Uterine Fibroids Nour ELETREBY MD Associate Professor Gynecologic
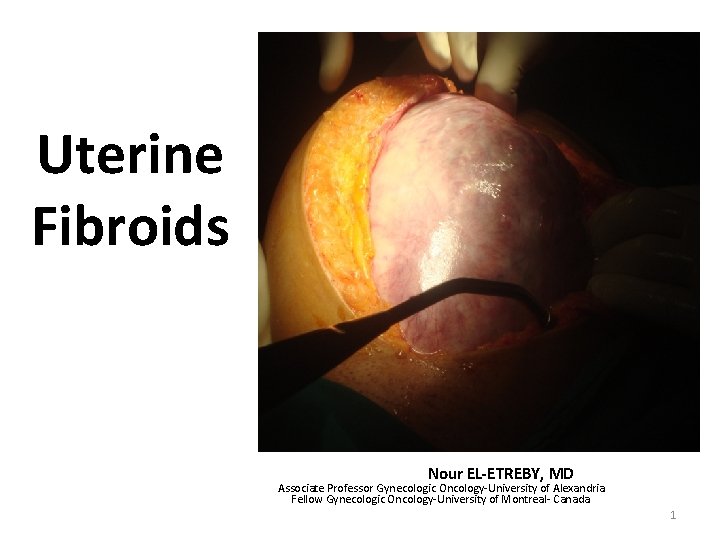
Uterine Fibroids Nour EL-ETREBY, MD Associate Professor Gynecologic Oncology-University of Alexandria Fellow Gynecologic Oncology-University of Montreal- Canada 1
Epidemiology • Fibroids (Myoma, Leiomyoma, Fibromyoma) • Most common Benign tumor of female reproductive system, arising in the smooth muscle cells of myometrium. • Contain large aggregation of extracellular matrix consisting of collagen, elastin, fibronectin and proteoglycan. 2
Epidemiology • Reproductive age group (late 20’s to mid 40’s). • 20%- 30% of women in their reproductive age are reported to have fibroids. • 77% of hysterectomy specimens were having fibroids of variable site, size and number. • White women have lower prevalence, more common in dark races. 3
Etiology • Precise cause of fibroids is not known. • Advances have been made in understanding the molecular biology of these benign tumors and there dependence on genetic, hormonal and growth factors. 4
Etiology Genetic • Fibroids are monoclonal and about 40% have chromosomal abnormalities, yet 60% have undetected mutations. (a) (b) (c) translocations between chromosomes 12 and 14 deletions of chromosome 7 Trisomy of chromosome 12 in large tumors • More than 100 genes were found to be up- down regulated in fibroid cells. Many of them appear to regulate cell growth, proliferation and differentiation. • Genetic differences between fibroid and leiomyosarcoma indicate that leiomyosarcomas do not result due to malignant changes in fibroids. 5
Etiology Hormonal • Both increase in number and responsiveness of estrogen receptors appear to promote fibroid growth, as these tumors are rarely found before puberty, develop and increase during reproductive life and regress after menopause. • Found more with hyperestrogenic states like obesity, ERT, endometriosis, endometrial hyperplasia and endometrial cancer. Also common with nulliparity and anovulatory infertility. • Decreased incidence are found in athletes with low body mass and in women with high parity. 6
Etiology Growth Factor • Growth factors are proteins polypeptides produced locally by smooth muscle cells and fibroblasts, appear to promote growth of fibroids primarily by increasing extracellular matrix. • Many growth factors are participating in proliferation and growth of fibroid Tumor Growth Factor-Beta, Basic- Fibroblast Growth Factor, Epidermal Growth factor, Platelet Derived Growth Factor, Insulin like growth factor, Vascular endothelial factor … etc 7
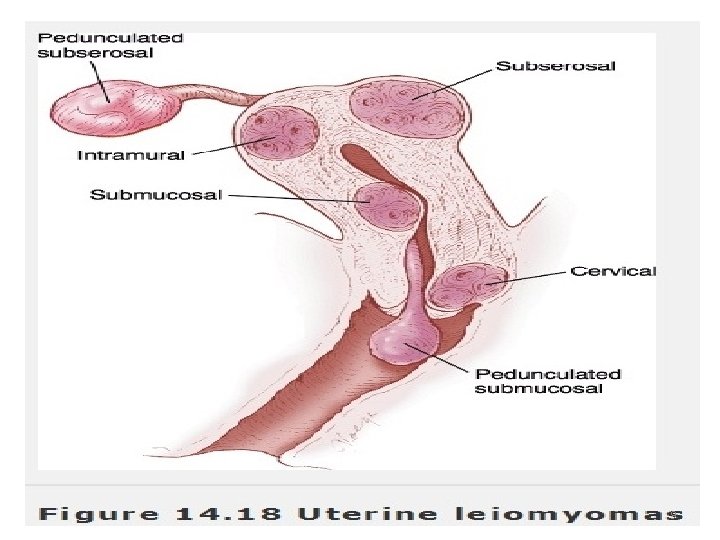
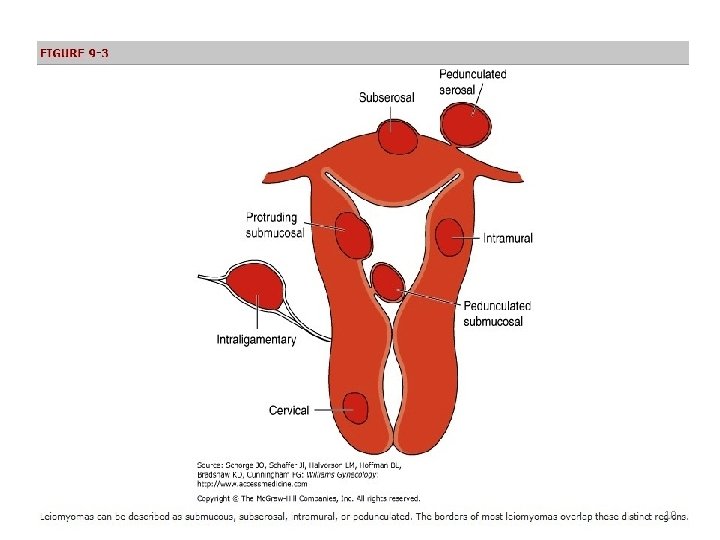
Types or Sites • Uterine body (95%) Intramural or interstitial 70% Submucous 15% (sessile/ pedunculated) Subserous 10% ( sessile/ pedunculated) • Cervical (4%). • Ligamentary (1%) (broad ligament fibroids). 8
9
10
Rare types • Parasitic leiomyomas. • Intravenous leiomyomatosis. • Leiomyomatosis peritonealis disseminata. 11
Pathology Gross • Well defined capsulated, firm, rubbery with a pseudo-capsule. Cut surface is pinkish white and has a whorled appearance. • Capsule consists of connective tissue which fixes tumor with myometrium. • Blood vessels supplying the tumor lie in capsule and send radial branch to tumor hence central part of tumor is comparatively less vascular, thereby degenerative changes are noted in the center while calcification at the periphery and spreads inwards along the vessels (Tombstone). Microscopic Tumor consists of bundles of plane cells, separated by varying amount of fibrous strands. Areas of embryonic muscle tissue may be present. 12

13
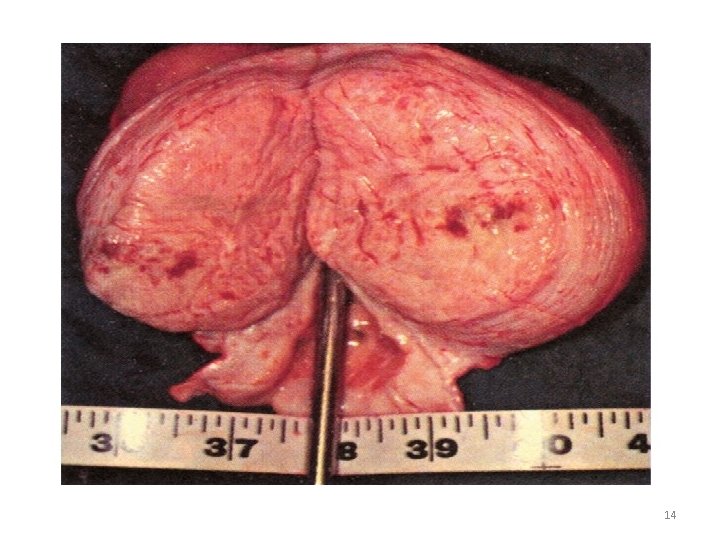
14
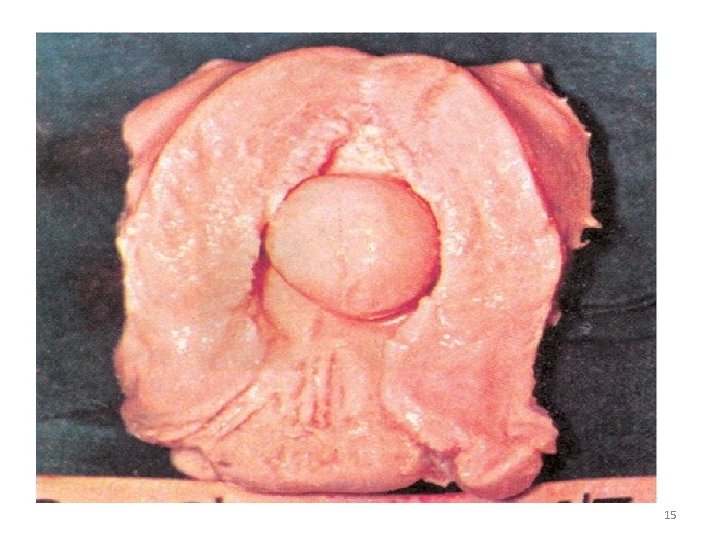
15
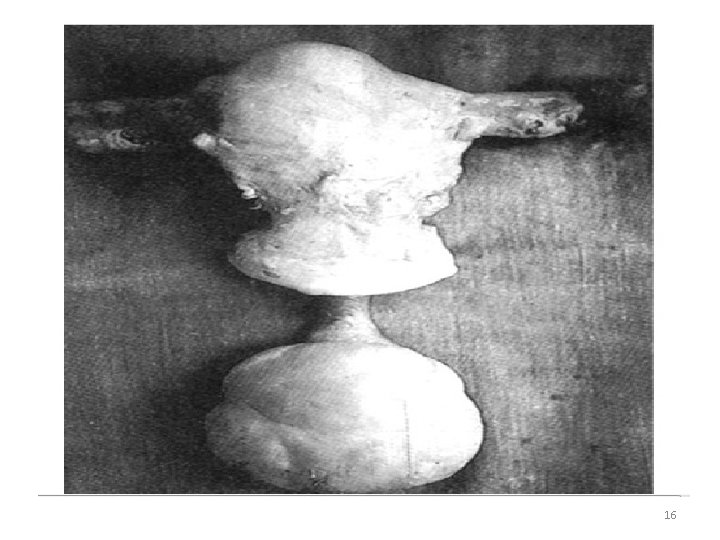
16
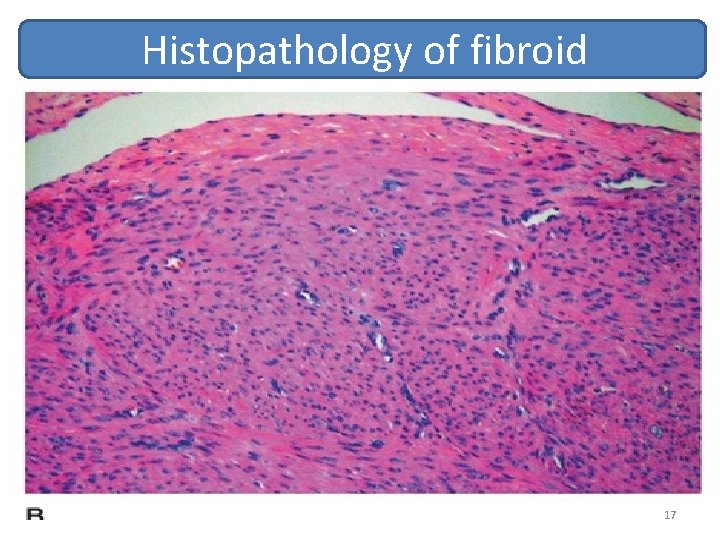
Histopathology of fibroid 17
Symptoms • Asymptomatic Fibroid size <4 cm / uterine size <12 cm (50%) • Abnormal uterine bleeding menorrhagia > 64% woman present with heavy blood loss. Metro menorrhagia present in cases of infected / ulcerated fibroid polyp. • Infertility tubal, cervical, RVF • Pain Dysmenorrhoea, slight discomfort to colicky pain in suprapubic region, low backache. Degenerated / torsion of fibroid may cause an acute abdomen. • Urinary symptoms Increased uterine volume due to fibroids may cause pressure and obstructive effect on urinary tract (frequency, nocturia, urgency, UTI ) • Secondary symptoms progressive anaemia due to chronic blood loss, CHF, loss of appetite and work capacity. • Some patients rarely develop polycythemia due to erythropoiten production. • Abdominal Lump. 18
Natural History of Fibroids • Most fibroid grow slowly 9% growth rate over 12 months, more depending on growth factors rather than hormones. • Growth rate decreases after age 35 yrs in white women, but not in blacks. • Most of them regress with onset of menopause. • Rapid uterine fibroid growth in premenopausal age almost never indicate sarcomatous change. • 0. 5% women with pre-exisiting fibroid may develop pain and bleeding in their postmenopausal age, as their fibroid might have under gone sarcomatous changes. • Fibroids may become calcified in menopausal women. • Fibroids may develop variety of degenerative changes. 19
Degenerative Changes • • Hyaline degeneration Cystic degeneration Fatty degeneration Red degeneration (Aseptic Necrobiosis) in pregnancy, postpartum Calcification (calcareous degeneration) Hemorrhage, torsion Sarcomatous changes < 0. 5% Infection/ulceration of pedunculated fibroid 20
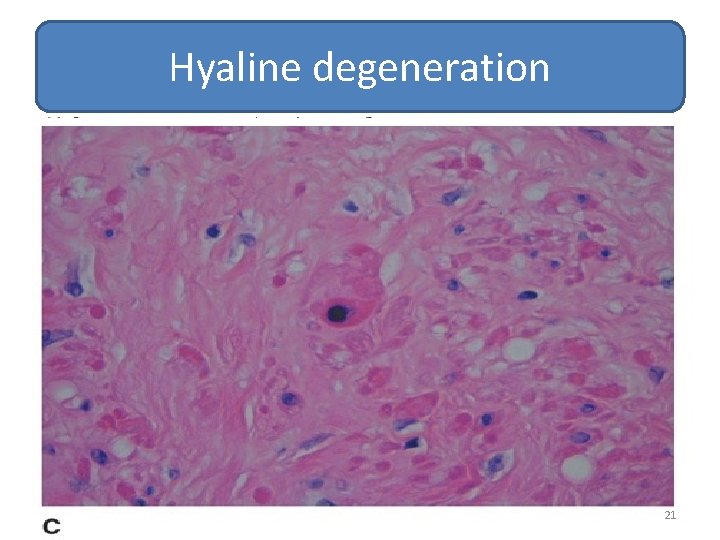
Hyaline degeneration 21
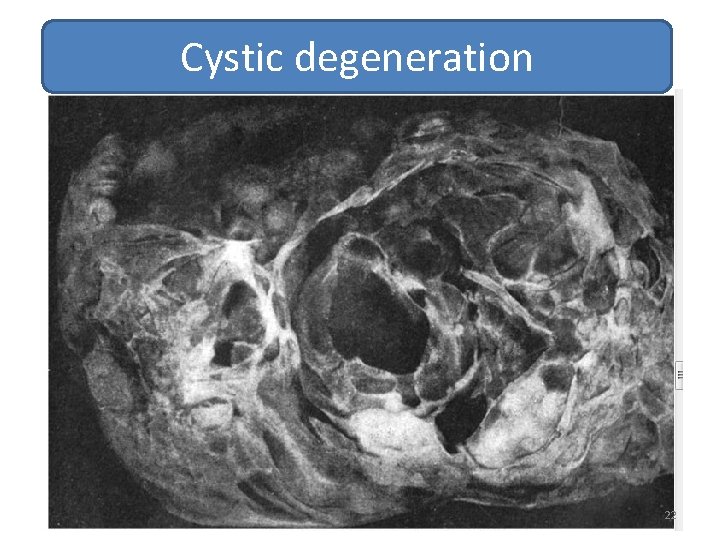
Cystic degeneration 22
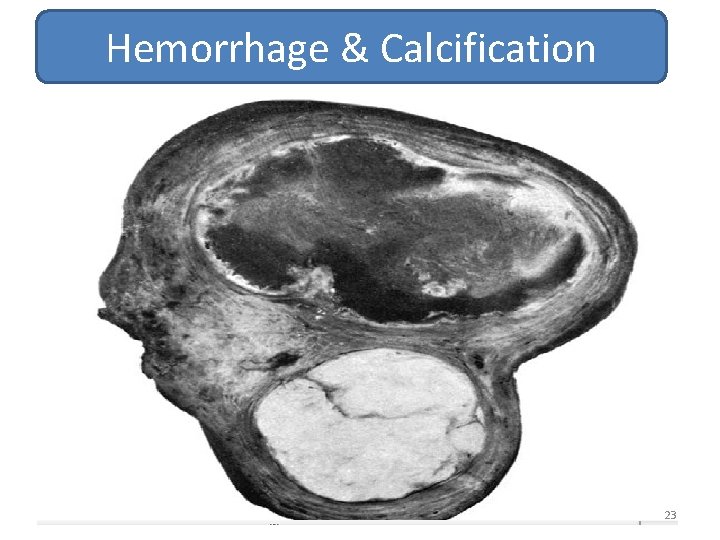
Hemorrhage & Calcification 23
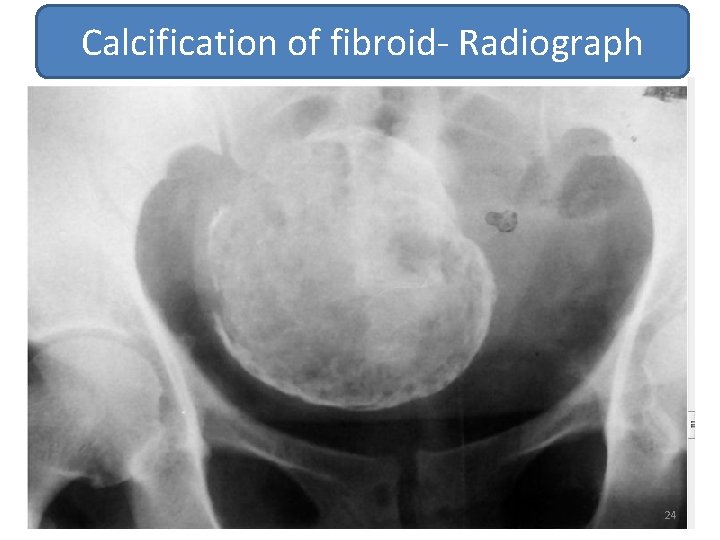
Calcification of fibroid- Radiograph 24
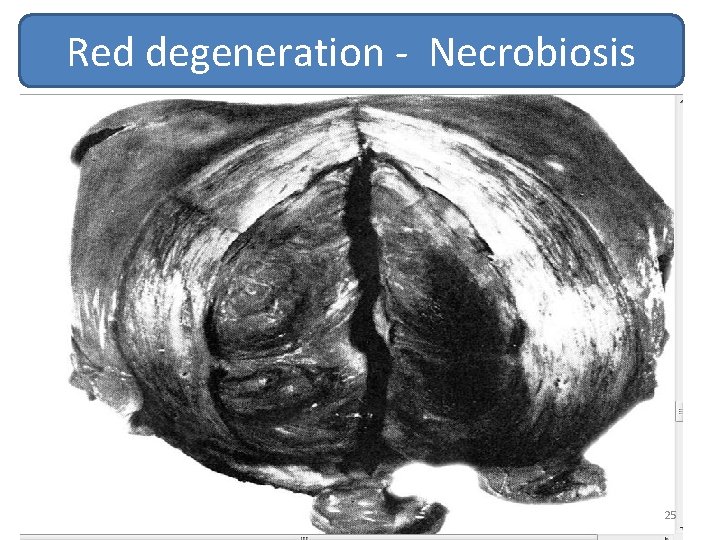
Red degeneration - Necrobiosis 25
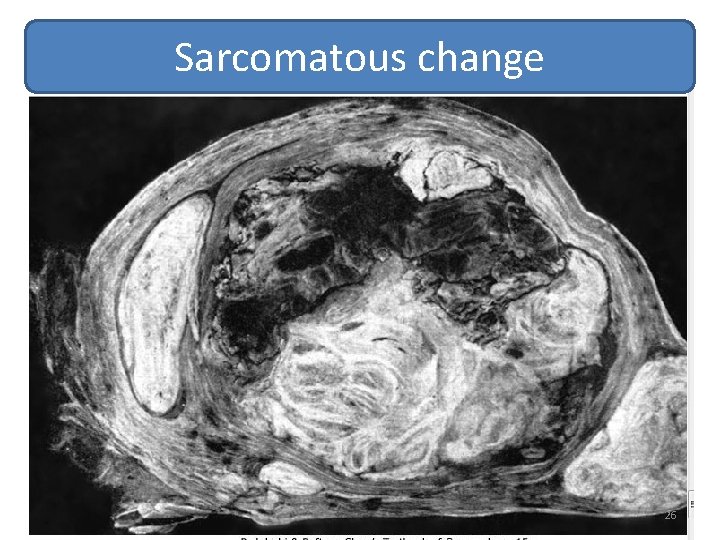
Sarcomatous change 26
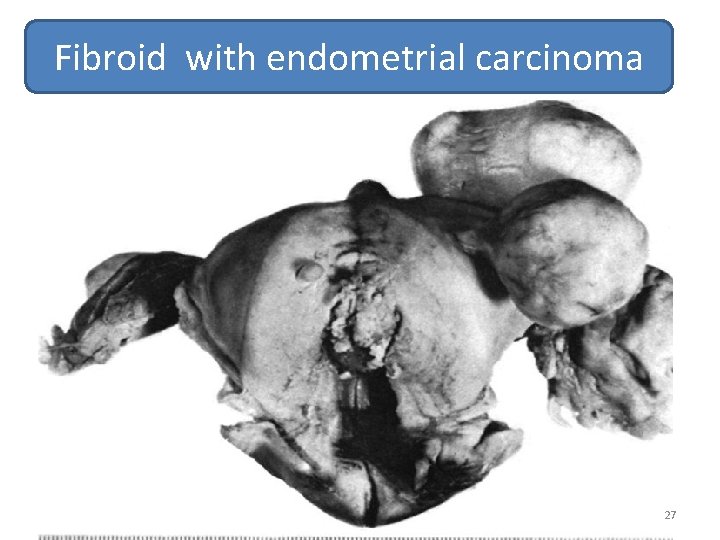
Fibroid with endometrial carcinoma 27
Diagnosis • Fibroid with uterus larger than 12 -14 wks of gestation are well palpable per abdomen. Surface is irregular, nodular, bossed, firm. • Enlarged uterus may be as big as term pregnancy. No Braxton Hick contractions, no palpable fetal parts or movements and no fetal heart sound. Uterine souffle due to increased blood supply to uterus may be audible, it has to be differentiated from umbilical souffle. 28
Diagnosis Pelvic Examination • Enlarged uterus due to fibroids is of variable size, irregular surface, nodular or bossed. • Associated cystic enlargement of ovary may be noted. • Enlarged uterus is firm and non-tender, freely mobile—up and down, side to side till it incarcerates in pelvis. • Uterus and cervix move together. 29
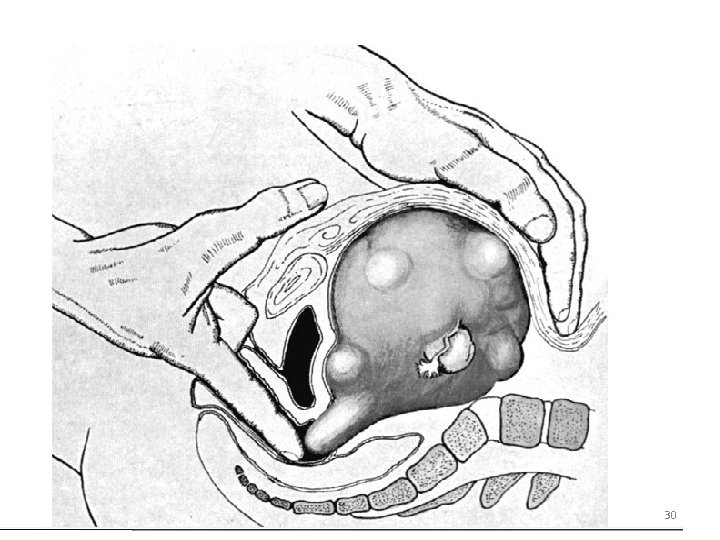
30
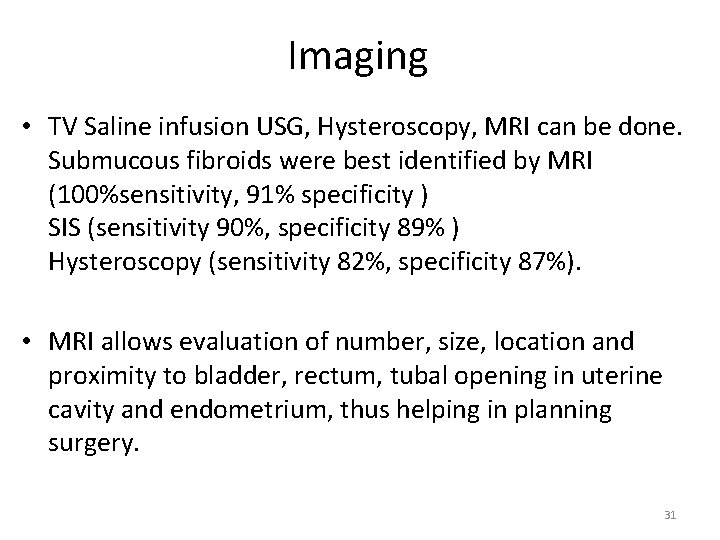
Imaging • TV Saline infusion USG, Hysteroscopy, MRI can be done. Submucous fibroids were best identified by MRI (100%sensitivity, 91% specificity ) SIS (sensitivity 90%, specificity 89% ) Hysteroscopy (sensitivity 82%, specificity 87%). • MRI allows evaluation of number, size, location and proximity to bladder, rectum, tubal opening in uterine cavity and endometrium, thus helping in planning surgery. 31
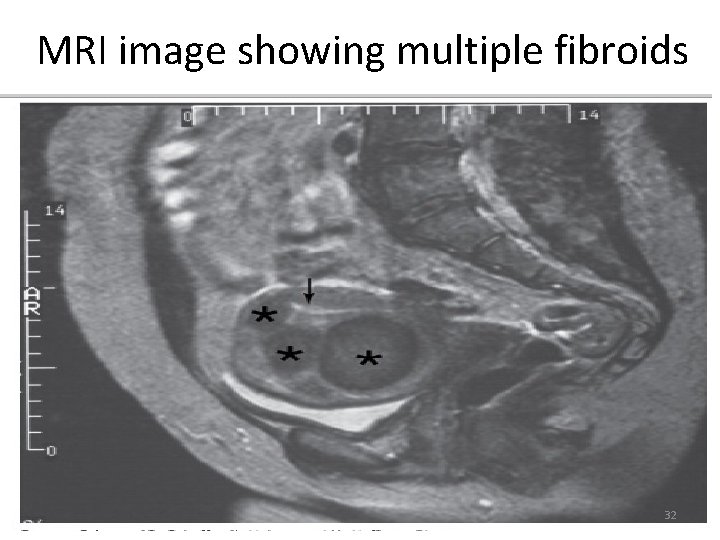
MRI image showing multiple fibroids 32
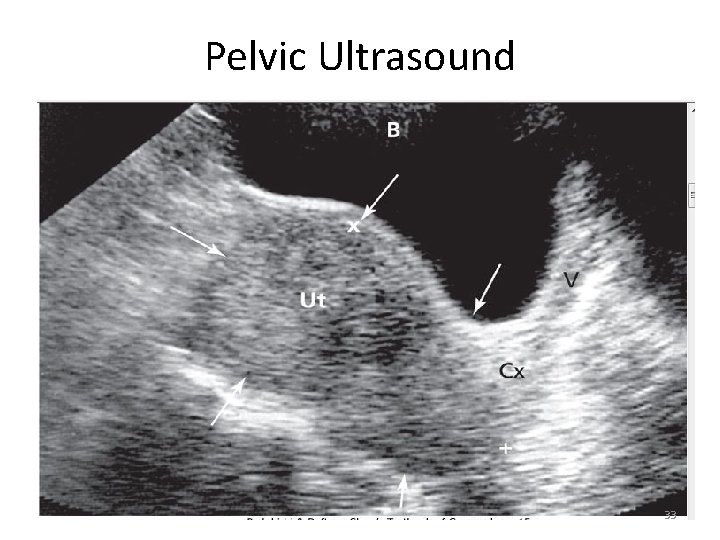
Pelvic Ultrasound 33
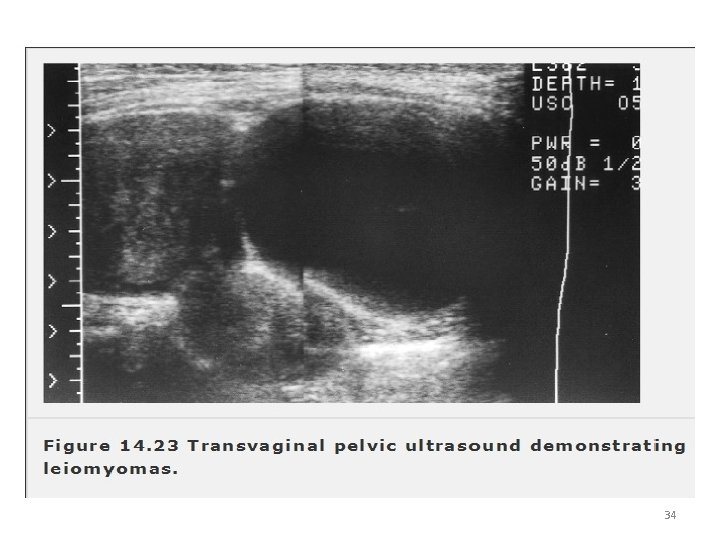
34

USG Image 35
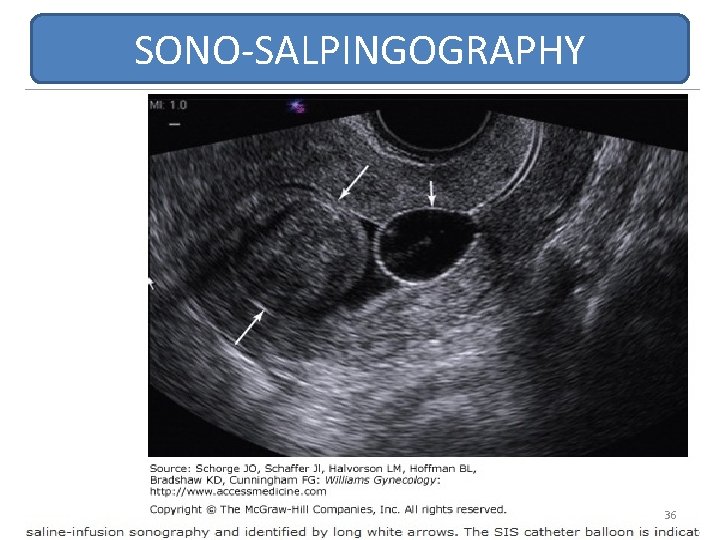
SONO-SALPINGOGRAPHY 36
Fertility and Fibroids • Presence of submucous fibroids decrease fertility and removing them increases fertility. • Subserous and intramural fibroid do not affect fertility but their removal may increase fertility depending on their location. • Myomectomy carries risk of anesthesia, surgery , infection, post- operative adhesions, likelihood of increased cesarean delivery, rupture of myomectomy scar, expanse of surgeries and time for recovery. • Therefore unless subserous, intramural fibroids are surely found to be the prime cause of infertility and repeated abortion, myomectomy is not advised. 37
Fibroid and Pregnancy Prevalence of fibroids in pregnancy is 18% based on 1 st trimester USG • Most of fibroids do not increase significantly in pregnancy. • Red degeneration of fibroids occurs in 5% cases. Patient develops pain, fever, local tenderness of fibroid, increased TLC and DLC, high ESR. Bed rest, analgesics and plenty of fluids are needed to treat them. Influence of fibroids on pregnancy Abortions , Malpresentation, malposition, IUGR, PROM, Premature onset of labour pains, uterine inertia, incoordinated uterine action, prolonged labor, obstructed labor due to cervical fibroid or incarcerated fibroid, APH (abruptio, placenta praevia), Atonic PPH, P Sepsis, inversion of uterus, sub involution of uterus. Rupture of Myomectomy scar. Fetal injury attributed to mechanical compression by fibroid(0. 2%) 38
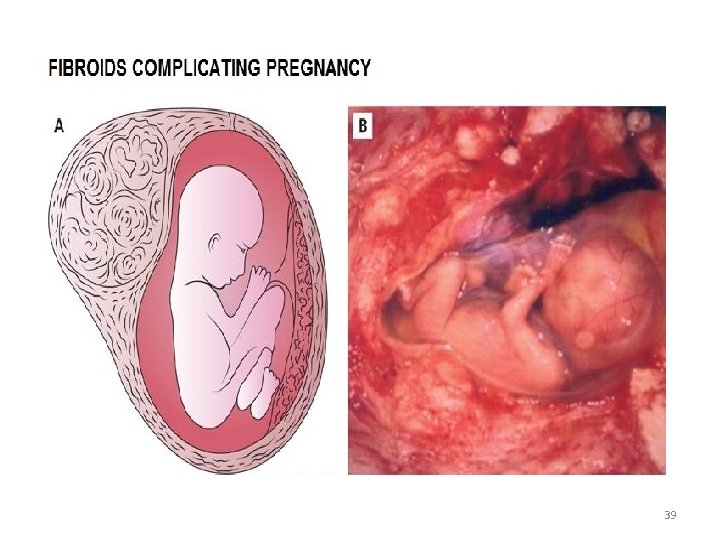
39
Differential Diagnosis • Pregnancy/pregnancy complications/ fibroid with pregnancy. • Full Bladder. • Haematometra/Pyometra • Adenomyosis • Bicornuate Uterus • Chronic Ectopic Pregnancy • Ovarian Chocolate cyst • Endometrial Carcinoma/uterine sarcoma • Ovarian Neoplasms/para- ovarian Cysts. • Pelvic Kidney. 40
Treatment • Watchful Waiting • Medical Therapy NSAID, Gn. RH- Agonists. Gn. RHAntagonist, Alternative therapy. • Surgical Treatment options (a)Myomectomy (b) Hysterectomy • Uterine Artery Embolization (UAE). • New modalities. 41
Watchful Waiting Not having treatment for fibroids rarely results in harm, except women with severe anemia from fibroid related menorrhagia or hydronephrosis from ureteric obstruction caused by massive fibroid pressing over. Therefore, for women who are asymptomatic or having mild to moderate discomfort with fibroids, watch full may allow treatment to be deferred, perhaps indefinitely. A woman approaching menopause, watchful waiting may be considered, because there is limited time to develop new symptoms and after menopause fibroids usually decrease in size. 42
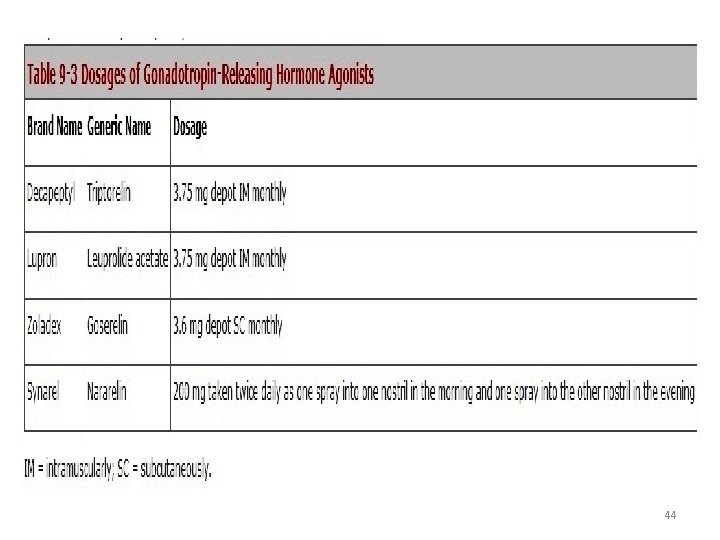
Medical Therapy Non steroidal Anti inflammatory drugs NSAIDS found to have minimal or no effect in controlling menorrhagia due to fibroids and no decrease in size of fibroids. Gn. RH Agonist Treatment with Gn. Rh Agonist decrease uterine volume, fibroid volume and bleeding. Monthly Gn. RH Agonist given for 6 months reduced fibroid volume by 30% and total uterine volume by 35%, bleeding also decreased well. Following discontinuation of Gn. RH –A , uterine volume and menses returns with in 4 --8 weeks, 2/3 rd women remained asymptomatic for 8 -12 months. 95% women developed side effects of hypo estrogen--iatrogenic menopuase and osteoporosis. Add back therapy given concurrently reduces these side effects. Gn. RH-A is recommended as temporary treatment for premenopausal women with heavy menorrhagia. 43
44
Medical Treatment Gn. RH –Antagonist Immediate suppression of endogenous Gn. Rh by daily SC injection 0 f Ganirelix results in 30% reduction in fibroid volume within 3 wks. Patient develops Hypo estrogenic symptoms. Availability of long acting compounds might be considered for medical treatment prior to surgery. 45
Medical Treatment Progesterone releasing IUCD Mirena. Levonorgestrel releasing IUCD may be a reasonable treatment for selected women of child bearing age with fibroid associated menorrhagia and interested to have contraception. 85% of such women returned to their normal bleeding within 3 months and 40% developed reversible amenorrhea at the end of 1. 5 -2 years. 46
Surgical Treatment • Myomectomy Laparotomy , Vaginal polypectomy, Laparoscopy (morcellation), Hysteroscopy. • Hysterectomy Abdominal, Vaginal, laparoscopic. 47
48
Preoperative management • Anemia can be rapidly corrected by recombinant forms erythropoietin alpha or epoetin 250 iu/kg weekly for 3 weeks and parentral iron therapy along with folic acid, vitamin C, protein supplementation. • Auto transfusion / donor blood transfusion • Control of bleeding Gn. RH agonist therapy • Control of associated medical problems like hypertension, CHF, Asthma, UTI, kidney or liver illness. 49
Myomectomy • Safe alternate to hysterectomy for young women who even have large fibroid and want to retain their fertility. • “The restoration and maintenance of physiological function is or should be the ultimate goal of surgery Victor Bonney -1931” • In carefully selected women myomectomy may be safely accomplished at the time of LSCS by experienced surgeon instead of caesarean hysterectomy. 50
Myomectomy Indications • Infertility caused by cornual fibroid blocking tube. • Habitual abortion due to sub mucous fibroid. • Pedunculated fibroid likely to undergo torsion. • Fibroid > 12 weeks. • Broad ligament fibroid pressing on ureter. • Fibroid pressing over bladder causing retention of urine / infection. • Rapidly growing uterine fibroid in post menopausal women. 51
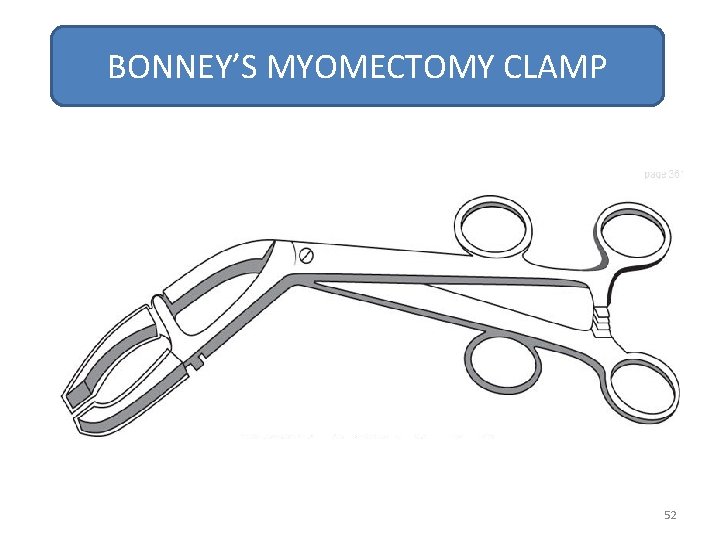
BONNEY’S MYOMECTOMY CLAMP 52
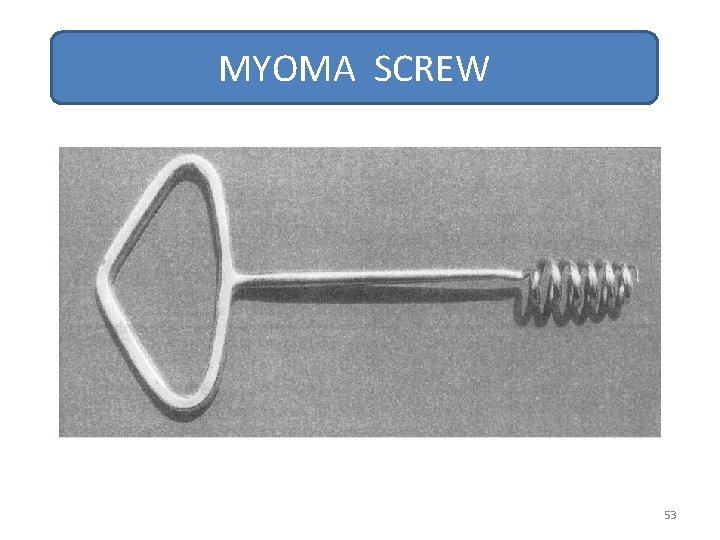
MYOMA SCREW 53
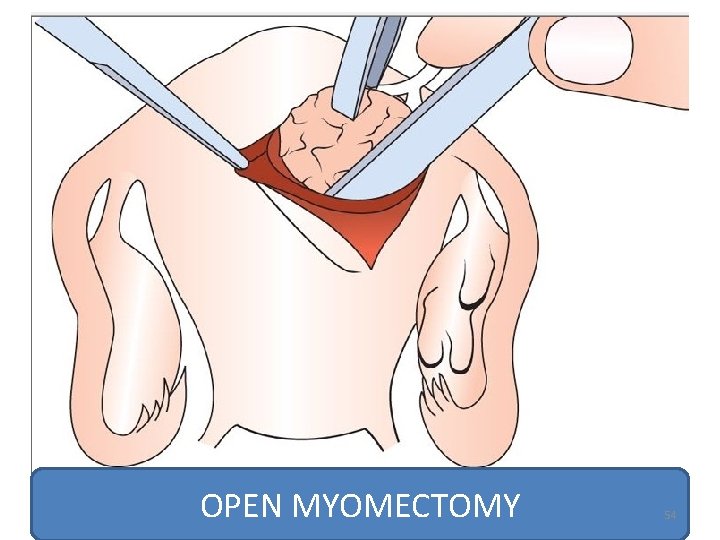
OPEN MYOMECTOMY 54
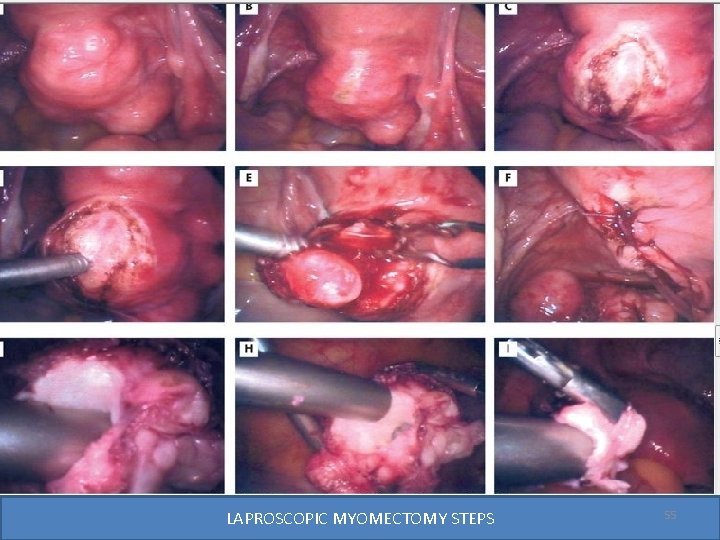
LAPROSCOPIC MYOMECTOMY STEPS 55
Disadvantages of laparoscopic Myomectomy • More hemorrhage because of no applicability of myomectomy clamp / tourniquet. • Longer duration of operation—longer anesthesia. • More chances of post operative adhesions – infertility, chronic abdominal pain, intestinal obstruction. • Increased incidence of scar rupture in pregnancy/ labour due to imperfect or inadequate suturing. • Laparoscopic myomectomy may not be safer for infertile women. • Unidentified or not removed small fibroid may grow later & show up as recurrence. 56
Hysteroscopic Myomectomy • Submucous fibroid < 1/3 rd buried in myometrium to avoid uterine perforation. • It can be excised either by electric cautery , laser or resectoscope. • It is best done under laparoscopic guidance to avoid myometrial perforation. 57
Complications of Myomectomy • • • Primary, reactionary or secondary hemorrhage. Trauma to urinary tract, gut. Infection. Adhesions. Intestinal obstruction. Recurrence of fibroid or menorrhagia. 58
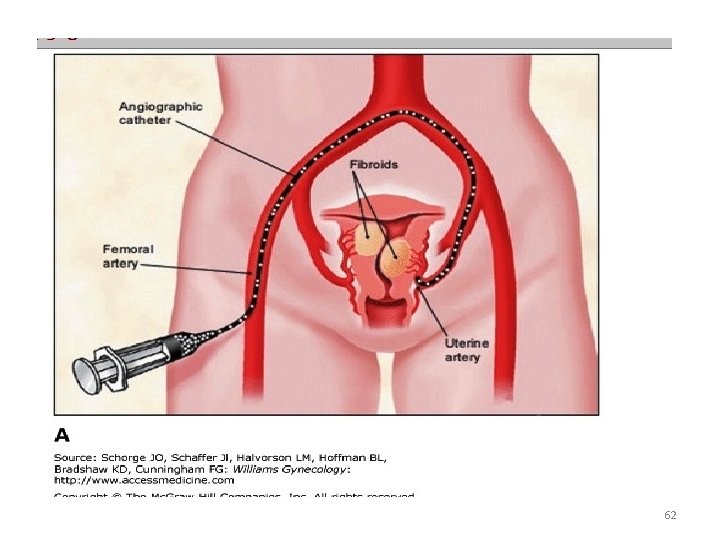
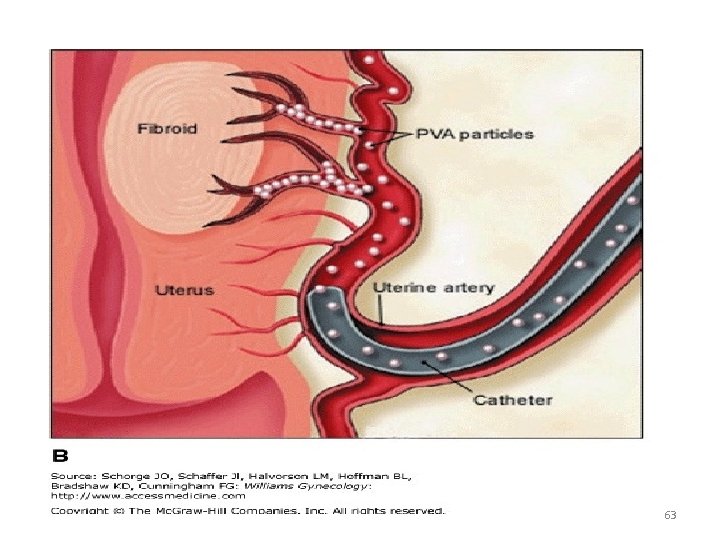
Uterine Artery Embolization(UAE) • Ravina (1991) first performed it to reduce blood supply to fibroid, results in reduction in size, further growth of fibroid reduced and minimum menstrual blood loss. • Menorrhagia reduced in 80 -90 % , pressure symptoms in 40 -70% and volume decreased by 50% at the end of 3 months. Contra indications Subserous and pedunculated fibroid necrosis and fall of tumor in peritoneal cavity. Very big fibroid are not suitable, submucous fibroid is not cured. It does not help the infertile women rather it may increase the problem. Technique under LA bilateral UAE approach through percutaneous femoral catheterization, using poly vinyl alcohol gel (PVA gel) particles are injected in the artery supplying the fibroid. 59
Results and complications of UAE • Vascularity and size reduced by 40% at 6 weeks and 75% at the end of 1 year. • Symptoms are relieved in 70% women. Post operative complications fever and infection, vaginal discharge and bleeding , unbearable ischemic pain, pulmonary embolism, premature ovarian failure if accidental occlusion of ovarian vessels occur, fertility rate is reduced due to adhesions, failure due to incomplete coagulation caused by arterial spasm or tortuosity of blood vessel. 60
Advantages of UAE • • • No major surgery. No intra-operative bleeding. Short hospital stay. No abdominal adhesions. 75 -80% women suffering from menorrhagia are satisfied. 61
62
63
Hysterectomy Indications Women over 40 years of age , multiparous women, complicated fibroids, unforeseen difficulties during myomectomy. Types of Hysterectomy Abdominal (total, sub total). Laparoscopic. Vaginal Hysterectomy. LAVH. 64
New techniques • MRI guided per cutaneous laser ablation. • High Intensity focused Ultrasound (HIFU) has been recently attempted –results are awaited. • Laparoscopic myolysis optimal surgery in multiparous women by using Nd : YAG laser, cryoprobe or diathermy to coagulate subserous fibroid. The contraindication are similar to UAE. 65
Conclusions • Fibroids are the most common benign tumor of female genital system. • Majority are Asymptomatic. • Different site and size, gives different presentations. • Liable to complications or degenerations. • Different modalities of treatment. 66
- Slides: 66