UROGENITAL SYSTEM Kidney Ureter PREPARED BY DR PANCHAJANI
UROGENITAL SYSTEM Kidney & Ureter PREPARED BY DR. PANCHAJANI. R
Kidney ANATOMY • Situated retroperitonially in the posterior abdominal wall one on each side of vertebral column. • Extends from upper border of T 12 to the centre of the body of L 3 vertebra. • 11 cm long , 6 cm broad, 3 cm thick, lateral border convex, medial border concave with a hylum. • Structures in hylum – renal artery , renal vein, renal pelvis. • upper pole –suprarenal gland, • lower pole- 1 inch above iliac crest • Capacity of renal pelvis- 10 ml
Kidney • Renal angle- angle between the 12 thrib & outer border of sacrospinalis. Pressure over this point elicits pain in kidney lesions. • Hepato renal pouch- related to upper pole of kidney. collection of extravasated fluid in this pouch following liver& biliary tract surgeries. • Outer brownish cortex , inner pale medulla • Pelvis divides 2 -3 major calyces which then divides in to 713 minor calyces. • Each kidney – 1 -3 million Uriniferous tubules, each has a Collecting part(Collecting tubule) & Secretory part( Nephrones )
Kidney • Blood supply- Renal artery arises from abdominal aorta. (between L 1 -L 2) • 95% of abdominal aneurism arises below the level of origin of Renal artery. • Nerve supply- T 10, 11, 12 • Lymphatic drainage- Para-aortic nodes.

URETER • 25 - 30 cm long, 3 -4 mm in diameter. • Begins with in the renal sinus as a funnel -shaped dilatation called renal pelvis. It open at the lateral wall of the trigone of the urinary bladder. Not attached to any fixed structures. so easily displaced or obstructed • In females uterine artery crosses the ureter about 2 cm lateral to the cervix. (important in hysterectomy) • Normal sites of constrictions - PUJ, At the brim of lesser pelvis, Along its passage through the bladder wall. • Arterial supply – upper- branches of renal & adrenal arteries, middle- branches of arteries of posterior abdominal wall. Lower(pelvic part) - branches of internal iliac arteries • The mean size of ureters on obstructed side was 7 mm, stones less than or about 5 mm in size can pass through the urinary tract on their own.
INVESTIGATIONS 1. 2. 3. • • Blood – RFT- urea, creatinine, BUN, Urine - microscopic, macroscopic, cytological, bacteriological, biochemical Plain X-ray-- KUB Taken in supine position which cover pubic symphysis & lower 2 ribs Bony parts looked any abnormality Kidney shadow- visualized in plain x-ray KUB due to difference in the density between kidney (high vascularity) & perinephric fat(low vascularity). Findings noted are size, location, calcification & stones. Perinephric fat is absent in children so kidney shadows are not visualized. Psoas shadow visualised in normal KUB. Obliterated in enlarged kidney, TB spine, psoasabscess, scoliosis, Ca, splenic injury. Ureteric line– looked for any radio opaque shadow( ureteric stone ) Any lesion in bladder, prostate, urethral areas.
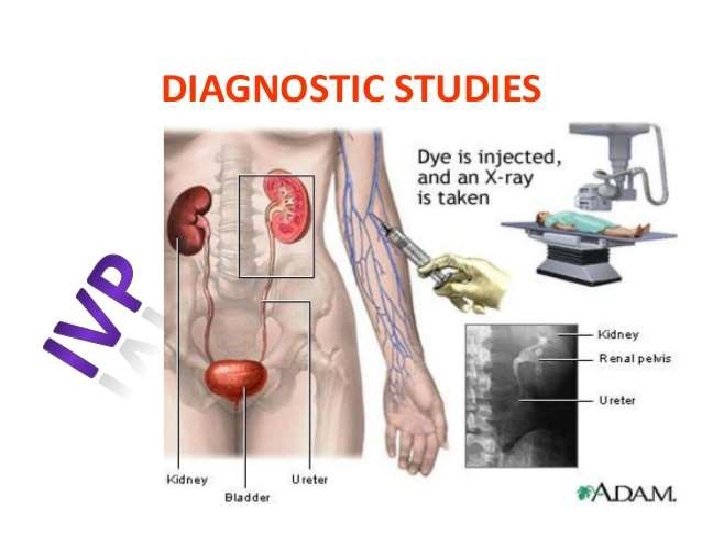
Investigations 4. Intra venous urogram (IVU/IVP) • Renal fuction must be normal • Hydronephrosis - clubbing of calyces • Hoarse shoe kidney - flower vase appearance • Ureterocele - cobra head appearance • Poly cystic kidney - spider leg appearance • RCC - irregular filling defect, spider leg • To see functions of kidney in stones , obstructions.

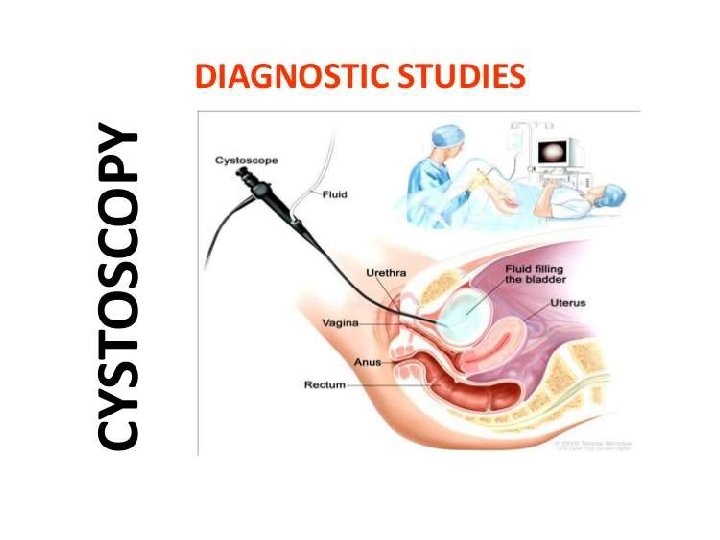
Investigations 3. Retrograde pylography(RGP) Urinary TB, Urothelial tumours 4. Renal angiogram Indications • Renal artery stenosis, RA atheroma, RA aneurysm , RCC • Arterial anomalies 5. Micturating cysto urethrography (MCU) Indications • Vescico ureteric reflux • Posterior urethral valves 6. Ascending urethrogram • Stricture urethra • USG - High resolution for size, thickness, obstructions • Trans rectal USG- for Ca prostate • CT, MRI, Isotope Renography, Cystoscopy
HAEMATURIA Gross – visible Microscopic-More than 5 RBC ‘S/ HPF • Early(initial) H – urethral origin distal to external sphincter • Terminal H - Bladder neck or prostate origin • Diffuse(total) – in the bladder or upper urinary tract • False H - Discolouration of urine from pigments such as food colouring and myoglobin • Silent H - Tumour of kidney or bladder
Haematuria – causes • • • Renal injury Urinary stones Wilm’s tumour TB RCC Cystitis Bladder tumour Urinary bilharziasis BPH, Ca prostrate Renal infart Glomerulonephritis Blood dyscrasias
Haematuria – investigations • Urine R/E, C&S • USG- Stones, tumours • Cystourethroscopy- for bladder& urethral pathology • IVU- for functions of kidney • Urinary cytology- for malignancy • BT, CT, Platelet count • CT abdomen • RFT Management- cause should be identified & treated
Hoarse shoe kidney • fusion of lower pole common • common site -in front of the 4 th lumbar vertibrae • Mass in the mid line of 4 th lumbar vertebrae • IVU – medialisation of lower calyces & curving of ureter like a flower vase •
Poly cystic kidney • Bilateral • Occurs at the junction of distal tubule and the collecting duct • Renal mass moves with respiration, ballotable, movable • 75% - hypertension, 25% haematuria • IVU- Spider leg pattern with an elongated compressed renal pelvis, narrowed & stretched calyces.

Retrocaval ureter • Developmental defect of IVC, right ureter passes behind the IVC, right hydronephrosis with hydroureter. • IVU - Hydronephrosis with reverse J sign • Treatment( Tt) - Anderson Hynes operation
URETEROCELE • Cystic enlargement of the intra mural portion of ureter due to congenital atresia of the ureteric orifice. • IVU - Adder head or cobra head appearance. • Cystoscopy – transluscent thin walled cyst surrounding the ureteric orifice • Tt. - Cystoscopic ureteric meatotomy. •
Renal injuries • Associated with Blunt injury abdomen • It is extraperitoneal Types- • small & large subcapsular • Cortical laceration • Laceration with haematoma • Medullary laceration with bleeding in to pelvis • Cortico - medullary complete laceration • Hilar injury – most dangerous
Renal injuries Clinical features • Features of Shock • Haematuria , sometimes delayed profuse haemorrhage ( haematuria between 3 rd day & 3 rd week), clot colic • Swelling & tenderness in loin. • Paralytic ileus with abdominal distension
Renal injuries Investigations • CT Scan - Grading of injury, Associated injuries, functions of kidney. • USG Abdomen - site& type of injury. , haemoperitoneum, associated injuries, effect of therapy by repeating it. • IVU - Functions of injured& normal Kidney , • RFT - Blood Urea, Creatinine, electrolytes, haematocrit, blood Grouping. • Other - Chest X-ray, CT, plain X-ray abdomen.
Renal injuries Treatment • Conservative - catheterization, blood transfusion, monitor vital signs, urea, creatinine etc. . • Surgical- indications- blood loss, haematoma, hilar injury • 10 - 20 % cases -Gentle suturing, Nephrostomy, Nephrectomy
RENAL TUBERCULOSIS • Secondary to pulmonary TB, Bacilli causes lesions in the renal cortex & it spreads along the ureter causing tubercular ureteritis & stricture ureter. Pathology • Through blood it reaches the glomeruli causing caseating granuloma with Langerhan’s type of giant cells & epitheloid cells. These granuloma united to form, • TB papillary ulcer • Cavernous form • Hydronephrosis • Pyonephrosis • perinephric abscess, calcification, casceous kidney, miliary TB, TB cystitis leads to golf hole ureter & thimble bladder, prostatitis, vesciculitis, stricture etc. .
RENAL TUBERCULOSIS Clinical features • Common in males, right side, frequency, polyuria, sterile pyuria painful micturition with often haematuria , renal pain, suprapubic pain. • Kidney rarely palpable. Enlarged prostate & seminal vescicles. Acute pyelonephritis. Features of urinary stones, UTI, Dyspareunia , menstrual irregularities. Fever& weight loss, cough, expectoration, haemoptysis.
RENAL TUBERCULOSIS Investigations • Hb % & ESR increased • Mantoux test positive. • Chest X- ray • Three consecutive early morning urine is sent for microscopy & culture • USG • Plain X- ray KUB - shows calcification • CT abdomen& pelvis – see hydronephrosis, shrunken kidney, stricture, necrosis • IVU – Hydrocalyx, narrowing of calyx, stricture ureter • RGP- is useful, ureter, pelvis, calyces seen, sampling of urine taken • CYSTOSCOPY- multiple tubercles, bladder spasm, oedema of ureteric orifice forming golf hole ureter • MCU- to see ureteric stricture , reflux
RENAL TUBERCULOSIS Treatment • Anti TB treatment • Hydronephrosis - anderson’s pyeloplasty • TB abscess- drainage • Ureteral stricture – Stenting/ Reimplantation of the ureter in to bladder • Thimble bladder - hydraulic dilatation/ ileocystoplasty/ caecocystoplasty/ sigmoid colocystoplasty • In unilateral lesion with gross impairement of renal function- nephroureterectomy
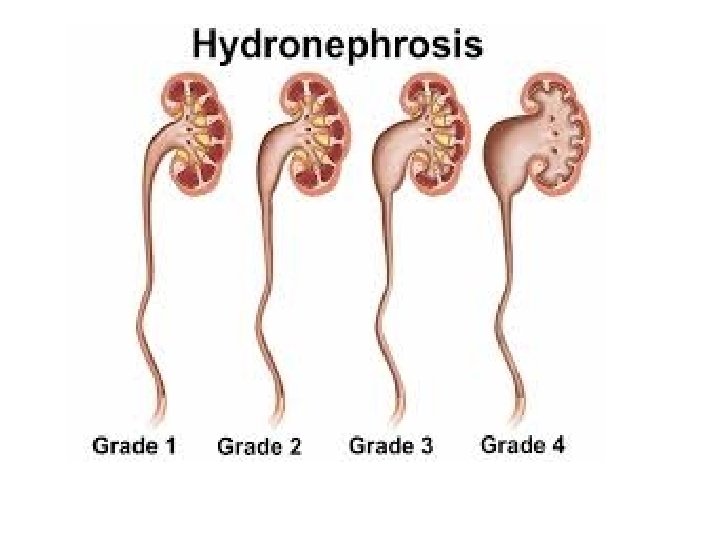
Hydronephrosis • It is an aseptic dilatation of whole or a part of pelvi-calyceal system of kidney due to partial or intermittent obstruction to the out flow of urine. • Hydronephrosis refers to dilatation of renal pelvis and calyces with accompanying atrophy of the parenchyma. • Cause by obstruction to the outflow of urine
Hydronephrosis – obstruction levels • • • Renal pelvis Pelviureteric junction Ureter Bladder Urethra
Hydronephrosis – causes • Aetiology ; it can be unilateral/ bilateral Unilateral Ø Extramural- • Aberrant renal vessels( vein/ artery)compressing the ureter - common on left side • Compression by a growth/ Tumour- Ca cervix, Ca rectum, prostrate, colon etc. . • Retroperitoneal fibrosis • Retrocaval ureter
Hydronephrosis – unilateral causes Intramural • Congenital PUJ obstruction • Ureterocele • Inflammatory stricture • Ca ureter • Narrow ureteric orifice • Stricture ureter (following removal of stones, pelvic surgeries, TB ureter) Intra luminal • Stone in the renal pelvis or ureter • Sloughed papilla in papillary necrosis
Hydronephrosis – Bilateral causes Bilateral • Congenital- stricture of external urethral meatus, pinhole meatus Congenital posterior urethral valve, urethral atresia. • Acquired - BPH Ca prostate Post operative bladder neck scarring Inflammatory / traumatic urethral stricture Phimosis Ca cervix involving both ureters Bladder Ca • Congenital PUJ obstruction is the most common cause of HN • Often it is bilateral & presentation on one side is earlier than the other side. • Aberrant renal artery or vein in the lower pole can compress PUJ causing HN. Renal angiogram confirms the diagnosis.
Pathophysiology • Due to aetiological factors obstruction of the urine flow fluid backs up in to the kidney causing dilatation of renal pelvis causing barotrauma/ pressure trauma higher pressure causes irreversible destruction of the nephrones hypertrophy of the kidney as a consequence of increased work load hydronephrosis renal failure
Pathology • Changes depends on whether the kidney has an extrarenal or intra renal pelvis- commonly extra renal • In extra renal pelvis first the pelvis alone become dilated , at time goes on if the obstruction is not relieved calyces become dilated& renal parenchyma is progressively destroyed by pressure atrophy • In a kidney with intra renal pelvis destruction of parenchyma occurs rapidly
Pathology • Kidney is massively enlarged with greatly distended pelvi calyceal system. • The renal parenchyma is compressed and atrophied with obliteration of the papilla and flattening of the pyramids. • Pressure changes on the pelvis later calyces & renal parenchyma. • Gradually parenchyma thins out due to destruction & it dilates& affects secretory function • Parenchymal thickness of less than 2 mm is unlikely to function. In bilateral cases such patients will go for renal failure. • Depending on obstruction one or both ureter may also dilated( hydroureter)
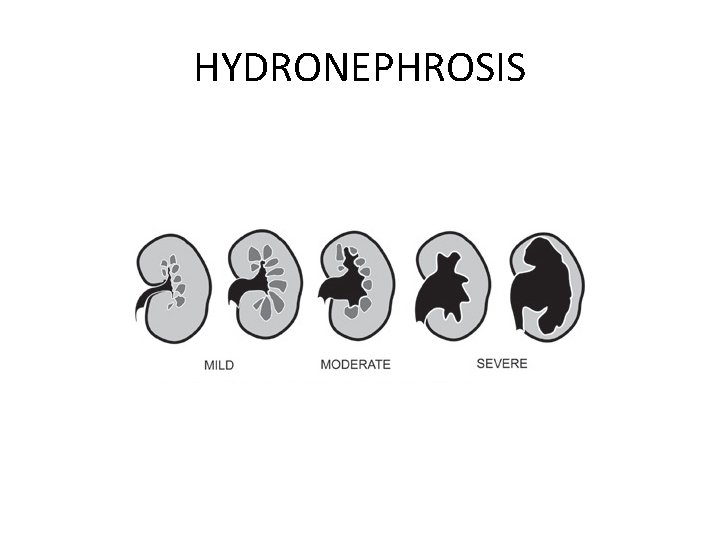
HYDRONEPHROSIS
Symptoms & signs of HN • • • • Male: female- 2: 1 Right side is more common Asymptomatic in some conditions Dull aching loin pain with dragging sensation or heaviness (Pain is felt in the renal area. ) worse by excessive fluid intake Haematuria Anuria/ oliguria Urinary infection, dysuria, frequency Calculi Azotemia – abnormaly high level of nitrogen containing compounds( urea, creatinine etc. . ) in blood Unexplained vague GIT symptoms Some large hydronephrosis can be palpable( mass in the loin which is mobile, ballotable, moves with respiration with dullness in renal angle). Dietl’s crisis- after an acute attack of renal colic , swelling in the loin is seen which disappears after passing large volume of urine. Occassionally hypertension. Distension of bladder if urethra is obstructed.
Clinical course • Bilateral complete obstruction produce anuria which need soon medical attention. • Incomplete bilateral obstruction produce polyuria rather than oliguria as a result of defect in tubular concentrating mechanism
Clinical course • Unilateral hydronephrosis may be silent for long period unless other kidney is affected • Bilateral hydronephrosis usually lead to uremia • Early removal of obstruction can return the kidney function • However with the time the changes become irreversible
INVESTIGATIONS - HN • • RFT- urea, creatinine Urine microscopy USG IVU CT Isotope renography- DTPA scan-pentetic acid Complications- pyonephrosis, perinephric abscess, renal failure in bilateral cases

Treatment -secondary to cause • Stones- pyelolithotomy/ ureterolithotomy • Stricture – stricturoplasty or excision and end to end anastamosis • Aberrant vessel- transection of the ureter and anastomosis in front of the vessel. • BPH- TURP • Ca prostrate- TURP+ Hormonal therapy • Urethral stricture- urethroplasty • Meatal stenosis- meatoplasty • Phimosis – circumcision
Management of congenital hydronephrosis • Patients with congenital PUJ dysfunction presents congenital hydronephrosis • Congenital hydronephrosis can be defined as more than 10 mm antero-posterior diameter of renal pelvis at 20 weeks of gestation. • Management differs according to the grades of hydronephrosis, which is based on renal pelvic diameter.
MANAGEMENT Grading- mild -11 -20 mm Moderate-21 - 35 mm Severe- > 35 mm Mild case is managed conservatively with serial monitoring of pelvic diameter by USG and of renal function. • Moderate is also managed by serial monitoring. Any deterioration of renal function is an indication for surgical intervension • Severe HN should be treated early Anderson – Hynes pyeloplasty to prevent permanent damage to kidney. • •
Anderson Hynes Pyeloplasty • In this operation , the upper third of the ureter and the renal pelvis are mobilised. • Anastomosis is made between ureteric end and kidney. • A nephrostomy tube is passed , which serves to protect the anastomosis
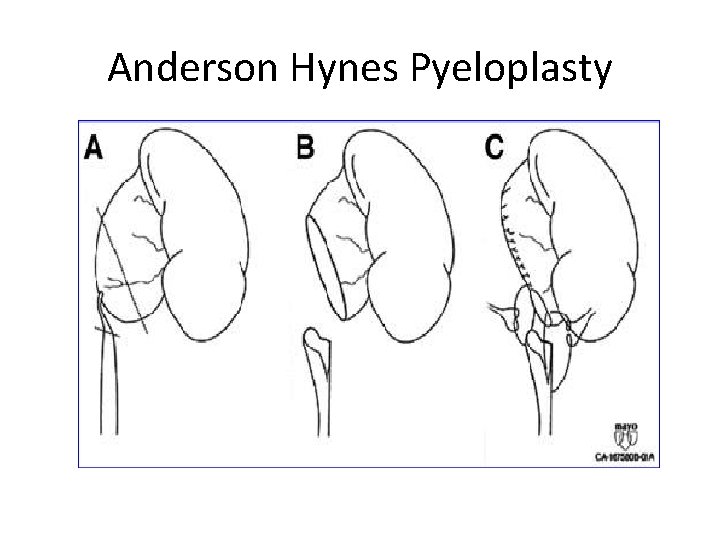
Anderson Hynes Pyeloplasty

Pyonephrosis • Collection of pus in the pelvicalyceal system (a multi loculated cyst). Causes – • Infection of hydronephrosis • Following acute pyelonephritis • Complication of renal calculi( stone in renal pelvis or stag horn calculi) Clinical features- usually unilateral • Triad – anemia, fever, loin swelling • Tender mass in loin, smooth, soft, not mobile , not move with resp. • Cystitis, pyuria, burning micturition. • Fever, chill, rigor

Pyonephrosis Investigations • Plain X-ray KUB – For Renal calculi • IVU- For HN • Cystoscopy – cystitis • USG • DTPA Scan Treatment – medicinal treatment • Drainage- through loin incision & nephrostomy tube • Kidney is totally destructed- sub capsular nephrectomy • In Bilateral- bilateral nephrostomy with J stending to keep ureter patent
RENAL CARBUNCLE • A localised inflammatory necrotic mass of tissue involving renal parenchyma. • Causative organism- staphylococcus aureus & coliforms. • Source- cutaneous infection like boil & carbuncle. • Presents as ill-defined tender swelling in the loin, with pyrexia, leucocytosis. • Staphylococci can be isolated from the urine. • IVU- obliteration of group of calyces like RCC • Treatment- Drainage with malecots catheter • Severe cases- Nephrectomy
PERINEPHRIC ABSCESS Causes • Infection of a perinephric haematoma • Perforation of renal abscess or carbuncle • TB perinephric abscess • Extension of cortical abscess • Haematogenous spread • Extension of appendicular abscess • Periureteral lymphatic spread C/F- high fever, fullness in the loin, tenderness and rigidity, scoliosis with concavity towards the side of abscess.
PERINEPHRIC ABSCESS Investigations- TC elevated • X- ray KUB- obliteration of psoas shadow, scoliosis, elevation of hemi diaphragm. • IVU- 2 films- lying down & erect position. Normally in erect posture downward displacement of kidney is seen. It is not seen in perinephric abscess- Mathe’s sign. • USG • CT Scan is diagnostic Treatment- medicinal • Under G/A drainage through lumbar incision , pus sent for C/S
RENAL CALCULI- Nephrolithiasis Introduction • A kidney stone is a hard solid mass of material that forms in the kidney from the substances in the urine. • Kidney stones or calculi develop as a result of various metabolic disorders which affect the fate of calcium and other mineral elements in the body. • Stones may be formed in the kidney, urinary bladder, ureter and urethra
RENAL CALCULI • 80% of Stones under 2 mm in size. • 90 % of stones pass through the urinary system spontaneously. • Generally stones smaller than 6 mm are passable. Risk factor: • Imbalance of p. H in urine Alkalic: -Calcium stone Acidic: -Uric & cystine stone
Renal calculi – aetiology • Unknown • Diet - vit. A deficiency – desquamation of epi. which act as a nidus for stone formation. • Climate- hot climate will increases urinary solutes with decrease in colloids. • Citrate level- high level causes • Infection in kidney • Prolonged immobilisation • Gout • Hyperparathyroidism • Hyper oxaluria
Renal calculi- aetiology Cystinuria Stasis of urine medullary sponge kidney Randell’s plaque theory – erosion & deposition of urinary salts as randall’s plaques at the apex of renal papillae. • Carr’s postulates- minute concretions called as microliths normally developed in subendothelial part of tubulewhich will be carried by renal lymphatics. If these lymphatics are blocked , microlith are enlarge & act as a nidus for stone formation. • Others- sarcoidosis, gout, hypervitaminosis D, hypomagnesuria Ca treatment • Renal tubular acidosis - causes calcium phosphate stones • •
Pathophysiology - Stages of stone formation • Urine saturation Supersaturation Nucleus formation Crystallisation Aggregation Matrix formation Stone (Retention and growth)
Renal calculi- types • Types: 1. Calcium oxalate stones (Is the most common 80% ) 2. Calcium phosphate stones 3. Struvite stone (Triple stone) 4. Uric acid stones 5. Urate stones 6. Cystine stone 7. Xanthine calculi 8. Indigo stones
Renal calculi- Types 1. Oxalate stone (Is the most common 80% ) • mulberry stones as brown in colour with sharp projections. • It is calcium oxalate stone, • shows an envelop crystals in urine. • Caused by super -saturation of urine with calcium & oxalate • Calcium oxalate stone tend to form in alkaline chemistry • Avoid food high in oxalate(beer, wheat germ, spinach, tea, cola, alcohol, citrus fruits)
Renal calculi- types 2. Phosphate stone (10 -15%): - • Caused by super -saturation of urine with calcium phosphate. • It is either calcium phosphate or calcium, magnesium, ammonium phosphate stone usually occurring in an infected urine. • It is smooth& white in color • Calcium phosphate stone tend to form in alkaline chemistry. • In an alkaline urine , it enlarges rapidly , filling renal calyces taking their shape called stag horn calculus. • it is radio-opaque & attains a large size. • Avoid food high in calcium (Milk & dairy product)

Renal calculi- types 3. Struvite stone (Triple phosphate stone): It is a compound of Magnesium , ammonium phosphate mixed with carbonate • It occurs in presence of ammonia & urea splitting organism in urine (Proteus, Pseudomonas, Klebsiella, Staphylococcus) • more common in women than the man because of UTI • Struvite stone tend to form in alkaline chemistry
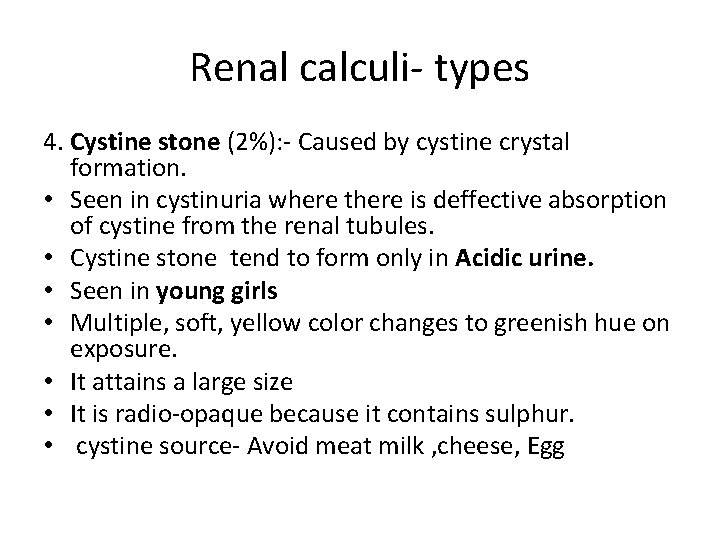
Renal calculi- types 4. Cystine stone (2%): - Caused by cystine crystal formation. • Seen in cystinuria where there is deffective absorption of cystine from the renal tubules. • Cystine stone tend to form only in Acidic urine. • Seen in young girls • Multiple, soft, yellow color changes to greenish hue on exposure. • It attains a large size • It is radio-opaque because it contains sulphur. • cystine source- Avoid meat milk , cheese, Egg
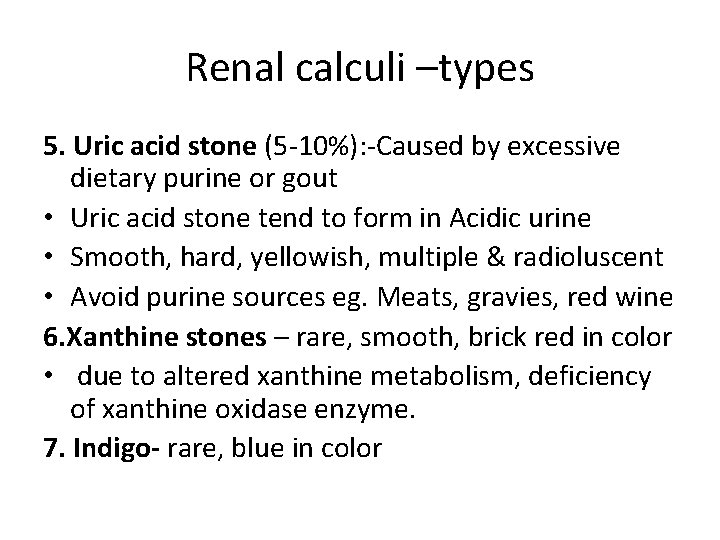
Renal calculi –types 5. Uric acid stone (5 -10%): -Caused by excessive dietary purine or gout • Uric acid stone tend to form in Acidic urine • Smooth, hard, yellowish, multiple & radioluscent • Avoid purine sources eg. Meats, gravies, red wine 6. Xanthine stones – rare, smooth, brick red in color • due to altered xanthine metabolism, deficiency of xanthine oxidase enzyme. 7. Indigo- rare, blue in color
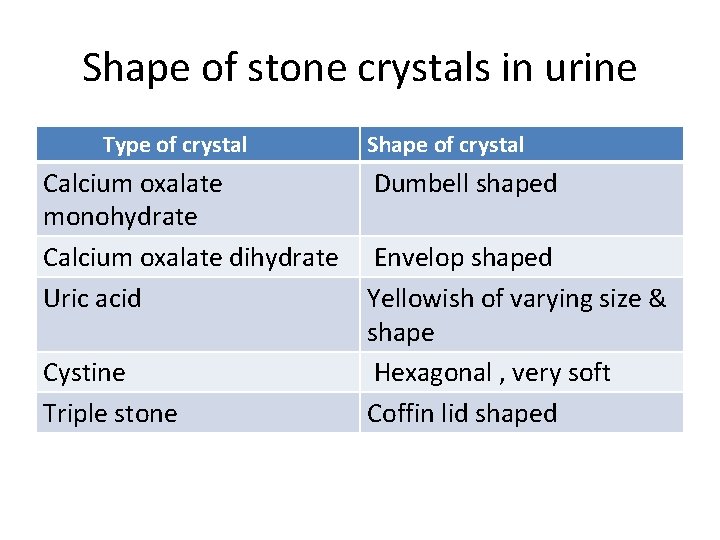
Shape of stone crystals in urine Type of crystal Shape of crystal Calcium oxalate Dumbell shaped monohydrate Calcium oxalate dihydrate Envelop shaped Uric acid Yellowish of varying size & shape Cystine Hexagonal , very soft Triple stone Coffin lid shaped
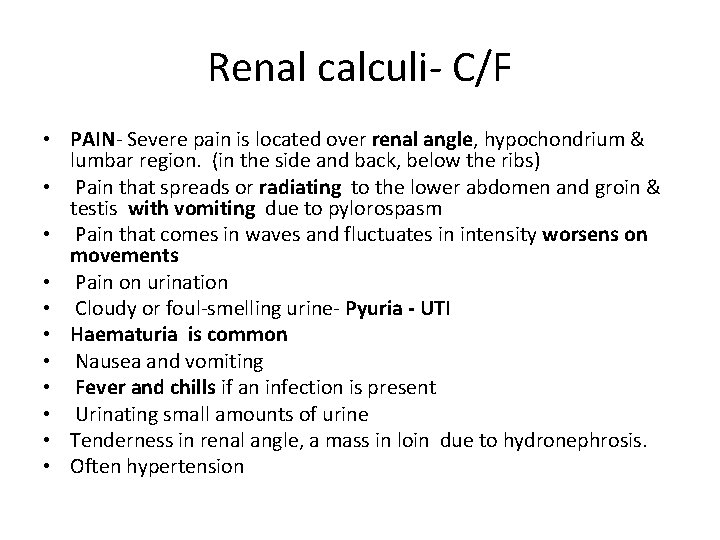
Renal calculi- C/F • PAIN- Severe pain is located over renal angle, hypochondrium & lumbar region. (in the side and back, below the ribs) • Pain that spreads or radiating to the lower abdomen and groin & testis with vomiting due to pylorospasm • Pain that comes in waves and fluctuates in intensity worsens on movements • Pain on urination • Cloudy or foul-smelling urine- Pyuria - UTI • Haematuria is common • Nausea and vomiting • Fever and chills if an infection is present • Urinating small amounts of urine • Tenderness in renal angle, a mass in loin due to hydronephrosis. • Often hypertension

DIAGNOSIS • Blood- ESR, calcium, phosphate, creatinine, urea, uric acid, • Urine analysis- calcium, urate, cystine, p. H, specific gravity, C/S • Plain X-ray KUB- Kidney shadow, stones (90% - radio- opaque) • Intravenous urogram (IVU) or intravenous Pyelogram- renal function, HN • USG- radioluscent stones, changes in renal parenchyma • Cystoscopy • CT scan – Small missed stones in ureter • MRI •
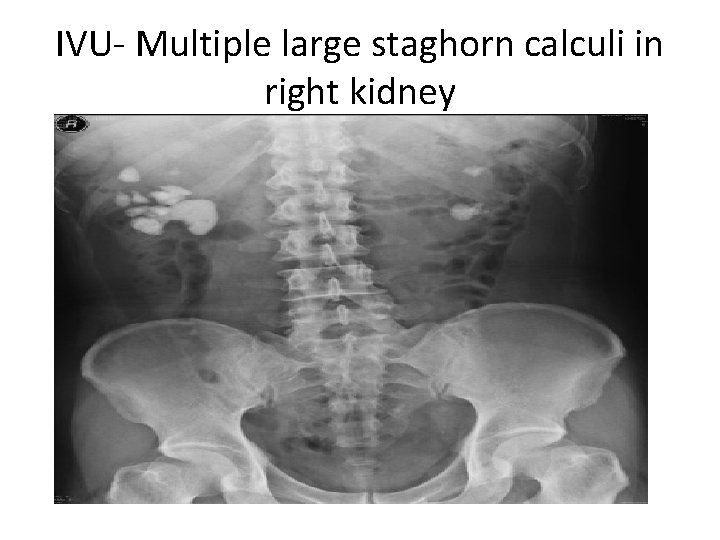
IVU- Multiple large staghorn calculi in right kidney
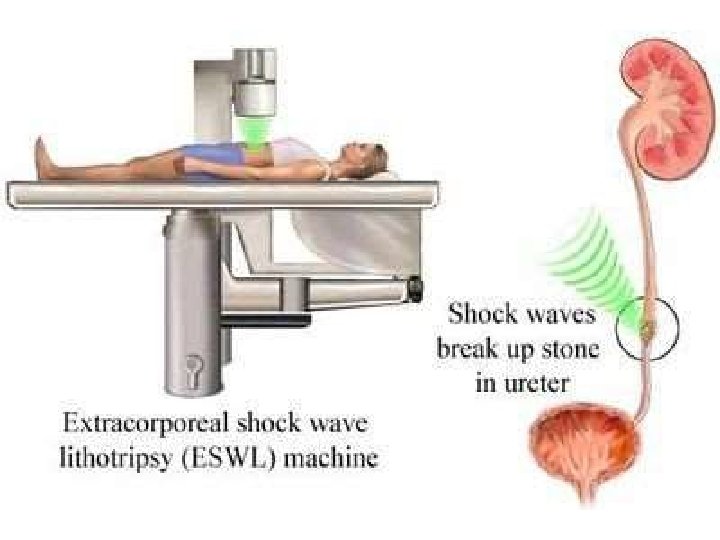
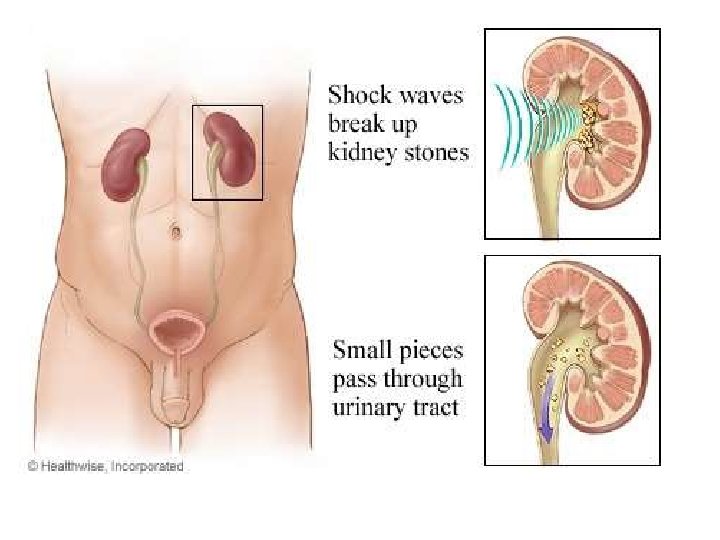
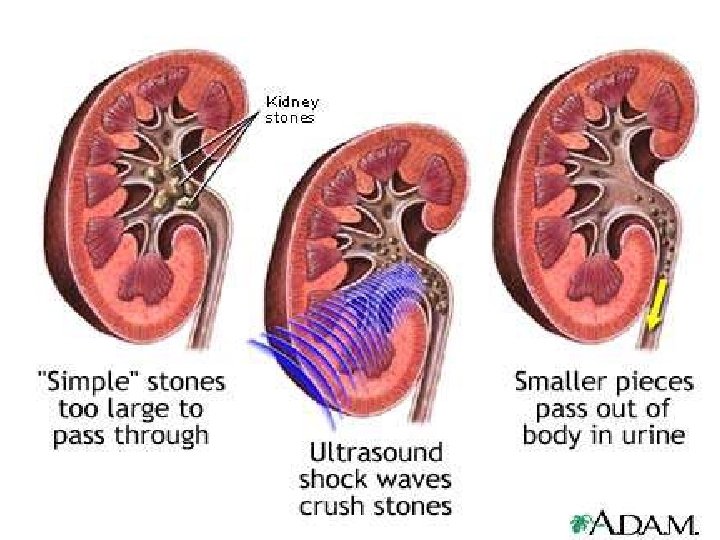
SURGICAL MANAGEMENT Close procedure: - Noninvasive Lithotripsy (Extracorporeal Shockwave lithotripsy ESWL) • Piezo- ceramic / electromagnetic waves are passed through water bath / water cushion which acts as a media • Stone is located & observed through flouroscope / ultrasound • Shock waves are triggered as a compressive waves over stone to fragment it. These fragments are flushed out.
ESWL - Advantages- • no anesthesia • done as an OP procedure, • less than 2. 5 cm stones are well fragmented. • Hard stones, oxalate stones are better eliminated by ESWL • It can be done repeatedly in different sittings • If It is not successful over to PCNL Contraindications • Pregnancy • Bleeding disorders • Pts. with abdominal aneurysms • Sepsis & renal failure (Serum creatinine more than 3 mg%) Complications – • Renal haematoma • Severe haematuria • Injury to adjacent structures • Fragmented stone retains in ureter

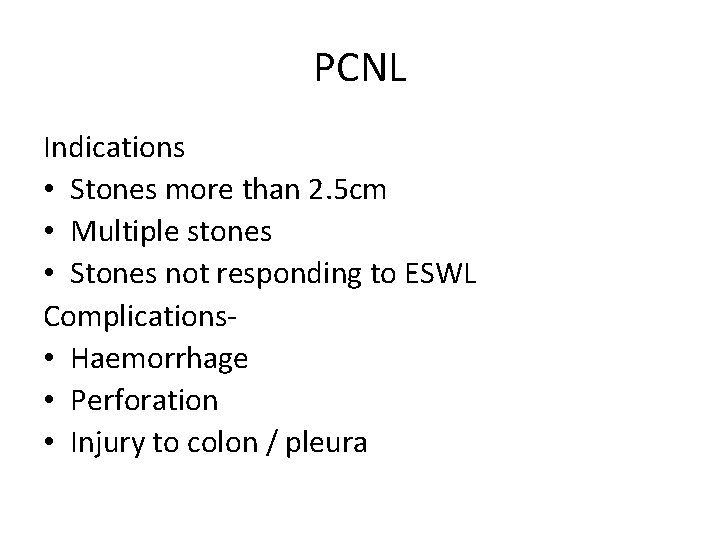
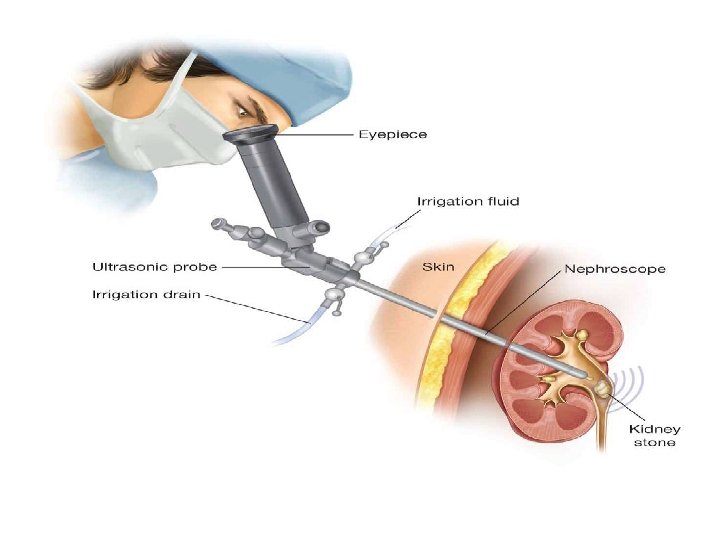
PCNL Indications • Stones more than 2. 5 cm • Multiple stones • Stones not responding to ESWL Complications- • Haemorrhage • Perforation • Injury to colon / pleura
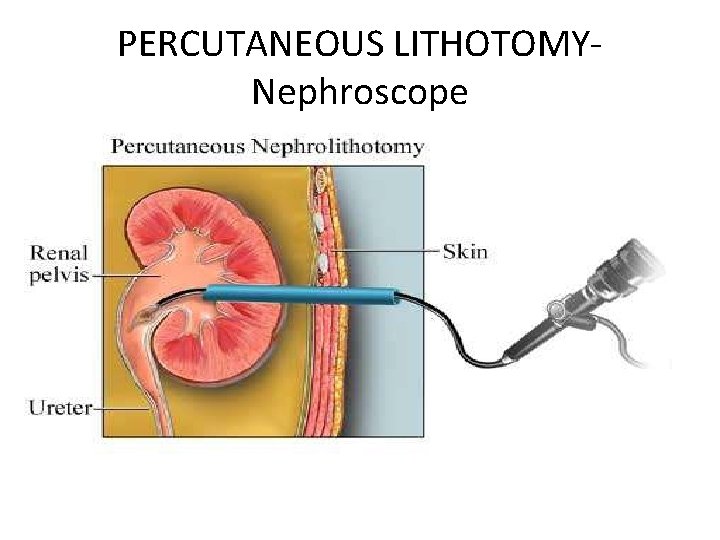
PERCUTANEOUS LITHOTOMYNephroscope
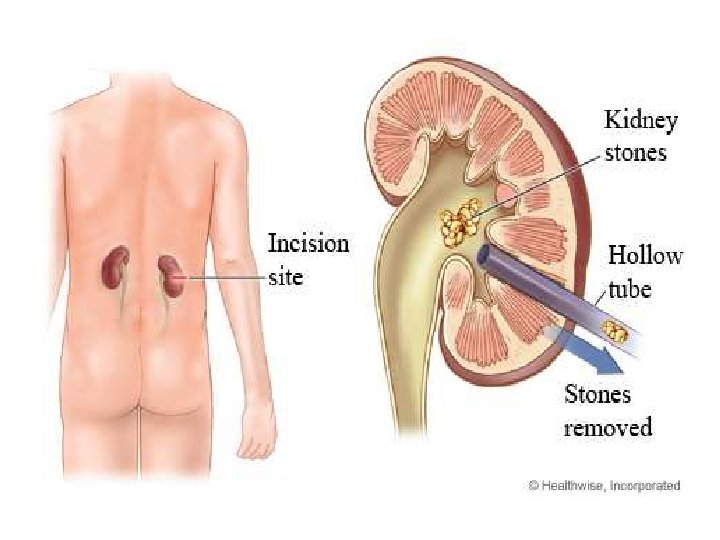

Renal calculi- surgery Open procedure: • Ureterolithotomy • Pyelolithotomy • Nephrolithotomy • Partial or total nephrectomy
MONITORING • • • Note increased redness in urine Monitor vital signs Fluid balance chart Observation for anuria Observation for signs of infection.
URETERIC CALCULI • Always renal origin • Nature of stone is same as that of renal stones • Elongated shape • Can get impacted in various narrow junction Sites – • PUJ • Where ureter crosses the iliac vessels • Ureter crosses vas deferens/broad ligament • Where ureter penetrates outer layer of bladder muscle. • In the intramural portion of ureter near the ureteric orifice. • Stones less than 5 -8 mm size may pass spontaneously.
Ureteric stone C/F- • Pain- Colicky type & radiates from loin to groin often to the tip of the genitalia, testes in males, labia majora in females ( along the genitofemoral nerve) Severe in intensity increases with exercise. • Nausea , vomiting , sweating, due to pain & reflex spasm. • Haematuria , dysuria, frequency, strangury • Tenderness in iliac fossa &renal angle
Ureteric calculi Complications – • Obstruction • Hydronephrosis • Infection • Impaction • Ureteral stricture D/D • Appendicitis • Cholecystitis • Ovarian cyst • Mesentric adinitis • Ruptured ectopic gestation
Ureteric calculi – Investigations • Urine- microscopy, C/S • Blood urea, creatinine, serum calcium, uric acid • Plain X-ray KUB- radio-opaque stones are visible in 90% cases in the line of ureter. ( late& oblique view) • IVU- hydronephrosis & hydroureter • Isotope renogram- functions of kidney • USG • CT scan is diagnostic
Ureteric calculi Treatment • Plenty of water orally • Diuretics • IV fluids Surgical Tt. Indications • Stone more than 5 -8 mm size • IVU shows deterioration of function • Presence of infection • If stone is impacted in the ureter with persistent symptoms
Ureteric calculi- surgery Upper third stone • ESWL • Stone is pushed in to the renal pelvis & then PCNL done • URS- Ureterorenoscopic stone removal- through ureteroscope , stone is visualised & fragmented using pneumatic bombarder. Then extracted by utereroscope. complications are perforation of ureter, bleeding, extraperitoneal leakage of urine • Open ureterolithotomy
Ureteric calculi - surgery Stone in middle third • URS • Open ureterolithotomy Stone in the lower third • URS • Dormia basketing- basket is passed in to the proximal ureter beyond the stone & opened. Stone is then pulled out Indications stone in lower third Stone below pelvic rim Stone less than 10 mm size Single stone
Ureteric calculi • Dormia basketing. Complications Stone dislodgement urethral injury Avulsion of ureter Stricture ureter • Open ureterolithotomy • Ureteric meatotomy using cystoscope for stone impacted at the ureteric orifice. • All ureteric stones can be removed through laparoscopy or retroperitoneoscopy
Recurrence of stones Types- False recurrence- during intervention tiny fragments may be left behind • True recurrence- recurred again once all stones are cleared Causes- hyperparathyroidism, hypercalciuria, hyperuricaemia, gout, cystinuria. Prevention- hydration is the main- 3 -4 L/day • Diet- avoid diet rich in calcium oxalate, sodium, vit. C, low calcium diet • Increased intake of dietary fibre.
Tumours of kidney • Benign -Rare Wilm’s tumour(nephroblastoma) ; • Arises from embryonic connective tissue containing epithelial & connective tissue elements. • Located in one pole of the kidney • Common in first 4 yr of life • Bilateral in 5% of cases Pathology- it is smooth, soft, fleshy pinkish white in color with haemorrhagic areas. microscopically premitive glomeruli & premitive tubules with epithelial & connective tissue cells exists side by side
REFERENCE • • • Bailey and Love’s short practice of Surgery Manipal manual of Surgery SRB’s Manual of surgery Text book of Surgery- ASI Clinical Surgery, Das
THANK YOU, DR. PANCHAJANI. R, Associate professor, Dept. of Surgery, SKHMC
- Slides: 89