Urinary System REGULATING THE INTERNAL ENVIRONMENT Organs Kidney
- Slides: 32
Urinary System REGULATING THE INTERNAL ENVIRONMENT
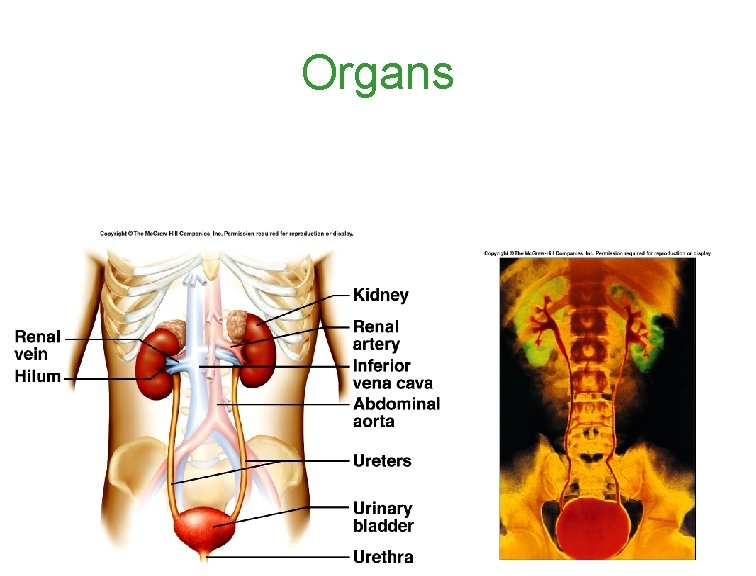
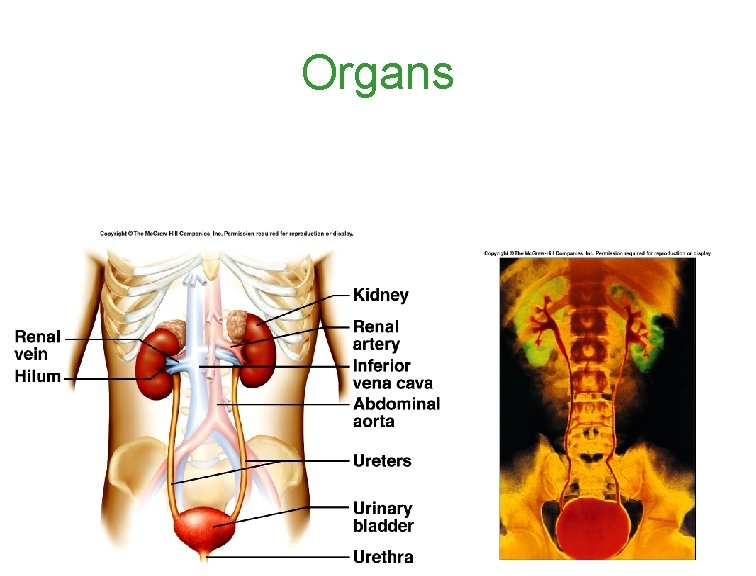
Organs
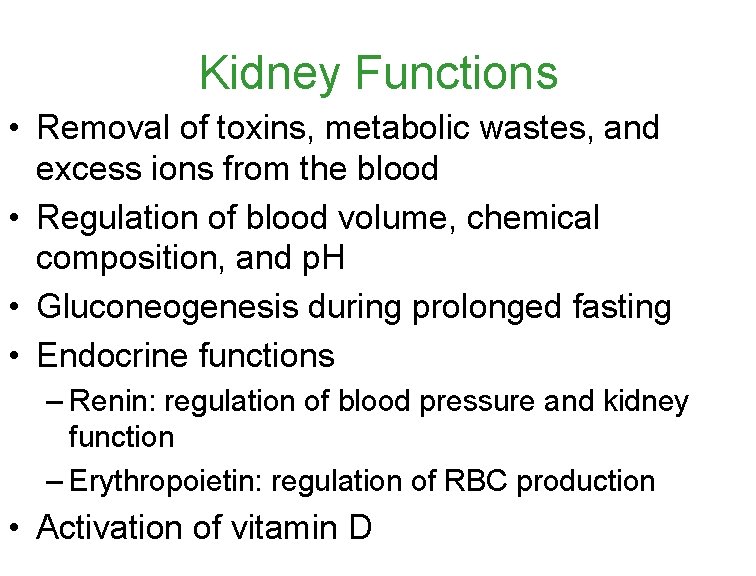
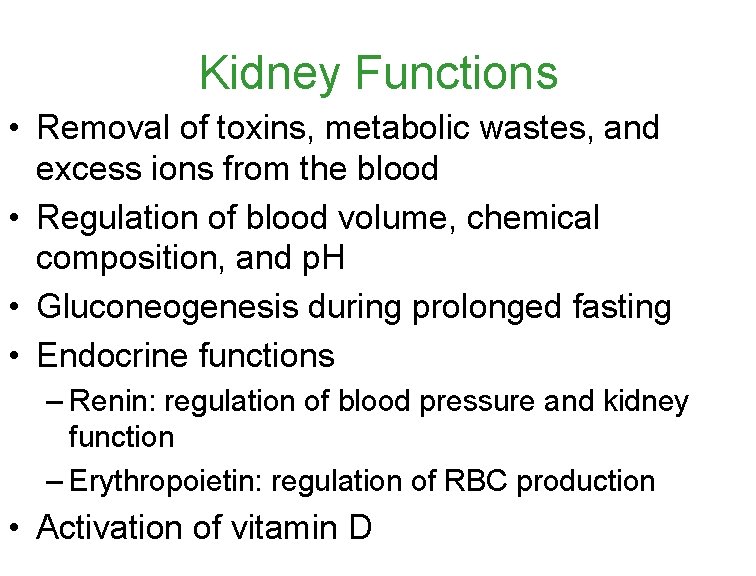
Kidney Functions • Removal of toxins, metabolic wastes, and excess ions from the blood • Regulation of blood volume, chemical composition, and p. H • Gluconeogenesis during prolonged fasting • Endocrine functions – Renin: regulation of blood pressure and kidney function – Erythropoietin: regulation of RBC production • Activation of vitamin D
Introduction: Two Major Functions of the Kidney • Osmoregulation: Management of the body’s water content and solute composition • Removing toxins and nitrogenous waste products that form from breaking down proteins before they accumulate to harmful levels
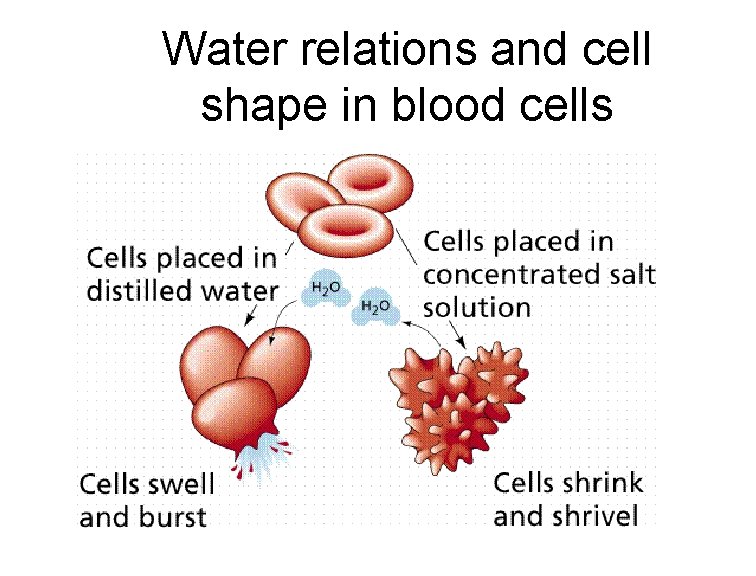
Osmoregulation • Over time, the rates of water uptake and loss must balance. • Lack of balance causes cells to swell or crenate. • Osmosis occurs whenever two solutions separated by a membrane differ in osmotic pressure, or osmolarity (moles of solute per liter of solution) • The osmolarity of human blood is about 300 mosm/L, while seawater has an osmolarity of about 1, 000 mosm/L.
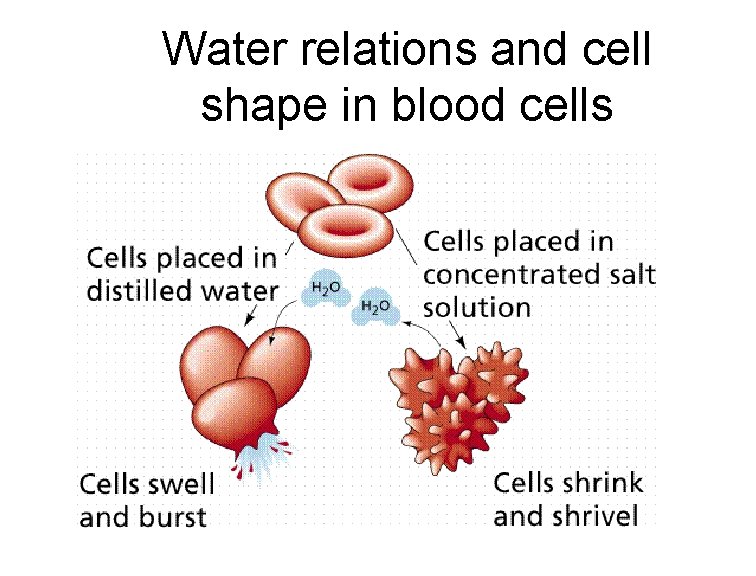
Water relations and cell shape in blood cells
Removal of Nitrogenous Wastes • the nitrogenous waste products are either ammonia or urea • Urea is far less toxic! – Urea is synthesized in the liver by combining ammonia with carbon dioxide and excreted by the kidneys.
General Structures – We have a pair of bean-shaped kidneys. Surrounded by fat - retroperitoneal – renal artery and a renal vein supply blood – less than 1% of body weight, receive 20% of resting cardiac output. – Urine exits the kidney through a duct called the ureter, and both ureters drain through a common urinary bladder. – urine is expelled from the urinary bladder through a tube called the urethra
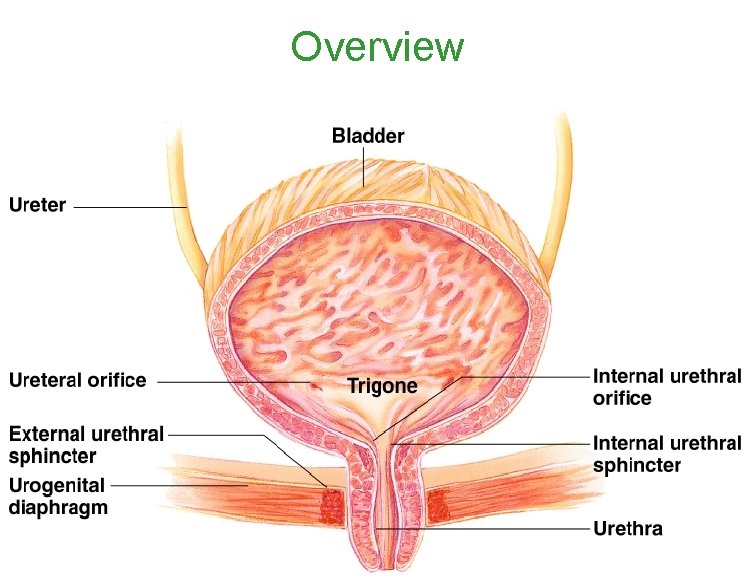
Ureters • Slender tubes attaching the kidney to the bladder – Continuous with the renal pelvis – Enter the posterior aspect of the bladder • Retroperitoneal • Peristalsis aids gravity in urine transport
Urinary Bladder • Smooth, collapsible, muscular sac • Temporarily stores urine • Trigone – triangle formed by the internal openings of the ureters and urethra • The lumen is lined with transitional epithelium • Bladder can expand significantly without increasing internal pressure
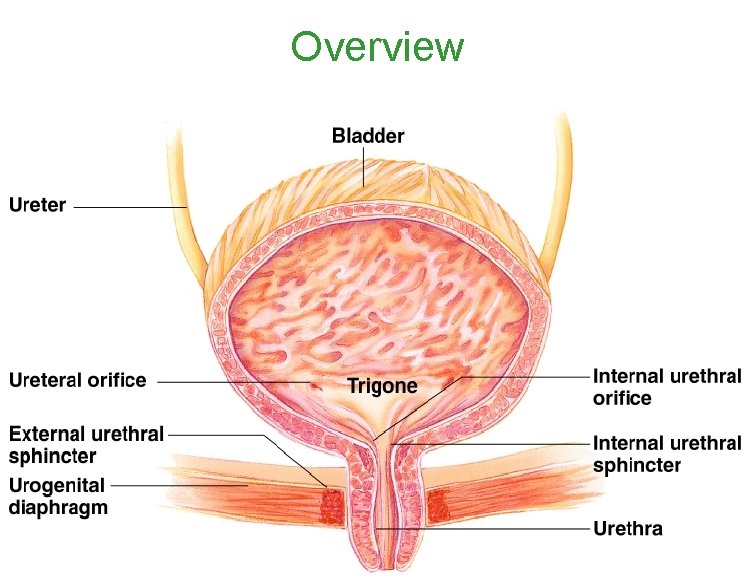
Overview
Urethra • carries urine from the bladder to the outside of the body by peristalsis • Release of urine is controlled by two sphincters – Internal urethral sphincter (involuntary) – External urethral sphincter (voluntary) • Length – Females – 3– 4 cm (1 inch) – Males – 20 cm (8 inches)
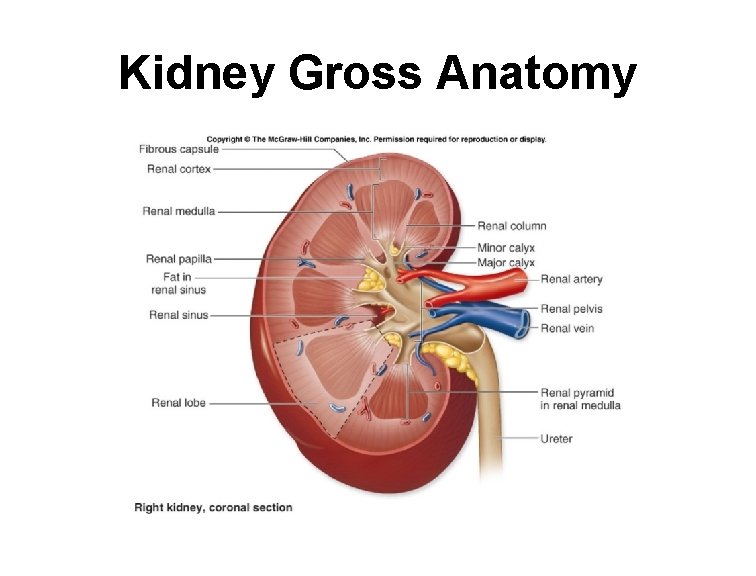
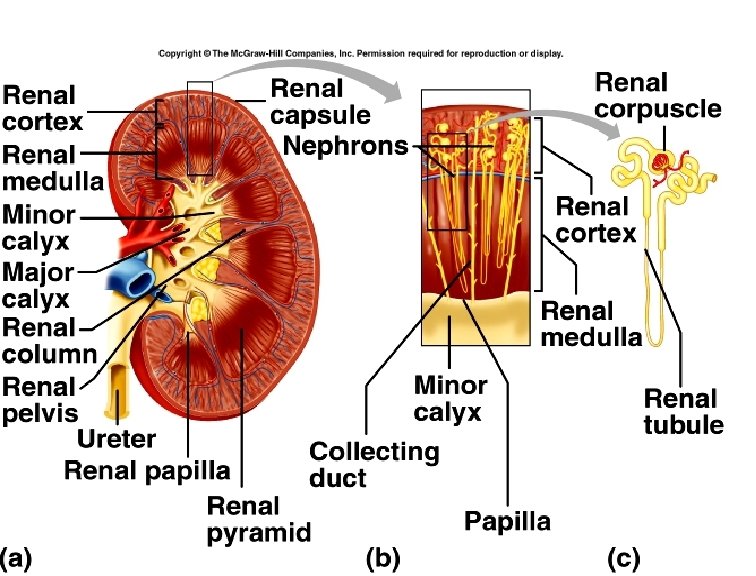
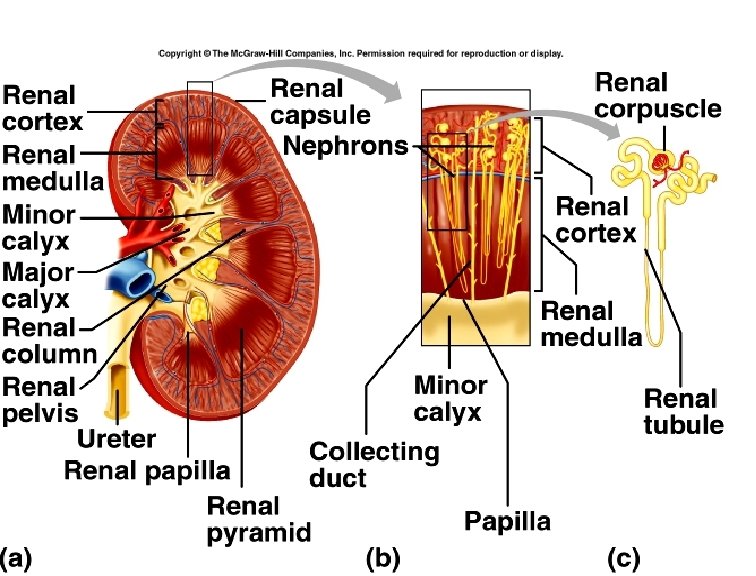
• kidney has two regions, renal cortex, and renal medulla. – Both regions are packed with microscopic excretory tubules called nephrons – Each human kidney packs about a million nephrons.
Renal Cortex • the outer part of the kidney. It contains the renal corpuscle and convoluted tubules. Ultrafiltration • Production of erythropoietin • The renal cortex is surrounded on its outer edges by the renal capsule, a layer of fatty tissue.
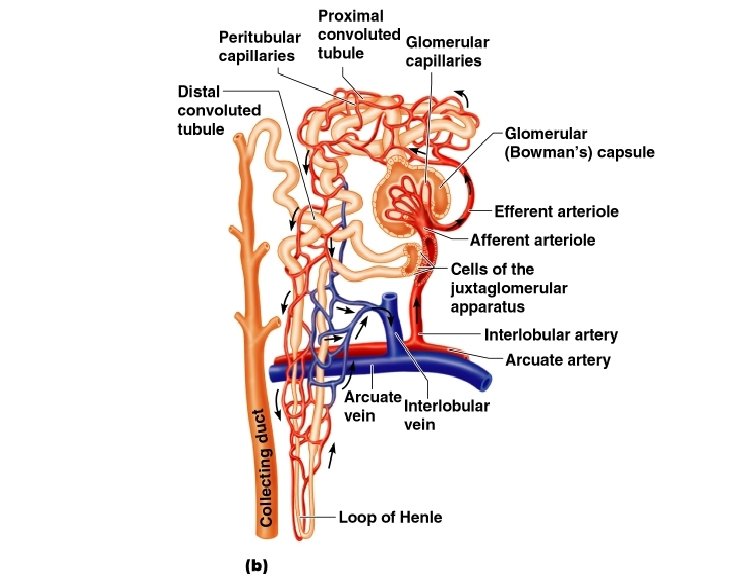
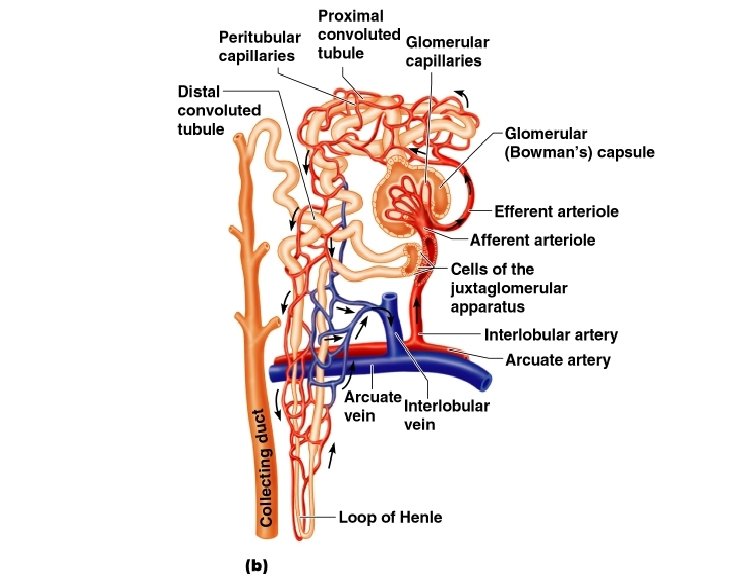
Renal corpuscle The renal corpuscle contains two structures: – a single long tubule and a ball of capillaries, called the glomerulus. – a cup-shaped swelling at the blind end of the tubule called Bowman’s or glomerular capsule
Renal Medulla • The smooth, inner tissue of the kidney. • Composed of loops of Henle and Renal Pyramids which are formed by the collecting ducts. • At the end of each nephron in the renal medulla is a collecting duct where filtered fluids exit the nephrons. • The fluid then moves on to its final stops in the renal pelvis
Renal Sinus • The renal sinus is a space between the renal medulla and hilum. Within the renal sinus are minor and major calyces and the renal pelvis • The first part of the renal pelvis contains the calyces. These are small cup-shaped spaces that collect fluid before it moves into the bladder. This is also where extra fluid and waste become urine.
• The renal pelvis is a funnel-shaped space in the innermost part of the kidney. It functions as a pathway for fluid on its way to the bladder
The Hilum A small opening located on the inner edge of the kidney, where it curves inward to create its distinct beanlike shape. The renal pelvis passes through it, as well as the: o Renal artery. This brings oxygenated blood from the heart to the kidney for filtration. o Renal vein. This carries filtered blood from the kidneys back to the heart.
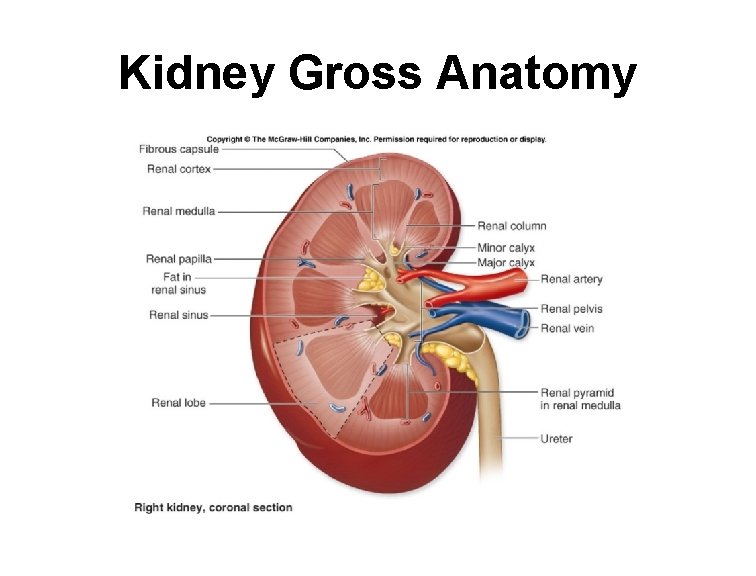
Kidney Gross Anatomy
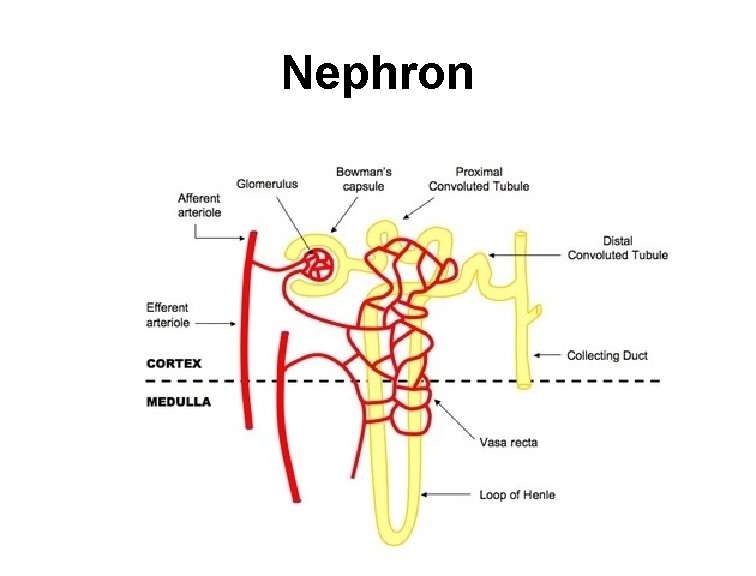
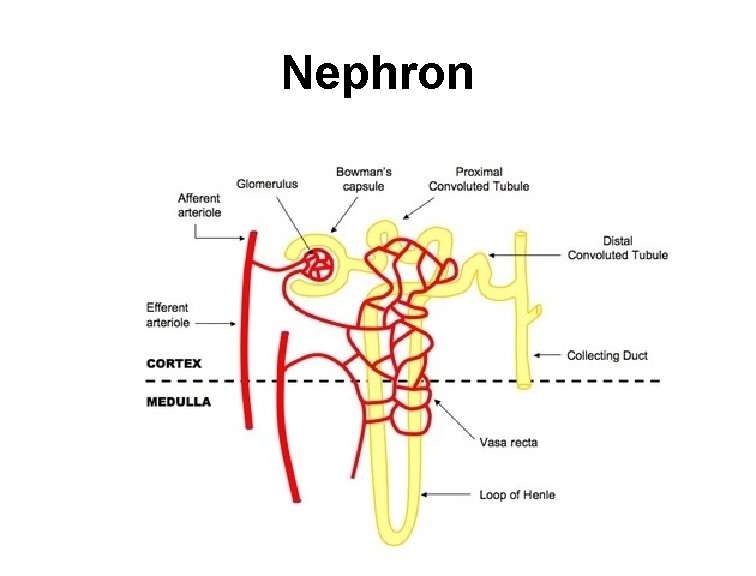
Nephron
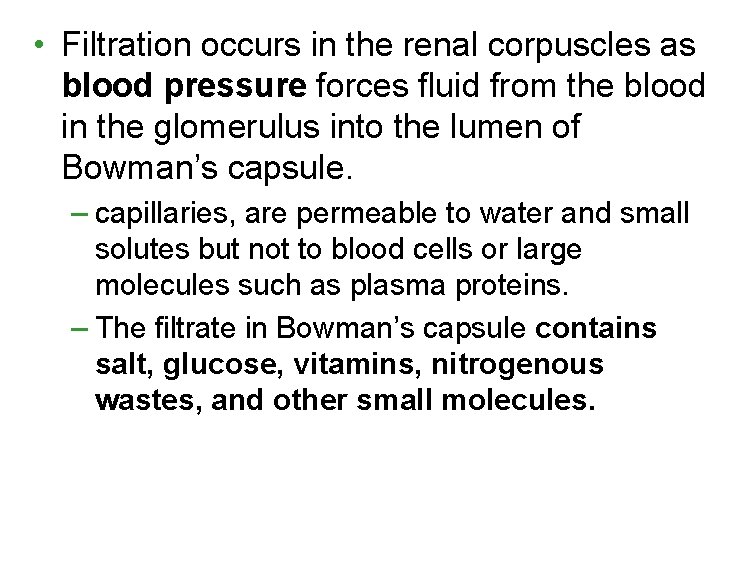
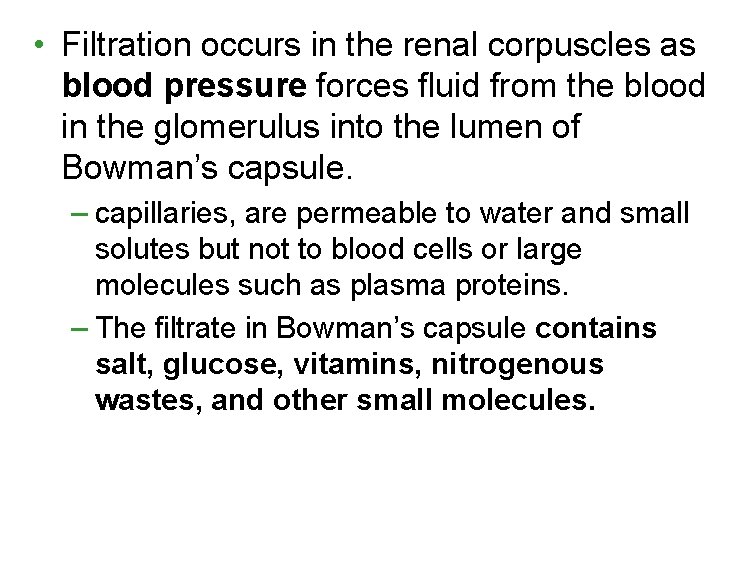
• Filtration occurs in the renal corpuscles as blood pressure forces fluid from the blood in the glomerulus into the lumen of Bowman’s capsule. – capillaries, are permeable to water and small solutes but not to blood cells or large molecules such as plasma proteins. – The filtrate in Bowman’s capsule contains salt, glucose, vitamins, nitrogenous wastes, and other small molecules.
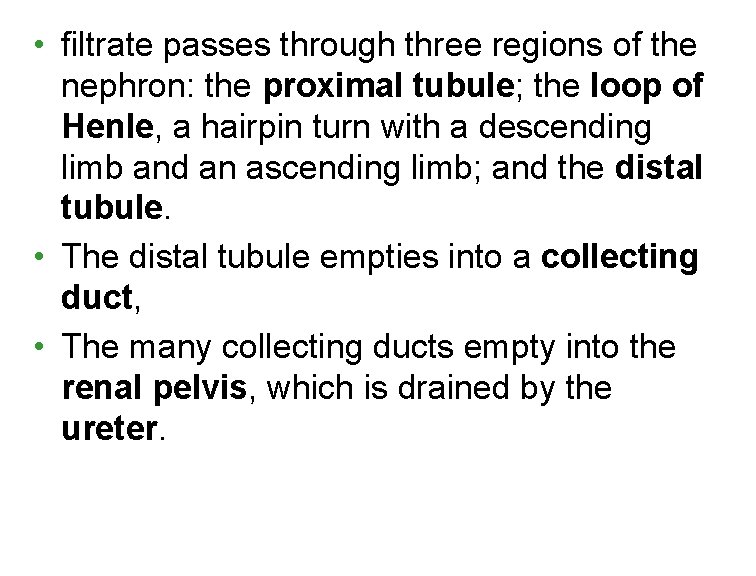
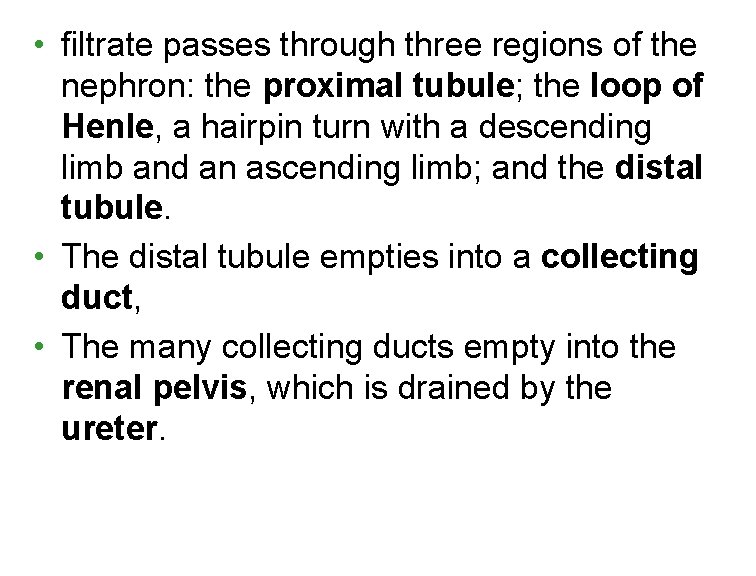
• filtrate passes through three regions of the nephron: the proximal tubule; the loop of Henle, a hairpin turn with a descending limb and an ascending limb; and the distal tubule. • The distal tubule empties into a collecting duct, • The many collecting ducts empty into the renal pelvis, which is drained by the ureter.
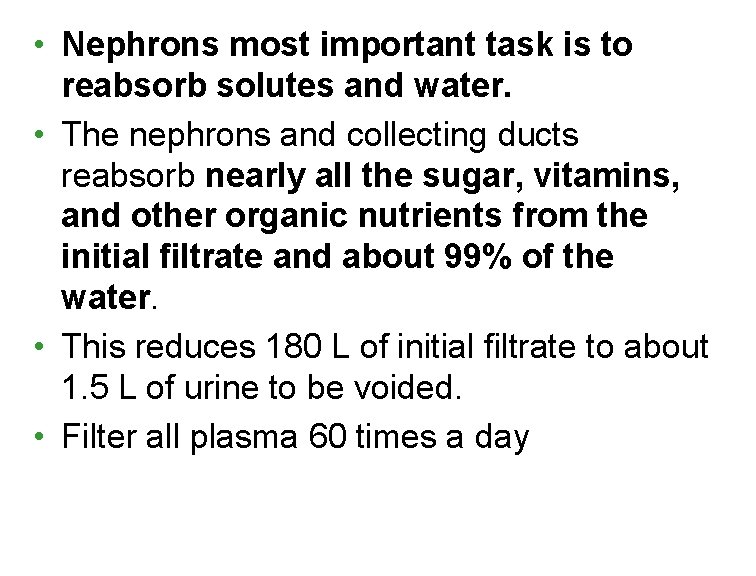
• Nephrons most important task is to reabsorb solutes and water. • The nephrons and collecting ducts reabsorb nearly all the sugar, vitamins, and other organic nutrients from the initial filtrate and about 99% of the water. • This reduces 180 L of initial filtrate to about 1. 5 L of urine to be voided. • Filter all plasma 60 times a day
Micturition • Or Voiding – the act of emptying the bladder.
Physical Characteristics of Urine • Color and transparency – Clear, pale to deep yellow (due to urochrome) – Drugs, vitamin supplements, and diet can alter the color – Cloudy urine may indicate a urinary tract infection
Physical Characteristics of Urine • Odor – Slightly aromatic when fresh – Develops ammonia odor upon standing – May be altered by some drugs and vegetables
Physical Characteristics of Urine • p. H – Slightly acidic (~p. H 6, with a range of 4. 5 to 8. 0) – Diet, prolonged vomiting, or urinary tract infections may alter p. H • Specific gravity – 1. 001 to 1. 035, dependent on solute concentration
Chemical Composition of Urine • 95% water and 5% solutes • Nitrogenous wastes: urea, uric acid, and creatinine • Other normal solutes – Na+, K+, PO 43–, and SO 42–, – Ca 2+, Mg 2+ and HCO 3– • Abnormally high concentrations of any constituent may indicate pathology
Substances not normally found in urine • • • Glucose Blood proteins Red blood cells White blood cells (pus) Bile