Use of the EHR in Treatment Prevention of



- Slides: 55
Use of the EHR in Treatment & Prevention of Sepsis Melissa Arnold, MBA, BSN, RN System Director, Clinical Informatics Providence St. Joseph Health
Disclosure • I have no actual or potential conflict of interest in relation to this presentation
Agenda • • • Sepsis Collaborative Meditech EHR Toolkit Program ED and Inpatient Workflow Maternal Sepsis Outcomes
Clinical Excellence • SJH Senior Leadership determined that we needed to move performance improvement to the next level: – More direct impact to clinical care- quality improvement and cost reduction – Physician leaders; hospital provides resources – Data and Best Practice driven • Dispel the notion we can’t improve quality and patient engagement while reducing cost
Why Sepsis Matters • Highest mortality • Debility and/or disability for survivor • Risk - chronic diseases - COPD, CHF, cancer, dementia, immune compromised • Hospitals are faulted if sepsis is not prevented in-house • Better quality & outcomes leads to lower cost • Conversion of negative contribution margin to positive contribution margin
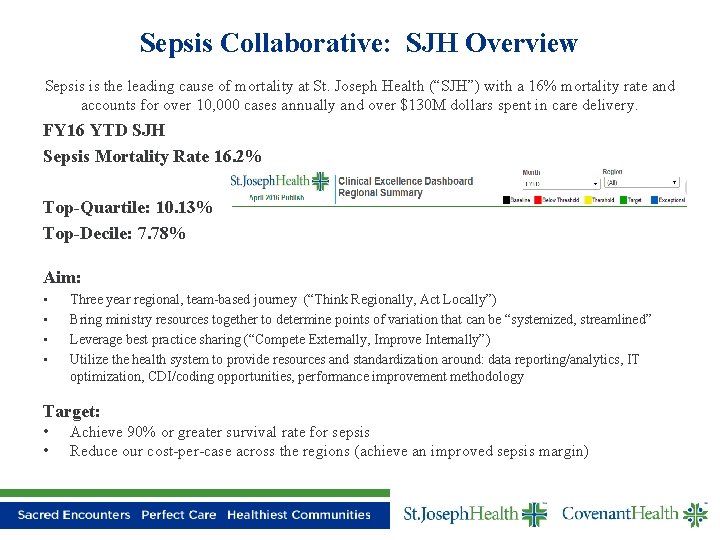
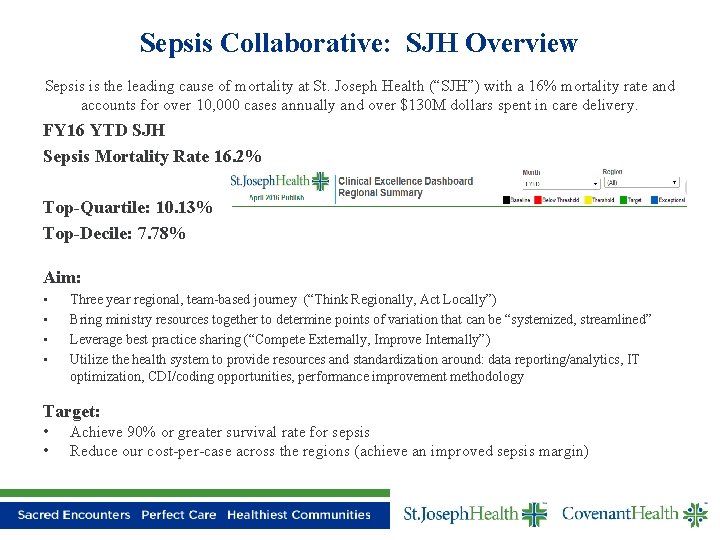
Sepsis Collaborative: SJH Overview Sepsis is the leading cause of mortality at St. Joseph Health (“SJH”) with a 16% mortality rate and accounts for over 10, 000 cases annually and over $130 M dollars spent in care delivery. FY 16 YTD SJH Sepsis Mortality Rate 16. 2% Top-Quartile: 10. 13% Top-Decile: 7. 78% Aim: • • Three year regional, team-based journey (“Think Regionally, Act Locally”) Bring ministry resources together to determine points of variation that can be “systemized, streamlined” Leverage best practice sharing (“Compete Externally, Improve Internally”) Utilize the health system to provide resources and standardization around: data reporting/analytics, IT optimization, CDI/coding opportunities, performance improvement methodology Target: • • Achieve 90% or greater survival rate for sepsis Reduce our cost-per-case across the regions (achieve an improved sepsis margin)
Sepsis Challenges & Opportunities Sepsis will expose all that is weak within the current system of care • Communication/Coordination of care between providers • Location of care • Documentation • Readmission (Pre/Post hospitalization care) • IT system • Data collection system • Speed and ability of health system to change • Ability for standardization of care across region • Stamina to continue, keep/maintain gains • Ability to educate workforce and keep updated • Horizontal vs vertical integration • Changing current culture
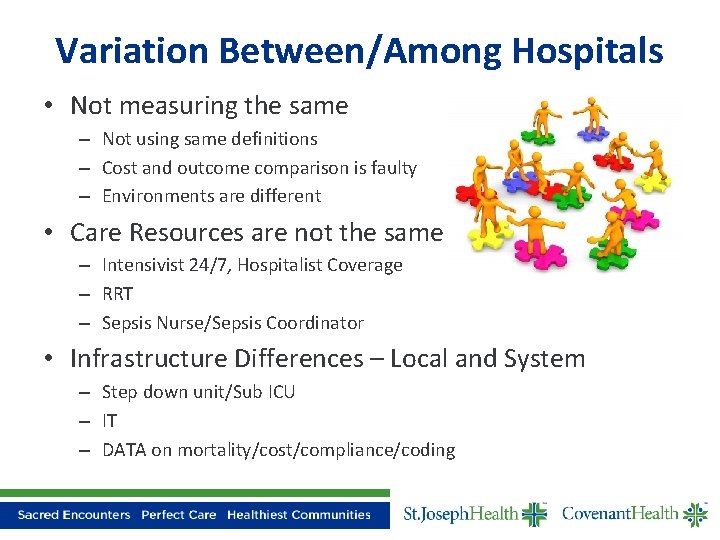
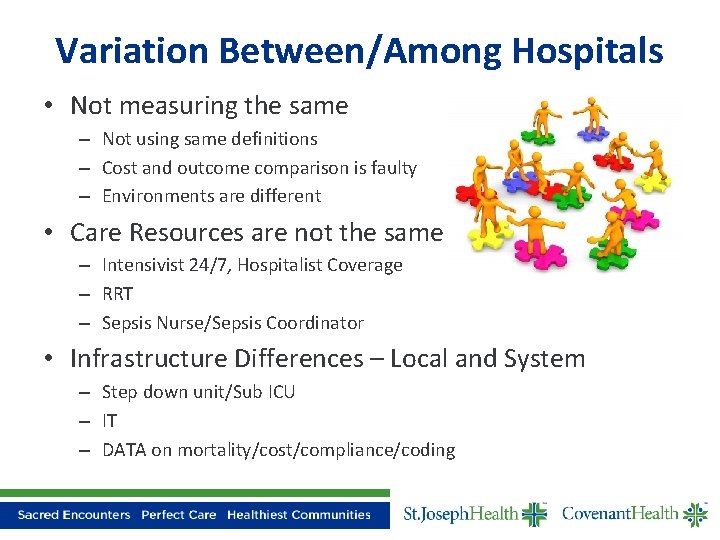
Variation Between/Among Hospitals • Not measuring the same – Not using same definitions – Cost and outcome comparison is faulty – Environments are different • Care Resources are not the same – Intensivist 24/7, Hospitalist Coverage – RRT – Sepsis Nurse/Sepsis Coordinator • Infrastructure Differences – Local and System – Step down unit/Sub ICU – IT – DATA on mortality/cost/compliance/coding
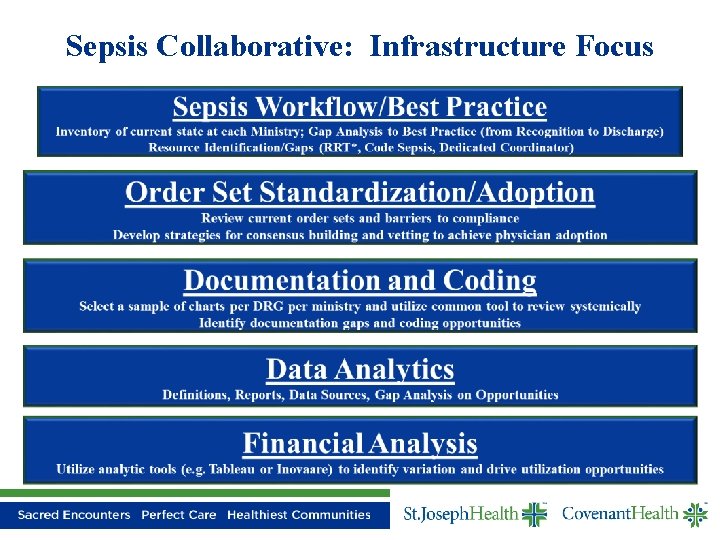
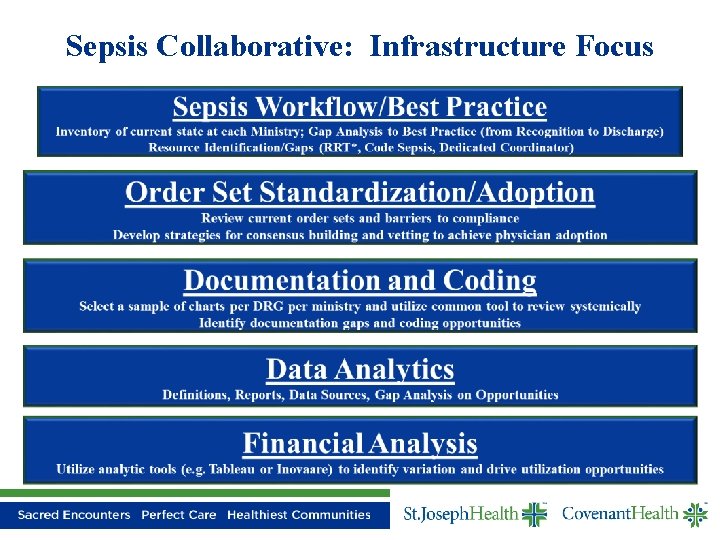
Sepsis Collaborative: Infrastructure Focus
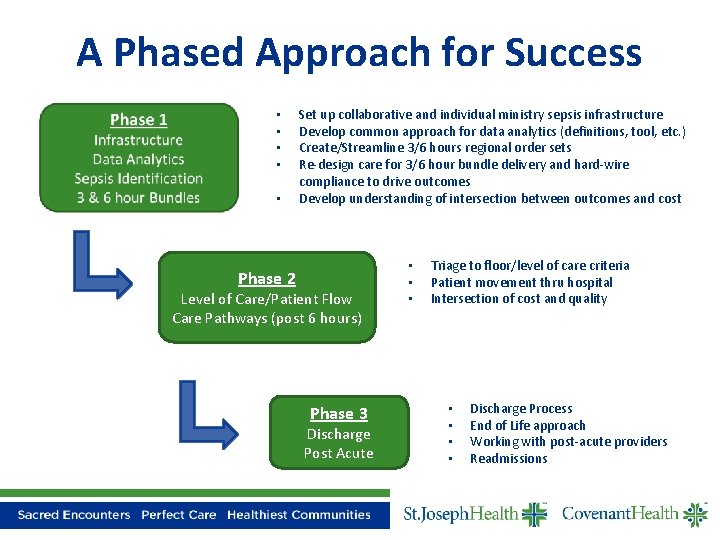
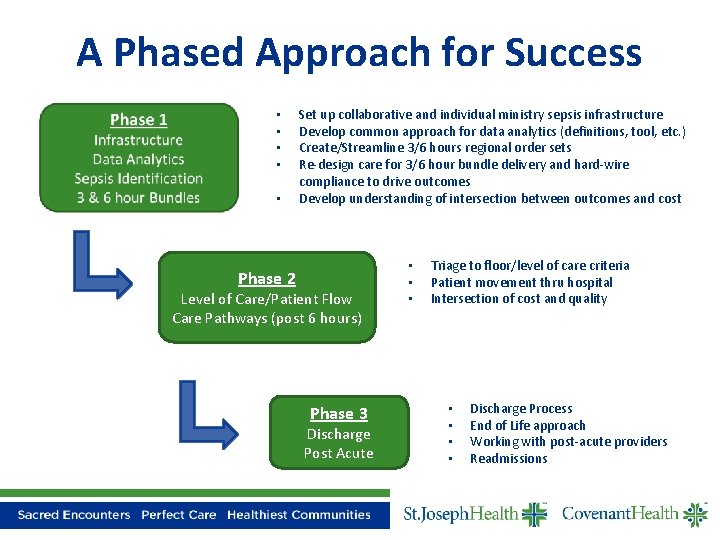
A Phased Approach for Success • • • Set up collaborative and individual ministry sepsis infrastructure Develop common approach for data analytics (definitions, tool, etc. ) Create/Streamline 3/6 hours regional order sets Re-design care for 3/6 hour bundle delivery and hard-wire compliance to drive outcomes Develop understanding of intersection between outcomes and cost Phase 2 Level of Care/Patient Flow Care Pathways (post 6 hours) Phase 3 Discharge Post Acute • • • Triage to floor/level of care criteria Patient movement thru hospital Intersection of cost and quality • • Discharge Process End of Life approach Working with post-acute providers Readmissions
Collaborative Commitment Any sepsis patient, at any of our ministries/hospitals will have the same quality of care and chance of survival Achieve 90% or greater survival rate for Sepsis Reduce our cost/case across the region
Collaborative Participants • • CMO/CNO ED Providers, Intensivist, Hospitalist ED, ICU, Med Surg Directors/Managers Rapid Response/Sepsis Nurse ED, ICU, Med Surg Staff Members Clinical Informatics Data Delivery (reports/analytics) Performance Improvement Specialist
Meditech EHR Excellence Toolkit Sepsis Management
Meditech EHR Excellence Program • The EHR Excellence Program promotes MEDITECH’s sophisticated EHR functionality to achieve clinical and operational excellence. • Provide your organization with outcome-based toolkits, best practice-driven education, and clinician-targeted content development. • Utilize these resources for: – – – Higher Quality of Care, with Maximum Productivity Evidence-Based Decision Making Satisfied physicians, clinicians and end users Improved Patient Experience Communication Across the Continuum Improved Financial Health
EHR Excellence Toolkit Components • Getting Started – Executive Summary – Project Plan • Implementation Guides – Integrated Workflow Guide – Build Guide • Education/Training – On Demand Education Videos – Presentation slide decks • Supporting Information – Helpful Links to outside sources used in research/design • FAQs • Change Log for tracking updates
Patient Presents to the Emergency Department • Clinical Presentation – 94 year old female – Abdominal Pain – Patient received in triage and nursing completing the assessment
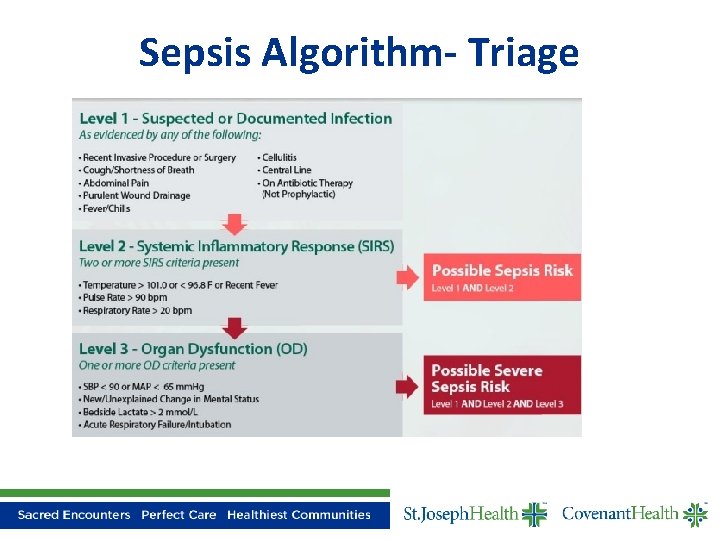
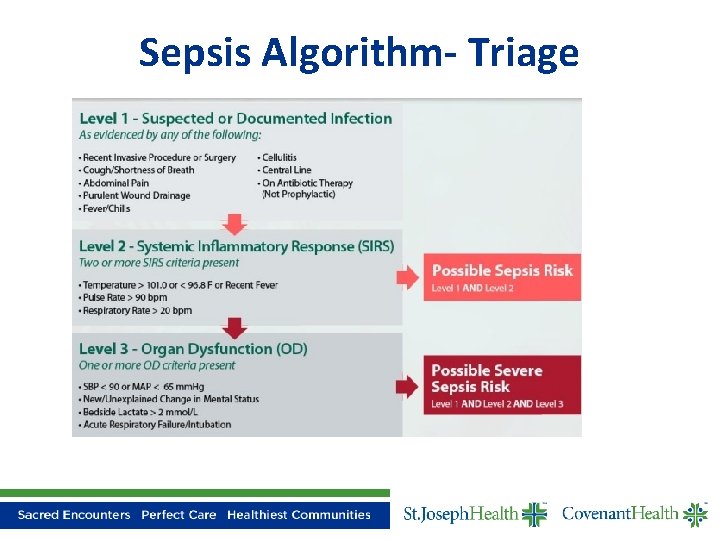
Sepsis Algorithm- Triage
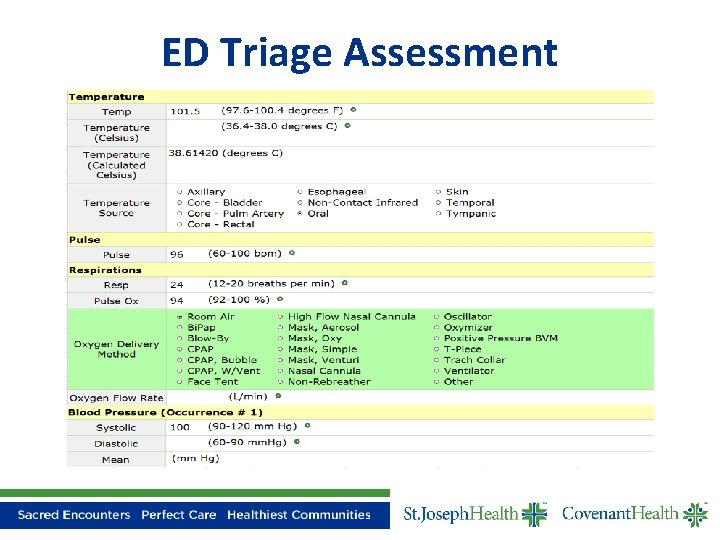
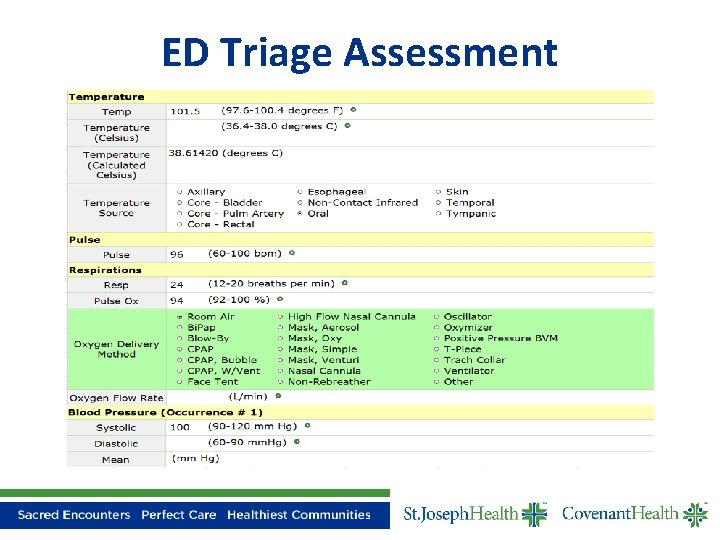
ED Triage Assessment
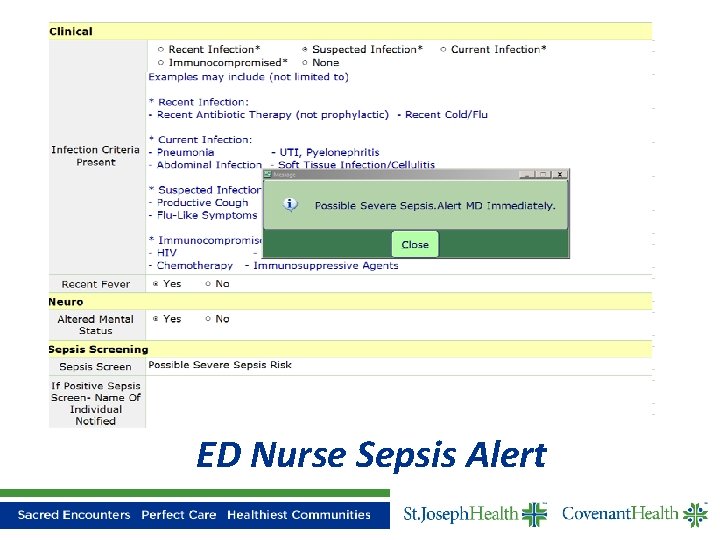
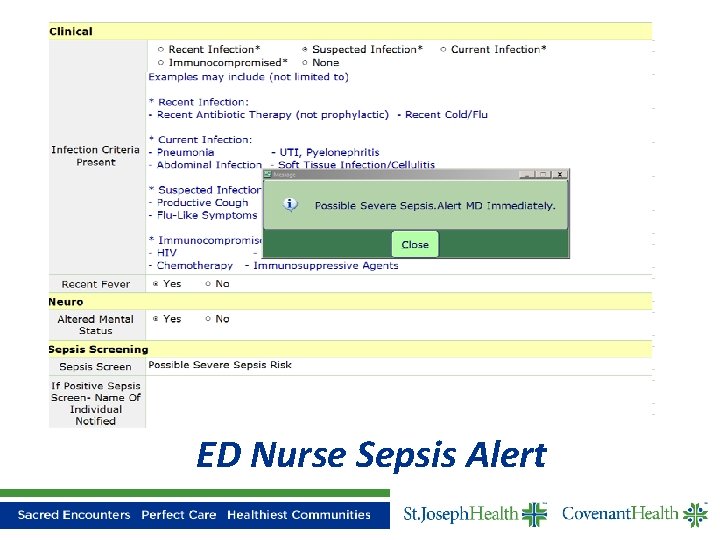
ED Nurse Sepsis Alert
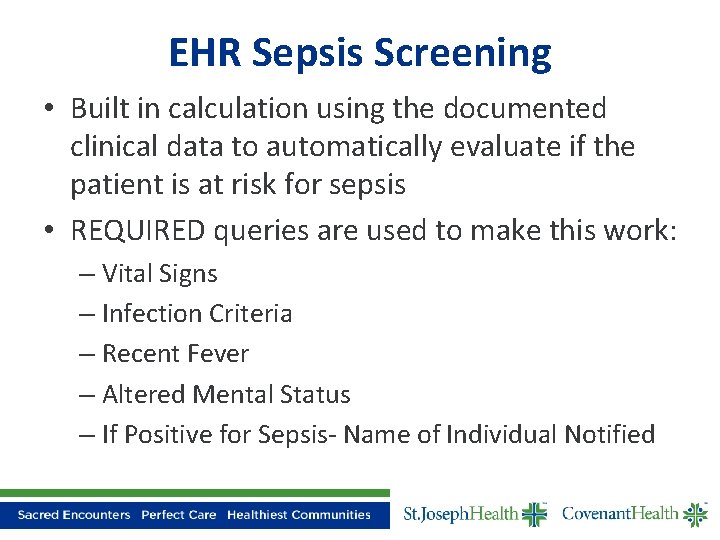
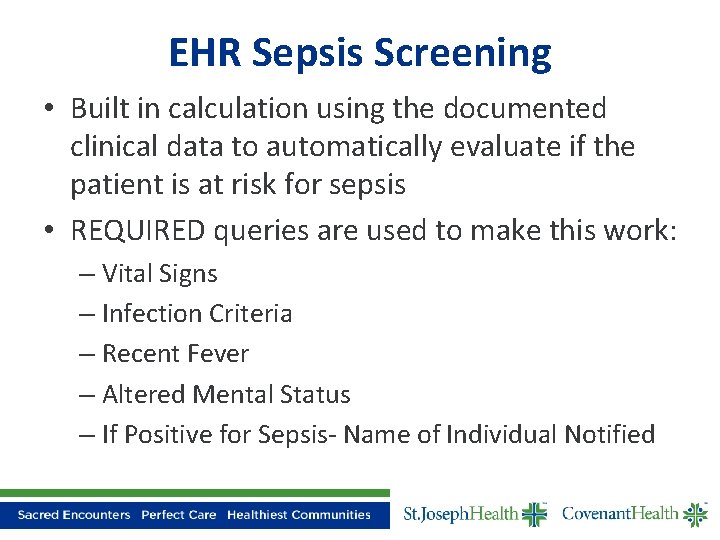
EHR Sepsis Screening • Built in calculation using the documented clinical data to automatically evaluate if the patient is at risk for sepsis • REQUIRED queries are used to make this work: – Vital Signs – Infection Criteria – Recent Fever – Altered Mental Status – If Positive for Sepsis- Name of Individual Notified
ED Physician Workflow
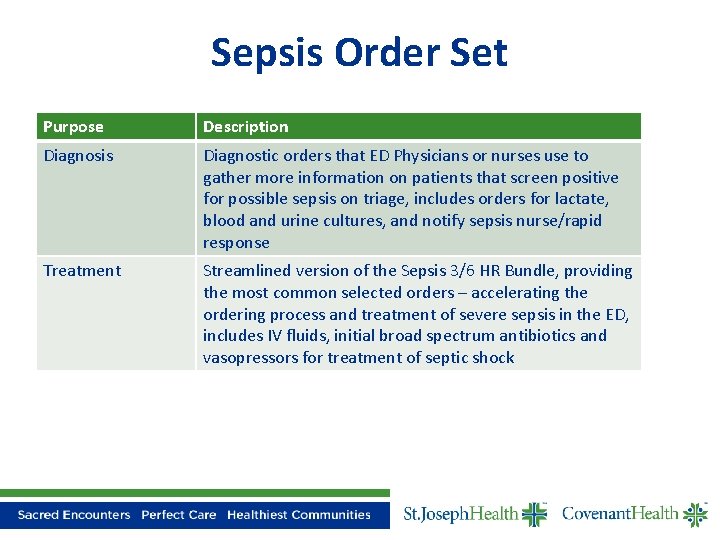
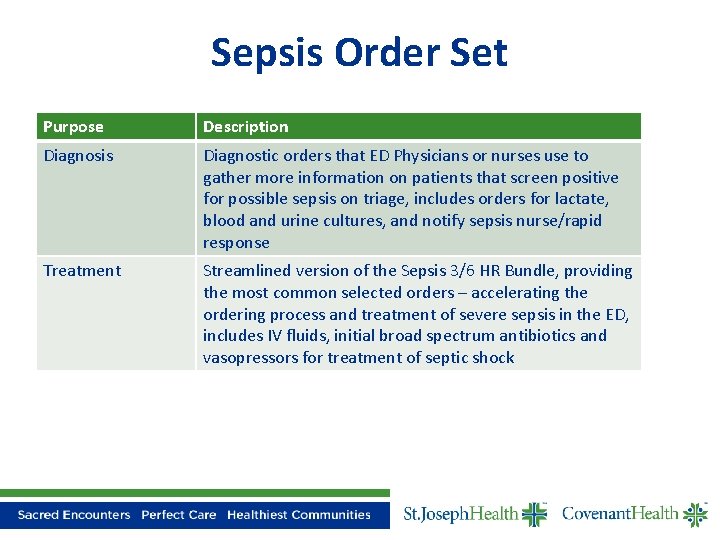
Sepsis Order Set Purpose Description Diagnosis Diagnostic orders that ED Physicians or nurses use to gather more information on patients that screen positive for possible sepsis on triage, includes orders for lactate, blood and urine cultures, and notify sepsis nurse/rapid response Treatment Streamlined version of the Sepsis 3/6 HR Bundle, providing the most common selected orders – accelerating the ordering process and treatment of severe sepsis in the ED, includes IV fluids, initial broad spectrum antibiotics and vasopressors for treatment of septic shock
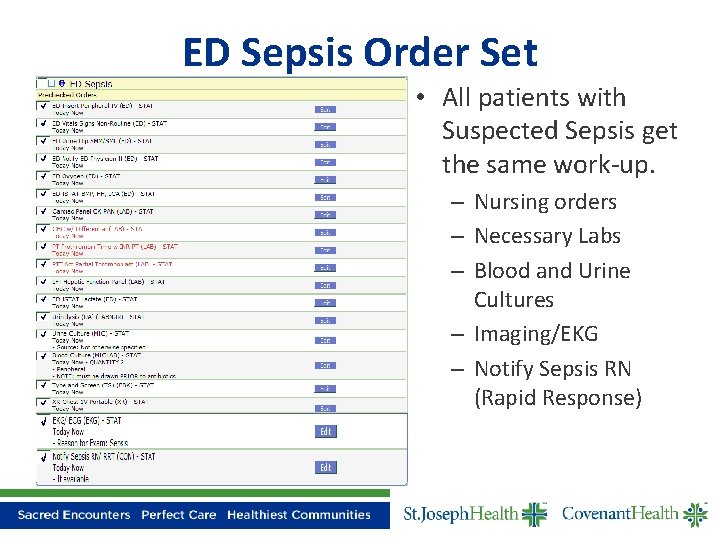
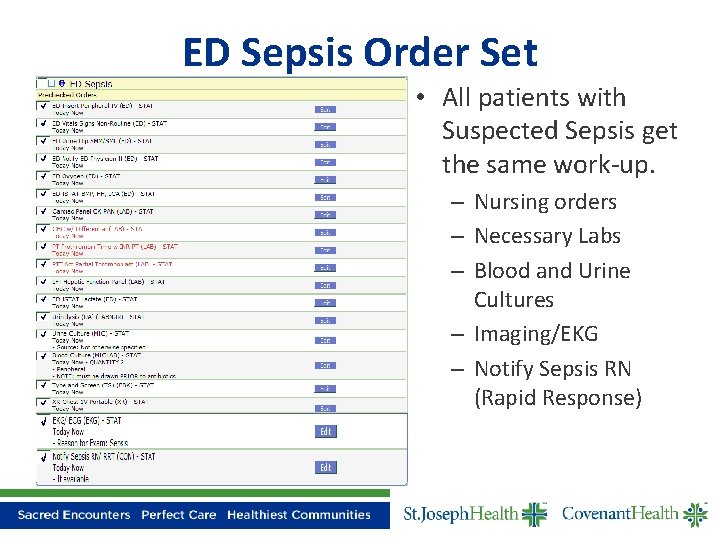
ED Sepsis Order Set • All patients with Suspected Sepsis get the same work-up. – Nursing orders – Necessary Labs – Blood and Urine Cultures – Imaging/EKG – Notify Sepsis RN (Rapid Response)
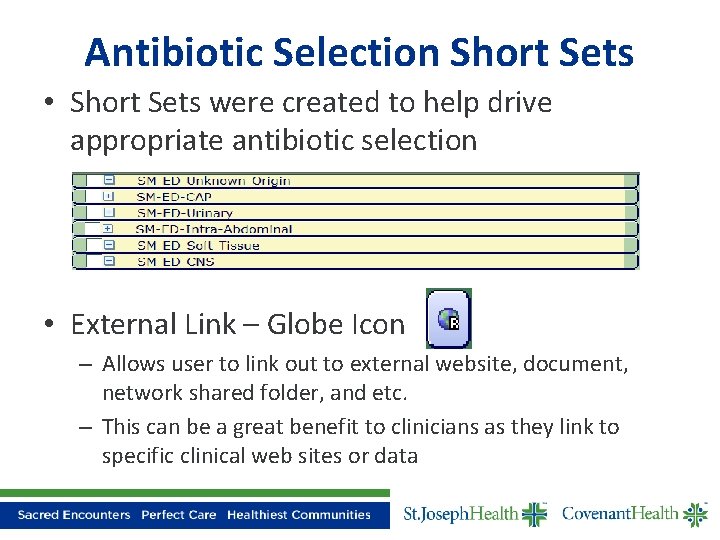
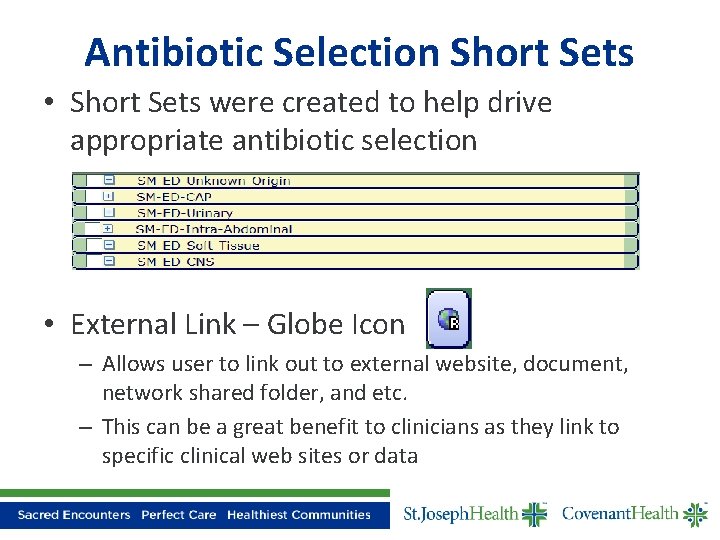
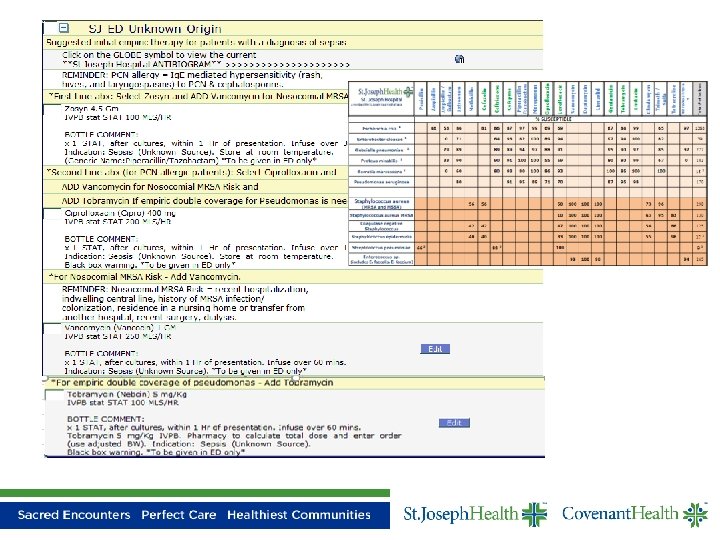
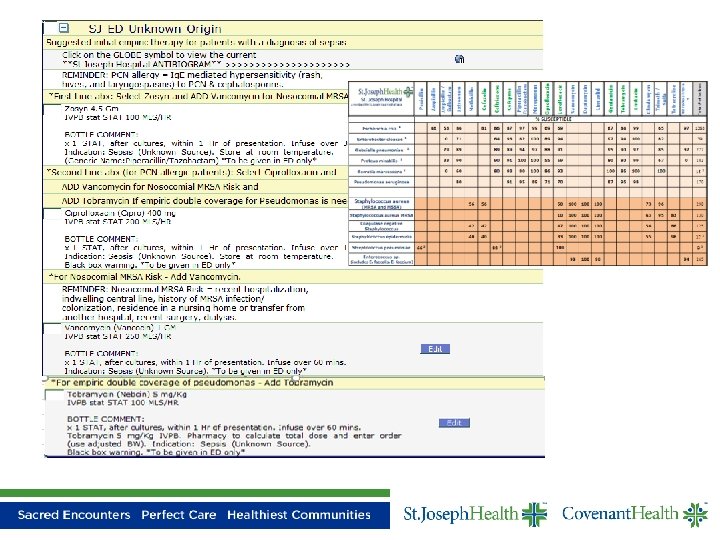
Antibiotic Selection Short Sets • Short Sets were created to help drive appropriate antibiotic selection • External Link – Globe Icon – Allows user to link out to external website, document, network shared folder, and etc. – This can be a great benefit to clinicians as they link to specific clinical web sites or data
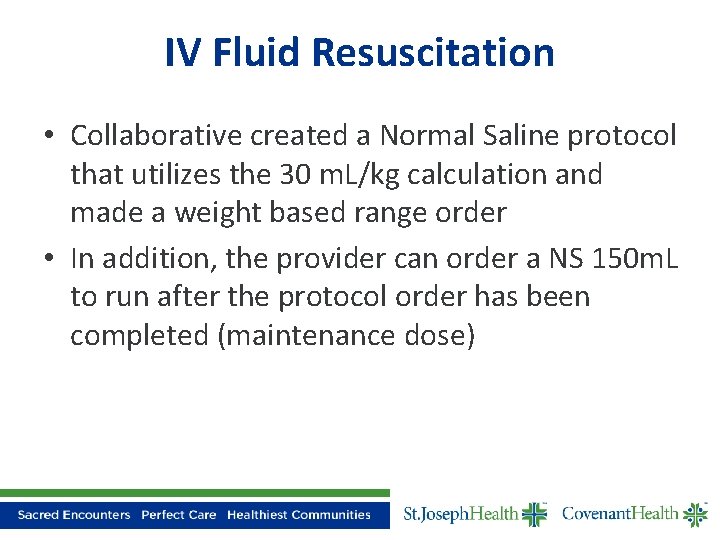
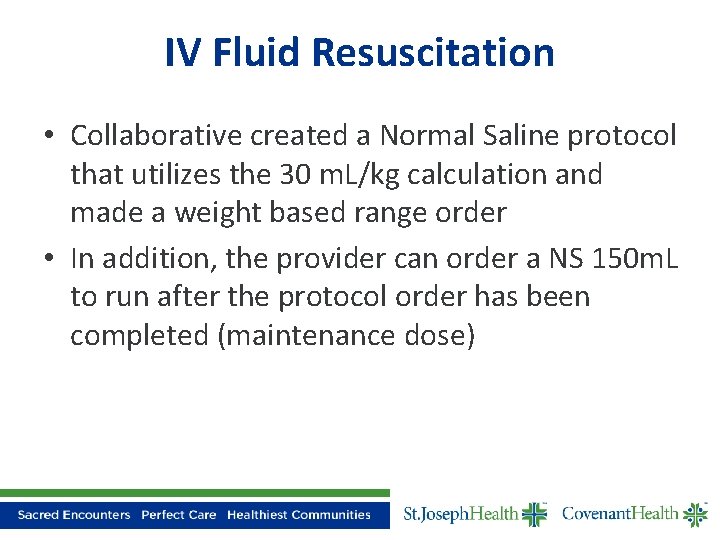
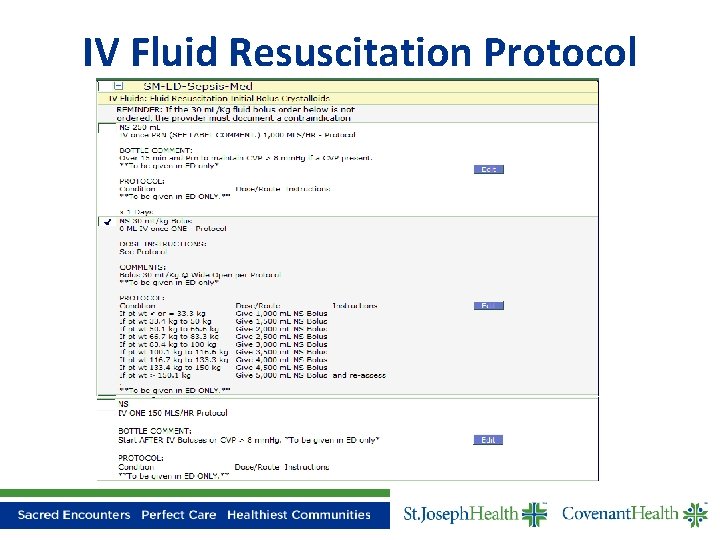
IV Fluid Resuscitation • Collaborative created a Normal Saline protocol that utilizes the 30 m. L/kg calculation and made a weight based range order • In addition, the provider can order a NS 150 m. L to run after the protocol order has been completed (maintenance dose)
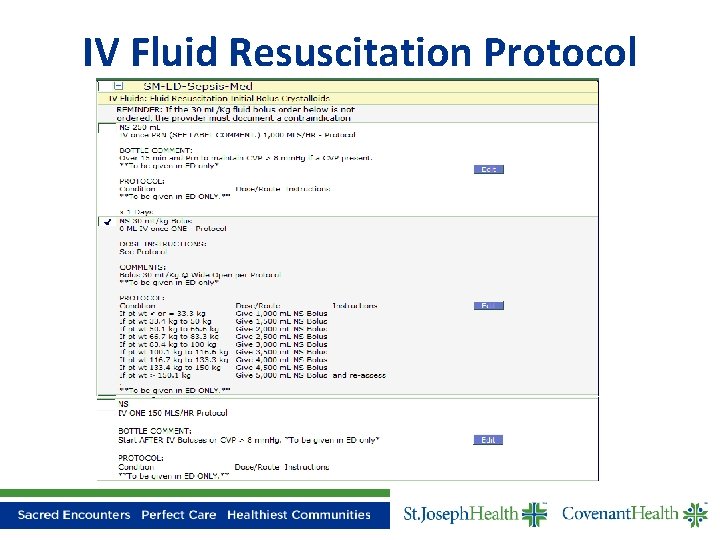
IV Fluid Resuscitation Protocol
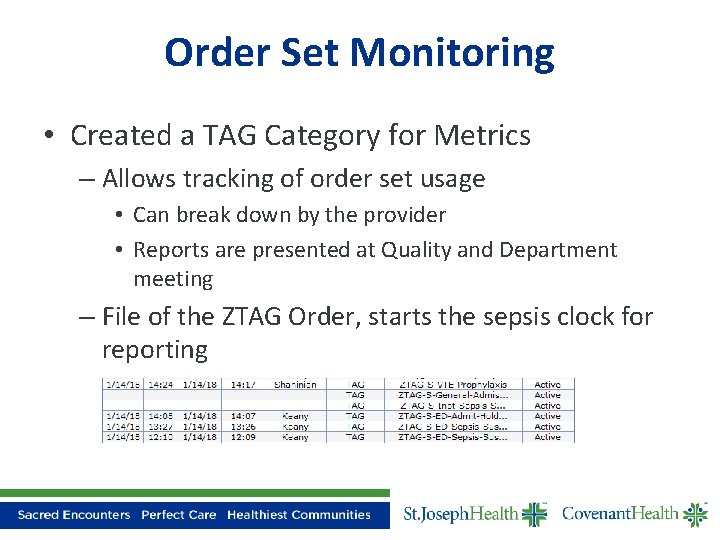
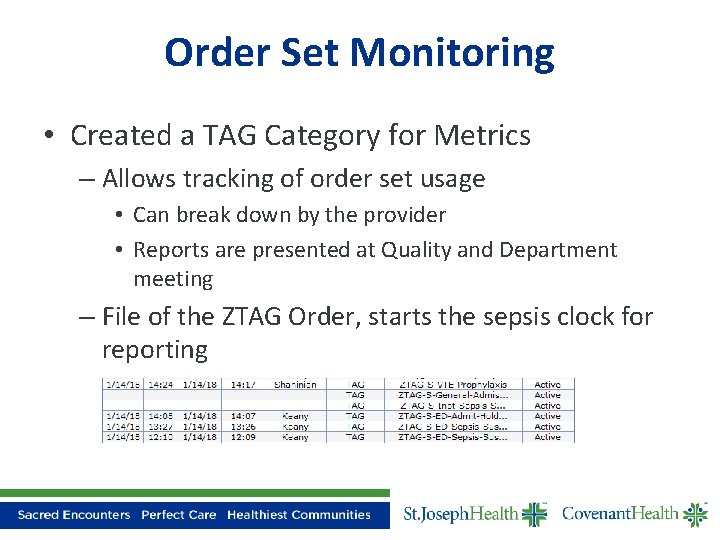
Order Set Monitoring • Created a TAG Category for Metrics – Allows tracking of order set usage • Can break down by the provider • Reports are presented at Quality and Department meeting – File of the ZTAG Order, starts the sepsis clock for reporting
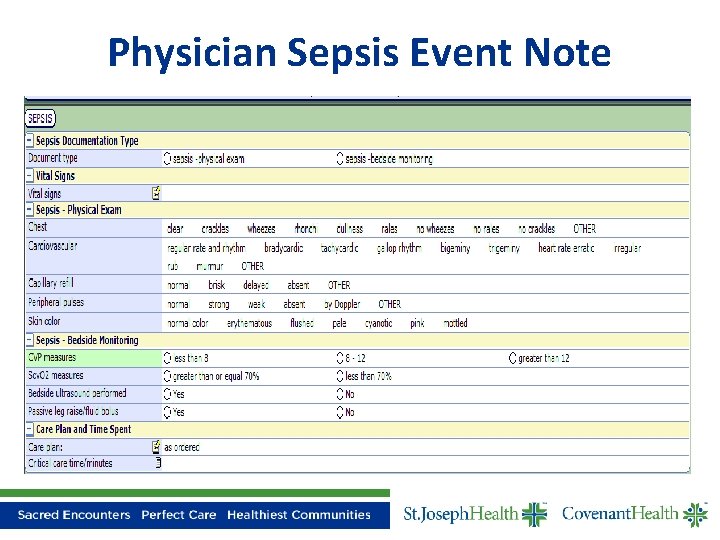
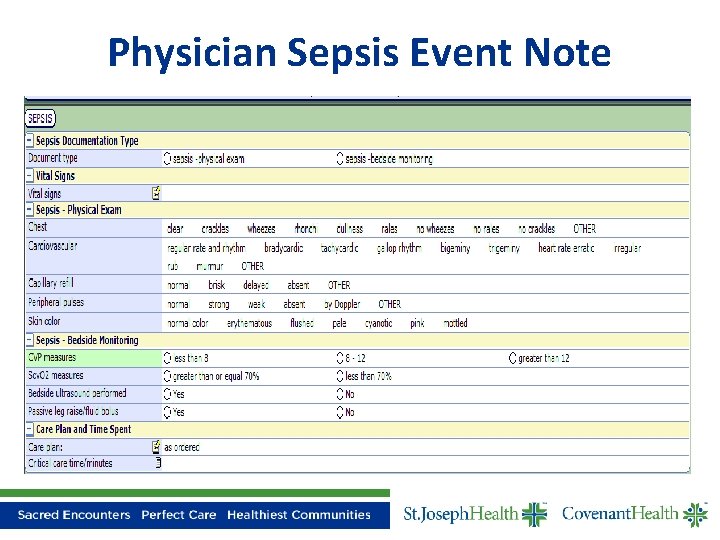
Physician Sepsis Event Note
Inpatient Scenario • Clinical Presentation – 86 year old male – Cough, weakness, abnormal CXR – Admitted with Suspected Pneumonia • Later on Hospital Day 1 – Temp, Pulse and Respiratory Rate spiked – BP Dropped
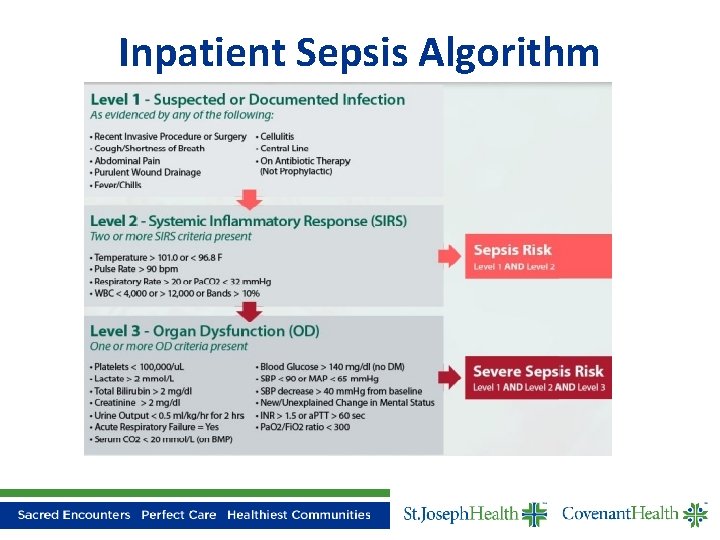
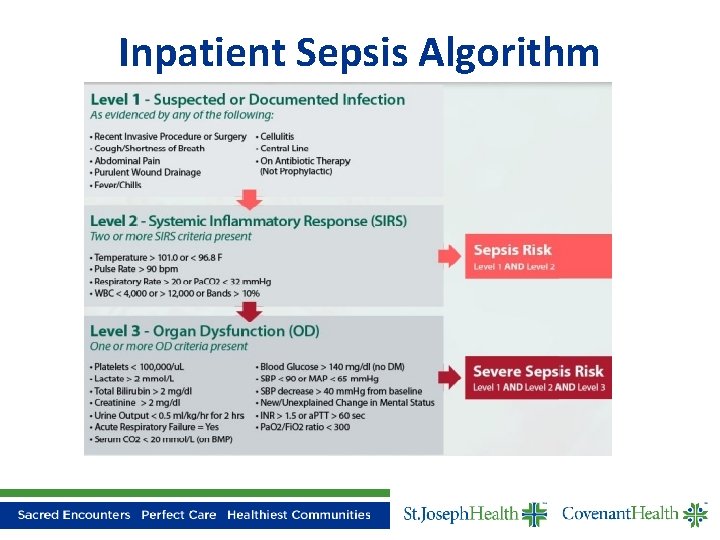
Inpatient Sepsis Algorithm
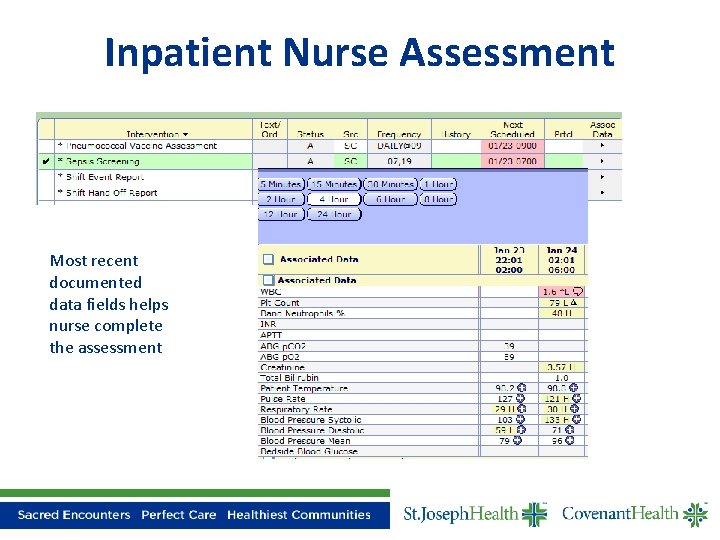
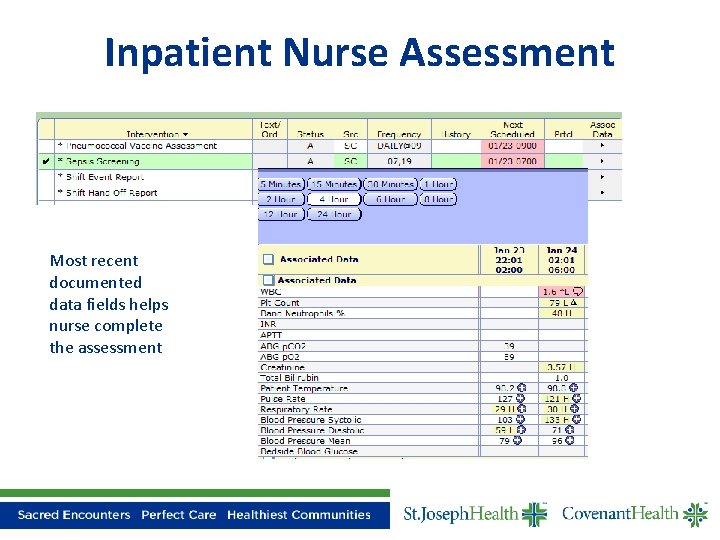
Inpatient Nurse Assessment Most recent documented data fields helps nurse complete the assessment
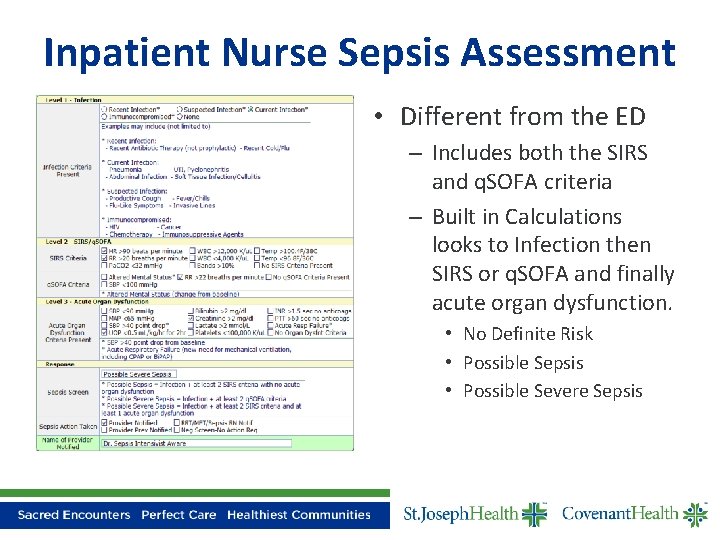
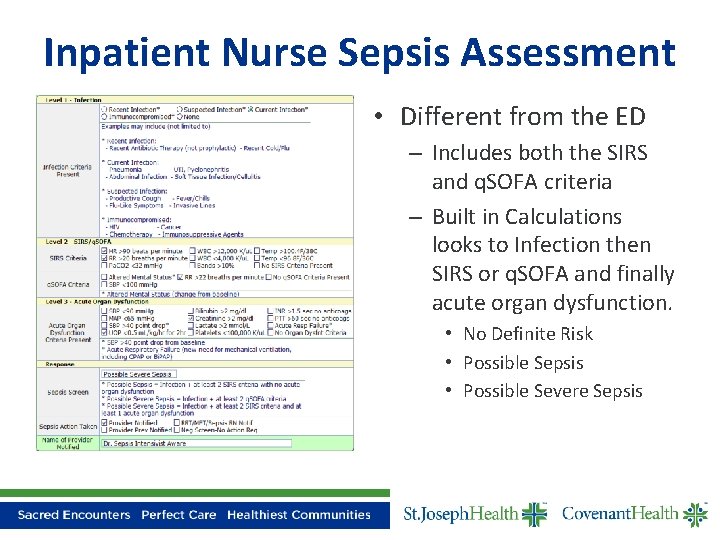
Inpatient Nurse Sepsis Assessment • Different from the ED – Includes both the SIRS and q. SOFA criteria – Built in Calculations looks to Infection then SIRS or q. SOFA and finally acute organ dysfunction. • No Definite Risk • Possible Sepsis • Possible Severe Sepsis
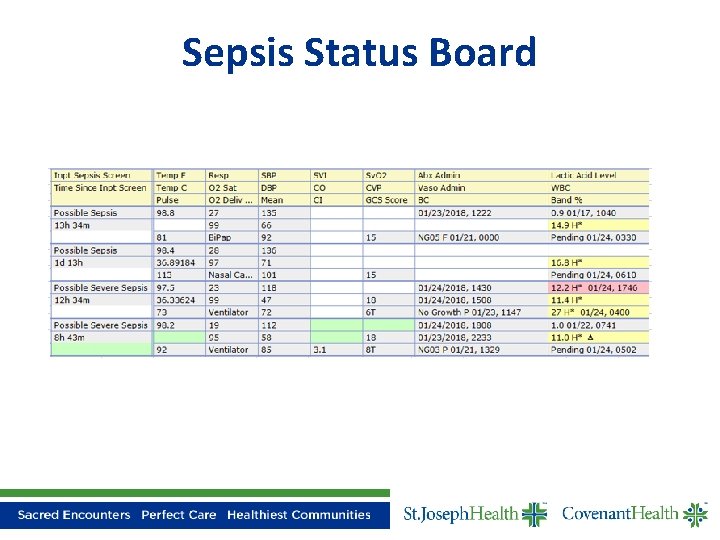
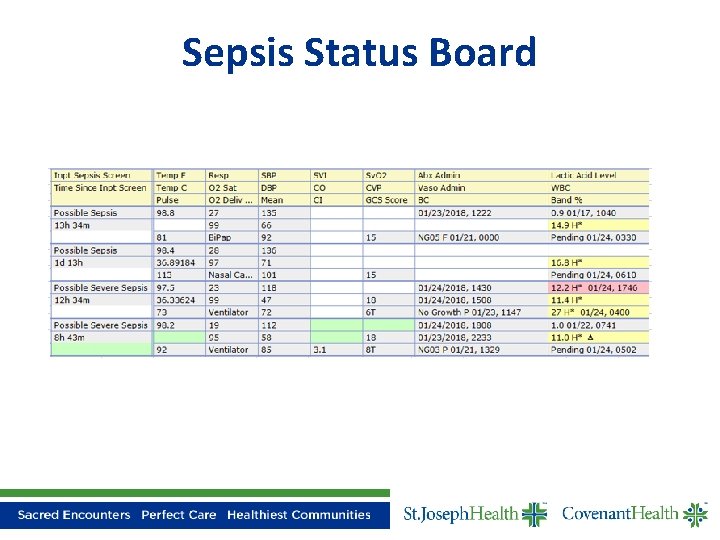
Sepsis Status Board
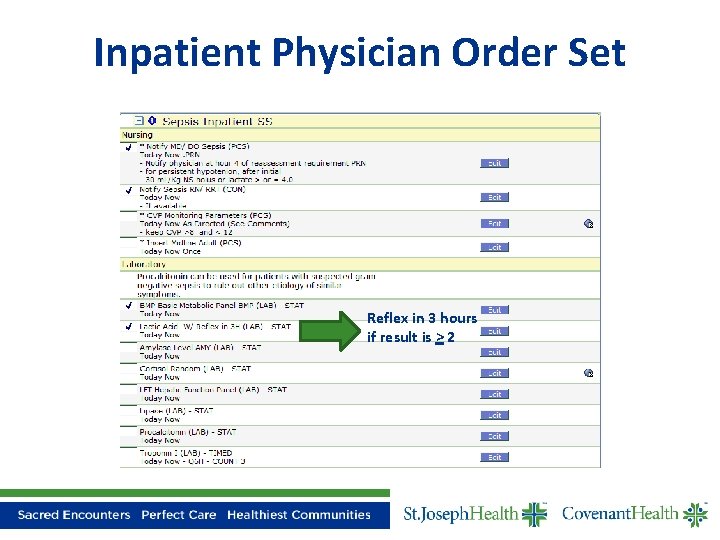
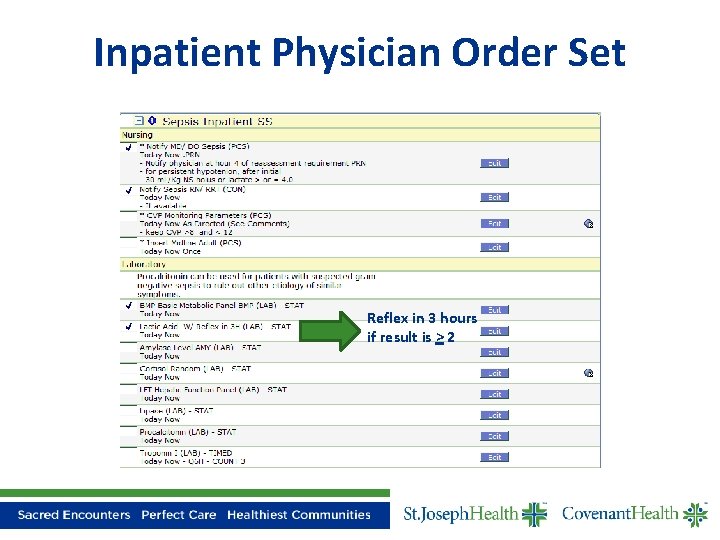
Inpatient Physician Order Set Reflex in 3 hours if result is > 2
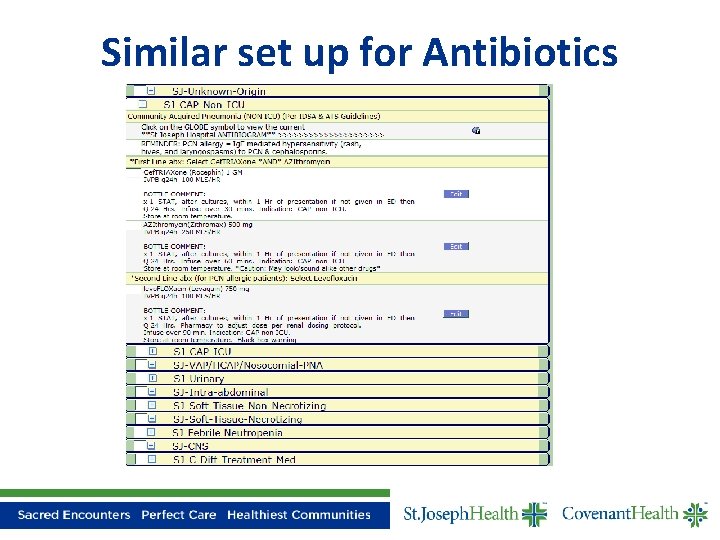
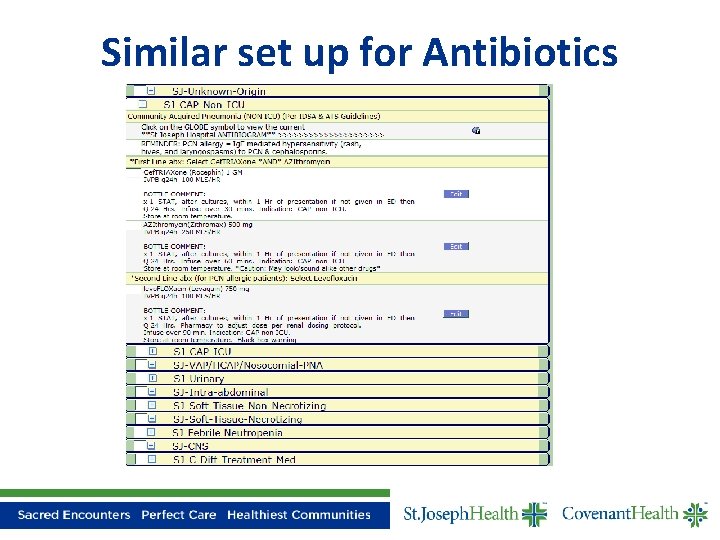
Similar set up for Antibiotics

EMR Fluid Volume Resuscitation
Maternal Sepsis
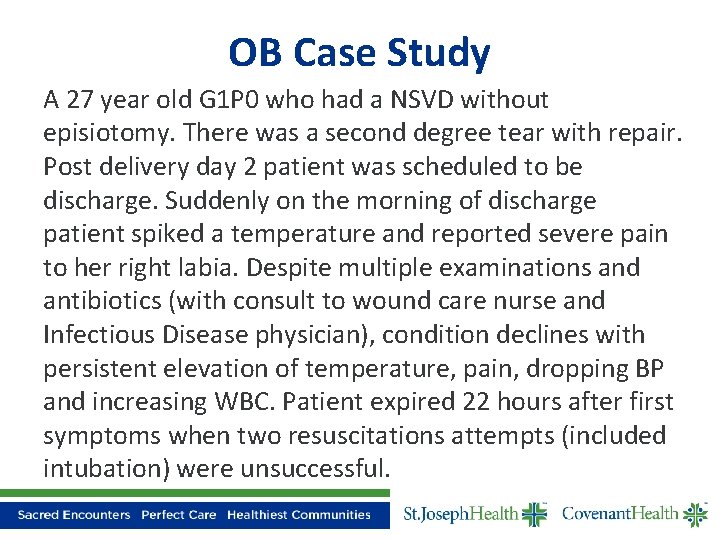
OB Case Study A 27 year old G 1 P 0 who had a NSVD without episiotomy. There was a second degree tear with repair. Post delivery day 2 patient was scheduled to be discharge. Suddenly on the morning of discharge patient spiked a temperature and reported severe pain to her right labia. Despite multiple examinations and antibiotics (with consult to wound care nurse and Infectious Disease physician), condition declines with persistent elevation of temperature, pain, dropping BP and increasing WBC. Patient expired 22 hours after first symptoms when two resuscitations attempts (included intubation) were unsuccessful.
Seeking Answers to… • How did we miss it? • How does the OB patient become so sick so quickly? • Was this an isolated incident?
Myths Healthy Young Women Don’t Become Septic! Problem: The Obstetric Patient Does Not Fit the Picture of Sepsis • • • Male Extremes of Age Immunodeficiency Cancer Chronic Illness • Surgical/Invasive Procedures • Malnutrition • Catheters • Implanted Medical Devices

Our Reality • A pregnant woman has diminished ability to compensate for metabolic acidosis when her condition is complicated by severe infection • Pregnant women may appear deceptively well before experiencing vascular collapse secondary to severe sepsis and/or septic shock.
Maternal Sepsis • Maternal sepsis is the leading cause of preventable maternal death, accounting for 15% worldwide • CDC reports infection/sepsis 12. 7% (3 rd cause) • Seen an increase over the last decade – Older maternal age at delivery – Multi-fetal gestation – Obesity – Data Source CDC
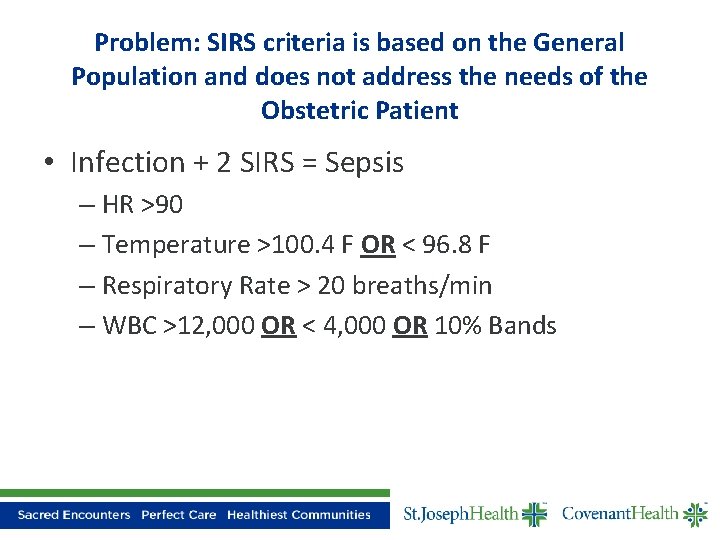
Problem: SIRS criteria is based on the General Population and does not address the needs of the Obstetric Patient • Infection + 2 SIRS = Sepsis – HR >90 – Temperature >100. 4 F OR < 96. 8 F – Respiratory Rate > 20 breaths/min – WBC >12, 000 OR < 4, 000 OR 10% Bands
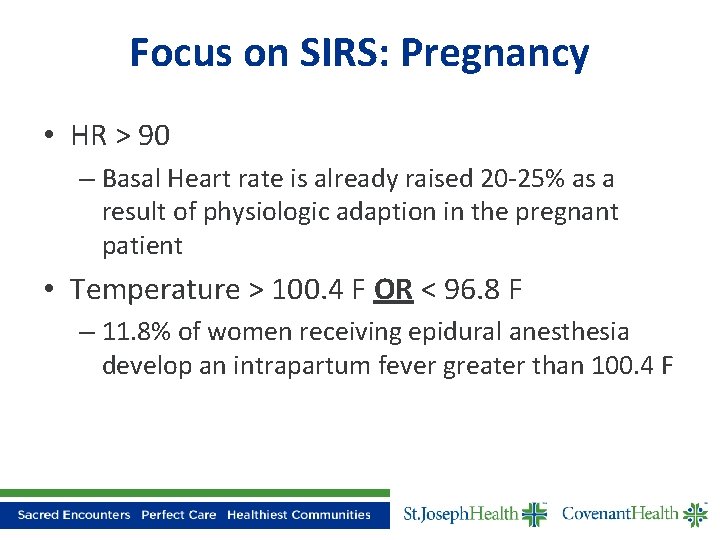
Focus on SIRS: Pregnancy • HR > 90 – Basal Heart rate is already raised 20 -25% as a result of physiologic adaption in the pregnant patient • Temperature > 100. 4 F OR < 96. 8 F – 11. 8% of women receiving epidural anesthesia develop an intrapartum fever greater than 100. 4 F
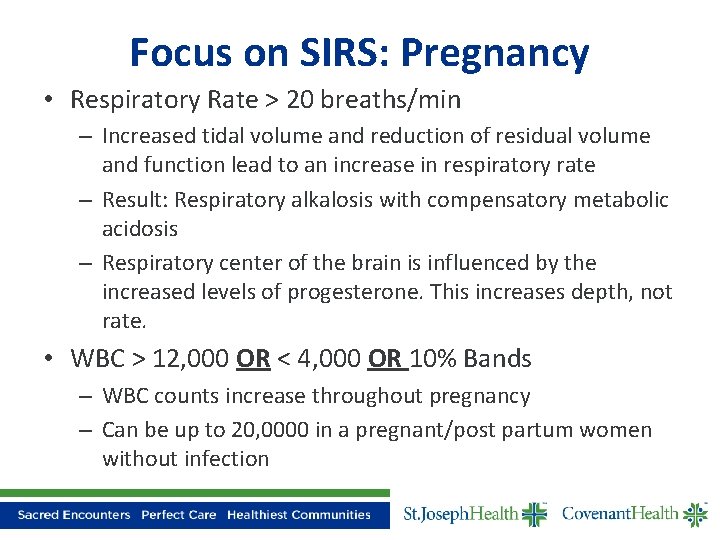
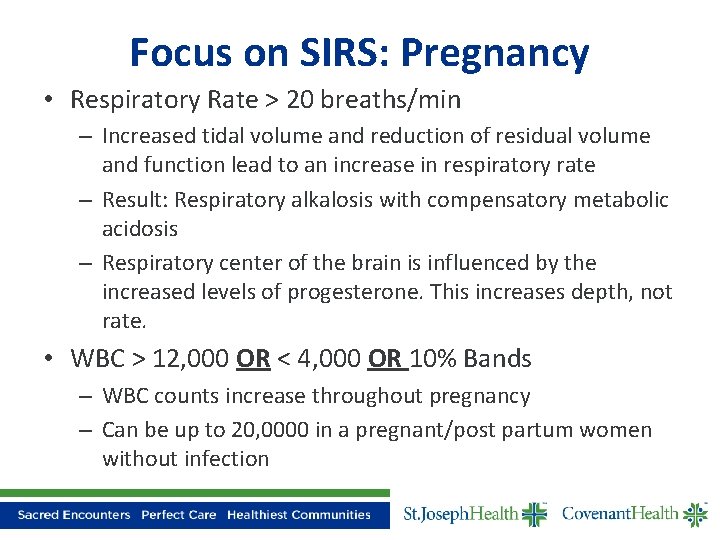
Focus on SIRS: Pregnancy • Respiratory Rate > 20 breaths/min – Increased tidal volume and reduction of residual volume and function lead to an increase in respiratory rate – Result: Respiratory alkalosis with compensatory metabolic acidosis – Respiratory center of the brain is influenced by the increased levels of progesterone. This increases depth, not rate. • WBC > 12, 000 OR < 4, 000 OR 10% Bands – WBC counts increase throughout pregnancy – Can be up to 20, 0000 in a pregnant/post partum women without infection
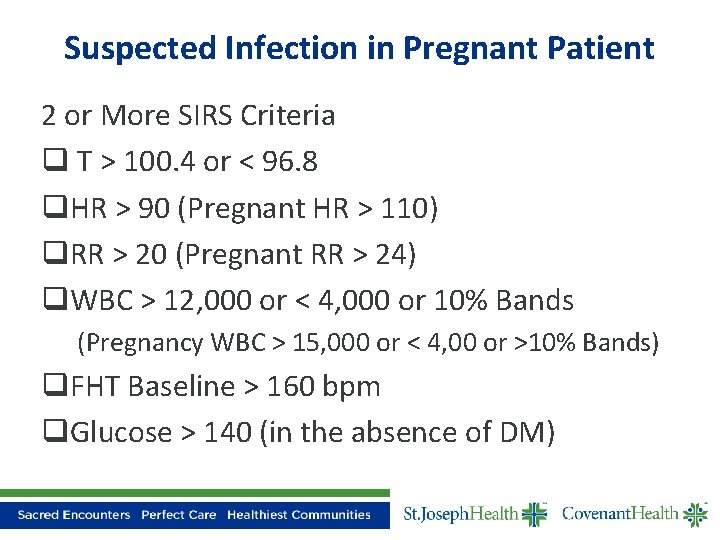
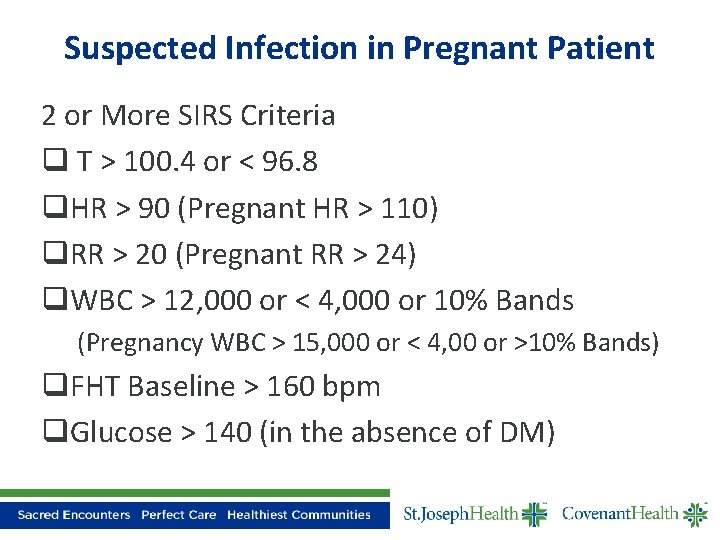
Suspected Infection in Pregnant Patient 2 or More SIRS Criteria q T > 100. 4 or < 96. 8 q. HR > 90 (Pregnant HR > 110) q. RR > 20 (Pregnant RR > 24) q. WBC > 12, 000 or < 4, 000 or 10% Bands (Pregnancy WBC > 15, 000 or < 4, 00 or >10% Bands) q. FHT Baseline > 160 bpm q. Glucose > 140 (in the absence of DM)
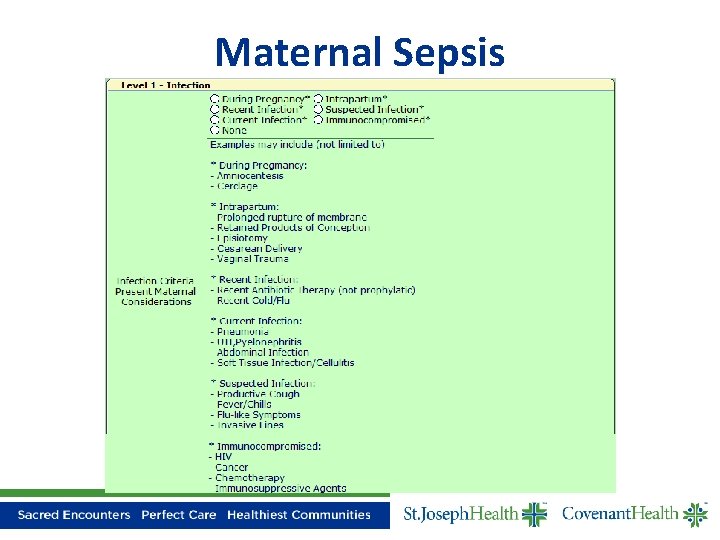
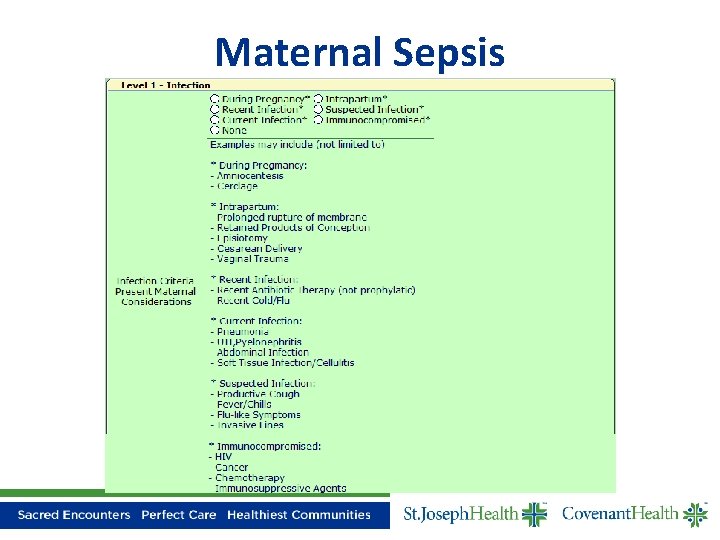
Maternal Sepsis
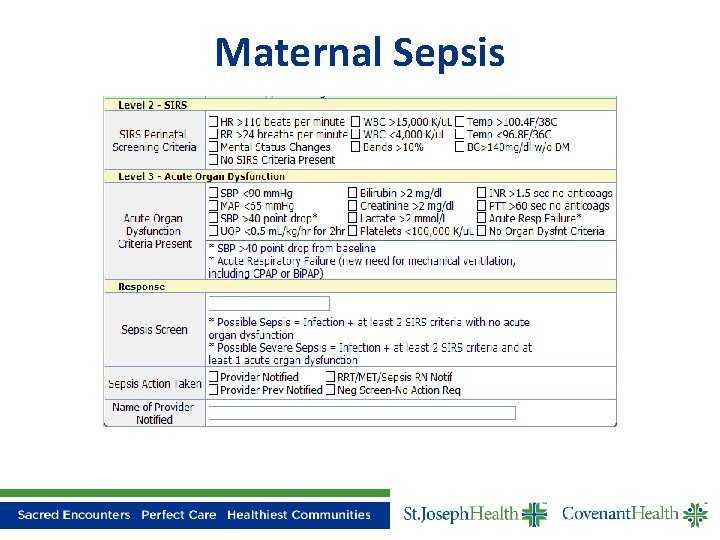
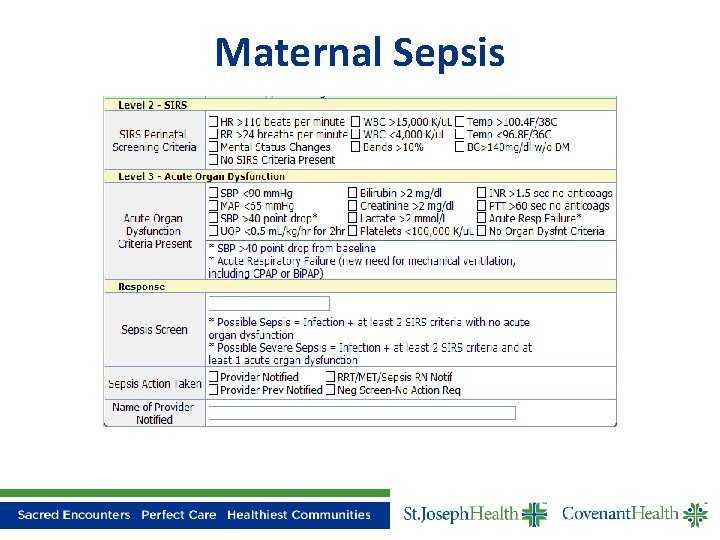
Maternal Sepsis
Outcomes

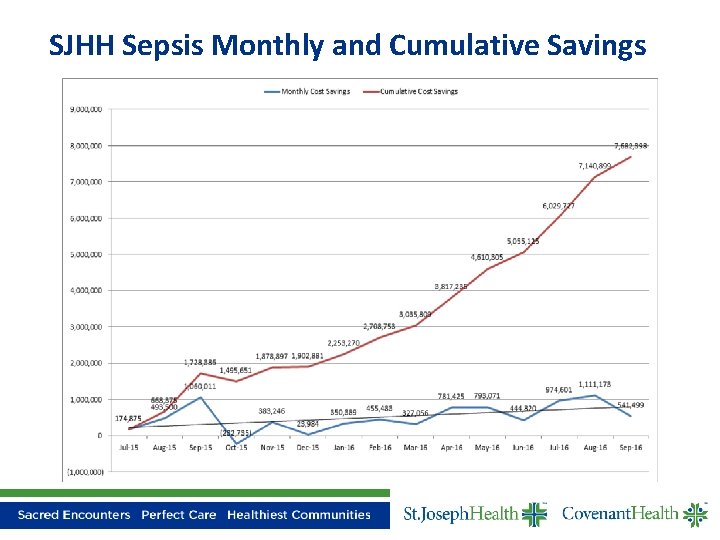
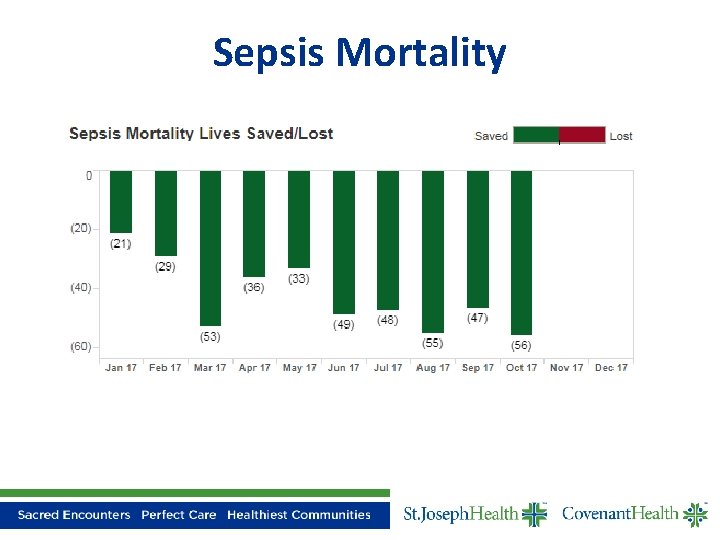
Phase 1 Accomplishments Standard Order Sets for Sepsis (ED and Inpatient) 37 to 2 Common Data Report; standards and definitions for measuring success Common tool for screening and documenting sepsis Creation of the Sepsis Nurse Role 270+ lives saved, $8. 4 M saved in cost/case
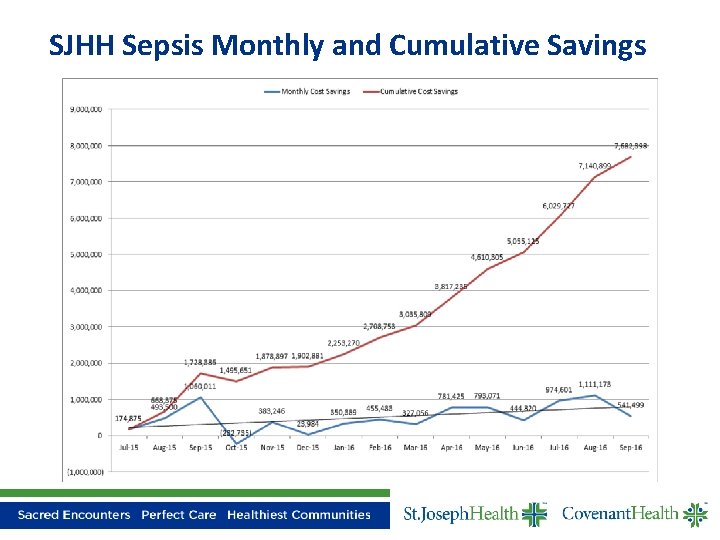
SJHH Sepsis Monthly and Cumulative Savings
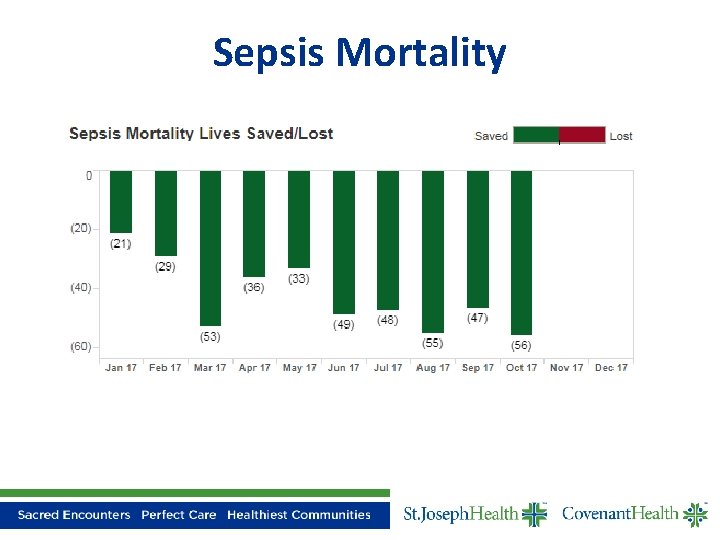
Sepsis Mortality
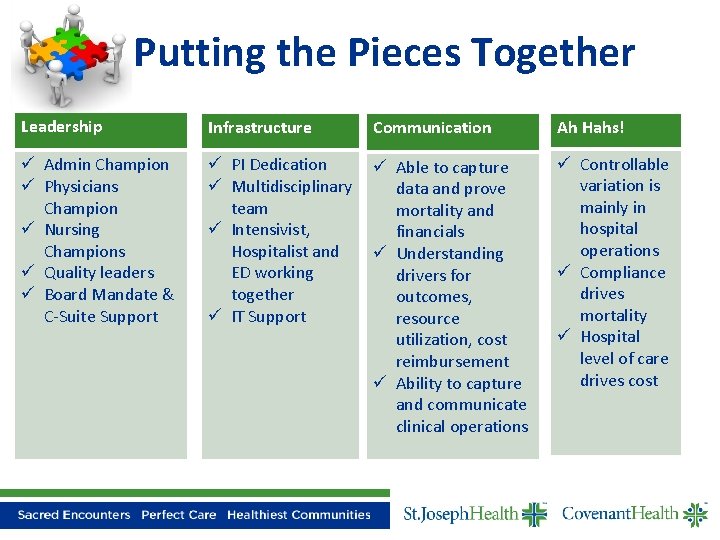
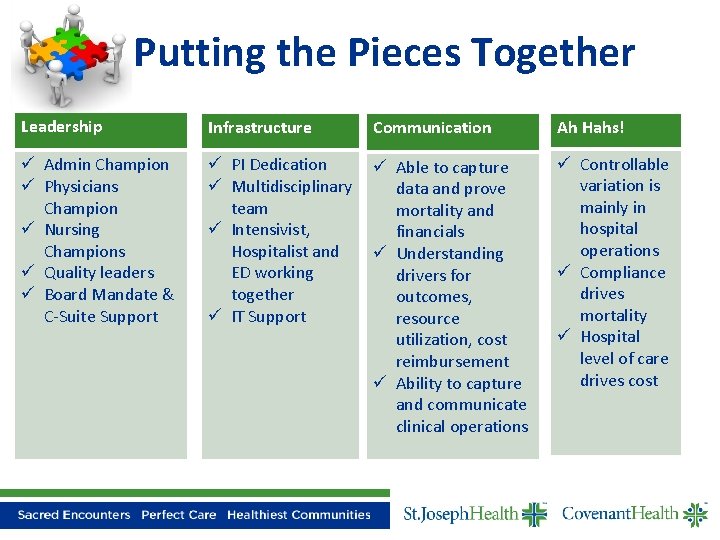
Putting the Pieces Together Leadership Infrastructure Communication Ah Hahs! ü Admin Champion ü Physicians Champion ü Nursing Champions ü Quality leaders ü Board Mandate & C-Suite Support ü PI Dedication ü Multidisciplinary team ü Intensivist, Hospitalist and ED working together ü IT Support ü Able to capture data and prove mortality and financials ü Understanding drivers for outcomes, resource utilization, cost reimbursement ü Ability to capture and communicate clinical operations ü Controllable variation is mainly in hospital operations ü Compliance drives mortality ü Hospital level of care drives cost