UTILIZING THE AOK PROTOCOL A Novel Approach to
- Slides: 1
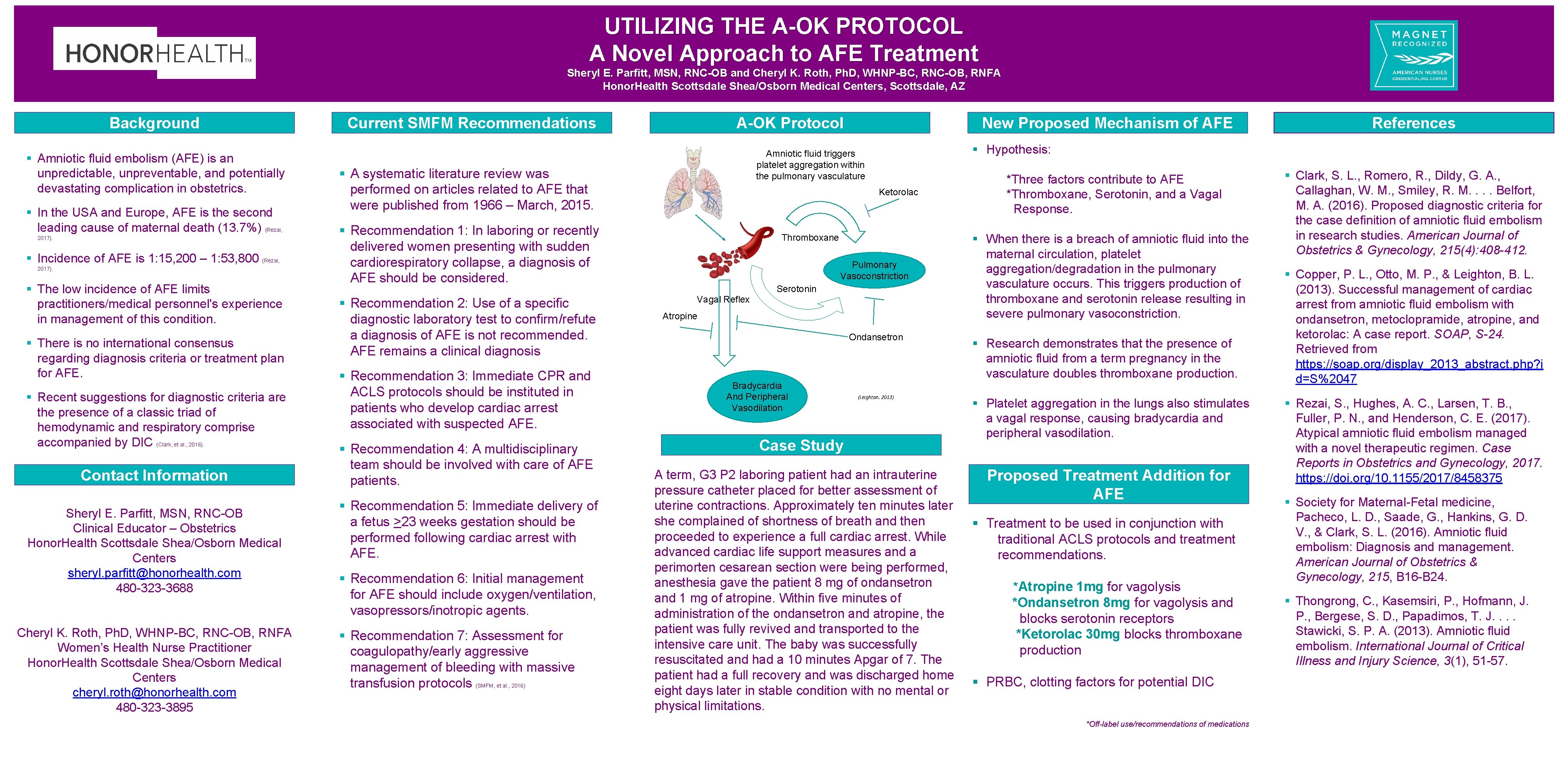
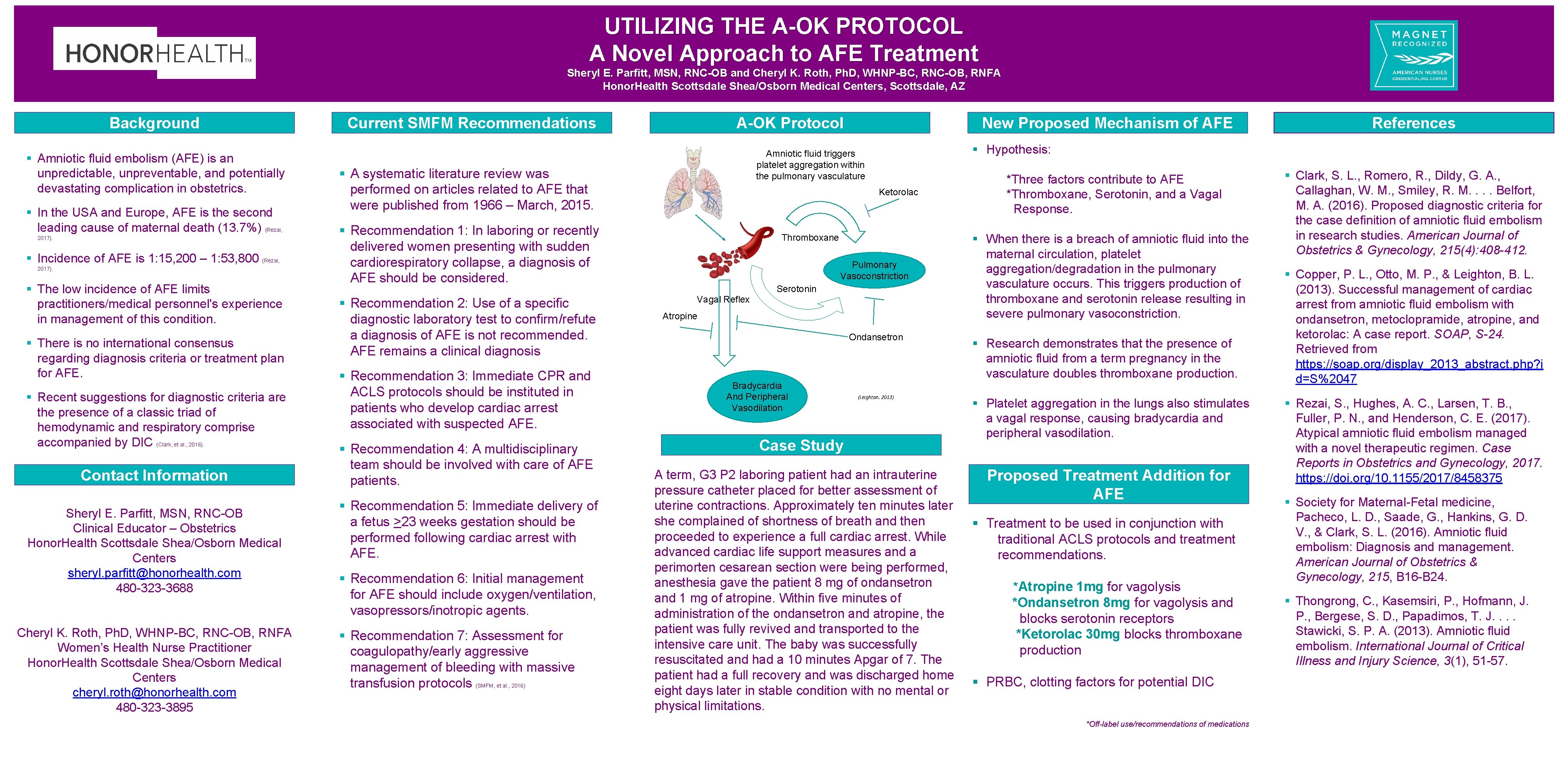
UTILIZING THE A-OK PROTOCOL A Novel Approach to AFE Treatment Sheryl E. Parfitt, MSN, RNC-OB and Cheryl K. Roth, Ph. D, WHNP-BC, RNC-OB, RNFA Honor. Health Scottsdale Shea/Osborn Medical Centers, Scottsdale, AZ Background § Amniotic fluid embolism (AFE) is an unpredictable, unpreventable, and potentially devastating complication in obstetrics. § In the USA and Europe, AFE is the second leading cause of maternal death (13. 7%) (Rezai, 2017). § Incidence of AFE is 1: 15, 200 – 1: 53, 800 (Rezai, 2017). § The low incidence of AFE limits practitioners/medical personnel's experience in management of this condition. § There is no international consensus regarding diagnosis criteria or treatment plan for AFE. § Recent suggestions for diagnostic criteria are the presence of a classic triad of hemodynamic and respiratory comprise accompanied by DIC (Clark, et al. , 2016). Contact Information Sheryl E. Parfitt, MSN, RNC-OB Clinical Educator – Obstetrics Honor. Health Scottsdale Shea/Osborn Medical Centers sheryl. parfitt@honorhealth. com 480 -323 -3688 Cheryl K. Roth, Ph. D, WHNP-BC, RNC-OB, RNFA Women’s Health Nurse Practitioner Honor. Health Scottsdale Shea/Osborn Medical Centers cheryl. roth@honorhealth. com 480 -323 -3895 Current SMFM Recommendations A-OK Protocol Ketorolac § Recommendation 1: In laboring or recently delivered women presenting with sudden cardiorespiratory collapse, a diagnosis of AFE should be considered. § Recommendation 3: Immediate CPR and ACLS protocols should be instituted in patients who develop cardiac arrest associated with suspected AFE. § Recommendation 4: A multidisciplinary team should be involved with care of AFE patients. § Recommendation 5: Immediate delivery of a fetus >23 weeks gestation should be performed following cardiac arrest with AFE. § Recommendation 6: Initial management for AFE should include oxygen/ventilation, vasopressors/inotropic agents. § Recommendation 7: Assessment for coagulopathy/early aggressive management of bleeding with massive transfusion protocols (SMFM, et al. , 2016) Thromboxane Pulmonary Vasoconstriction Serotonin Vagal Reflex Atropine Ondansetron Bradycardia And Peripheral Vasodilation References § Hypothesis: Amniotic fluid triggers platelet aggregation within the pulmonary vasculature § A systematic literature review was performed on articles related to AFE that were published from 1966 – March, 2015. § Recommendation 2: Use of a specific diagnostic laboratory test to confirm/refute a diagnosis of AFE is not recommended. AFE remains a clinical diagnosis New Proposed Mechanism of AFE (Leighton, 2013) Case Study A term, G 3 P 2 laboring patient had an intrauterine pressure catheter placed for better assessment of uterine contractions. Approximately ten minutes later she complained of shortness of breath and then proceeded to experience a full cardiac arrest. While advanced cardiac life support measures and a perimorten cesarean section were being performed, anesthesia gave the patient 8 mg of ondansetron and 1 mg of atropine. Within five minutes of administration of the ondansetron and atropine, the patient was fully revived and transported to the intensive care unit. The baby was successfully resuscitated and had a 10 minutes Apgar of 7. The patient had a full recovery and was discharged home eight days later in stable condition with no mental or physical limitations. *Three factors contribute to AFE *Thromboxane, Serotonin, and a Vagal Response. § When there is a breach of amniotic fluid into the maternal circulation, platelet aggregation/degradation in the pulmonary vasculature occurs. This triggers production of thromboxane and serotonin release resulting in severe pulmonary vasoconstriction. § Research demonstrates that the presence of amniotic fluid from a term pregnancy in the vasculature doubles thromboxane production. § Platelet aggregation in the lungs also stimulates a vagal response, causing bradycardia and peripheral vasodilation. Proposed Treatment Addition for AFE § Treatment to be used in conjunction with traditional ACLS protocols and treatment recommendations. *Atropine 1 mg for vagolysis *Ondansetron 8 mg for vagolysis and blocks serotonin receptors *Ketorolac 30 mg blocks thromboxane production § PRBC, clotting factors for potential DIC *Off-label use/recommendations of medications § Clark, S. L. , Romero, R. , Dildy, G. A. , Callaghan, W. M. , Smiley, R. M. . Belfort, M. A. (2016). Proposed diagnostic criteria for the case definition of amniotic fluid embolism in research studies. American Journal of Obstetrics & Gynecology, 215(4): 408 -412. § Copper, P. L. , Otto, M. P. , & Leighton, B. L. (2013). Successful management of cardiac arrest from amniotic fluid embolism with ondansetron, metoclopramide, atropine, and ketorolac: A case report. SOAP, S-24. Retrieved from https: //soap. org/display_2013_abstract. php? i d=S%2047 § Rezai, S. , Hughes, A. C. , Larsen, T. B. , Fuller, P. N. , and Henderson, C. E. (2017). Atypical amniotic fluid embolism managed with a novel therapeutic regimen. Case Reports in Obstetrics and Gynecology, 2017. https: //doi. org/10. 1155/2017/8458375 § Society for Maternal-Fetal medicine, Pacheco, L. D. , Saade, G. , Hankins, G. D. V. , & Clark, S. L. (2016). Amniotic fluid embolism: Diagnosis and management. American Journal of Obstetrics & Gynecology, 215, B 16 -B 24. § Thongrong, C. , Kasemsiri, P. , Hofmann, J. P. , Bergese, S. D. , Papadimos, T. J. . Stawicki, S. P. A. (2013). Amniotic fluid embolism. International Journal of Critical Illness and Injury Science, 3(1), 51 -57.