Urothelial carcinoma cancers of the bladder ureter renal

Urothelial carcinoma cancers of the bladder, ureter & renal pelvis S. VAHIDI Shahid rahnamoon hospital
Bladder carcinomas Incidence: • 2 Th most common cancers of G. U tract • 7% of new cancer cases in men & 2% of women • Average at diagnosis: 65 • At diagnosis time: 75% localized to the bladder
Bladder carcinoma Risk factors & pathogenesis -cigarette smoking: risk: two fold. (alpha & betanephthylamine) -occupational exposure(chemical-dyerubber, petroleum, leather and printing industries) Specific occupational carcinogenes: benzidine, βnephtylamine, 4 aminobiphenyl -cyclophosfamide, artifitial sweetners? -physical trauma: calculi, instrument, infection. -Genetic

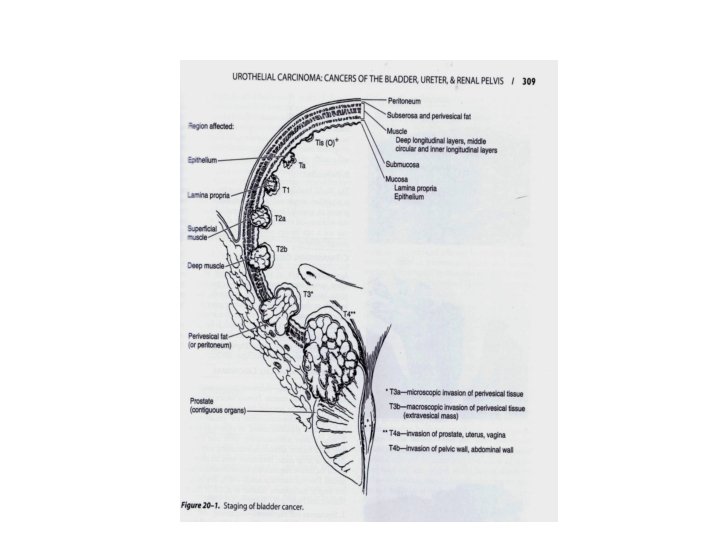
Bladder carcinoma Staging: TNM: the most commonly used staging system. nodal stage: NX: can not be assessed. N 0: no nodal metastasis. N 1: single node<2 cm N 2: node, nodes 2 -5 cm N 3: node, nodes>5 cm Metastasis stage: Mx: can not be defined M 0: no distant metastasis M 1: distant metastasis -clinical stage -pathologic stage overstaging: uncommon understaging: 53%
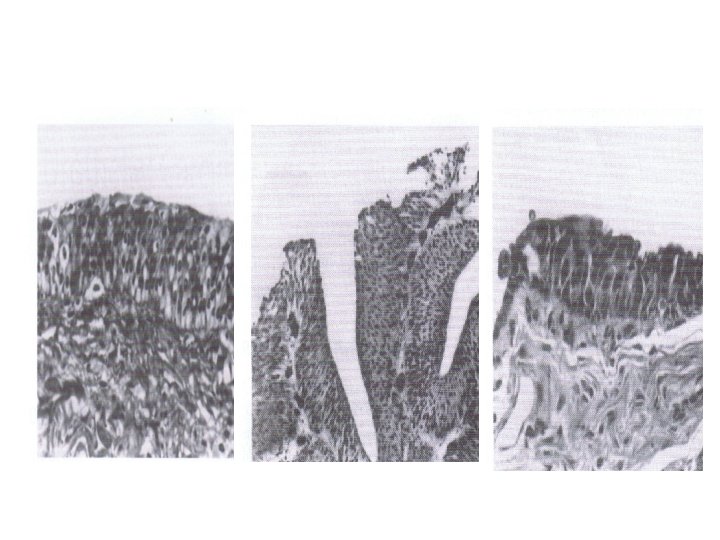
Bladder carcinoma Histopathology: -98% epithelial(most TCC) • normal urothelium. Papilloma: rare benigne condition. • Transitional cell carcinoma: 90% of all bladder cancers (papillary-sessile). Non transitional cell carcinomas -adencarcinoma<2% -squamous cell carcinoma 5 -10% -undifferentiated carcinoma -mixed carcinoma -Rare ep. & non ep. Cancers: melanoma-carcino sarcomacarcinoidtumor The most common tumor metastatic to bladder include: melanomastomach, breast, kidney, lung & liver
Clinical findings A: symptoms hematuria(presenting symptoms in 85 -90% of B. C. ) irritable symptoms of advanced disease B: Signes palpable mass, bladder wall thickening hepatomegaly, lymphadenopathylymphedema
Laboratory findings 1 - routin testing: hematuria, pyuria, azotemia, anemia 2 -urine cytology: high grade, cis 3 -other markers: BTA test. NMP 22. immunocyt, urovision, lewis x antigen (detect cancer specific proteins-augment cytology)
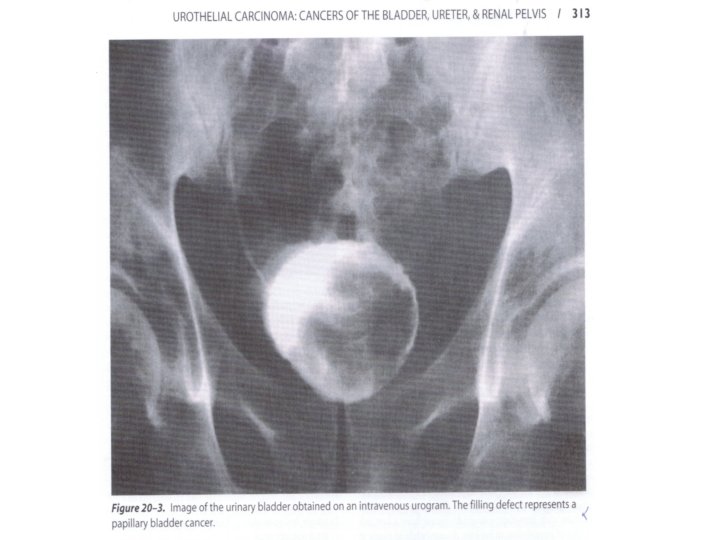
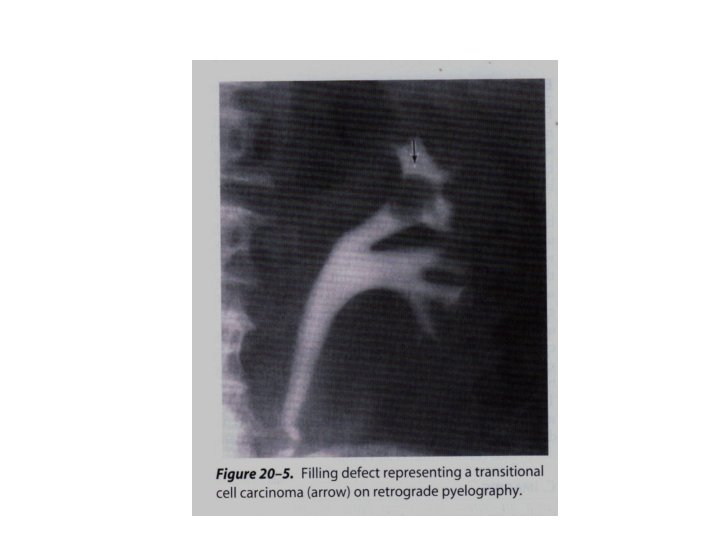
Immaging • Evaluation of upper urinary tract • Assess the depth of muscle wall infiltration & metastasis IVP, CT scan, MRI(40 -90% accuracy in staging), CXR -bone scan. (bone scan be avoided if Alk Ph is normal. )
Cystoscopy & tumor resection • For diagnosis, early staging & excision • Fluorescant cystoscopy with blue light: 20% enhamce detection • Random biopsy?
Natural history & selection of treatment • Natural history: tumor recurrence tumor progression • Treatment decisions are based on tumor stage & grade • At initial presentation: 50 -70% superficial 28% invasion to lamina propria 24% invasion to muscles *25% metastasis • 80% of patients with invasive or metastatic disease have no previous history of bladder cancer • Grade: (43% gi, 25%gii & 32%giii)
Natural history & selection of treatment • There are strong correlation between tumor grade & stage and tumor recurrence, progression and survival • In patient with organ-confined disease , the presence of pelvic lymph node metastasis appear to be the most important prognosis factor • Tumor recurrence is related to history of disease and grade, number and size of the tumor. it is more common in the first 12 -24 months after diagnosis • Tumor are high risk or low risk • Molecular markers: p 53 -Rb(retinoblastoma) gene.
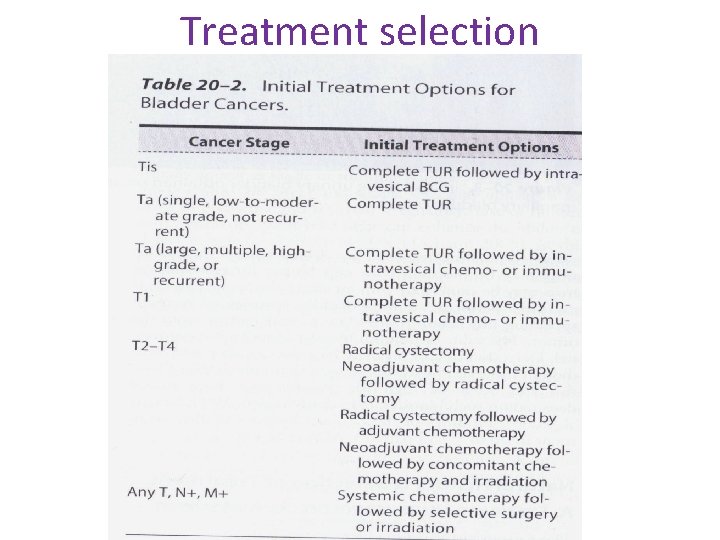
Treatment selection
Intravesical chemotherapy • Mitomycin c thiotepa BCG • Weekly for 6 week *mitomycinc: antibiotic-anti tumor alkylating agent, that inhibit DNA synthesis 40 mg/40 cc water or saline 39 -78% of patients with residual tumors→complete response Side effeets: 10 -43%( irritative voiding syptoms ) *thiotepa : alkylating agent 30 mg/week 55% complete response. Side effects: cystitis-myelosuppresion
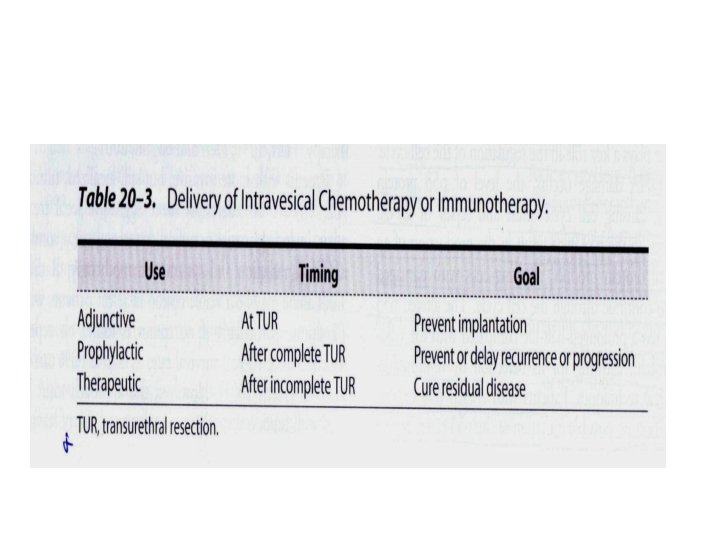
Intravesical chemotherapy *B. C. G. attenuated strain of mycobacterium bovis -mechanism of anti tumor effect: ? (immunologically mediated) -most efficacious for CIS Side effects: irritative voiding symptoms-hemorrhagic cystitis-distant infection *new intravesical agents and approachs: inter feronalpha, valrubicin
Surgery 1 -TUR-the initial form of treatment for all bladder cancers 2 -partial cystectomy: solitary, infiltrating tumors(T 1 –T 3)localized along the posterior lateral wall or dome of the bladder and tumor in diverticulum. 3 -radical cystectomy: men: bladder with surrounding fat and peritoneal attachments, prostate, seminal vesicles women: bladder, servix uterus. anterior vaginal vault-urethra and ovari “gold standard”treatment for patients with muscle invasive bladder cancer. 5 years disease free survival: 88%(po-p. A-pis) 80%(p 1 -p 2) 68%(p 3 a)-47%(p 3 b)
Radiotherapy 5000 -7000 CGY 5 -8 weeks period bowl, bladder, rectal complications in 15% 5 years survival rates: 18 -44% in T 2 , T 3 -radiation as monotherapy is usually offered only to those patient who are poor surgical candidate.
Chemotherapy • 15% of patients who present with bladder cancer and 30 -40% with invasive disease develop distant metastasis despite radical cystectomy or radiotherapy • Cisplatian, methotraxate, doxorubicin, vinblastine, cyc lophosphomid, gemcitabine and 5 -flurouracil • Combined therapy, (MVAC): 13 -35% complete response. • Newer agents: ifosfamide, gemcitabine, paclitaxel & galium nitrate
Combination therapy Neoadjuant chemotherapy Chemoradiotherapy Adjuant radiotherapy

- Slides: 25