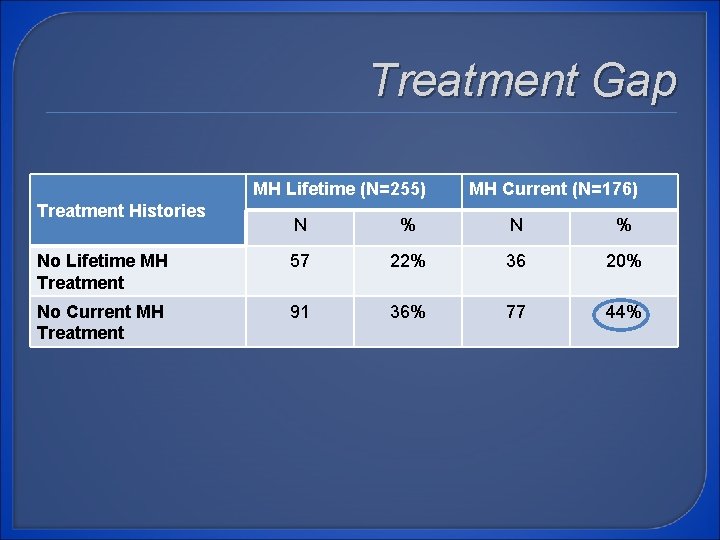
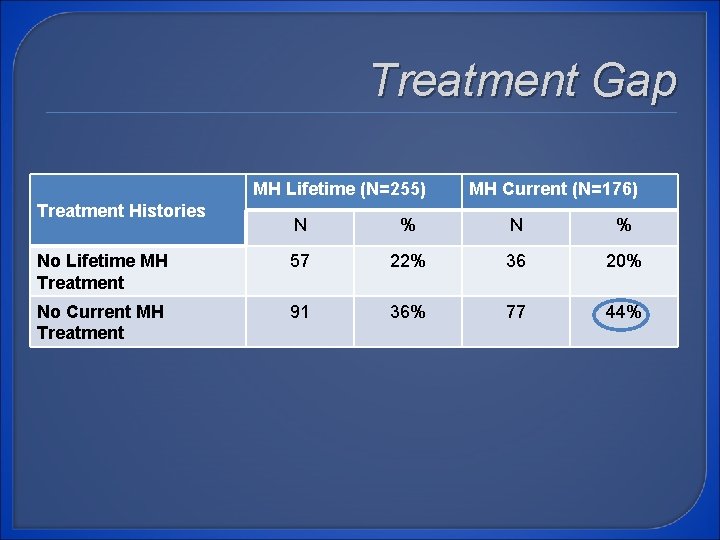
Treatment Gap MH Lifetime (N=255) Treatment Histories MH Current (N=176) N % No Lifetime MH Treatment 57 22% 36 20% No Current MH Treatment 91 36% 77 44%
Decision Rules
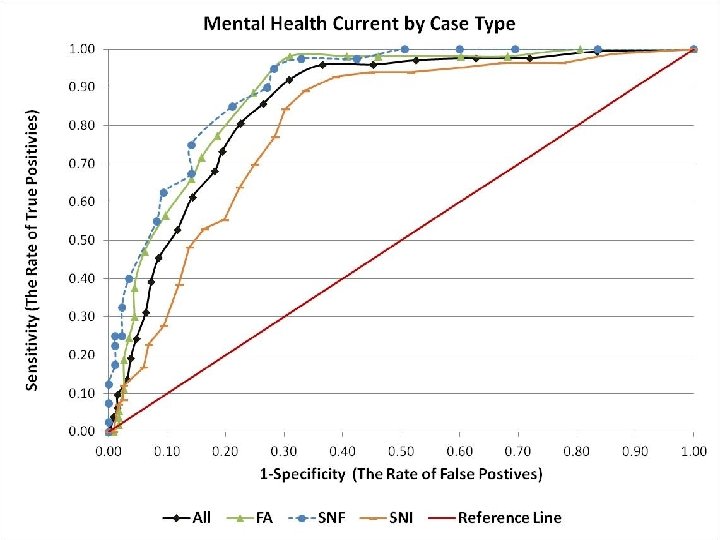
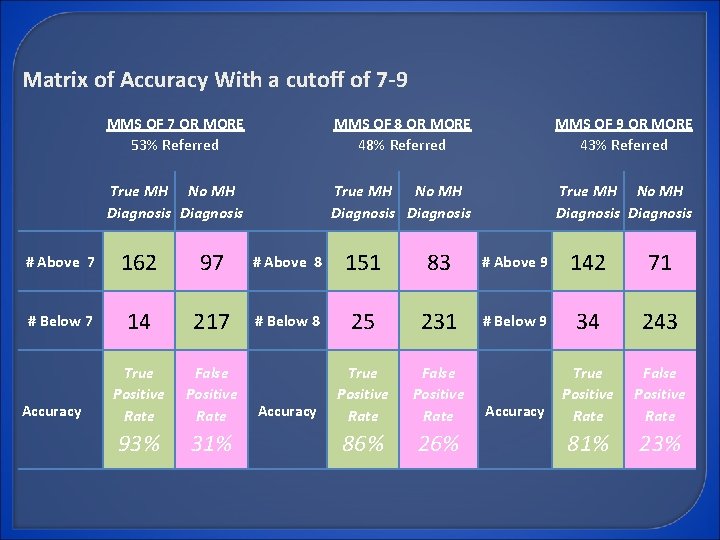
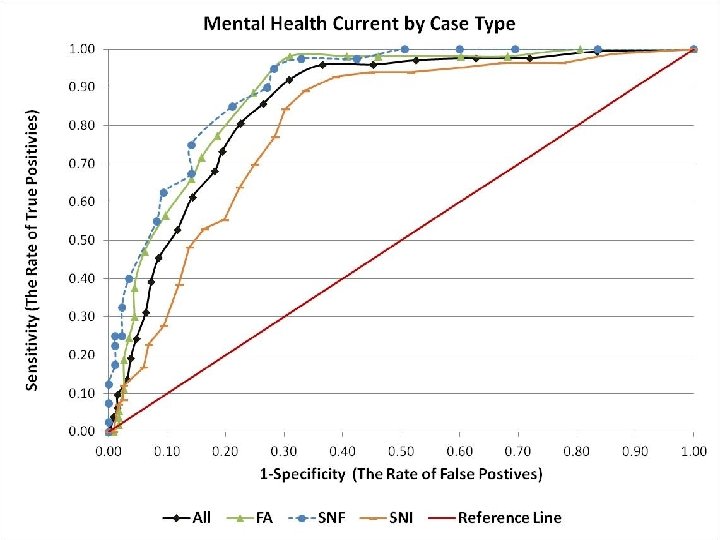
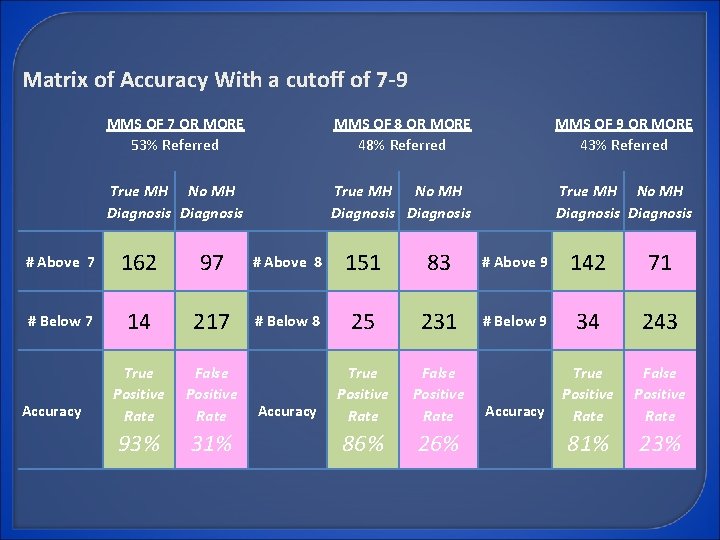
Matrix of Accuracy With a cutoff of 7 -9 MMS OF 7 OR MORE 53% Referred MMS OF 8 OR MORE 48% Referred MMS OF 9 OR MORE 43% Referred True MH No MH Diagnosis True MH No MH Diagnosis # Above 7 162 97 # Above 8 151 83 # Above 9 142 71 # Below 7 14 217 # Below 8 25 231 # Below 9 34 243 True Positive Rate False Positive Rate Accuracy True Positive Rate False Positive Rate 93% 31% 86% 26% 81% 23% Accuracy
Policy considerations
Policy Implications The MMS is a reliable and accurate screen for use in Local Social Service Departments Best “statistical” balance between true and false positives occurs between MMS scores 7 -9 Decision rules should be based on local capacity Screen should be optional for localities Screen should be optional for individuals
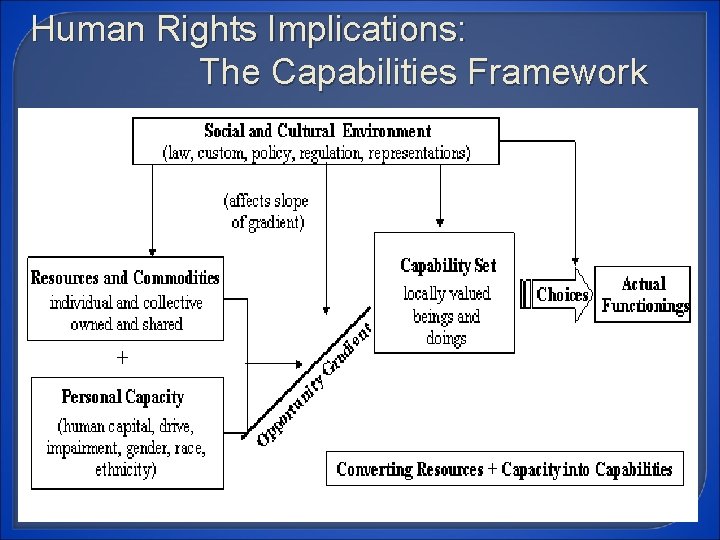
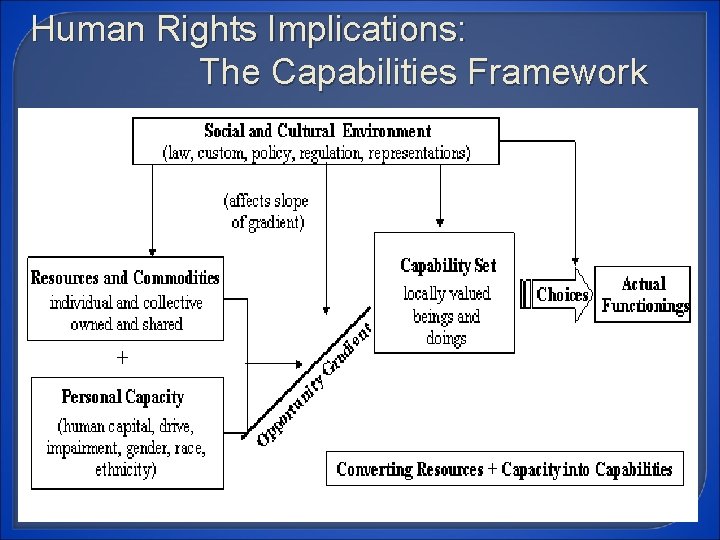
Human Rights Implications: The Capabilities Framework NKI Center to Study Recovery in Social Contexts. Adapted from Sen