Urinary tract infection Dr Mai Banakhar UTI inflammatory
Urinary tract infection Dr. Mai Banakhar
UTI • inflammatory response of urothelium to bacterial invasion.
• • Bacteriuria : bacteria in urine Asymptomatic or symptomatic Bacteriuria + pyuria= infection Bacteriuria NO pyuria = colonization
• • • Pyuria : WBCs in urine. Infection T. B Bladder stone.
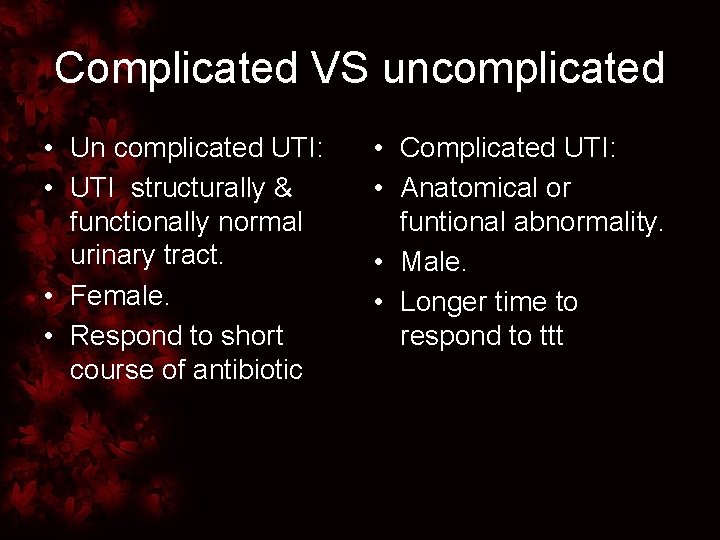
Complicated VS uncomplicated • Un complicated UTI: • UTI structurally & functionally normal urinary tract. • Female. • Respond to short course of antibiotic • Complicated UTI: • Anatomical or funtional abnormality. • Male. • Longer time to respond to ttt

• Isolated UTI: • 6 months between infections.
• • • Recurrent UTI: >2 infections in 6 months 3 UTI in 12 months. Reinfection by different bacteria. Persistence : same organism from focus within the urinary tract. Struvate stone. Bacterial prostatitis. Fistula Urethral diverticulum. atrophic infected kidney.
• Unresolved infection: • in adequate therapy , bacterial resistance to ttt.
Risk factors to bacteriuria • Female • Age • Low estrogen ( menopause) • Pregnancy. • D. M • Previous UTI. • FC • • • Stone GU malignancy. Obstruction. Voiding dysfunction. Institutionalized elderly
Microbiology Faecal-drived bacteria Uncomplicated UTI E. Coli, G-ve baccillus, (85%- 50%) Staph saprophyticus Enterococ faecalis Proteus Klebsiella. • • • Complicated UTI E. coli 505 Enterococ faecalis. Staph aureus Staph epidermidis Pseudomonas aeruginosa
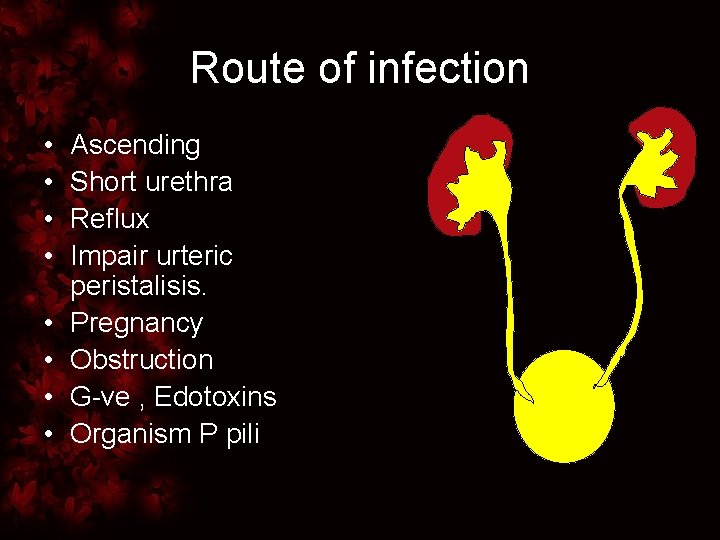
Route of infection • • Ascending Short urethra Reflux Impair urteric peristalisis. Pregnancy Obstruction G-ve , Edotoxins Organism P pili
Route of infection • • • Haematogenous: Uncommon. Staph aureus. Candida fungemia. T. B • Lymphatics: • Rarely in inflammatory bowel disease, reteroperitoneal abscess
• Increase UTI risk • Protect against UTI • Increase bacterial virulence • Host defences
Factors increasing bacterial virulence • • Adhesion factors Toxins Enzyme production. Avoidance of host defense mechanisms
Factors increasing bacterial virulence • Adhesion factors • G-ve bacteria, Pili • Attachment to host urothelial cells. • Single type or different types e. x E. coli • Defined functionally be mediating hemagglutination (HA) of specific erythrocytes • Mannose –sensitive • (type 1) • Produced by all strains E. coli • Certain pathogenic types of E. coli mannose resistant pili ( pyelonephritis)
Factors increasing bacterial virulence • Avoidance of host defense mechanisms • E. coli • Extracellular capsule • Immunogenisity • Toxins: • E. coli cytokines, pathogenic effect on host tissues phagocytosis • M. Tuberculosis reisit phagocytosis by preventing phagolysosome fusion • Enzyme production: • Proteus ureases • Ammonia struvite stone formation
Host defences • Protective • Mechanical (flushing of urine) antegrade flow of urine • Tamm-Horsfall protein (mucopolysaccharide coating bladder prevent bacterial attachment) • chemical : Low Urine PH & high osmolality • Urinary Immunoglobulin I g. A inhibit adherence
Lower UTI • Cystitis: infection& inflammation of the bladder • Frequency, samll volumes, dysuria, urgency, offensive urine SP pain, haematuria, fever & incontinence.
Investigation • Dipstick of MSU • WBC ( pyuria ) • 75 -95% sensitivity infection • False –ve • False +ve • Other causes of pyuria • • • Nitrite testing: Bacteriuria. Specificity >90% Sensitivity 35 - 85% + test ------- infection ----infection
Investigation • • Microscopy : Bacteria : False –ve low bacterial count False +ve contamination (lactobacilli & corynebacteria ) epithelial cells • RBCs & pyuria
Investigation Indications for further investigations in LUTI. • Symptoms of Upper UTI. • Recurrent UTI. • Pregnancy • Unusal infecting organism ( proteus suggest infection stone) • • KUB Ultrasound IVU cystoscopy
DD • • • Non-infective cystitis: radiation cystitis Drud cystitis ( cyclophosphamide ) Haemorrhagic cystitis Urethritis
Treatment • Aim : • Resistance : • Eliminate bacterial • Intrinsic (proteus) growth from urine. • Genetically • Empirical ttt before transferred between culture & sensitivity bacteria by R for the most likely plasmids. organism. • Adgusted according to the culture & sensitivity.
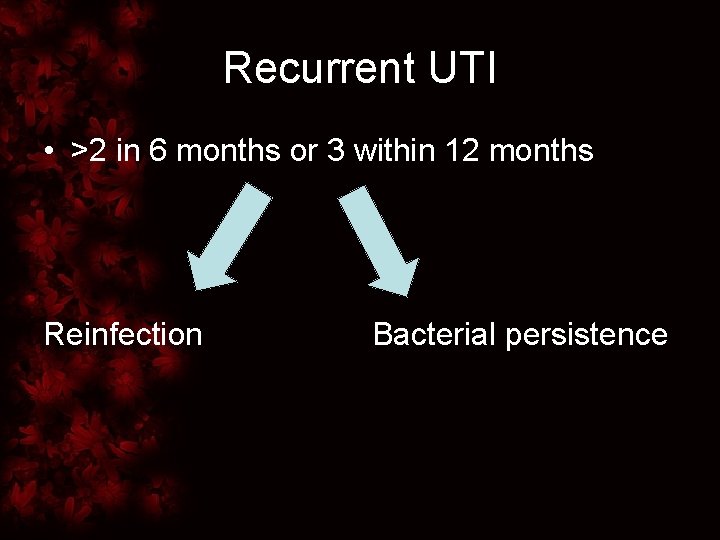
Recurrent UTI • >2 in 6 months or 3 within 12 months Reinfection Bacterial persistence
Recurrent UTI • Reinfection ( different • Bacterial persistance ( bacteria) same organism from a focus within tract) • After prolonged within short interval with adifferent organism • Functional or anatomical problem. • Reinfection in females • The underlying • No anatomical nor problem should be functional pathology treated • In males BOO, urethral stricture
Management Reinfection UTI • Females • KUB, Ultrasound, cystoscopy • Simple Reinfection TTT Avoid spermicides Estrogen replacement therapy Low dose antibiotic prophylaxis
Female recurrent reinfection • Prophylactic antibiotic: • Reduce infection 90% at bed time 6 -12 months • Symptomatic reinfection • Trimethoprim • Nitrofurantoin • Cephalexin • Fluoroquinolones
Female recurrent reinfection • Natural youghart • Post-intercourse antibiotic prophylactic • Self-started therapy
Management of bacteria persistance • • Investigations: Kub, renal ultrasound. C. T, IVU Cystoscopy • Treatment : • For the functional or anatomical anomaly
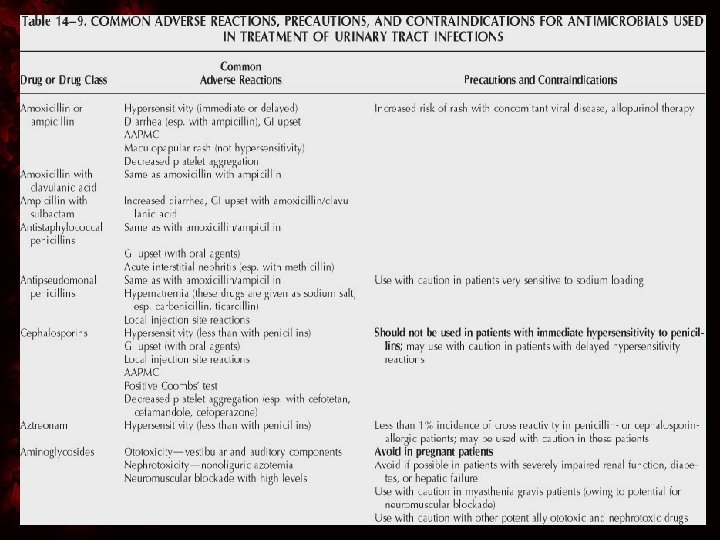
Antibiotics • Empirical therapy. • Definitive therapy. • Bacterial resistance to drug therapy.
Acute pyelonephritis • • Clinical Dx: Flank pain Fever. Elevated WBCs • DD: • acute cholecystitis. • Pancreatitis.
Acute pyelonephritis • • Risk factors: VUR UTO Spinal cord injury D. M Malformation pregnancy FC

Acute pyelonephritis • Pathogenisis : • Initially patchy • Inflammatory bands from renal papilla to cortex. • 80% E. coli, others klebsiella, proteus& pseudomonas.
Acute pyelonephritis • Urine analysis & culture. • CBC , U&E • KUB & ultrasoundif no response with I. V antibiotic for 3 days go for CTU
Perinephric abscess • • • Pathogenesis. Suspected? ? C. T, ultrasound PC drainage. Open surgical
Pyonephrosis • • • Infected hydronephrosis. Pus accumulation Causes Ultrasound. C. T Management: PCN, I. V antibiotic, I. V fluids.
Emphysematous pyelonephritis • Severe form of acute pyelonephritis • Gas forming organism • Fever, abdominal pain with radiographic evidence of gas within the kidney. • D. M • Urinary obstruction. • High glucose level-------fermentation, CO 2 production
Emphysematous pyelonephritis • • Presentation: sever acute pyelonephritis High fever & systemic upset E. coli, commonly, Klebsiella & proteus less frequent
Management • • KUB Ultrasound, C. T Patients are unwell Mortality is high
Management • • Conservative ? I. V antibiotic , IVF PC drainage Control D. M • Sepsis is poorly controlled • Nephrectomy
Xanthogranulomatous pyelonephritis • • • Severe renal infection Renal calculi & obstruction. Result in non-functioning kidney E. coli & proteus common. Macrophage full of fat deposit around the abscess • Kidney, perinephric fat
Xanthogranulomatous pyelonephritis • Acute flank pain • Fever & tender flank mass • C. T , Ultrasound • Stone , mass ? ? RCC
Xanthogranulomatous pyelonephritis • IV antibiotic , • Nephrectomy
- Slides: 46