URINE EXAMINATION DR JOHN OCHEI URINE EXAMINATION Why

- Slides: 36
URINE EXAMINATION DR. JOHN OCHEI
URINE EXAMINATION Why examine urine? To diagnose urinary tract infection and kidney dysfunction! Urine specimen – MSU, CCU, CSU, TSU and Supra pubic aspirate ( SPA ).
Urine Examination: 1. Physical 2. Chemical 3. Microscopic 4. Culture
Physical Examination 1. Volume Proportional to water in take by a person. Useful terms: - Polyuria – consistent abnormal excretion of large volume of urine (Diabetes) - Oliguria – Opposite of polyuria (Diarrhoea) - Anuria – Complete absence of urine formation

- Nocturia – Passing of >500 ml of urine by adult at night - Diuresis – any increase in urine volume! 2. Specific gravity A measure of amount of dissolved substances in urine, a diagnostic tool. 3. Colour – Clear, Pale yellow depending on concentration.
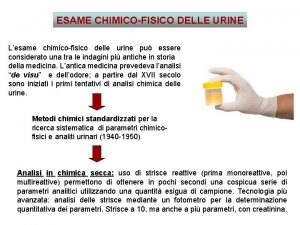
• Chemical Examination of Urine analysis Used to detect glucose, protein, p. H, blood, ketone, esterase, bilirubin etc. Various methods for the detection of abnormal chemical substances are available. Most of the methods are qualitative. Traditional chemical tests:
Dry reagent strips: Plastic strips impregnated with appropriate reagents. Strip is dipped in urine, a chemical reaction denoted by change of colour takes place. Automated method is available to read the tests.
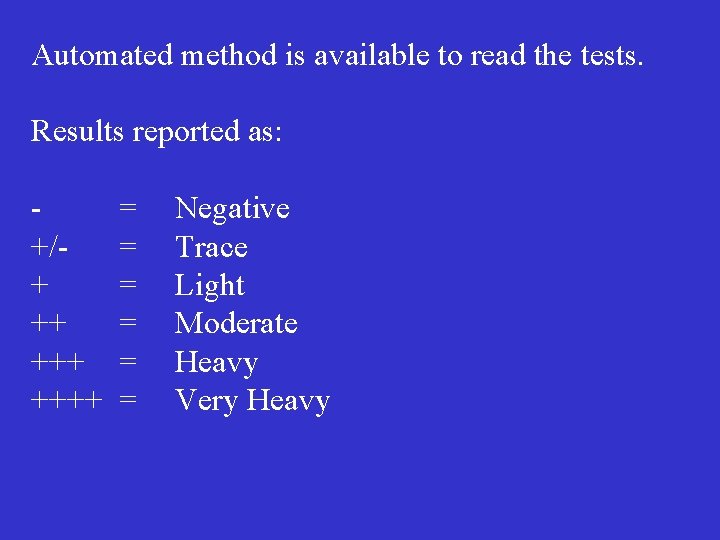
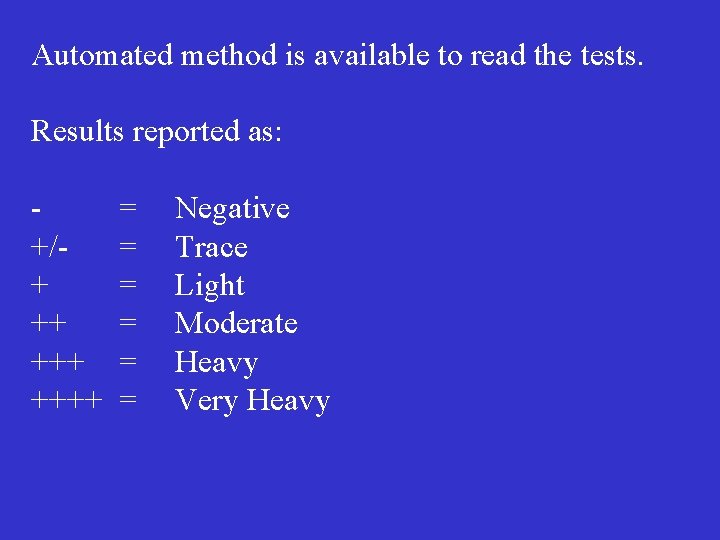
Automated method is available to read the tests. Results reported as: +/+ ++ ++++ = = = Negative Trace Light Moderate Heavy Very Heavy
Examination of Urine Microscopy: 1. Wet preparation: a. Neat Urine b. Centrifuged urine Examination: At least in 4 hpf, count the number of pus cells, rbc and casts in each field and take the average. Report as e. g. 2 -4/hpf. Other findings are scored qualitatively i. e. +, +++ etc.
Interpretation: Neat Urine: 1 -2 pus cells per hpf is significant. Urine to be cultured. Centrifuged urine: Normal Urine may contain <5 pus cells/hpf. Urine may not be cultured; but if >5/hpf, then culture.
Limitations: Neat urine: Not fully representative as casts and ova may not be seen. Centrifuged urine. Representative but more time consuming. 2. WHO method: A known volume of 60 ul of well mixed urine is placed in pre-labeled 96 flat well micro-titre tray. Allow to settle for at least 5 minutes. Examine with x 20 objective of an inverted microscope.
Reporting: WBC count recorded as: <10/ml 10 -100/ml 100 -500/ml >500/ml Other findings may be recorded as: -/+ = Scanty + = Few ++ = Moderate +++ = Many
Limitations: In experienced hand, the method is ideal though costly. There is no need for centrifugation. Many samples are examined in one preparation. 3. Gram Stain: Some workers do Gram stain on samples containing pus cells and bacteria. This is an additional test and may not necessarily be advantageous. Contamination is indicated by mixed flora of bacteria.
4. Darkground Microscopy: This is performed when leptospirosis is suspected. A wet prep. of centrifuged urine is made for DG examination. 5. Ziehl-Neelsen Stain: This is done if renal tuberculosis is suspected. Make smear of the sediment from three centrifuged early morning urine specimens.
Clinical significance of abnormal microscopic findings: 1. Pus cells: Indicates inflammation of UT, referred to as pyuria. i. Infection-cystitis, urethritis etc. ii. Acute or chronic bacterial pyelonephritis iii. Calculi
2. Red blood cells: Indicates haematuria, indicative of: i. Renal diseases – glomerulonephritis ii. S. haematobium infection iii. Physiological changes. 3. Yeast cells: can be differentiated from red cells by their oval shape and some of the yeasts usually show single budding. Indicates faecal contamination, vaginal candidasis or diabetes due to high content of glycogen.
4. Epithelial cells: Nucleated and vary in size and shape Usually few in normal urine but large numbers, however, usually indicate inflammation of the UT or vaginal contamination of the specimen. 5. Casts Consist of solidified protein and are cylindrical in shape, because they are formed in the kidney tubules. There are several types of casts:
Hylanine casts Colourless and empty Associated with damage of the glomerular filter membrane Waxy casts: Hyaline casts that have remained in the kidney tubules for a long time, they are thicker and denser than hyaline casts, often indented or twisted. Indicate tubular damage or renal failure.
Cellular casts: Contain white blood cells or red blood cells: - Rbcs casts indicate haemorrhage into the renal tubules or glomerular bleeding - Wbc casts found in inflammation of the kidney pelvis or tubules. Granular Casts: Contain irregular size granules originating from degenerate cells and protein. Associated with renal damage.
6. Crystals Normal urine contains many chemicals from which crystals can form, and therefore the finding of most crystals are of little clinical importance. Crystals which may be found in metabolic disorders include: Cystine Crystals Six sides, soluble Found in cystinuria
Tyrosine crystals -Yellow or dark coloured, like needles massed together, - Insoluble in ethanol - Occasionally found in severe liver diseases Cholesterol crystals - Rectangular with cut-out corners - Insoluble in acid and alkalines - Rarely found except in severe kidney disease
Other crystals found in Urine: - Sulphonamide – Patient treated with sulphonamides, can cause haematuria and other complications. - Triple phosphate crystals found in alkaline urine. No clinical significance. - Calcium oxalate and uric acid may indicate calculi in the urinary tract.
7. Parasite These include - Eggs of Schistosoma haematobium. The urine contains Rbc’s and protein - Trichomonas vaginalis 8. Bacteria: - Indicates a urinary infection in the presence of pus cells - Usually rods, but sometimes cocci
9. Spermatozoa - Large number may be pathological. In the absence of urine microscopy, urinanalysis (reagent strips) can give enough indication for bacteriological culture of urine. e. g. Esterase # = increase in WBC count in urine. Blood # = increase in RBC Protein # = Bacterial infection
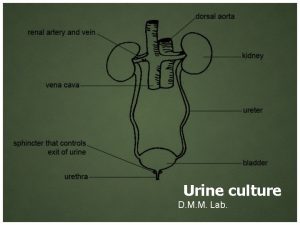
Urine Culture A definite proof of infection in the urinary tract. Pyuria is suggestive but not necessarily so. Some laboratories do not culture urine that are biochemicaly and microscopically normal. Some laboratories culture all samples so as not to misdiagnose asymptomatic bacteriuria.
Significant bacteruria: - The magic number is 105 CFU/ml which indicates infection. - Several methods are available to determine significant bacteriuria. - These are semi-quantitative culture methods.
Pour plate method: A known quantity of urine is diluted in cooled molten nutrient agar, poured into petri dish, allowed to set and incubated. The colonies in and on the medium are counted. Surface drop method (Miles Misra). Time consuming and laborious. Not meant for routine work.
Standard Loop Method: The most popular and convenient method: - Holding a sterile calibrated loop vertically, dip the loop into a well mixed uncentrifuged urine and inoculate the medium of choice. e. g. CLED. |- Incubate plate overnight and count colonies. - A single colony is accepted to represent one colony forming unit (CFU).
Calculation of significant bacteruria: Using 0. 001 ml loop: If 1 loopful (0. 001) produces 100 cfu. Therefore, the number of bacteria/ml = 100 ÷ 0. 001 = 100 x 1000 = 100, 000 (105) Filter paper method: Now superseded by The Standard loop method.
Dipslide method - Unit of universal container into which slide containing media on both sides, is enclosed. - Minimises contamination otherwise no special advantage over the standard loop method. Additional cultures 1. If typhoid fever is indicated: - Centrifuge 10 ml urine in a sterile tube at high speed for 10 minutes.
Re-suspend sediment and transfer to a container of selenite F broth. Incubate overnight and subculture to XLD or DCA. 2. If TB is indicated: Early morning urine for 3 consecutive days. Pool the samples and centrifuge. Decontaminate and inoculate 200 ul on an LJ medium. 3. Direct antibiotic sensitivity may be done in the presence of numerous pus cells and bacteria.
Interpretation of bacterial count (urine quantitative culture) In our SQUH diagnostic laboratory. Standard 1/300 ml loop is used. Culture yielded 333 cfu i. e. 1/300 ml of urine produced 333 cfu. 300 x 333 = 105 CFU/ml Since 100, 000 CFU/ml is significant bacteriuria, any count of 333 and above is significant
Less than 33 cfu = <104 organisms/ml 333 cfu = 105 More than 333 cfu = >105 Reporting: Using 1/300 ml Standard loop. 1. If less than 33 cfu of any organisms and if the patient is not on antibiotic, report as: No significant growth.
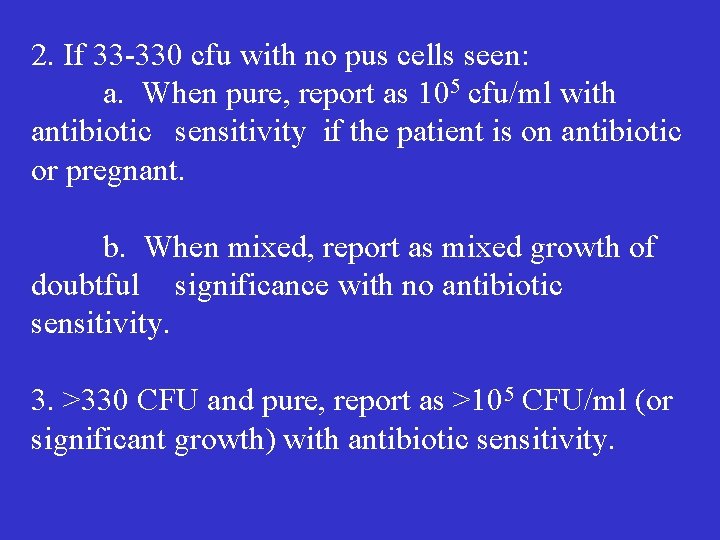
2. If 33 -330 cfu with no pus cells seen: a. When pure, report as 105 cfu/ml with antibiotic sensitivity if the patient is on antibiotic or pregnant. b. When mixed, report as mixed growth of doubtful significance with no antibiotic sensitivity. 3. >330 CFU and pure, report as >105 CFU/ml (or significant growth) with antibiotic sensitivity.
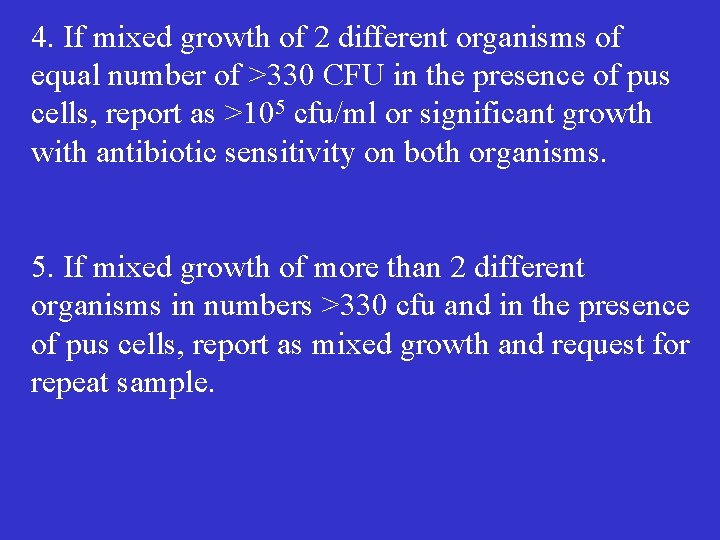
4. If mixed growth of 2 different organisms of equal number of >330 CFU in the presence of pus cells, report as >105 cfu/ml or significant growth with antibiotic sensitivity on both organisms. 5. If mixed growth of more than 2 different organisms in numbers >330 cfu and in the presence of pus cells, report as mixed growth and request for repeat sample.
6. In SPA specimens, any isolate is treated as significant and reported with sensitivity. Merci
 Dr ochei
Dr ochei Wanda ochei
Wanda ochei Why why why why
Why why why why Dari hasil tes urine ternyata pak amir mengandung glukosa
Dari hasil tes urine ternyata pak amir mengandung glukosa Leukocytes in urine
Leukocytes in urine Routine examination of urine
Routine examination of urine General urine examination
General urine examination Centrifuged
Centrifuged Amorphous in urine
Amorphous in urine Dont ask why why why
Dont ask why why why Why was john calvin important to the reformation
Why was john calvin important to the reformation What is john cabot remembered for
What is john cabot remembered for Matt 3:15
Matt 3:15 Tolerates no challenge to his authority
Tolerates no challenge to his authority Kotter leading change why transformation efforts fail
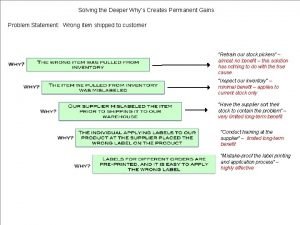
Kotter leading change why transformation efforts fail Why-why analysis
Why-why analysis Why willy why do you cry
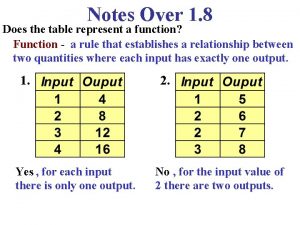
Why willy why do you cry Does this table represent a function why or why not
Does this table represent a function why or why not What does a table represent
What does a table represent Why or why not
Why or why not Why why analysis
Why why analysis Urine chain of custody form
Urine chain of custody form Principle of benedict test
Principle of benedict test Hyaline casts in urine
Hyaline casts in urine Urine sperm
Urine sperm Normal specific gravity of urine
Normal specific gravity of urine Epithelial cells in urine images
Epithelial cells in urine images Characteristics of normal urine
Characteristics of normal urine çno
çno Urine chemical formula
Urine chemical formula Proses pembentukan urine
Proses pembentukan urine Urine scure cause
Urine scure cause Ketones in urine moderate
Ketones in urine moderate Pipet tetes
Pipet tetes Nefron unit terkecil pembentuk urine terdapat pada bagian
Nefron unit terkecil pembentuk urine terdapat pada bagian Vin rose urine
Vin rose urine Pathological components of urine
Pathological components of urine