Using Appreciative Inquiry for a QSEN Integration Project

- Slides: 18
Using Appreciative Inquiry for a QSEN Integration Project in a Private Urban BSN Program Danielle Walker Ph. D, RN, CNE Caitlin Dodd MSN, RN, CNE Linda Humphries DNP, RN, ACNS-BC, CCRN Gina Alexander Ph. D, MPH, MSN, RN Lynnette Howington DNP, RNC, WHNP-BC, CNL Barb Patten MS, RN, CNE OFFICE OF XYZ

How it all began • Administrative Suggestion – Charges • Taskforce creation – Volunteers with interest in QSEN • Attendance at QSEN conference in 2016
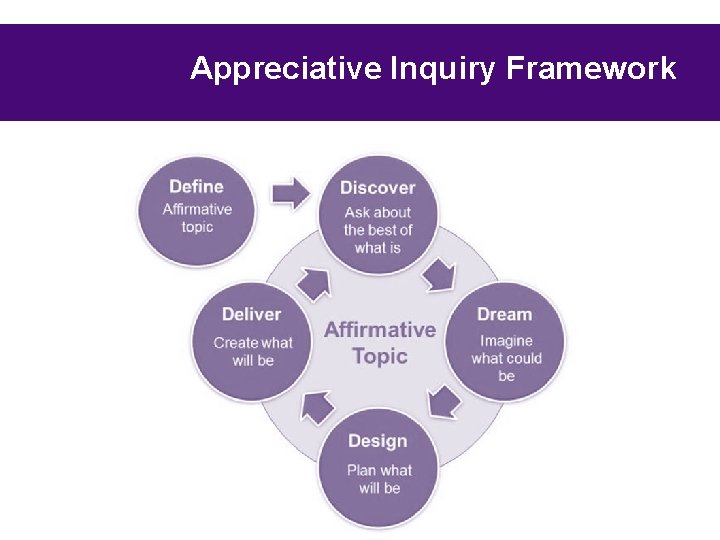
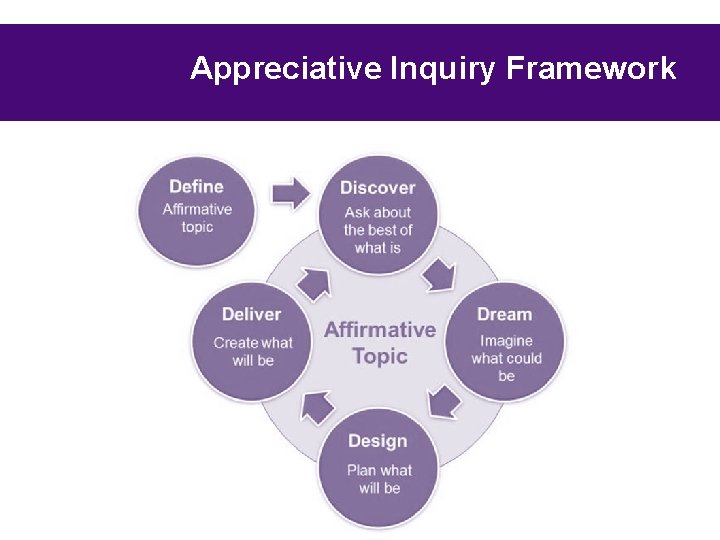
Appreciative Inquiry Framework
How Appreciative Inquiry Impacted our Process • Valued our faculty’s time • Knew that quality and safety was being addressed – How – Where – Common Language • Didn’t want the “just one more thing” mentality
Define • What is QSEN – Faculty education • Creating a common language – Is “Informatics” the same for everyone? – Are these descriptions what you think of? • Invoking a desire to work on QSEN – Why do we care? – Extrinsic motivation – Valuing the contributions already occurring
Discover • Getting buy in • Current measurement methods in place – ATI results • Organizing the discovery process – 1 st attempt – Regroup and Restart
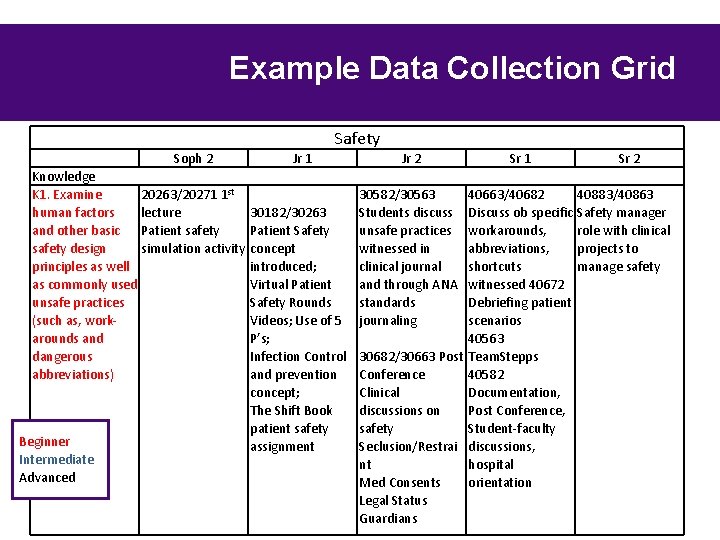
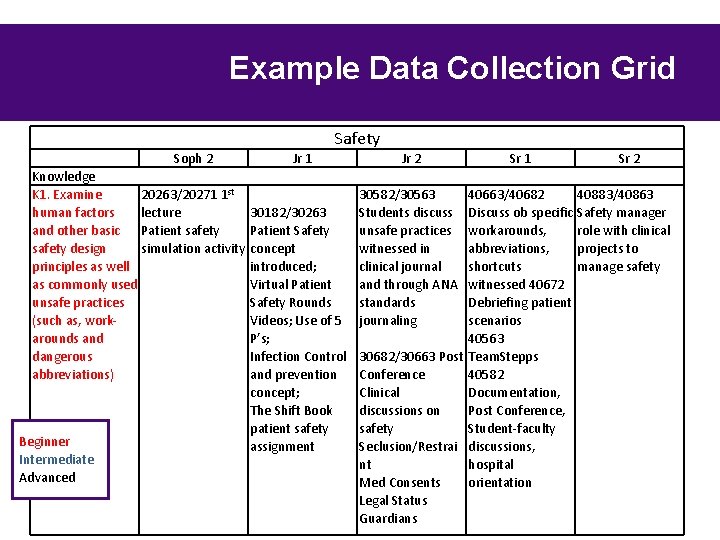
Example Data Collection Grid Safety Soph 2 Knowledge K 1. Examine 20263/20271 1 st human factors lecture and other basic Patient safety design simulation activity principles as well as commonly used unsafe practices (such as, workarounds and dangerous abbreviations) Beginner Intermediate Advanced Jr 1 Jr 2 30582/30563 Students discuss unsafe practices witnessed in clinical journal and through ANA standards journaling Sr 1 Sr 2 40663/40682 40883/40863 30182/30263 Discuss ob specific Safety manager Patient Safety workarounds, role with clinical concept abbreviations, projects to introduced; shortcuts manage safety Virtual Patient witnessed 40672 Safety Rounds Debriefing patient Videos; Use of 5 scenarios P’s; 40563 Infection Control 30682/30663 Post Team. Stepps and prevention Conference 40582 concept; Clinical Documentation, The Shift Book discussions on Post Conference, patient safety Student-faculty assignment Seclusion/Restrai discussions, nt hospital Med Consents orientation Legal Status Guardians
Identification of Gaps • Looked at data collected as a whole • Identified broad areas of overall weakness – The attitudinal domain across all competencies – Evidence Based Practice – Safety – Quality Improvement
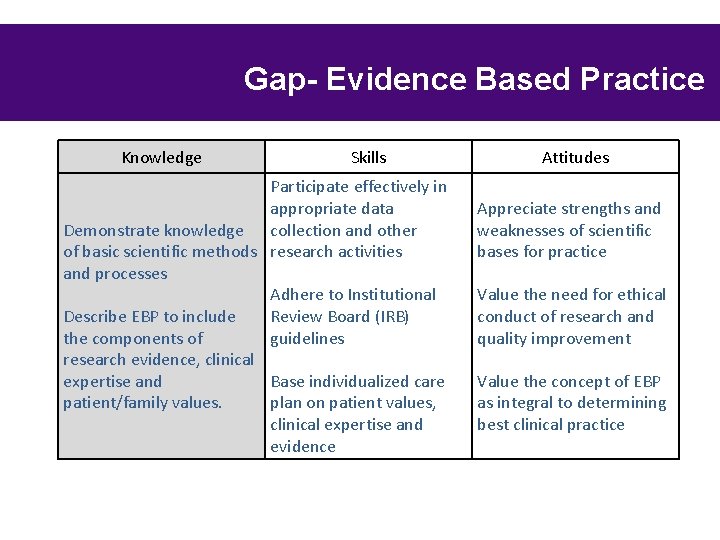
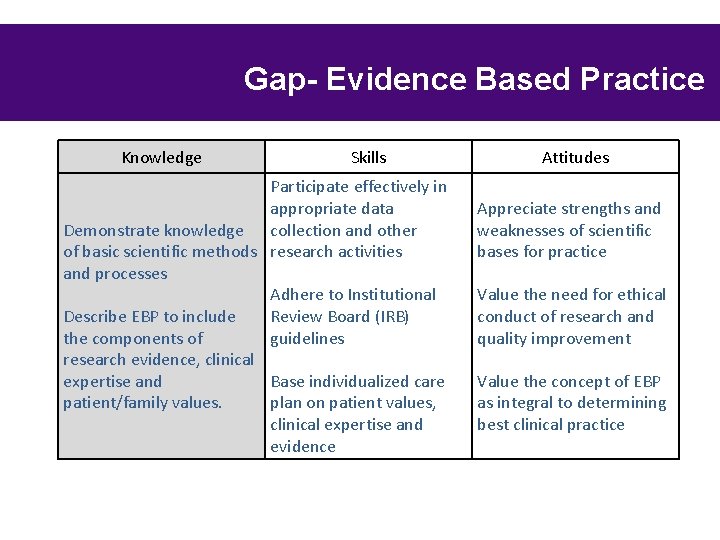
Gap- Evidence Based Practice Knowledge Skills Participate effectively in appropriate data Demonstrate knowledge collection and other of basic scientific methods research activities and processes Adhere to Institutional Review Board (IRB) Describe EBP to include guidelines the components of research evidence, clinical Base individualized care expertise and plan on patient values, patient/family values. clinical expertise and evidence Attitudes Appreciate strengths and weaknesses of scientific bases for practice Value the need for ethical conduct of research and quality improvement Value the concept of EBP as integral to determining best clinical practice
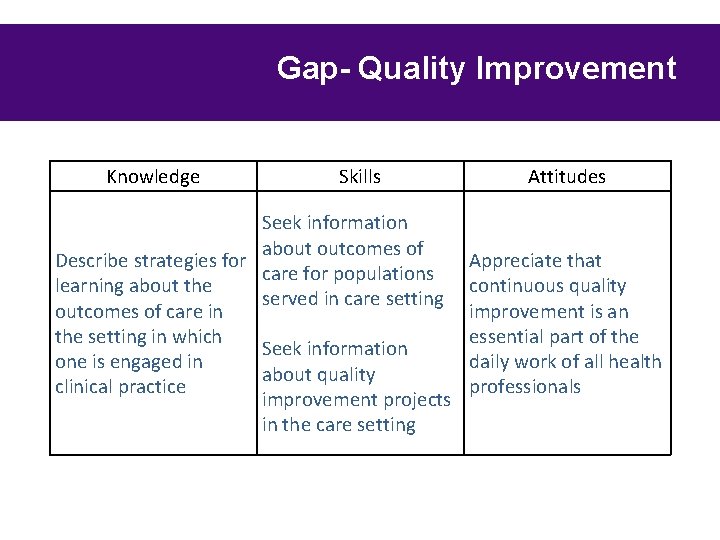
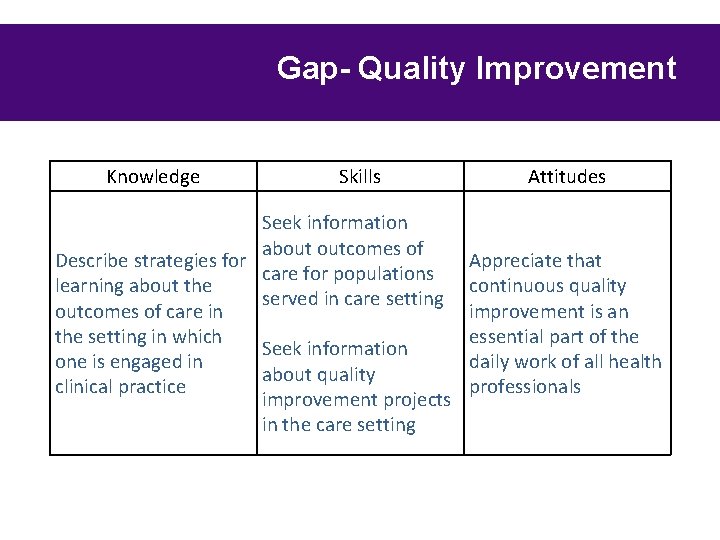
Gap- Quality Improvement Knowledge Skills Seek information about outcomes of Describe strategies for care for populations learning about the served in care setting outcomes of care in the setting in which Seek information one is engaged in about quality clinical practice improvement projects in the care setting Attitudes Appreciate that continuous quality improvement is an essential part of the daily work of all health professionals
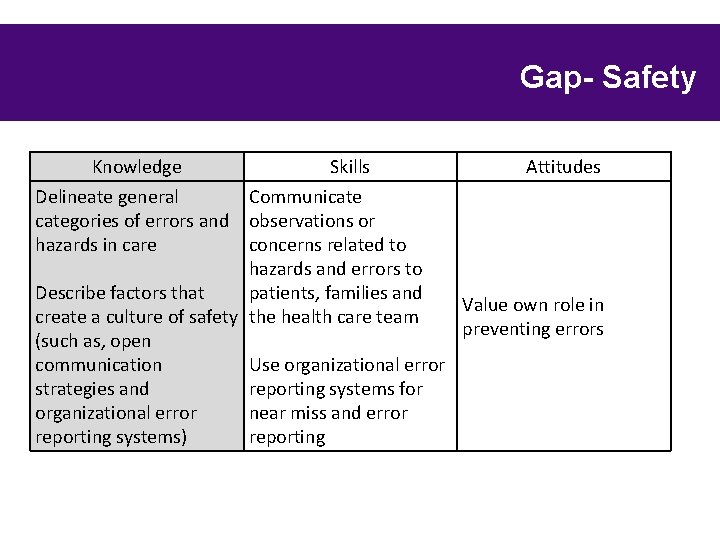
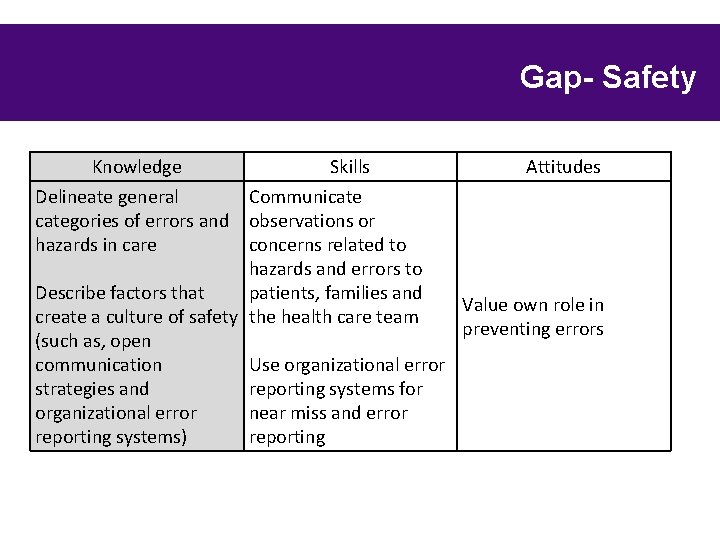
Gap- Safety Knowledge Skills Attitudes Delineate general Communicategories of errors and observations or hazards in care concerns related to hazards and errors to Describe factors that patients, families and Value own role in create a culture of safety the health care team preventing errors (such as, open communication Use organizational error strategies and reporting systems for organizational error near miss and error reporting systems) reporting
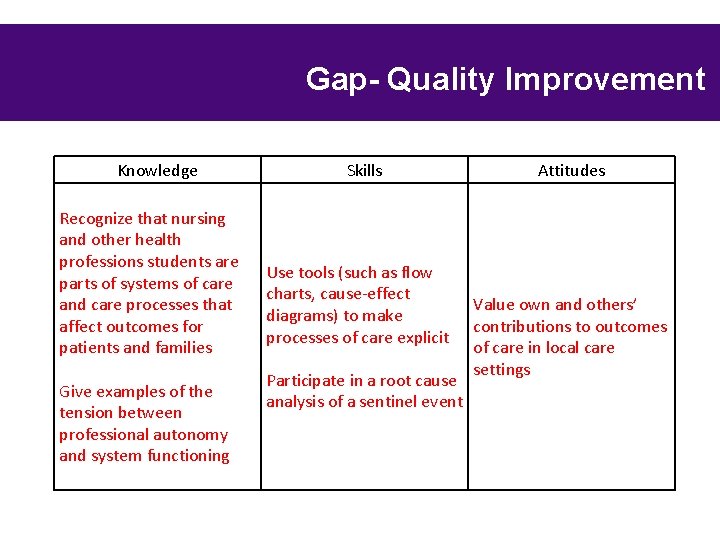
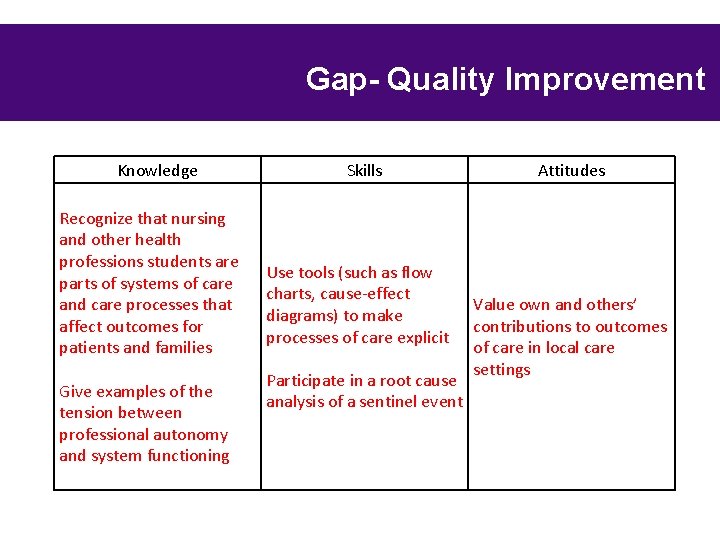
Gap- Quality Improvement Knowledge Recognize that nursing and other health professions students are parts of systems of care and care processes that affect outcomes for patients and families Give examples of the tension between professional autonomy and system functioning Skills Use tools (such as flow charts, cause-effect diagrams) to make processes of care explicit Participate in a root cause analysis of a sentinel event Attitudes Value own and others’ contributions to outcomes of care in local care settings
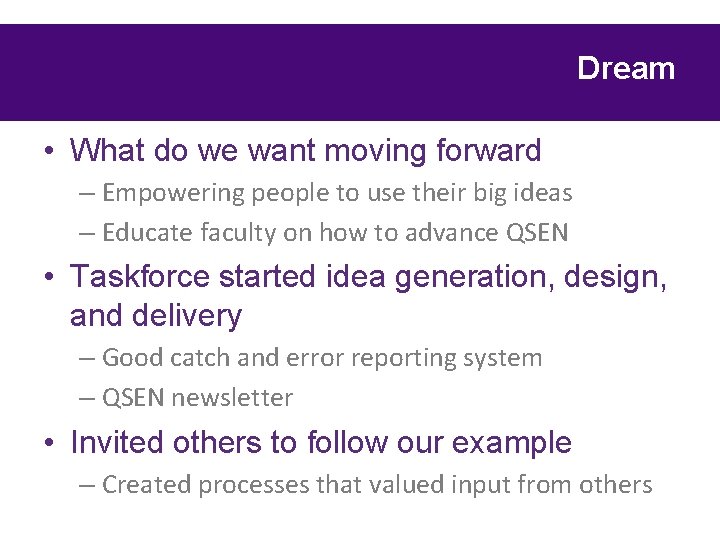
Dream • What do we want moving forward – Empowering people to use their big ideas – Educate faculty on how to advance QSEN • Taskforce started idea generation, design, and delivery – Good catch and error reporting system – QSEN newsletter • Invited others to follow our example – Created processes that valued input from others
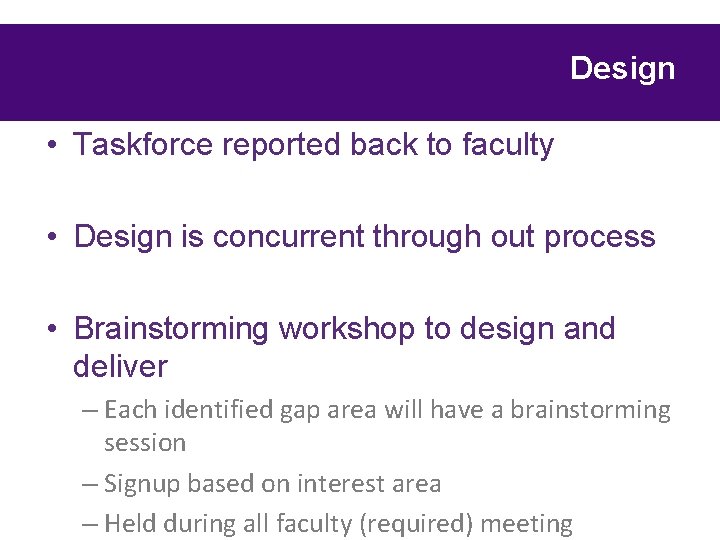
Design • Taskforce reported back to faculty • Design is concurrent through out process • Brainstorming workshop to design and deliver – Each identified gap area will have a brainstorming session – Signup based on interest area – Held during all faculty (required) meeting
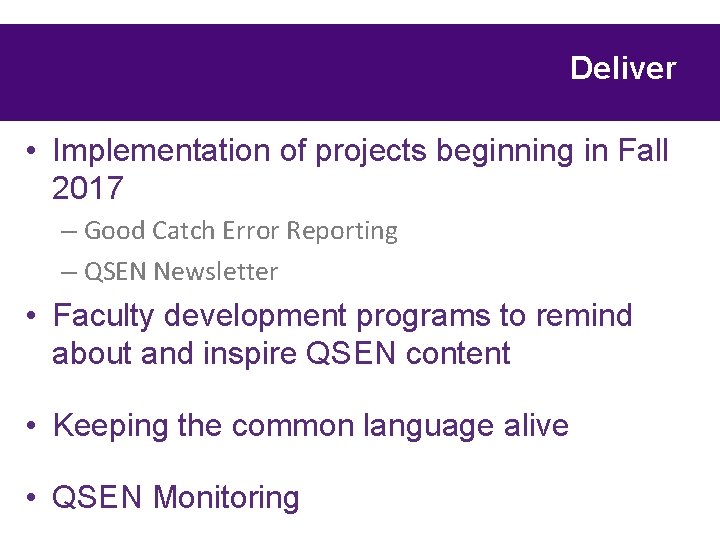
Deliver • Implementation of projects beginning in Fall 2017 – Good Catch Error Reporting – QSEN Newsletter • Faculty development programs to remind about and inspire QSEN content • Keeping the common language alive • QSEN Monitoring
Research We Valued and Used • Barton, A. J. , Armstrong, G. , Preheim, G. , Gelmon, S. B. , & Andrus, L. C. (2009). A national Delphi to determine developmental progression of quality and safety competencies in nursing education. Nursing Outlook, 57(6), 313 -322. doi: 10. 1016/j. outlook. 2009. 08. 003 • Beischel, K. P. , & Davis, D. S. (2014). A Time for Change QSENizing the Curriculum. Nurse Educator, 39(2), 65 -71. doi: 10. 1097/nne. 000000020 • Brady, D. S. (2011). Using Quality and Safety Education for Nurses (QSEN) as a Pedagogical Structure for Course Redesign and Content. International Journal of Nursing Education Scholarship, 8(1). doi: 10. 2202/1548 -923 X. 2147
Questions?