Urogenital Tract Module Gonorrhea Lecture 3 Assoc Prof


- Slides: 33
Urogenital Tract Module Gonorrhea (Lecture 3) Assoc. Prof. Eman Albataineh Department of Microbiology and immunology Faculty of Medicine, Mu’tah University
Learning Objectives Upon completion of this content, you should know the: Epidemiology of gonorrhea Pathogenesis of gonorrhea Clinical manifestations of gonorrhea Common methods used in the diagnosis of gonorrhea Prevention of gonorrhea
History • Neisseria gonorrhoeae described by Albert Neisser in 1879 • Observed in smears of purulent exudates of urethritis, cervicitis, opthalmia neonatorum • Thayer Martin medium enhanced isolation of gonococcus in 1960
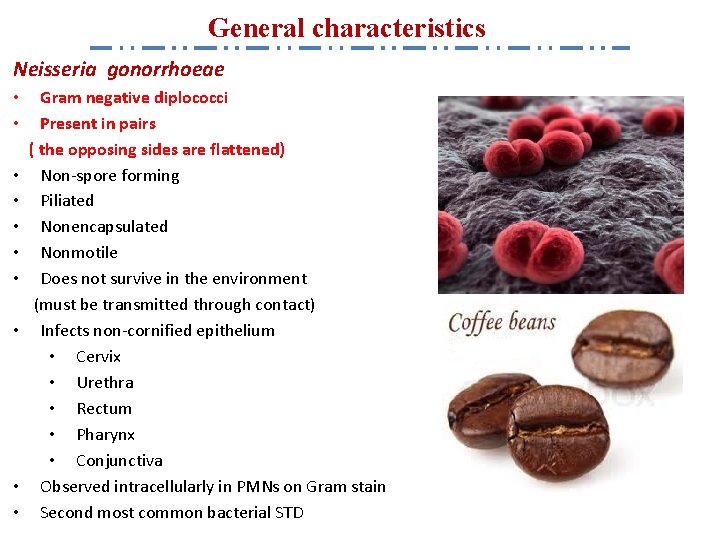
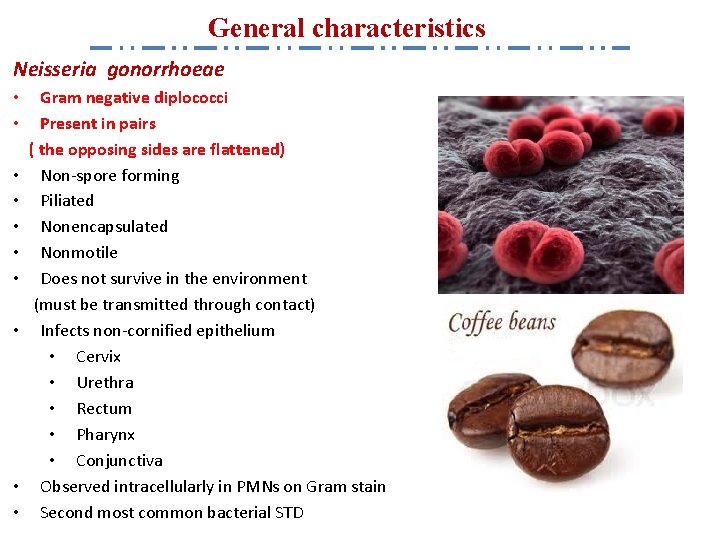
General characteristics Neisseria gonorrhoeae • • • Gram negative diplococci Present in pairs ( the opposing sides are flattened) Non-spore forming Piliated Nonencapsulated Nonmotile Does not survive in the environment (must be transmitted through contact) Infects non-cornified epithelium • Cervix • Urethra • Rectum • Pharynx • Conjunctiva Observed intracellularly in PMNs on Gram stain Second most common bacterial STD
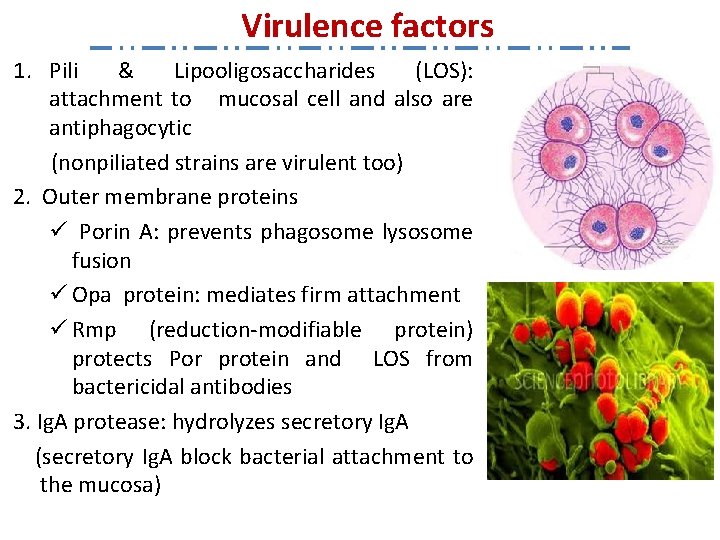
Virulence factors 1. Pili & Lipooligosaccharides (LOS): attachment to mucosal cell and also are antiphagocytic (nonpiliated strains are virulent too) 2. Outer membrane proteins ü Porin A: prevents phagosome lysosome fusion ü Opa protein: mediates firm attachment ü Rmp (reduction-modifiable protein) protects Por protein and LOS from bactericidal antibodies 3. Ig. A protease: hydrolyzes secretory Ig. A (secretory Ig. A block bacterial attachment to the mucosa)
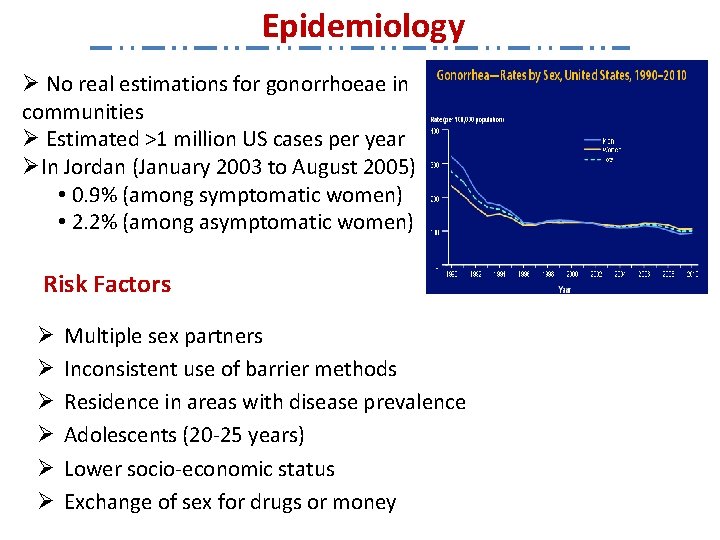
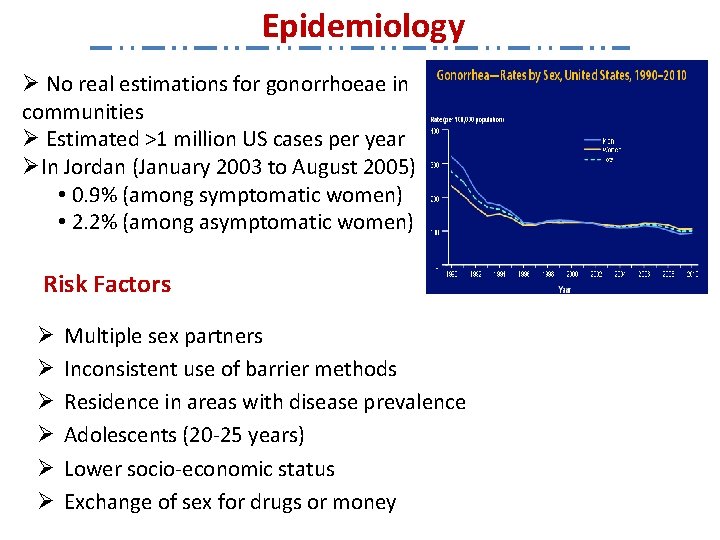
Epidemiology Ø No real estimations for gonorrhoeae in communities Ø Estimated >1 million US cases per year ØIn Jordan (January 2003 to August 2005) • 0. 9% (among symptomatic women) • 2. 2% (among asymptomatic women) Risk Factors Ø Ø Ø Multiple sex partners Inconsistent use of barrier methods Residence in areas with disease prevalence Adolescents (20 -25 years) Lower socio-economic status Exchange of sex for drugs or money
Epidemiology Transmission Ø Asymptomatic patients are the major source of infections (infectious for several months) Ø Greater efficiency of transmission from male to female • Male to female: 50 – 90% • Female to male: 20 – 80% Ø Rectal oral transmission Ø Perinatal transmission (mother to infant)
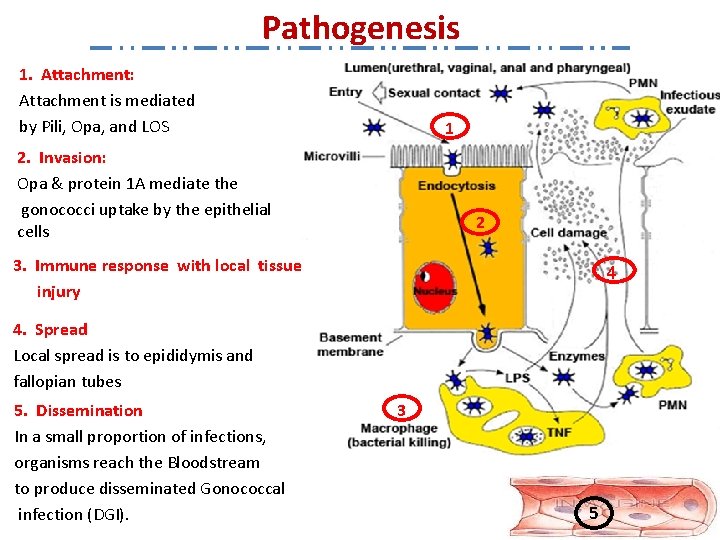
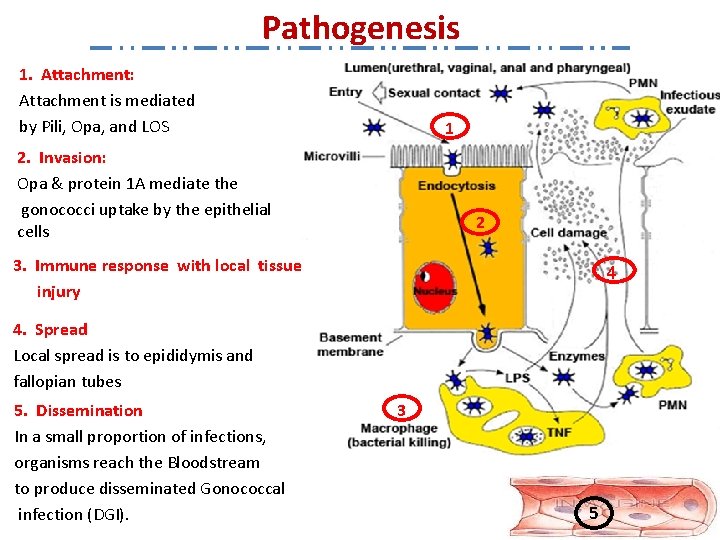
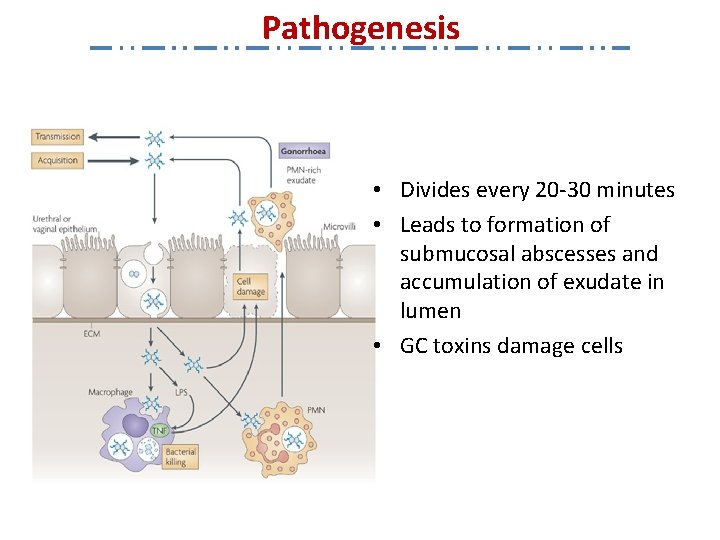
Pathogenesis 1. Attachment: Attachment is mediated by Pili, Opa, and LOS 1 2. Invasion: Opa & protein 1 A mediate the gonococci uptake by the epithelial cells 2 3. Immune response with local tissue injury 4 4. Spread Local spread is to epididymis and fallopian tubes 5. Dissemination In a small proportion of infections, organisms reach the Bloodstream to produce disseminated Gonococcal infection (DGI). 3 5
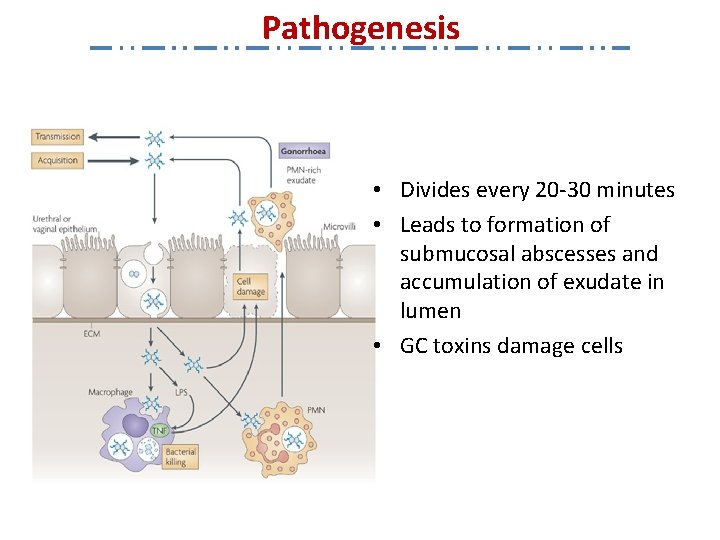
Pathogenesis • Divides every 20 -30 minutes • Leads to formation of submucosal abscesses and accumulation of exudate in lumen • GC toxins damage cells
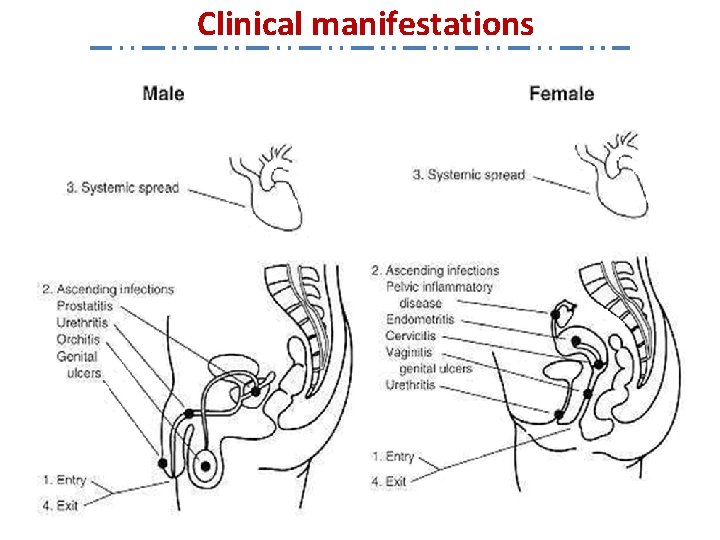
Clinical manifestations Levels of Gonococcal infection
Clinical manifestations 1. Genital Infection In men: a- Urethritis Ø Urethra is the primary infection site Ø 2 -7 days incubation period Ø Symptoms – frequency, urgency, dysuria – purulent urethral dischargethick white or yellow/greenish discharge – blood in the semen or urine Ø Asymptomatic in 10% of cases Ø Male seeks treatment early preventing serious complications, but not soon enough to prevent transmission to other sex partners
Clinical manifestations 1. Genital Infection In men: b. Epididymitis Ø Signs and symptoms • abdominal or lower back pain • fever, nausea • testicular pain and swelling • discharge from the urethra • pain on urination, occasionally blood in the urine
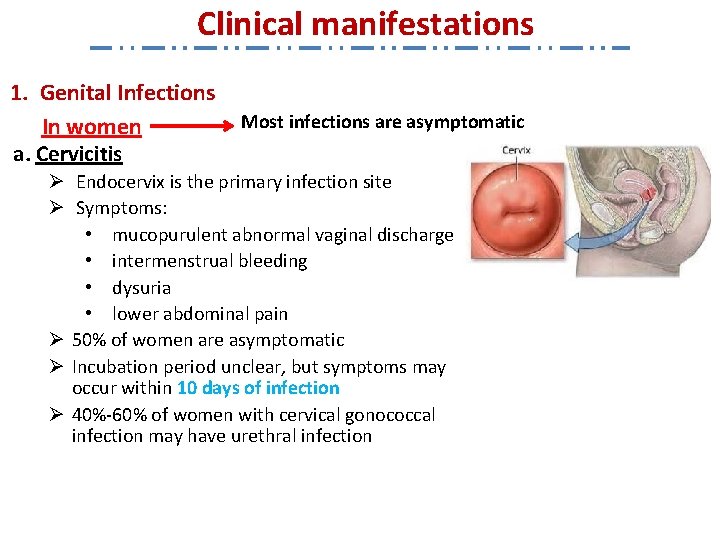
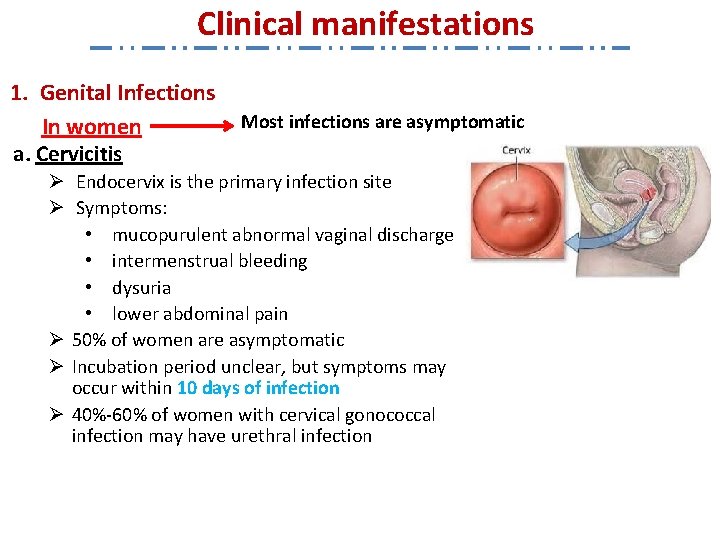
Clinical manifestations 1. Genital Infections In women a. Cervicitis Most infections are asymptomatic Ø Endocervix is the primary infection site Ø Symptoms: • mucopurulent abnormal vaginal discharge • intermenstrual bleeding • dysuria • lower abdominal pain Ø 50% of women are asymptomatic Ø Incubation period unclear, but symptoms may occur within 10 days of infection Ø 40%-60% of women with cervical gonococcal infection may have urethral infection
Clinical manifestations 1. Genital Infections In women b. Urethritis Ø Inflammation of the urethra Ø Symptoms • frequency, urgency, dysuria • Pain during sex • Discharge from the urethral opening or vagina 14
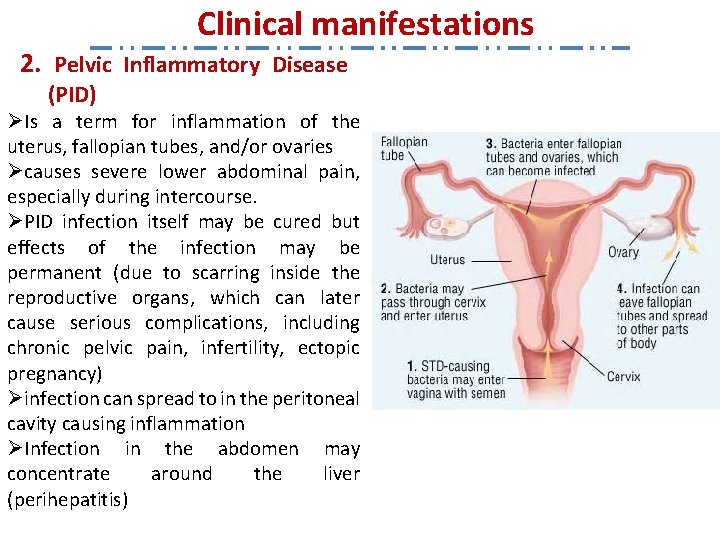
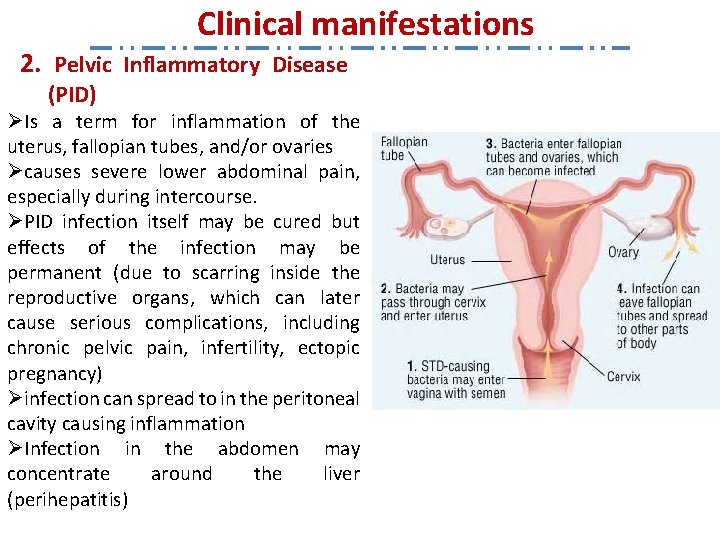
Clinical manifestations 2. Pelvic Inflammatory Disease (PID) ØIs a term for inflammation of the uterus, fallopian tubes, and/or ovaries Øcauses severe lower abdominal pain, especially during intercourse. ØPID infection itself may be cured but effects of the infection may be permanent (due to scarring inside the reproductive organs, which can later cause serious complications, including chronic pelvic pain, infertility, ectopic pregnancy) Øinfection can spread to in the peritoneal cavity causing inflammation ØInfection in the abdomen may concentrate around the liver (perihepatitis)
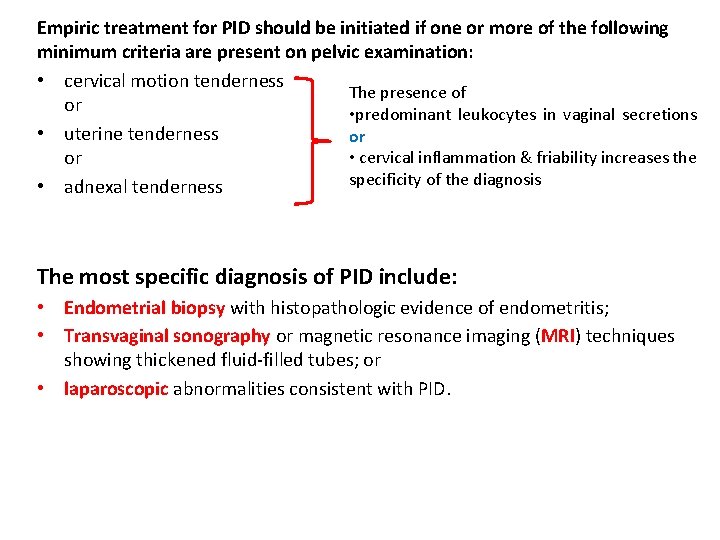
Empiric treatment for PID should be initiated if one or more of the following minimum criteria are present on pelvic examination: • cervical motion tenderness The presence of or • predominant leukocytes in vaginal secretions • uterine tenderness or • cervical inflammation & friability increases the or specificity of the diagnosis • adnexal tenderness The most specific diagnosis of PID include: • Endometrial biopsy with histopathologic evidence of endometritis; • Transvaginal sonography or magnetic resonance imaging (MRI) techniques showing thickened fluid-filled tubes; or • laparoscopic abnormalities consistent with PID.
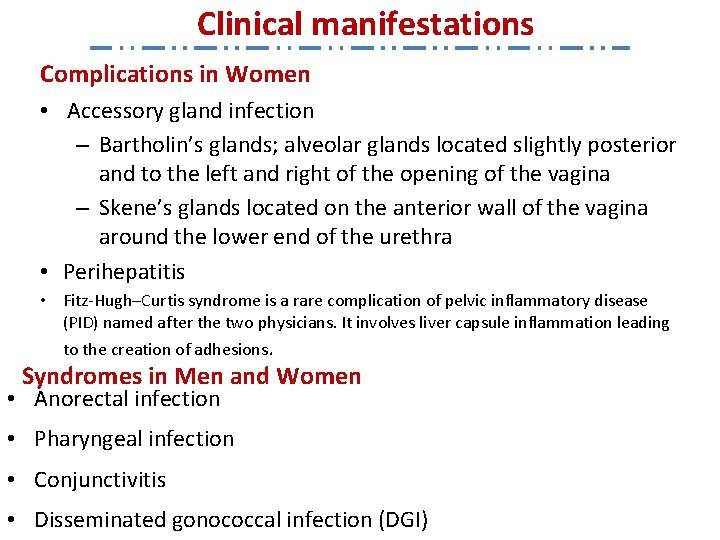
Clinical manifestations Complications in Women • Accessory gland infection – Bartholin’s glands; alveolar glands located slightly posterior and to the left and right of the opening of the vagina – Skene’s glands located on the anterior wall of the vagina around the lower end of the urethra • Perihepatitis • Fitz-Hugh–Curtis syndrome is a rare complication of pelvic inflammatory disease (PID) named after the two physicians. It involves liver capsule inflammation leading to the creation of adhesions. Syndromes in Men and Women • Anorectal infection • Pharyngeal infection • Conjunctivitis • Disseminated gonococcal infection (DGI)
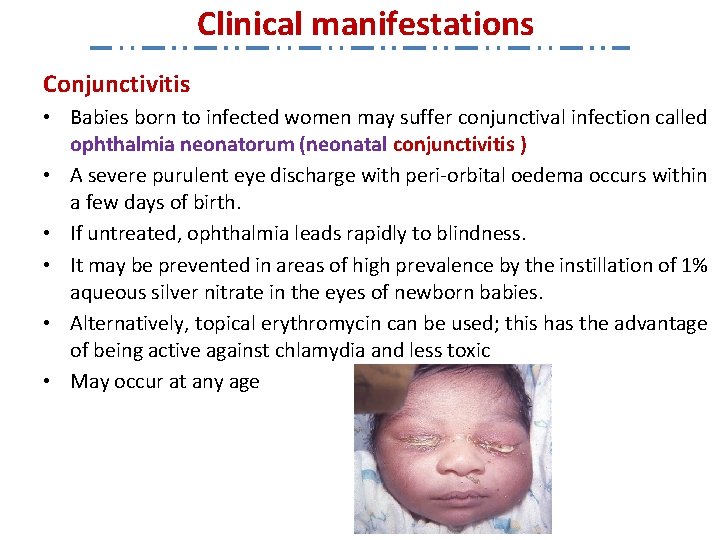
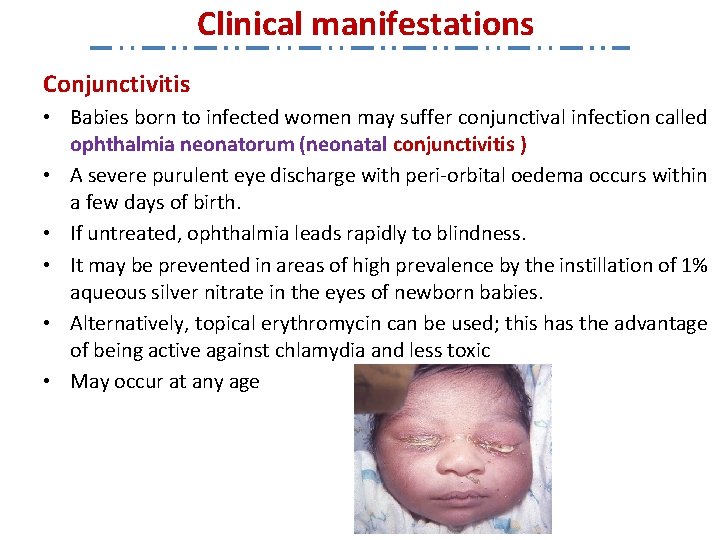
Clinical manifestations Conjunctivitis • Babies born to infected women may suffer conjunctival infection called ophthalmia neonatorum (neonatal conjunctivitis ) • A severe purulent eye discharge with peri-orbital oedema occurs within a few days of birth. • If untreated, ophthalmia leads rapidly to blindness. • It may be prevented in areas of high prevalence by the instillation of 1% aqueous silver nitrate in the eyes of newborn babies. • Alternatively, topical erythromycin can be used; this has the advantage of being active against chlamydia and less toxic • May occur at any age
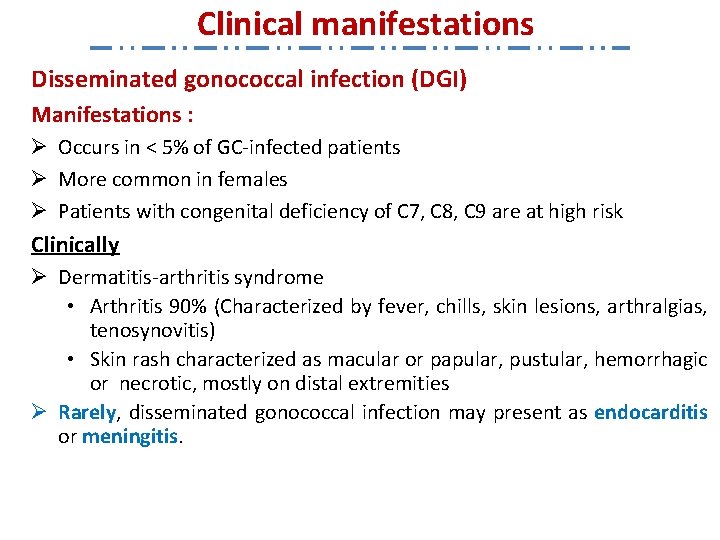
Clinical manifestations Disseminated gonococcal infection (DGI) Manifestations : Ø Occurs in < 5% of GC-infected patients Ø More common in females Ø Patients with congenital deficiency of C 7, C 8, C 9 are at high risk Clinically Ø Dermatitis-arthritis syndrome • Arthritis 90% (Characterized by fever, chills, skin lesions, arthralgias, tenosynovitis) • Skin rash characterized as macular or papular, pustular, hemorrhagic or necrotic, mostly on distal extremities Ø Rarely, disseminated gonococcal infection may present as endocarditis or meningitis.

DGI Skin Lesion
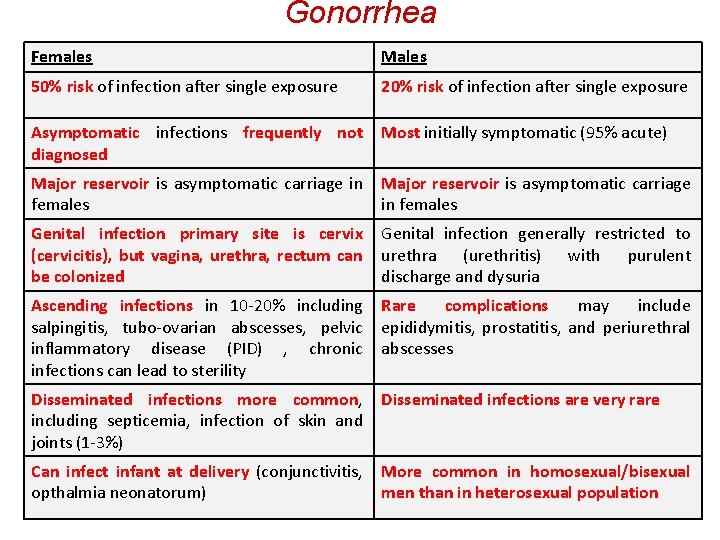
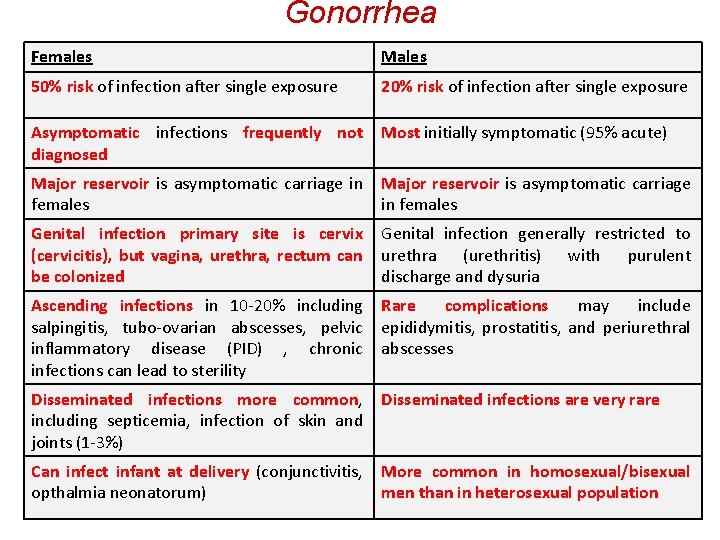
Gonorrhea Females Males 50% risk of infection after single exposure 20% risk of infection after single exposure Asymptomatic infections frequently not diagnosed Most initially symptomatic (95% acute) Major reservoir is asymptomatic carriage in females Genital infection primary site is cervix (cervicitis), but vagina, urethra, rectum can be colonized Genital infection generally restricted to urethra (urethritis) with purulent discharge and dysuria Ascending infections in 10 -20% including salpingitis, tubo-ovarian abscesses, pelvic inflammatory disease (PID) , chronic infections can lead to sterility Rare complications may include epididymitis, prostatitis, and periurethral abscesses Disseminated infections more common, including septicemia, infection of skin and joints (1 -3%) Disseminated infections are very rare Can infect infant at delivery (conjunctivitis, opthalmia neonatorum) More common in homosexual/bisexual men than in heterosexual population
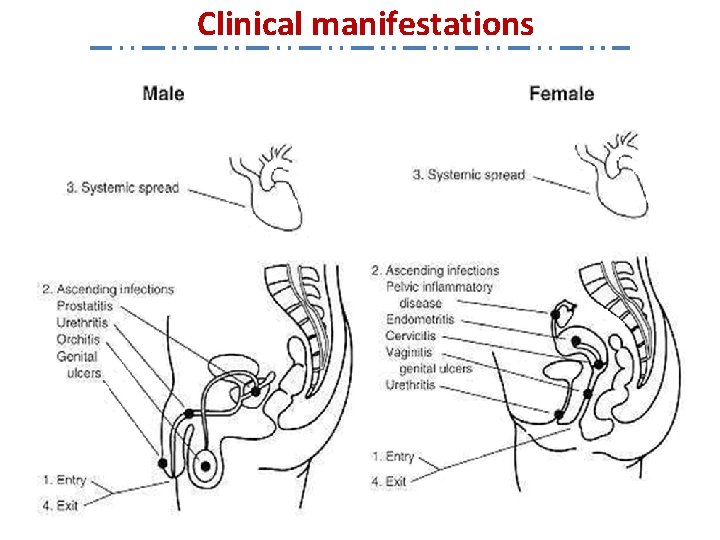
Clinical manifestations
Diagnosis Type of specimens ü Discharge swab tests ü Urine tests ü Cervix swab test ü Throat swab Methods of diagnosis 1. Staining 2. Culture 3. Direct detection
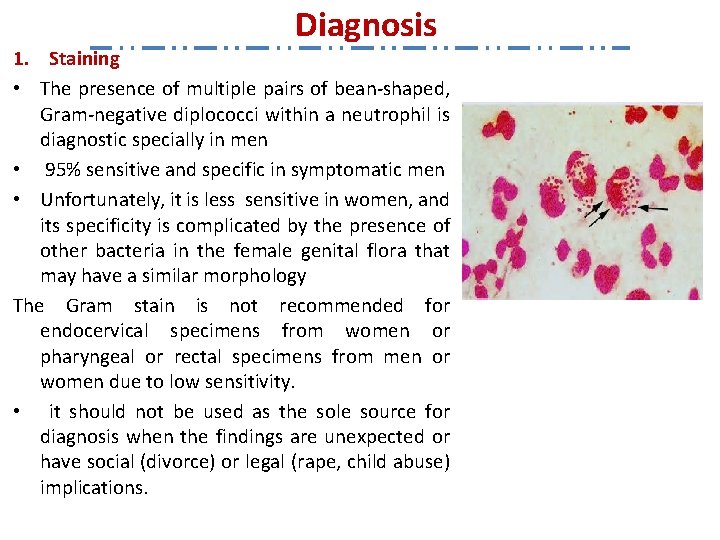
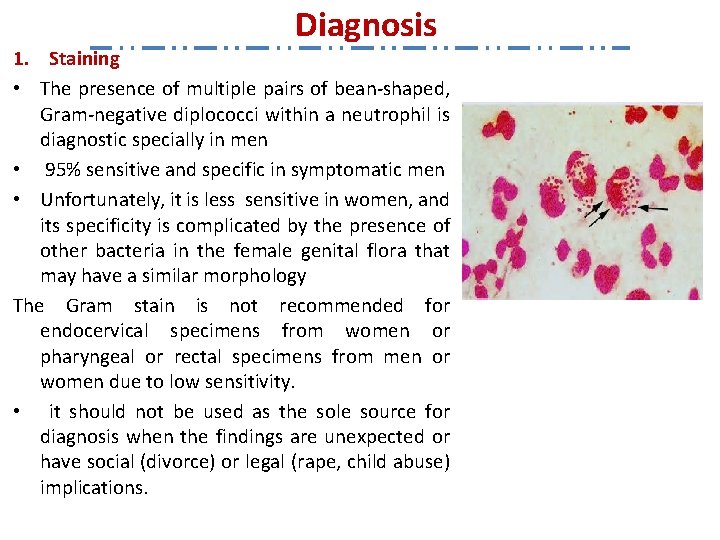
Diagnosis 1. Staining • The presence of multiple pairs of bean-shaped, Gram-negative diplococci within a neutrophil is diagnostic specially in men • 95% sensitive and specific in symptomatic men • Unfortunately, it is less sensitive in women, and its specificity is complicated by the presence of other bacteria in the female genital flora that may have a similar morphology The Gram stain is not recommended for endocervical specimens from women or pharyngeal or rectal specimens from men or women due to low sensitivity. • it should not be used as the sole source for diagnosis when the findings are unexpected or have social (divorce) or legal (rape, child abuse) implications.
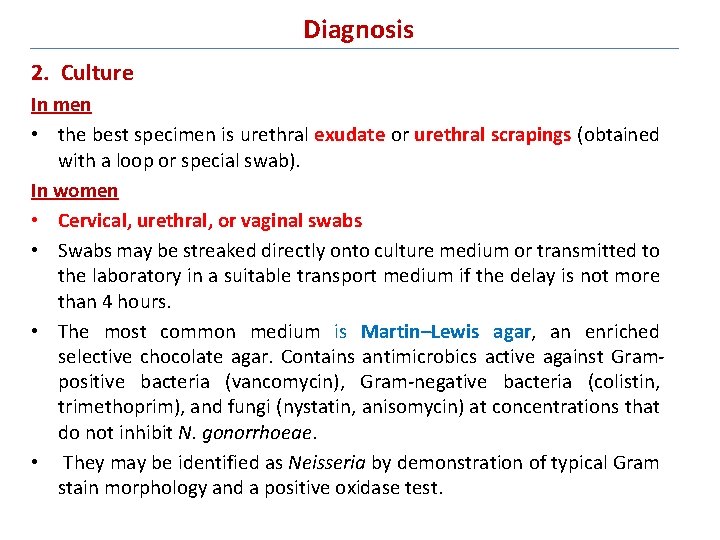
Diagnosis 2. Culture In men • the best specimen is urethral exudate or urethral scrapings (obtained with a loop or special swab). In women • Cervical, urethral, or vaginal swabs • Swabs may be streaked directly onto culture medium or transmitted to the laboratory in a suitable transport medium if the delay is not more than 4 hours. • The most common medium is Martin–Lewis agar, an enriched selective chocolate agar. Contains antimicrobics active against Grampositive bacteria (vancomycin), Gram-negative bacteria (colistin, trimethoprim), and fungi (nystatin, anisomycin) at concentrations that do not inhibit N. gonorrhoeae. • They may be identified as Neisseria by demonstration of typical Gram stain morphology and a positive oxidase test.
culture • Requires prompt placement in high-CO 2 environment (candle jar, bag and pill, CO 2 incubator) • In cases of suspected sexual abuse, culture is the only test accepted for legal purposes

GC Culture After 24 Hours
Diagnosis 3. Direct detection DNA amplification methods that detecting gonococci in clinical specimens without culture Vaccine • Hard to develop – No animal model • No immune memory to Neisseria gonorrhoeae – Antigenic variation strategy • Difficulty finding target common to all strains • Research continues to identify possible vaccine targets – DNA vaccines – Mucosal immunization
Gonorrhea Treatment Genital & Rectal Infections in Adults Recommended regimens: n n n Cefixime 400 mg PO x 1 or Ceftriaxone 125 mg IM x 1 or Ciprofloxicin 500 mg PO x 1 or Ofloxacin 400 mg PO x 1 or Levofloxacin 500 mg PO x 1 PLUS if chlamydia is not ruled out: n Doxycycline 100 mg PO BID x 7 d All sex partners within past 60 days need evaluation and treatment CDC 2002 Guidelines
Gonorrhea Treatment Pregnancy Must avoid quinolones & tetracycline Recommended regimens: u Cefixime 400 mg PO x 1 u Ceftriaxone 125 mg IM x 1 PLUS if chlamydia is not ruled out: u u Azithromycin 1 g PO x 1 Other appropriate chlamydial regimen Test of cure in 3 -4 weeks Cal. STDCB 2001 CDC 2002 Guidelines
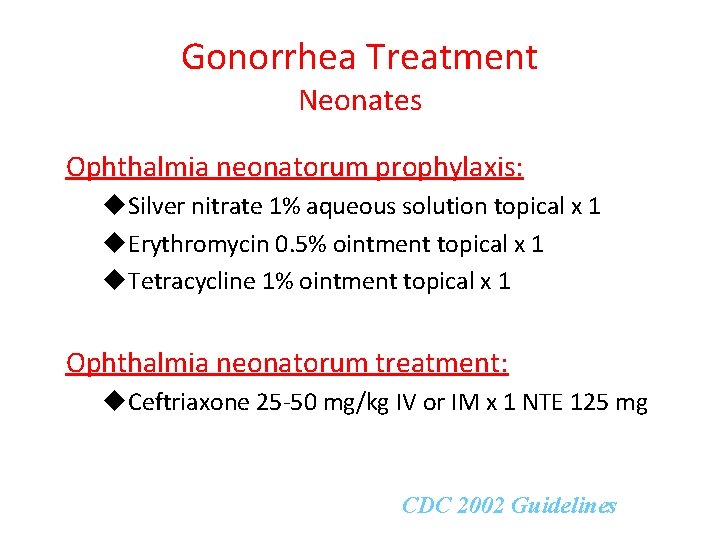
Gonorrhea Treatment Neonates Ophthalmia neonatorum prophylaxis: u. Silver nitrate 1% aqueous solution topical x 1 u. Erythromycin 0. 5% ointment topical x 1 u. Tetracycline 1% ointment topical x 1 Ophthalmia neonatorum treatment: u. Ceftriaxone 25 -50 mg/kg IV or IM x 1 NTE 125 mg NTE = not to exceed CDC 2002 Guidelines
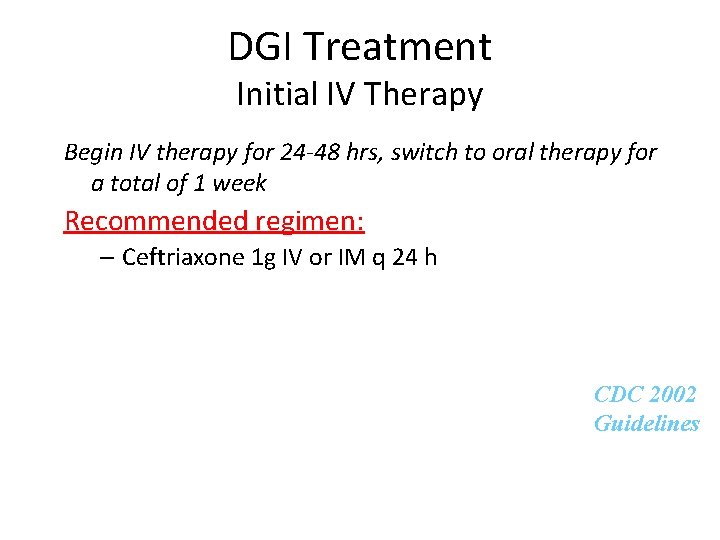
DGI Treatment Initial IV Therapy Begin IV therapy for 24 -48 hrs, switch to oral therapy for a total of 1 week Recommended regimen: – Ceftriaxone 1 g IV or IM q 24 h CDC 2002 Guidelines
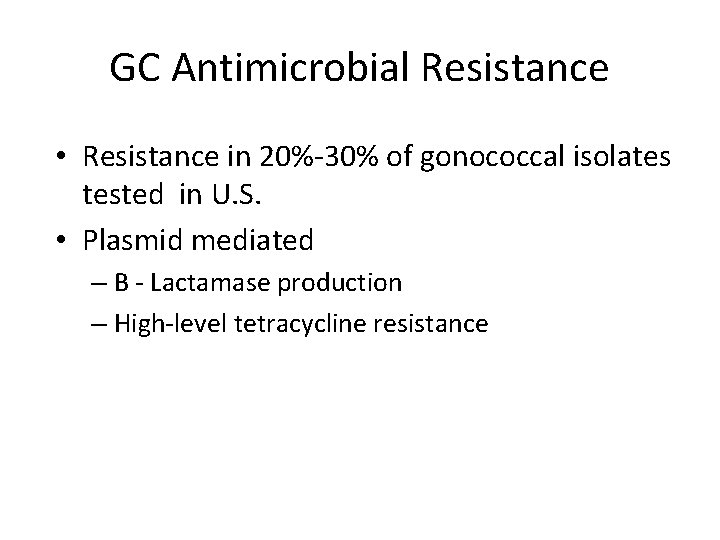
GC Antimicrobial Resistance • Resistance in 20%-30% of gonococcal isolates tested in U. S. • Plasmid mediated – B - Lactamase production – High-level tetracycline resistance