Urine formation and excretion Urine Formation3 steps What

- Slides: 12
Urine formation and excretion
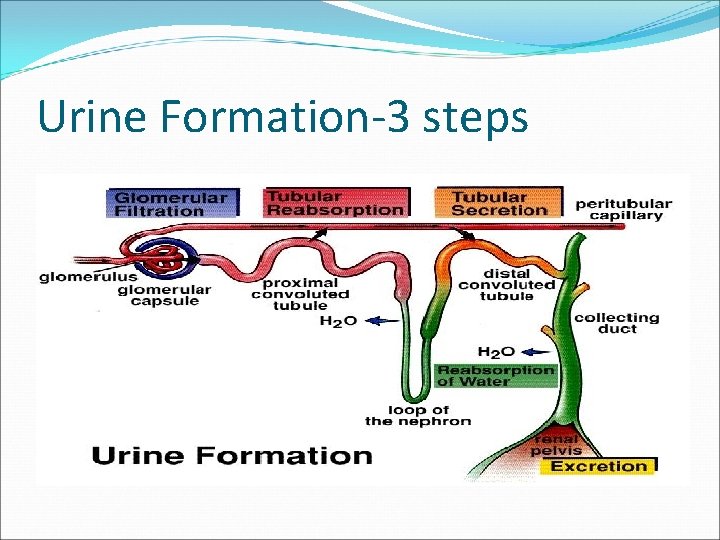
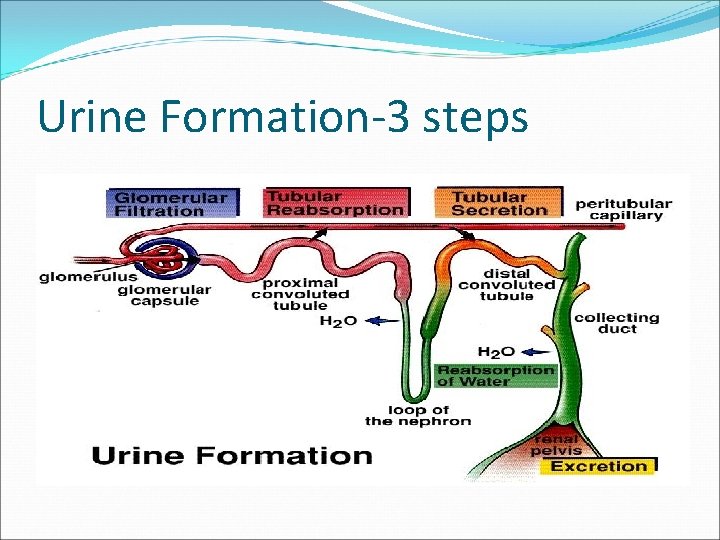
Urine Formation-3 steps
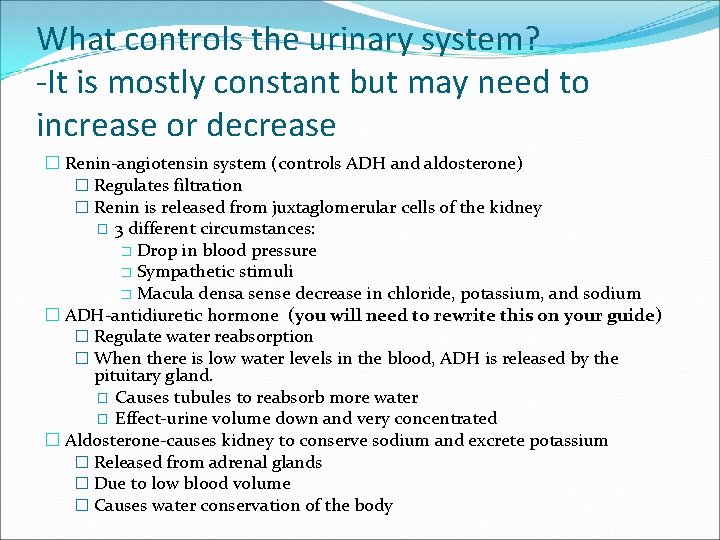
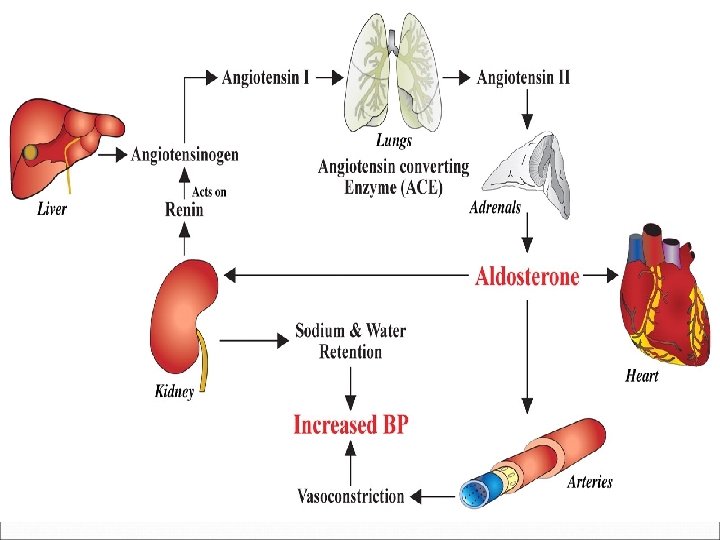
What controls the urinary system? -It is mostly constant but may need to increase or decrease � Renin-angiotensin system (controls ADH and aldosterone) � Regulates filtration � Renin is released from juxtaglomerular cells of the kidney � 3 different circumstances: � Drop in blood pressure � Sympathetic stimuli � Macula densa sense decrease in chloride, potassium, and sodium � ADH-antidiuretic hormone (you will need to rewrite this on your guide) � Regulate water reabsorption � When there is low water levels in the blood, ADH is released by the pituitary gland. � Causes tubules to reabsorb more water � Effect-urine volume down and very concentrated � Aldosterone-causes kidney to conserve sodium and excrete potassium � Released from adrenal glands � Due to low blood volume � Causes water conservation of the body
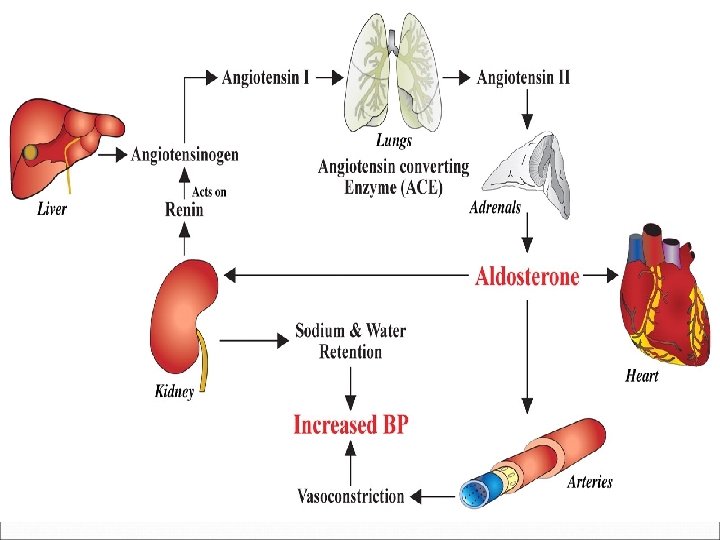
Renin-angiotensin system �Renin is released �It reacts with angiotensinogen �Renin will form angiotensin I �Angiotensin I combines with an enzyme (released by lungs and in plasma) to form angiotensin II. �Angiotensin II �Maintains water, sodium, and blood pressure � Causes vasoconstriction (less filtering) � Causes vasodialation (more filtering)
r
Glomerulus Filtration �Capillaries drop off particles in the blood the body needs to get rid of �Driven by blood pressure (filtration pressure) �Produces 180 L of fluid every 24 hours �Particles filter into the glomerulus capsule (mostly water) �Composition is very close to tissue fluid
Tubular Reabsorption �Occurs mostly in the proximal tubule �Transports items out of the tubular fluid (urine) back into the blood (peritubular capillary) �What the body still needs (what is reabsorbed) � Glucose, acid amino acids, water, urea (about 50% of it), and uric � 65% of filtrate is reabsorbed here �Reabsorption of sodium and potassium
Tubular secretion �Late filtering process �Transports items out of the blood (peritubular capillaries) into the renal tubules �Processing of potassium, water, and some uric acid and urea
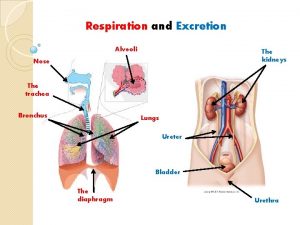
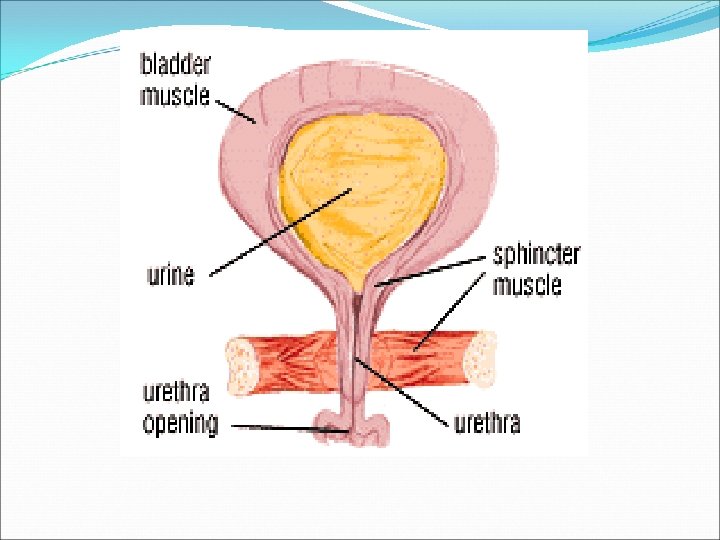
Elimination of Urine �Urine passes through the collecting ducts to the renal papillae �Then to the minor and major calyces �Out the renal pelvis to the ureters �To the bladder �To the urethra and out of the body
Urine Summary �Urine composition �Reflects the quantities of water and solutes that the kidney must eliminate for the body to maintain homeostasis �Diet �Activity levels �Urine � 95% water �Also has urea, uric acid, trace amounts of amino acids, and electrolytes

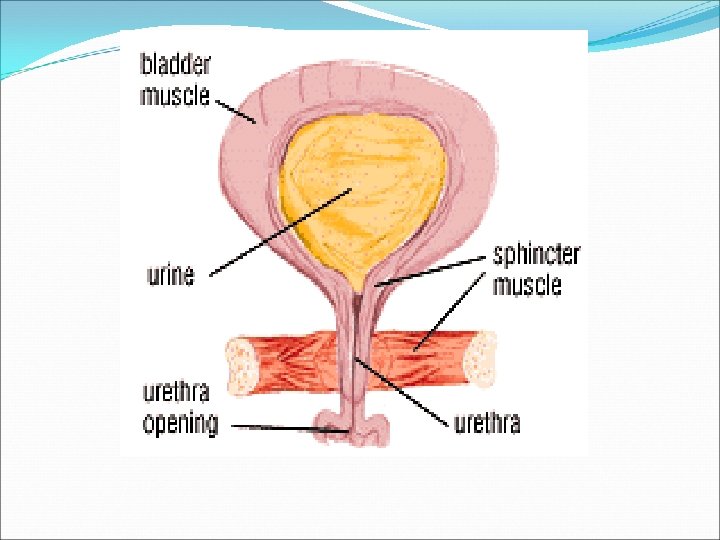
Micturition (not on noteguide) �Urinating (write this one) �Contracts detrusor muscle and relaxes the external urethral sphincter �Distension stimulates stretch receptors in the bladder �Impulses are sent to the detrusor muscle from the CNS �As bladder fills, internal pressure increases, and forces sphincter to open �A second reflex relaxes the sphincter unless voluntary control maintains its contraction
 Urine formation introduction
Urine formation introduction Dari hasil tes ternyata urin pak yudha mengandung glukosa
Dari hasil tes ternyata urin pak yudha mengandung glukosa Urinary system introduction
Urinary system introduction Urine formation
Urine formation Urethra
Urethra Urine formation video
Urine formation video Chapter 37 respiration circulation and excretion
Chapter 37 respiration circulation and excretion What is the function of glomerulus class 10
What is the function of glomerulus class 10 Alveoli
Alveoli Egestion vs excretion
Egestion vs excretion Digestion and excretion lesson 3
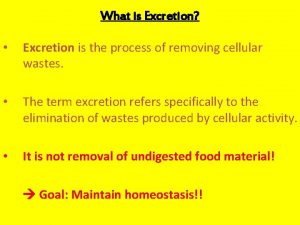
Digestion and excretion lesson 3 What is excretion
What is excretion Ion trapping
Ion trapping