Use of Simulation The Pros Cons Prof K

- Slides: 24
Use of Simulation – The Pros (& Cons) Prof K. R. Sethuraman Dean – Faculty of Medicine & Deputy VC – Academic/International Affairs AIMST University
Viewpoints From • • • Students’ perspective Educators’ , , Pedagogy support Research , , Patient safety & rights
How Learning Used to be… • • • No Computer No Internet No TV No Video No Mobile Phone • Less Diversions!
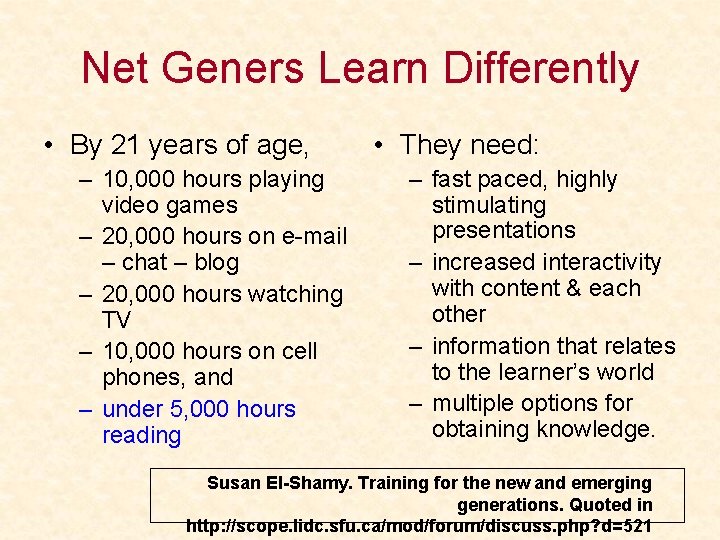
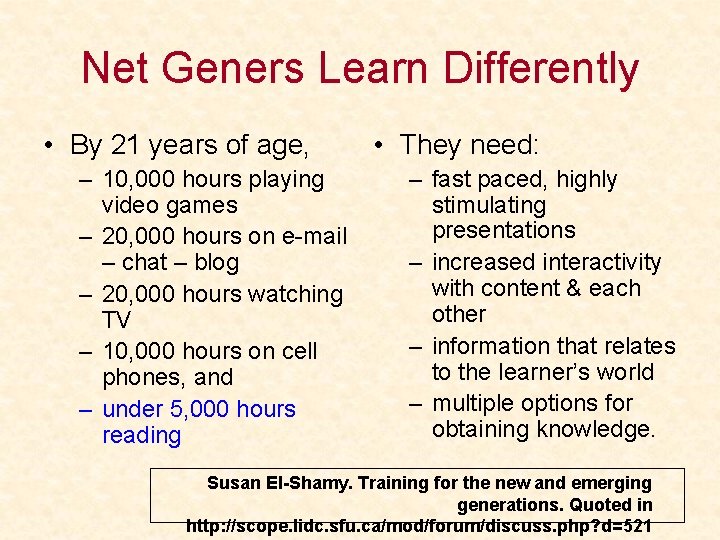
Net Geners Learn Differently • By 21 years of age, – 10, 000 hours playing video games – 20, 000 hours on e-mail – chat – blog – 20, 000 hours watching TV – 10, 000 hours on cell phones, and – under 5, 000 hours reading • They need: – fast paced, highly stimulating presentations – increased interactivity with content & each other – information that relates to the learner’s world – multiple options for obtaining knowledge. Susan El-Shamy. Training for the new and emerging generations. Quoted in http: //scope. lidc. sfu. ca/mod/forum/discuss. php? d=521
Parenting Net Generation!
Educating the Next-Generation • Medical education has responded by increasing the amount of : – multimodal content (visual, auditory, kinesthetic “hands on” practice) – active learning (read, write, discuss) – experiential/contextual learning (job shadowing, simulation labs) – problem based learning, team projects.
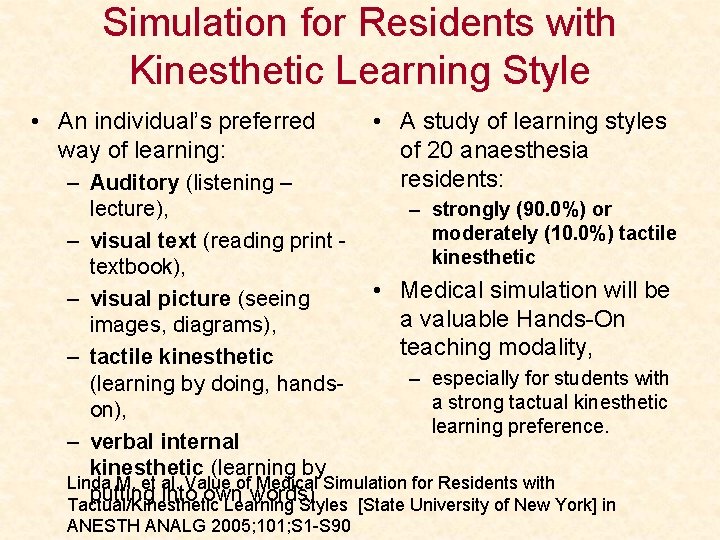
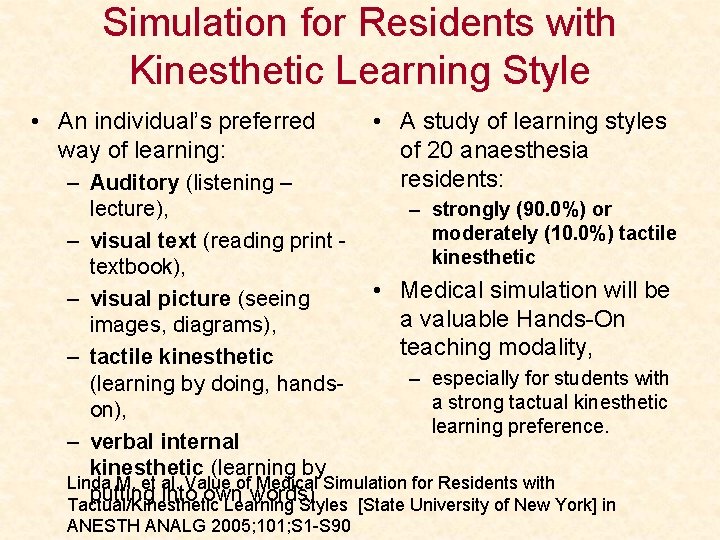
Simulation for Residents with Kinesthetic Learning Style • An individual’s preferred way of learning: • A study of learning styles of 20 anaesthesia residents: – Auditory (listening – – strongly (90. 0%) or lecture), moderately (10. 0%) tactile – visual text (reading print kinesthetic textbook), • Medical simulation will be – visual picture (seeing a valuable Hands-On images, diagrams), teaching modality, – tactile kinesthetic – especially for students with (learning by doing, handsa strong tactual kinesthetic on), learning preference. – verbal internal kinesthetic (learning by Linda M. et al. Value of Medical Simulation for Residents with putting into own words) Tactual/Kinesthetic Learning Styles [State University of New York] in ANESTH ANALG 2005; 101; S 1 -S 90
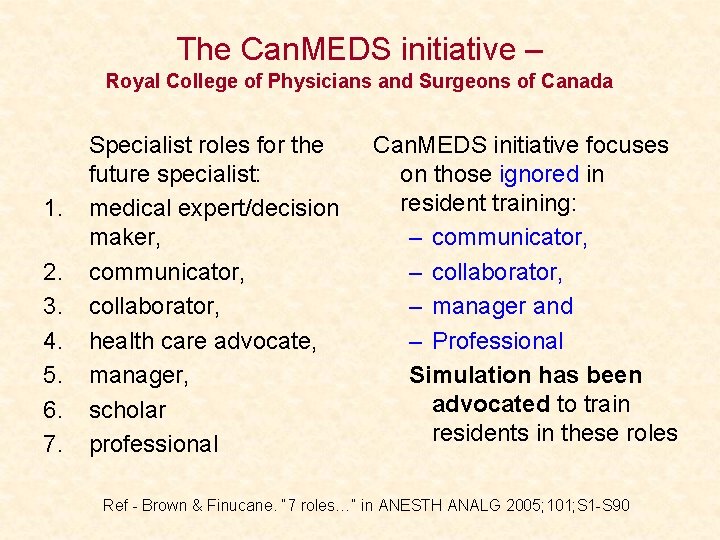
The Can. MEDS initiative – Royal College of Physicians and Surgeons of Canada 1. 2. 3. 4. 5. 6. 7. Specialist roles for the future specialist: medical expert/decision maker, communicator, collaborator, health care advocate, manager, scholar professional Can. MEDS initiative focuses on those ignored in resident training: – communicator, – collaborator, – manager and – Professional Simulation has been advocated to train residents in these roles Ref - Brown & Finucane. “ 7 roles…” in ANESTH ANALG 2005; 101; S 1 -S 90
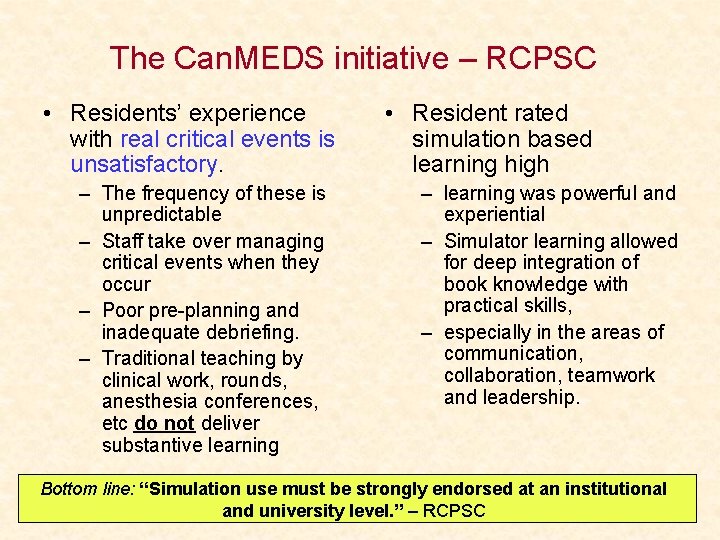
The Can. MEDS initiative – RCPSC • Residents’ experience with real critical events is unsatisfactory. – The frequency of these is unpredictable – Staff take over managing critical events when they occur – Poor pre-planning and inadequate debriefing. – Traditional teaching by clinical work, rounds, anesthesia conferences, etc do not deliver substantive learning • Resident rated simulation based learning high – learning was powerful and experiential – Simulator learning allowed for deep integration of book knowledge with practical skills, – especially in the areas of communication, collaboration, teamwork and leadership. Bottom line: “Simulation use must be strongly endorsed at an institutional and university level. ” – RCPSC
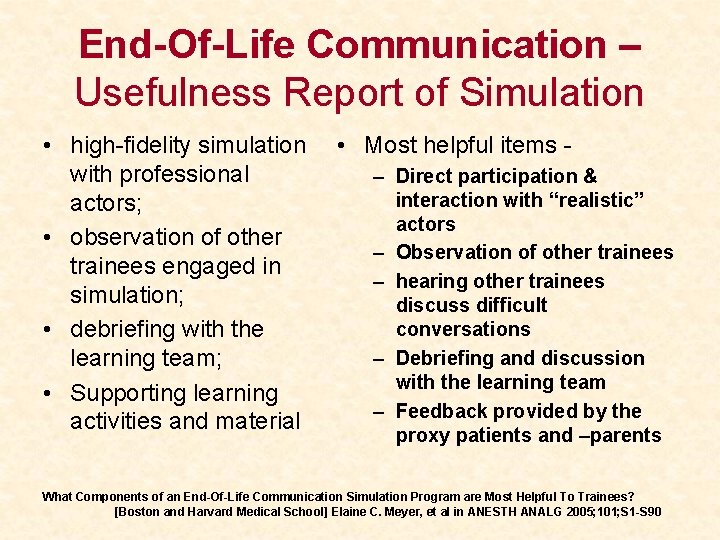
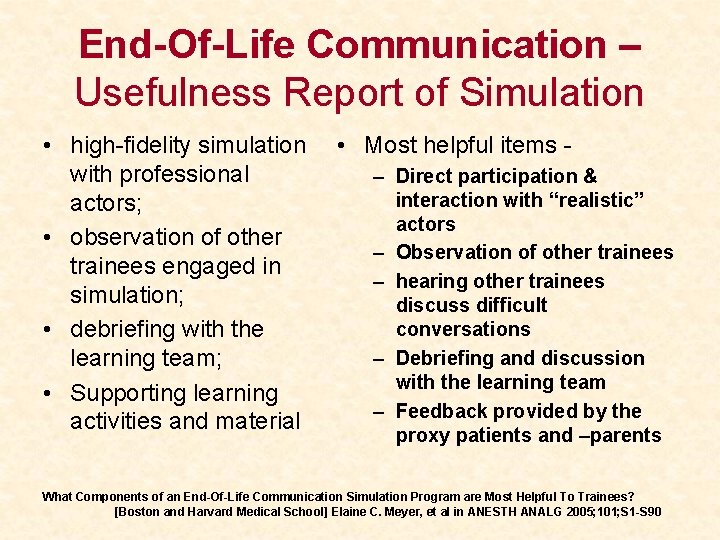
End-Of-Life Communication – Usefulness Report of Simulation • high-fidelity simulation with professional actors; • observation of other trainees engaged in simulation; • debriefing with the learning team; • Supporting learning activities and material • Most helpful items – Direct participation & interaction with “realistic” actors – Observation of other trainees – hearing other trainees discuss difficult conversations – Debriefing and discussion with the learning team – Feedback provided by the proxy patients and –parents What Components of an End-Of-Life Communication Simulation Program are Most Helpful To Trainees? [Boston and Harvard Medical School] Elaine C. Meyer, et al in ANESTH ANALG 2005; 101; S 1 -S 90
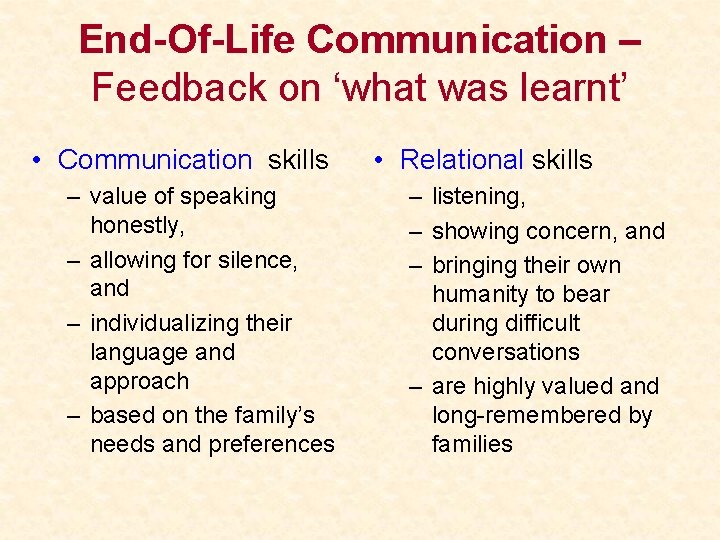
End-Of-Life Communication – Feedback on ‘what was learnt’ • Communication skills – value of speaking honestly, – allowing for silence, and – individualizing their language and approach – based on the family’s needs and preferences • Relational skills – listening, – showing concern, and – bringing their own humanity to bear during difficult conversations – are highly valued and long-remembered by families
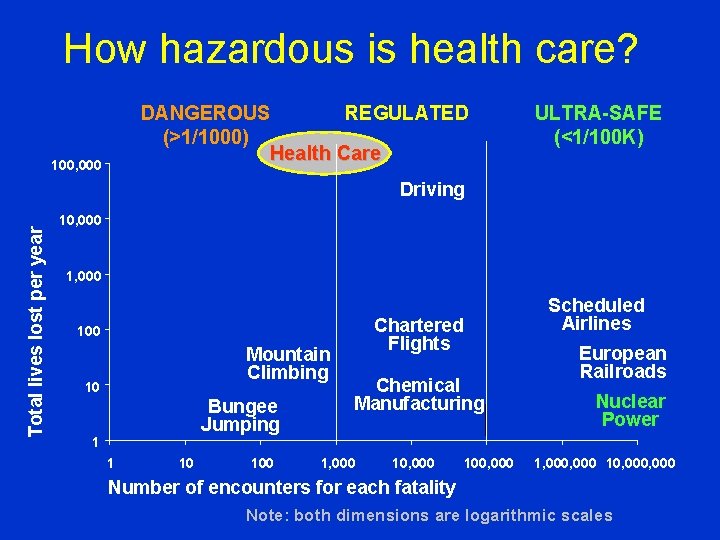
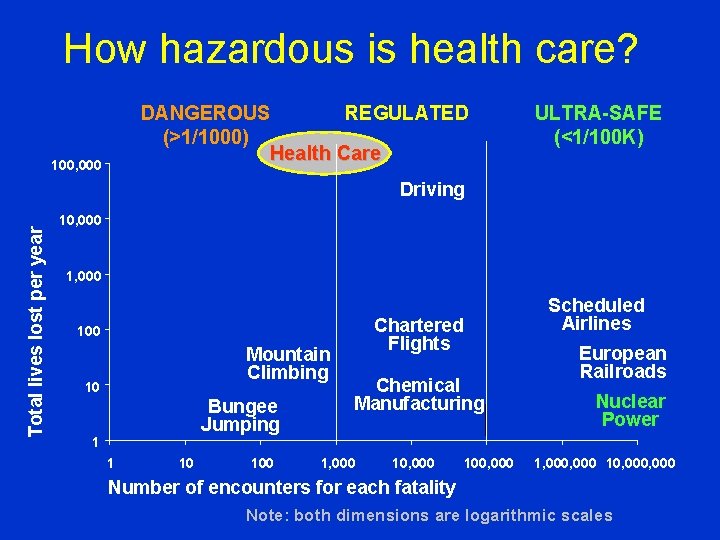
How hazardous is health care? DANGEROUS REGULATED (>1/1000) Health Care 100, 000 ULTRA-SAFE (<1/100 K) Total lives lost per year Driving 10, 000 1, 000 Chartered Flights 100 Mountain Climbing 10 Bungee Jumping 1 1 10 100 Scheduled Airlines Chemical Manufacturing 1, 000 100, 000 European Railroads Nuclear Power 1, 000 10, 000 Number of encounters for each fatality Note: both dimensions are logarithmic scales
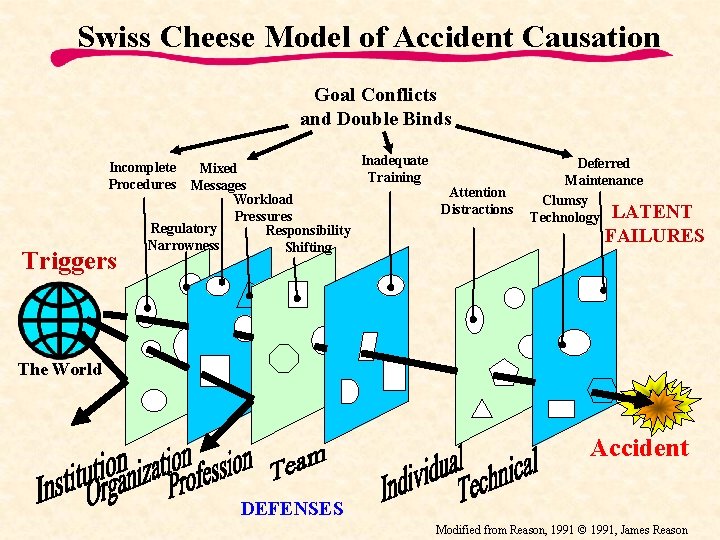
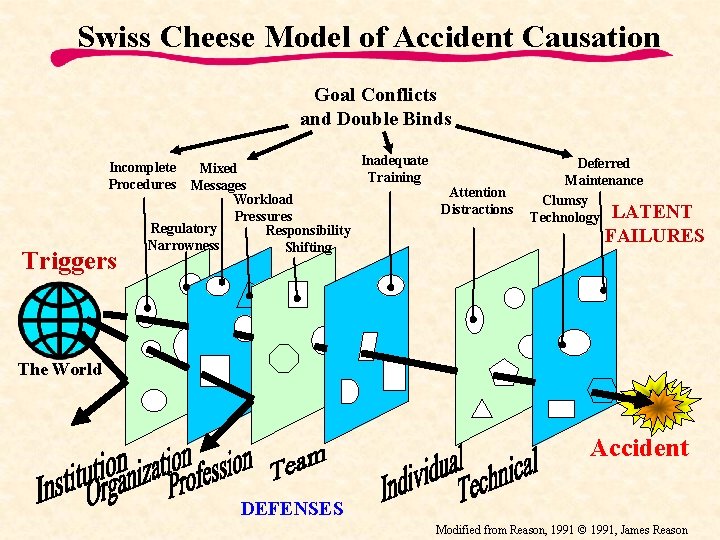
Swiss Cheese Model of Accident Causation Goal Conflicts and Double Binds Incomplete Procedures Triggers Mixed Messages Workload Pressures Regulatory Responsibility Narrowness Shifting Inadequate Training Attention Distractions Deferred Maintenance Clumsy Technology LATENT FAILURES The World Accident DEFENSES Modified from Reason, 1991 © 1991, James Reason
SBME is Now Becoming a Vital Need • Bristol Case of high mortality in Paed Card – The training of doctors in advanced procedures – How to approach the so called learning curve of doctors for standard procedures – How clinical competence and technical expertise are assessed and evaluated – How doctors explain risks to patients • GMC inquiry raised several such issues Editorial - All changed, changed utterly. BMJ 1998; 316: 1917 -1918
An Ethical Mandate for All • Patients are to be protected from all avoidable harm • They are not commodities to be used as conveniences of training Amitai Ziv, et al. Simulation-Based Medical Education: An Ethical Imperative. Acad. Med. 2003; 78: 783– 788.
Barriers to Student Access to Patients • Bedside teaching is in steady decline – Only about 50% were accessible – 35% (70% of above) agreed to give history – 34% agreed to be examined – Assessed by repeated cross-sectional audit – too few to provide current student population with extensive clinical experience • We must use Simulated Patient encounters Leslie G Olson et al. Barriers to student access to patients in a group of teaching hospitals. MJA 2005; 183 (9): 461 -463
SBME (Simulation-Based Medical Education) is an Ethical Imperative • Medical training must use live patients to hone the skills of health professionals. • But we have an obligation to ensure patients’ safety and well-being by providing optimal treatment. • Balancing these two creates ethical tension in medical education. • SBME can mitigate this tension by taking care of – best standards of care and training, – error management and patient safety, – patient autonomy, & – social justice
Simulation of Vaginal Birth for Third Year Harvard Medical Students • it is not unusual for students to complete their labor rotation without conducting a normal vaginal delivery. • The goal of this pilot program was to provide a realistic simulation of a normal & abnormal vaginal deliveries to students of 3 rd year. • Post-course evaluations were uniformly positive. • Sample comments include: – “Wonderful way to learn”; – “I forgot it was Friday evening”; and – “Great combo of didactics and teaching” Roxane Gardner et al. in ANESTH ANALG 2005; 101; S 1 -S 90
Simulations may be effective if used wisely • Evidence of the effectiveness of carefully implemented simulations: • A review of 109 studies looked at whether medical simulations actually facilitate learning. • The best available evidence shows a benefit for simulations when four conditions are met: 1. educational feedback is provided, 2. learners are given the opportunity for repetitive practice 3. exercises based on the simulation are integrated with the curriculum, & 4. tasks range in difficulty. Editorial – Med Teacher 2005; 27: 10 -28
Cynic is one who • Knows the Cost of Everything… but the Value of Nothing – Oscar Wilde
The Future of Simulation The IOM report made strong recommendations with regard to medical simulation: Ø “Establish interdisciplinary team training programs, such as simulation. . . ” Ø Use procedures to mitigate injury through simulation training. Ø Create a learning environment. “Use simulations whenever possible. ” Ø (IOM Report: To Err Is Human: Building a Safer Health System, Institute of Medicine. National Academy of Sciences. 1999)
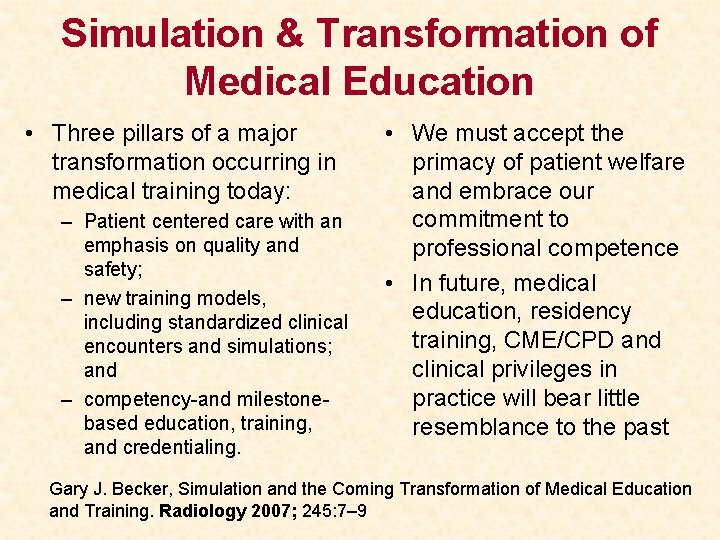
Simulation & Transformation of Medical Education • Three pillars of a major transformation occurring in medical training today: – Patient centered care with an emphasis on quality and safety; – new training models, including standardized clinical encounters and simulations; and – competency-and milestonebased education, training, and credentialing. • We must accept the primacy of patient welfare and embrace our commitment to professional competence • In future, medical education, residency training, CME/CPD and clinical privileges in practice will bear little resemblance to the past Gary J. Becker, Simulation and the Coming Transformation of Medical Education and Training. Radiology 2007; 245: 7– 9
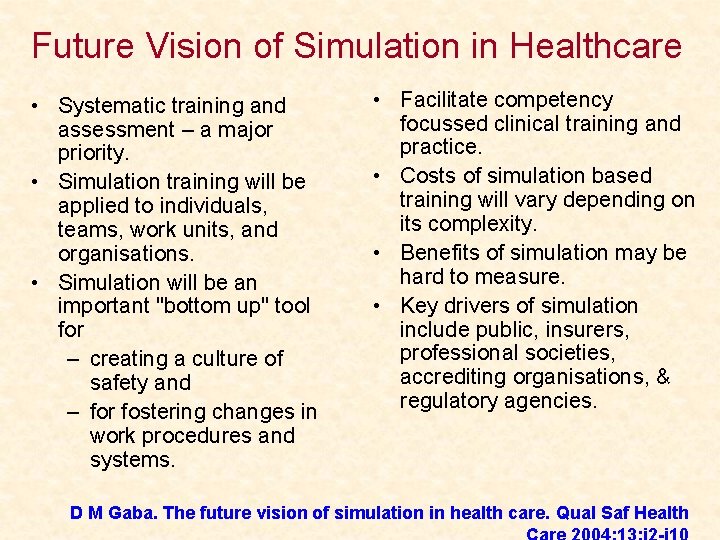
Future Vision of Simulation in Healthcare • Systematic training and assessment – a major priority. • Simulation training will be applied to individuals, teams, work units, and organisations. • Simulation will be an important "bottom up" tool for – creating a culture of safety and – for fostering changes in work procedures and systems. • Facilitate competency focussed clinical training and practice. • Costs of simulation based training will vary depending on its complexity. • Benefits of simulation may be hard to measure. • Key drivers of simulation include public, insurers, professional societies, accrediting organisations, & regulatory agencies. D M Gaba. The future vision of simulation in health care. Qual Saf Health

Vote for Simulation !