VA Office of Community Care Provider Overview February
VA Office of Community Care Provider Overview February 11, 2020 Charlotte Mc. Grath National Office of Community Care Regional Provider Experience Manager Community Care Network (CCN) Region 2
Outline and Agenda o Referrals/Authorizations • Emergency and Urgent Care o Medical Records o Claims and Payments o Resources o Questions 2

REFERRALS AND AUTHORIZATIONS 3
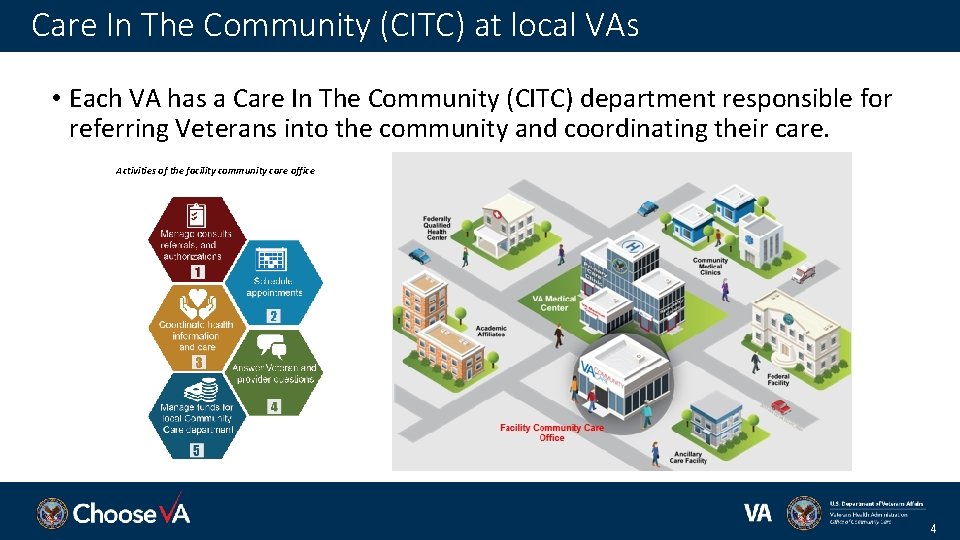
Care In The Community (CITC) at local VAs • Each VA has a Care In The Community (CITC) department responsible for referring Veterans into the community and coordinating their care. Activities of the facility community care office 4

Referrals and Authorizations VA Community Care requires authorization in advance/preauthorization prior to providing services. Without an authorization, the services performed may not be reimbursable by VA or its TPA. *Exceptions of VA preauthorization include Emergency and Urgent Care. Veteran is in need of care. VA provider orders care in the community for Veterans eligibility Veteran eligibility verified. for Community Care. 01 02 CITC finds community provider and authorizes care. 03 Community provider: accepts referral, treats Veteran, returns medical records to CITC. Coordinates care and collects community provider documentation. 04 5
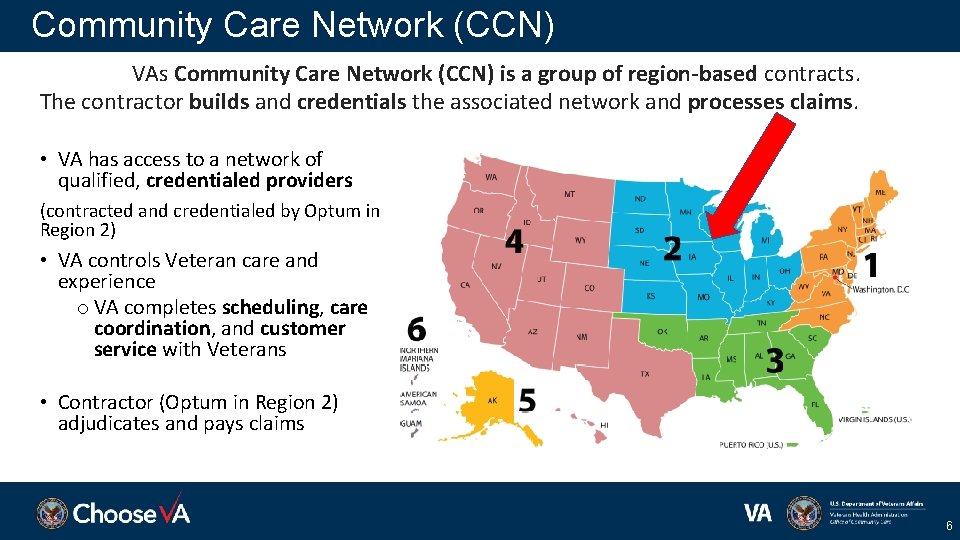
Community Care Network (CCN) VAs Community Care Network (CCN) is a group of region-based contracts. The contractor builds and credentials the associated network and processes claims. • VA has access to a network of qualified, credentialed providers (contracted and credentialed by Optum in Region 2) • VA controls Veteran care and experience o VA completes scheduling, care coordination, and customer service with Veterans • Contractor (Optum in Region 2) adjudicates and pays claims 6
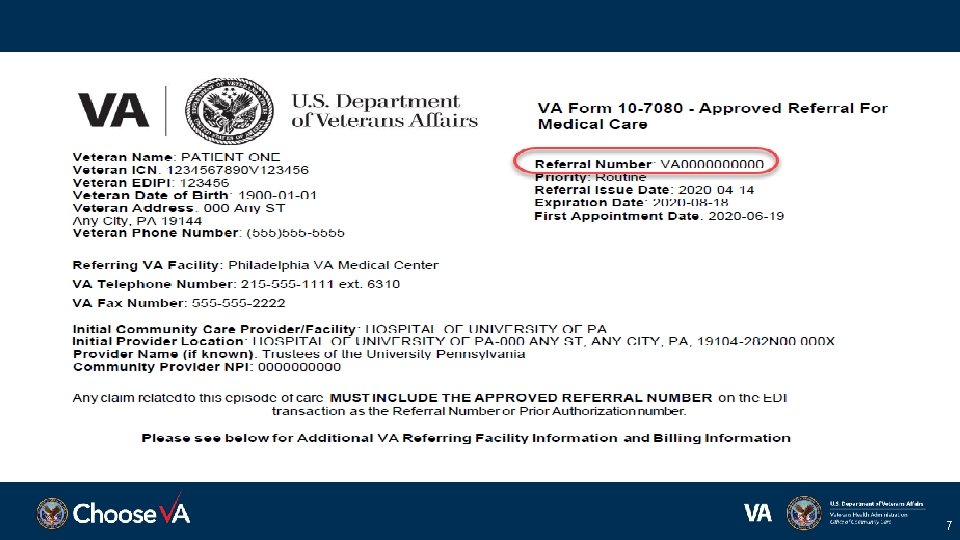
7

8
Standardized Episode of Care VA uses SEOCs (Standardized Episodes of Care) to refer and authorize Care in the Community https: //www. va. gov/COMMUNITYCARE/providers/PRCT_requirements. asp • Prior to viewing the VA SEOC Billing Code List, you must accept the terms and conditions defined in the License for Use Of Current Procedural Terminology 9
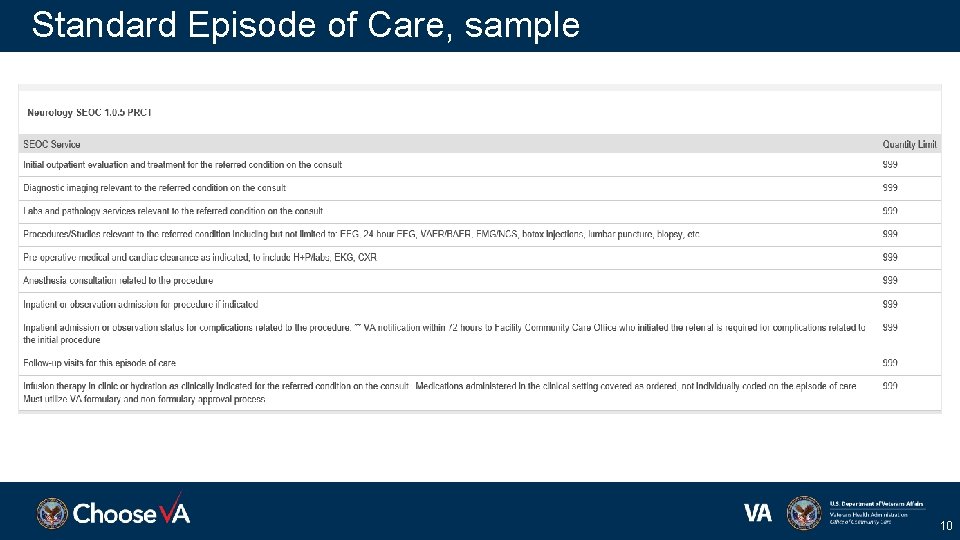
Standard Episode of Care, sample 10
Care beyond original referral • Note the dates on the referral – start date and extent of authorization • CPT codes on SEOCs • For additional or continued care beyond the original authorization: Utilize Request for Services • Sent to the VA, who provided the original authorization, for review and approval/disapproval https: //www. va. gov/vaforms/form_detail. asp? Form. No=10172 11
AUTHORIZED EMERGENCY CARE UNAUTHORIZED EMERGENCY CARE https: //www. va. gov/COMMUNITYCARE/providers/info_Emergency. Care. asp 12
Centralized Notification VETERAN PRESENTS FOR ER CARE WITHIN 72 hours, provide notification to VA (includes weekends and holidays) Online: Emergency Care Reporting Phone: 844 -72 HRVHA (844 -724 -7842) Do NOT contact, phone, or fax your local VA of notification. A decision of eligibility will be returned to you. 13
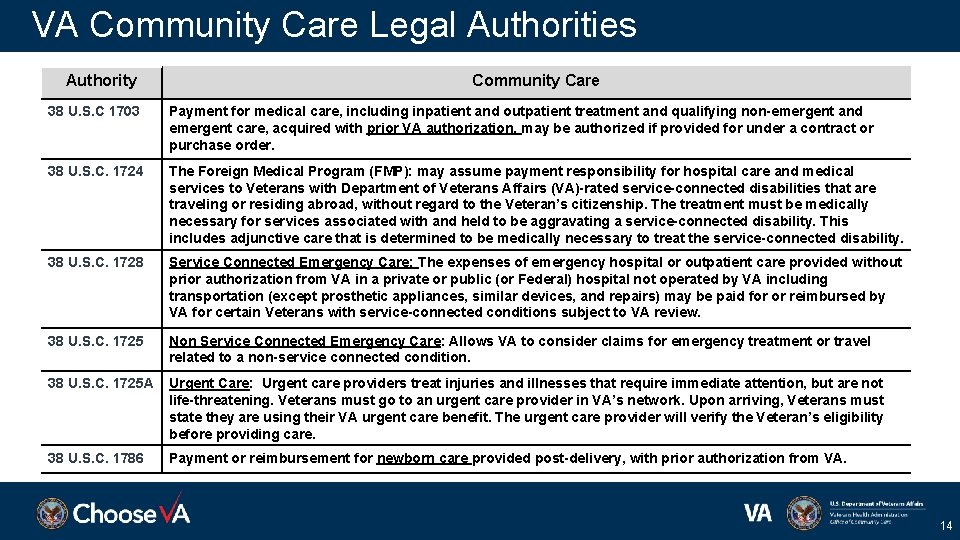
VA Community Care Legal Authorities Authority Community Care 38 U. S. C 1703 Payment for medical care, including inpatient and outpatient treatment and qualifying non-emergent and emergent care, acquired with prior VA authorization, may be authorized if provided for under a contract or purchase order. 38 U. S. C. 1724 The Foreign Medical Program (FMP): may assume payment responsibility for hospital care and medical services to Veterans with Department of Veterans Affairs (VA)-rated service-connected disabilities that are traveling or residing abroad, without regard to the Veteran’s citizenship. The treatment must be medically necessary for services associated with and held to be aggravating a service-connected disability. This includes adjunctive care that is determined to be medically necessary to treat the service-connected disability. 38 U. S. C. 1728 Service Connected Emergency Care: The expenses of emergency hospital or outpatient care provided without prior authorization from VA in a private or public (or Federal) hospital not operated by VA including transportation (except prosthetic appliances, similar devices, and repairs) may be paid for or reimbursed by VA for certain Veterans with service-connected conditions subject to VA review. 38 U. S. C. 1725 Non Service Connected Emergency Care: Allows VA to consider claims for emergency treatment or travel related to a non-service connected condition. 38 U. S. C. 1725 A Urgent Care: Urgent care providers treat injuries and illnesses that require immediate attention, but are not life-threatening. Veterans must go to an urgent care provider in VA’s network. Upon arriving, Veterans must state they are using their VA urgent care benefit. The urgent care provider will verify the Veteran’s eligibility before providing care. 38 U. S. C. 1786 Payment or reimbursement for newborn care provided post-delivery, with prior authorization from VA. 14
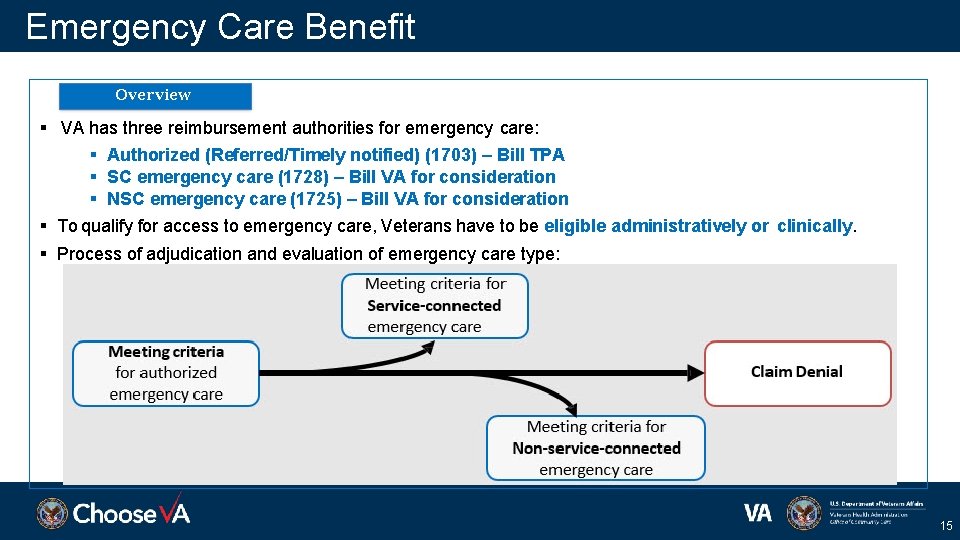
Emergency Care Benefit Overview VA has three reimbursement authorities for emergency care: Authorized (Referred/Timely notified) (1703) – Bill TPA SC emergency care (1728) – Bill VA for consideration NSC emergency care (1725) – Bill VA for consideration To qualify for access to emergency care, Veterans have to be eligible administratively or clinically. Process of adjudication and evaluation of emergency care type: 15
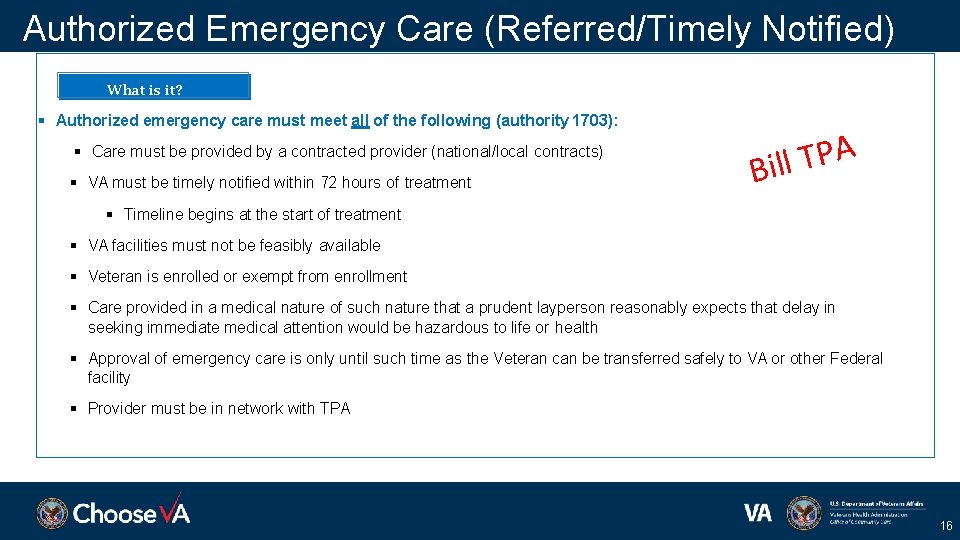
Authorized Emergency Care (Referred/Timely Notified) What is it? Authorized emergency care must meet all of the following (authority 1703): Care must be provided by a contracted provider (national/local contracts) VA must be timely notified within 72 hours of treatment A P T l Bil Timeline begins at the start of treatment VA facilities must not be feasibly available Veteran is enrolled or exempt from enrollment Care provided in a medical nature of such nature that a prudent layperson reasonably expects that delay in seeking immediate medical attention would be hazardous to life or health Approval of emergency care is only until such time as the Veteran can be transferred safely to VA or other Federal facility Provider must be in network with TPA 16
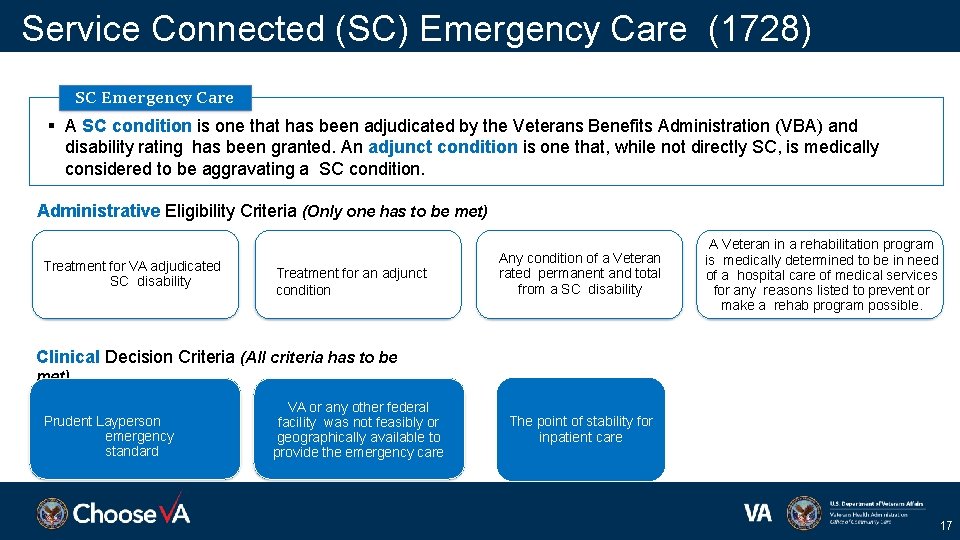
Service Connected (SC) Emergency Care (1728) SC Emergency Care A SC condition is one that has been adjudicated by the Veterans Benefits Administration (VBA) and disability rating has been granted. An adjunct condition is one that, while not directly SC, is medically considered to be aggravating a SC condition. Administrative Eligibility Criteria (Only one has to be met) Treatment for VA adjudicated SC disability Treatment for an adjunct condition Any condition of a Veteran rated permanent and total from a SC disability A Veteran in a rehabilitation program is medically determined to be in need of a hospital care of medical services for any reasons listed to prevent or make a rehab program possible. Clinical Decision Criteria (All criteria has to be met) Prudent Layperson emergency standard VA or any other federal facility was not feasibly or geographically available to provide the emergency care The point of stability for inpatient care 17
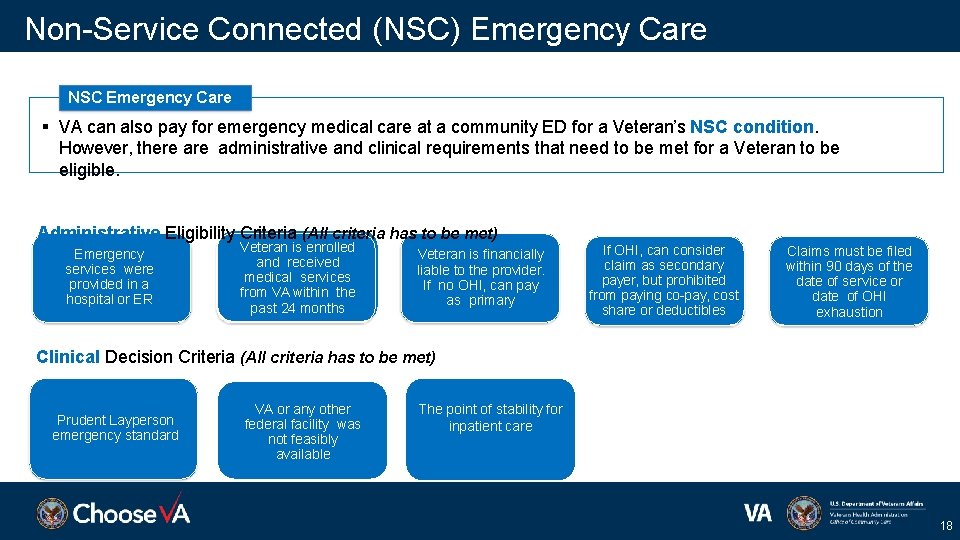
Non-Service Connected (NSC) Emergency Care NSC Emergency Care VA can also pay for emergency medical care at a community ED for a Veteran’s NSC condition. However, there administrative and clinical requirements that need to be met for a Veteran to be eligible. Administrative Eligibility Criteria (All criteria has to be met) Emergency services were provided in a hospital or ER Veteran is enrolled and received medical services from VA within the past 24 months Veteran is financially liable to the provider. If no OHI, can pay as primary If OHI, can consider claim as secondary payer, but prohibited from paying co-pay, cost share or deductibles Claims must be filed within 90 days of the date of service or date of OHI exhaustion Clinical Decision Criteria (All criteria has to be met) Prudent Layperson emergency standard VA or any other The point facility of stability federal wasfor inpatient not feasiblycre available The point of stability for inpatient care 18
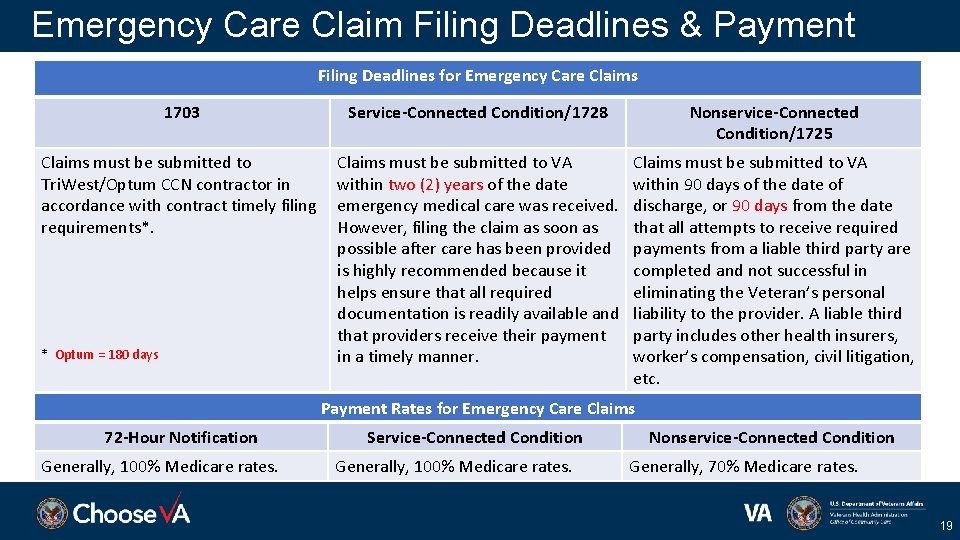
Emergency Care Claim Filing Deadlines & Payment Filing Deadlines for Emergency Care Claims 1703 Service-Connected Condition/1728 Nonservice-Connected Condition/1725 Claims must be submitted to Tri. West/Optum CCN contractor in accordance with contract timely filing requirements*. Claims must be submitted to VA within two (2) years of the date emergency medical care was received. However, filing the claim as soon as possible after care has been provided is highly recommended because it helps ensure that all required documentation is readily available and that providers receive their payment in a timely manner. Claims must be submitted to VA within 90 days of the date of discharge, or 90 days from the date that all attempts to receive required payments from a liable third party are completed and not successful in eliminating the Veteran’s personal liability to the provider. A liable third party includes other health insurers, worker’s compensation, civil litigation, etc. * Optum = 180 days Payment Rates for Emergency Care Claims 72 -Hour Notification Generally, 100% Medicare rates. Service-Connected Condition Generally, 100% Medicare rates. Nonservice-Connected Condition Generally, 70% Medicare rates. 19
Emergency Care Claim Filing to VA • Medical documentation must accompany your claim to VA for 1725/1728 consideration • VA can be secondary payer ONLY on 1725 ER claims Coinsurance and Deductible only; not copays Claim must include OHI EOB Paper to Electronic Claims - Community Care (va. gov) 20

MEDICAL RECORDS 21
Medical Documentation • Utilize Health. Share Referral Manager (HSRM) for referrals, authorizations and documentation exchange • Join Veterans Health Information Exchange (VHIE), enables bidirectional sharing of Veteran Health Information • Use Azure Rights Management Services (Azure RMS) for encrypted email • E-fax – documentation sent via email to VAMC’s fax machine. Contact referring VAMC for number. 22
Health. Share Referral Manager (HSRM), is VA’s new secure online portal for managing referrals and authorizations. It revolutionizes the way community providers partner with VA to serve Veterans • Standardizes referrals with consistent format and data from VA • Facilitates Health information Exchange (HIE) between community providers and VA via one unified platform • Tracks healthcare delivery by monitoring and recording services provided • Captures and retains details regarding unique patient requirements • Gives community providers the flexibility to easily refer Veterans for other specialized care • Generates reports to inform decision-making and track workflow 23
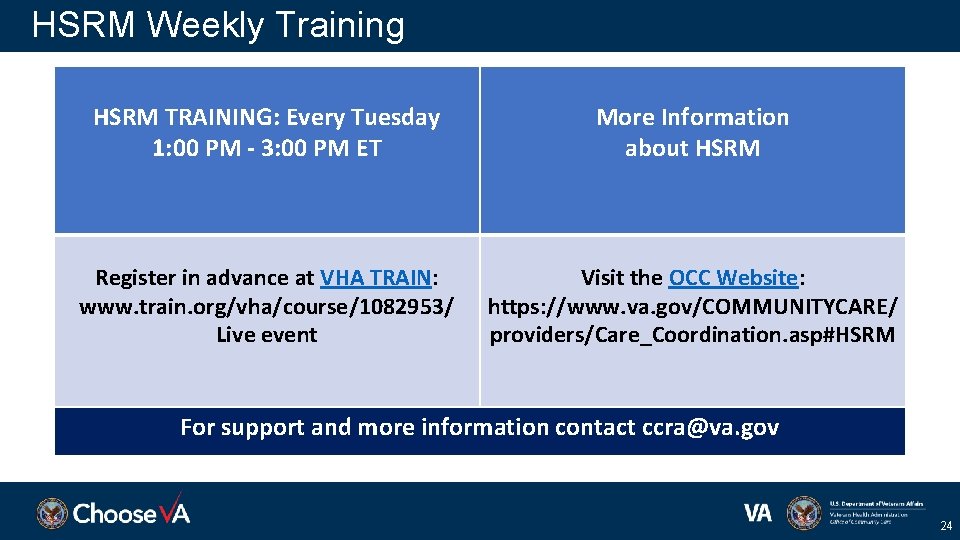
HSRM Weekly Training HSRM TRAINING: Every Tuesday 1: 00 PM - 3: 00 PM ET More Information about HSRM Register in advance at VHA TRAIN: www. train. org/vha/course/1082953/ Live event Visit the OCC Website: https: //www. va. gov/COMMUNITYCARE/ providers/Care_Coordination. asp#HSRM For support and more information contact ccra@va. gov 24

CLAIMS AND PAYMENTS 25
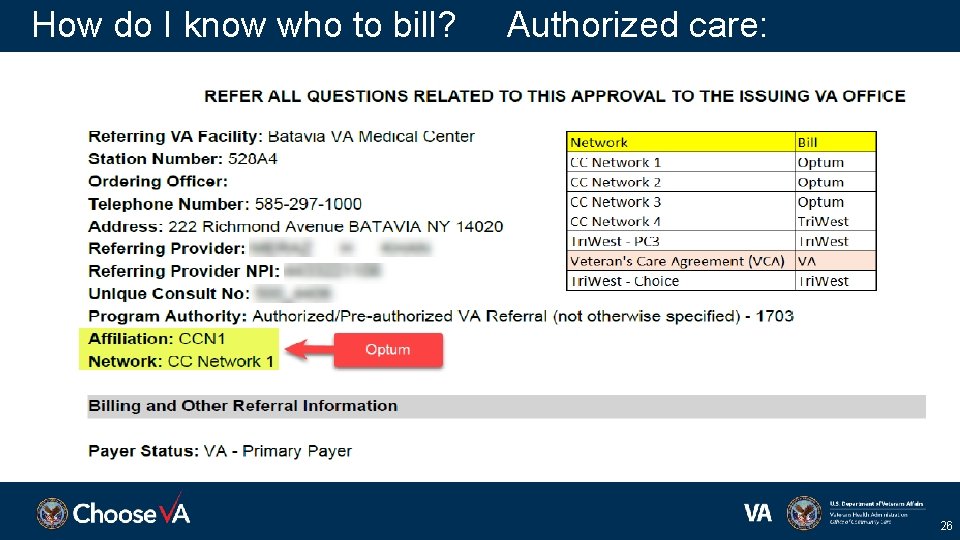
How do I know who to bill? Authorized care: 26
Claims Processing • An authorization/referral number must be submitted on all claims that are for pre-approved services. • For paper claims, include this information in field 23 on a HCFA 1500 or field 63 on a UB-04. For EDI 837, Referral Number is Loop = 2300, Segment = REF*9 F, Position = REF 02 or Prior Authorization, Loop = 2300, Segment = REF*G 1, Position = REF 02. 27
How do I know who to bill? ER and Urgent Care ER Care (subsequent observation or inpatient stay) Follow your 72 -hour notification center decision: • 1703 – submit claim to Optum (Must include authorization number on the claim) • 1725/1728 – submit claim to VA for consideration (Must include medical documentation with claim; there will be NO authorization number) • Didn’t notify VA within 72 hours? Submit claim to VA for consideration Urgent Care • Submit claim to Optum with UCERN 28
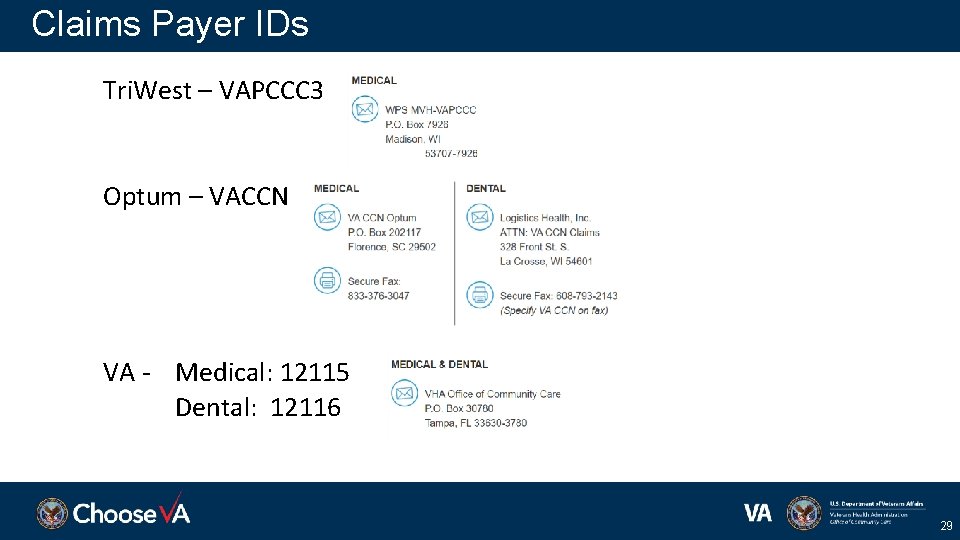
Claims Payer IDs Tri. West – VAPCCC 3 Optum – VACCN VA - Medical: 12115 Dental: 12116 29
Linking Paper-Based Documentation to Electronic Claims • Emergency care claims and associated records sent to VA in a paper format will undergo electronic conversion to 837 and 275 transactions. In order to process claims properly, the VA must link supporting documentation submitted with its corresponding claim. • For linkage to occur, community providers should submit all paper-based supporting documentation with enough data to associate it with an emergency care claim, and can do so by including the following with their paper submission: • A paper claim or a copy of the claim AND • An accurately completed cover sheet https: //www. va. gov/COMMUNITYCARE/providers/info_claims. P 2 E. asp 30
Unpaid claims • Check referral/authorization • Billed correct DOS and care? • Submitted to correct payor? • Referral/authorization number on claim? • Tri. West or Optum – contact Provider Service line o Tri. West Provider Services Line 866 -651 -4977 (Tri. West claims assistance) o Optum Provider Services 844 -839 -6108 (Optum claims assistance) • VA – check CEP; contact C 4 o Community Care Call Ctr 877 -881 -7618 (VA claims assistance) 31
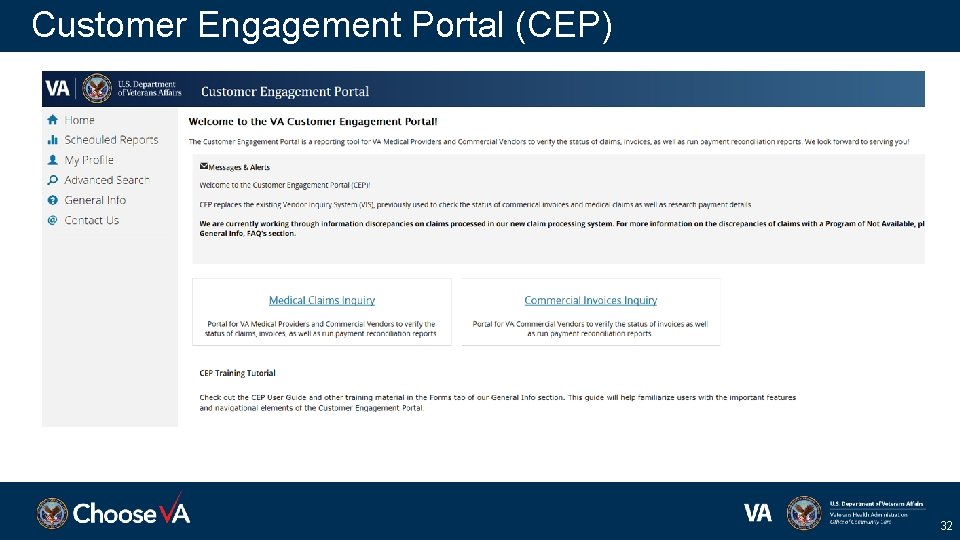
Customer Engagement Portal (CEP) 32
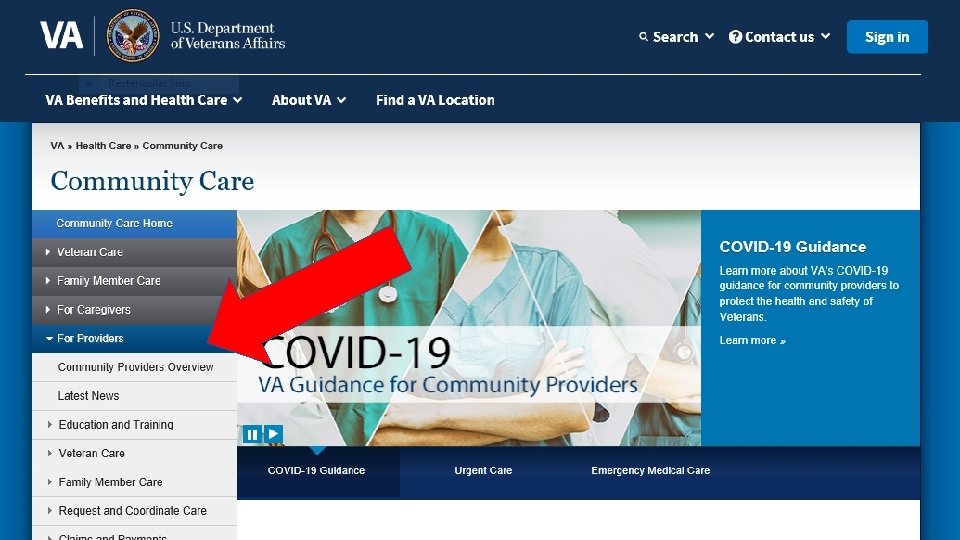
Resources • Information for Providers: – VA Community Care Website – Fact Sheet: How to Become a VA Community Provider – Monthly Provider Webinar – Monthly Provider Newsletter – Provider Reference Guide – Care Coordination – Health. Share Referral Manager/HSRM – – – Emergency Care Webpage Urgent Care Webpage VA Claims Payment Webpage VA Community Care Call Ctr 877 -881 -7618 (VA claims assistance) Tri. West Provider Services Line 866 -651 -4977 (Tri. West claims assistance) Optum Provider Services 844 -839 -6108 (Optum claims assistance) 33
Resources, continued • Tri. West Website • Optum Website • Viewing VA Claims Status: o Customer Engagement Portal (CEP) Webpage o Online viewing of EOBs and EOPs Webpage • Community Provider Training Information: o Provider Education & Training Resources Webpage o VHA TRAIN MISSION Act curriculum training site (VHA TRAIN MA) No cost, Veteran-focused training for community providers • VA’s Regional Provider Experience Manager – Community Care Network (CCN) Region 2 Charlotte. Mc. Grath@va. gov 34
35
- Slides: 35