Usefulness of BMD Testing BMD measurement can be
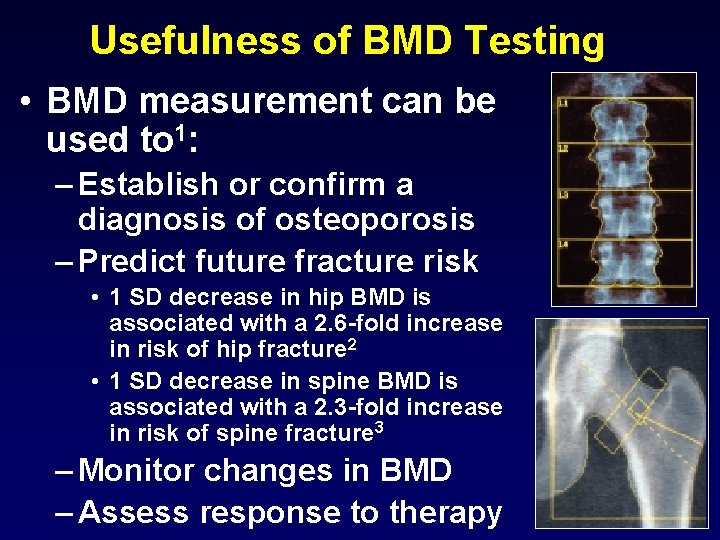
Usefulness of BMD Testing • BMD measurement can be used to 1: – Establish or confirm a diagnosis of osteoporosis – Predict future fracture risk • 1 SD decrease in hip BMD is associated with a 2. 6 -fold increase in risk of hip fracture 2 • 1 SD decrease in spine BMD is associated with a 2. 3 -fold increase in risk of spine fracture 3 – Monitor changes in BMD – Assess response to therapy
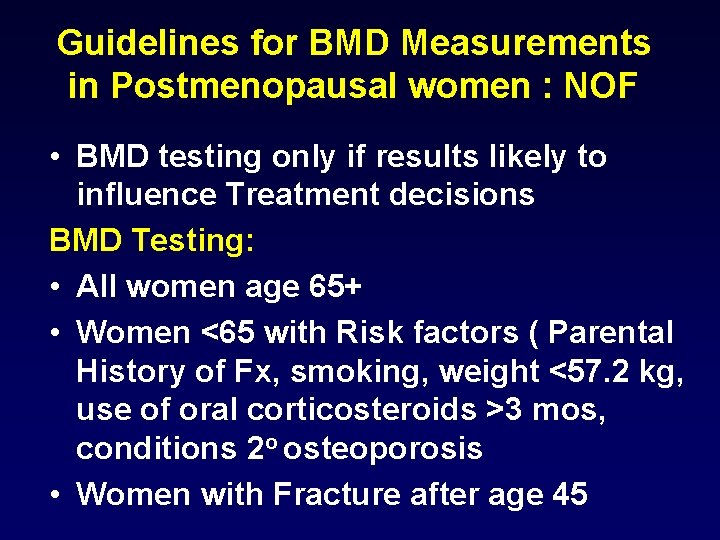
Guidelines for BMD Measurements in Postmenopausal women : NOF • BMD testing only if results likely to influence Treatment decisions BMD Testing: • All women age 65+ • Women <65 with Risk factors ( Parental History of Fx, smoking, weight <57. 2 kg, use of oral corticosteroids >3 mos, conditions 2 o osteoporosis • Women with Fracture after age 45
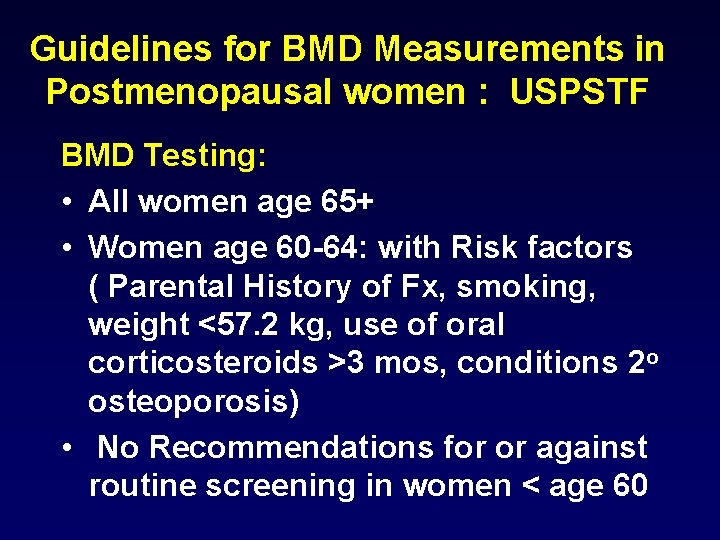
Guidelines for BMD Measurements in Postmenopausal women : USPSTF BMD Testing: • All women age 65+ • Women age 60 -64: with Risk factors ( Parental History of Fx, smoking, weight <57. 2 kg, use of oral corticosteroids >3 mos, conditions 2 o osteoporosis) • No Recommendations for or against routine screening in women < age 60
4
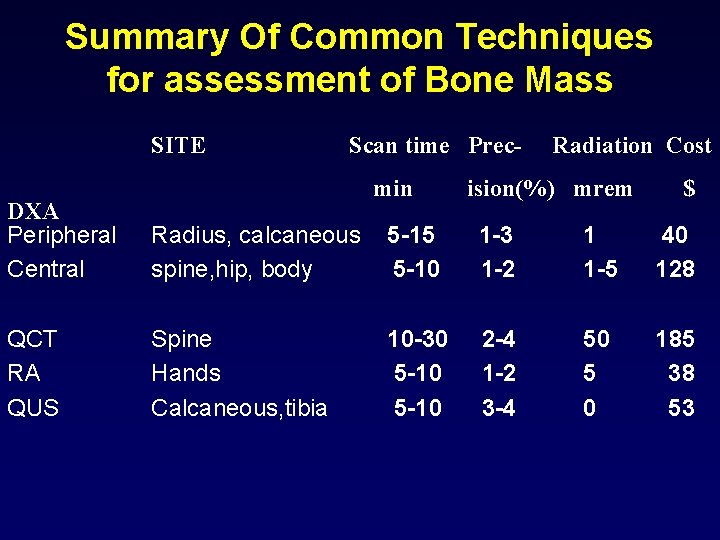
Summary Of Common Techniques for assessment of Bone Mass SITE Scan time Precmin Radiation Cost ision(%) mrem $ DXA Peripheral Central Radius, calcaneous spine, hip, body 5 -15 5 -10 1 -3 1 -2 1 1 -5 40 128 QCT RA QUS Spine Hands Calcaneous, tibia 10 -30 5 -10 2 -4 1 -2 3 -4 50 5 0 185 38 53
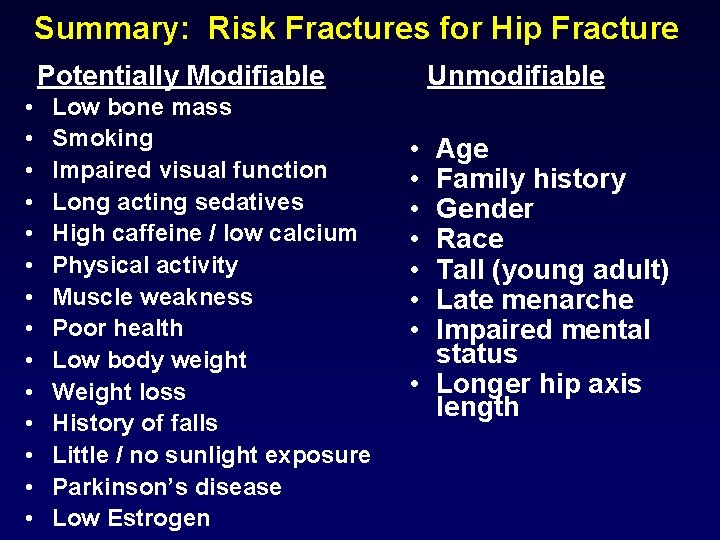
Summary: Risk Fractures for Hip Fracture Potentially Modifiable • • • • Low bone mass Smoking Impaired visual function Long acting sedatives High caffeine / low calcium Physical activity Muscle weakness Poor health Low body weight Weight loss History of falls Little / no sunlight exposure Parkinson’s disease Low Estrogen Unmodifiable • • Age Family history Gender Race Tall (young adult) Late menarche Impaired mental status • Longer hip axis length 6
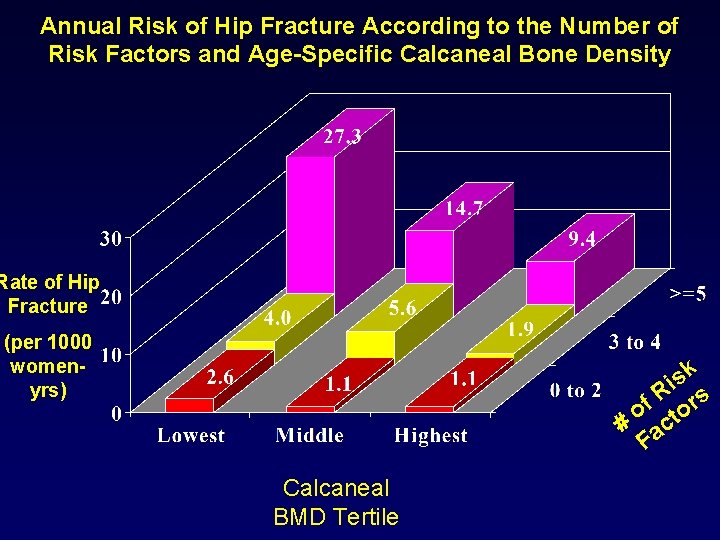
Annual Risk of Hip Fracture According to the Number of Risk Factors and Age-Specific Calcaneal Bone Density Rate of Hip Fracture (per 1000 womenyrs) sk i R rs f o o # act F Calcaneal BMD Tertile
What is Our Desired Outcome in Osteoporosis? Fracture Reduction Fractures are the cause of osteoporosis morbidity and mortality!
Conclusions Key is Prevention • Maximize Peak Skeletal Mass • Prevent or Slow-down Rates of Bone Loss • Prevent Falls
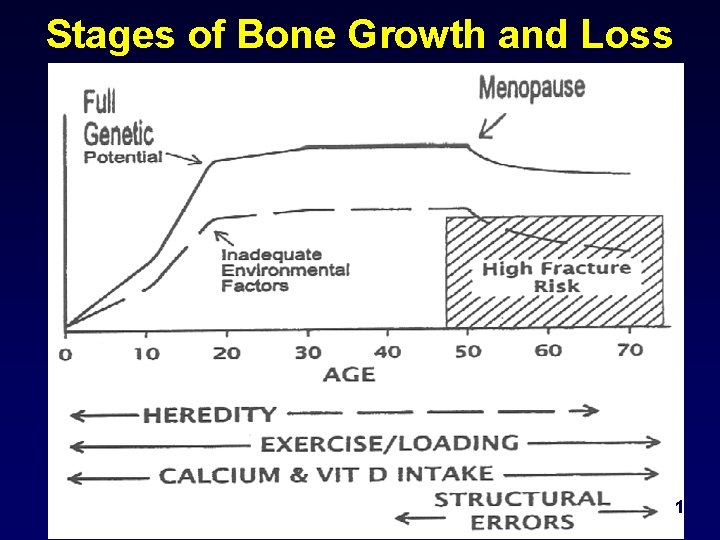
Stages of Bone Growth and Loss 10
Enhance the Development of Peak Bone Mass • Proper Nutrition • Exercise • Avoidance of Premenopausal Estrogen Deficiency • No Smoking or Excessive Alcohol • Subgroups at High Risk (cystic fibrosis, ? asthma, IBD, celiac, Hypo-gonadism, anorexia) 11
Strategies to Reduce Fracture Incidence Population Approach • Influence the Overall Distribution of BMD • Adequate dietary calcium: 1200 mg/day • Vitamin D: 400 to 800 IU • Exercise • Stop smoking 12
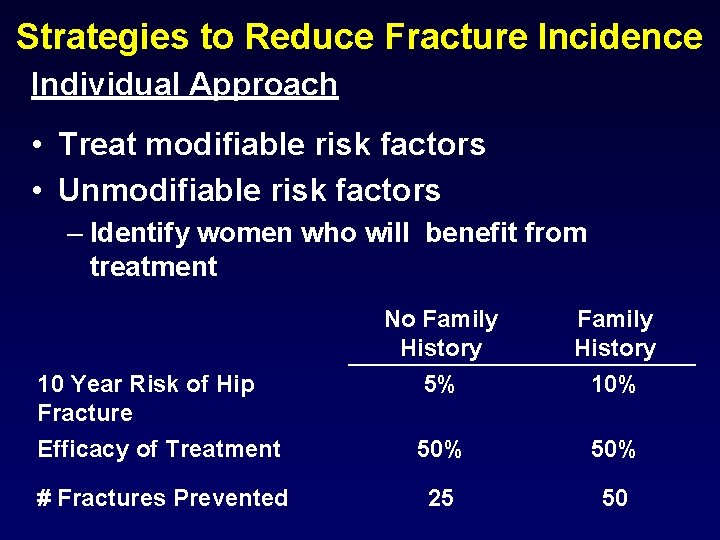
Strategies to Reduce Fracture Incidence Individual Approach • Treat modifiable risk factors • Unmodifiable risk factors – Identify women who will benefit from treatment No Family History 10 Year Risk of Hip Fracture Efficacy of Treatment 5% 10% 50% # Fractures Prevented 25 50
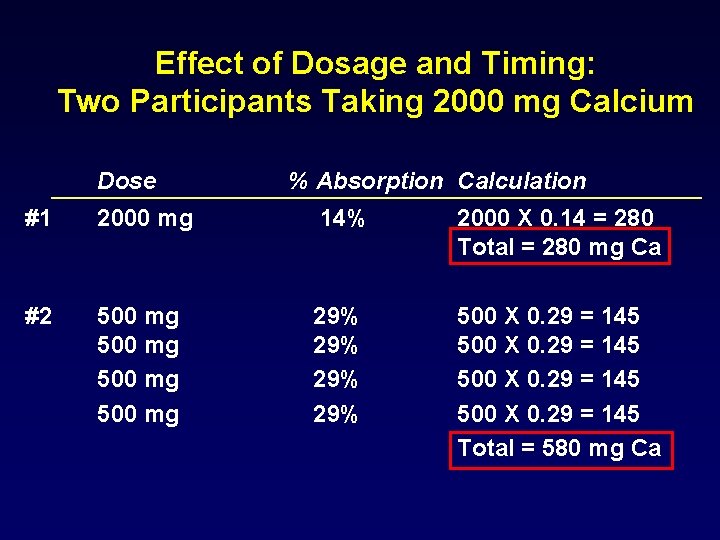
Effect of Dosage and Timing: Two Participants Taking 2000 mg Calcium Dose % Absorption Calculation #1 2000 mg 14% 2000 X 0. 14 = 280 Total = 280 mg Ca #2 500 mg 29% 29% 500 X 0. 29 = 145 Total = 580 mg Ca 14
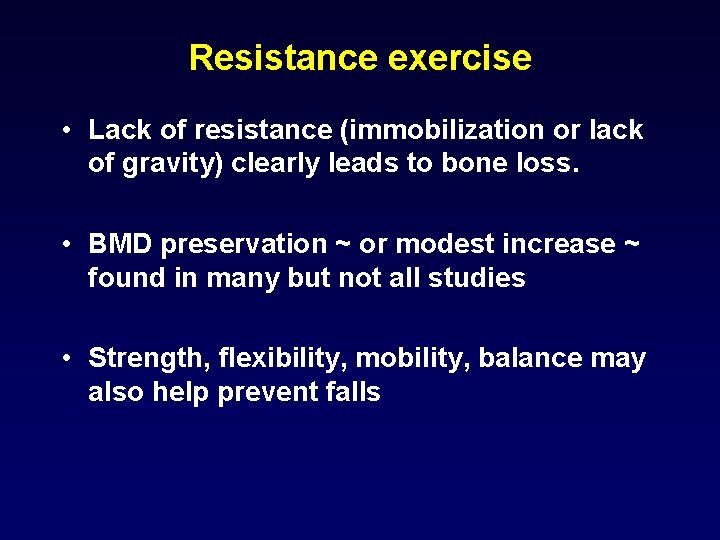
Resistance exercise • Lack of resistance (immobilization or lack of gravity) clearly leads to bone loss. • BMD preservation ~ or modest increase ~ found in many but not all studies • Strength, flexibility, mobility, balance may also help prevent falls
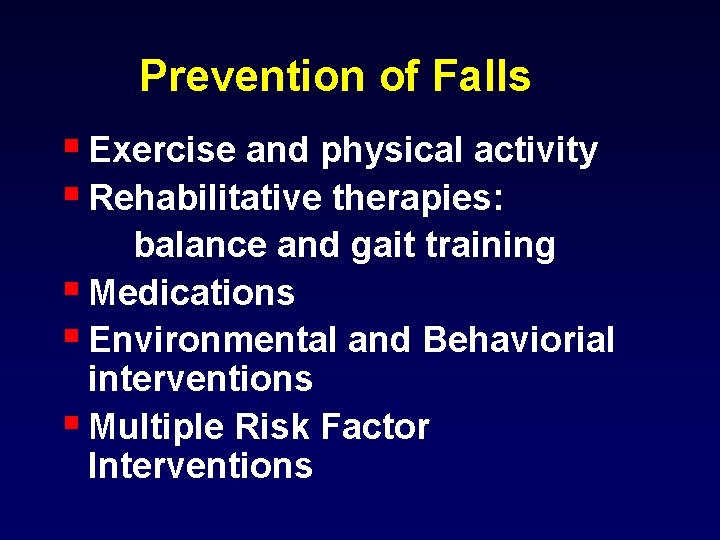
Prevention of Falls § Exercise and physical activity § Rehabilitative therapies: balance and gait training § Medications § Environmental and Behaviorial interventions § Multiple Risk Factor Interventions
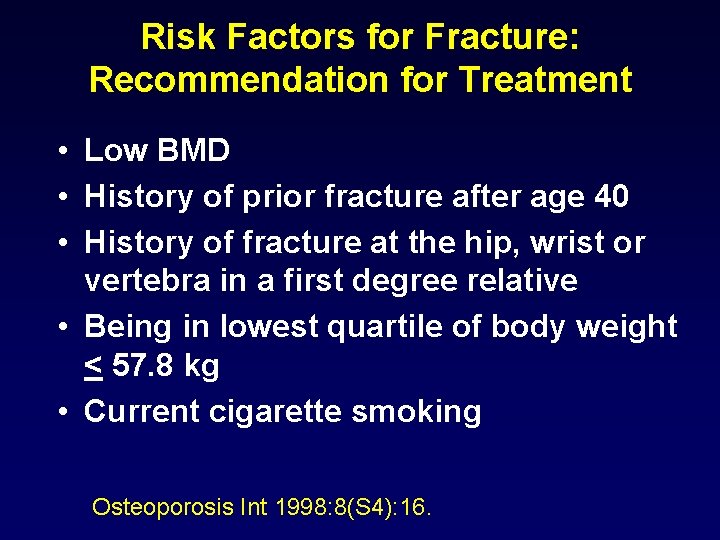
Risk Factors for Fracture: Recommendation for Treatment • Low BMD • History of prior fracture after age 40 • History of fracture at the hip, wrist or vertebra in a first degree relative • Being in lowest quartile of body weight < 57. 8 kg • Current cigarette smoking Osteoporosis Int 1998: 8(S 4): 16.
The 2001 NIH Consensus Panel: • “There is not yet good evidence to support the efficacy of early initiation of preventive drugs…”
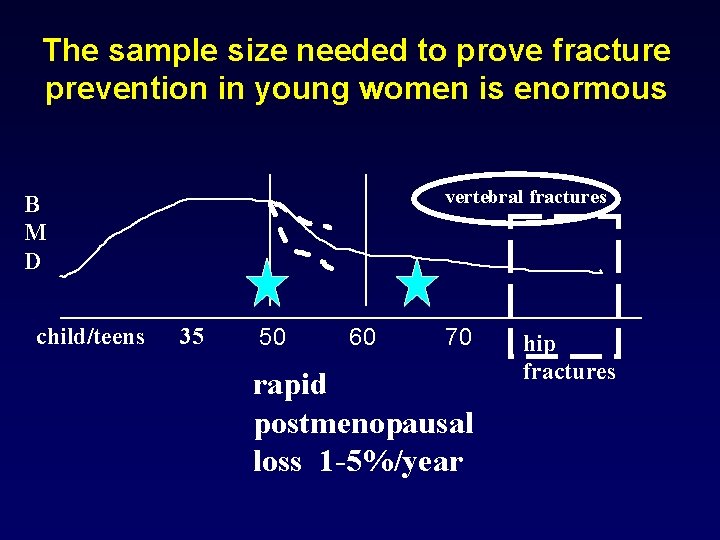
The sample size needed to prove fracture prevention in young women is enormous vertebral fractures B M D child/teens 35 50 60 70 rapid postmenopausal loss 1 -5%/year hip fractures 19
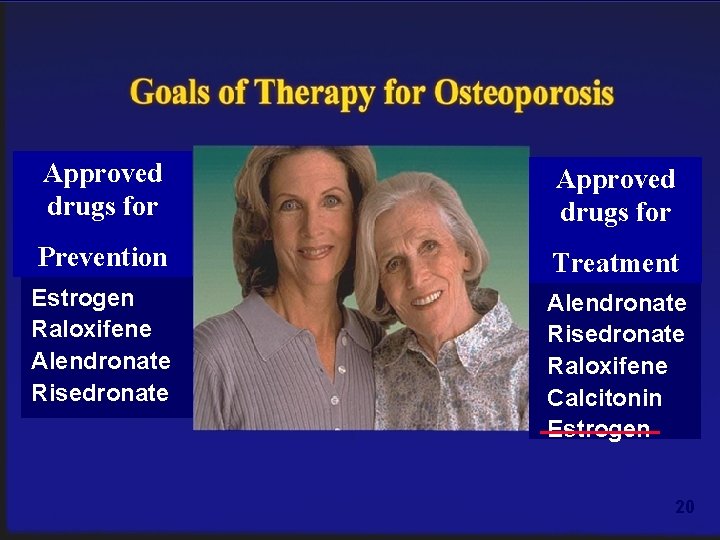
Approved drugs for Prevention Treatment Estrogen Raloxifene Alendronate Risedronate Raloxifene Calcitonin Estrogen 20
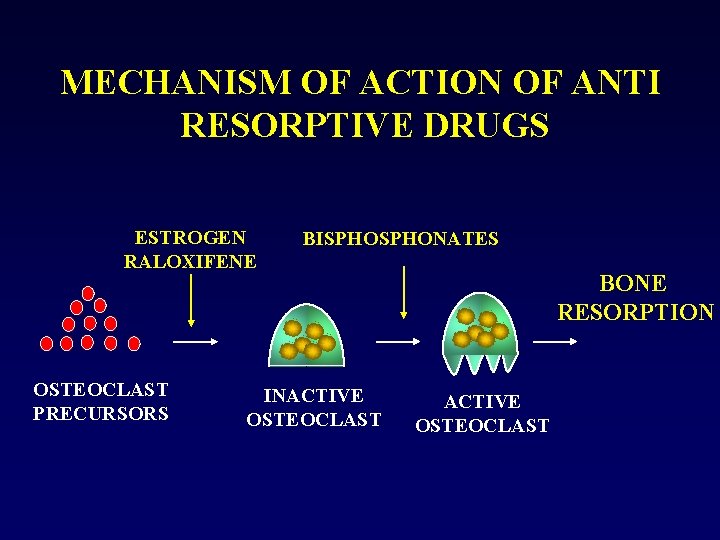
MECHANISM OF ACTION OF ANTI RESORPTIVE DRUGS ESTROGEN RALOXIFENE OSTEOCLAST PRECURSORS BISPHONATES INACTIVE OSTEOCLAST BONE RESORPTION ACTIVE OSTEOCLAST 21

HRT
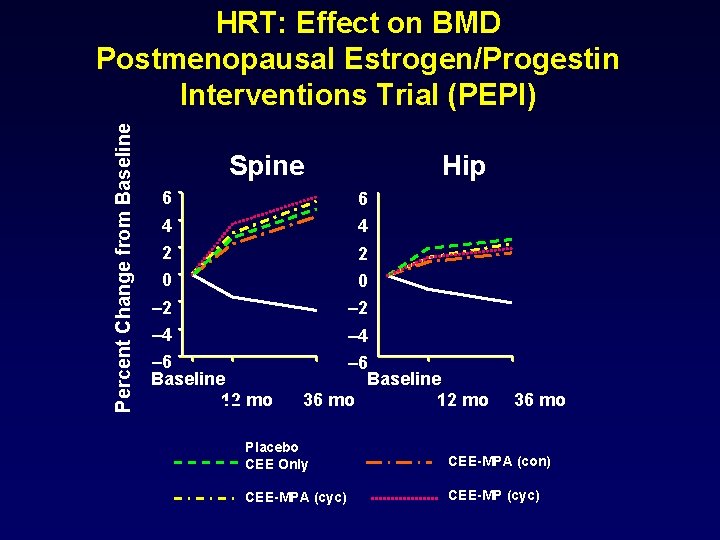
Percent Change from Baseline HRT: Effect on BMD Postmenopausal Estrogen/Progestin Interventions Trial (PEPI) Spine Hip 6 6 4 4 2 0 – 2 – 4 – 6 Baseline 12 mo – 6 Baseline 36 mo 12 mo 36 mo Placebo CEE Only CEE-MPA (con) CEE-MPA (cyc) CEE-MP (cyc) 23
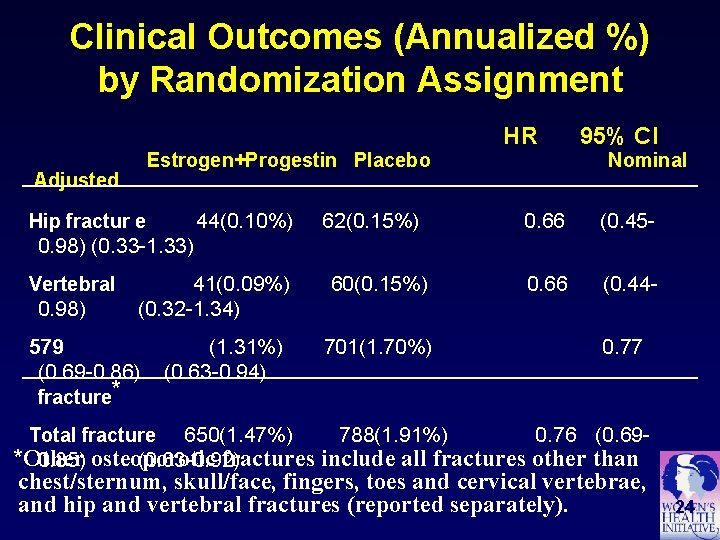
Clinical Outcomes (Annualized %) by Randomization Assignment Estrogen+Progestin Placebo Adjusted 44(0. 10%) Hip fractur e 62(0. 15%) HR 95% CI Nominal 0. 66 (0. 45 - 0. 66 (0. 44 - 0. 98) (0. 33 -1. 33) Vertebral 0. 98) 41(0. 09%) (0. 32 -1. 34) 579 (0. 69 -0. 86) fracture* (1. 31%) (0. 63 -0. 94) 60(0. 15%) 701(1. 70%) 0. 77 650(1. 47%) 788(1. 91%) 0. 76 (0. 69*Other fractures include all fractures other than 0. 85) osteoporotic (0. 63 -0. 92) Total fracture chest/sternum, skull/face, fingers, toes and cervical vertebrae, and hip and vertebral fractures (reported separately). 24
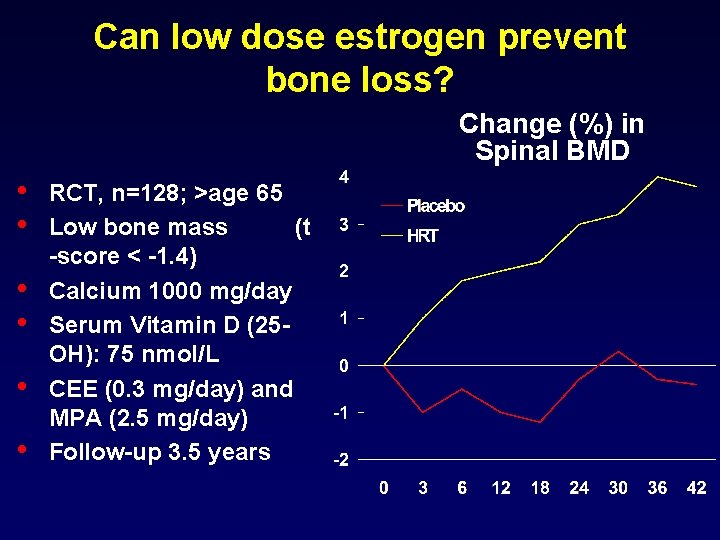
Can low dose estrogen prevent bone loss? Change (%) in Spinal BMD • • • RCT, n=128; >age 65 Low bone mass (t -score < -1. 4) Calcium 1000 mg/day Serum Vitamin D (25 OH): 75 nmol/L CEE (0. 3 mg/day) and MPA (2. 5 mg/day) Follow-up 3. 5 years 25
WHI Estrogen+Progestin Trial Implications • Estrogen plus progestin should not be initiated or continued for the primary prevention of chronic disease in healthy women • The risks for CHD, stroke, PE and breast cancer must be weighed against the benefit for fracture in selecting from the available agents to prevent osteoporosis
- Slides: 26