Using The Accountability Shared Model To Support Connected
Using The Accountability Shared Model To Support Connected Care Rima Gibbings and Nilmini Wickramasinghe
Agenda Background Research Objective Quality Measures Evaluation Framework Proposed Model Discussion and Conclusion
Background • Rising cost (18% of GDP) and improving quality in U. S. healthcare systems. • Assessing value by evaluating quality of service, outcome, and cost. • Massive transformation in healthcare due to evolution of care systems. • Care systems impacted by regulatory agencies and incentive programs. • Incentive programs focus on enhancing efficiency and minimizing cost.
Background • Health information technology adoption pose considerable challenges • Care setting transformation • • Volume-based to value-based Require comprehensive reform Requires uniformity at all levels of care Align performance measures to care services
Research Objectives • Design value-based care based on cost and care effectiveness • Lack of precise quality measures linked to financial rewards • Including all stakeholders in the process of measuring care quality • Measures designed based on outcomes, patient satisfaction, and clinical resources. • Integration of all care components through shared accountability avoids erroneous risk sharing

Quality Measures • Promoting care quality within care services highlighted by pay-forperformance models. • Care quality measures • • Timely data Accurate data Comprehensive clinical practice dynamics Easy access and applicability to clinical practices • Implementing care coordination, cost efficiency, shared saving programs. • Quality measures must identify and track healthcare stakeholders’ contributions
Evaluation Framework • Care quality evaluation frameworks have been designed to emphasize on broad evaluation of value-based models. • Comprehensive evaluation systems: • • System functionality aspects Care outcome measures Cost efficiency indicators Improvement plans that include all stakeholders
Evaluation Framework • Care delivery systems entail a broad scope • Comparing the efficiency in use of healthcare resources and care services not by cost analysis alone • Lack of standardization in U. S. healthcare system resulted in a ‘craft’ culture • Establishing clinical guidelines requires promoting complete value analysis in care systems. • Value equals outcome divided by cost • Scope of beneficiaries impacted by outcome • Inclusion of all stakeholder input • Time periods estimated for the outcome and cost calculation • Implementing information systems that are capable monitoring measures that can capture all measures in addition to leadership commitment
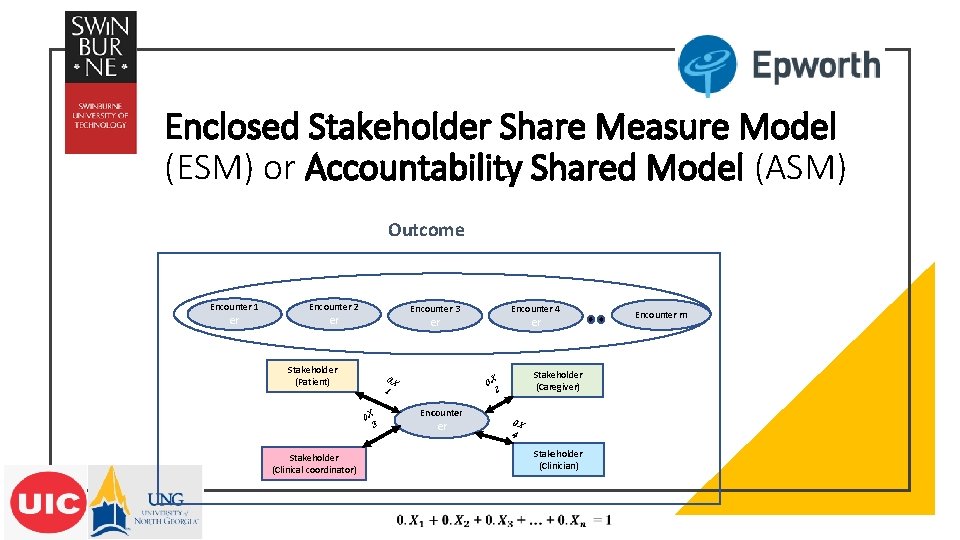
Enclosed Stakeholder Share Measure Model (ESM) or Accountability Shared Model (ASM) Outcome Encounter 1 er Encounter 2 Encounter 3 er Stakeholder (Patient) 0. X 1 0. X 3 Stakeholder (Clinical coordinator) Encounter 4 er er Stakeholder (Caregiver) 0. X 2 Encounter er 0. X 4 Stakeholder (Clinician) Encounter m

Discussion • Healthcare characterization includes multifaceted stakeholder engagement in care delivery services. • Required model must be comprehensive to gather relevant clinical and patient data and organize it into actionable steps. • Merit-based Incentive Payment System (MIPS) target care performance in 4 main categories • • Quality Resource use Advancing care information Clinical practice improvement • MIPS reimbursement rates are not closely linked to the resource use category. MIPS also lacks a robust risk adjustment model to capture all patient contributions in the process of care.
Thank you Q&A • nilmini. work@gmail. com • rgibbi 2@uic. edu
- Slides: 11