VA Hand Hygiene Improvement Project Improving Hand Hygiene


- Slides: 28
VA Hand Hygiene Improvement Project: Improving Hand Hygiene by Using Targeted Solutions® Tool (TST)* Infection Prevention Medicine Service Nursing Service Volunteers * Joint Commission Center for Transforming Healthcare
Disclosures The views expressed in this presentation are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or the University of Texas Health Science Center at San Antonio. I have a small IIR grant from Pfizer to study clinical outcomes of coccidioidomycosis.
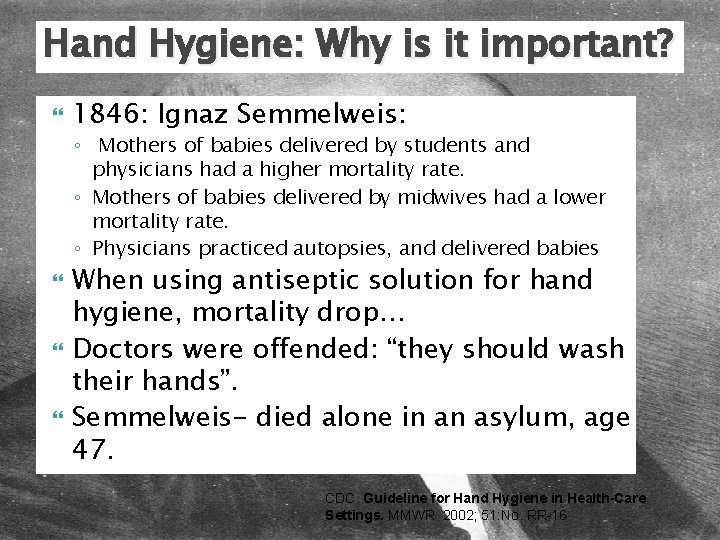
Hand Hygiene: Why is it important? 1846: Ignaz Semmelweis: ◦ Mothers of babies delivered by students and physicians had a higher mortality rate. ◦ Mothers of babies delivered by midwives had a lower mortality rate. ◦ Physicians practiced autopsies, and delivered babies When using antiseptic solution for hand hygiene, mortality drop… Doctors were offended: “they should wash their hands”. Semmelweis- died alone in an asylum, age 47. CDC. Guideline for Hand Hygiene in Health-Care Settings. MMWR 2002; 51: No. RR-16
An estimated 2 million patients get a hospital -related infection every year and 90, 000 die from their infection. – Centers for Disease Control and Prevention “…(Hand washing) gradually became accepted as one of the most important measures for preventing transmission of pathogens in health-care facilities” NPSG 07. 01 Comply with HH guidelines CDC. Guideline for Hand Hygiene in Health-Care Settings. MMWR 2002; 51: No. RR-16
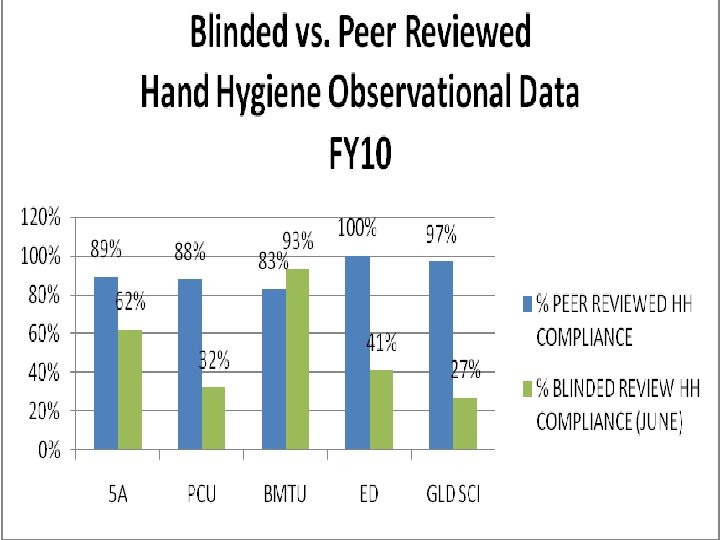
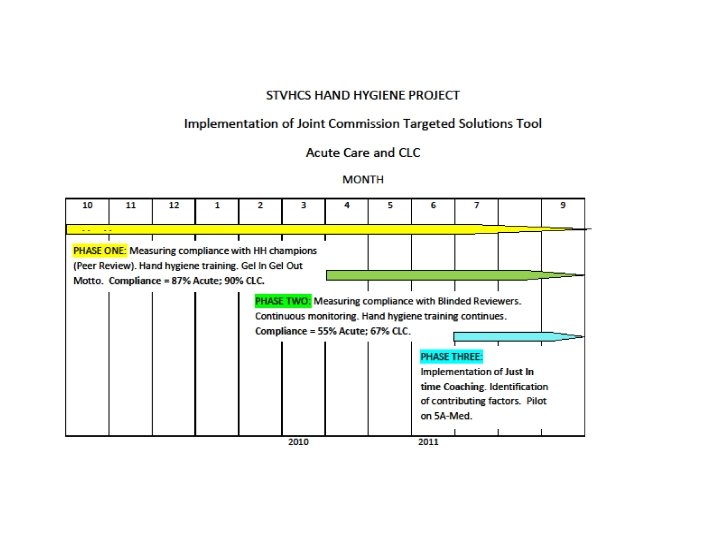
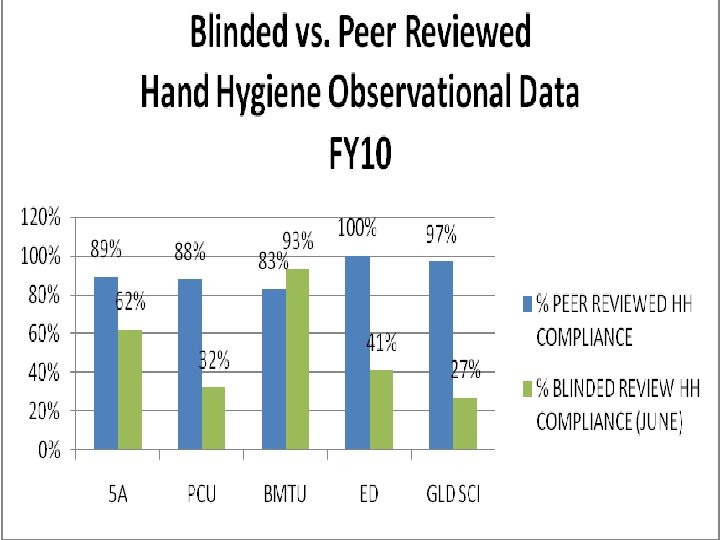
The problem Discrepancy between peer review and blinded review HH observations in acute care at ALM Hospital
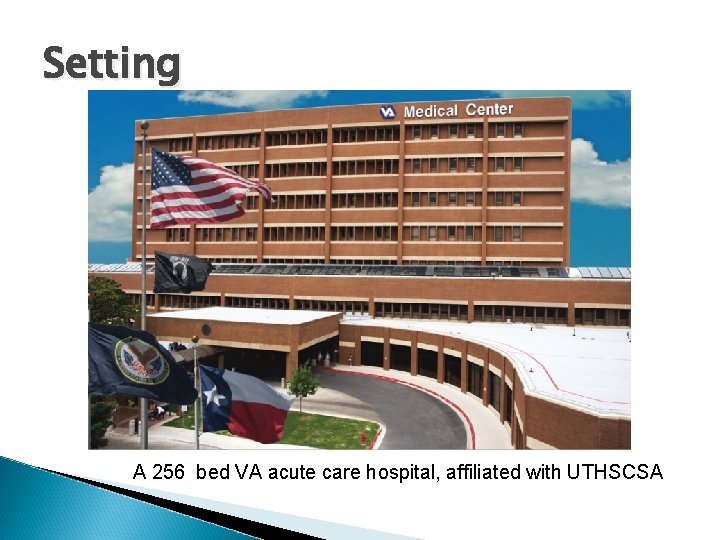
Setting A 256 bed VA acute care hospital, affiliated with UTHSCSA
Team Members Medical service: Infectious Diseases and Hospital Epidemiology Nursing: Nurse Managers, Nursing Staff Leadership: Hospital Director, Chief of Staff, Nursing Leadership Quality improvement: Infection Prevention and Control Staff Volunteers: Healthcare students

Goal To improve HH compliance by changing the culture of patient safety
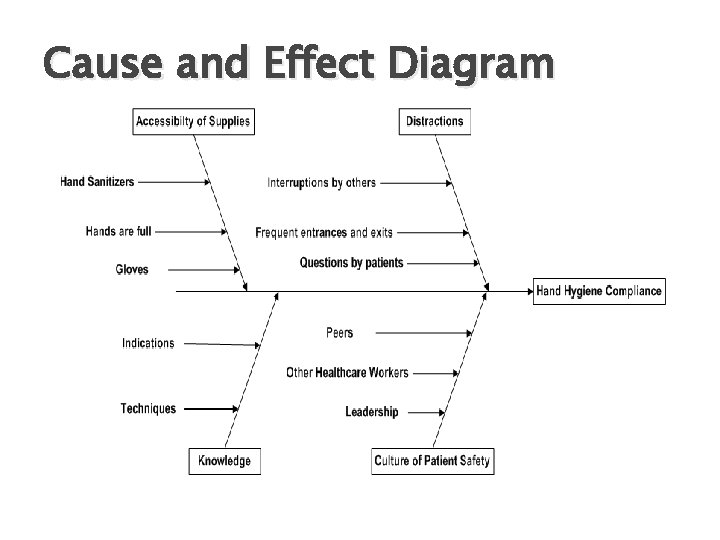
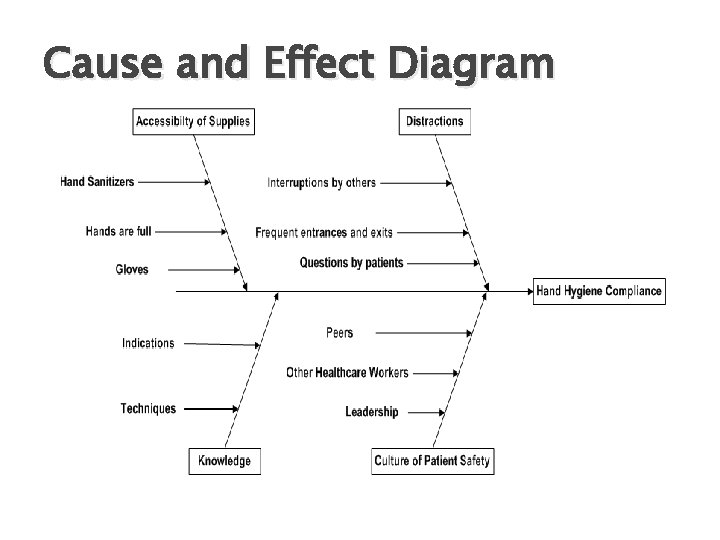
Cause and Effect Diagram
Center for Transforming Healthcare Mission: to transform healthcare to high reliability
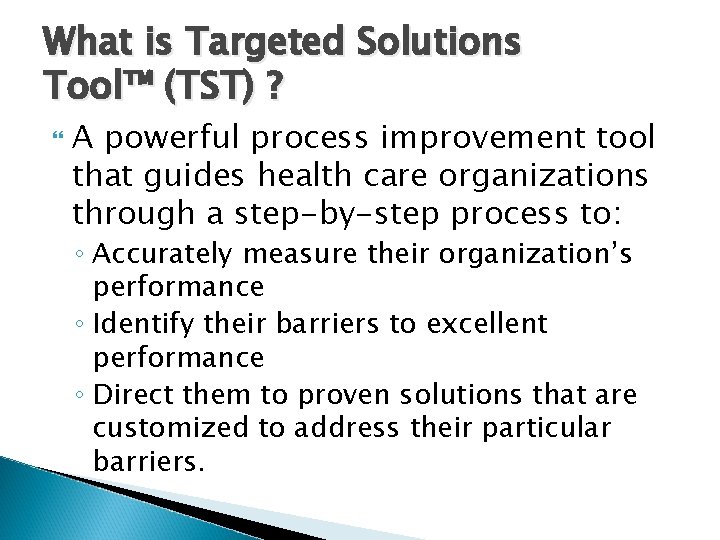
What is Targeted Solutions Tool™ (TST) ? A powerful process improvement tool that guides health care organizations through a step-by-step process to: ◦ Accurately measure their organization’s performance ◦ Identify their barriers to excellent performance ◦ Direct them to proven solutions that are customized to address their particular barriers.
Participating Hospitals Cedars-Sinai Cleveland Exempla Clinic Fairview Froedtert Intermountain Johns Hopkins Kaiser. Permanente Mayo Clinic Memorial Hermann NY-Presbyterian North Shore-LIJ Northwestern OSF Partners Health. Care Stanford Hospital Trinity Health Virtua Wake Forest Baptist
Effective HH is in our HANDS • • • Habit- as automatic as looking around before crossing the road… Gel in, Gel out Active Feedback- Coaching, Voice expectation to all staff, Engage staff, Frequent communication, Celebrate improvement No One is Excused- Protect the patients, Hold everyone accountable, Commitment, Role modeling, Apply progressive discipline from the top Data Driven Systems- Focus on the systems, not the individual.
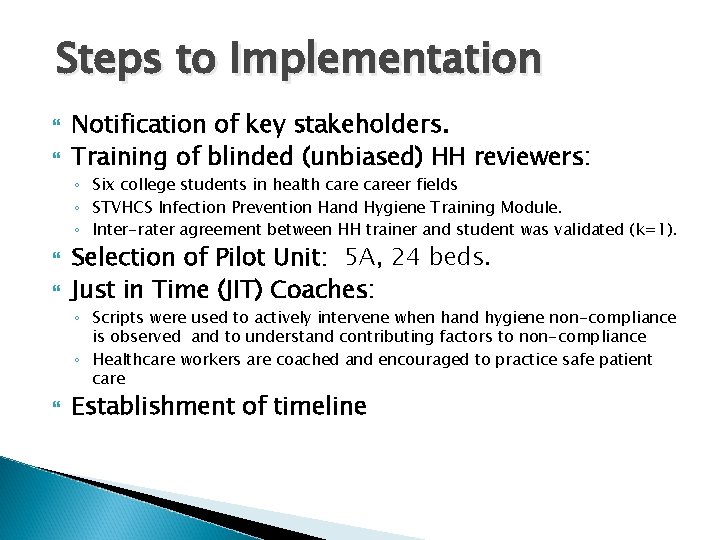
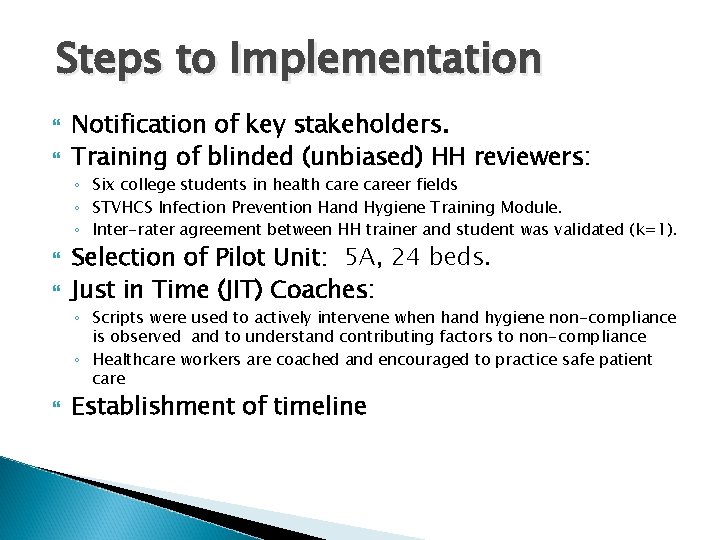
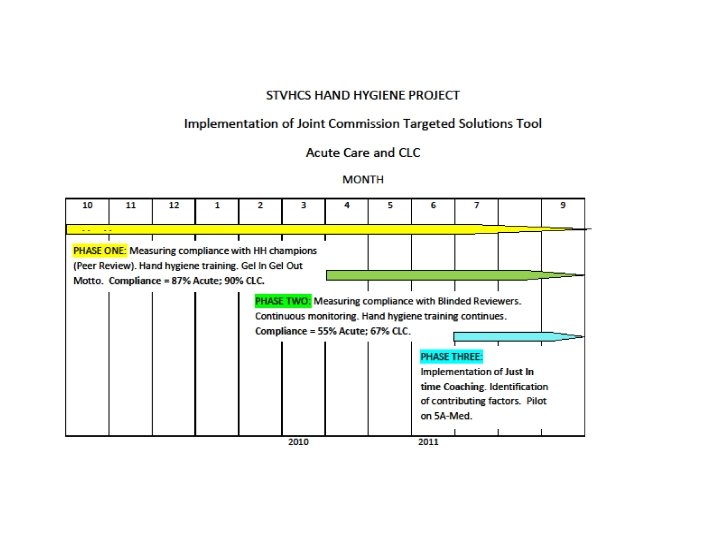
Steps to Implementation Notification of key stakeholders. Training of blinded (unbiased) HH reviewers: ◦ Six college students in health career fields ◦ STVHCS Infection Prevention Hand Hygiene Training Module. ◦ Inter-rater agreement between HH trainer and student was validated (k=1). Selection of Pilot Unit: 5 A, 24 beds. Just in Time (JIT) Coaches: ◦ Scripts were used to actively intervene when hand hygiene non-compliance is observed and to understand contributing factors to non-compliance ◦ Healthcare workers are coached and encouraged to practice safe patient care Establishment of timeline
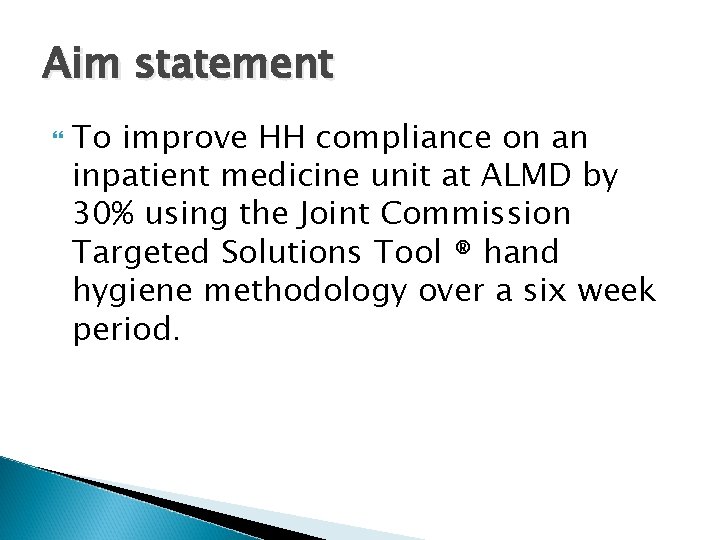
Aim statement To improve HH compliance on an inpatient medicine unit at ALMD by 30% using the Joint Commission Targeted Solutions Tool ® hand hygiene methodology over a six week period.
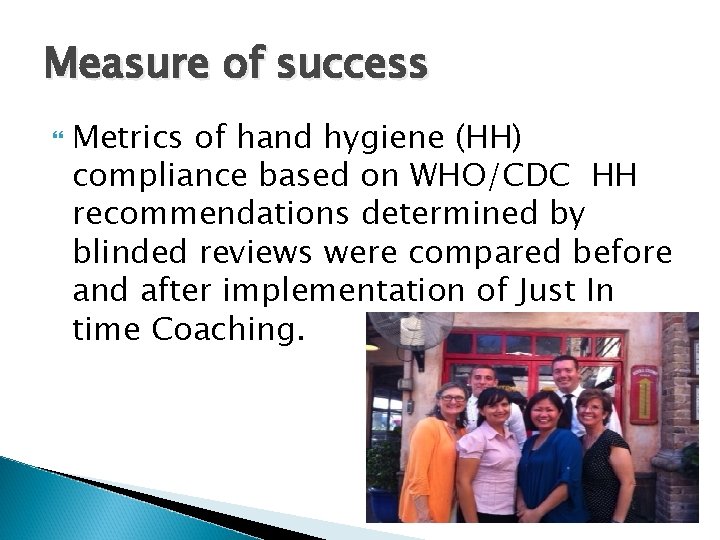
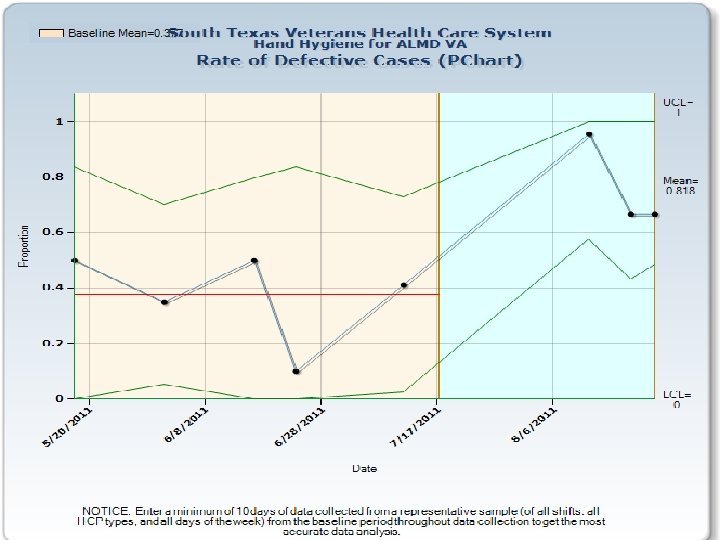
Measure of success Metrics of hand hygiene (HH) compliance based on WHO/CDC HH recommendations determined by blinded reviews were compared before and after implementation of Just In time Coaching.

Quality Improvement Tools and Results
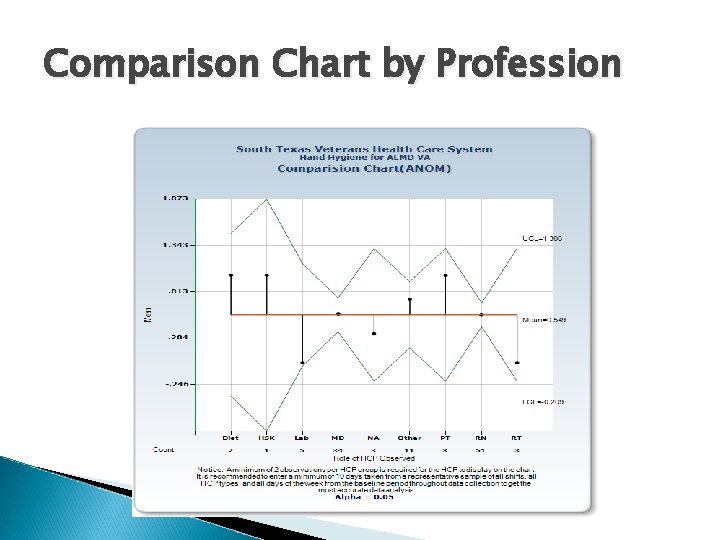
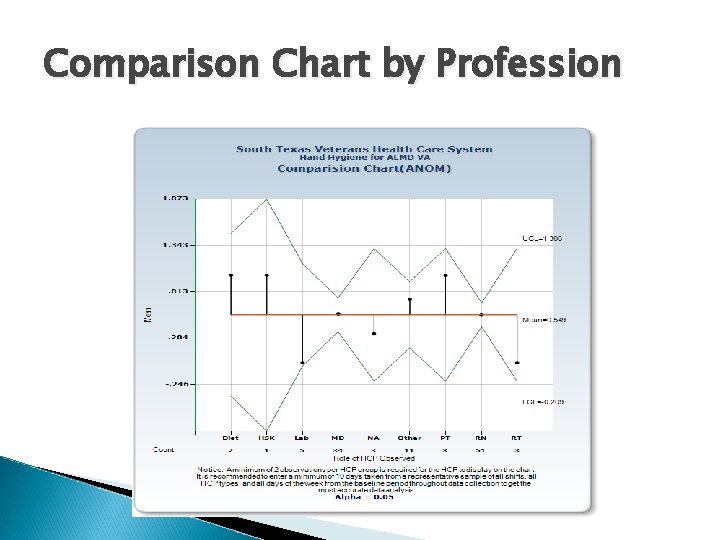
Comparison Chart by Profession
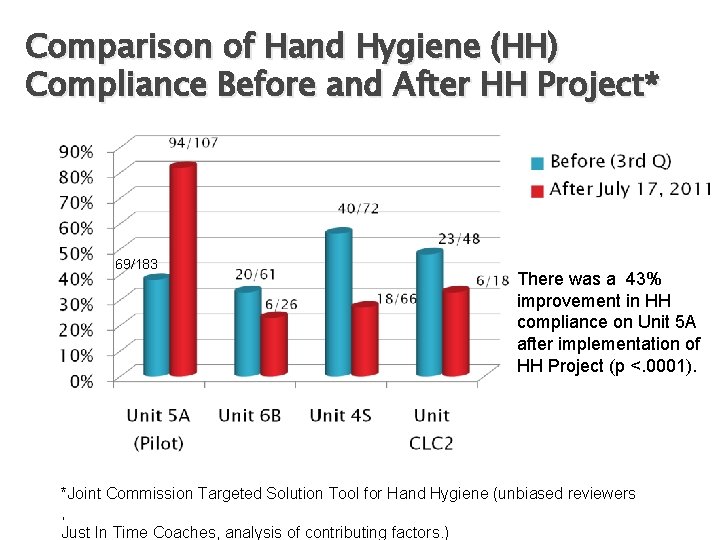
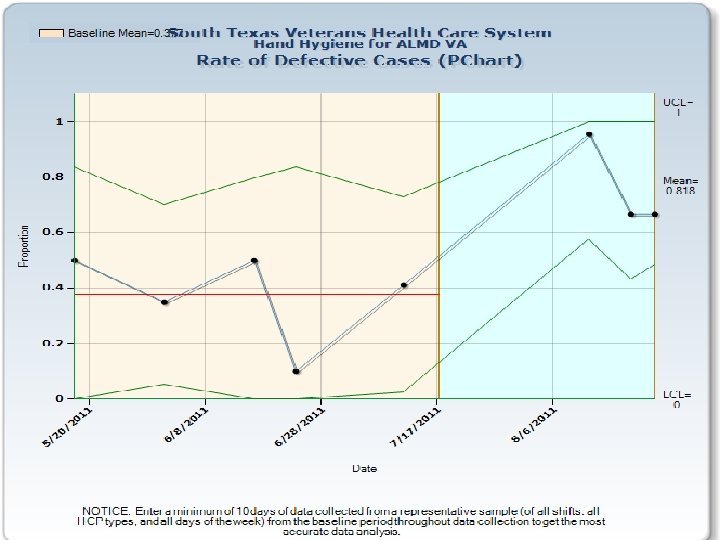
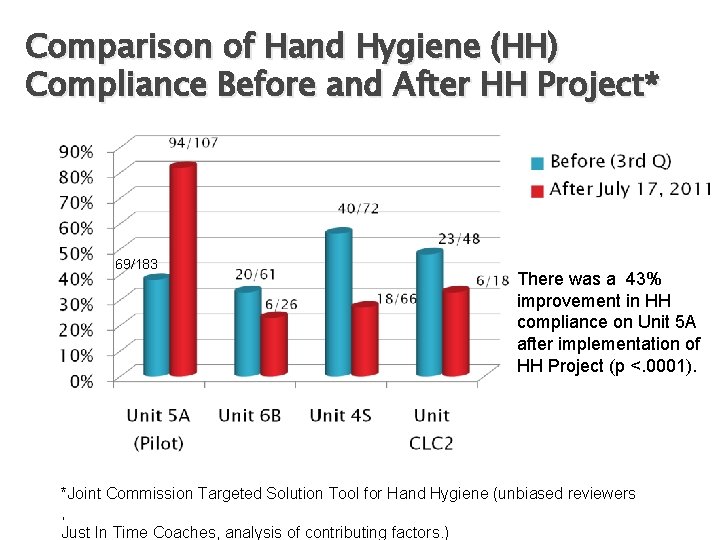
Comparison of Hand Hygiene (HH) Compliance Before and After HH Project* 69/183 There was a 43% improvement in HH compliance on Unit 5 A after implementation of HH Project (p <. 0001). *Joint Commission Targeted Solution Tool for Hand Hygiene (unbiased reviewers , Just In Time Coaches, analysis of contributing factors. )
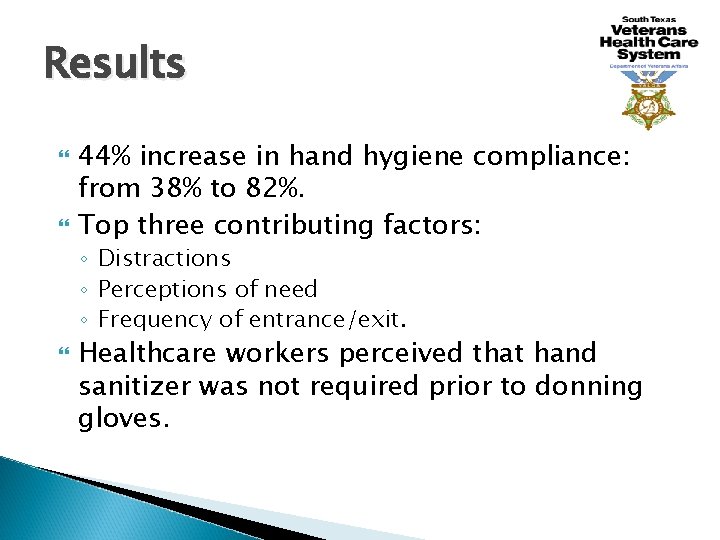
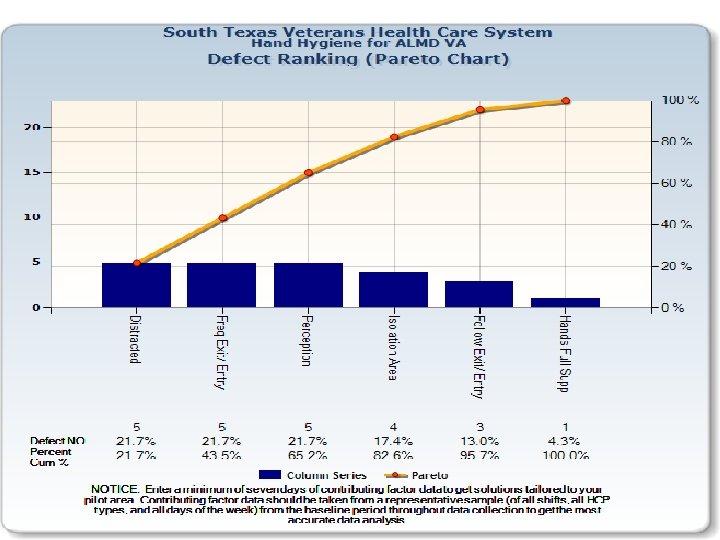
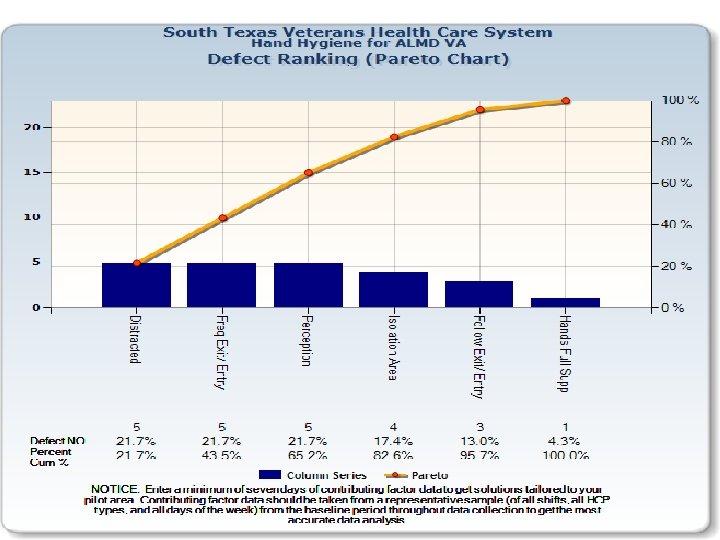
Results 44% increase in hand hygiene compliance: from 38% to 82%. Top three contributing factors: ◦ Distractions ◦ Perceptions of need ◦ Frequency of entrance/exit. Healthcare workers perceived that hand sanitizer was not required prior to donning gloves.
Cost Avoidance A 1% improvement in HH compliance = savings of approximately $39, 650 a year in a 200 bed hospital by mathematical modeling. Taking into account an increment of 43% in HH compliance, savings of $204, 504 a year in MRSA transmission prevention alone is projected. Cummings, Anderson, & Kaye, Infection Control and Hospital Epidemiol 2010; 31: 357 -364
Conclusions JIT coaching was associated with improvement in hand hygiene compliance. Distraction was the key contributing factor for noncompliance. Healthcare workers identified that they did not recognize hand hygiene was needed prior to donning gloves, a misperception.
Next steps The project will be extended to other acute care units, including surgery and hemodialysis. Solutions to contributing factors are being explored in greater depth. One solution that is being considered for implementation is a patient education program “It is okay to ask. ” to address factor of distraction.
References The Joint Commission’s Targeted Solutions Tool, Joint Commission Center for Transforming Health Care, retrieved 9/12/2011 http: //www. centerfortransforminghealthcare. org/service CDC. Guideline for Hand Hygiene in Health-Care Settings. MMWR 2002; 51: No. RR-16 Cummings, Anderson, & Kaye, Infection Control and Hospital Epidemiol 2010; 31: 357 -364 WHO Guidelines on Hand Hygiene in Healthcare, 2009. Available at: http: //whqlibdoc. who. int/publications/2009/9789241597906_eng. pdf Accessed 10/4/2011