Urinary System The urinary system functions to keep




















- Slides: 58

Urinary System § The urinary system functions to keep the body in homeostasis by controlling the composition and volume of the blood. § This is accomplished by removing water and solutes from the blood and then selectively restoring them. § The excessive water, ions and solutes including toxins are excreted in the form of urine
§ The urinary system is composed of 4 different organs: 2 kidneys, 2 ureters, 1 bladder and 1 urethra
Other functions § Regulates blood pressure by producing and excreting the enzyme renin which regulates blood volume by water retention § Producing and secreting the hormone Erythropoiten, which stimulates erythropoiesis § Regulate blood p. H ( acidity) § Activate vitamin D
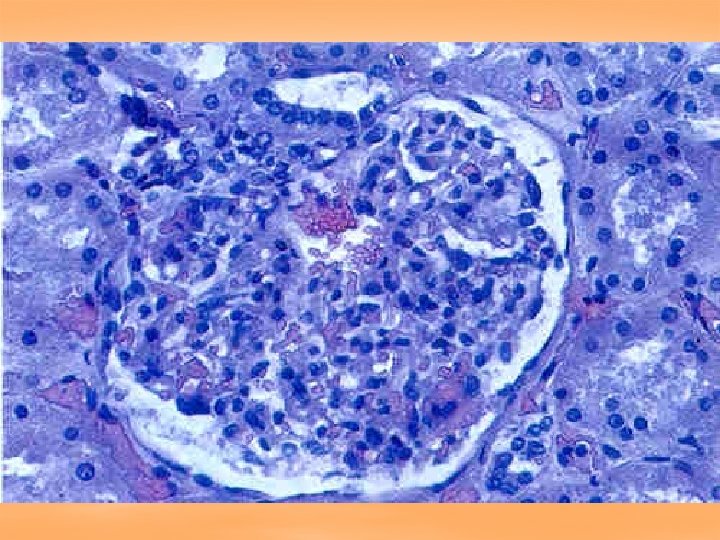
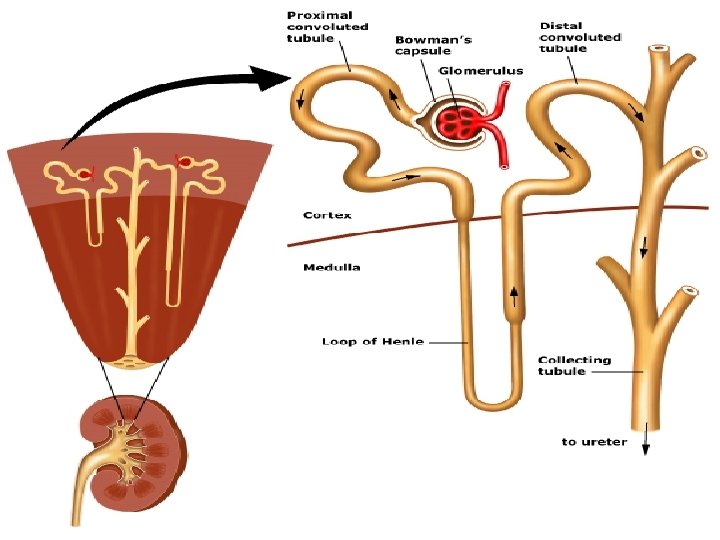
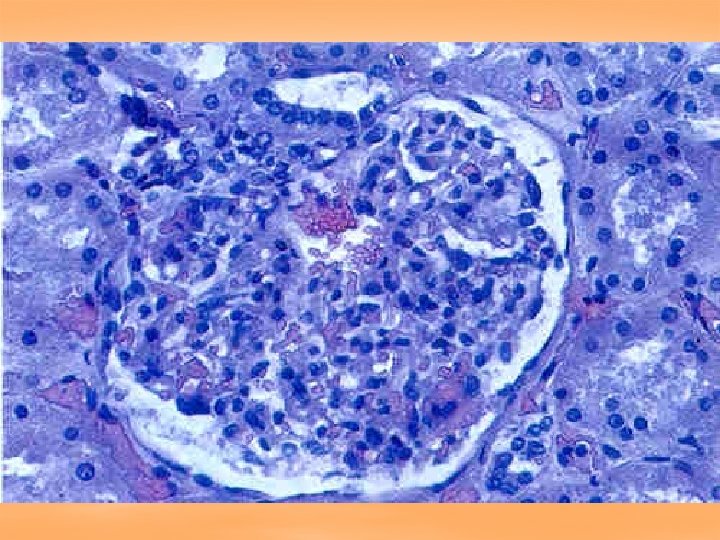
Nephron: Functional unit of the kidney § There are over 1 million nephrons that process and filter the blood, selectively reabsorbing the filtrate or allowing it to become urine. § A nephron consist of a renal tubule and a capillary network called a glomerulus § The end of the renal tubule expands into a cup shaped capsule which encloses the glomerulus ( it is called the glomerular capsule) (Bowmans capsule)

§ Together the glomerulus and its capsule are called the renal corpuscle § The glomerular capillaries are fenestrated ( very porous) allowing virtually all substances except blood cells and large proteins to pass from the capillaries into the glomerular capsule
§ The glomerular capsule surrounding these fenestrated capillaries consists of an outer (parietal) layer of simple squamous epithelium and a visceral layer ( next to the glomerulus) made of epithelial cells called podocytes ( the arms of these “octopus” like cells are called pedicles and they wrap around the fenestrated capillaries leaving openings called filtration slits, which control the openings to the pores in the capillaries)
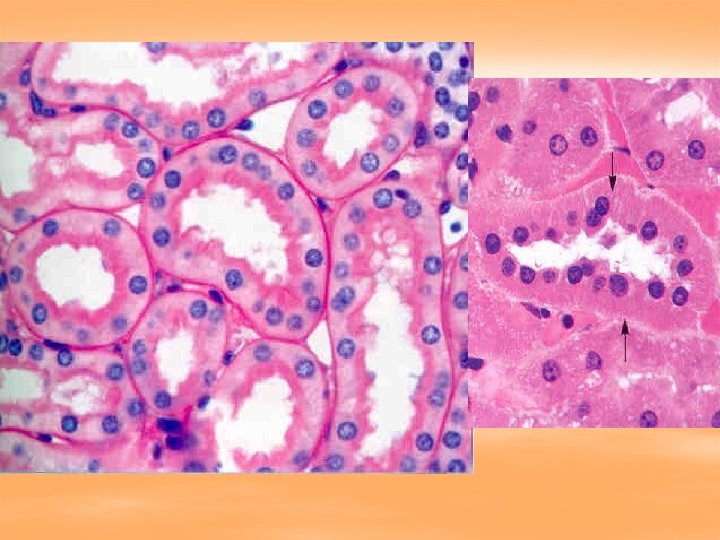
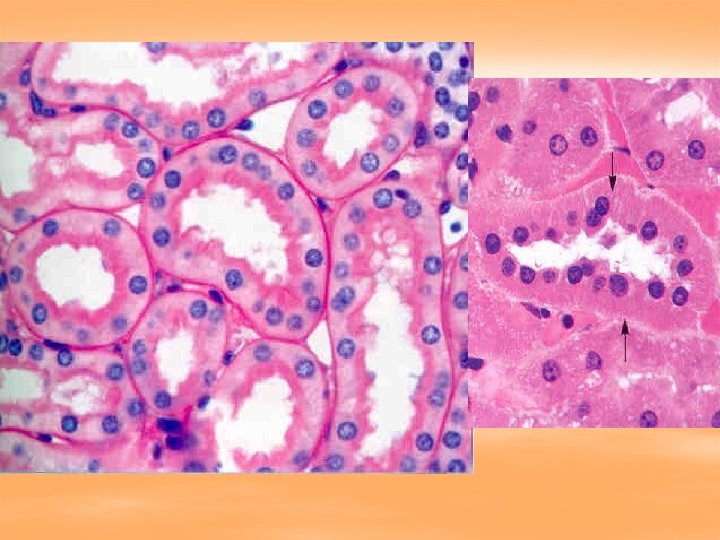
Proximal convoluted tubules § First section of tubule that connects to Bowman’s capsule § composed of simple cuboidal epithelium with microvilli ( fuzzy)
Ascending and descending loop of Henle § Ascending loop has simple cuboidal epithelium § Descending loop has simple squamous epithelium

Distal convoluted tubules § Shorter and has fewer microvilli than PCT (so not fuzzy)
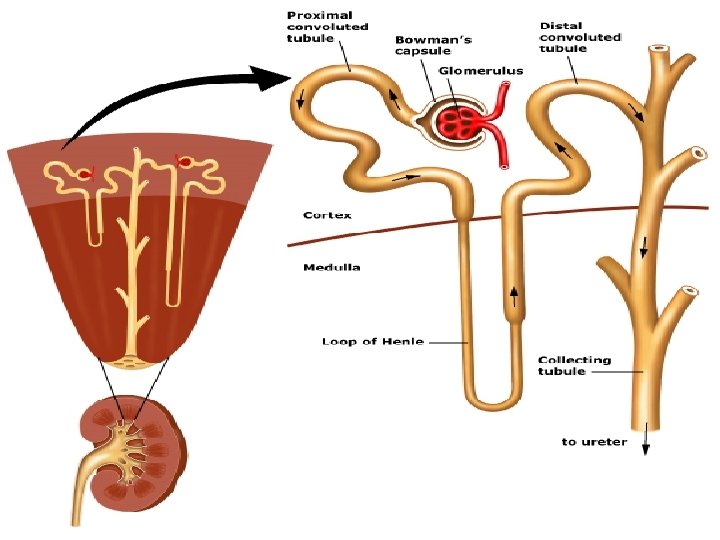



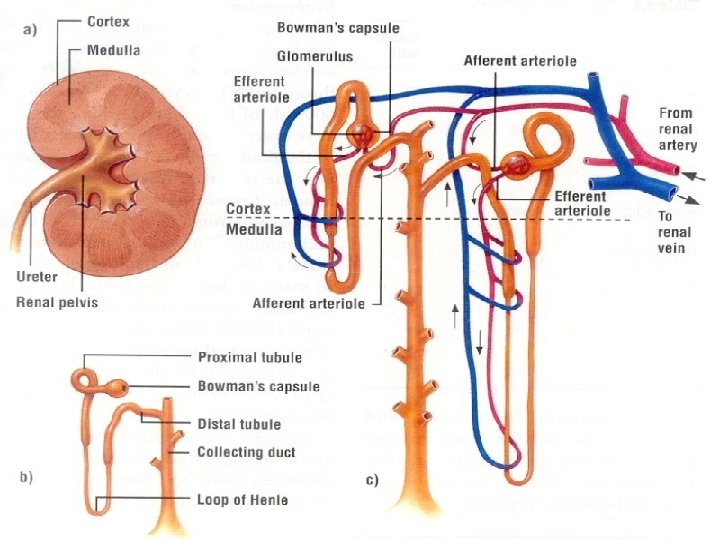
Types of nephrons classified according to position in kidney § § § 1. Juxtamedullary nephron: originated in inner 1/3 of the cortex , have long loops of Henle that extend deep into the medulla 2. Cortical nephrons: Originated in outer 2/3 of cortex Very short loops of Henle which do not extend deep into the medulla
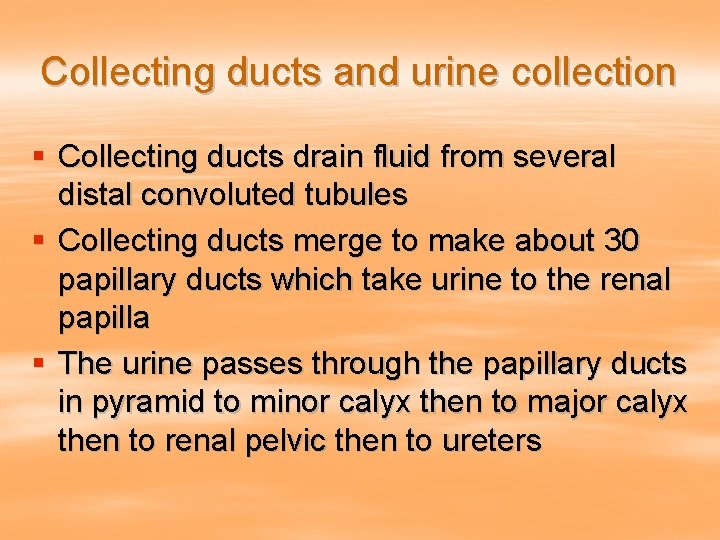
Collecting ducts and urine collection § Collecting ducts drain fluid from several distal convoluted tubules § Collecting ducts merge to make about 30 papillary ducts which take urine to the renal papilla § The urine passes through the papillary ducts in pyramid to minor calyx then to major calyx then to renal pelvic then to ureters
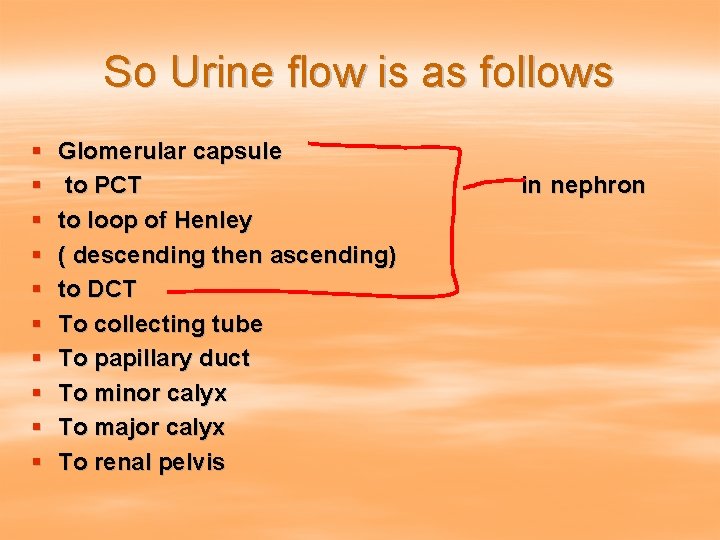
So Urine flow is as follows § § § § § Glomerular capsule to PCT to loop of Henley ( descending then ascending) to DCT To collecting tube To papillary duct To minor calyx To major calyx To renal pelvis in nephron
§ § § Out kidney to ureter To bladder To urethra Out body
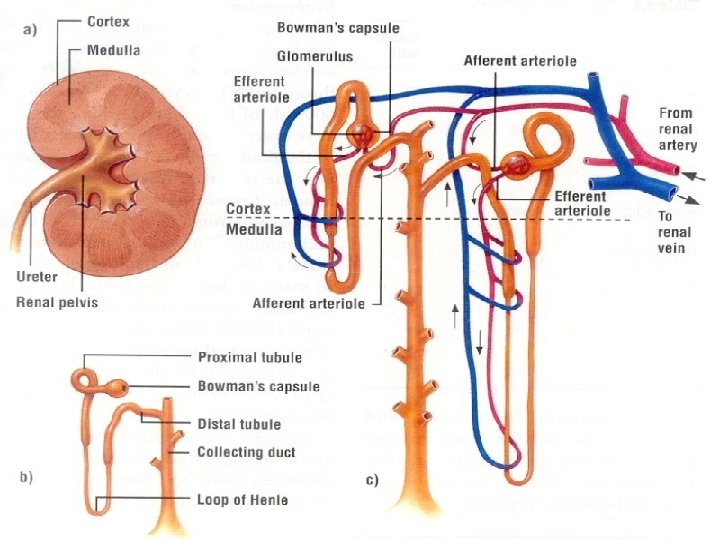
Blood supply to the kidneys § Renal artery: brings blood to kidney § Segmental artery: branches of renal artery supplying segments in plevis § Interlobar artery: takes blood up renal columns § Arcuate artery: takes blood across base of pyramid § Interlobular artery: takes blood up into cortex
§ Afferent arteriole: microscopic vessel taking blood to glomerulus § Glomerulus: capillary bed in Bowman’s capsule § Efferent arteriole: arteriole with a smaller diameter that takes blood away from glomerulus
§ Peritubular capillaries: takes blood from efferent arterioles to interlobular vein § Veins in the kidney corresponds to arteries in kidneys
Kidneys § Is retroperitoneal: behind the parietal peritoneum) attached to the posterior body wall right below the 12 th thoracic vertebrae ( lowest rib) § Renal Ptosis: kidney drops due to inadequate support § This can cause a “kink” in the ureter § Occurs most often in old, thin, or anorexic people
Kidney functions § § § Remove nitrogen waste Regulate p. H Excrete excess metabolic substances Maintain water balance Help regulate blood pressure Secrete erythropoietin to stimulate RBC production § Participates in synthesizing vitamin D

Anatomy of Kidney § 3 layers of tissue surround, support and protect each kidney: 1. renal capsule: inner most layer, primary barrier to infection 2. Adipose capsule: fatty tissue which holds kidney in place and protects it against trauma ( cushions it) 3. Renal fascia: thin fibrous connective tissue which anchors kidney to body wall
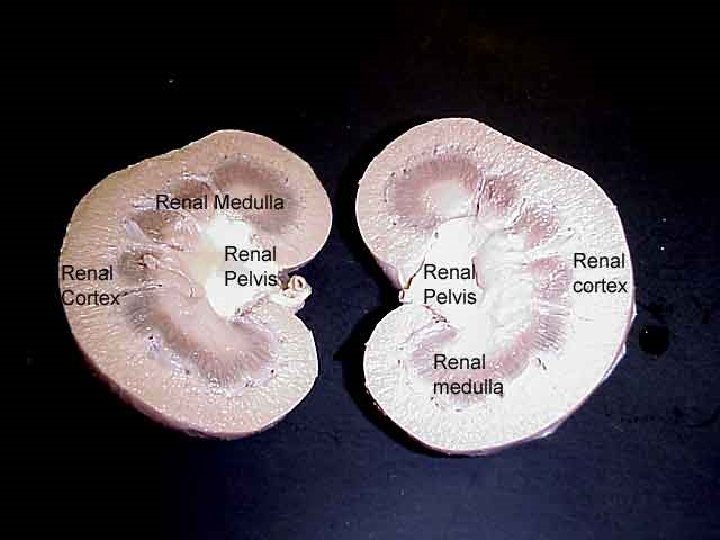
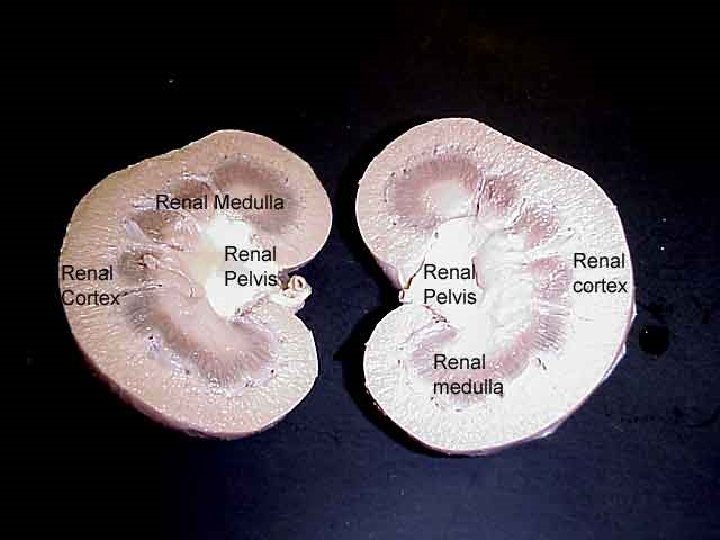
Internal anatomy § Cortex: outer layer § Medulla: inner layer contains the renal pyramids § Renal pelvis: where major calyx empties into and ureter enters kidney




Ureter § A slender tube running retroperitoneally ( 10 t 0 12 inches) from kidney to bladder § The ureters enter the bladder at its base in such a manner that during the pressure of urination, the ureters are compressed and closed preventing backflow of urine to the kidneys § This also prevents the spread of bladder infections § Works via wave-like contractions that carry urine through ureters ( peristalysis)
Bladder § Retroperitoneal § Storage sac with maximum capacity of 700 to 800 ml § Located posterior to pubic symphysis and anterior to rectum § It is a collapsible hollow sac composed of transitional epithelium ( stretch changing from cuboid to squamous shape)

Urethra: § Tube draining from floor of bladder to outside § Since female urethra’s (1 ½ inch) are shorter than males (8 inches), they are more prone to bladder infections § Has 2 sphincter muscles: § Internal urethral sphincter: involuntary § External urethral sphincter: voluntary


Micturition ( urination) § Involves both the involuntary and voluntary nervous systems § There are 2 sphincter muscles that control the opening form bladder to urethra § The internal ( involuntary) open when bladder is ¼ to ½ full) the external is voluntary and under conscious control § Lack of control is called incontinence § In infants it is normal. . Since the voluntary nerve does not develop until around 12 to 18 months § In adults it is due to nerve/muscle damage or unconsciousness, or overriding physical/emotional stress
A few Conditions § § § Nephritis: inflammation of kidney tissue Cystitis: inflammation of the bladder Enuresis ( or nocturia) bed wetting Retention: failure to void Suppression or anuria: failure the kidneys to make urine or daily output of less than 50 ml § Renal calculi: kidney stones, crystals of slats solidify not insoluble stones common components are calcium oxalate, uric acid and calcium phosphate
Fluid and Electrolytes § Depending on age, sex, health our bodies are about 50 to 75% water § Intracellular fluid (IFC) inside cells = 2/3 of total body fluids § Extracellular fluids: (ECF): 1/3 of total body fluid and is outside the cells
Types of Extracellular fluids: (ECF): 1. 2. 3. Plasma: within blood vessels Interstitial fluids: between cells Other: lymph, gastric juices, tears, synovial fluids Water serves as the universal solvent in which a variety of solutes are dissolved This internal environment bathes our cells and caries dissolved nutrients, gases, waste, etc. .

The solutes are broadly classified as: 1. Electrolytes: chemical substances such as salts, acids and bases, which when they dissolve, they dissociate ( break up) into ions ( charged particles) 2. Non-electrolytes: chemical substances which do not dissociate or form ions when dissolved ex glucose, lipids, some proteins
§ To control the water balance in our bodies, we simply control the number of solutes § The most important solutes for controlling osmosis are electrolytes. § They dissociate when dissolved creating more particles
3 General electrolyte functions 1. Many are essential minerals 2. They control osmosis ( between body compartments) 3. They help maintain the proper p. H (acid/base balance)

Examples of electrolytes 1. Sodium : most abundant extracellular ion. Involved in verve transmission, muscle contraction and in fluid/electrolyte balance 2. Chloride: primarily extracellular and involved in osmotic regulation 3. Potassium: most abundant cation in the intracellular fluids. Key to maintaining fluid volume of cells and to controlling p. H
Examples of electrolytes 4. Calcium: extracellular electrolyte. A component of bone, blood clotting and muscle and nerve impulses 5. Phosphate: intracellular electrolytes. A bone component, necessary part of nucleic acids including the “p” in ATP
Osmotic Regulation § Is the maintenance of normal water and salt balance in body fluids § Water enters animal bodies in various ways depending on the animal § The water is lost through evaporation, feces and excretion § To be fluid balance, the amount of water that exits the body must equal the amount that enters
Physiology § The work of the urinary system is done by the nephrons… other parts are simply passage ways and storage areas ( system fillters 45 gallons of blood per day, the plasma is filtered and removed, and replaced 60 times a day)
3 steps of nephron urine formation 1. Glomerular filtration: The fluids and solutes ( plasma) are force out of the glomerular capillaries by hydrostatic pressure (blood pressure). This is a non-selective process where by the plasma is forced through a filtration membrane ( consists of fenestrated capillary endothelium, basement membrane, and filtration slits of visceral wall of glomerular capsule)

Pressure involved in Glomerular filtration § Glomerular (blood) hydrostatic pressure: (G. H. P. ): § Means blood pressure entering glomerulus § Is kept high because the afferent arteriole is much bigger than the efferent arteriole § Pressure moves fluid out of glomerulus at a force of 60 mm. Hg
2 forces oppose the G. H. P: § 1. Capsular hydrostatic pressure: (C. H. P) § Resistant pressure due to the fluids already in the glomerular capsule § Is about 20 mmhg § 2. Blood osmotic pressure (B. O. P) § Since blood remains more concentrated than the filtrate, the water tries to move back into the gloverular capillaries at a pressure of 30 mm. Hg
Net Filtration Pressure § The net result of the three above pressures § N. F. P. = G. H. P - C. H. P - B. O. P =10 § 60 mm. Hg - 20 mm. Hg - 30 mm. Hg § G. F. R ( golmerular filtration rate): § The amount of filtrate flowing out of all the renal corpuscles ( both kidneys) per minute § Normal 125 ml/min (or 48 gallons per day) § 99% of this filtrate is reabsorbed back into the boold ( leaving 1 ½ liters of urine)
3 steps of nephron urine formation 2. Tubular reabsorption § The movement of filtrate from the renal tubules back into the blood vessels § Needed substances are removed from the filtrate and returned to the peritubular capillary system § Reabsorption occurs both passively and actively
§ The permeability of the epithelial cells of the distal and collecting renal tubules is controlled by ADH § so urine concentration is controlled by ADH which increases permeability and thus reabsorption § The proximal renal tubules absorb 80% of filtrate that is absorbed § Certain substances are not reabsorbed usually because the body does not need them
steps of nephron urine formation 3. Tubular secretion § Chemicals still in the blood which are not needed by the body are discharged inot the urine by tubular secretion § Important in: § Eliminating substances to large to pass thru pores § Eliminating undesirable or excess substance which have been reabsorbed § Rid body of potasium ions § Control blood p. H

Urinary System