Using Learning Teams for Reflective Adaptation A Quality
- Slides: 19
Using Learning Teams for Reflective Adaptation: A Quality Improvement Intervention to Enhance Diabetes and Hypertension Care in Primary Care Practices Bijal Balasubramanian, MBBS, MPH Sabrina Chase, Ph. D, Pamela Ohman-Strickland, Ph. D, Jesse C. Crosson, Ph. D, Paul Nutting, MD, MPH, Benjamin F. Crabtree, Ph. D UMDNJ-Robert Wood Johnson Medical School
Background n Intervention trials to enhance adherence to evidence-based guidelines have resulted in modest or no improvement n Barriers to compliance with clinical guidelines differ from setting to setting n Greater individualization of intervention strategies based on understanding of local barriers is needed
Practices as Complex Adaptive Systems n Practices evolve locally with communities to meet the particular needs of patients. ü Miller WL, Crabtree BF, Mc. Daniel R, Stange KC. Understanding change in primary care practice using complexity theory. J Fam Pract 1998; 46: 369 -376. n Important features of practices that make them unique: • • History & initial conditions (founder’s vision & how things got started) Particular agents (people) and patterns of interaction Local fitness landscape (local community and environment) Regional and global influences ü Miller WL, Mc. Daniel RR, Crabtree BF, Stange KC. Practice jazz: understanding variation in family practices using complexity science. J Fam Pract, 2001; 50(10): 872 -8.
Change in emphasis: n Instead of a vision that focuses on improved components and improved measurement to improve patient outcomes; n To have a vision that focuses on increased capacity for learning, improved systems, and richer connections and relationships that can improve patient outcomes.
Change in emphasis: n Instead of encouraging leadership to create a better run organization with increased efficiency and effectiveness (e. g. , predictability, and control); n Leadership needs to optimize the potential to co- evolve in ways that increase organizational fitness.
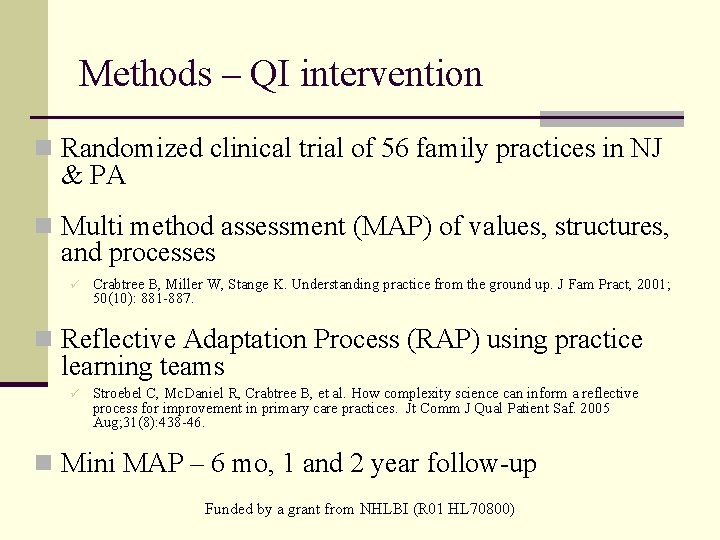
Methods – QI intervention n Randomized clinical trial of 56 family practices in NJ & PA n Multi method assessment (MAP) of values, structures, and processes ü Crabtree B, Miller W, Stange K. Understanding practice from the ground up. J Fam Pract, 2001; 50(10): 881 -887. n Reflective Adaptation Process (RAP) using practice learning teams ü Stroebel C, Mc. Daniel R, Crabtree B, et al. How complexity science can inform a reflective process for improvement in primary care practices. Jt Comm J Qual Patient Saf. 2005 Aug; 31(8): 438 -46. n Mini MAP – 6 mo, 1 and 2 year follow-up Funded by a grant from NHLBI (R 01 HL 70800)
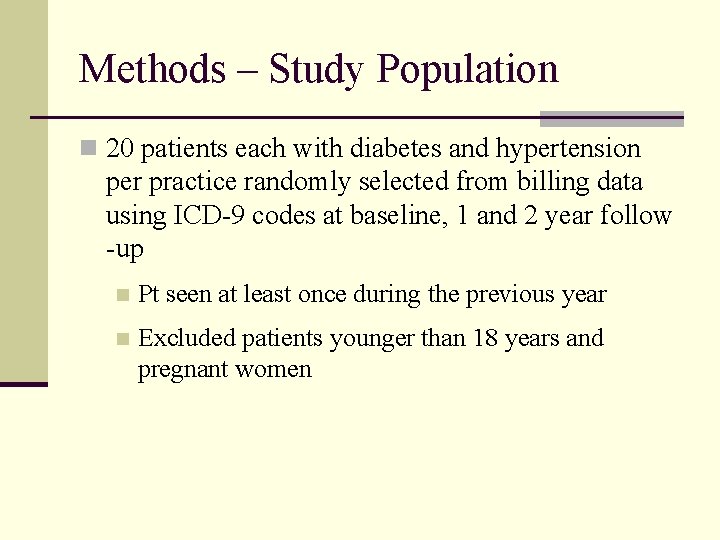
Methods – Study Population n 20 patients each with diabetes and hypertension per practice randomly selected from billing data using ICD-9 codes at baseline, 1 and 2 year follow -up n Pt seen at least once during the previous year n Excluded patients younger than 18 years and pregnant women
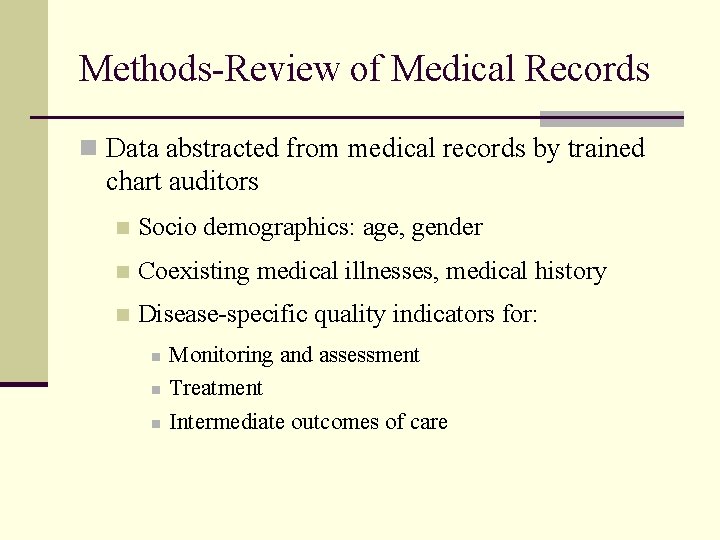
Methods-Review of Medical Records n Data abstracted from medical records by trained chart auditors n Socio demographics: age, gender n Coexisting medical illnesses, medical history n Disease-specific quality indicators for: n n n Monitoring and assessment Treatment Intermediate outcomes of care
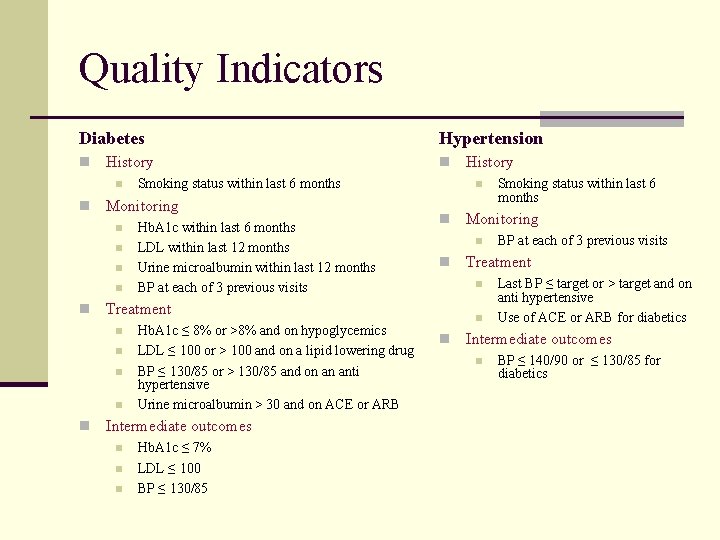
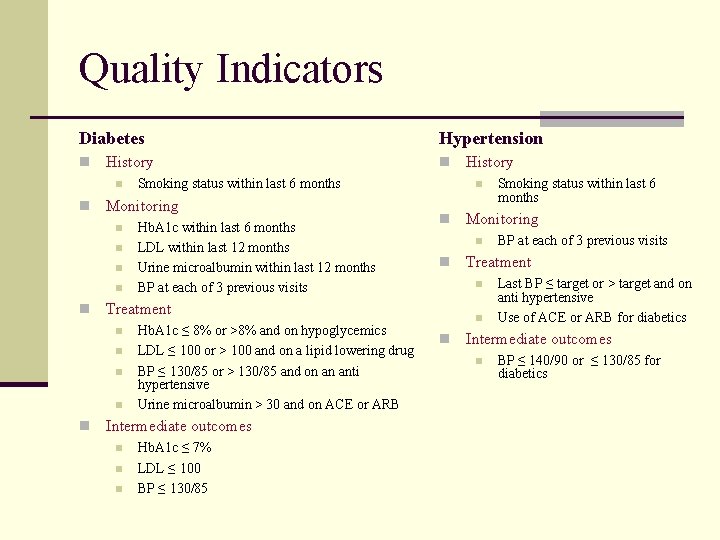
Quality Indicators Diabetes n History n n n Hb. A 1 c within last 6 months LDL within last 12 months Urine microalbumin within last 12 months BP at each of 3 previous visits n n n Hb. A 1 c ≤ 8% or >8% and on hypoglycemics LDL ≤ 100 or > 100 and on a lipid lowering drug BP ≤ 130/85 or > 130/85 and on an anti hypertensive Urine microalbumin > 30 and on ACE or ARB Intermediate outcomes n n n Hb. A 1 c ≤ 7% LDL ≤ 100 BP ≤ 130/85 History n n n BP at each of 3 previous visits Treatment n n n Smoking status within last 6 months Monitoring n Hypertension Last BP ≤ target or > target and on anti hypertensive Use of ACE or ARB for diabetics Intermediate outcomes n BP ≤ 140/90 or ≤ 130/85 for diabetics
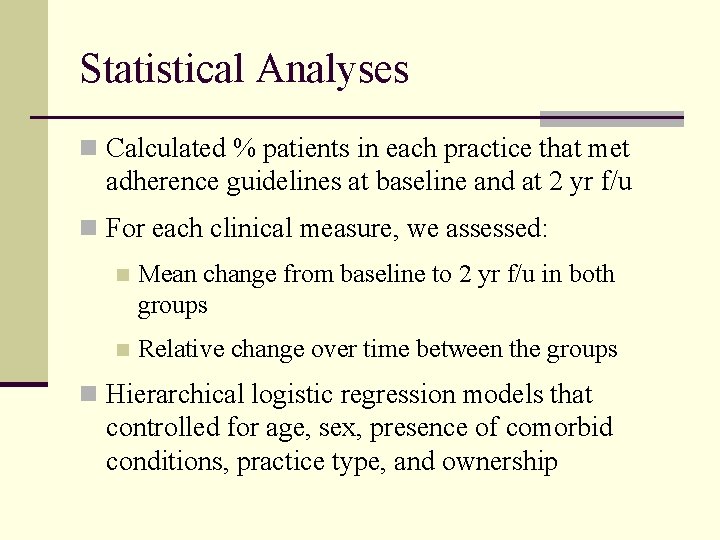
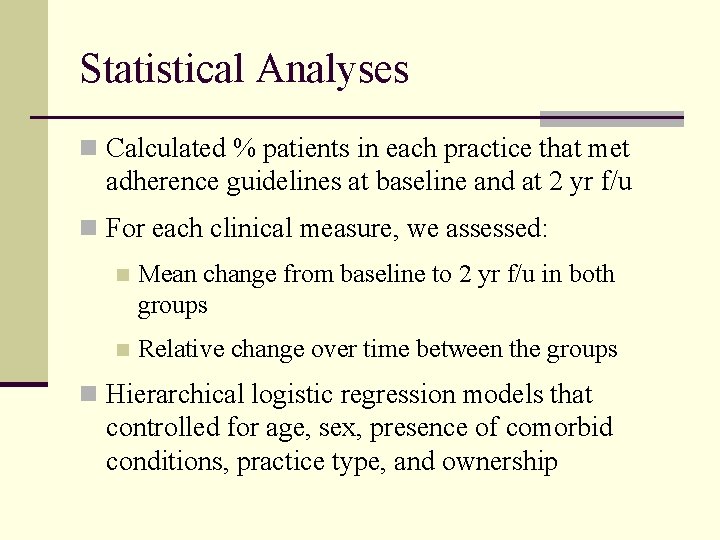
Statistical Analyses n Calculated % patients in each practice that met adherence guidelines at baseline and at 2 yr f/u n For each clinical measure, we assessed: n Mean change from baseline to 2 yr f/u in both groups n Relative change over time between the groups n Hierarchical logistic regression models that controlled for age, sex, presence of comorbid conditions, practice type, and ownership
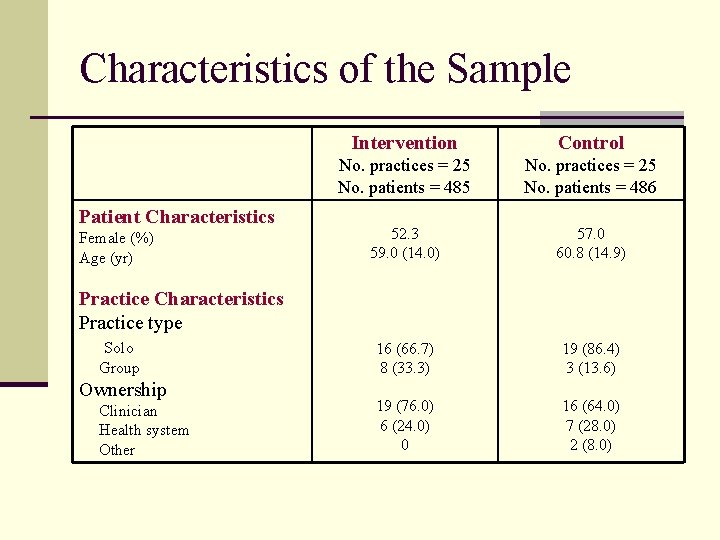
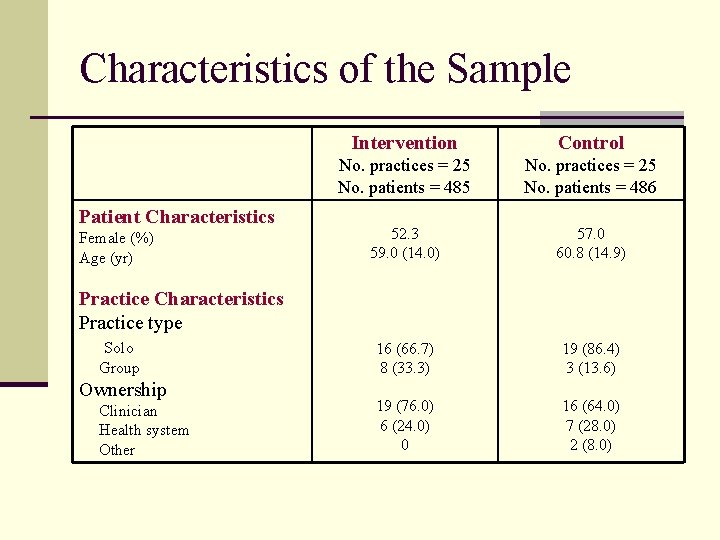
Characteristics of the Sample Patient Characteristics Female (%) Age (yr) Intervention Control No. practices = 25 No. patients = 485 No. practices = 25 No. patients = 486 52. 3 59. 0 (14. 0) 57. 0 60. 8 (14. 9) 16 (66. 7) 8 (33. 3) 19 (86. 4) 3 (13. 6) 19 (76. 0) 6 (24. 0) 0 16 (64. 0) 7 (28. 0) 2 (8. 0) Practice Characteristics Practice type Solo Group Ownership Clinician Health system Other
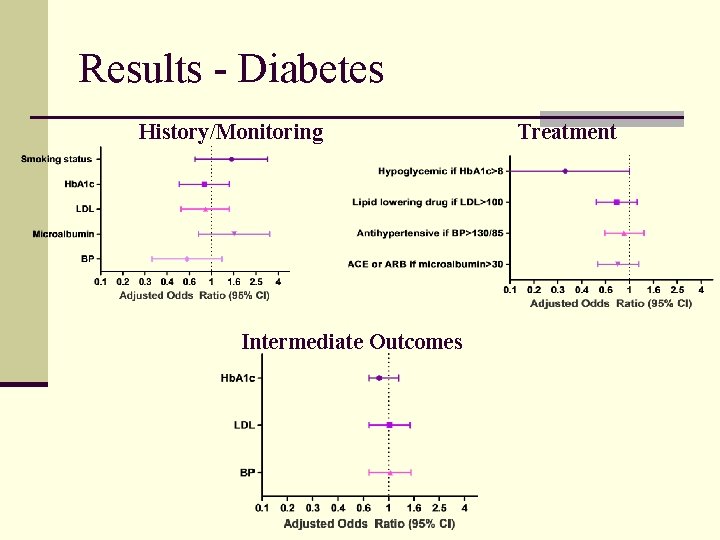
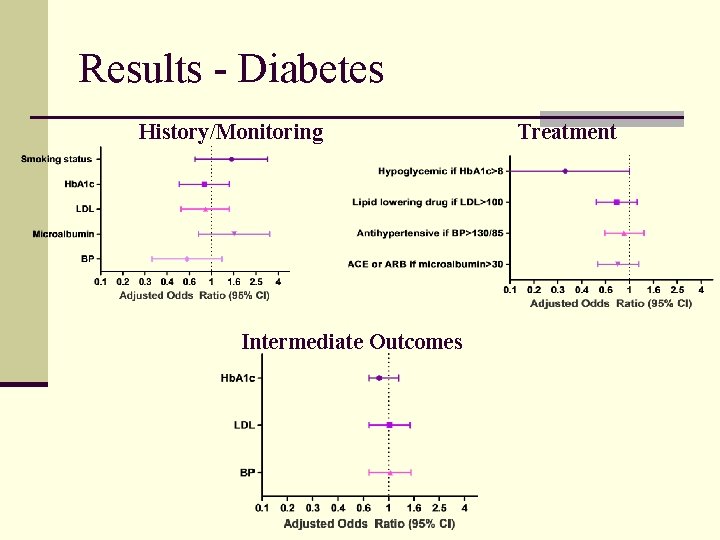
Results - Diabetes History/Monitoring Intermediate Outcomes Treatment
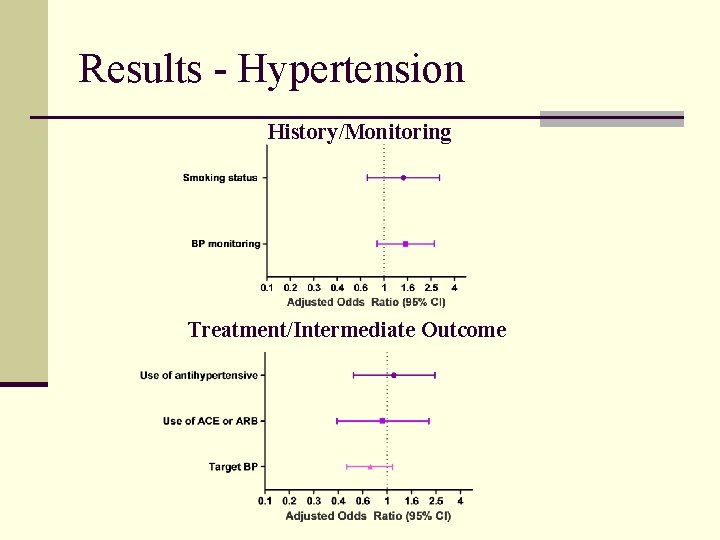
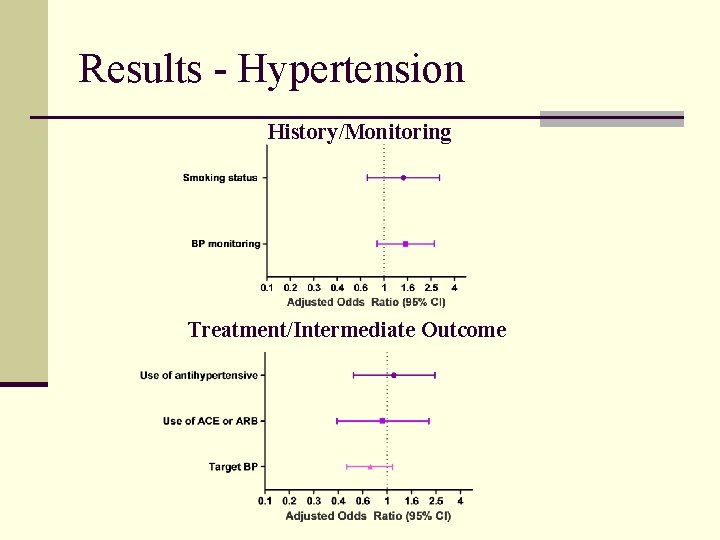
Results - Hypertension History/Monitoring Treatment/Intermediate Outcome
A more in-depth look n There is a wealth of qualitative field notes, RAP recordings, and interview data n These data provide a context to understanding the implementation of the intervention
Practice A n MAP n Large practice on 2 floors n OM – command control personality, gatekeeper of information, power and favor n Lack of teamwork, lack of trust, opaque decision making process
Practice A n RAP n Early In/out tensions; rumored RAP team “hand picked” by OM. Outsider called it “your secretive little group. ” n Dual organization (OM and physician as a power faction). n Mid n First focus: customer service, patient survey n First time that group really connected n Late n n n Physician and OM not a power block anymore. Several issues raised, but team not brainstorming about ways to improve/change things
Practice B n MAP n Small practice, 3 physicians, 1 receptionist, 1 MA, practice values patient care – familiar with patients n Practice purchased a pediatric practice about 10 min away n Communication issues around scheduling n RAP n Early n n generated a long list of potential issues through effective brainstorming initial focus on chart documentation
Practice B n RAP n Mid n n n handling 2 -3 ‘small’ issues every week. Physicians seem very comfortable letting the staff speak up and make suggestions Practice demonstrated commitment to the RAP process RAP occurred at a pivotal moment Late n n Addressed all issues on original list, generated new list based on issues surrounding the new practice Several changes noted § “ … procedures have been written, there are protocols, the flow has improved. Things are coordinated, people are ‘more aware of what’s going on’ “
Discussion n A preliminary look at these data indicate that the intervention addressed practices’ capacity to take on change efforts n Future steps - complete qualitative analyses and integrate the results with the quantitative findings