Using Patient Panels to Improve Access Continuity and

- Slides: 54
Using Patient Panels to Improve Access, Continuity, and Quality in Family Medicine Teaching Practices Bruce Soloway, M. D. Jonathan Swartz, M. D. Department of Family and Social Medicine Albert Einstein College of Medicine Montefiore Medical Center Bronx, N. Y.
Project Aims n n n To identify the physician who is the first source of primary care for each patient at two family medicine teaching sites To create a “panel list” of all patients for whom each physician acts as PCP To explore the consequences of explicit PCP assignments and panel lists
What is a “Primary Care Provider”? n n n The first source of care for each patient The provider ultimately responsible for each patient’s chronic and preventive care Principle: Every patient should have one and only one PCP
What is a “Panel”? n n n The list of patients for whom each provider serves as PCP The basis of continuity and patient satisfaction The source of demand for appointments for each provider
Why are panels important? n n n Help to define and equitably divide the work of the practice, improving access, efficiency and continuity. Allow individual feedback to providers on aggregate demographics, processes and outcomes for the patients they treat Allow rational transfer of patients from one PCP to another when a provider enters or leaves a practice
Panels in teaching practices n Special challenges to continuity n n Most providers practice part-time Care often shared between providers Acute care often rendered by covering MD Frequent provider turnover
Project setting n n Montefiore Residency Program in Family Medicine (Bronx, NY) Two teaching practices, each with n n n 15 residents 4 attendings actings as resident team leaders Several non-teaching attending physicians
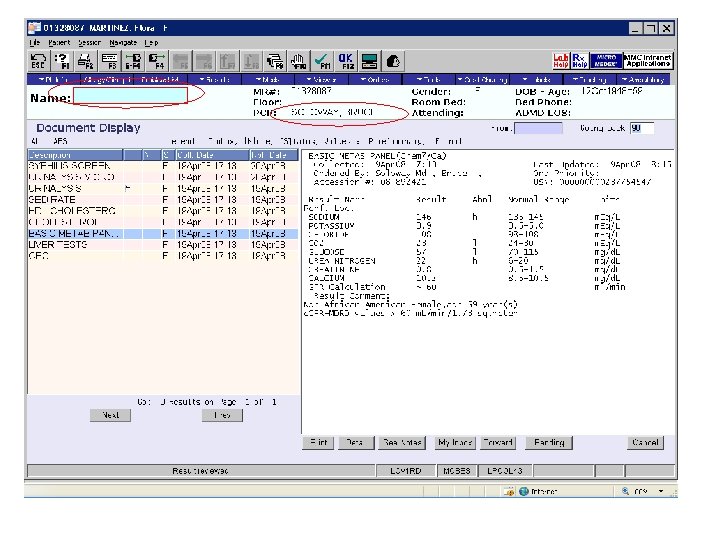
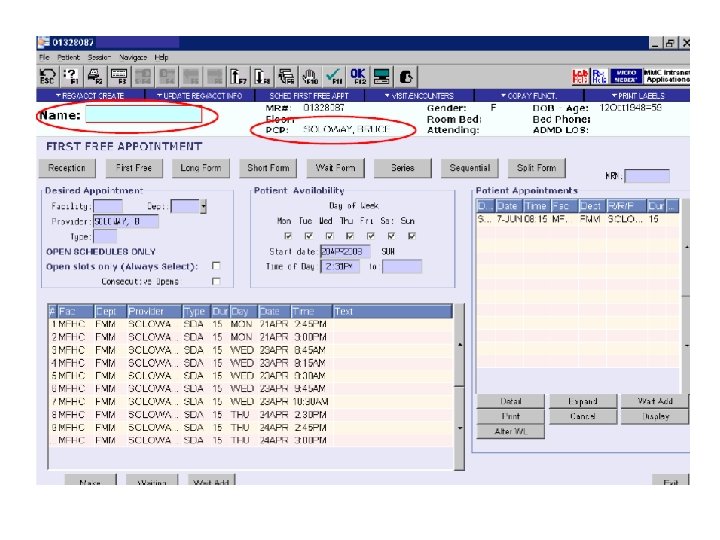
Project setting n Electronic medical record n n n GE Centricity Enterprise (a/k/a “Care. Cast”) Robust hospital-based system with rudimentary outpatient component Contains outpatient visit histories, labs, problem lists, medication lists, allergy lists —but not progress notes In process of converting to full-scope EMR All users see “PCP” for each patient
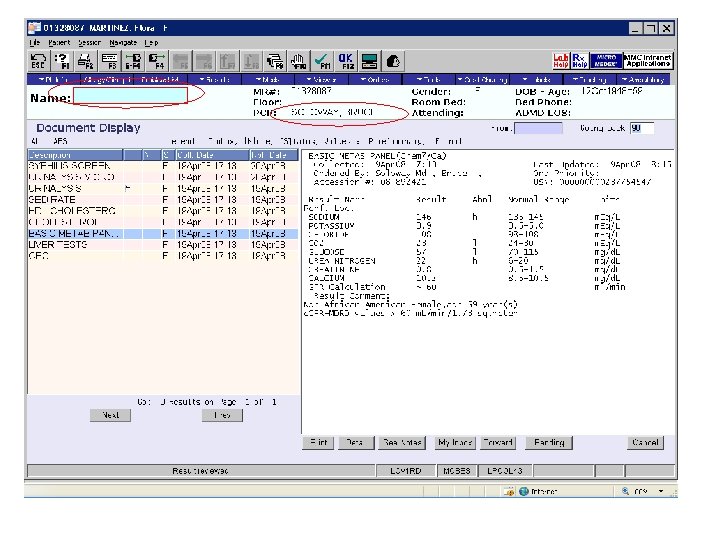
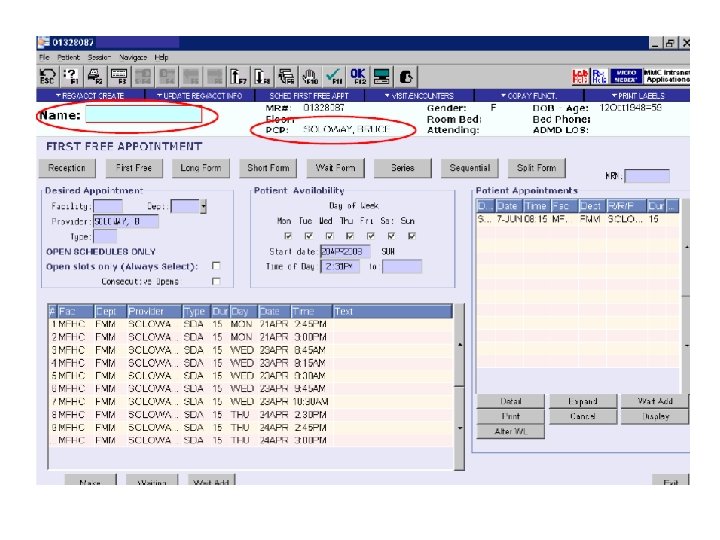
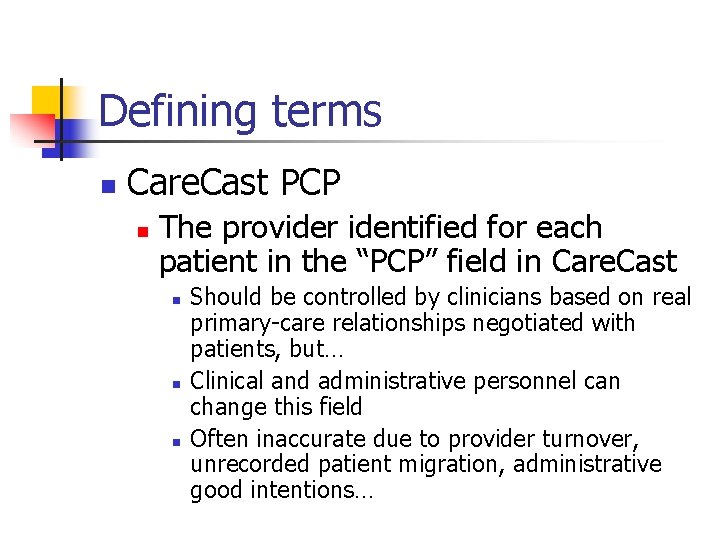
Defining terms n Care. Cast PCP n The provider identified for each patient in the “PCP” field in Care. Cast n n n Should be controlled by clinicians based on real primary-care relationships negotiated with patients, but… Clinical and administrative personnel can change this field Often inaccurate due to provider turnover, unrecorded patient migration, administrative good intentions…
Defining terms n Visit-based PCP n n n The active provider seen most often by each patient in the last 18 months Or, if there is a tie, the active provider seen most recently in the last 18 months Some patients are “orphan patients” n n No visit-based PCP, no active Care. Cast PCP During the past 18 months, have only seen providers who have since left the practice
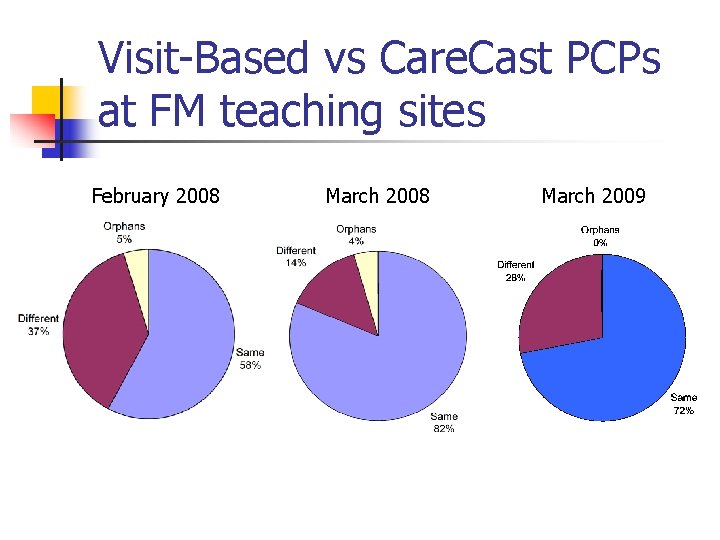
Pushing the button n On March 4, 2008, Care. Cast PCP fields were updated for nearly 6000 patients at both teaching sites using a providerapproved algorithm based on recent visit history.
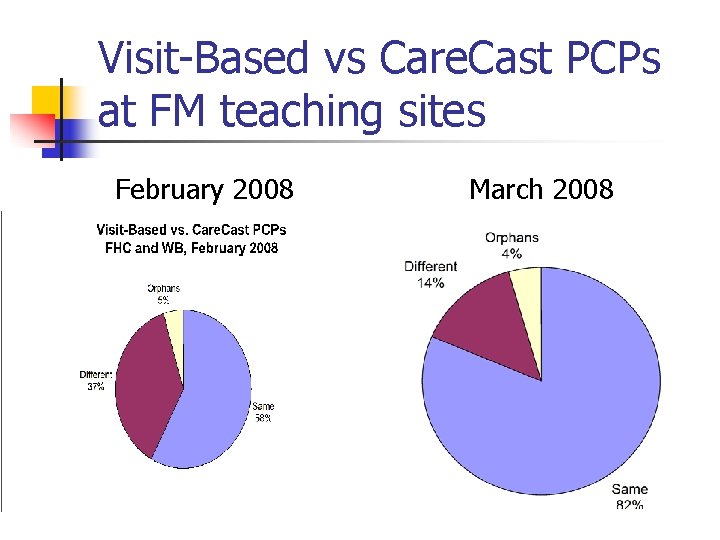
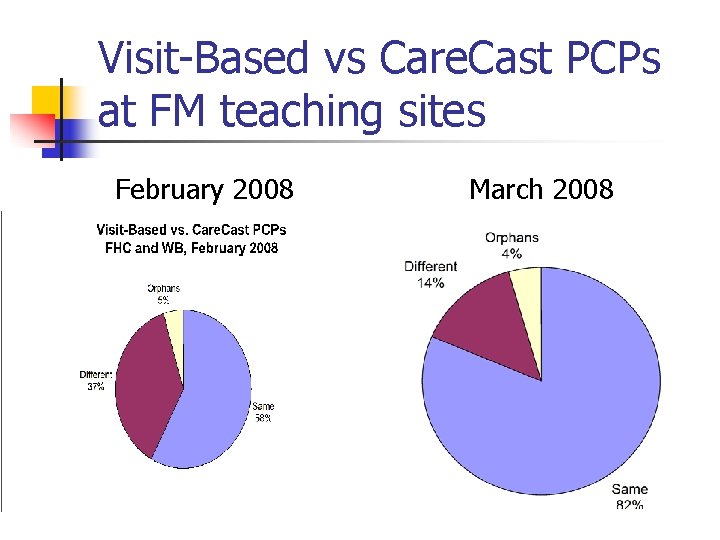
Visit-Based vs Care. Cast PCPs at FM teaching sites February 2008 March 2008
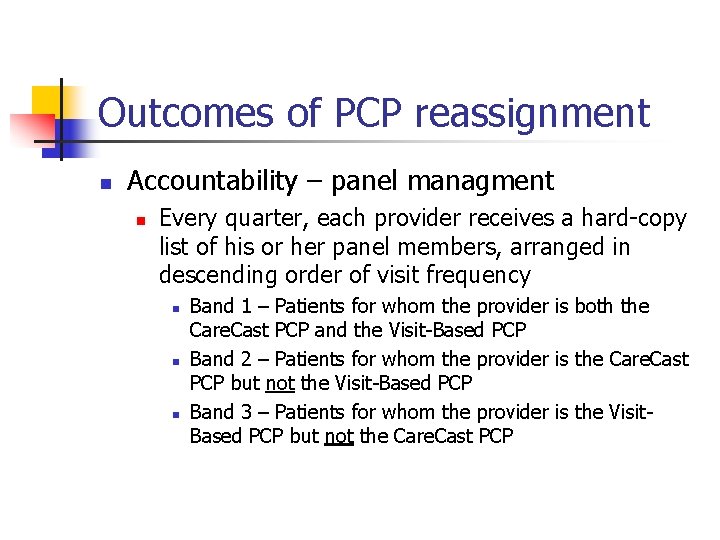
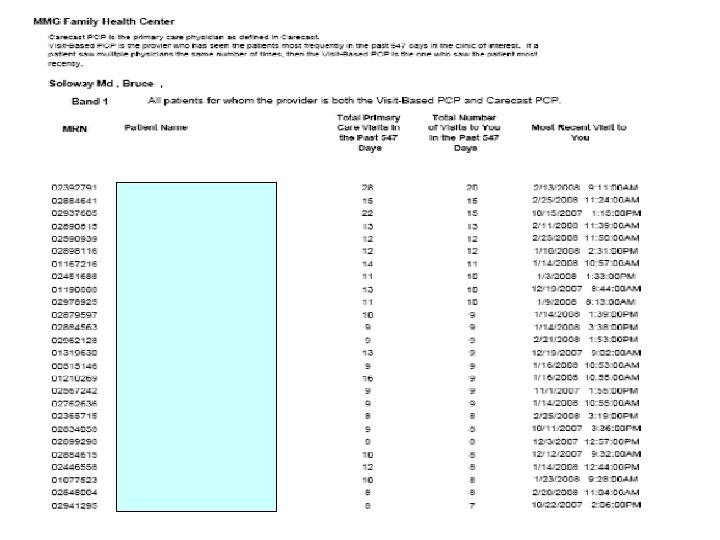
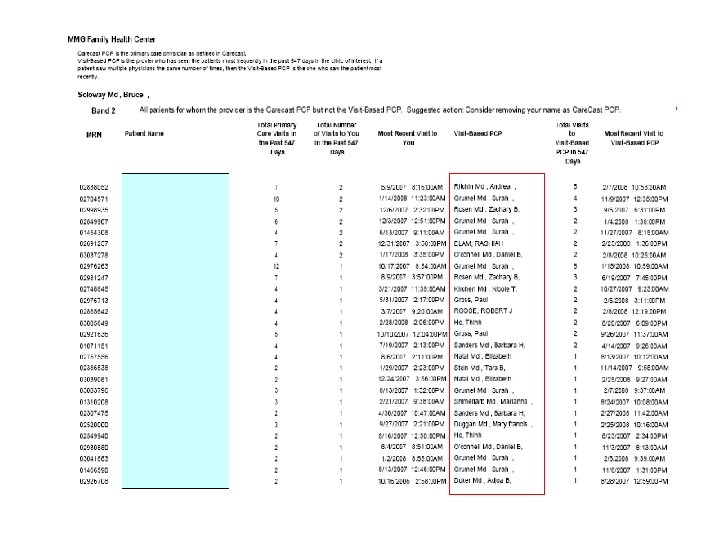
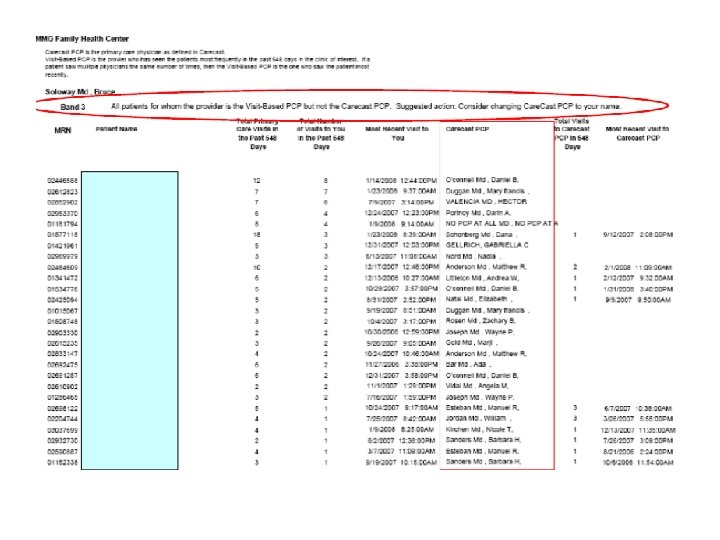
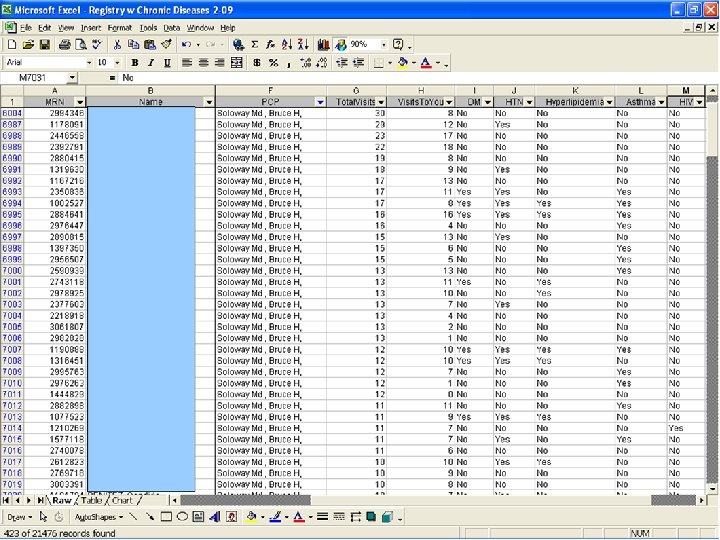
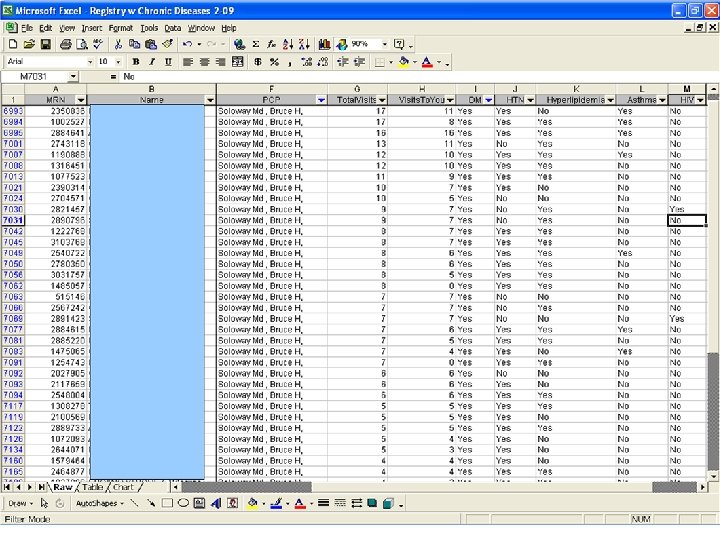
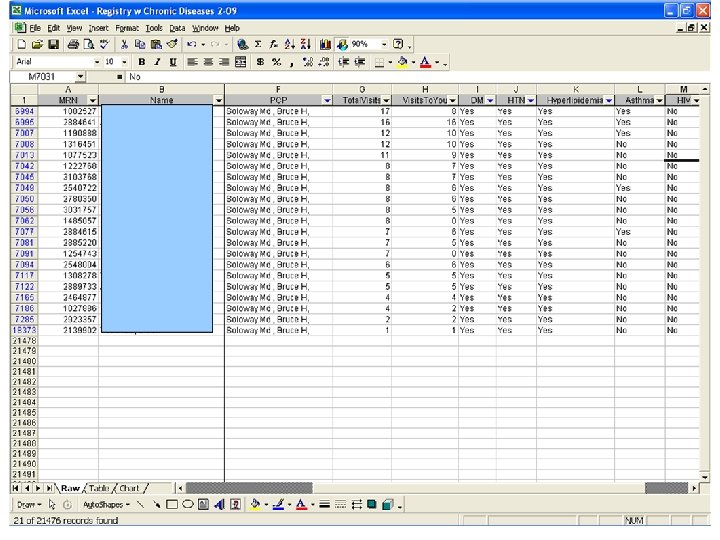
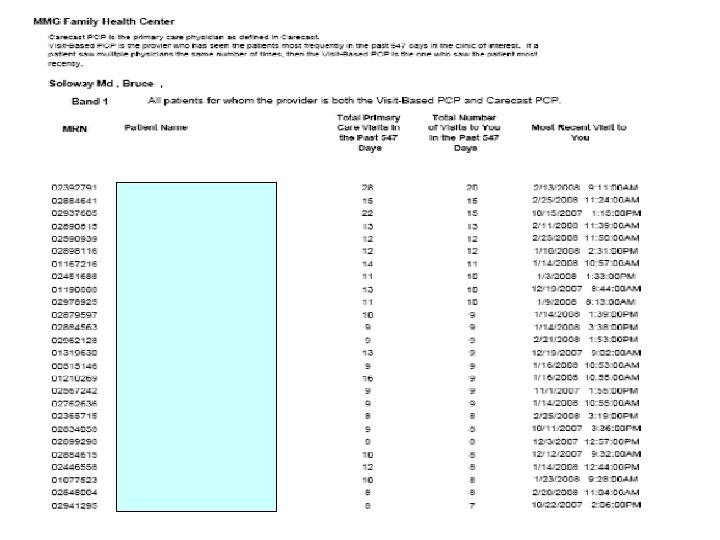
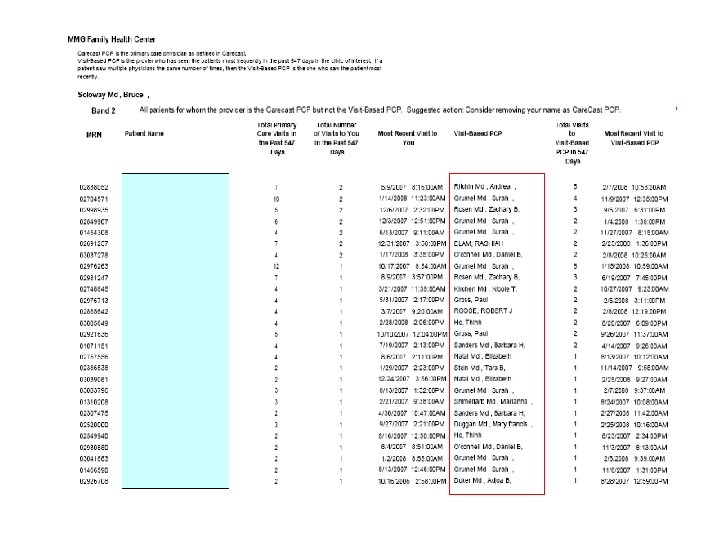
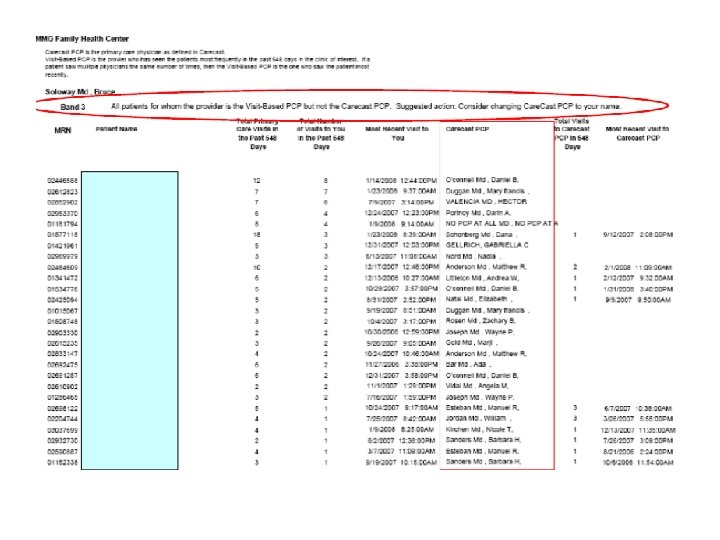
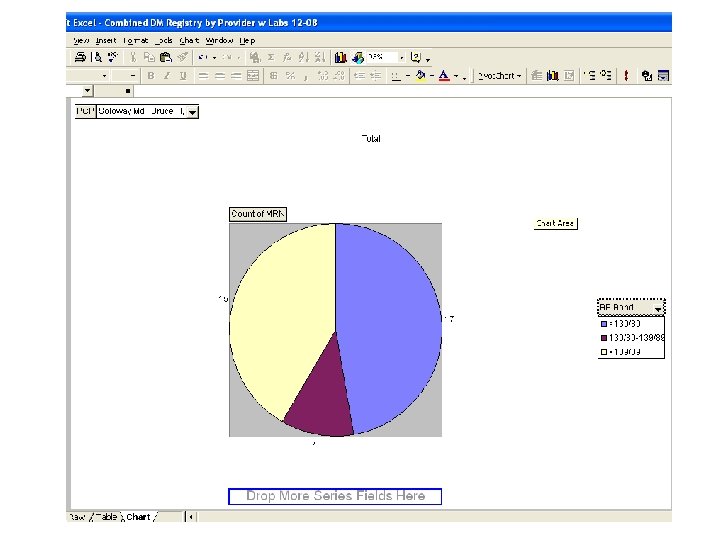
Outcomes of PCP reassignment n Accountability – panel managment n Every quarter, each provider receives a hard-copy list of his or her panel members, arranged in descending order of visit frequency n n n Band 1 – Patients for whom the provider is both the Care. Cast PCP and the Visit-Based PCP Band 2 – Patients for whom the provider is the Care. Cast PCP but not the Visit-Based PCP Band 3 – Patients for whom the provider is the Visit. Based PCP but not the Care. Cast PCP
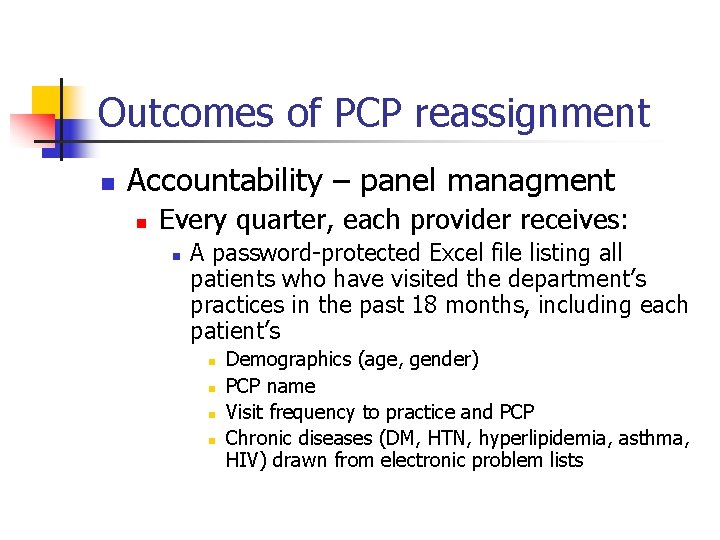
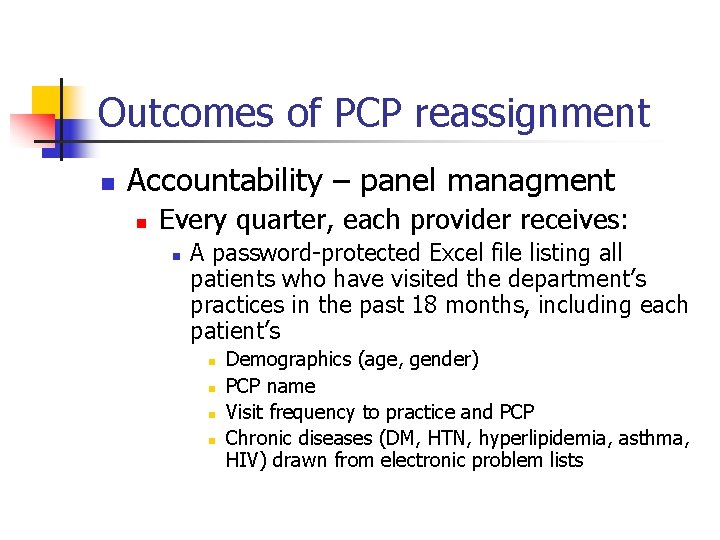
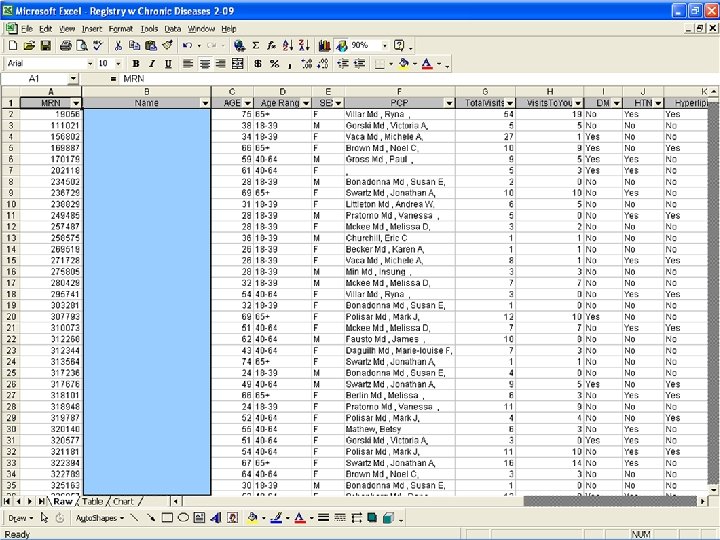
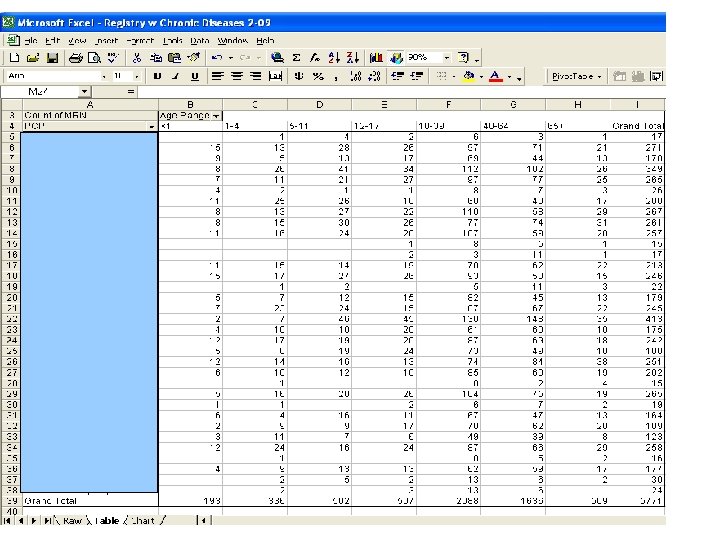
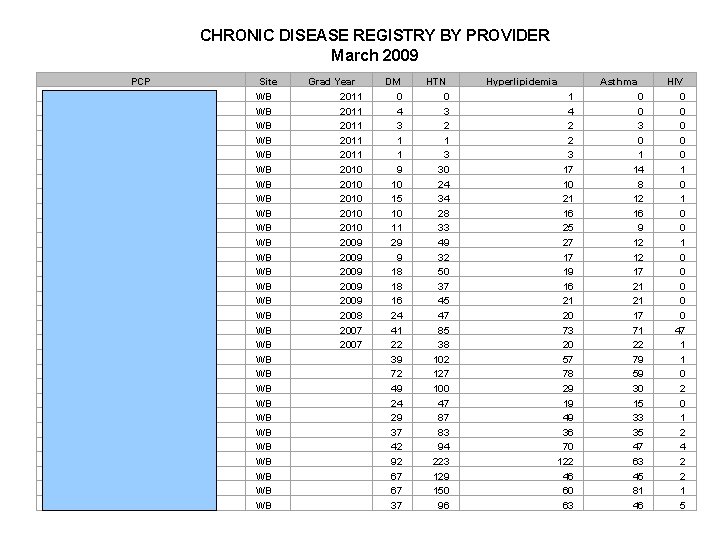
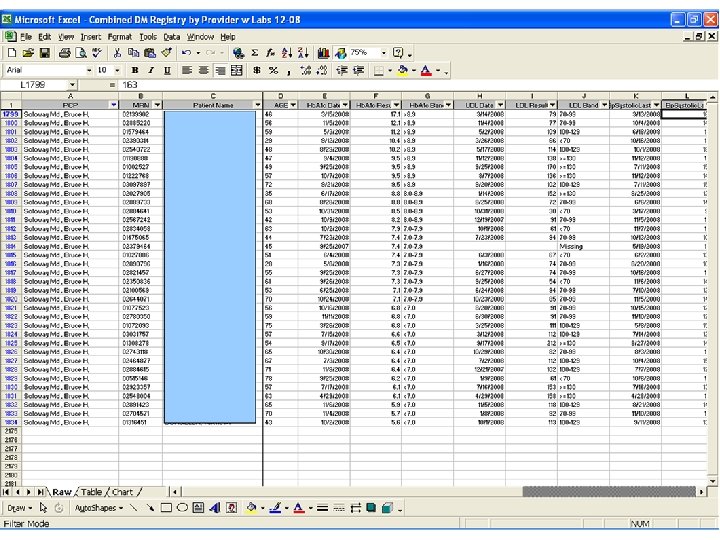
Outcomes of PCP reassignment n Accountability – panel managment n Every quarter, each provider receives: n A password-protected Excel file listing all patients who have visited the department’s practices in the past 18 months, including each patient’s n n Demographics (age, gender) PCP name Visit frequency to practice and PCP Chronic diseases (DM, HTN, hyperlipidemia, asthma, HIV) drawn from electronic problem lists
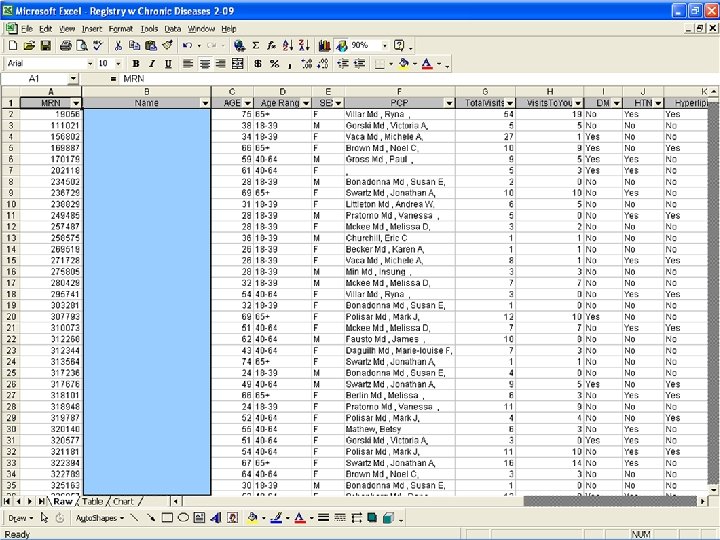
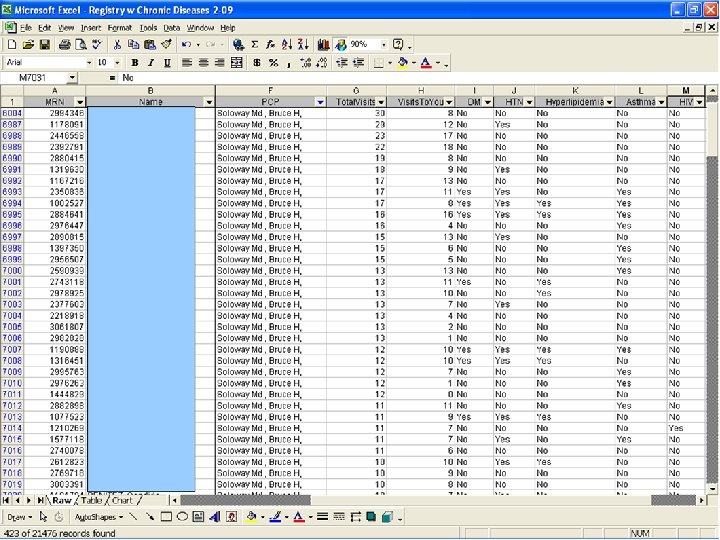
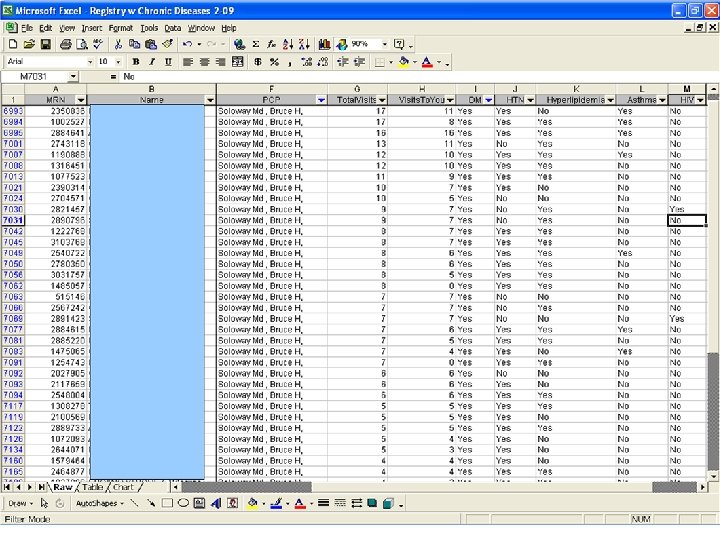
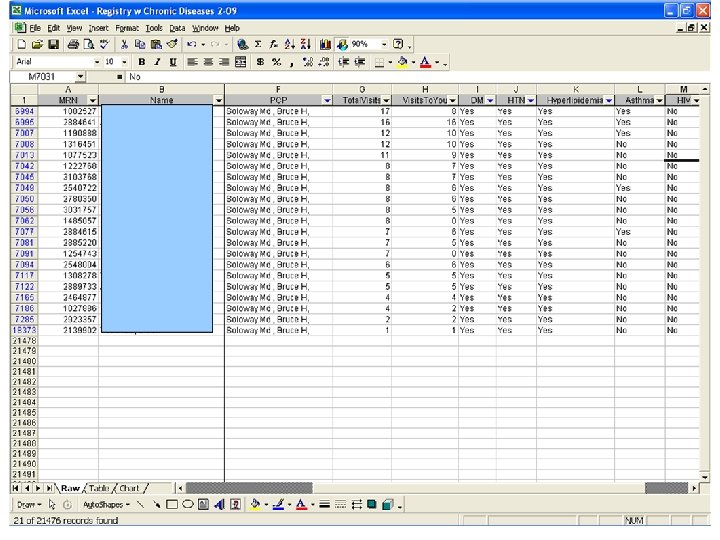
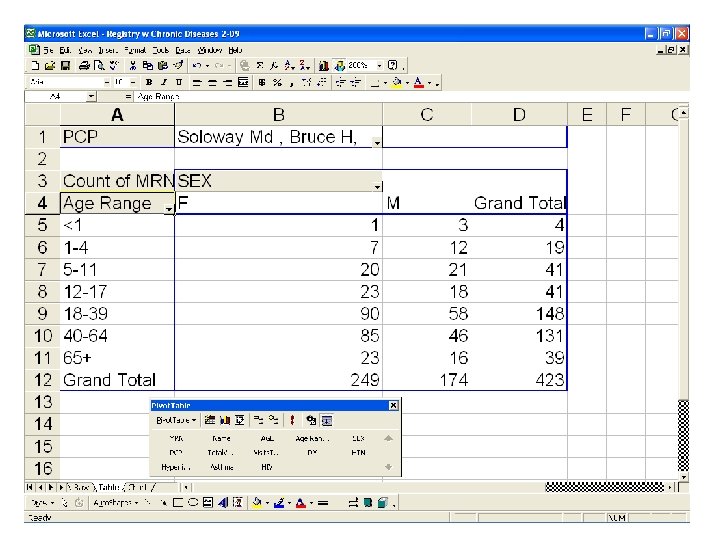
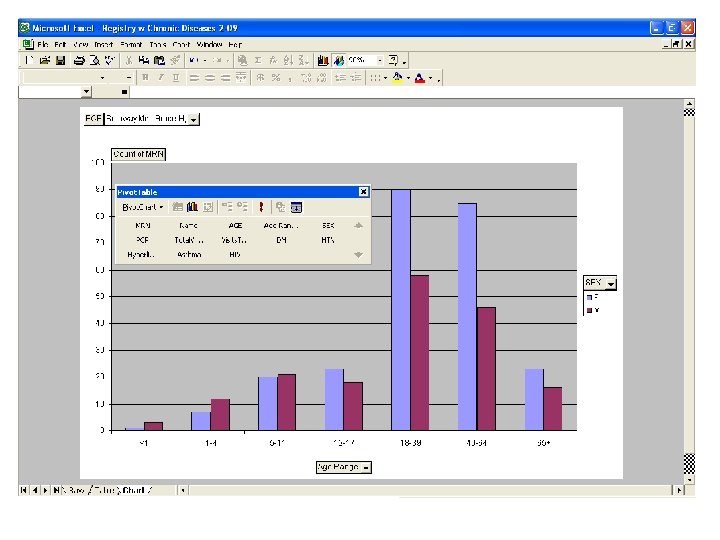
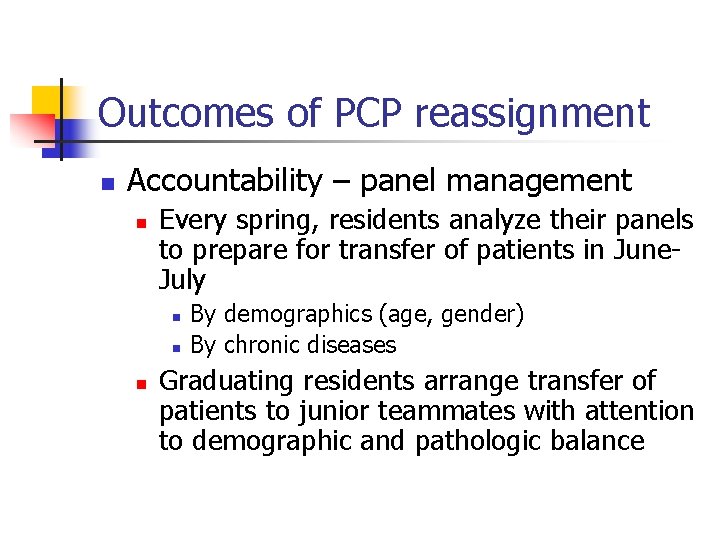
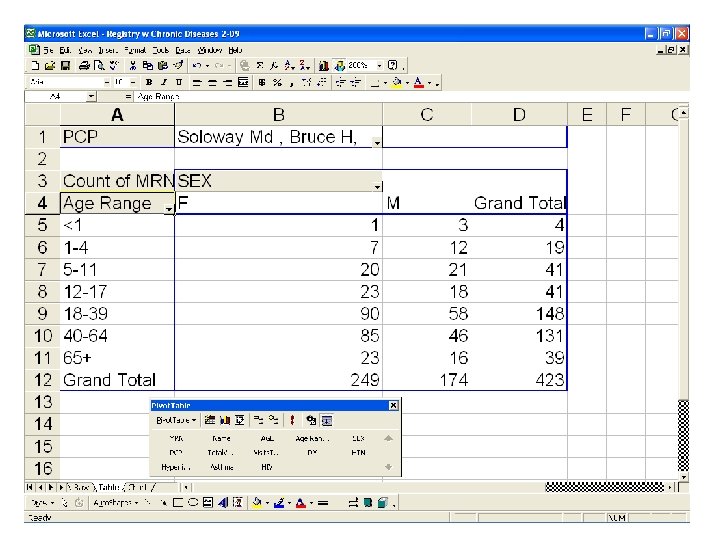
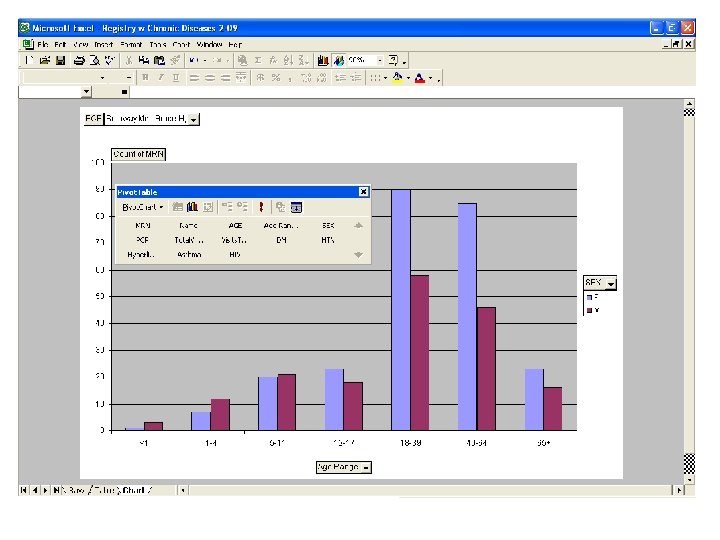
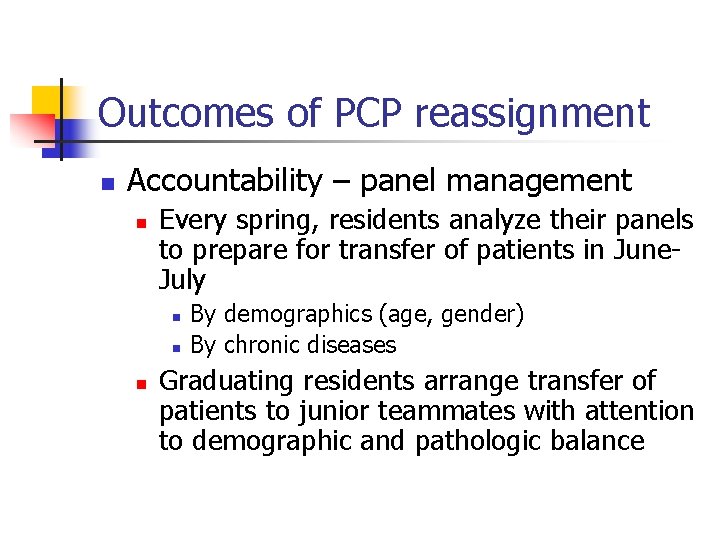
Outcomes of PCP reassignment n Accountability – panel management n Every spring, residents analyze their panels to prepare for transfer of patients in June. July n n n By demographics (age, gender) By chronic diseases Graduating residents arrange transfer of patients to junior teammates with attention to demographic and pathologic balance
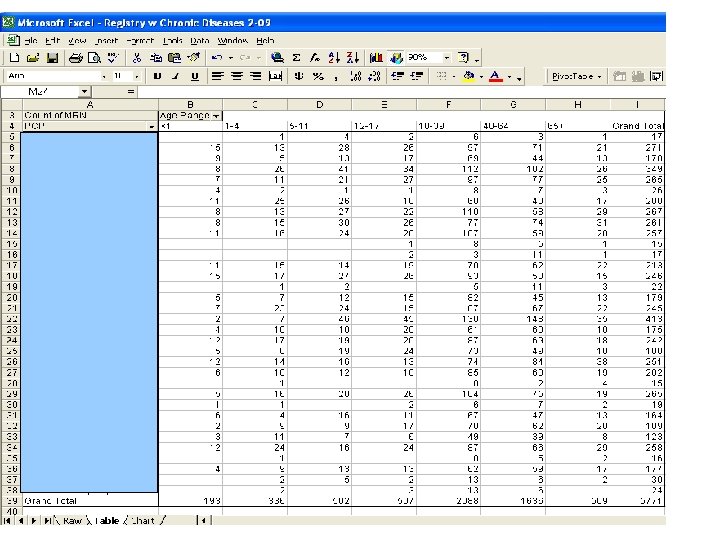
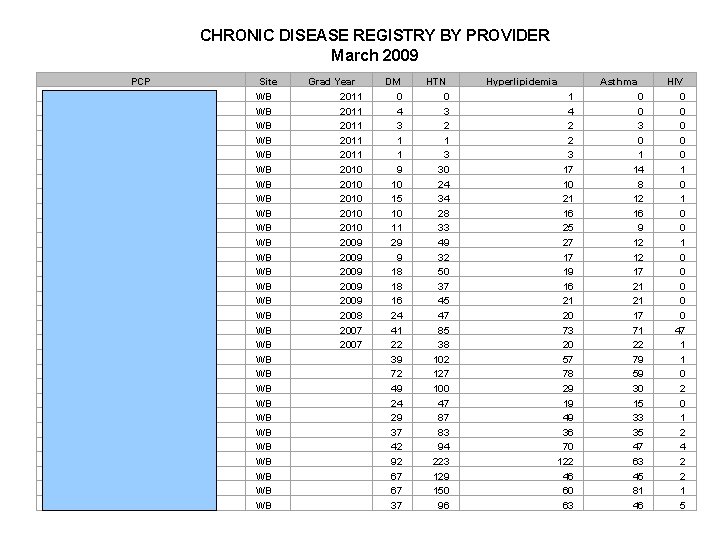
CHRONIC DISEASE REGISTRY BY PROVIDER March 2009 PCP Akanki Md , Feyisara , Hwang Res, Irene , Kumar Res, Harini , Reddy Res, Anjani , Wilson Res, April , Berlin Md , Melissa , Lapman Md , Lisa , Min Md , Insung , Pratomo Md , Vanessa , Wadke Md , Rahul , Fausto Md , James , Hodgson, Sybil Mathew, Betsy Parker, Sharissa B Rieper, Leigh A Churchill, Eric C Chu Md , Carolyn , Harris Md , Marissa A, Becker Md , Karen A, Brown Md , Noel C, Daguilh Md , Marie-louise F, Johnston-briggs Md , Belinda Kumar Md , Vanita , Lee Md , Elizabeth T, Mckee Md , Melissa D, Polisar Md , Mark J, Swartz Md , Jonathan A, Vaca Md , Michele A, Villar Md , Ryna , Site WB WB WB WB WB WB WB WB Grad Year 2011 2011 2010 2010 2009 2009 2008 2007 DM 0 4 3 1 1 9 10 15 10 11 29 9 18 18 16 24 41 22 39 72 49 24 29 37 42 92 67 67 37 HTN 0 3 2 1 3 30 24 34 28 33 49 32 50 37 45 47 85 38 102 127 100 47 87 83 94 223 129 150 96 Hyperlipidemia 1 4 2 2 3 17 10 21 16 25 27 17 19 16 21 20 73 20 57 78 29 19 49 36 70 122 46 60 63 Asthma 0 0 3 0 1 14 8 12 16 9 12 12 17 21 21 17 71 22 79 59 30 15 33 35 47 63 45 81 46 HIV 0 0 0 1 0 0 0 47 1 1 0 2 0 1 2 4 2 2 1 5
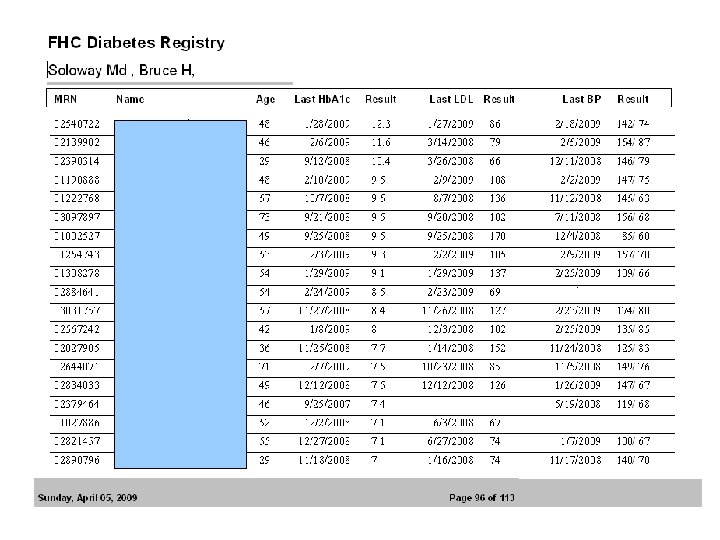
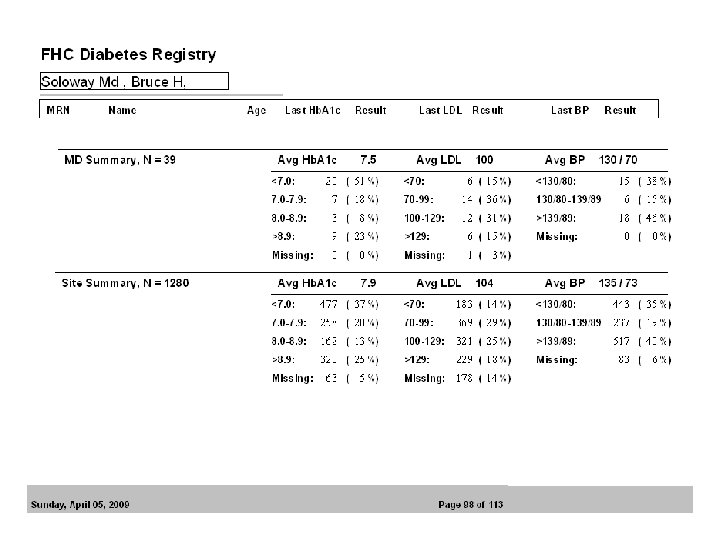
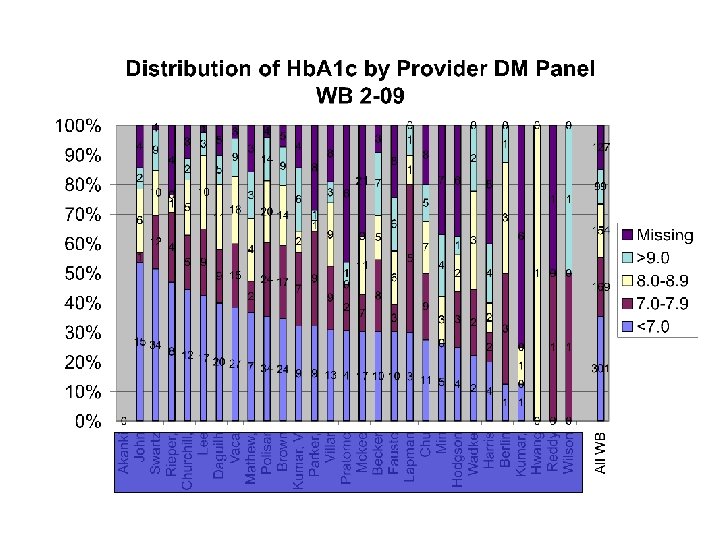
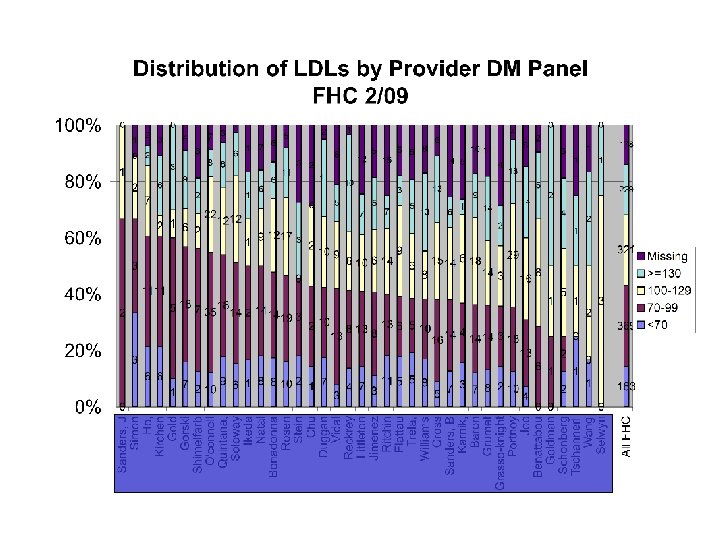
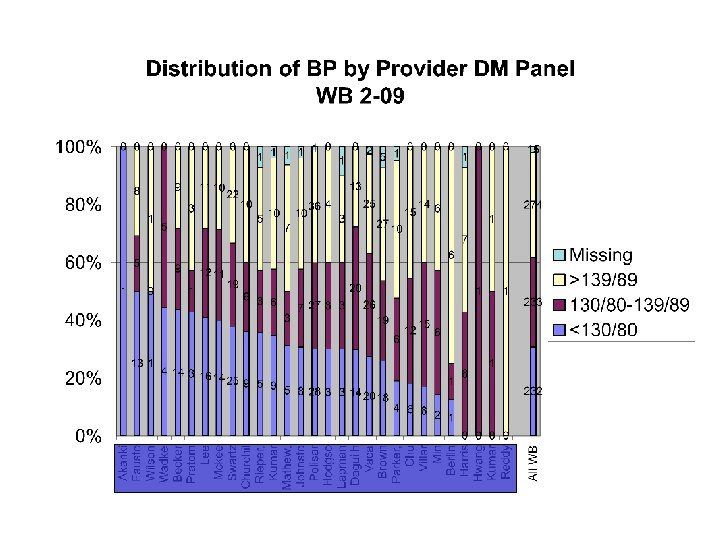
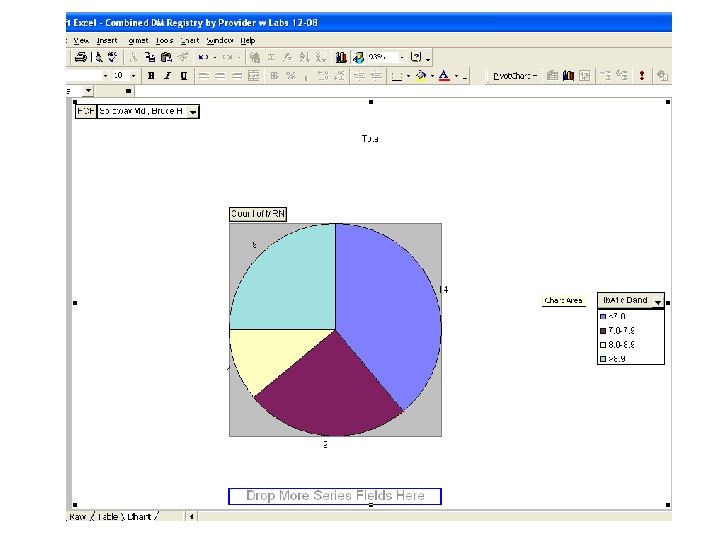
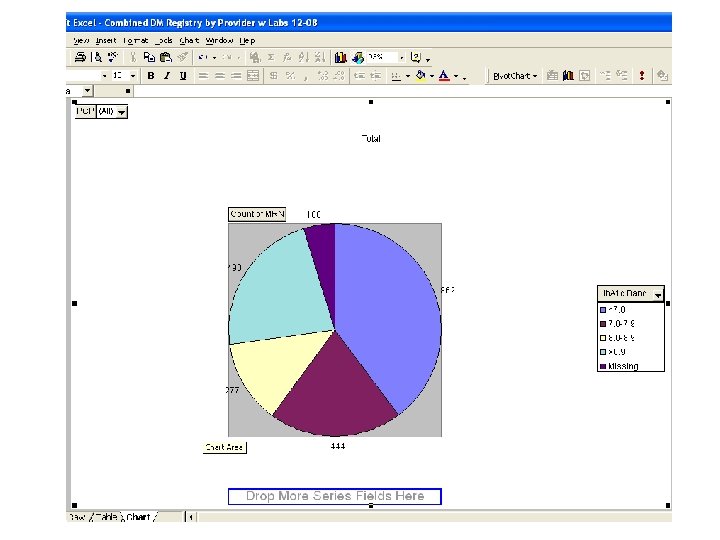
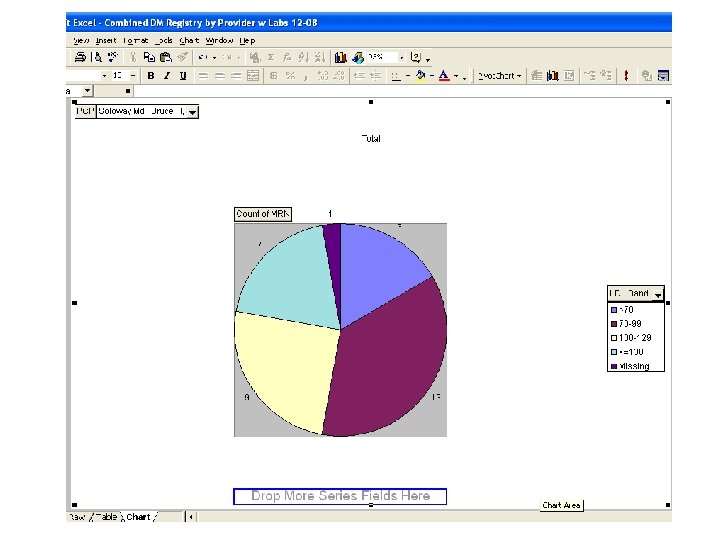
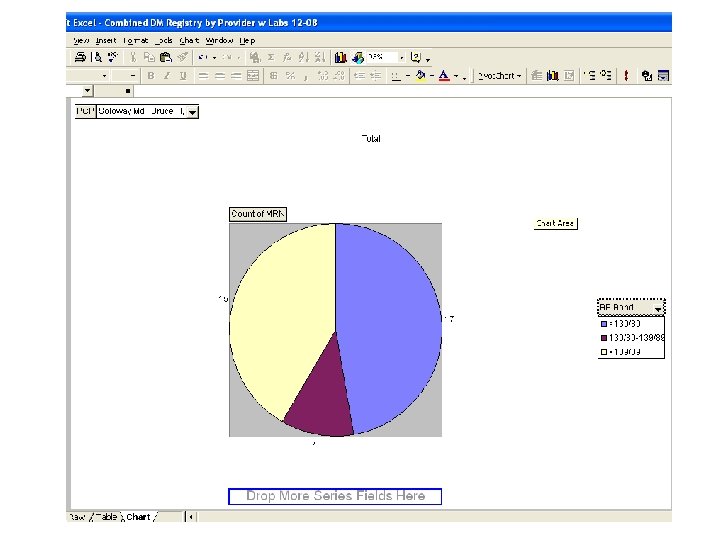
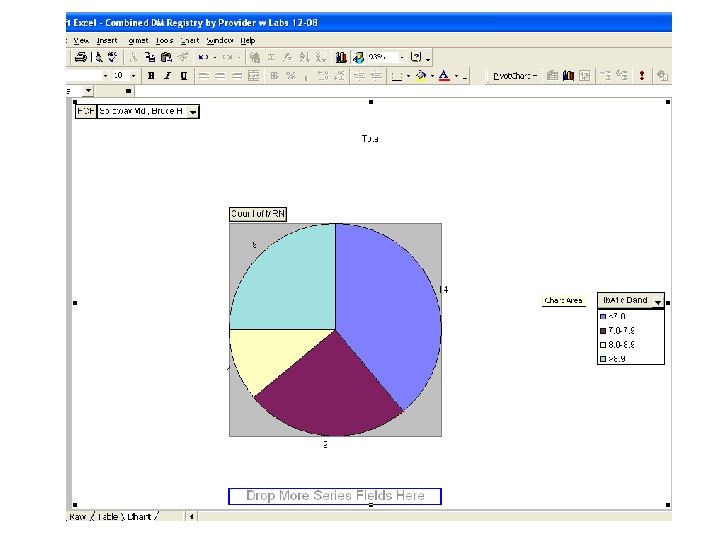
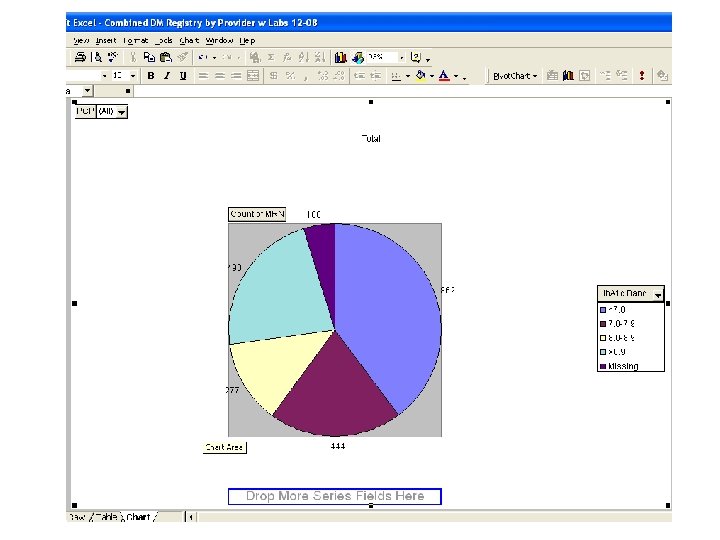
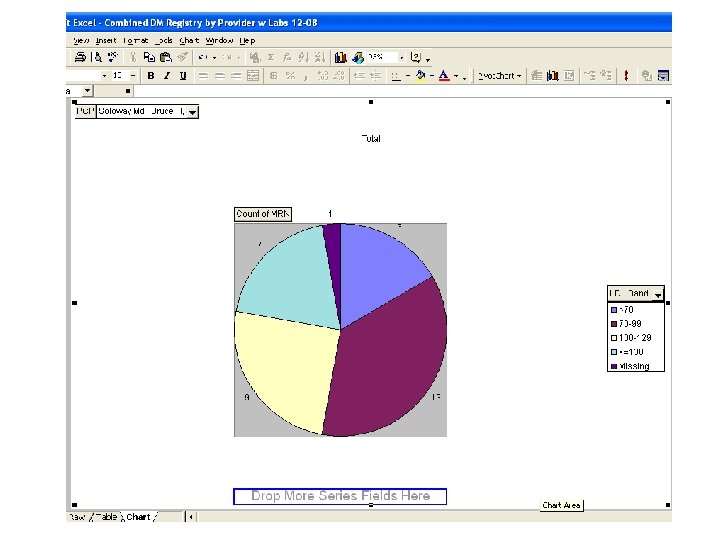
Outcomes of PCP reassignment n Accountability – DM management n Every quarter, each provider receives a hard-copy report with n n A list of all the provider’s patients with diabetes Each patient’s Hb. A 1 c, blood pressure, and LDL The average Hb. A 1 c, blood pressure, and LDL for the provider and for the practice Graphs situating the provider’s outcomes relative to those of his or her peers
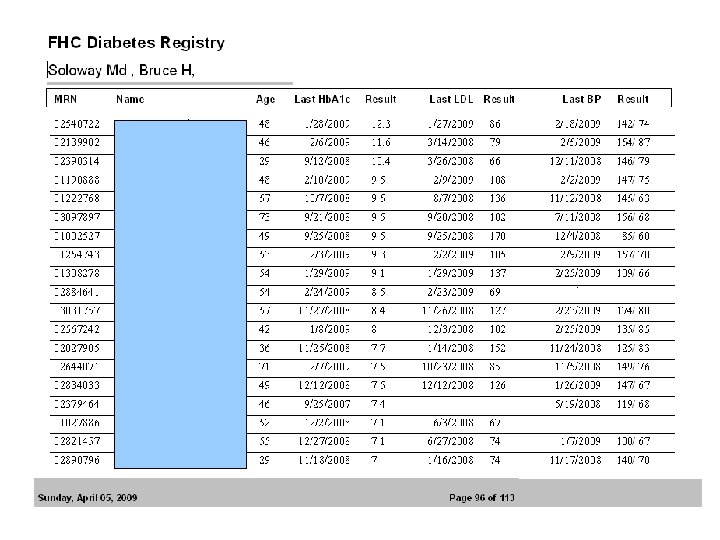
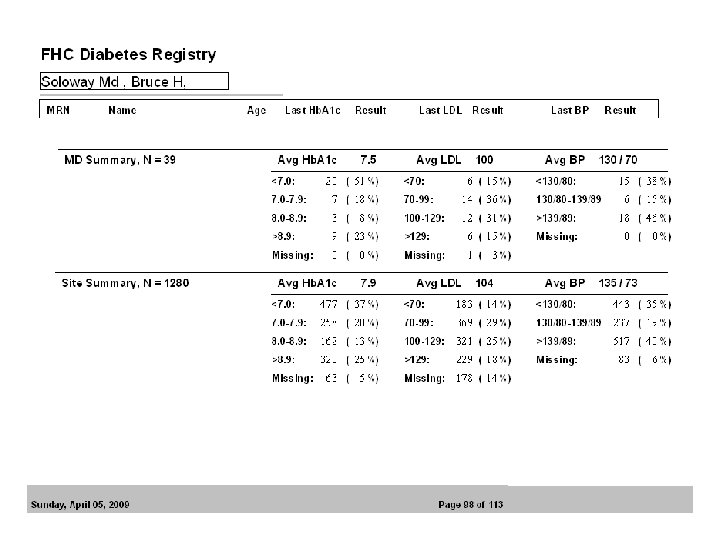
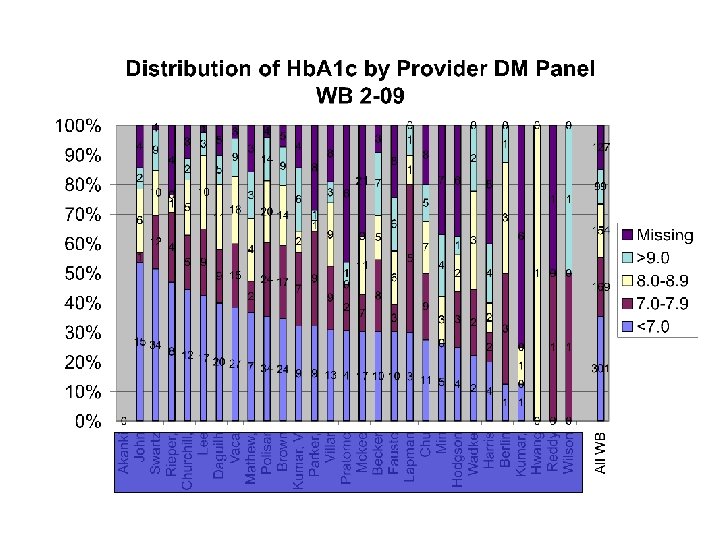
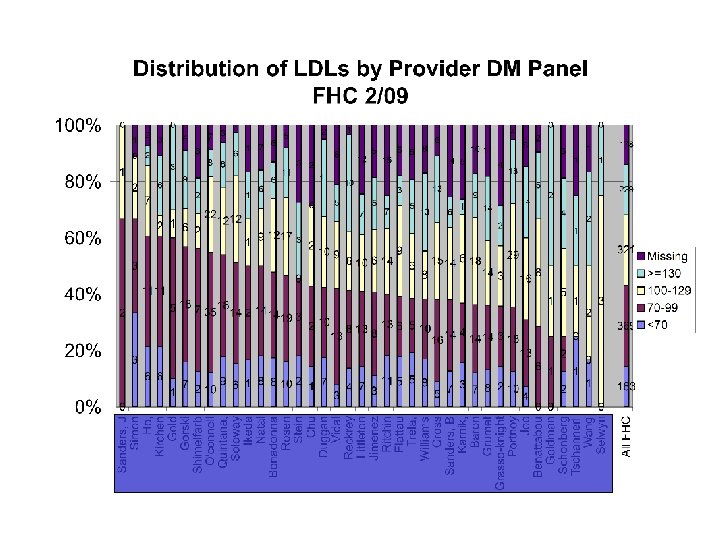
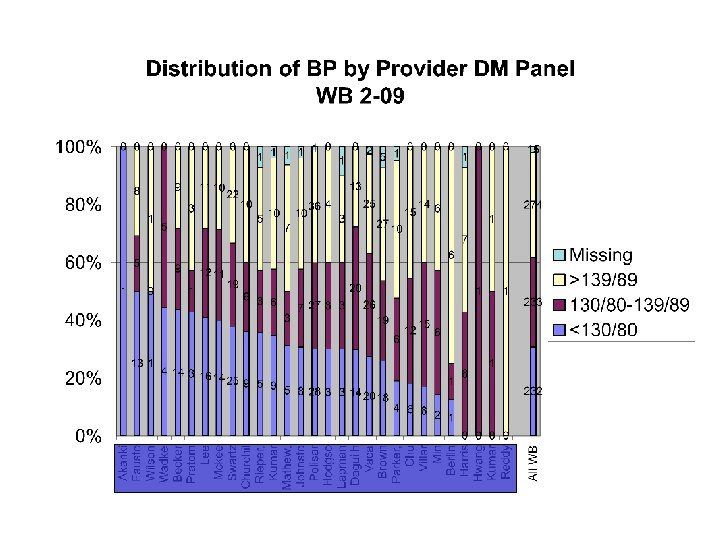
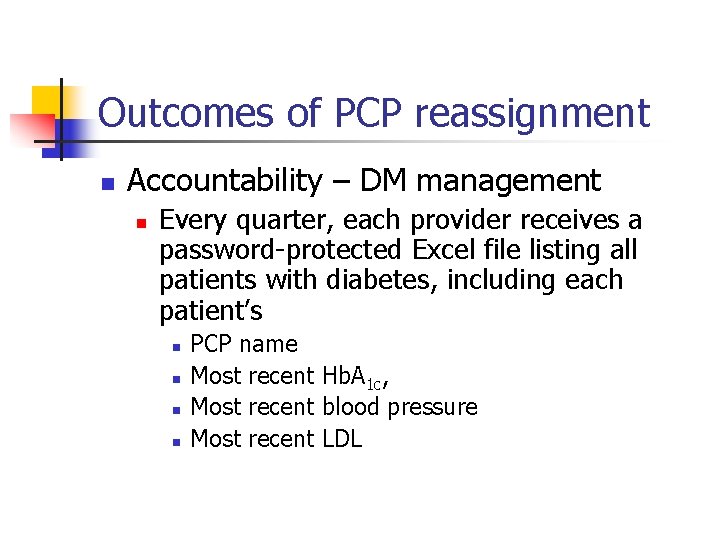
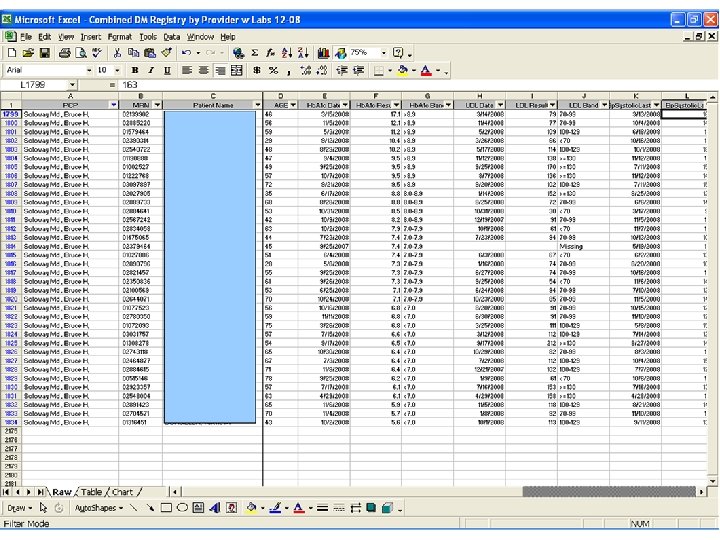
Outcomes of PCP reassignment n Accountability – DM management n Every quarter, each provider receives a password-protected Excel file listing all patients with diabetes, including each patient’s n n PCP name Most recent Hb. A 1 c, Most recent blood pressure Most recent LDL
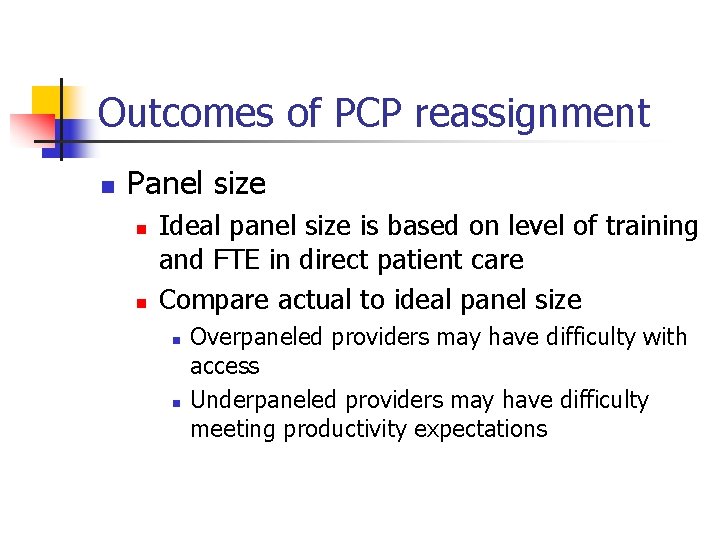
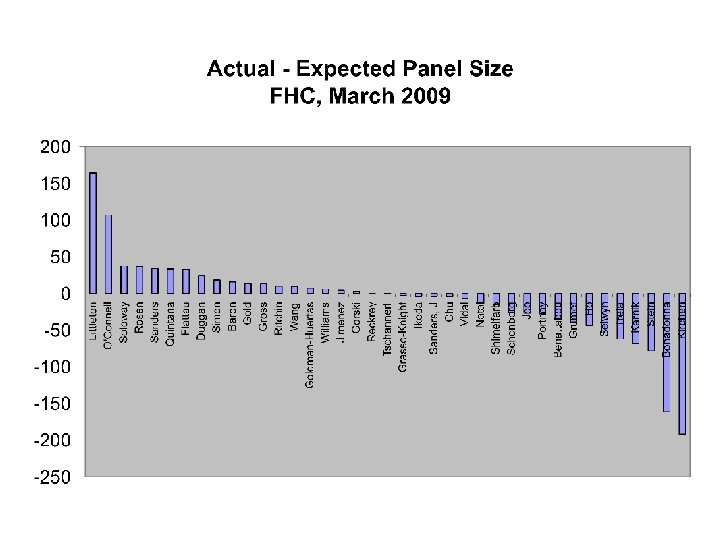
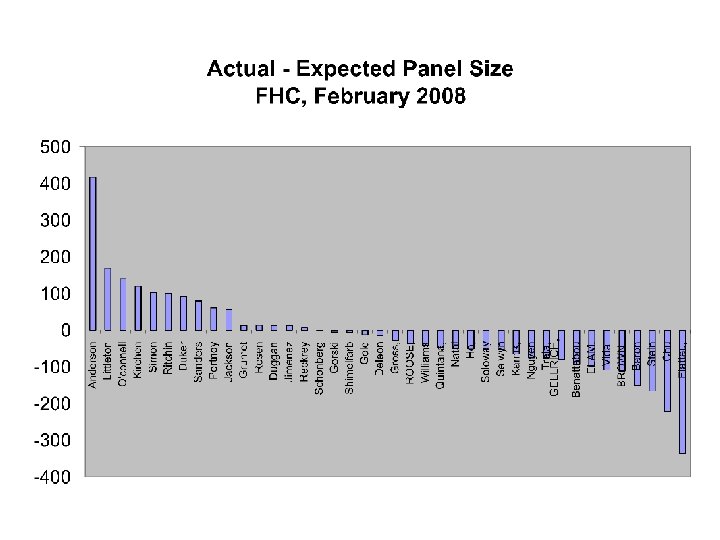
Outcomes of PCP reassignment n Panel size n n Ideal panel size is based on level of training and FTE in direct patient care Compare actual to ideal panel size n n Overpaneled providers may have difficulty with access Underpaneled providers may have difficulty meeting productivity expectations
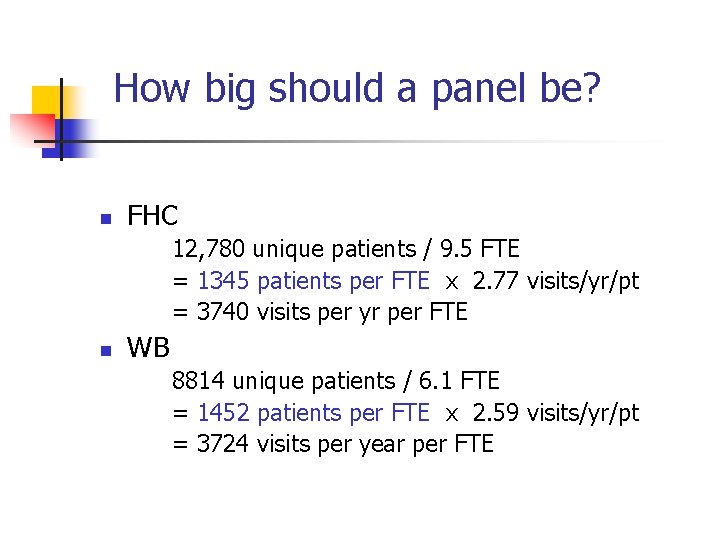
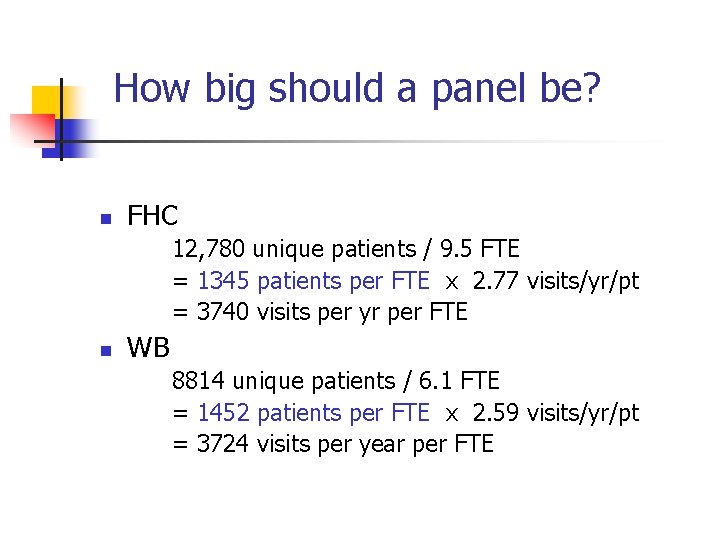
How big should a panel be? n FHC 12, 780 unique patients / 9. 5 FTE = 1345 patients per FTE x 2. 77 visits/yr/pt = 3740 visits per yr per FTE n WB 8814 unique patients / 6. 1 FTE = 1452 patients per FTE x 2. 59 visits/yr/pt = 3724 visits per year per FTE
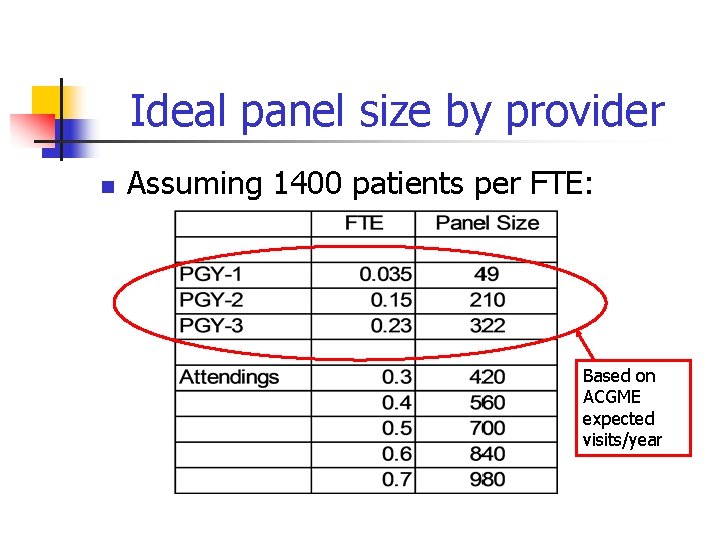
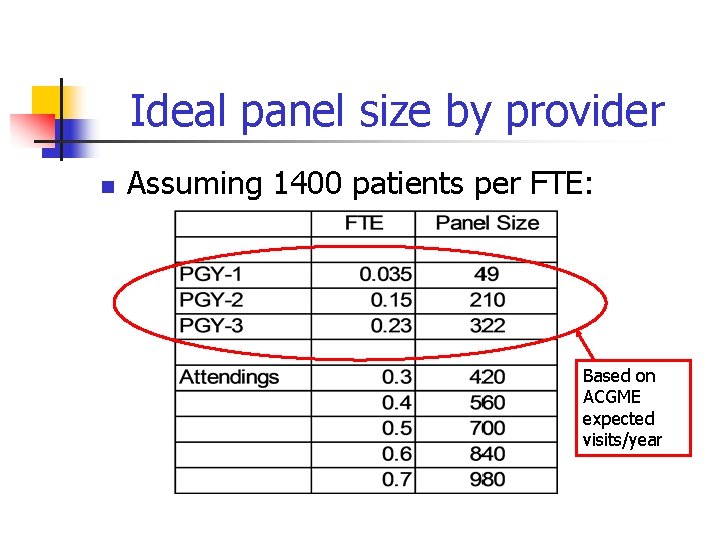
Ideal panel size by provider n Assuming 1400 patients per FTE: Based on ACGME expected visits/year
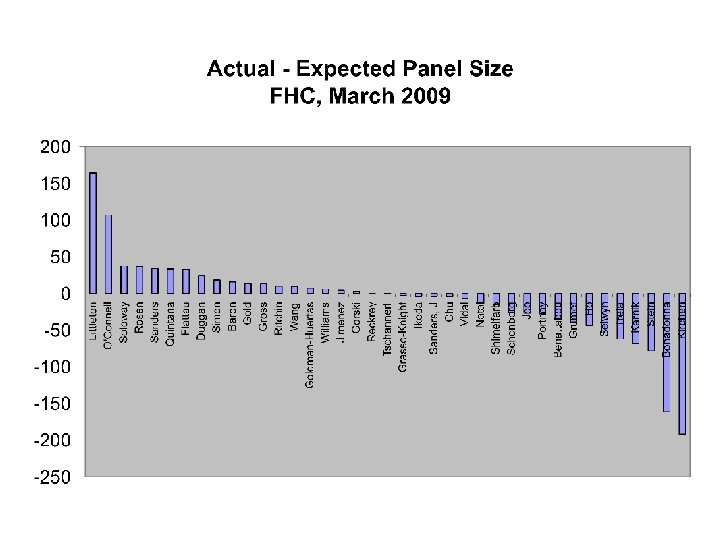
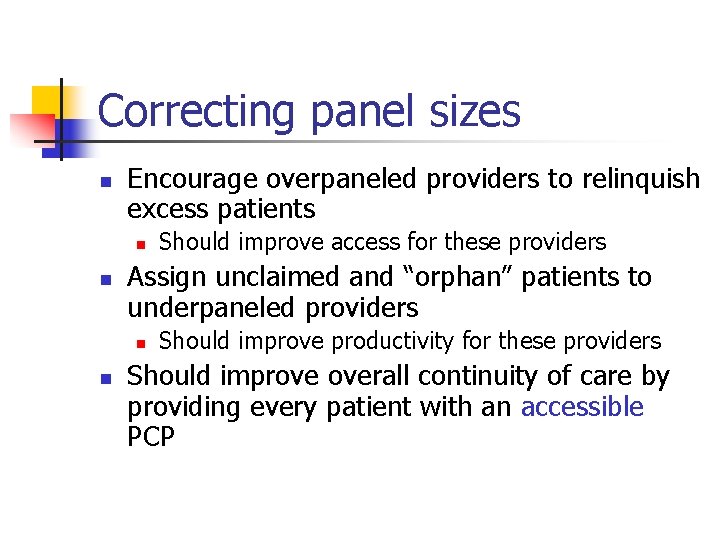
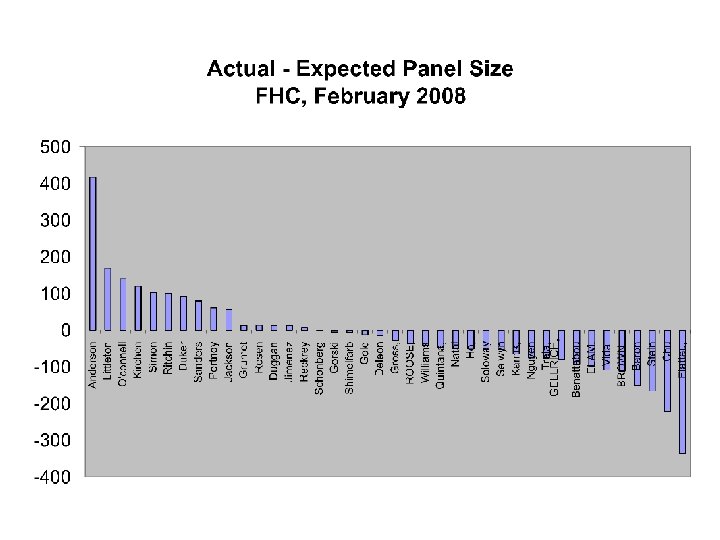
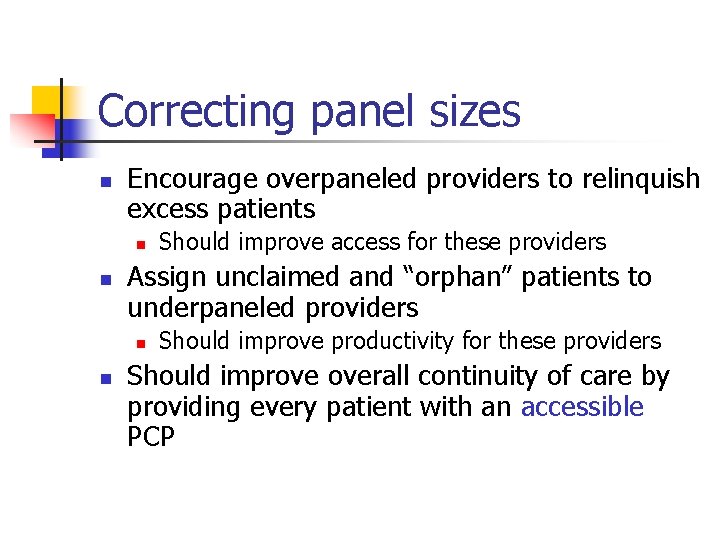
Correcting panel sizes n Encourage overpaneled providers to relinquish excess patients n n Assign unclaimed and “orphan” patients to underpaneled providers n n Should improve access for these providers Should improve productivity for these providers Should improve overall continuity of care by providing every patient with an accessible PCP
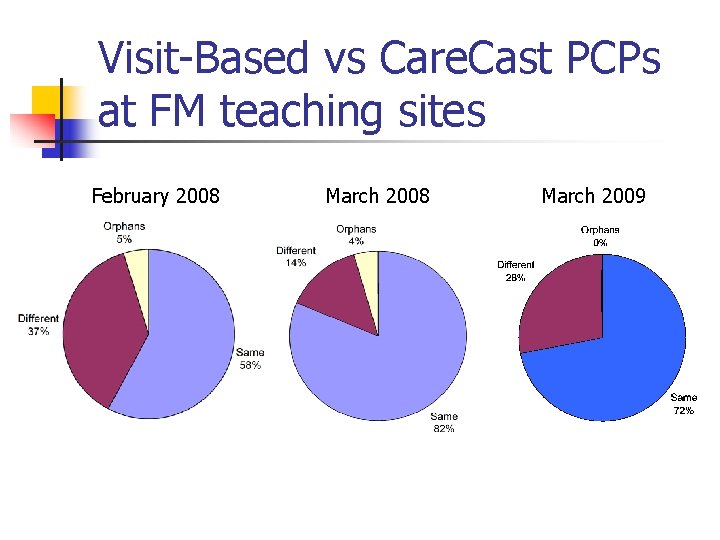
Visit-Based vs Care. Cast PCPs at FM teaching sites February 2008 March 2009
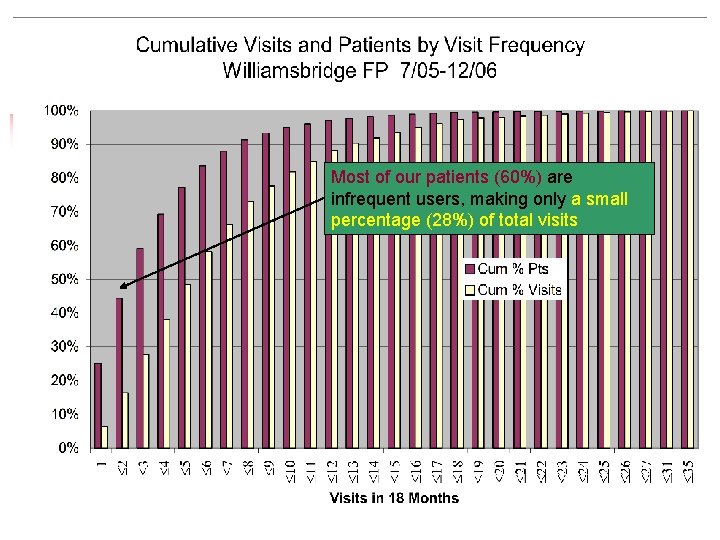
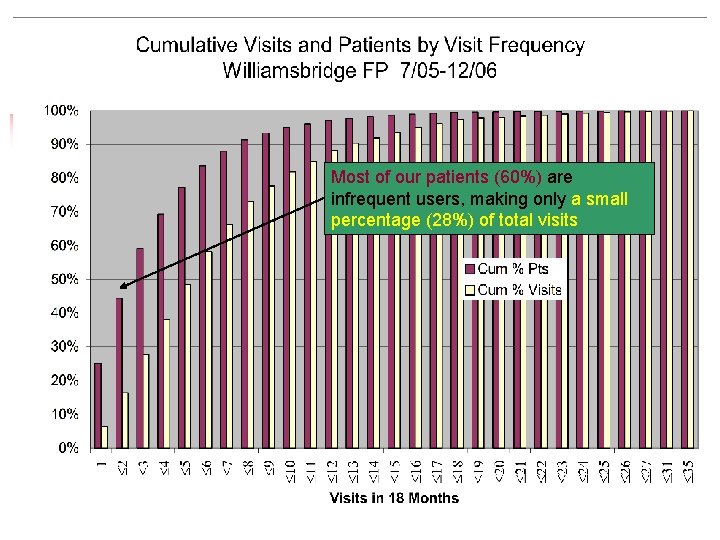
Most of our patients (60%) are infrequent users, making only a small percentage (28%) of total visits
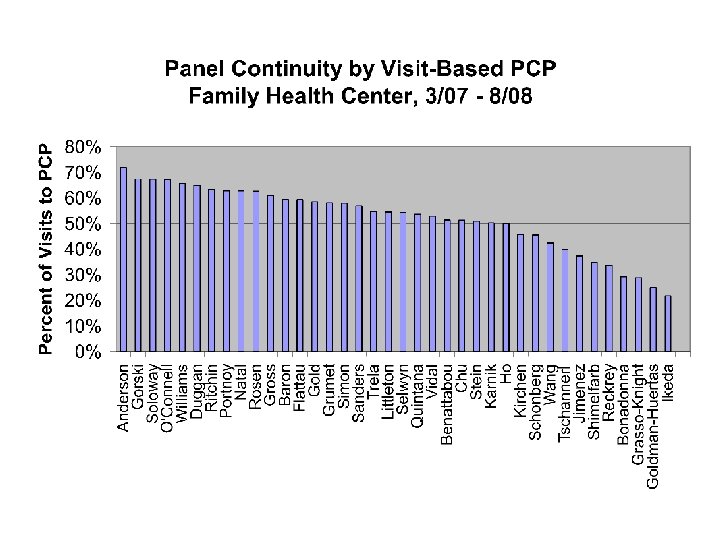
Outcomes of PCP reassignment n Measuring continuity of care n From the patient’s perspective n During a given interval (e. g. 18 months), at what percent of all visits made by members of a provider’s panel did the patient see the PCP (rather than another provider)?
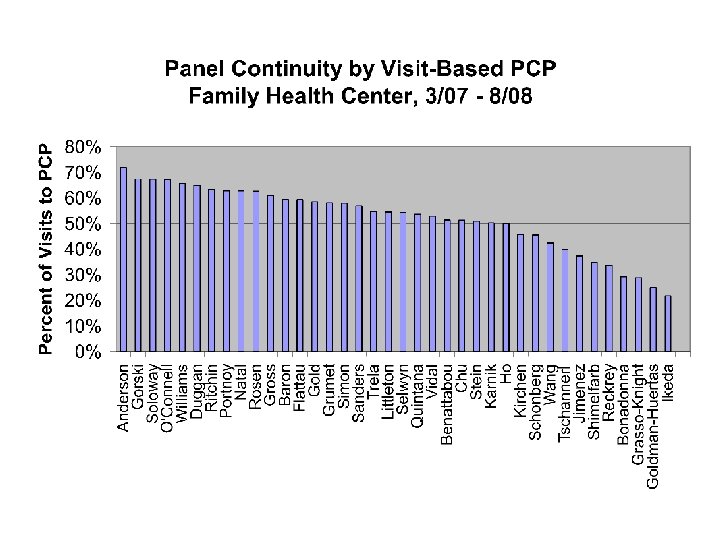
Outcomes of PCP reassignment n Measuring continuity of care n From the physician’s perspective n n During a given interval (e. g. 18 months), what percent of all visits with each provider are with members of that provider’s own panel? What percent of all visits with each provider are devoted to cross-coverage of other providers’ patients?

Conclusions n n Meaningful patient panels can be constructed from retrospective visit histories in the hospital database Panel lists have many potential applications: n n Characterization, balance, and rational transfer of resident panels Accountability for patient care and outcomes Correction of panel sizes to balance productivity and access Measurement of continuity
Questions for discussion n Can you assign a meaningful PCP to each patient in your practice? Can you generate a list of all the patients in each provider’s panel? If you have (or could have) this data, how do (or would) you use it?