Vaginitis Pelvic Inflammatory Disease Denver Prevention Training Center


- Slides: 65
Vaginitis & Pelvic Inflammatory Disease Denver Prevention Training Center Denver Public Health 2016
Disclosures Source: Grace Alfonsi, MD, has no paid professional relationships to disclose
Objectives Source: Be able to identify epidemiology, symptomatology, diagnosis, and treatment modalities for vaginal infections.
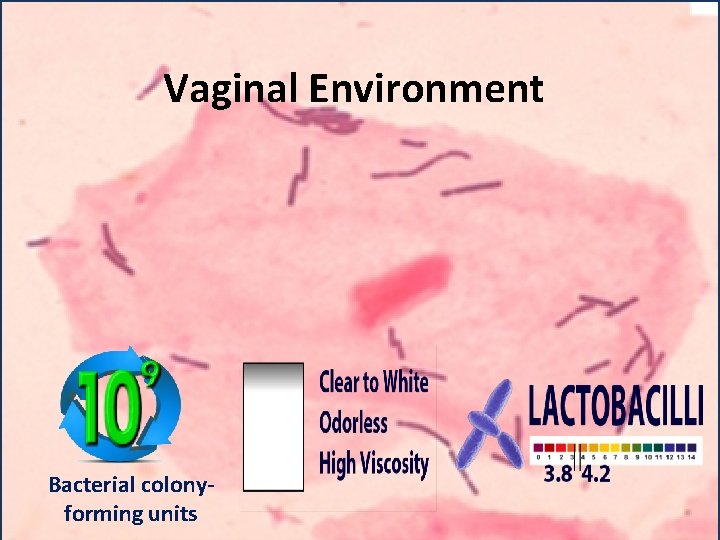
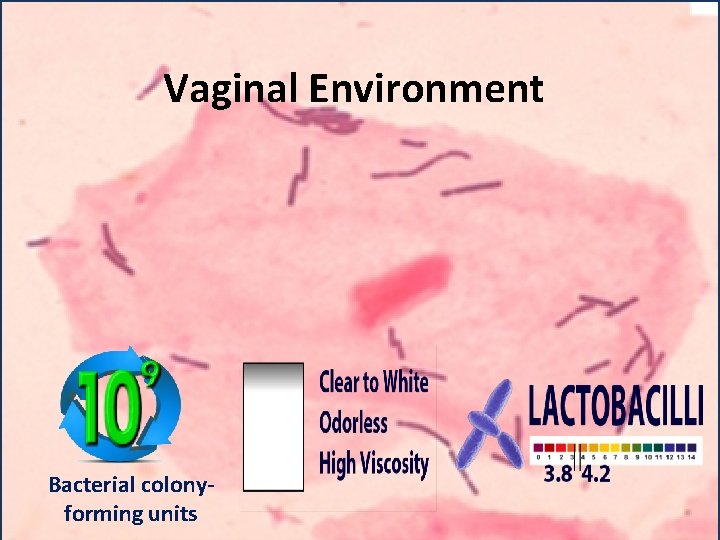
Vaginal Environment Bacterial colonyforming units
Vaginal discharge Clinical manifestations of vaginitis Vulvar itching Irritation Odor
Which of the following types of vaginitis occurs most frequently? 1. 2. 3. 4. Bacterial vaginosis Candidiasis Trichomoniasis Atrophic vaginitis
Which of the following types of vaginitis occurs most frequently? 1. 2. 3. 4. Bacterial vaginosis Candidiasis Trichomoniasis Atrophic vaginitis
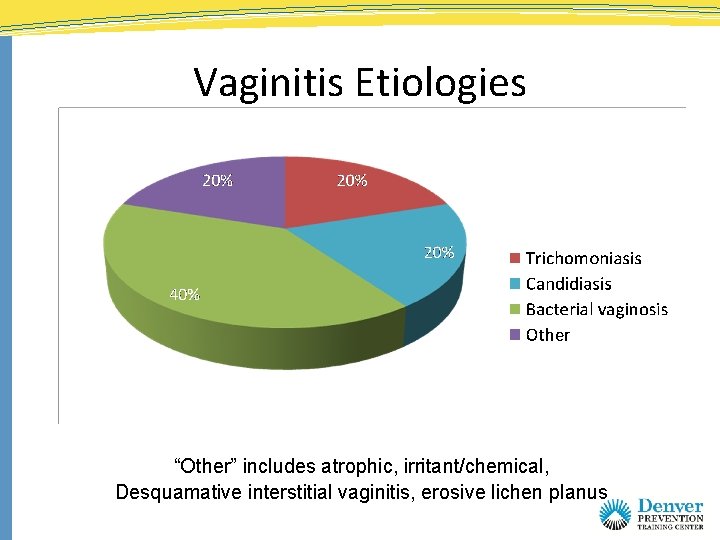
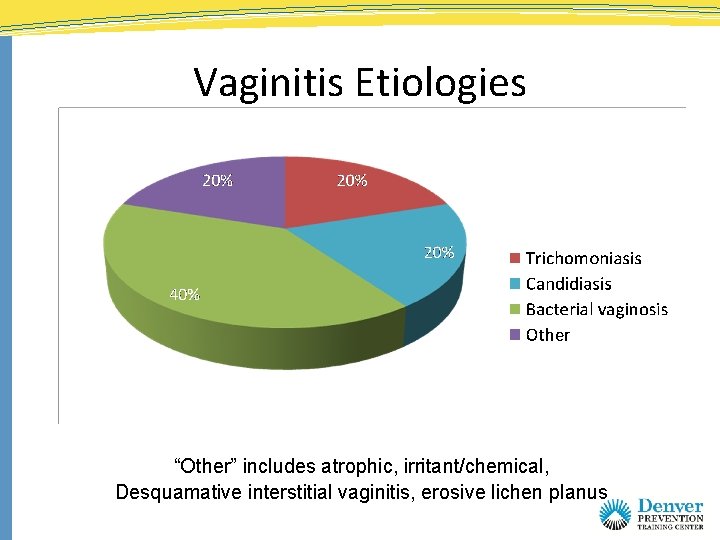
Vaginitis Etiologies “Other” includes atrophic, irritant/chemical, Desquamative interstitial vaginitis, erosive lichen planus
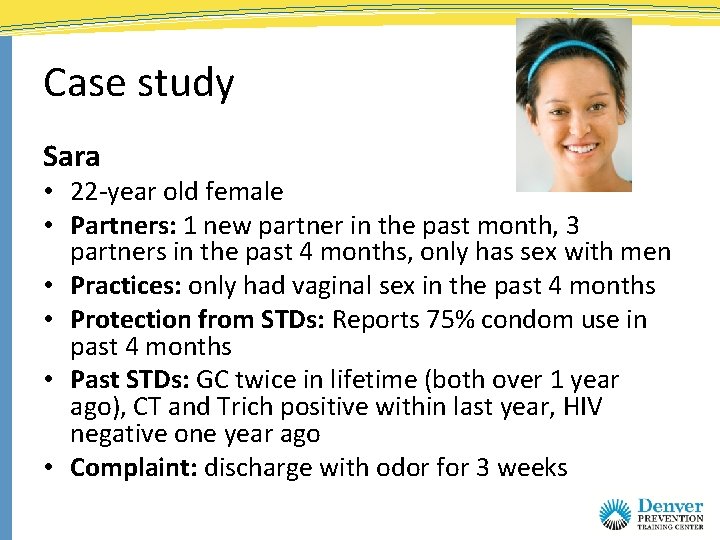
Case study Sara • 22 -year old female • Partners: 1 new partner in the past month, 3 partners in the past 4 months, only has sex with men • Practices: only had vaginal sex in the past 4 months • Protection from STDs: Reports 75% condom use in past 4 months • Past STDs: GC twice in lifetime (both over 1 year ago), CT and Trich positive within last year, HIV negative one year ago • Complaint: discharge with odor for 3 weeks
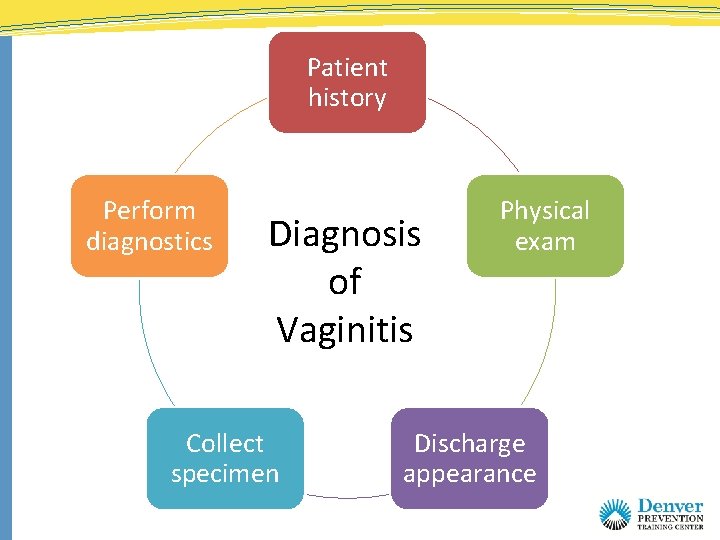
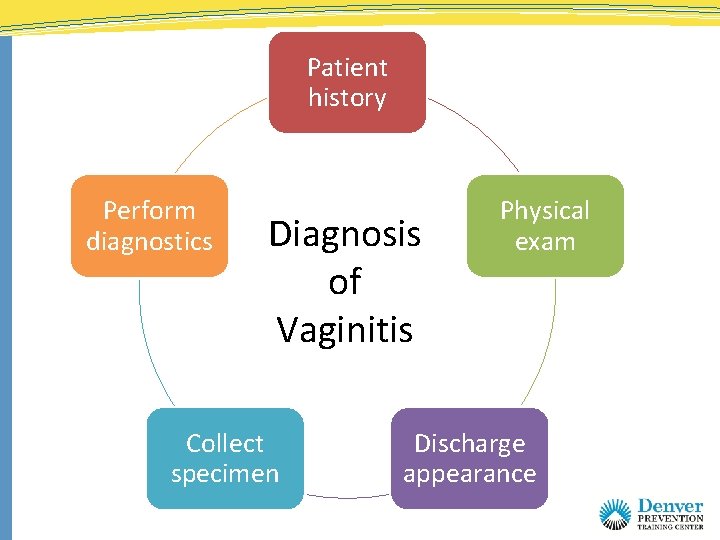
Patient history Perform diagnostics Diagnosis of Vaginitis Collect specimen Physical exam Discharge appearance

Source: DMHC
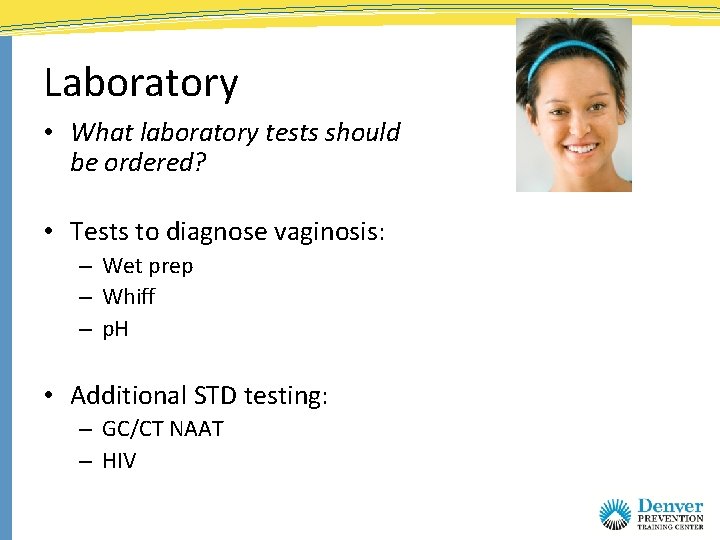
Laboratory • What laboratory tests should be ordered? • Tests to diagnose vaginosis: – Wet prep – Whiff – p. H • Additional STD testing: – GC/CT NAAT – HIV
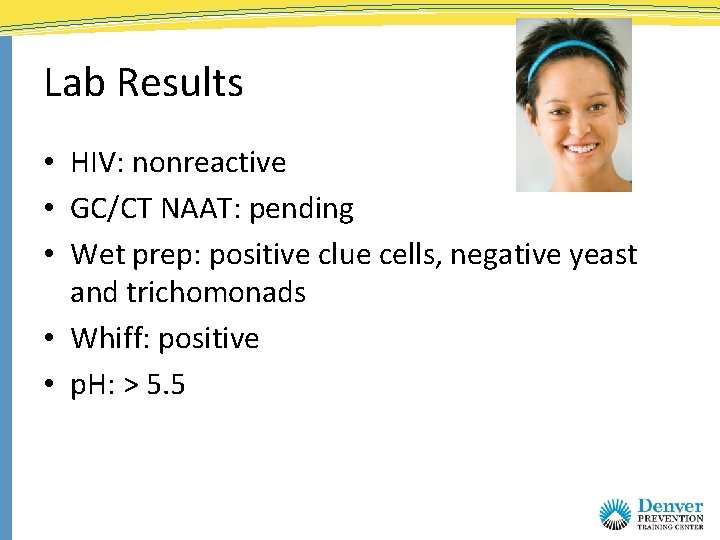
Lab Results • HIV: nonreactive • GC/CT NAAT: pending • Wet prep: positive clue cells, negative yeast and trichomonads • Whiff: positive • p. H: > 5. 5
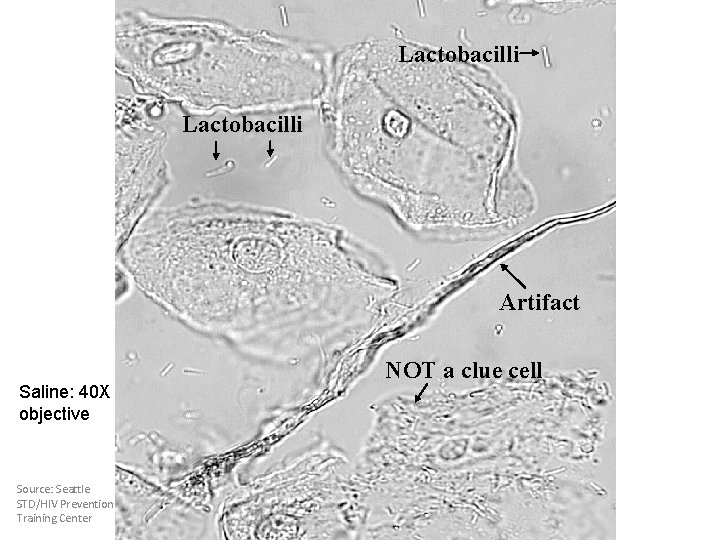
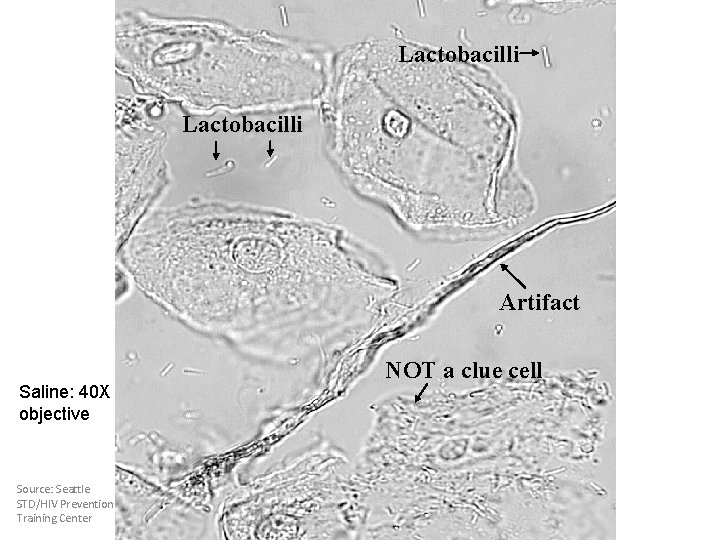
Lactobacilli Artifact Saline: 40 X objective Source: Seattle STD/HIV Prevention Training Center NOT a clue cell
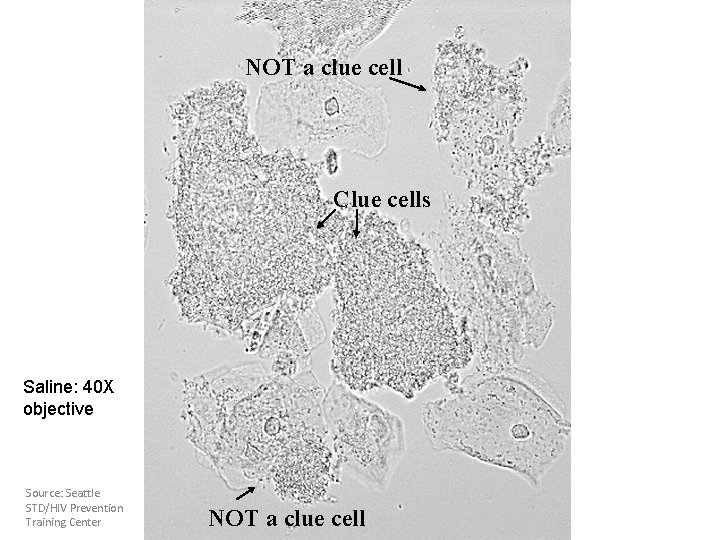
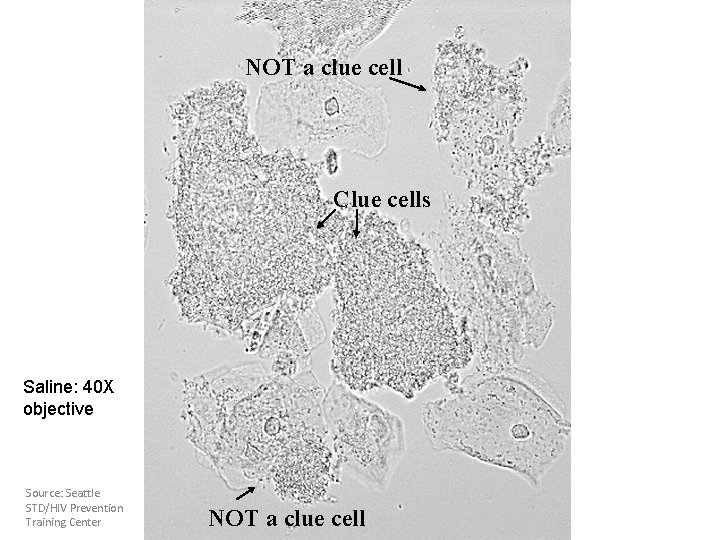
NOT a clue cell Clue cells Saline: 40 X objective Source: Seattle STD/HIV Prevention Training Center NOT a clue cell
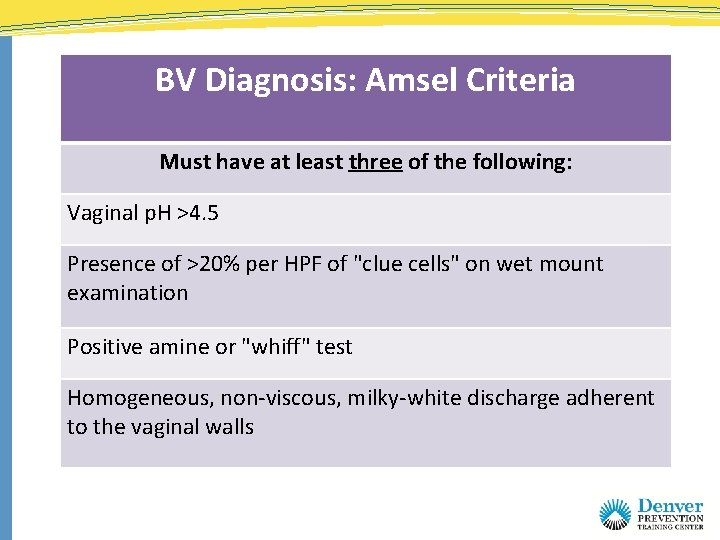
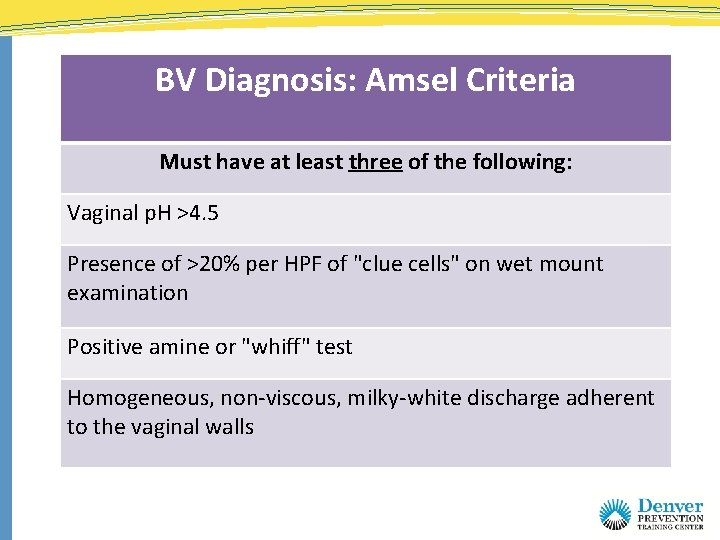
BV Diagnosis: Amsel Criteria Must have at least three of the following: Vaginal p. H >4. 5 Presence of >20% per HPF of "clue cells" on wet mount examination Positive amine or "whiff" test Homogeneous, non-viscous, milky-white discharge adherent to the vaginal walls
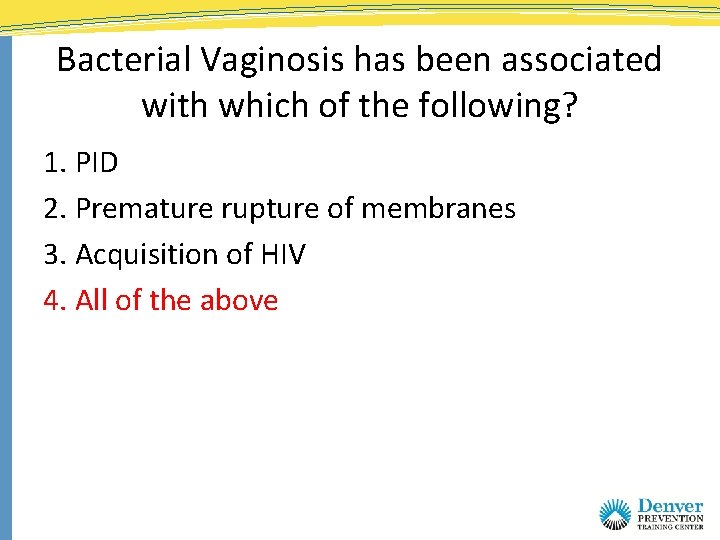
Bacterial Vaginosis has been associated with which of the following? 1. 2. 3. 4. PID Premature rupture of membranes Acquisition of HIV All of the above
Bacterial Vaginosis has been associated with which of the following? 1. PID 2. Premature rupture of membranes 3. Acquisition of HIV 4. All of the above
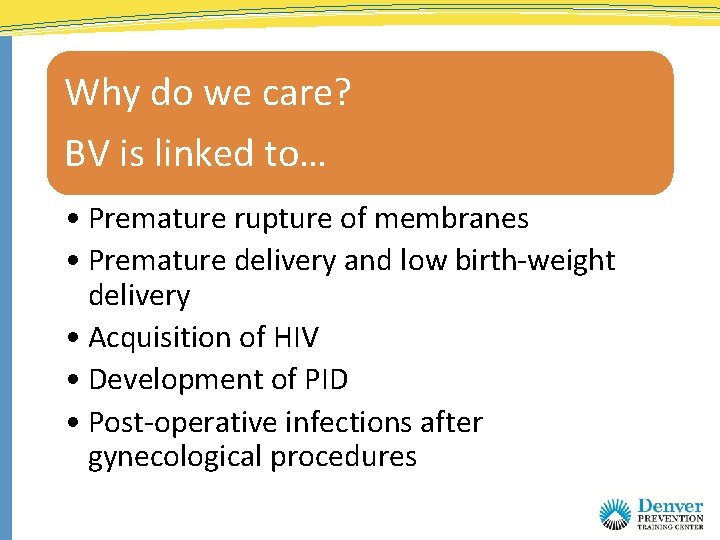
Why do we care? BV is linked to… • Premature rupture of membranes • Premature delivery and low birth-weight delivery • Acquisition of HIV • Development of PID • Post-operative infections after gynecological procedures
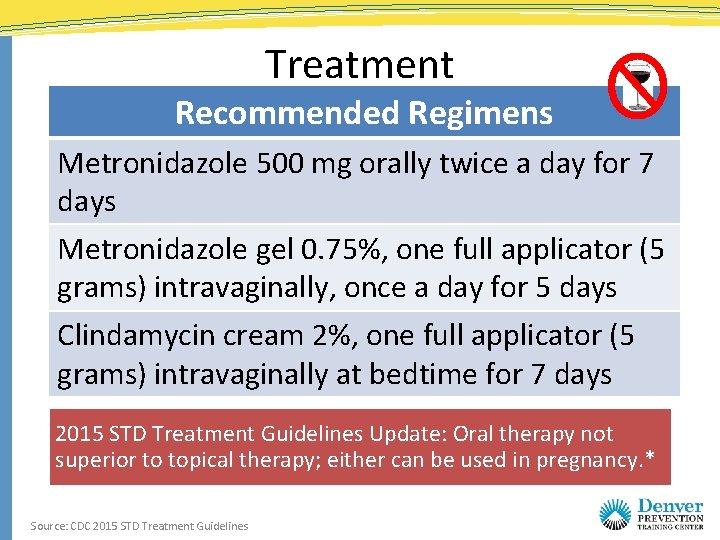
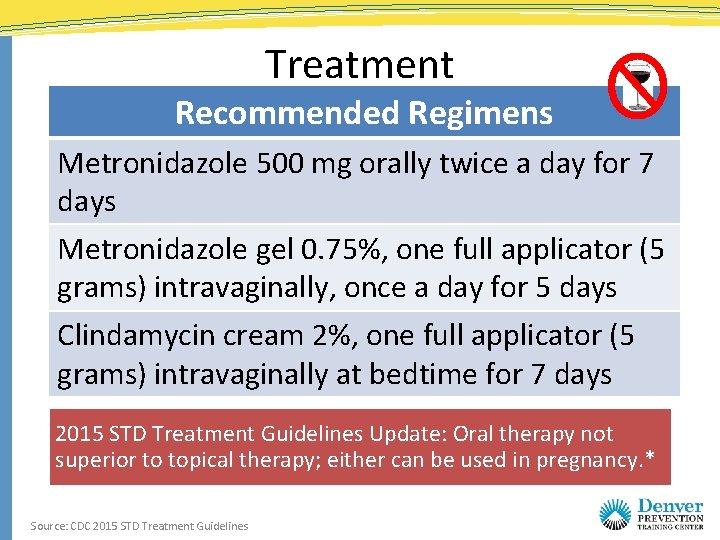
Treatment Recommended Regimens Metronidazole 500 mg orally twice a day for 7 days Metronidazole gel 0. 75%, one full applicator (5 grams) intravaginally, once a day for 5 days Clindamycin cream 2%, one full applicator (5 grams) intravaginally at bedtime for 7 days 2015 STD Treatment Guidelines Update: Oral therapy not superior to topical therapy; either can be used in pregnancy. * Source: CDC 2015 STD Treatment Guidelines
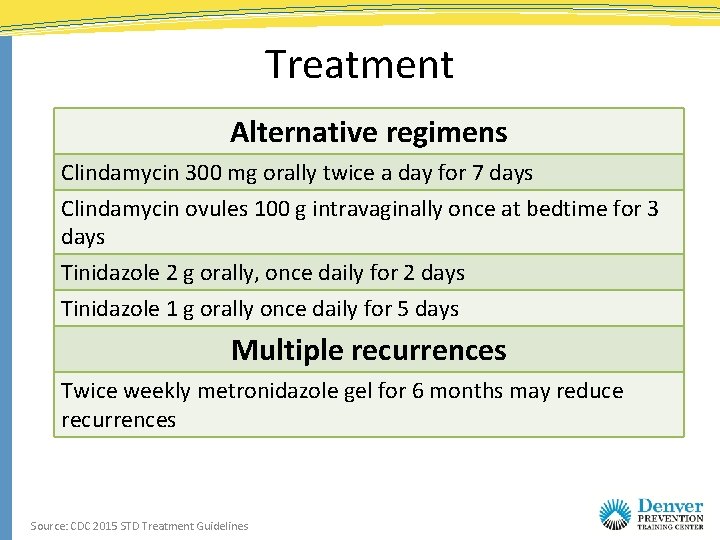
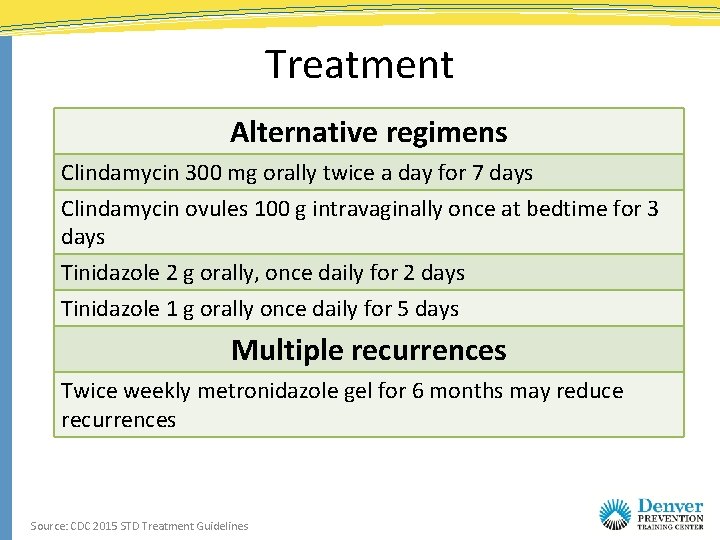
Treatment Alternative regimens Clindamycin 300 mg orally twice a day for 7 days Clindamycin ovules 100 g intravaginally once at bedtime for 3 days Tinidazole 2 g orally, once daily for 2 days Tinidazole 1 g orally once daily for 5 days Multiple recurrences Twice weekly metronidazole gel for 6 months may reduce recurrences Source: CDC 2015 STD Treatment Guidelines
Screening and Treatment in Asymptomatic Patients
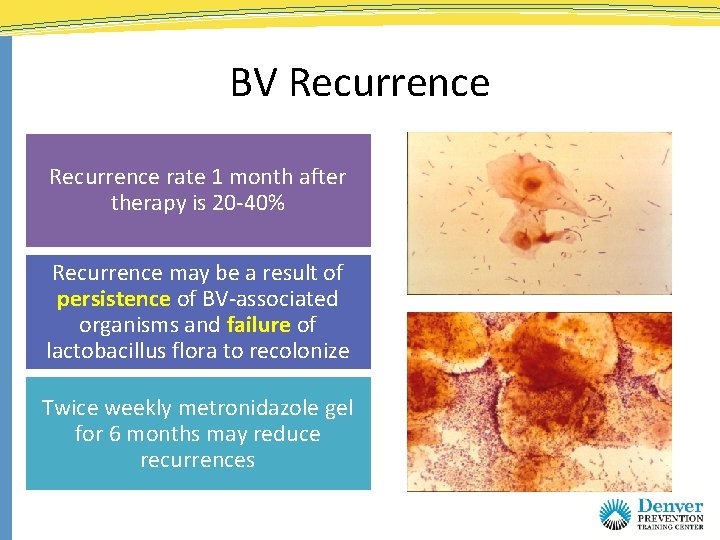
BV Recurrence rate 1 month after therapy is 20 -40% Recurrence may be a result of persistence of BV-associated organisms and failure of lactobacillus flora to recolonize Twice weekly metronidazole gel for 6 months may reduce recurrences
Risk factors for Developing BV • Sexual activity – new and multiple male and female partners • Douching • Cigarette Smoking (women) Potentially protective • Estrogen containing contraceptives • Condom use
Case study Tanya • 24 -year-old single female • Partners: 2 sex partners during the past year • Protection from STDs: no condoms with recent partners • Past history: Trichomoniasis 1 year ago at last check-up • Protection from pregnancy: oral contraceptives • Complaint: Smelly, yellow vaginal discharge and slight dysuria for 1 week; no vulvar itching, pelvic pain, or fever
Physical Exam • External genitalia: Normal with a few excoriations near the introitus, but no other lesions • Speculum exam: Moderate amount of frothy, yellowish, malodorous discharge, without visible cervical mucopus or easily induced cervical bleeding • Bimanual examination: Normal without uterine or adnexal tenderness
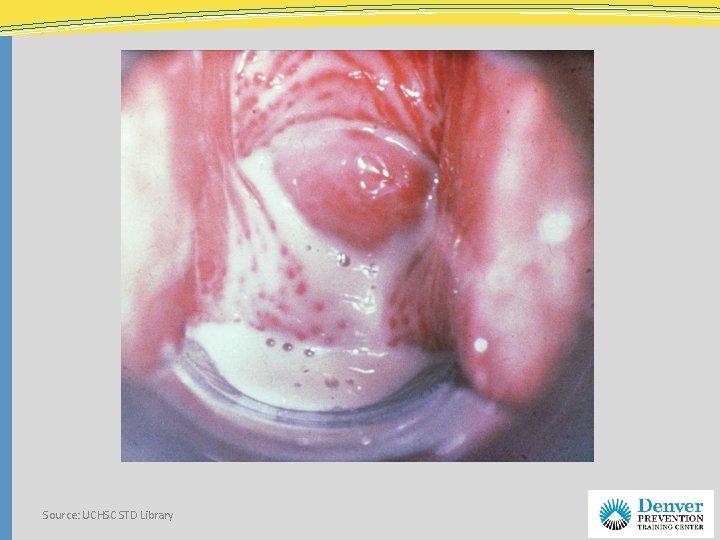
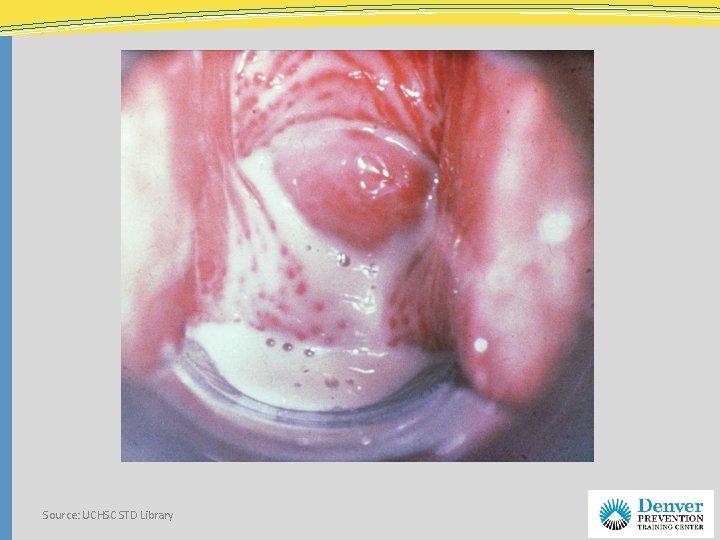
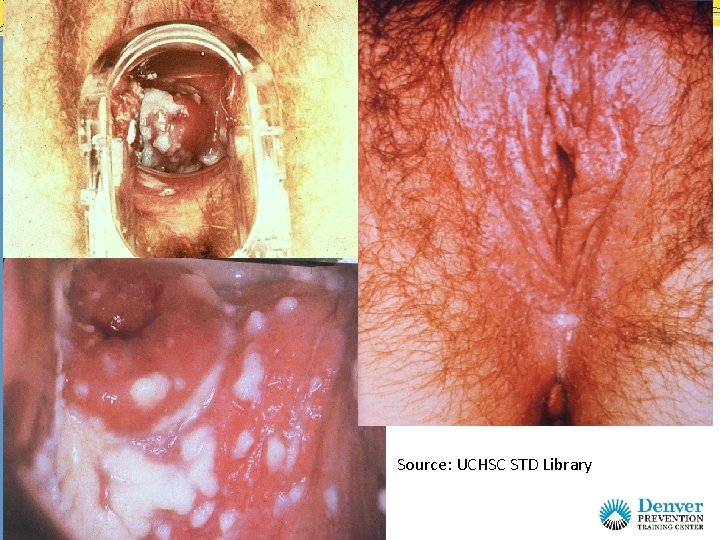
Source: UCHSC STD Library
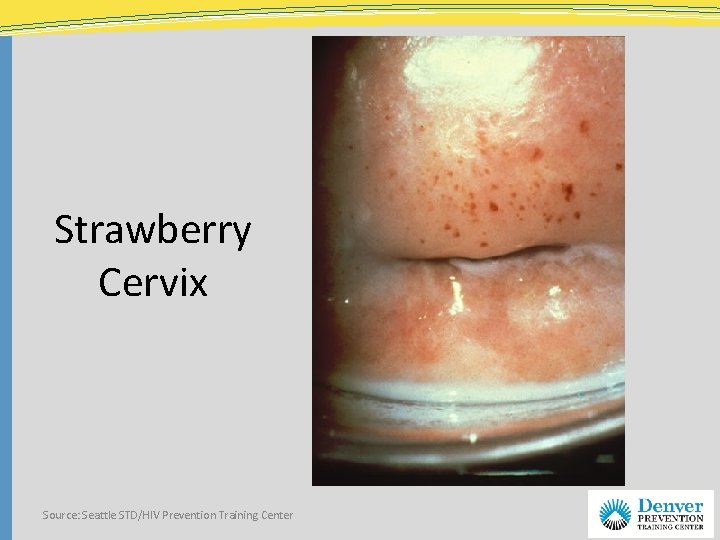
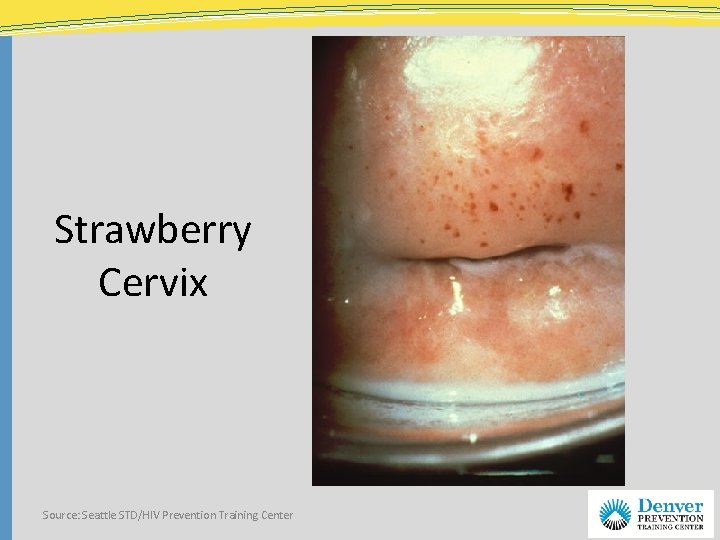
Strawberry Cervix Source: Seattle STD/HIV Prevention Training Center
Based on history and exam, what tests should we do now? Vaginal Ph Whiff test Wet Prep
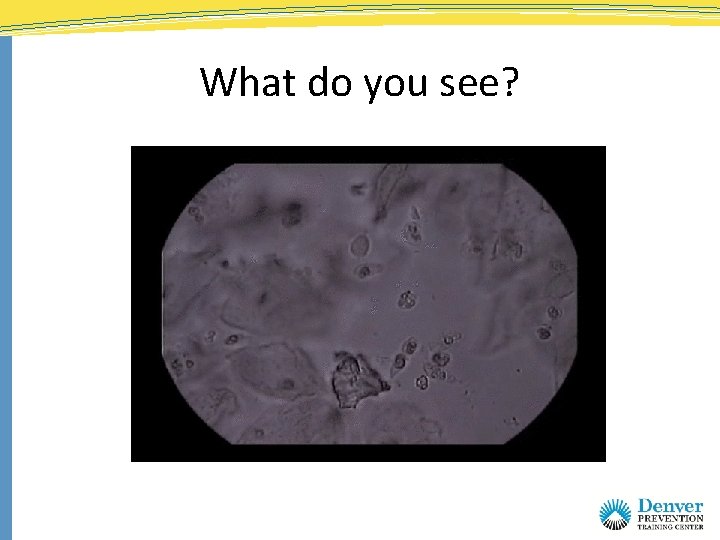
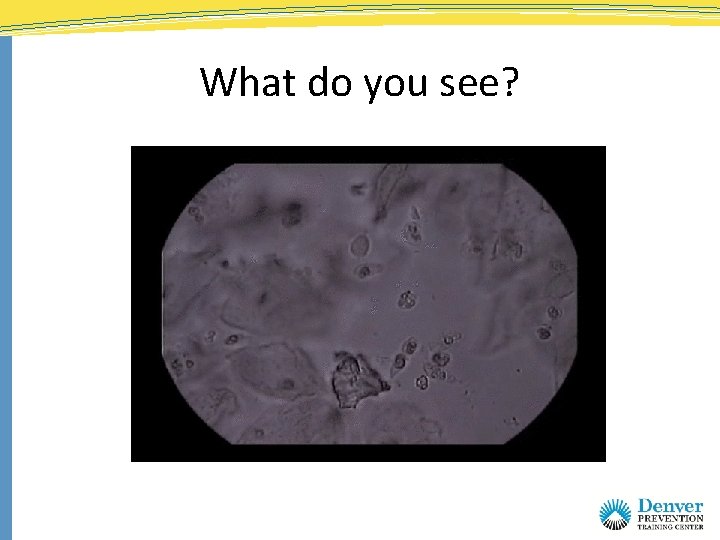
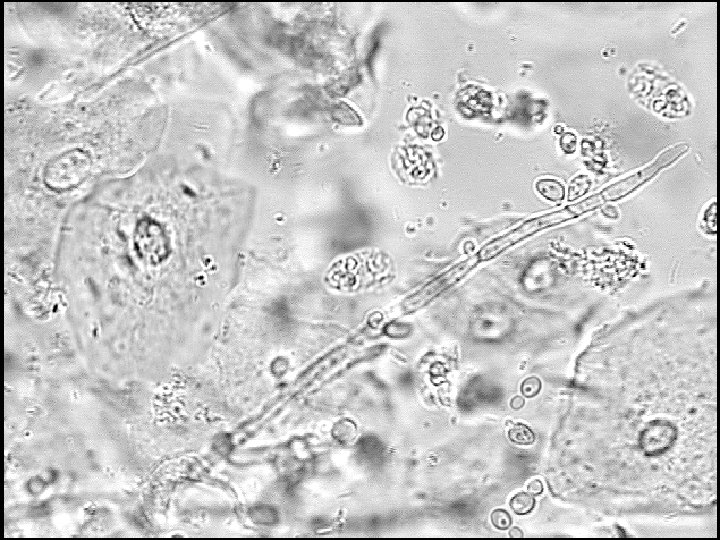
What do you see?
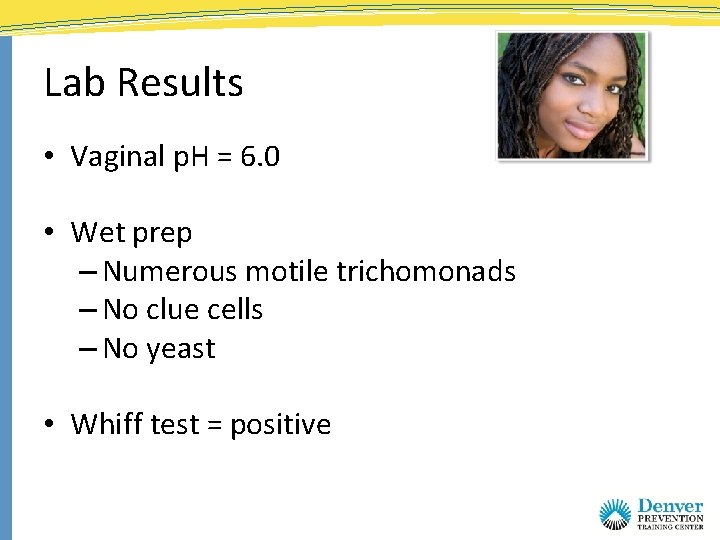
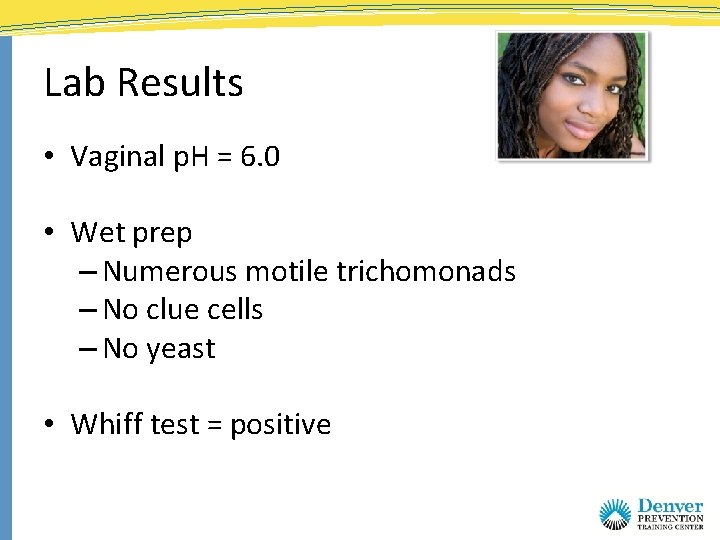
Lab Results • Vaginal p. H = 6. 0 • Wet prep – Numerous motile trichomonads – No clue cells – No yeast • Whiff test = positive
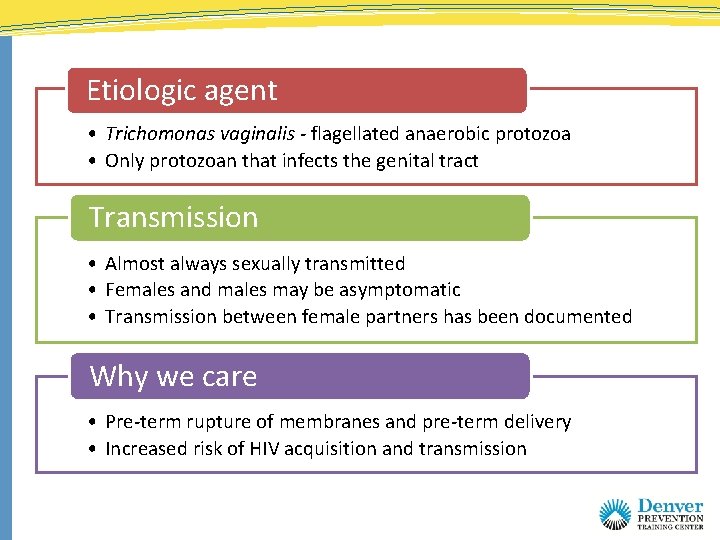
Etiologic agent • Trichomonas vaginalis - flagellated anaerobic protozoa • Only protozoan that infects the genital tract Transmission • Almost always sexually transmitted • Females and males may be asymptomatic • Transmission between female partners has been documented Why we care • Pre-term rupture of membranes and pre-term delivery • Increased risk of HIV acquisition and transmission
T. Vaginalis in Men • Found in 13 -17 % men with NGU • Found in 11 – 14% of asymptomatic men • Most infected men are asymptomatic • Diagnostic test seldom available • Men treated usually through partner diagnosis Source: Sexually Transmitted Diseases, 4 th ed. Sex Transm Infect 2000; 76: 355. J Infect Dis 2003; 188: 465 -8.
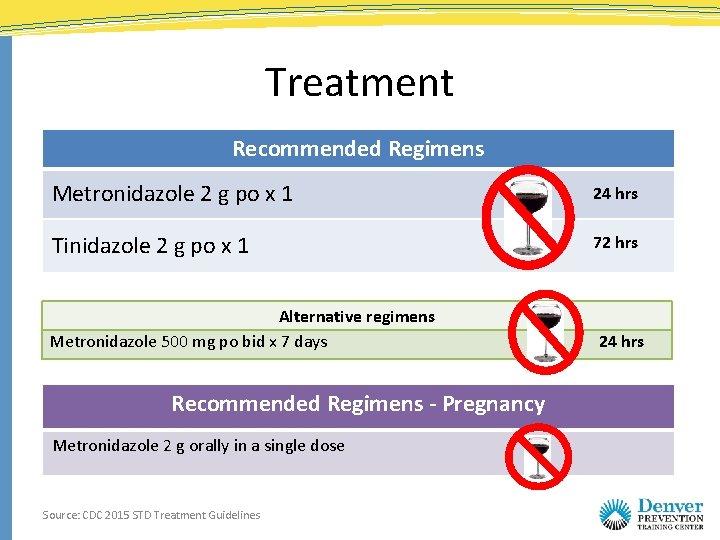
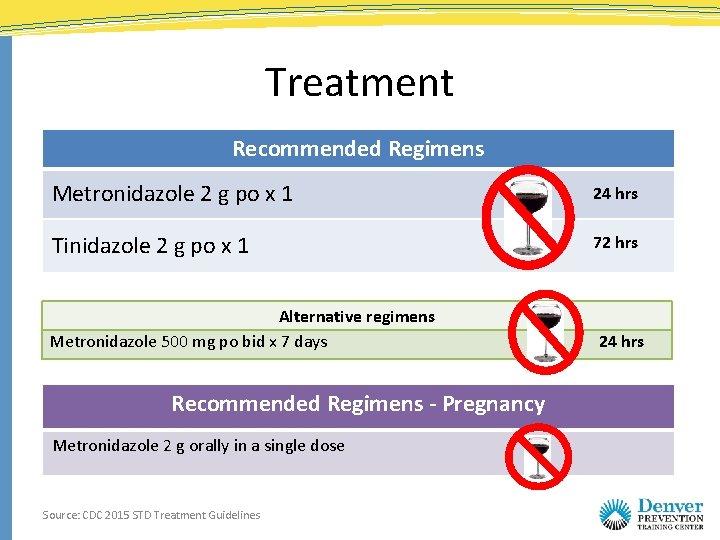
Treatment Recommended Regimens Metronidazole 2 g po x 1 24 hrs Tinidazole 2 g po x 1 72 hrs Alternative regimens Metronidazole 500 mg po bid x 7 days Recommended Regimens - Pregnancy Metronidazole 2 g orally in a single dose Source: CDC 2015 STD Treatment Guidelines 24 hrs
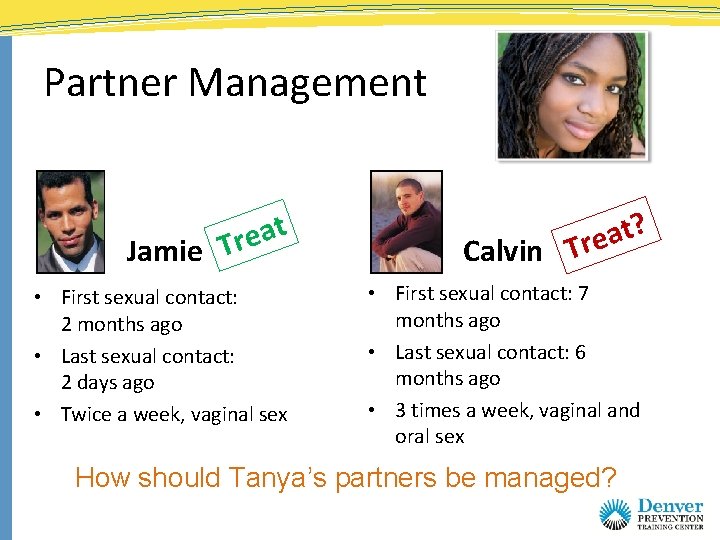
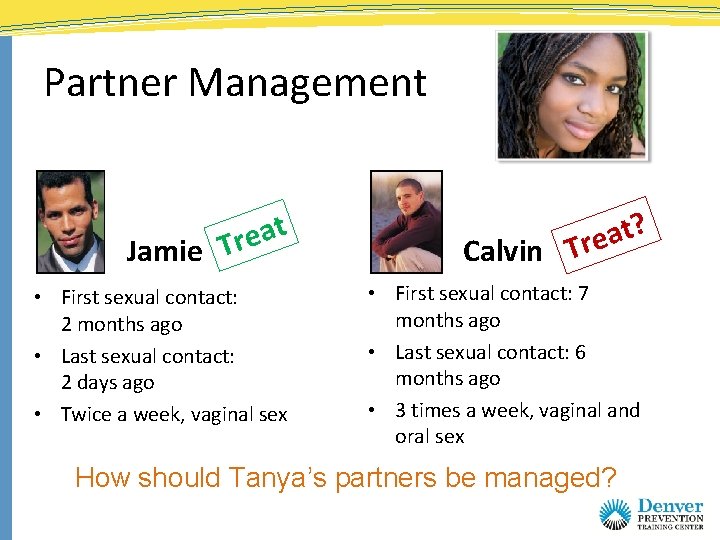
Partner Management t a e r Jamie T • First sexual contact: 2 months ago • Last sexual contact: 2 days ago • Twice a week, vaginal sex ? t a Calvin Tre • First sexual contact: 7 months ago • Last sexual contact: 6 months ago • 3 times a week, vaginal and oral sex How should Tanya’s partners be managed?
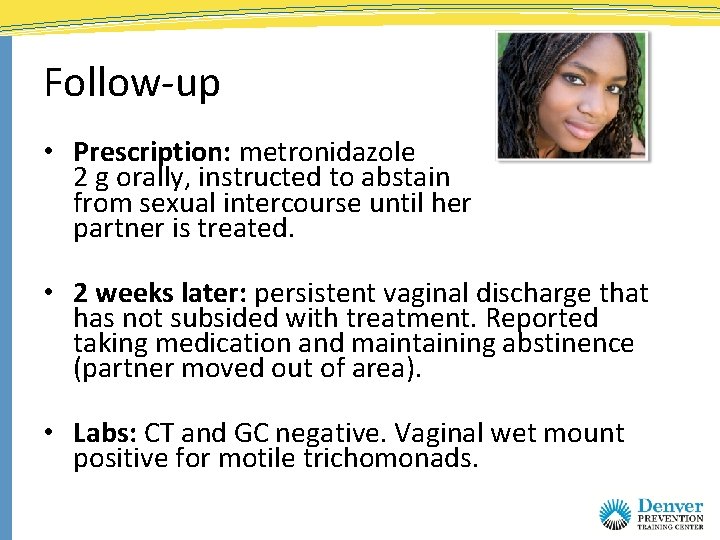
Follow-up • Prescription: metronidazole 2 g orally, instructed to abstain from sexual intercourse until her partner is treated. • 2 weeks later: persistent vaginal discharge that has not subsided with treatment. Reported taking medication and maintaining abstinence (partner moved out of area). • Labs: CT and GC negative. Vaginal wet mount positive for motile trichomonads.
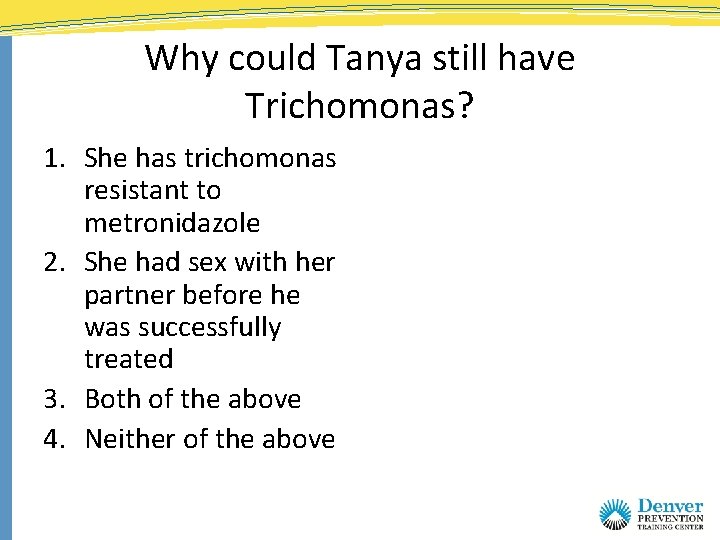
Why could Tanya still have Trichomonas? 1. She has trichomonas resistant to metronidazole 2. She had sex with her partner before he was successfully treated 3. Both of the above 4. Neither of the above
Why could Tanya still have Trichomonas? 1. She has trichomonas resistant to metronidazole 2. She had sex with her partner before he was successfully treated 3. Both of the above 4. Neither of the above
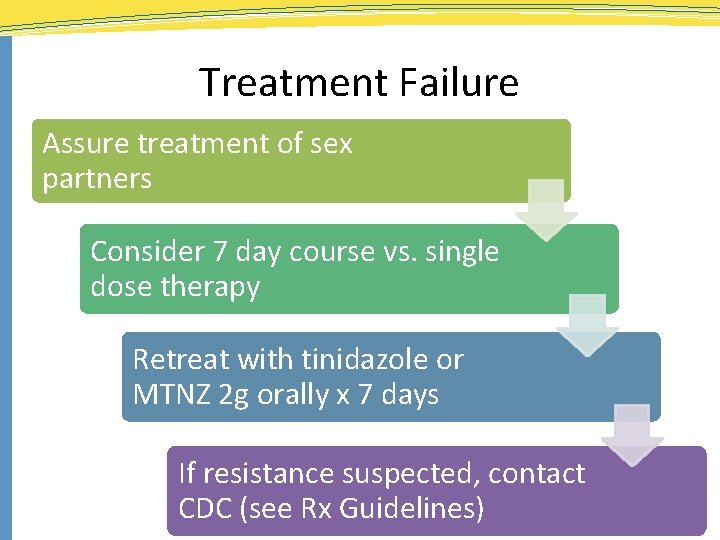
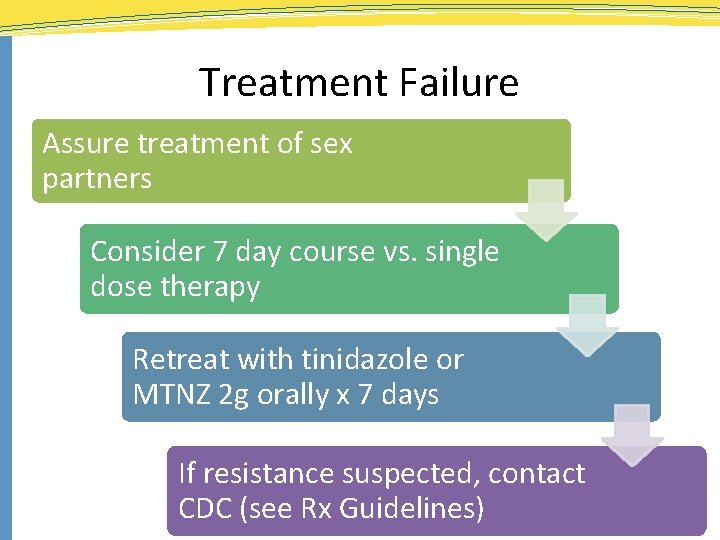
Treatment Failure Assure treatment of sex partners Consider 7 day course vs. single dose therapy Retreat with tinidazole or MTNZ 2 g orally x 7 days If resistance suspected, contact CDC (see Rx Guidelines)
Case study Alexa • 24 year old female • Partners: one partner in last year; no partner in last 3 months, male partners only • Protection from STDs: occasional condom use • Past history: + CT 4 years ago • Protection from pregnancy: oral contraceptives • Complaint: vaginal discharge for 1 week with vulvar irritation and itching; dyspareunia and dysuria
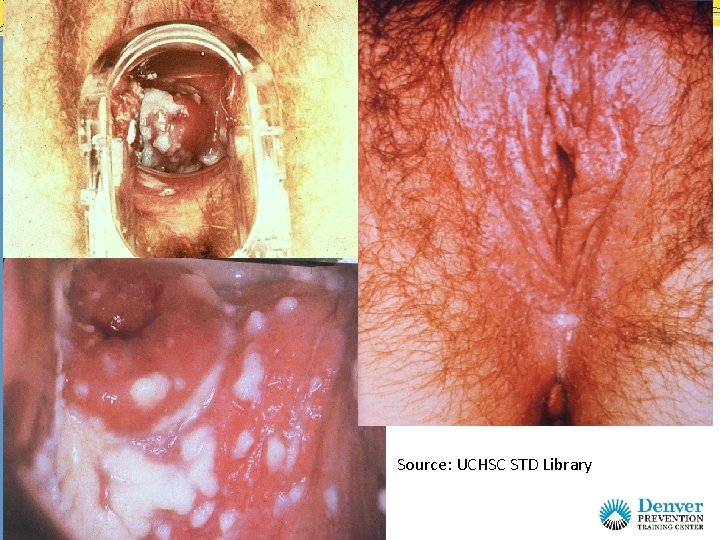
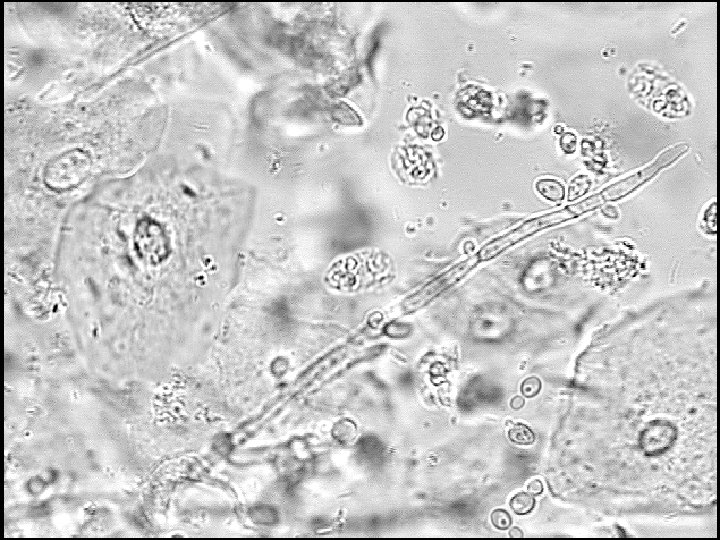
Source: UCHSC STD Library Source: CDC

Source: CDC
Source:
Case Summary • Diagnosis: vulvo-vaginal candidiasis (VVC) • Treatment: You recommend an OTC cream preparation, but patient requests the fluconazole pill
Does fluconazole have better efficacy than topical azoles when treating Candida vaginitis? 1. Yes 2. No
Does fluconazole have better efficacy than topical azoles when treating Candida vaginitis? 1. Yes 2. No
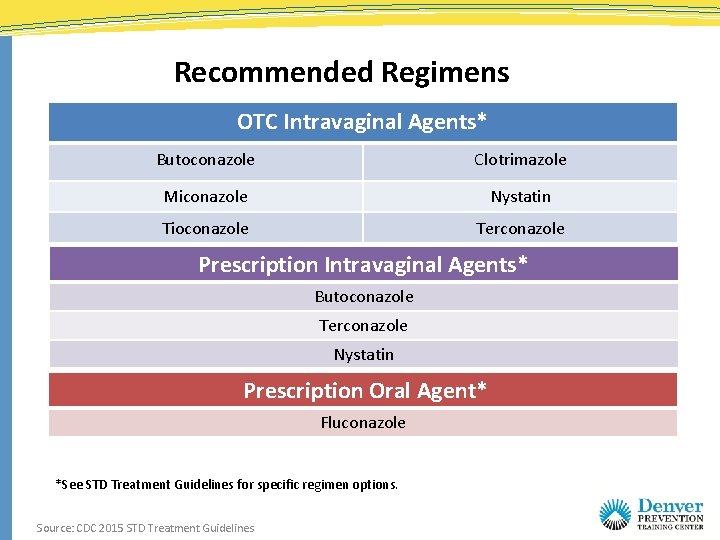
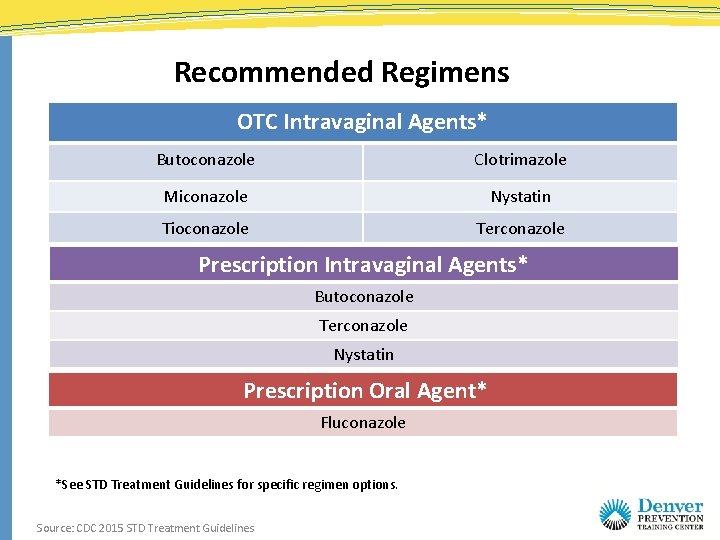
Recommended Regimens OTC Intravaginal Agents* Butoconazole Clotrimazole Miconazole Nystatin Tioconazole Terconazole Prescription Intravaginal Agents* Butoconazole Terconazole Nystatin Prescription Oral Agent* Fluconazole *See STD Treatment Guidelines for specific regimen options. Source: CDC 2015 STD Treatment Guidelines
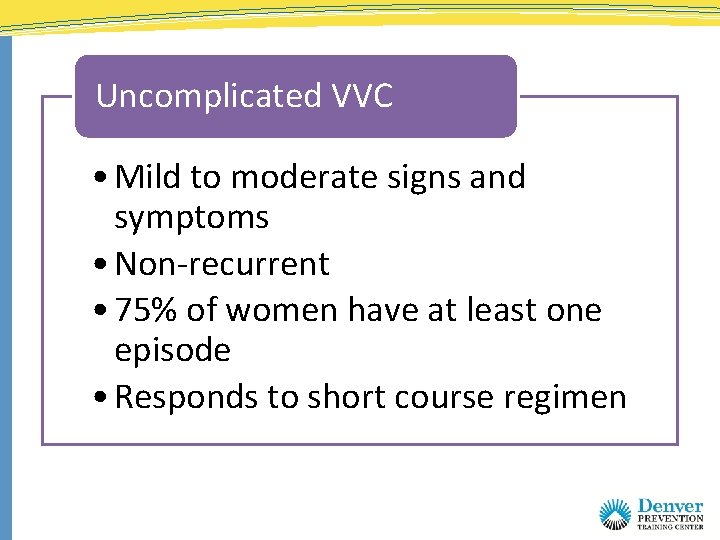
Uncomplicated VVC • Mild to moderate signs and symptoms • Non-recurrent • 75% of women have at least one episode • Responds to short course regimen
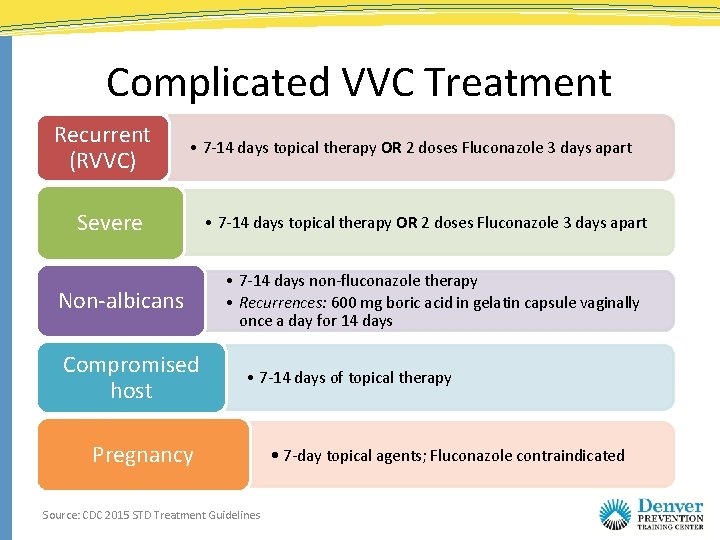
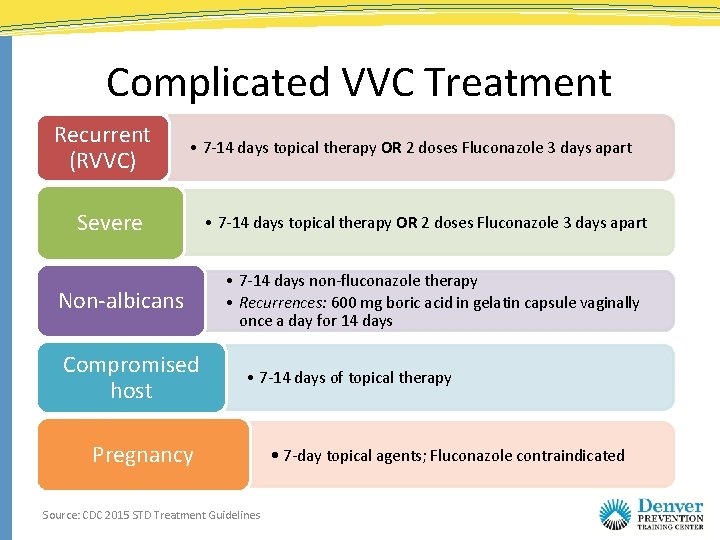
Complicated VVC Treatment Recurrent (RVVC) • 7 -14 days topical therapy OR 2 doses Fluconazole 3 days apart Severe Non-albicans Compromised host • 7 -14 days topical therapy OR 2 doses Fluconazole 3 days apart • 7 -14 days non-fluconazole therapy • Recurrences: 600 mg boric acid in gelatin capsule vaginally once a day for 14 days • 7 -14 days of topical therapy Pregnancy Source: CDC 2015 STD Treatment Guidelines • 7 -day topical agents; Fluconazole contraindicated
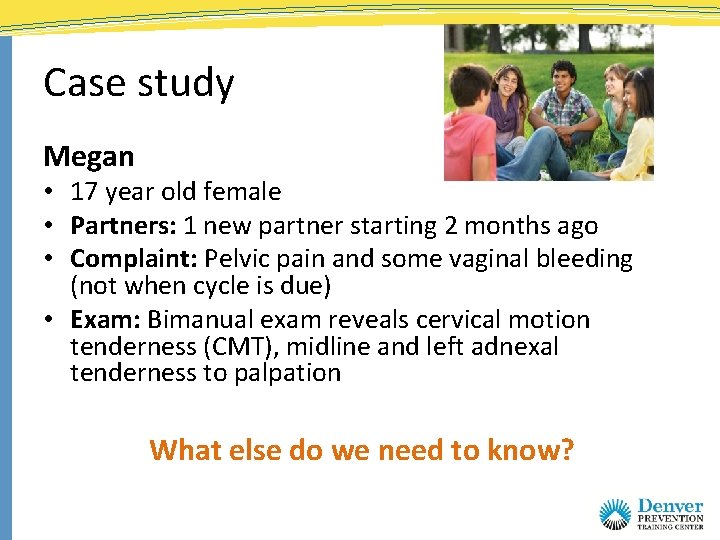
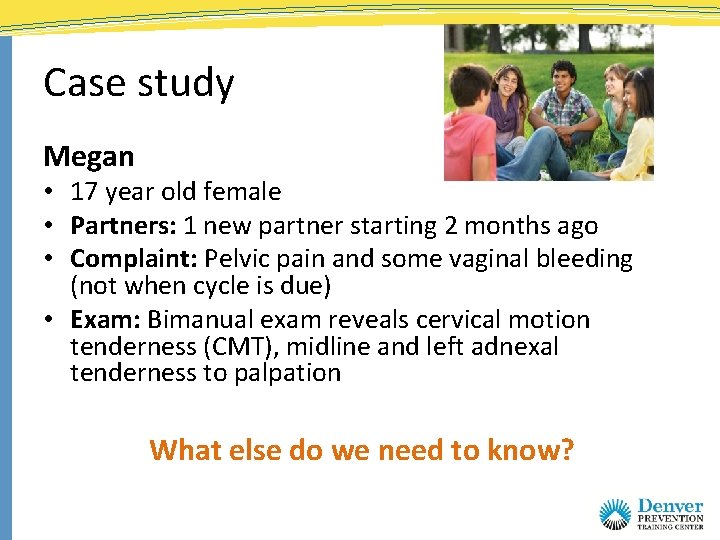
Case study Megan • 17 year old female • Partners: 1 new partner starting 2 months ago • Complaint: Pelvic pain and some vaginal bleeding (not when cycle is due) • Exam: Bimanual exam reveals cervical motion tenderness (CMT), midline and left adnexal tenderness to palpation What else do we need to know?
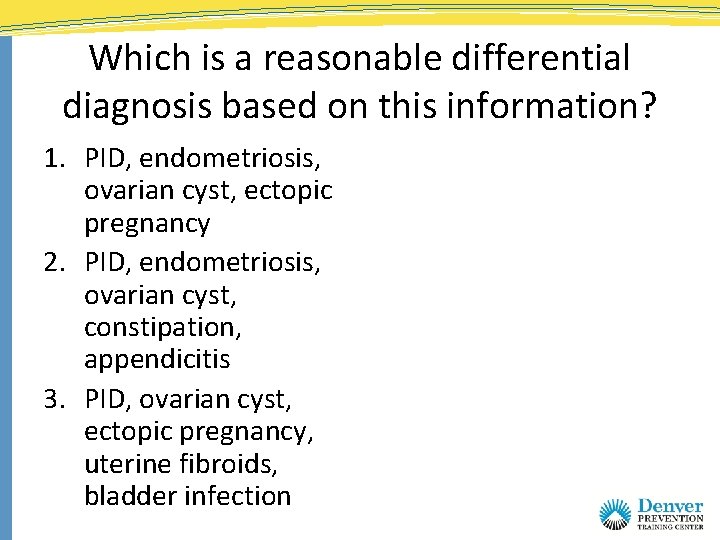
Which is a reasonable differential diagnosis based on this information? 1. PID, endometriosis, ovarian cyst, ectopic pregnancy 2. PID, endometriosis, ovarian cyst, constipation, appendicitis 3. PID, ovarian cyst, ectopic pregnancy, uterine fibroids, bladder infection
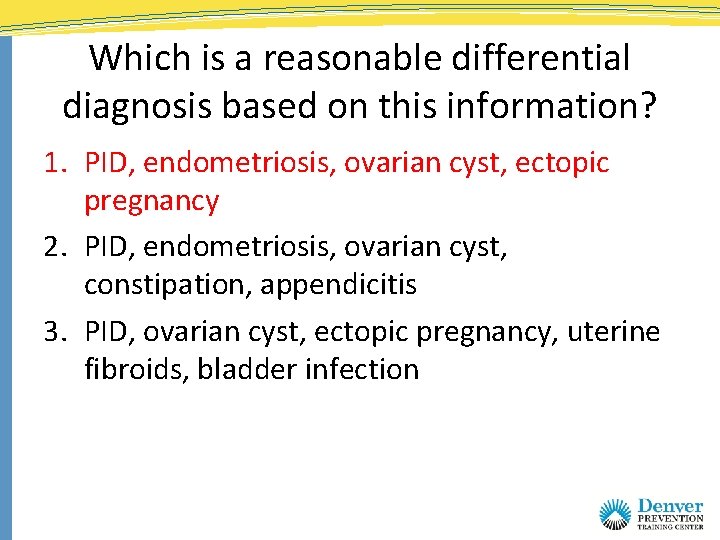
Which is a reasonable differential diagnosis based on this information? 1. PID, endometriosis, ovarian cyst, ectopic pregnancy 2. PID, endometriosis, ovarian cyst, constipation, appendicitis 3. PID, ovarian cyst, ectopic pregnancy, uterine fibroids, bladder infection
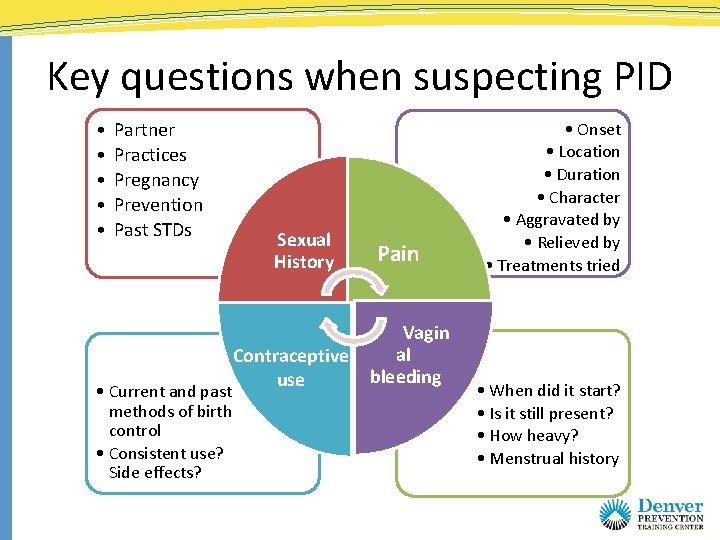
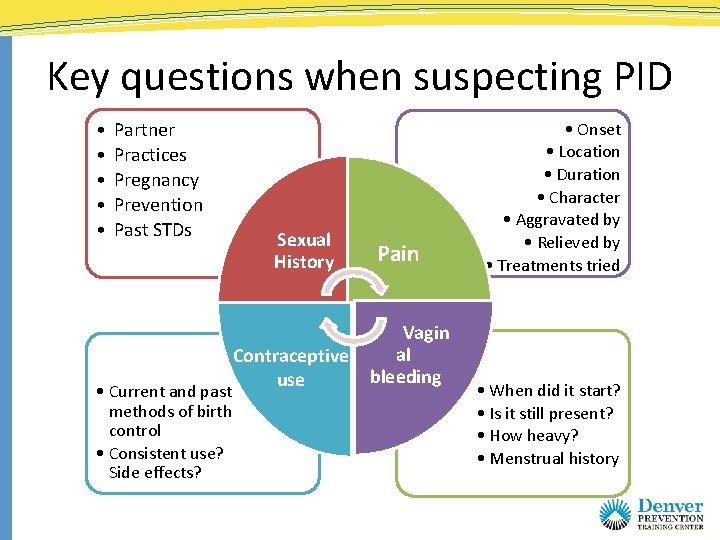
Key questions when suspecting PID • • • Partner Practices Pregnancy Prevention Past STDs • Current and past methods of birth control • Consistent use? Side effects? Sexual History Contraceptive use Pain Vagin al bleeding • Onset • Location • Duration • Character • Aggravated by • Relieved by • Treatments tried • When did it start? • Is it still present? • How heavy? • Menstrual history
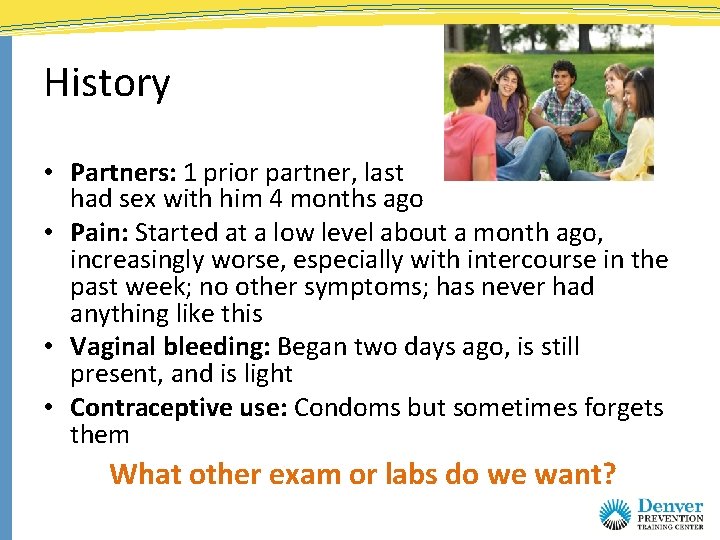
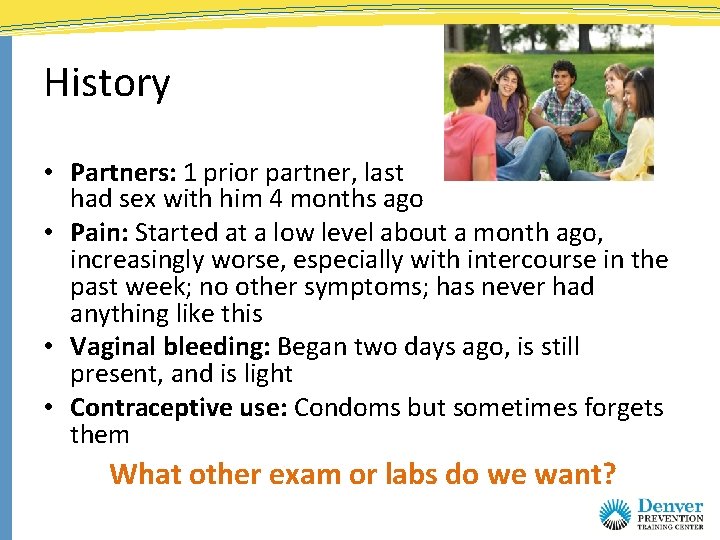
History • Partners: 1 prior partner, last had sex with him 4 months ago • Pain: Started at a low level about a month ago, increasingly worse, especially with intercourse in the past week; no other symptoms; has never had anything like this • Vaginal bleeding: Began two days ago, is still present, and is light • Contraceptive use: Condoms but sometimes forgets them What other exam or labs do we want?
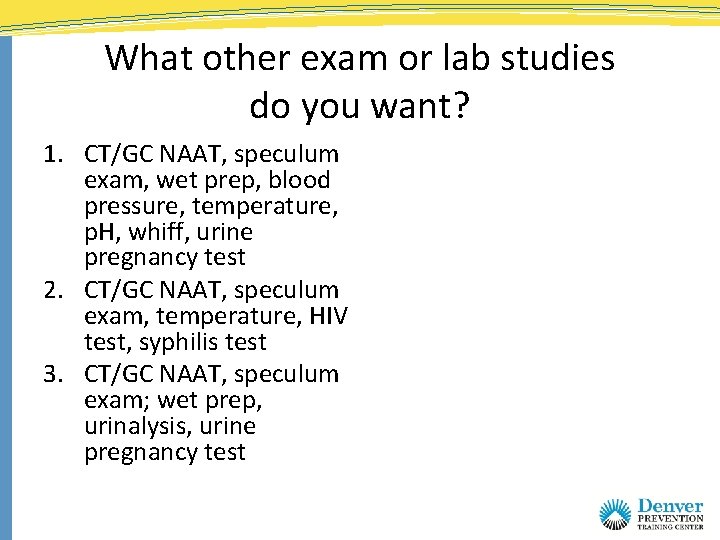
What other exam or lab studies do you want? 1. CT/GC NAAT, speculum exam, wet prep, blood pressure, temperature, p. H, whiff, urine pregnancy test 2. CT/GC NAAT, speculum exam, temperature, HIV test, syphilis test 3. CT/GC NAAT, speculum exam; wet prep, urinalysis, urine pregnancy test
What other exam or lab studies do you want? 1. CT/GC NAAT, speculum exam, wet prep, blood pressure, temperature, p. H, whiff, urine pregnancy test 2. CT/GC NAAT, speculum exam, temperature, HIV test, syphilis test 3. CT/GC NAAT, speculum exam; wet prep, urinalysis, urine pregnancy test
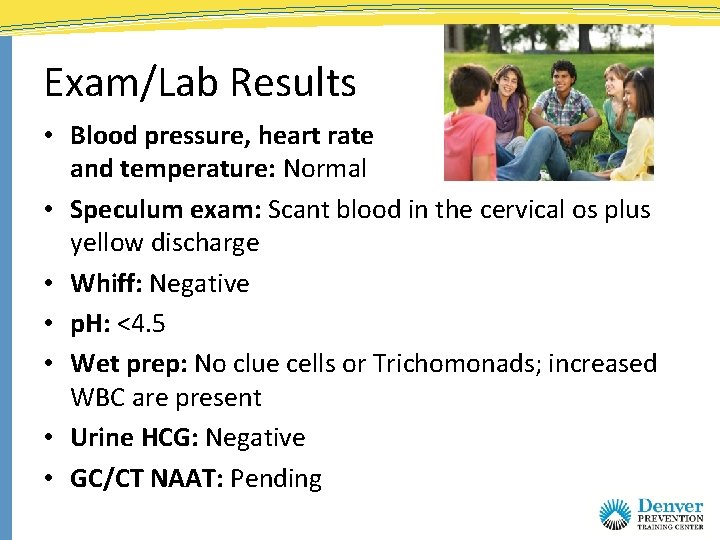
Exam/Lab Results • Blood pressure, heart rate and temperature: Normal • Speculum exam: Scant blood in the cervical os plus yellow discharge • Whiff: Negative • p. H: <4. 5 • Wet prep: No clue cells or Trichomonads; increased WBC are present • Urine HCG: Negative • GC/CT NAAT: Pending
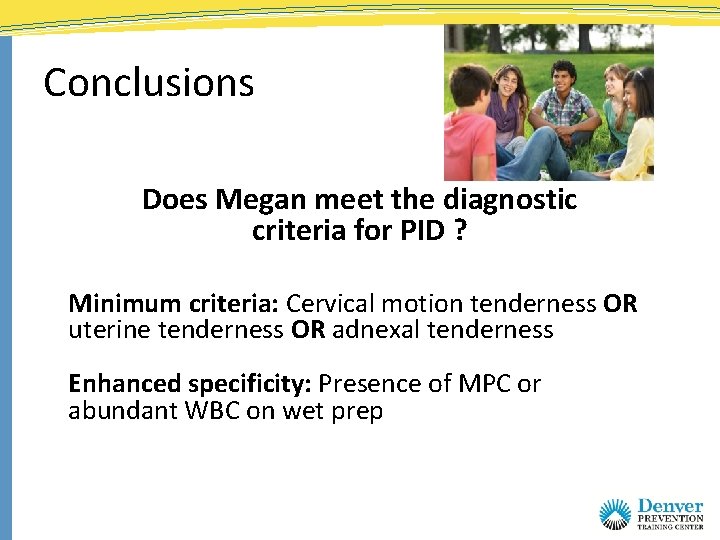
Conclusions Does Megan meet the diagnostic criteria for PID ? Minimum criteria: Cervical motion tenderness OR uterine tenderness OR adnexal tenderness Enhanced specificity: Presence of MPC or abundant WBC on wet prep
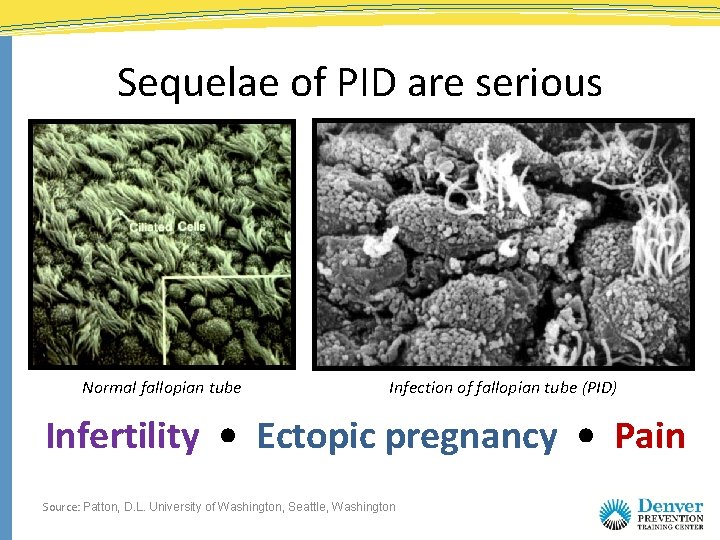
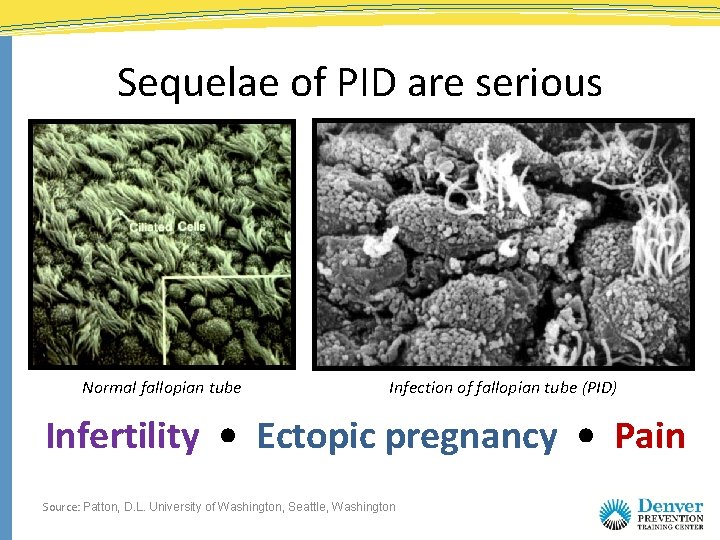
Sequelae of PID are serious Normal fallopian tube Infection of fallopian tube (PID) Infertility • Ectopic pregnancy • Pain Source: Patton, D. L. University of Washington, Seattle, Washington
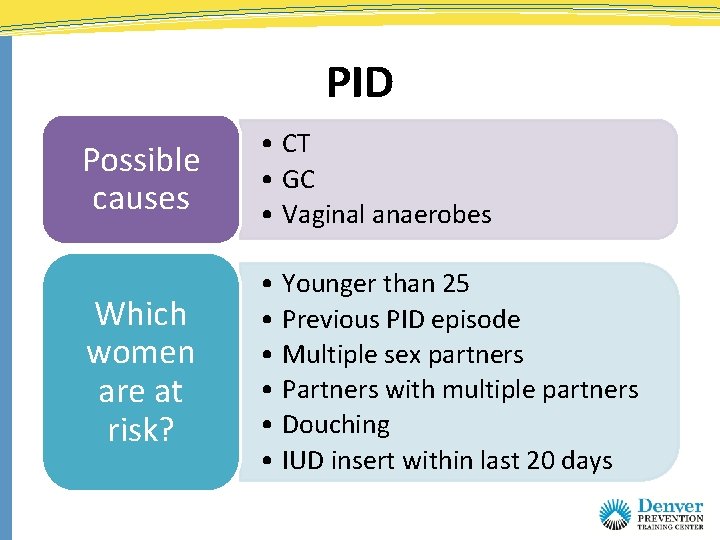
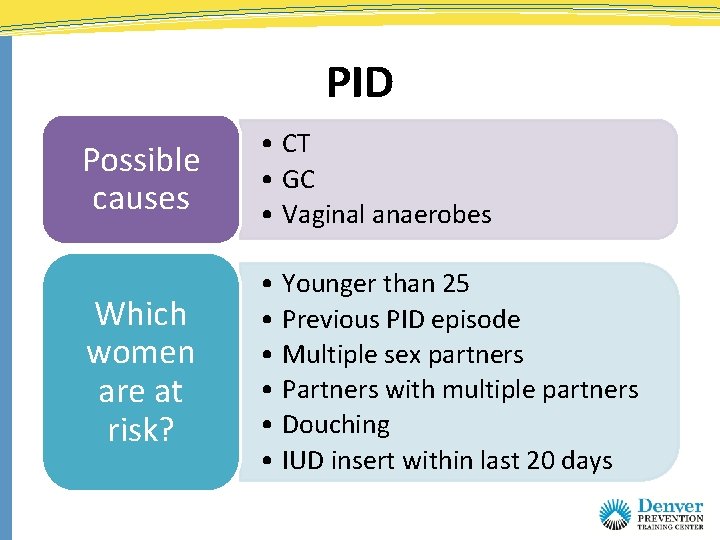
PID Possible causes • CT • GC • Vaginal anaerobes Which women are at risk? • Younger than 25 • Previous PID episode • Multiple sex partners • Partners with multiple partners • Douching • IUD insert within last 20 days
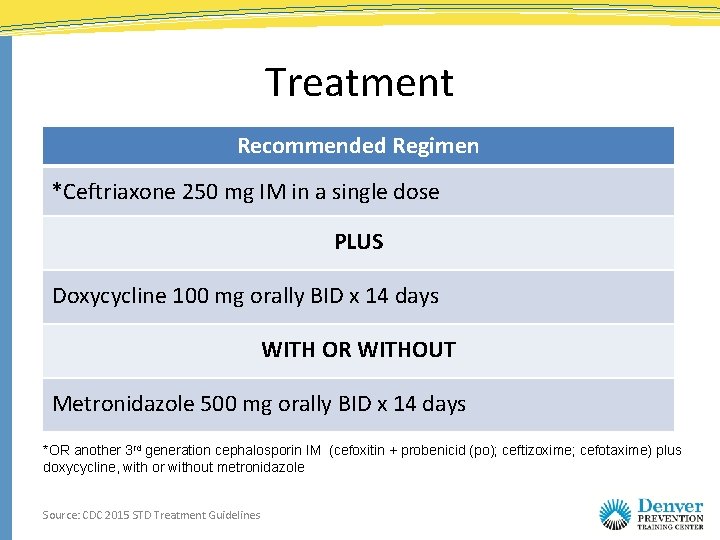
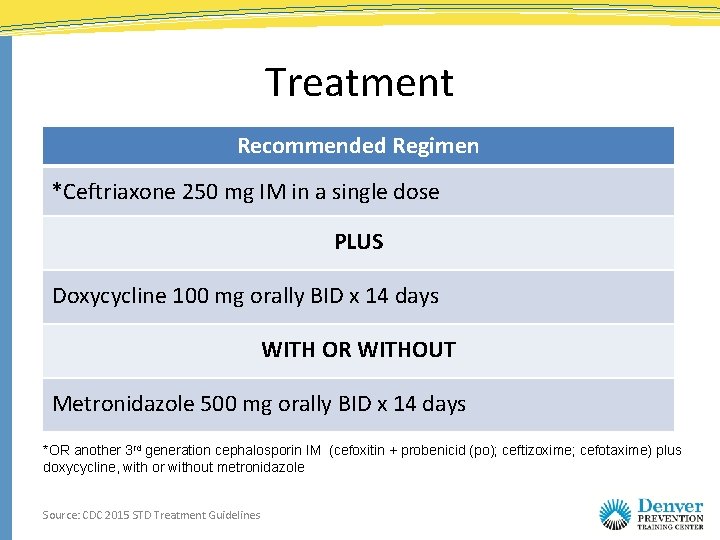
Treatment Recommended Regimen *Ceftriaxone 250 mg IM in a single dose PLUS Doxycycline 100 mg orally BID x 14 days WITH OR WITHOUT Metronidazole 500 mg orally BID x 14 days *OR another 3 rd generation cephalosporin IM (cefoxitin + probenicid (po); ceftizoxime; cefotaxime) plus doxycycline, with or without metronidazole Source: CDC 2015 STD Treatment Guidelines
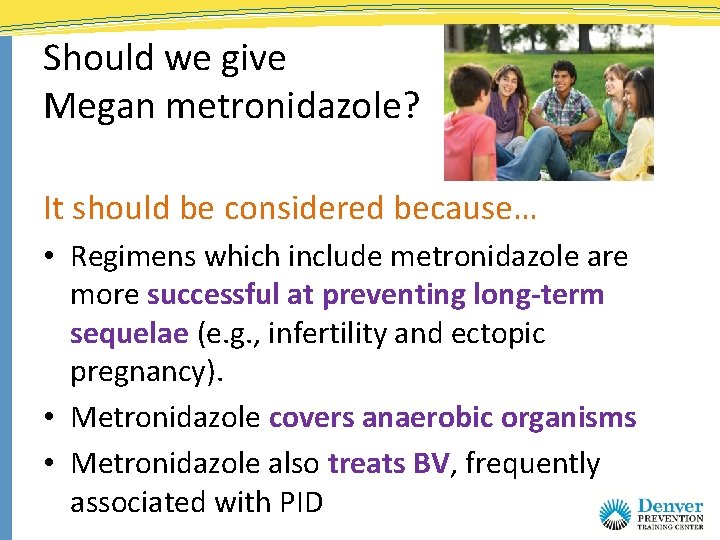
Should we give Megan metronidazole? It should be considered because… • Regimens which include metronidazole are more successful at preventing long-term sequelae (e. g. , infertility and ectopic pregnancy). • Metronidazole covers anaerobic organisms • Metronidazole also treats BV, frequently associated with PID
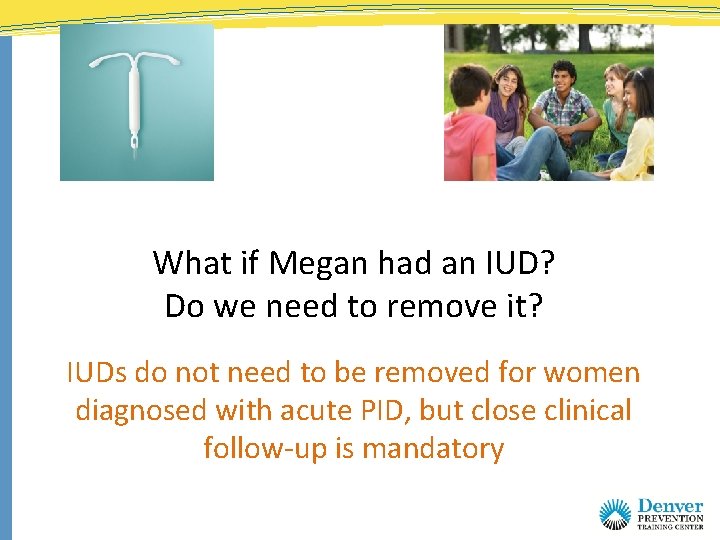
What if Megan had an IUD? Do we need to remove it? IUDs do not need to be removed for women diagnosed with acute PID, but close clinical follow-up is mandatory
Case Summary • Diagnose and treat for PID with ceftriaxone and doxycycline • Have Megan return for re-check in 48 – 72 hours – Repeat bimanual – Assess clinical improvement • Partner management • No IC until therapy completed Source: CDC 2015 STD Treatment Guidelines
Key Points • Vaginitis is common with multiple etiologies • The key to treatment of vaginitis is proper diagnosis • Trich (and ? BV) is associated with increased risk of HIV acquisition and transmission • PID is difficult to diagnose with certainty • Providers should have a low threshold for diagnosing PID in at-risk patient • Why do we care? Infertility, ectopic pregnancy and chronic pelvic pain