Using EvidenceBased Practice in Treatment Planning It is
Using Evidence-Based Practice in Treatment Planning
“It is far better to grasp the universe as it really is than to persist in delusion, however satisfying and reassuring. ” Carl Sagan
The need for evidence-based practice Imagine that your own parent or grandparent has been diagnosed with dementia, and is receiving speech-language pathology services for cognitive rehabilitation. You are glad to hear they are receiving services, but when you observe one of their sessions, something seems off to you. The SLP’s treatment seems to consist of having your loved one do crossword puzzles and word searches from a workbook, and encouraging them by saying things like “The brain is a muscle you need to work out, just like going to the gym!” When you ask the SLP about her approach, she says “This is how I’ve been doing cog treatment for 20 years! Why should I change now? ” She assured you she can tell her clients are making progress. How would you respond to this SLP? Why might she think her treatment is effective?
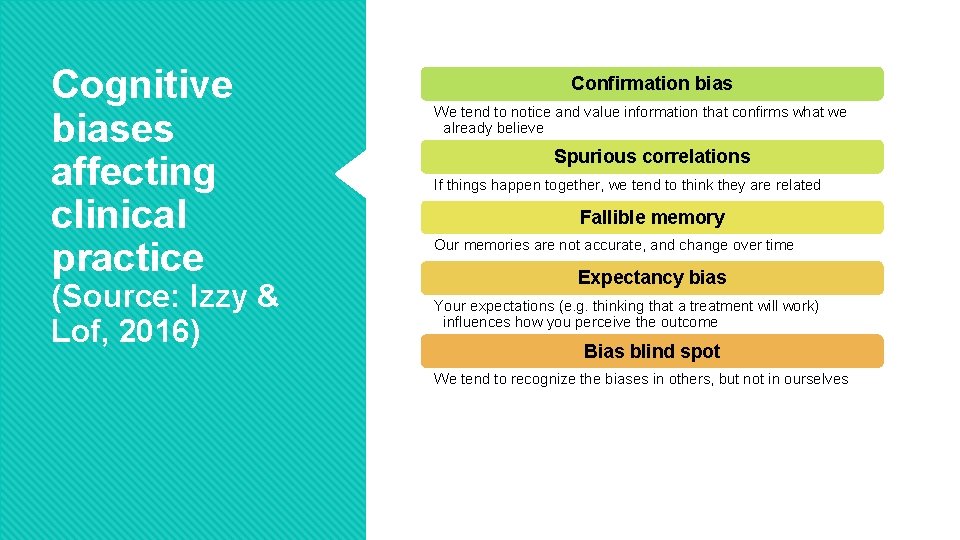
Cognitive biases affecting clinical practice (Source: Izzy & Lof, 2016) Confirmation bias We tend to notice and value information that confirms what we already believe Spurious correlations If things happen together, we tend to think they are related Fallible memory Our memories are not accurate, and change over time Expectancy bias Your expectations (e. g. thinking that a treatment will work) influences how you perceive the outcome Bias blind spot We tend to recognize the biases in others, but not in ourselves

EBP pyramid

EBP Step 1: Framing the question (PICO) Population Intervention Comparison Outcome Older adults with aphasia Early initiation of aphasia treatment Aphasia treatment after initial/spontaneous recovery time Functional communication abilities Kindergarteners with articulation disorders Individual pull-out treatment Group pull-out treatment Ability to consistently produce /s/ Adolescent with a severe head injury Cognitive rehab No cognitive rehab Return to work/school

EBP Step 2: Finding the Evidence Filtered vs. Unfiltered evidence Learning to search databases: e. g. Psych. NET, Pub. MED http: //psycnet. apa. org/search? fa=search. advanced. Search. Form ASHA Evidence Maps http: //www. asha. org/Evidence-Maps/ Many evidence-based clinical practice guidelines already exist To search for a key word (e. g. NMES) in the evidence maps, use the search bar on the right (“Search the Evidence Maps”) You can also click on individual topics

Some EBP resources http: //www. asha. org/Research/EBP/ http: //www. asha. org/Evidence-Maps/ (ASHA Evidence Maps) http: //speechbite. com/ https: //researchguides. uoregon. edu/cds Scottish Intercollegiate Guidelines Network (SIGN) The National Guideline Clearinghouse U. S. Department of Veterans Affairs Academy of Neurologic Communication Disorders and Sciences (ANCDS) National Electronic Library for Health (National Health Service of the UK) The Catalog of Bias https: //catalogofbias. org/

Use ASHA Evidence Maps to Answer the Question Population Adults with mild acquired brain injury Intervention Comparison Internal memory strategies/mnemonics Memory drills/practice https: //www. asha. org/Evidence-Maps/ Outcome Retention/recall of information
EBP Step 3: Assessing the Evidence Systematic Reviews Make sure to consider the specific population you are interested in Notice who wrote and published the review Individual studies Consider level of evidence (see next slide) Consider study quality
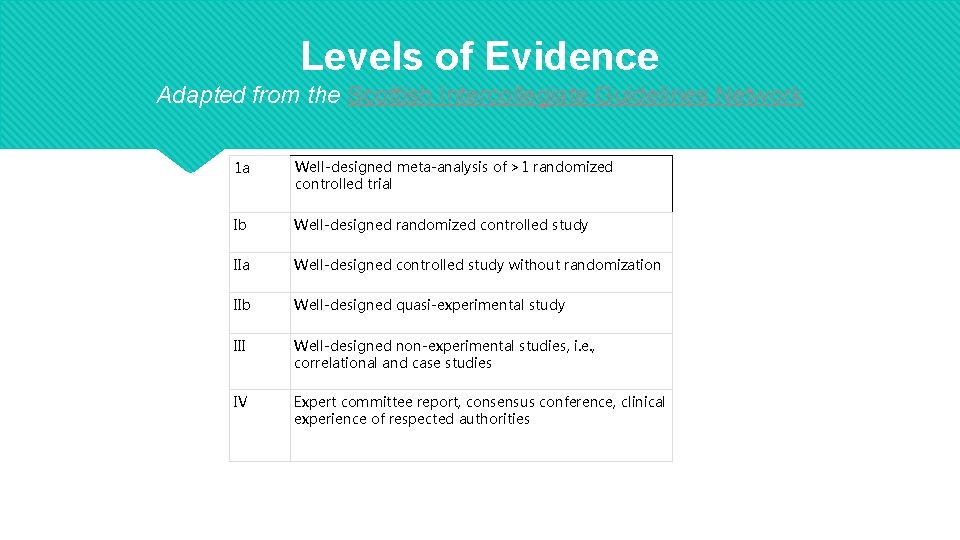
Levels of Evidence Adapted from the Scottish Intercollegiate Guidelines Network 1 a Well-designed meta-analysis of >1 randomized controlled trial Ib Well-designed randomized controlled study IIa Well-designed controlled study without randomization IIb Well-designed quasi-experimental study III Well-designed non-experimental studies, i. e. , correlational and case studies IV Expert committee report, consensus conference, clinical experience of respected authorities
EBP Step 4: Making the Clinical Decision When guidelines exist for your clinical question, it is generally best practice to follow the guidelines When no guidelines exist, you must evaluate the evidence you’ve found critically and make a decision for your client There is no magic formula for determining how much evidence is "enough. " Factors such as patient preference, potential for harm, and availability of alternative treatments all come into play in ultimately making the treatment decision
Critical thinking: Separating good science from bad Pseudoscience describes a methodology, belief or practice that has the trappings of science but does not adhere to the appropriate methodologies of science. Skepticism is a method of examining claims, beliefs and ideas using the scientific method before accepting them as true.
Your Assignment Choose a client and approach you will be using for that client—see the Intervention Selection Table for example approaches. Look for evidence-based treatment recommendations for using that approach with the population your client is in. Read 2 articles summarizing the evidence for your treatment approach. Make a Powerpoint presentation containing between 5 -10 slides covering how you went through all 4 EBP steps to answer your specific PICO question, and presenting what you found out and what you decided to do for your client Give an oral presentation to the group next week. Your oral presentation should be between 5 -8 minutes. Be prepared to answer questions from your peers.
- Slides: 14