Urinary Tract Infections UTIs in The Elderly To


- Slides: 20
Urinary Tract Infections (UTIs) in The Elderly “To Dip or Not To Dip? ” Improving the quality of UTI care by working together across Hertfordshire
UTI Background • The reason for 1– 3% of all GP consultations • About one in three women will have at least one UTI by 24 years of age • About 1 in 2 women will be treated for a symptomatic UTI during their lifetime • The annual incidence of UTI in women increases with age • Escherichia coli account for about 80% of UTIs
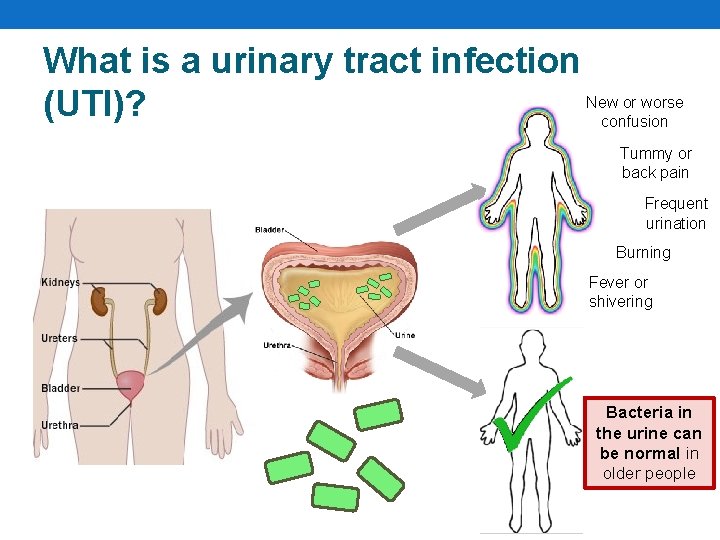
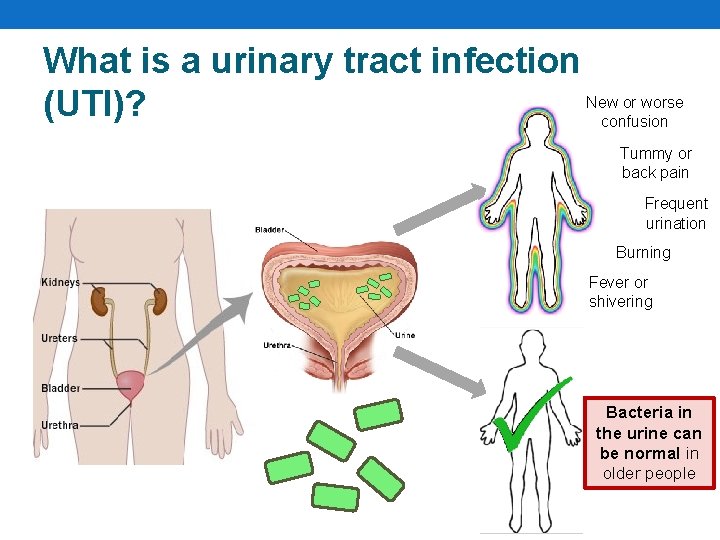
What is a urinary tract infection New or worse (UTI)? confusion Tummy or back pain Frequent urination Burning Fever or shivering Bacteria in the urine can be normal in older people
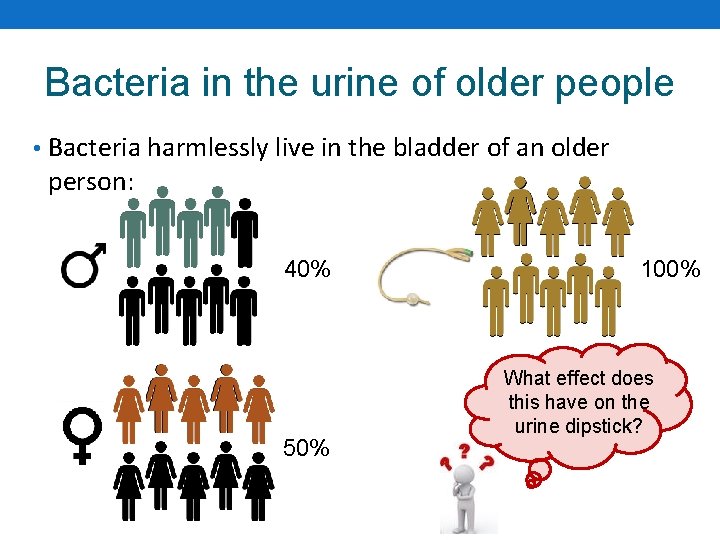
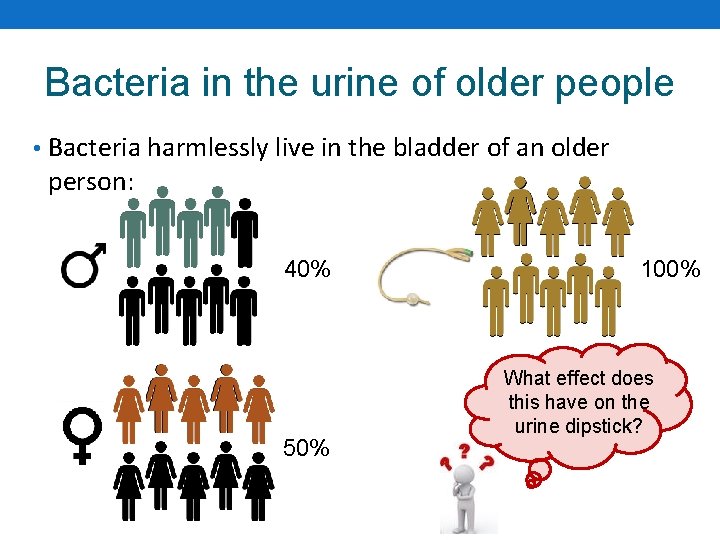
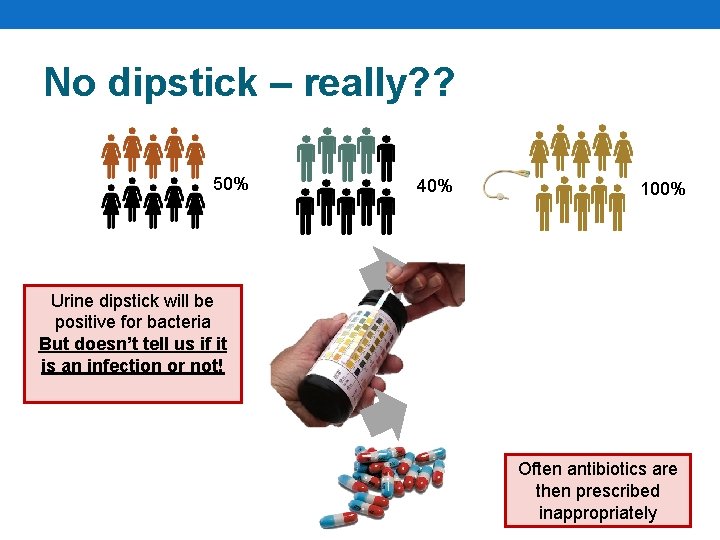
Bacteria in the urine of older people • Bacteria harmlessly live in the bladder of an older person: 40% 50% 100% What effect does this have on the urine dipstick?
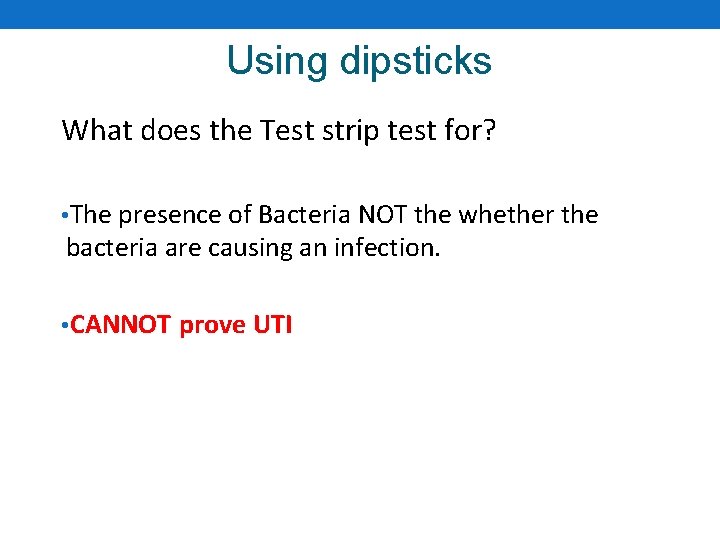
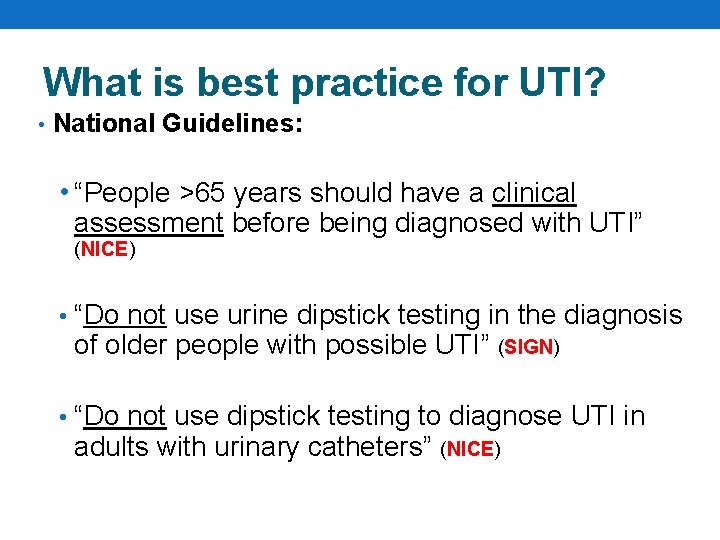
Using dipsticks What does the Test strip test for? • The presence of Bacteria NOT the whether the bacteria are causing an infection. • CANNOT prove UTI
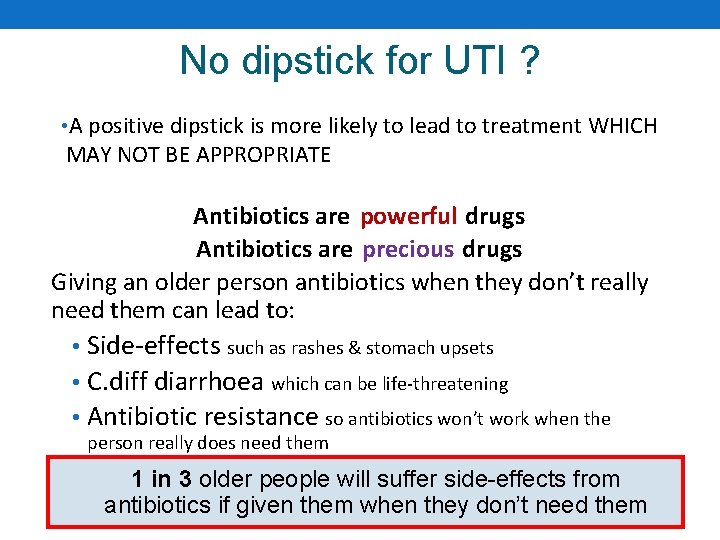
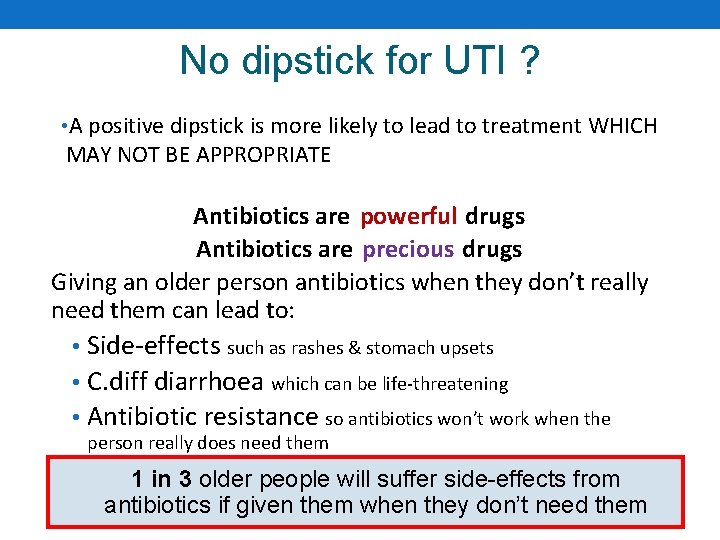
No dipstick for UTI ? • A positive dipstick is more likely to lead to treatment WHICH MAY NOT BE APPROPRIATE Antibiotics are powerful drugs Antibiotics are precious drugs Giving an older person antibiotics when they don’t really need them can lead to: • Side-effects such as rashes & stomach upsets • C. diff diarrhoea which can be life-threatening • Antibiotic resistance so antibiotics won’t work when the person really does need them 1 in 3 older people will suffer side-effects from antibiotics if given them when they don’t need them
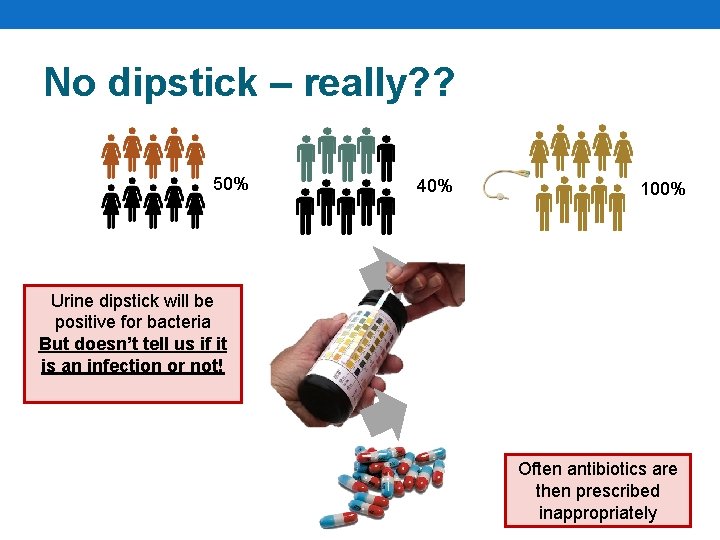
No dipstick – really? ? 50% 40% 100% Urine dipstick will be positive for bacteria But doesn’t tell us if it is an infection or not! Often antibiotics are then prescribed inappropriately
What is best practice for UTI? • National Guidelines: • “People >65 years should have a clinical assessment before being diagnosed with UTI” (NICE) • “Do not use urine dipstick testing in the diagnosis of older people with possible UTI” (SIGN) • “Do not use dipstick testing to diagnose UTI in adults with urinary catheters” (NICE)
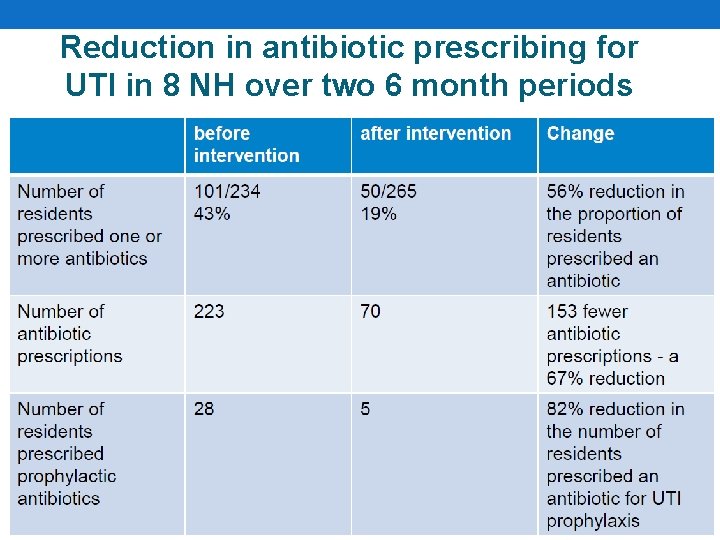
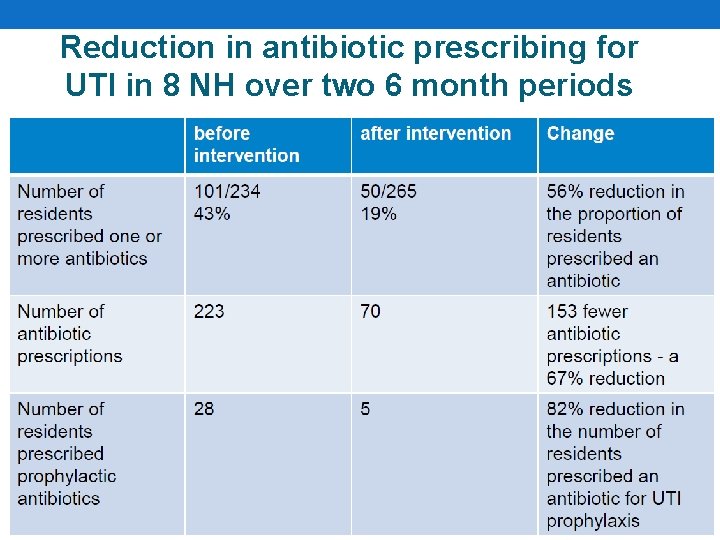
Reduction in antibiotic prescribing for UTI in 8 NH over two 6 month periods
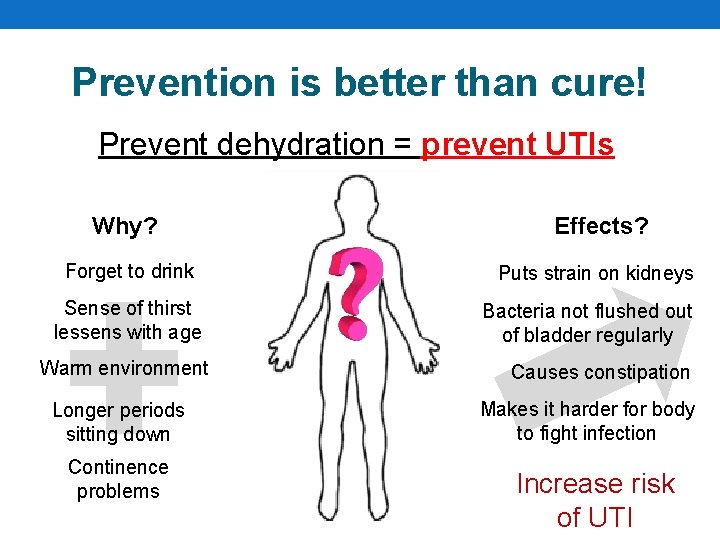
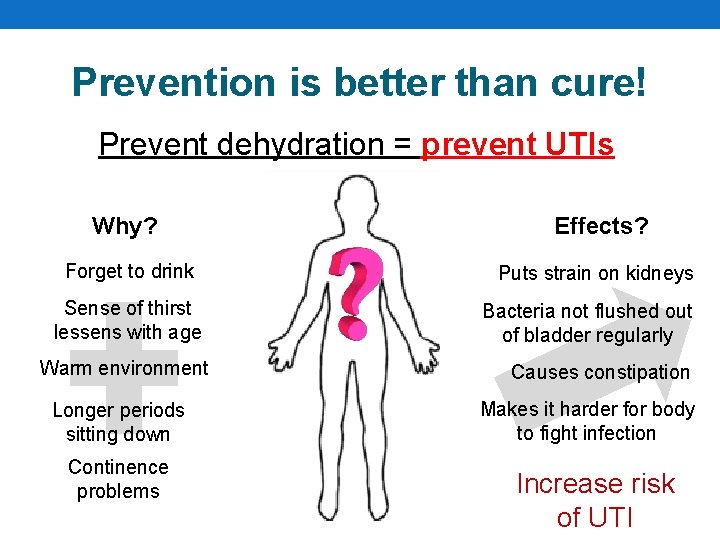
Prevention is better than cure! Prevent dehydration = prevent UTIs Why? Effects? Forget to drink Puts strain on kidneys Sense of thirst lessens with age Warm environment Longer periods sitting down Continence problems Bacteria not flushed out of bladder regularly Causes constipation Makes it harder for body to fight infection Increase risk of UTI
Staying hydrated Some residents may need further support to stay hydrated. For example: • Choose a cup suitable for the resident – they may prefer to use a straw • Support and encouragement to maintain fluid intake throughout the day • It could be as simple as set drink routines rather than relying on thirst alone • Jelly and other food rich in fluid can be offered to increase fluid intake if the resident doesn’t want to drink • Encourage fluids when giving care at night
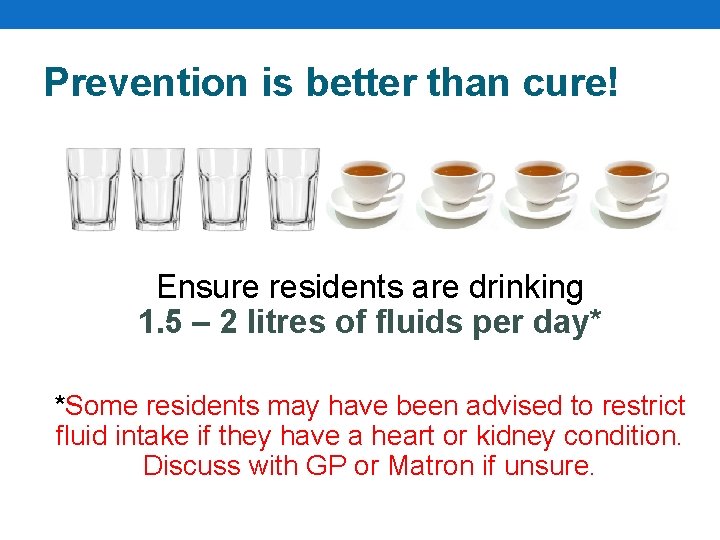
Prevention is better than cure! Ensure residents are drinking 1. 5 – 2 litres of fluids per day* *Some residents may have been advised to restrict fluid intake if they have a heart or kidney condition. Discuss with GP or Matron if unsure.
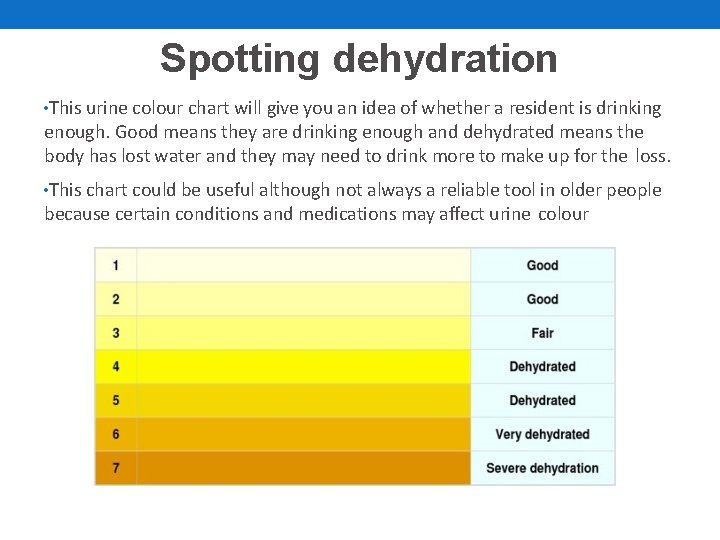
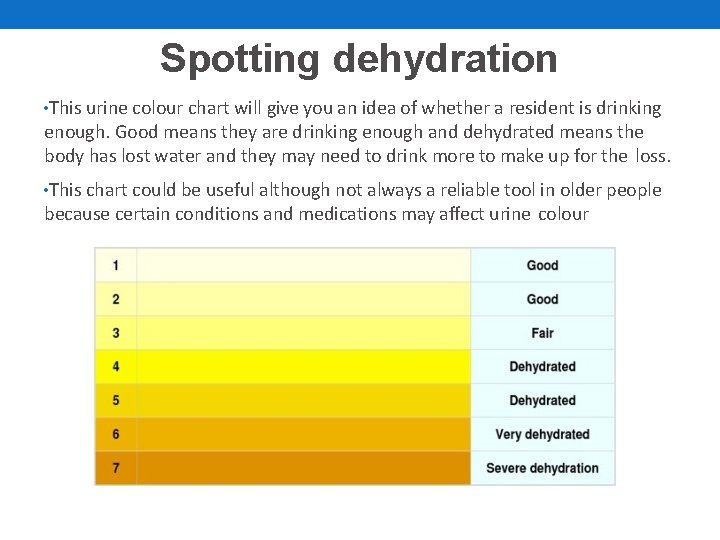
Spotting dehydration • This urine colour chart will give you an idea of whether a resident is drinking enough. Good means they are drinking enough and dehydrated means the body has lost water and they may need to drink more to make up for the loss. • This chart could be useful although not always a reliable tool in older people because certain conditions and medications may affect urine colour
Signs of dehydration • Thirst • Dark urine • Sunken eyes • Irritability • Confusion • Cool hands or feet • Low blood pressure • Raised heart rate • Headaches • If a person has AKI they may pass less urine than usual, or pass no urine at all

Training Video https: //www. youtube. com/watch? v=r. Z 5 T 1 Cz 7 DHQ&featur e=youtu. be How will this work in your Care Home?

This is a Herts-wide initiative Success elsewhere The first ‘To Dip Or Not To Dip’ project was in South-West England: • Reduced antibiotic use in Care Home residents by over 60% • Reduced emergency admissions for UTI and dehydration by 50% Across the UK, ‘To Dip Or Not To Dip’ is taking off! Your help and feedback is vital!
Summary • Training for GP practice staff complete • Training for Care Home staff taking place across October 2017 • Specially designed resources available on CCG website: (http: //www. enhertsccg. nhs. uk/urinary-tract-infections-utis-carehomes) – one laminated set of posters will be sent to all Care Homes via post* • All Homes and GP staff to use forms from October 30 th 2017 • Follow-up webinars towards the end of the year • This is a culture change – What are the pitfalls? Are you concerned about not dipping? • Dipsticks needed for other diagnosis e. g. diabetes • Post-launch survey and audit *Care Homes can print more posters using the source documents on the CCG website if required
Next Steps for Attendees • Disseminate training to all carers • Work with your aligned GP practice to agree form process • Support culture change within your home (and within your aligned GP practice) • Attend follow-up webinars (dates to be confirmed) • Request further training (see next slide) • Report any ‘road blocks’ to the CCG (see next slide)
Key Contacts All queries and training requests: • David. Ladenheim@enhertsccg. nhs. uk (Senior Pharmaceutical Adviser, Pharmacy & Medicines Management, East and North Hertfordshire CCG) • Jamie. Archer@enhertsccg. nhs. uk • (Project Manager, East and North Hertfordshire CCG) *Supporting resources, key contact details, etc. will be disseminated after this seminar
 Symptoms of urinary tract infection
Symptoms of urinary tract infection ç
ç Tumor in the urinary tract
Tumor in the urinary tract Complicated urinary tract infection
Complicated urinary tract infection Urinary tract infection in pregnancy ppt
Urinary tract infection in pregnancy ppt Histological structure of kidney
Histological structure of kidney Nursing management for urinary tract infection
Nursing management for urinary tract infection Urethra
Urethra Difference between pyramidal and extrapyramidal tract
Difference between pyramidal and extrapyramidal tract Anterior spinothalamic tract
Anterior spinothalamic tract Johnson and johnson botnet infections
Johnson and johnson botnet infections Bone and joint infections
Bone and joint infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Methotrexate yeast infection
Methotrexate yeast infection Classification of acute gingival infections
Classification of acute gingival infections Infections opportunistes digestives
Infections opportunistes digestives Genital infections
Genital infections Opportunistic infections
Opportunistic infections Storch infections
Storch infections Bacterial vaginosis
Bacterial vaginosis Amber blumling
Amber blumling