VAGINAL HYGIENE AND VAGINITIS Original outline by Ellen
VAGINAL HYGIENE AND VAGINITIS Original outline by Ellen Mitchell Original slides by Maryellen Donnelly Revised by Susan Flagler January 2007 Revised by Stephanie Sola March 2007, March 2009, April 2011 (Updated 4/7/11 to include CDC STD Treatment Guidelines, 2010)
Vaginal Discharge as a Problem: o If you take care of women, you will diagnose and treat vaginitis! o Frequent reason for office visits (Accounts for over 10 million office visits per year)1. o Women complain of unaccustomed or excessive amount of vaginal secretions, frequently accompanied by vulvar or perineal pruritus, irritation, or burning. 1. Kent HL. Epidemiology of vaginitis. Am J Obstet Gynecol 1991 Oct; 165(4 Pt 2): 1168 -76.

Vaginal Discharge as a Problem: o 90% of vaginitis is caused by one of three problems: n Bacterial vaginosis (40 -50%)2, 3 n Vulvovaginal candidiasis (25 -33%)4 n Trichomoniasis (4 -35%)5 o Postmenopausal women may have atrophic vaginitis complicating or causing symptoms o Cases may be difficult to diagnose/treat due to atypical presentations, mixed infections, drug resistance, or recurrence 2. Joesoef, M, Schmid, G. Bacterial vaginosis. In: Clinical evidence. BMJ Publishing Group, London 2001; 4: 887. 3. Morris M; Nicoll A; Simms I; Wilson J; Catchpole M. Bacterial vaginosis: a public health review. BJOG 2001 May; 108(5): 439 -50. 4. Fleury, FJ. Adult vaginitis. Clin Obstet Gynecol 1981; 24: 407. 5. Anderson MR; Klink K; Cohrssen A. Evaluation of vaginal complaints. JAMA 2004 Mar 17; 291(11): 1368 -79.
The Vaginal Environment: A Dynamic and Delicate Ecosystem Cervical mucus Upper genital tract secretions Sweat Sebaceous secretions Bartholin’s and Skene’s gland secretions Exfoliation of epithelial cells and vaginal mucosa o Normal flora (lactobacillus, diphtheroids, S. epidermidis, other anaerobes like Gardnerella vaginalis, candida species) o o o
Factors that Affect the Vaginal Ecosystem o The maintenance of an optimal p. H balance involves a complex interplay of hormonal, microbiologic, and other unknown factors: n n n Estrogen level Thickness of the vaginal epithelium Glycogen level of epithelial cells Number of lactobacilli Vaginal p. H
Vaginal Ecosystem: ESTROGEN o Thickens the superficial epithelial cells of the vagina that contain glycogen, the main nutrient for lactobacilli o Creates a cleansing action through an increase in vaginal secretions
Vaginal Ecosystem: EPITHELIUM o More estrogen = thicker vaginal epithelium o More thickness = more protection from trauma and significant irritations
Vaginal Ecosystem: GLYCOGEN o Found in vaginal epithelial cells o Higher glycogen results in more abundant lactobacilli (helpful factor) o Too high can encourage yeast to grow
Vaginal Ecosystem: LACTOBACILLI o Metabolism of glycogen by lactobacilli production of lactic acid maintains vaginal p. H of 3. 8 -4. 2 suppression of opportunistic organisms o Hydrogen peroxide is also produced which is toxic to anaerobes
Vaginal Ecosystem: p. H o Normal p. H in premenopausal women is 3. 8 -4. 2 o Certain pathogens thrive at higher p. H (decreased hydrogen ion concentration favors adherence of the pathogen to vaginal epithelial cells)

Additional Factors that Affect the Vaginal Ecosystem: o o Amount of vaginal secretions Number of pathogens present Immune status Individual sensitivity of the vaginal epithelium to chemicals or allergens

Causes of Imbalance in the Vaginal Ecosystem: o Antibiotics decrease lactobacilli o Oral contraceptives and pregnancy increase estrogen and glycogen o Menstruation increases the vaginal p. H o Altered immune status

Causes of Imbalance in the Vaginal Ecosystem (continued): o Irritants (chemical or mechanical) and allergens can cause tissue injury or inflammation o Diabetes increases glycogen o Moisture causes cell maceration o Douching removes lactobacilli and may damage tissue

Causes of Imbalance in the Vaginal Ecosystem (continued): o Menopause and perimenopause result in decreased estrogen levels o Genital or pelvic infections can cause tissue inflammation and/or overgrowth of organisms o Sexual intercourse may cause tissue inflammation, introduce organisms or allergens
Patient Education: Genital Hygiene o Wipe from front to back after BM o Use lubricating agent during sexual intercourse (Astroglide) o Wash sex toys in hot soapy water o Avoid hot tubs containing organisms or high levels of chlorine o DON’T DOUCHE unless it is recommended by your provider
Patient Education: Genital Hygiene (continued) o Avoid feminine hygiene products with deodorants o Avoid toilet paper with dyes o Avoid underwear made from synthetic fabric o Avoid tight pants o Avoid perfumed dryer sheets and detergents o Avoid Nonoxynal 9 if sensitive (use smallest effective amount)

Vaginal Discharge: DIFFERENTIAL DIAGNOSIS o o o o o Benign physiologic discharge / “normal” Contact dermatitis or semen allergies Foreign body Cervicitis (HPV, GC, CT, trich) Carcinoma of the cervix Condyloma acuminata Endometritis PID Anatomical sources n n o o Vaginal or cervical lesions (ectropion, polyps, granulation tissue, neoplasm) Fistula between bladder/vagina or rectum/vagina Vaginitis (candidiasis, trich, BV, atrophic vaginitis) Other vaginitis (desquamative inflammatory vaginitis, cytolytic vaginosis, Group A or B Streptococcal infections)

HISTORY o o o Anatomic site Duration Aggravating and alleviating factors Recent hygiene changes Sexual activity Systemic disease complicating condition

PHYSICAL EXAM AND LAB o o o Pelvic exam Vaginal p. H Wet prep (or wet mount) Possible cultures Possible NAATs (nucleic acid amplification tests)

WET PREP o Sample of vaginal discharge from high on side of vagina (avoiding cervical discharge) o Put sample in small amount of normal saline n Test tube with 1 cc n Directly into gtts of saline on slide

WET PREP: Saline Slide o Place cover slip over 1 -2 gtts of saline containing vaginal sample o Example under 10 x to survey specimen o Look for mobile organisms o Find area to examine at 40 x n n n Squamous epithelial cells Lactobacilli Yeast buds and pseudohyphae Clue cells Mobile trichomonads WBCs and polymorphonuclear cells (PMNs)
WET PREP: KOH Whiff Test & Slide o Add 1 -2 gtts of KOH to sample of vaginal discharge o Sniff for amine odor – “whiff test” n Vaporization of the byproducts of anaerobic metabolism, cadaverine and putrescine o Place cover slip and examine saline prep first o Examine for yeast hyphae or buds (not lysed by KOH)

Resource for Wet Preps o Training video for wet preps available online. o URL is: http: //depts. washington. edu/nnptc/online_ training/wet_preps_video. html

Clinical Features of Vaginitis Syndrome Diagnostic Criteria Normal Bacterial Vaginosis Trichomoniasis Candida Vulvovaginitis 3. 8 – 4. 2 > 4. 5 < 4. 5 (usually) Vaginal Discharge Clear or white, flocculent/fluffy Thin, homogenous, milky white or gray, adherent, often increased Yellow-green, frothy, adherent, increased White, cottage cheeselike, sometimes increased Amine Odor (KOH “whiff” test) Absent Present (“fishy”) May be present (“fishy”) Absent None Discharge, bad odor (possibly worse after intercourse), itching may be present Frothy, discharge, bad odor, vulvar pruritus, dysuria Discharge, itching, burning Vaginal p. H Main Patient Complaints

NORMAL VAGINAL DISCHARGE
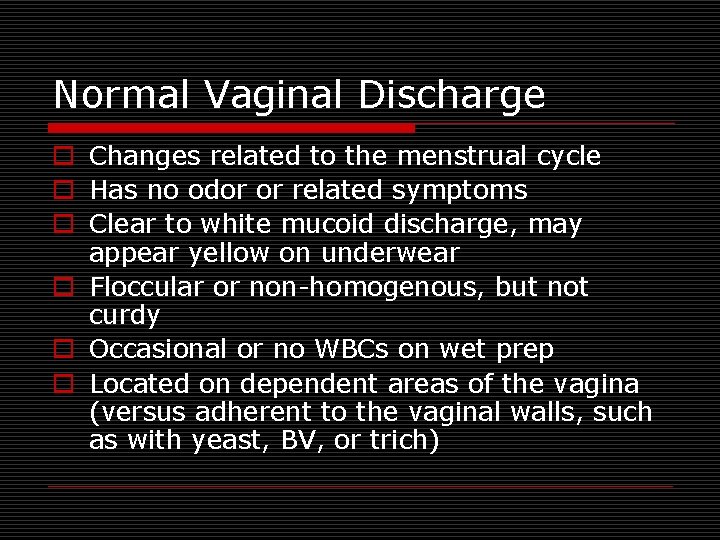
Normal Vaginal Discharge o Changes related to the menstrual cycle o Has no odor or related symptoms o Clear to white mucoid discharge, may appear yellow on underwear o Floccular or non-homogenous, but not curdy o Occasional or no WBCs on wet prep o Located on dependent areas of the vagina (versus adherent to the vaginal walls, such as with yeast, BV, or trich)

Epithelial Cell – Gram Stain Slide on the right from http: //www. bu. edu/cme/std/images/slide 5 -vwp_g 420. jpg
YEAST VAGINITIS
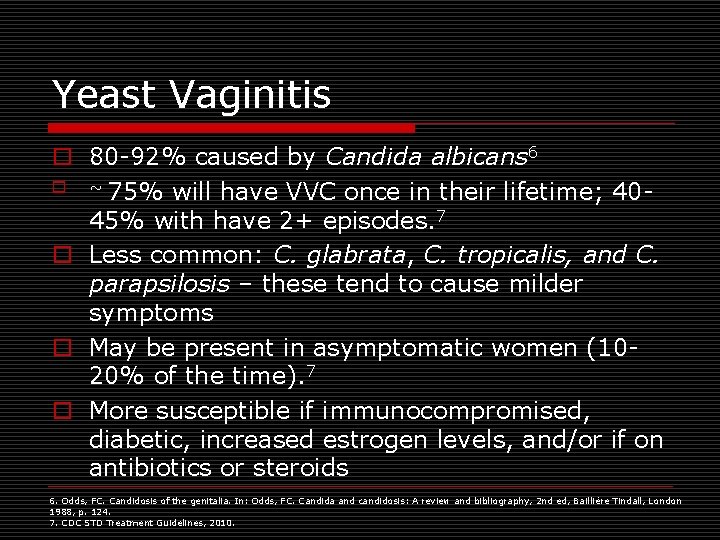
Yeast Vaginitis o 80 -92% caused by Candida albicans 6 o ~ 75% will have VVC once in their lifetime; 4045% with have 2+ episodes. 7 o Less common: C. glabrata, C. tropicalis, and C. parapsilosis – these tend to cause milder symptoms o May be present in asymptomatic women (1020% of the time). 7 o More susceptible if immunocompromised, diabetic, increased estrogen levels, and/or if on antibiotics or steroids 6. Odds, FC. Candidosis of the genitalia. In: Odds, FC. Candida and candidosis: A review and bibliography, 2 nd ed, Bailliére Tindall, London 1988, p. 124. 7. CDC STD Treatment Guidelines, 2010.
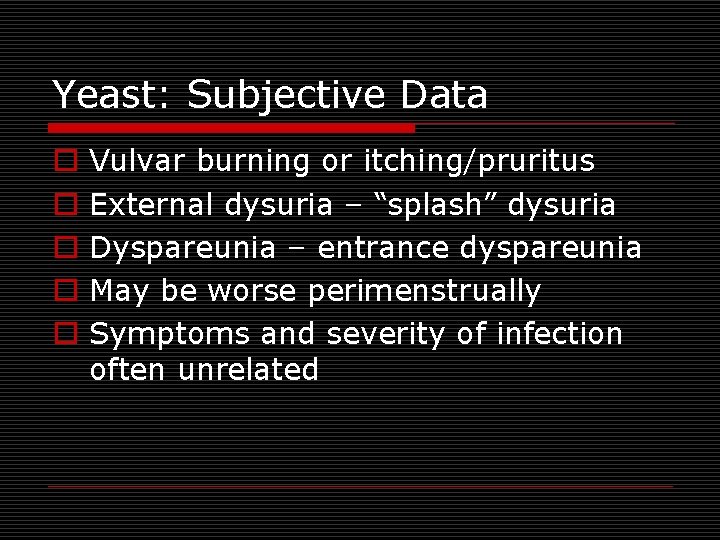
Yeast: Subjective Data o o o Vulvar burning or itching/pruritus External dysuria – “splash” dysuria Dyspareunia – entrance dyspareunia May be worse perimenstrually Symptoms and severity of infection often unrelated

Yeast: Objective Data Thick, white, curdy discharge No odor Discharge adherent to vaginal walls Vaginal mucosa red Satellite lesions possible on inner thigh Hyphae or budding yeast cells seen on KOH slide o p. H < 4. 5 o Tests: wet mount, Gram stain, culture o o o
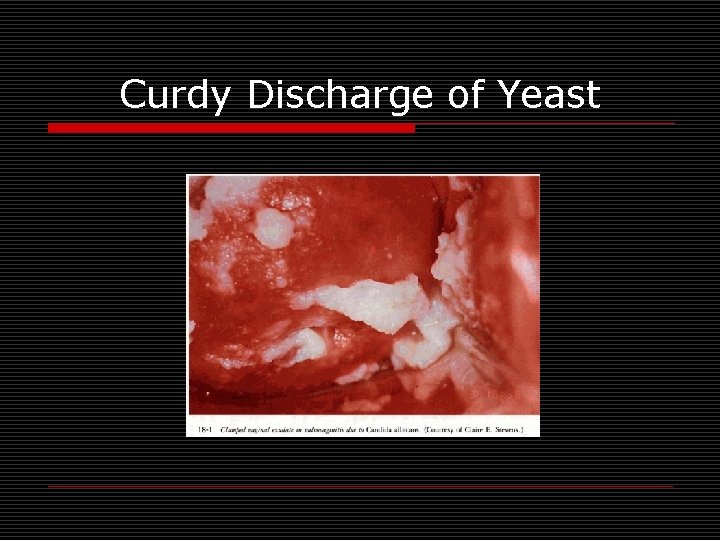
Curdy Discharge of Yeast

Yeast – KOH Prep Slide on the right from http: //www. bu. edu/cme/std/images/slide 1 -vwp_g 420. jpg
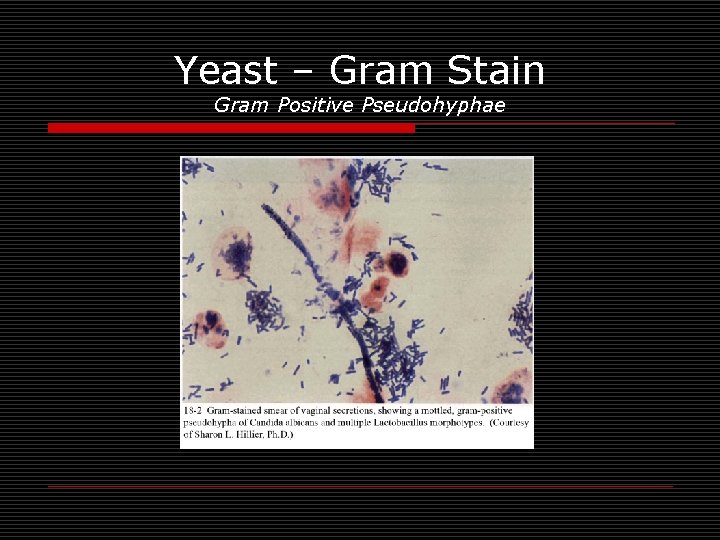
Yeast – Gram Stain Gram Positive Pseudohyphae
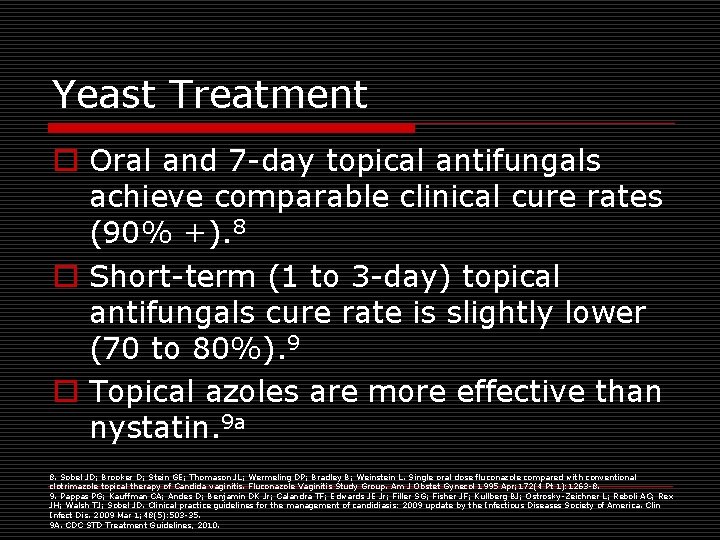
Yeast Treatment o Oral and 7 -day topical antifungals achieve comparable clinical cure rates (90% +). 8 o Short-term (1 to 3 -day) topical antifungals cure rate is slightly lower (70 to 80%). 9 o Topical azoles are more effective than nystatin. 9 a 8. Sobel JD; Brooker D; Stein GE; Thomason JL; Wermeling DP; Bradley B; Weinstein L. Single oral dose fluconazole compared with conventional clotrimazole topical therapy of Candida vaginitis. Fluconazole Vaginitis Study Group. Am J Obstet Gynecol 1995 Apr; 172(4 Pt 1): 1263 -8. 9. Pappas PG; Kauffman CA; Andes D; Benjamin DK Jr; Calandra TF; Edwards JE Jr; Filler SG; Fisher JF; Kullberg BJ; Ostrosky-Zeichner L; Reboli AC; Rex JH; Walsh TJ; Sobel JD. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis. 2009 Mar 1; 48(5): 503 -35. 9 A. CDC STD Treatment Guidelines, 2010.
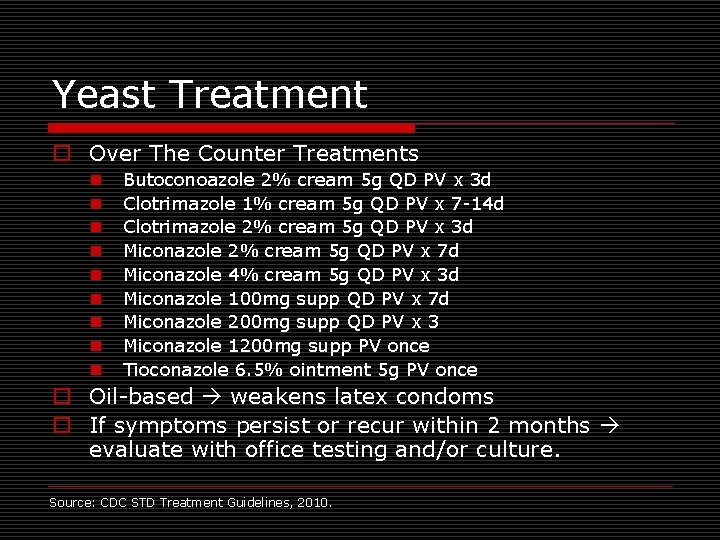
Yeast Treatment o Over The Counter Treatments n n n n n Butoconoazole 2% cream 5 g QD PV x 3 d Clotrimazole 1% cream 5 g QD PV x 7 -14 d Clotrimazole 2% cream 5 g QD PV x 3 d Miconazole 2% cream 5 g QD PV x 7 d Miconazole 4% cream 5 g QD PV x 3 d Miconazole 100 mg supp QD PV x 7 d Miconazole 200 mg supp QD PV x 3 Miconazole 1200 mg supp PV once Tioconazole 6. 5% ointment 5 g PV once o Oil-based weakens latex condoms o If symptoms persist or recur within 2 months evaluate with office testing and/or culture. Source: CDC STD Treatment Guidelines, 2010.

Yeast Treatment o By Prescription Only n Butoconazole 2% cream (single-dose bioadhesive product) 5 g PV once n Nystatin 100000 unit vaginal tablet QD x 14 d n Terconazole 0. 4% cream 5 g QD PV x 7 d n Terconazole 0. 8% cream 5 g QD PV x 3 d n Terconazole 80 mg supp QD PV x 3 d n Fluconazole 150 mg tab po once Source: CDC STD Treatment Guidelines, 2010.

Yeast: Treatment During Pregnancy o Only topical azoles x 7 days Source: CDC STD Treatment Guidelines, 2010.
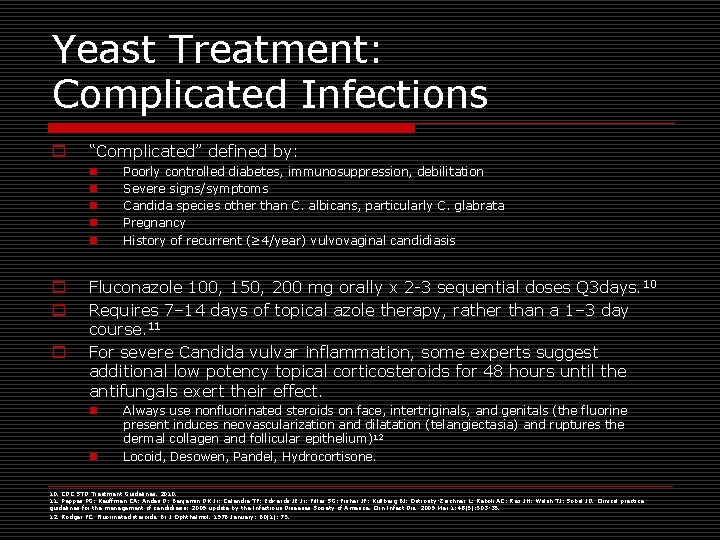
Yeast Treatment: Complicated Infections o “Complicated” defined by: n n n o o o Poorly controlled diabetes, immunosuppression, debilitation Severe signs/symptoms Candida species other than C. albicans, particularly C. glabrata Pregnancy History of recurrent (≥ 4/year) vulvovaginal candidiasis Fluconazole 100, 150, 200 mg orally x 2 -3 sequential doses Q 3 days. 10 Requires 7– 14 days of topical azole therapy, rather than a 1– 3 day course. 11 For severe Candida vulvar inflammation, some experts suggest additional low potency topical corticosteroids for 48 hours until the antifungals exert their effect. n n Always use nonfluorinated steroids on face, intertriginals, and genitals (the fluorine present induces neovascularization and dilatation (telangiectasia) and ruptures the dermal collagen and follicular epithelium)12 Locoid, Desowen, Pandel, Hydrocortisone. 10. CDC STD Treatment Guidelines, 2010. 11. Pappas PG; Kauffman CA; Andes D; Benjamin DK Jr; Calandra TF; Edwards JE Jr; Filler SG; Fisher JF; Kullberg BJ; Ostrosky-Zeichner L; Reboli AC; Rex JH; Walsh TJ; Sobel JD. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis. 2009 Mar 1; 48(5): 503 -35. 12. Rodger FC. Fluorinated steroids. Br J Ophthalmol. 1976 January; 60(1): 75.
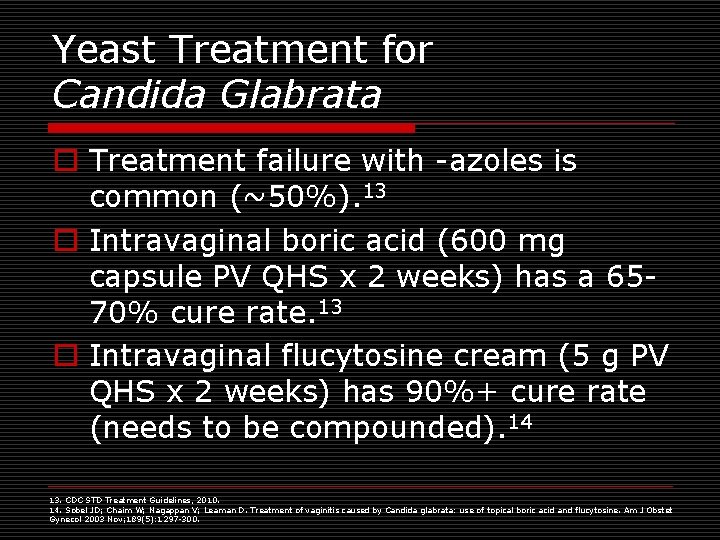
Yeast Treatment for Candida Glabrata o Treatment failure with -azoles is common (~50%). 13 o Intravaginal boric acid (600 mg capsule PV QHS x 2 weeks) has a 6570% cure rate. 13 o Intravaginal flucytosine cream (5 g PV QHS x 2 weeks) has 90%+ cure rate (needs to be compounded). 14 13. CDC STD Treatment Guidelines, 2010. 14. Sobel JD; Chaim W; Nagappan V; Leaman D. Treatment of vaginitis caused by Candida glabrata: use of topical boric acid and flucytosine. Am J Obstet Gynecol 2003 Nov; 189(5): 1297 -300.
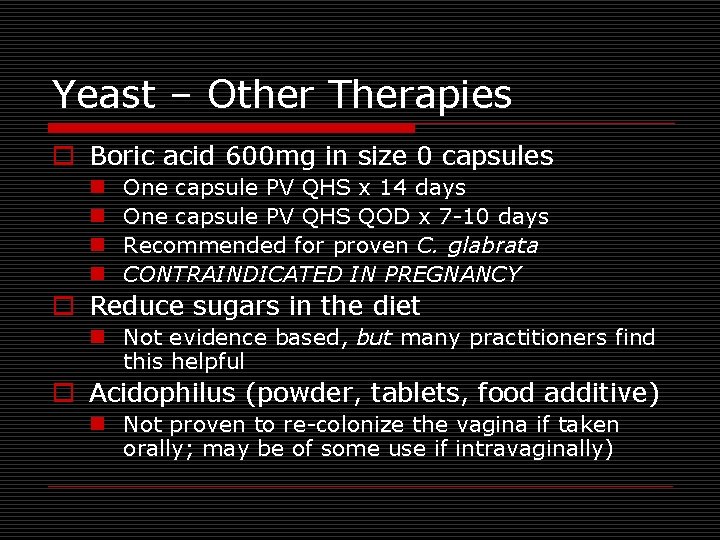
Yeast – Other Therapies o Boric acid 600 mg in size 0 capsules n n One capsule PV QHS x 14 days One capsule PV QHS QOD x 7 -10 days Recommended for proven C. glabrata CONTRAINDICATED IN PREGNANCY o Reduce sugars in the diet n Not evidence based, but many practitioners find this helpful o Acidophilus (powder, tablets, food additive) n Not proven to re-colonize the vagina if taken orally; may be of some use if intravaginally)

Recurrent Yeast Infections o Look for predisposing causes (HIV, Diabetes, Medication Use) o Consider culture (confirm C. albicans and rule out other pathogen) o Switch to another antifungal cream, use a longer second course, try fluconazole o Use one time topical during susceptible time (postcoitally, perimenstrually, etc. ) o Reduce risk factors for infection
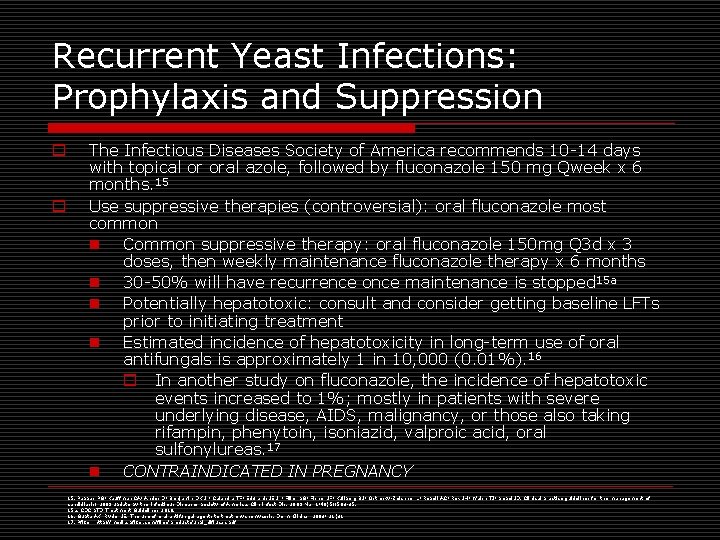
Recurrent Yeast Infections: Prophylaxis and Suppression o o The Infectious Diseases Society of America recommends 10 -14 days with topical or oral azole, followed by fluconazole 150 mg Qweek x 6 months. 15 Use suppressive therapies (controversial): oral fluconazole most common n Common suppressive therapy: oral fluconazole 150 mg Q 3 d x 3 doses, then weekly maintenance fluconazole therapy x 6 months n 30 -50% will have recurrence once maintenance is stopped 15 a n Potentially hepatotoxic: consult and consider getting baseline LFTs prior to initiating treatment n Estimated incidence of hepatotoxicity in long-term use of oral antifungals is approximately 1 in 10, 000 (0. 01%). 16 o In another study on fluconazole, the incidence of hepatotoxic events increased to 1%; mostly in patients with severe underlying disease, AIDS, malignancy, or those also taking rifampin, phenytoin, isoniazid, valproic acid, oral sulfonylureas. 17 n CONTRAINDICATED IN PREGNANCY 15. Pappas PG; Kauffman CA; Andes D; Benjamin DK Jr; Calandra TF; Edwards JE Jr; Filler SG; Fisher JF; Kullberg BJ; Ostrosky-Zeichner L; Reboli AC; Rex JH; Walsh TJ; Sobel JD. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis. 2009 Mar 1; 48(5): 503 -35. 15 a. CDC STD Treatment Guidelines 2010. 16. Gupta AK, Ryder JE. The use of oral antifungal agents to treat onychomycosis. Derm Clinics, 2003; 21(3). 17. Pfizer, http: //media. pfizer. com/files/products/uspi_diflucan. pdf

BACTERIAL VAGINOSIS

Bacterial Vagnosis (BV) o Not an “-itis” or inflammation o An “-osis” or general condition or process o Previously known as Gardnerella vaginalis n Most common pathogen n Other anaerobes also involved o Associated with reduced lactobacilli n p. H rises increased Gardnerella decreased oxygen further increase in anaerobes decrease in lactobacilli decrease in H 2 O 2 maintenance of basic p. H o Linked with sexual activity, but not “STI” o 50 -75% of women with BV are asymptomatic 17 17. Klebanoff MA; Schwebke JR; Zhang J; Nansel TR; Yu KF; Andrews WW. Vulvovaginal symptoms in women with bacterial vaginosis. Obstet Gynecol 2004 Aug; 104(2): 267 -72.

BV Risk Factors o Multiple or new sexual partners o Oral genital sex may be greater risk than penile intromission into the vagina o Douching o Cigarette smoking

BV: Subjective Data o Fishy, sour, or musty genital odor n Caused by metabolic byproducts of anaerobes, cadaverine and putrescine n May be worse after sex and/or menses o Increased vaginal discharge n Gray, thin, homogenous o Some may have complaints of vulvar irritation but erythema, pruritus, and inflammation are typically absent

BV: Objective Data o Minimal WBCs and lactobacilli o No inflammation of vagina or cervix o Requires 3 of these 4 criteria: n n Thin off-white or gray vaginal discharge adherent to vaginal walls p. H 5. 5 – 6. 5 Clue cells on wet prep o 75% of cell border covered in 20% of cells in high power field Amine odor with drop of 10% KOH (positive whiff test) o Tests: wet mount, Gram stain (cultures are not specific, pap tests have low sensitivity)17 a 17 a. CDC STD Treatment Guidelines, 2010.

BV Homogenous Discharge
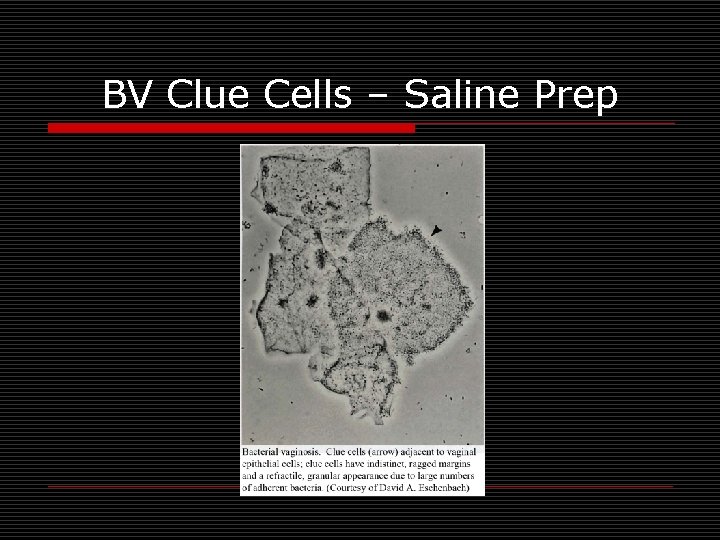
BV Clue Cells – Saline Prep

BV Clue Cells – Gram Stain Gram Variable – depending on age of cultures Gardnerella is typically gram negative small bacilli

BV: Treatment o Reduce risk factors for infection o Can spontaneously resolve in up to 1/3 of nonpregnant and pregnant women 18, 19 o Who to treat: n Symptomatic patients n Prevent postoperative infection in those with asymptomatic infection prior to abortion or hysterectomy n Asymptomatic women with previous preterm births n Can reduce risk of acquiring other STIs, including HIV 18. Klebanoff MA; Hauth JC; Mac. Pherson CA; Carey JC; Heine RP; Wapner RJ; Iams JD; Moawad A; Miodovnik M; Sibai BM; van. Dorsten JP; Dombrowski MP. Time course of the regression of asymptomatic bacterial vaginosis in pregnancy with and without treatment. Am J Obstet Gynecol 2004 Feb; 190(2): 363 -70. 19. Schwebke JR. Asymptomatic bacterial vaginosis: response to therapy. Am J Obstet Gynecol 2000 Dec; 183(6): 1434 -9.
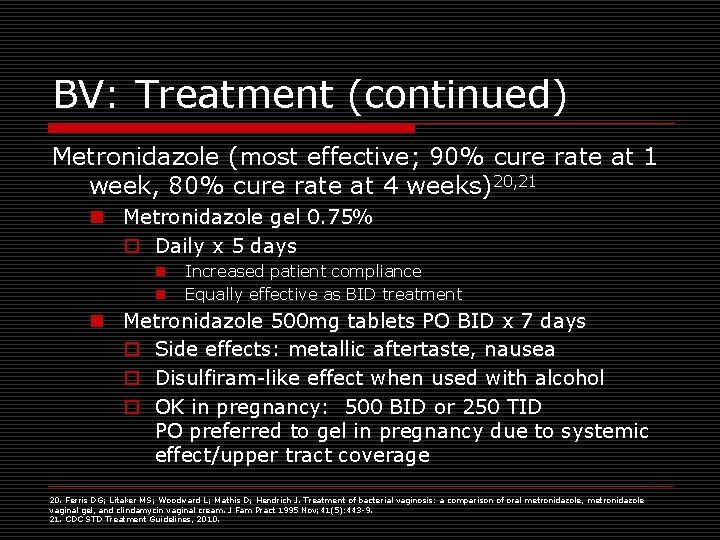
BV: Treatment (continued) Metronidazole (most effective; 90% cure rate at 1 week, 80% cure rate at 4 weeks)20, 21 n Metronidazole gel 0. 75% o Daily x 5 days n n Increased patient compliance Equally effective as BID treatment n Metronidazole 500 mg tablets PO BID x 7 days o Side effects: metallic aftertaste, nausea o Disulfiram-like effect when used with alcohol o OK in pregnancy: 500 BID or 250 TID PO preferred to gel in pregnancy due to systemic effect/upper tract coverage 20. Ferris DG; Litaker MS; Woodward L; Mathis D; Hendrich J. Treatment of bacterial vaginosis: a comparison of oral metronidazole, metronidazole vaginal gel, and clindamycin vaginal cream. J Fam Pract 1995 Nov; 41(5): 443 -9. 21. CDC STD Treatment Guidelines, 2010.
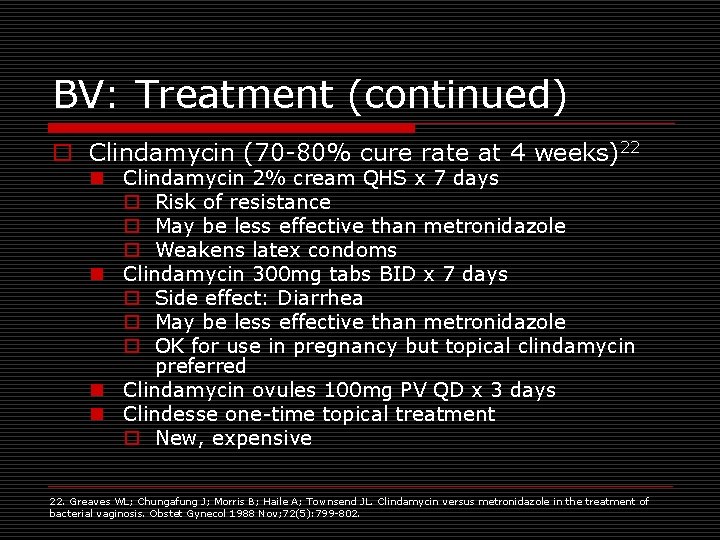
BV: Treatment (continued) o Clindamycin (70 -80% cure rate at 4 weeks)22 n Clindamycin 2% cream QHS x 7 days o Risk of resistance o May be less effective than metronidazole o Weakens latex condoms n Clindamycin 300 mg tabs BID x 7 days o Side effect: Diarrhea o May be less effective than metronidazole o OK for use in pregnancy but topical clindamycin preferred n Clindamycin ovules 100 mg PV QD x 3 days n Clindesse one-time topical treatment o New, expensive 22. Greaves WL; Chungafung J; Morris B; Haile A; Townsend JL. Clindamycin versus metronidazole in the treatment of bacterial vaginosis. Obstet Gynecol 1988 Nov; 72(5): 799 -802.

BV: Treatment (continued) o Consider patient preference when choosing treatment regimen. o Refrain from intercourse during treatment or use condoms consistently/correctly. o Douching increases the risk for relapse. o Alternative Regimens: o Tinidazole 2 g po QD x 2 d o Tinidazole 1 g po QD x 5 d o Limited data on performance of these regimens Source: CDC STD Treatment Guidelines, 2010.

Recurrent BV o ~30% will have recurrence within 3 months, ~50% within 12 months 23 Repeat and/or prolonged treatment to 10 -14 days Suppression or long-term maintenance Change therapies Consider treating partner (orally) and/or recommend consistent condom use o Consider obtaining cultures o Little evidence for recolonization with lactobacilli or vaginal acidifying agents o o 23. Hillier, S, Holmes, KK. Bacterial vaginosis. In: Holmes, KK, Mardh, PA, Sparling, PF, Wiesner, PJ (Eds), Sexually Transmitted Diseases, 2 nd ed, Mc. Graw-Hill, New York: 1990, p. 547.

Recurrent BV: Suppression o More than 3 documented episodes of BV in 12 months o Avoid long-term clindamycin due to toxicity and lack of documented efficacy o Metronidazole gel 0. 75% x 10 days, then twice weekly for 3 -6 months 24 n Symptoms tend to recur once suppressive tx DC’d o Limited data on these suppressive tx’s: 24 a n Oral nitroimidazole followed by vaginal boric acid + suppressive metronidazole gel n Monthly oral metronidazole + fluconazole 24. Sobel JD; Ferris D; Schwebke J; Nyirjesy P; Wiesenfeld HC; Peipert J; Soper D; Ohmit SE; Hillier SL. Suppressive antibacterial therapy with 0. 75% metronidazole vaginal gel to prevent recurrent bacterial vaginosis. 24 A. CDC STD Treatment Guidelines, 2010.

BV in Pregnancy o Treat if symptoms present: n Oral preferred over topical to cover subclinical upper genital tract infections n Metronidazole 500 mg po BID x 7 d n Metronidazole 250 mg po TID x 7 d n Clindamycin 300 mg po BID x 7 d o Asymptomatic pregnant women: n High risk for preterm delivery o Studies yield mixed results; insufficient evidence for screening for BV n Low risk for preterm delivery o USPSTF recommends against screening Source: CDC STD Treatment Guidelines, 2010.

TRICHOMONAS VAGINALIS
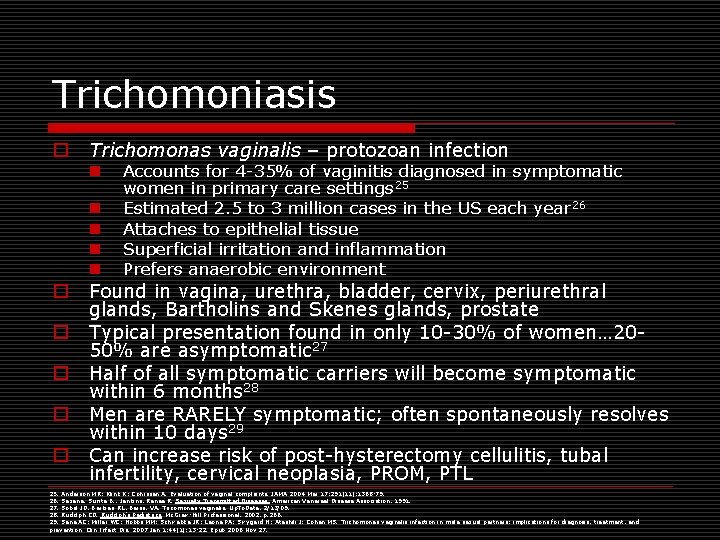
Trichomoniasis o Trichomonas vaginalis – protozoan infection n n o o o Accounts for 4 -35% of vaginitis diagnosed in symptomatic women in primary care settings 25 Estimated 2. 5 to 3 million cases in the US each year 26 Attaches to epithelial tissue Superficial irritation and inflammation Prefers anaerobic environment Found in vagina, urethra, bladder, cervix, periurethral glands, Bartholins and Skenes glands, prostate Typical presentation found in only 10 -30% of women… 2050% are asymptomatic 27 Half of all symptomatic carriers will become symptomatic within 6 months 28 Men are RARELY symptomatic; often spontaneously resolves within 10 days 29 Can increase risk of post-hysterectomy cellulitis, tubal infertility, cervical neoplasia, PROM, PTL 25. Anderson MR; Klink K; Cohrssen A. Evaluation of vaginal complaints. JAMA 2004 Mar 17; 291(11): 1368 -79. 26. Saxena, Sunita B. , Jenkins, Renee R. Sexually Transmitted Diseases. American Venereal Disease Association, 1991. 27. Sobel JD, Barbieri RL, Barss, VA. Tricomonas vaginalis. Up. To. Date, 2/13/09. 28. Rudolph CD. Rudolph’s Pediatrics. Mc. Graw-Hill Professional, 2002, p. 266. 29. Sena AC; Miller WC; Hobbs MM; Schwebke JR; Leone PA; Swygard H; Atashili J; Cohen MS. Trichomonas vaginalis infection in male sexual partners: implications for diagnosis, treatment, and prevention. Clin Infect Dis. 2007 Jan 1; 44(1): 13 -22. Epub 2006 Nov 27.
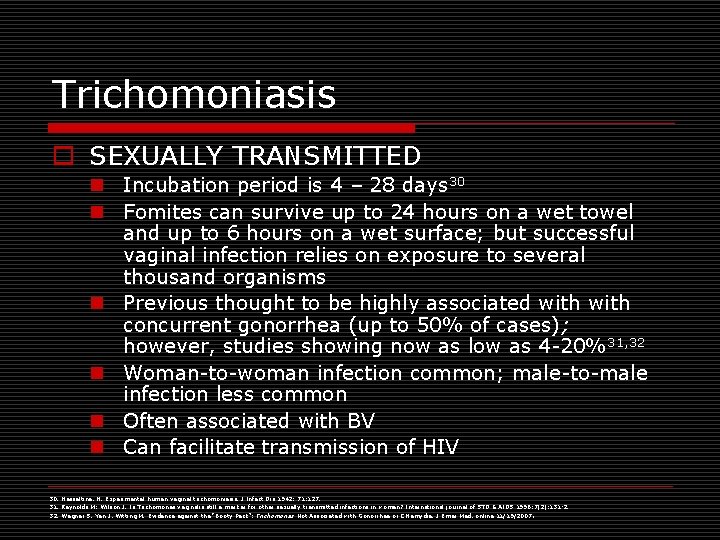
Trichomoniasis o SEXUALLY TRANSMITTED n Incubation period is 4 – 28 days 30 n Fomites can survive up to 24 hours on a wet towel and up to 6 hours on a wet surface; but successful vaginal infection relies on exposure to several thousand organisms n Previous thought to be highly associated with concurrent gonorrhea (up to 50% of cases); however, studies showing now as low as 4 -20%31, 32 n Woman-to-woman infection common; male-to-male infection less common n Often associated with BV n Can facilitate transmission of HIV 30. Hesseltine, H. Experimental human vaginal trichomoniasis. J Infect Dis 1942; 71: 127. 31. Reynolds M; Wilson J. Is Trichomonas vaginalis still a marker for other sexually transmitted infections in women? International journal of STD & AIDS 1996; 7(2): 131 -2. 32. Wegner S, Yen J, Witting M. Evidence against the “Booty Pack”: Trichomonas Not Associated with Gonorrhea or Chlamydia. J Emer Med, online 11/19/2007.

Trich: Subjective Data o Increased malodorous vaginal discharge o Vulvar pruritus o Dyspareunia o Dysuria
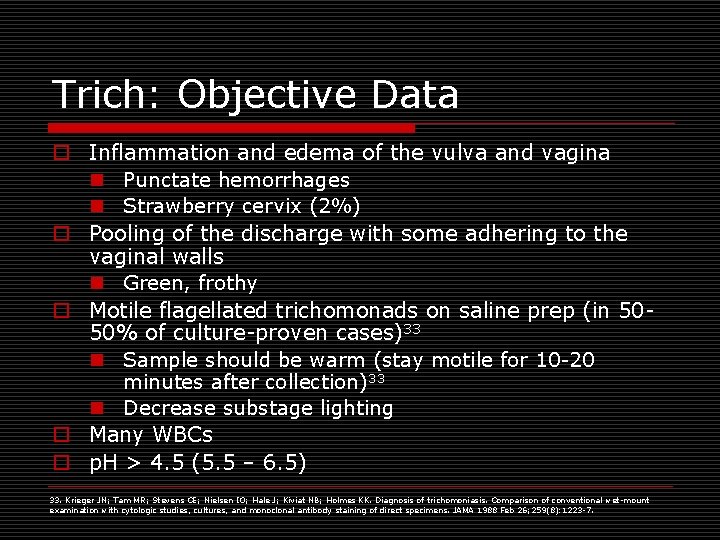
Trich: Objective Data o Inflammation and edema of the vulva and vagina n Punctate hemorrhages n Strawberry cervix (2%) o Pooling of the discharge with some adhering to the vaginal walls n Green, frothy o Motile flagellated trichomonads on saline prep (in 5050% of culture-proven cases)33 n Sample should be warm (stay motile for 10 -20 minutes after collection)33 n Decrease substage lighting o Many WBCs o p. H > 4. 5 (5. 5 – 6. 5) 33. Krieger JN; Tam MR; Stevens CE; Nielsen IO; Hale J; Kiviat NB; Holmes KK. Diagnosis of trichomoniasis. Comparison of conventional wet-mount examination with cytologic studies, cultures, and monoclonal antibody staining of direct specimens. JAMA 1988 Feb 26; 259(8): 1223 -7.

Trich: Saline Prep Slide on right from http: //2. bp. blogspot. com/_m. Lmek. Y 8 za. QA/Rw. Vk. Zdh. BHz. I/AAAAA 0/l 0 y. IAKb. HVPY/s 320/Trichomonas%2520 vaginalis. gif
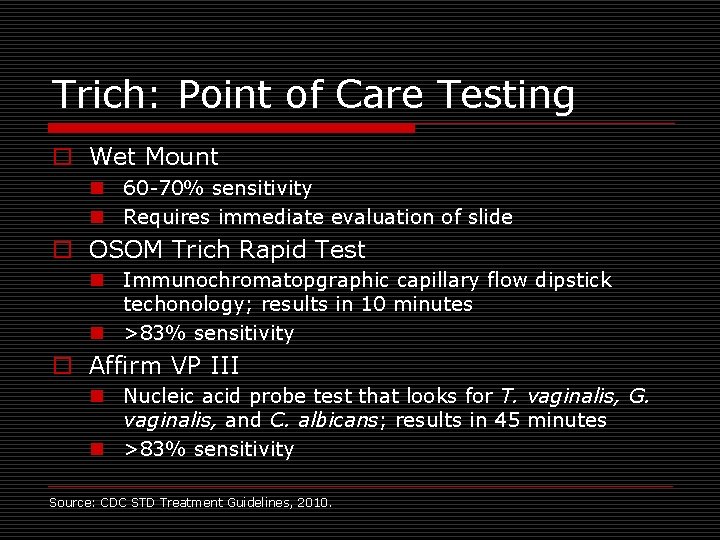
Trich: Point of Care Testing o Wet Mount n 60 -70% sensitivity n Requires immediate evaluation of slide o OSOM Trich Rapid Test n Immunochromatopgraphic capillary flow dipstick techonology; results in 10 minutes n >83% sensitivity o Affirm VP III n Nucleic acid probe test that looks for T. vaginalis, G. vaginalis, and C. albicans; results in 45 minutes n >83% sensitivity Source: CDC STD Treatment Guidelines, 2010.

Trich: Alternative Testing o Collect culture if trich is suspected but POC testing is negative n Can take up to 2 -7 days; $ o Pap test n n Poor sensitivity; sensitivity improved with liquid-based paps Recommend confirmatory testing with wet prep/other o PCR (Amplicor) n n n Polymerase Chain Reaction (amplifies DNA) Takes days; $ Sensitivity 88 -97% o TMA (APTIMA) n n n Transcription Mediated Amplificxn (amplifies RNA) Takes days; $ Sensitivity 74 -98% Source: CDC STD Treatment Guidelines, 2010.
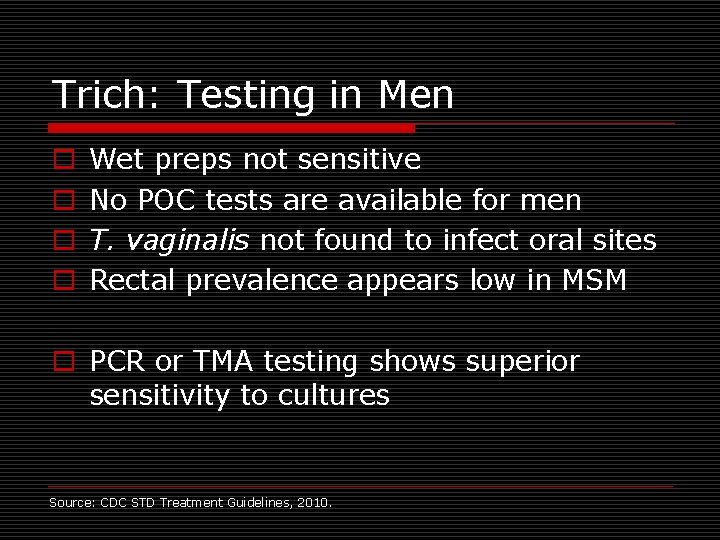
Trich: Testing in Men o o Wet preps not sensitive No POC tests are available for men T. vaginalis not found to infect oral sites Rectal prevalence appears low in MSM o PCR or TMA testing shows superior sensitivity to cultures Source: CDC STD Treatment Guidelines, 2010.
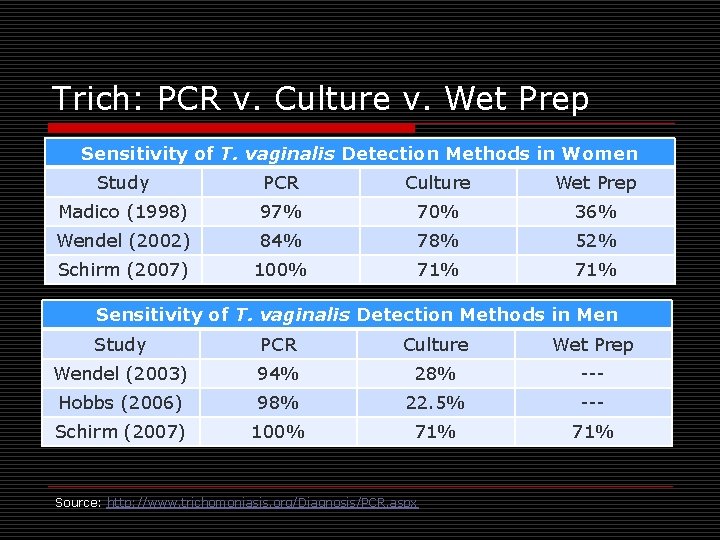
Trich: PCR v. Culture v. Wet Prep Sensitivity of T. vaginalis Detection Methods in Women Study PCR Culture Wet Prep Madico (1998) 97% 70% 36% Wendel (2002) 84% 78% 52% Schirm (2007) 100% 71% Sensitivity of T. vaginalis Detection Methods in Men Study PCR Culture Wet Prep Wendel (2003) 94% 28% --- Hobbs (2006) 98% 22. 5% --- Schirm (2007) 100% 71% Source: http: //www. trichomoniasis. org/Diagnosis/PCR. aspx

Trich: Treatment o Metronidazole 2 grams po single dose 34 n Cure rate of 90 -95%34 n Treat partner simultaneously n 1 st trimester of pregnancy: o May cross placenta and have potential for teratogenicity o Meta-analysis showed no relationship between metronidazole exposure during 1 st trimester and birth defects 35 o CDC no longer discourages use of metronidazole in the 1 st trimester n No intercourse for 48 hours after last dose of either partner (or use condoms) n Avoid breastfeeding for 12 -24 hours (metronidazole) or 72 hours (tinidazole) after dose 34. CDC STD Treatment Guidelines, 2010. 35. Caro-Paton, et al. Is metronidazole teratogenic? A meta-analysis. Br J Clin Pharmacol. 1997; 44: 179
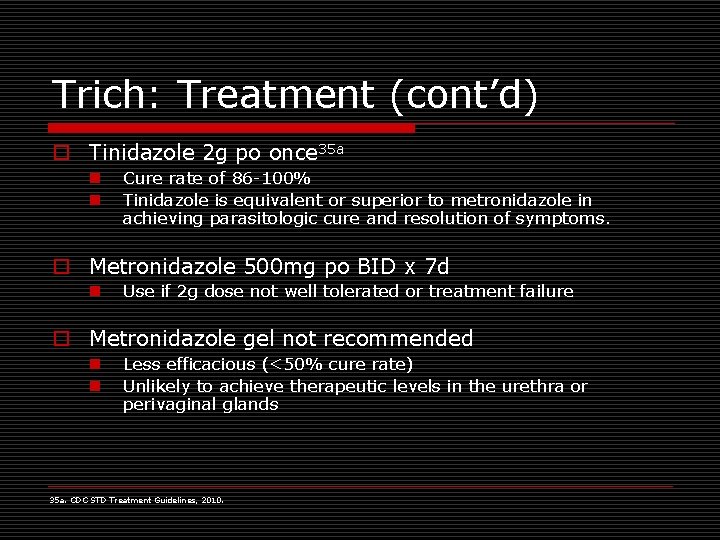
Trich: Treatment (cont’d) o Tinidazole 2 g po once 35 a n n Cure rate of 86 -100% Tinidazole is equivalent or superior to metronidazole in achieving parasitologic cure and resolution of symptoms. o Metronidazole 500 mg po BID x 7 d n Use if 2 g dose not well tolerated or treatment failure o Metronidazole gel not recommended n n Less efficacious (<50% cure rate) Unlikely to achieve therapeutic levels in the urethra or perivaginal glands 35 a. CDC STD Treatment Guidelines, 2010.
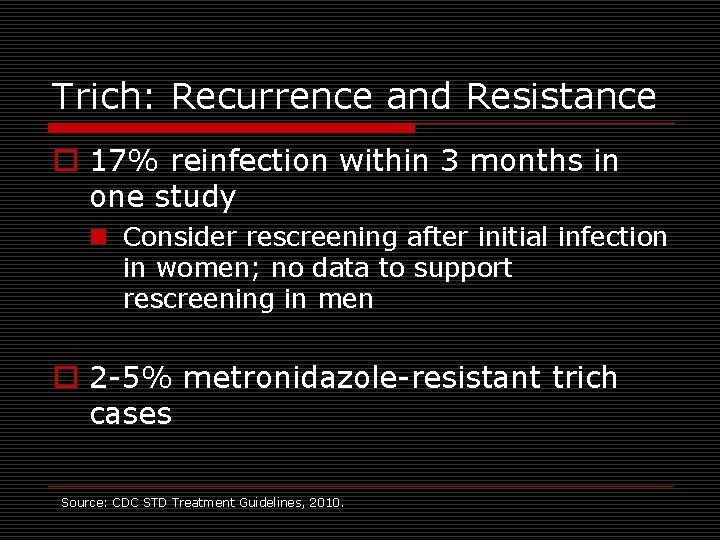
Trich: Recurrence and Resistance o 17% reinfection within 3 months in one study n Consider rescreening after initial infection in women; no data to support rescreening in men o 2 -5% metronidazole-resistant trich cases Source: CDC STD Treatment Guidelines, 2010.
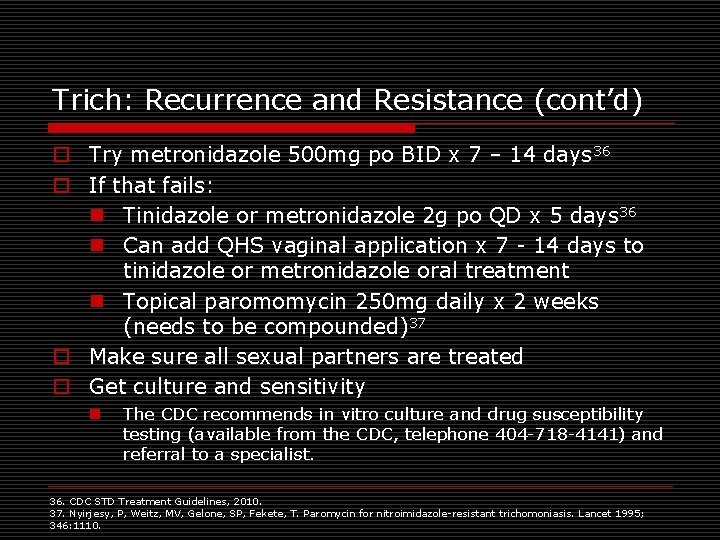
Trich: Recurrence and Resistance (cont’d) o Try metronidazole 500 mg po BID x 7 – 14 days 36 o If that fails: n Tinidazole or metronidazole 2 g po QD x 5 days 36 n Can add QHS vaginal application x 7 - 14 days to tinidazole or metronidazole oral treatment n Topical paromomycin 250 mg daily x 2 weeks (needs to be compounded)37 o Make sure all sexual partners are treated o Get culture and sensitivity n The CDC recommends in vitro culture and drug susceptibility testing (available from the CDC, telephone 404 -718 -4141) and referral to a specialist. 36. CDC STD Treatment Guidelines, 2010. 37. Nyirjesy, P, Weitz, MV, Gelone, SP, Fekete, T. Paromycin for nitroimidazole-resistant trichomoniasis. Lancet 1995; 346: 1110.

ATROPHIC VAGINITIS

Atrophic Vaginitis o Result of decreased estrogen n Estrogen maintains collagen content of epithelium and thus effects its thickness and elasticity atrophy n Decreased estrogen results in incomplete maturation and gradual loss of the glycogen-rich squamous epithelium n The lactobacilli disappear o Increased p. H to > 5. 0 o Vagina now more susceptible to pathogens n Reduction of vaginal secretions from 3 -4 g/four hours to 1. 7 g/four hours 38 38. Greendale GA; Judd HL. The menopause: health implications and clinical management. J Am Geriatr Soc. 1993 Apr; 41(4): 426 -36.

Atrophic Vaginitis o Largest cause is natural menopause o Also: Radiation therapy Ovarian failure Postpartum/lactational state Medications with anti-estrogen effects (tamoxifen, danazol, medroxyprogesterone, leuprolide, and nafarelin) n Bilateral oopherectomy n n
Atrophic Vaginitis o Other factors that modulate the degree of atrophy 39: n Cigarette smoking (reduces vaginal blood perfusion)40 n Vaginal nulliparity n Cessation of coital activity (enhances atrophic changes of contraction and rigidity) 39. Bachmann GA; Nevadunsky NS. Diagnosis and treatment of atrophic vaginitis. Am Fam Physician. 2000 May 15; 61(10): 3090 -6. 40. Castelo-Branco C; Cancelo MJ; Villero J; Nohales F; Julia MD. Management of post-menopausal vaginal atrophy and atrophic vaginitis. Maturitas. 2005 Nov 15; 52 Suppl 1: S 46 -52. Epub 2005 Sep 1.

Atrophic Vaginitis: Subjective Data o Pruritis o Vulvar irritation o Dysuria, frequency, urgency n Bladder has estrogen receptors, too! o Dyspareunia o Vaginal spotting o Leukorrhea or yellow malodorous vaginal discharge
Atrophic Vaginitis: Objective Data o Related to decreased estrogen state: n n n Sparse, brittle pubic hair Thinning and shrinking of vulva Narrow vaginal introitus Smooth, flattened rugae Small, pale cervix NOTE: May need to use a pediatric-sized speculum

Atrophic Vaginitis: Objective Data o Diffuse vaginal erythema and/or petechial hemorrhages o Few or no lactobacilli o Bacteria o Increased WBCs o p. H 5. 5 – 7. 0 o Parabasal squamous cells (immature in appearance)
Atrophic Vaginitis: Treatment o o Topical vaginal estrogen: n Cream: Premarin or Estrace 1/8 (0. 5 g) to one (2. 0 g) applicator PV QHS x 7 -14 days, then taper to 1/8 to ¼ applicator once to twice weekly, titrated to symptoms o Maximum doses 2. 0 g/day should not be used long term because it causes premenopausal plasma levels of estradiol 41 n Tablet: Vagifem 25 mcgs PV daily x 2 weeks and then twice per week 42 o Estradiol levels in plasma minimally increase during use of these tablets, although not to premenopausal levels 43 Estring 2 mg estradiol in ring x 90 days 44 n Estimated to have approximately 10% systemic absorption 45 May use oral estrogen, but consider pros and cons! A progestin is probably not necessary to protect against endometrial hyperplasia in women receiving low dose local estrogen therapy 41. Mandel FP; Geola FL; Meldrum DR; Lu JH; Eggena P; Sambhi MP; Hershman JM; Judd HL. Biological effects of various doses of vaginally administered conjugated equine estrogens in postmenopausal women. J Clin Endocrinol Metab 1983 Jul; 57(1): 133 -9. 42. The role of local vaginal estrogen for treatment of vaginal atrophy in postmenopausal women: 2007 position statement of The North American Menopause Society. Menopause. 2007 May-Jun; 14(3): 357 -69. 43. Kendall A; Dowsett M; Folkerd E; Smith I. Caution: Vaginal estradiol appears to be contraindicated in postmenopausal women on adjuvant aromatase inhibitors. Ann Oncol. 2006 Apr; 17(4): 584 -7. Epub 2006 Jan 27. 44. Baker VL. Alternatives to oral estrogen replacement. Transdermal patches, percutaneous gels, vaginal creams and rings, implants, other methods of delivery. Obstet Gynecol Clin North Am 1994 Jun; 21(2): 271 -97. 45. Weisberg E; Ayton R; Darling G; Farrell E; Murkies A; O'Neill S; Kirkegard Y; Fraser IS Endometrial and vaginal effects of low-dose estradiol delivered by vaginal ring or vaginal tablet. Climacteric. 2005 Mar; 8(1): 83 -92.
Atrophic Vaginitis: Treatment o Moisturizers and lubricants n Replens o polycarbophilp-based bioadhesive polymer that binds to vaginal epithelium, releases purified water, and produces a moist film o Replens should not be used immediately prior to intercourse, but should be used regularly to maintain chronic moisturization n Water-based lubricant during sex
DESQUAMATIVE INFLAMMATORY VAGINITIS

Desquamative Inflammatory Vaginitis o o Rare chronic clinical syndrome of unknown etiology Symptoms: n Dyspareunia n Vaginal/introital pain n Diffuse exudative vaginitis n Epithelial cell exfoliation n Profuse vaginal discharge Diagnosis: n Presence of purulent vaginal discharge n Leukocyte to epithelial cell ratio greater than 1: 1 n Vaginal p. H > 4. 5 n Excluded bacterial vaginosis, N. gonorrhoeae, C. trachomatis, and T. vaginalis infection Treatment: n Clindamycin suppositories 200 mg PV QHS x 14 days n 10% hydrocortisone PV daily with gradual withdrawal as symptoms resolve n Clindamycin 150 mg PO BID + vaginal clobetasol QOD x 4 -6 weeks Source: Sobel JD, Barbieri RL, Barss VA. Chronic and acute causes of vaginal discharge other than bacterial vaginosis, candidiasis, or trichomoniasis. Up. To. Date, 2/4/09.

CYTOLYTIC VAGNINOSIS
Cytolytic Vaginosis o o o Syndrome of vaginal hyperacidity due to overgrowth by lactobacilli The existence of this entity is controversial Symptoms: n Pruritus n Dyspareunia n Vulvar dysuria n Cyclical increase in symptoms during the luteal phase Diagnosis: n Presence of white vaginal discharge n Vaginal p. H between 3. 5 and 4. 5 n Gram's stain showing overgrowth of lactobacilli n Few WBCs n Evidence of cytolysis (bare nuclei, shreds of cytoplasm) n Exclusion of candidal infection Treatment: n Sodium bicarbonate douches - solution of one rounded teaspoon of sodium bicarbonate in 600 m. L of water is used for irrigating the vagina, once per day for 7 to 14 days Source: Sobel JD, Barbieri RL, Barss VA. Chronic and acute causes of vaginal discharge other than bacterial vaginosis, candidiasis, or trichomoniasis. Up. To. Date, 2/4/09.
GROUP A STREPTOCOCCAL VAGINITIS
![Group A Streptococcal Vaginitis o Group A streptococcus (Streptococcus pyogenes [GAS]) is an uncommon Group A Streptococcal Vaginitis o Group A streptococcus (Streptococcus pyogenes [GAS]) is an uncommon](http://slidetodoc.com/presentation_image/2a1d80f9c9e6ea0540eb0d1ba368b914/image-87.jpg)
Group A Streptococcal Vaginitis o Group A streptococcus (Streptococcus pyogenes [GAS]) is an uncommon cause of vulvovaginitis n Typically occurs in prepubertal girls and in mothers whose children suffer from active GAS infection or who serve as GAS carriers n Carriage or exposure to a carrier is an important source of recurrent GAS infection n GAS can colonize and be transmitted from skin (especially in individuals with chronic dermatological conditions), nasopharynx, and the gastrointestinal tract (including the perianal area) n Symptoms: o Acute onset of frankly purulent discharge o Pruritus, soreness and irritation, erythema, and labial edema n Diagnosis: o Microscopy of the discharge reveals a marked increase in PMNs o Gram's stain shows chains of gram-positive cocci o Culture? n Treatment: o Penicillin VK 500 mg PO QID for 10 to 14 days o Clindamycin cream 2% PV for 7 to 10 days Source: Sobel JD, Barbieri RL, Barss VA. Chronic and acute causes of vaginal discharge other than bacterial vaginosis, candidiasis, or trichomoniasis. Up. To. Date, 2/4/09.
GROUP B STREPTOCOCCAL VAGINITIS

Group B Streptococcal Vaginitis o Group B streptococcus (GBS) commonly colonizes the vagina and causes neonatal sepsis and maternal upper tract infection (endometritis) n Whether GBS is a pathogen in the vagina is controversial o Some clinicians believe it has a pathogenic role in vaginitis and report an ameliorative effect on symptoms with antibiotic treatment (oral penicillin or clindamycin cream) o Others question whether this organism has a pathogenic role in causing vaginitis, thus they avoid both culture and treatment of positive culture results. Source: Sobel JD, Barbieri RL, Barss VA. Chronic and acute causes of vaginal discharge other than bacterial vaginosis, candidiasis, or trichomoniasis. Up. To. Date, 2/4/09.

QUESTIONS? Stephanie Sola MN RNC ARNP Seattle University Student Health Center (206) 296 -2574 padillas@seattleu. edu
- Slides: 90