Urinary System Exercises 40 and 41 Organs of
- Slides: 44
Urinary System Exercises 40 and 41
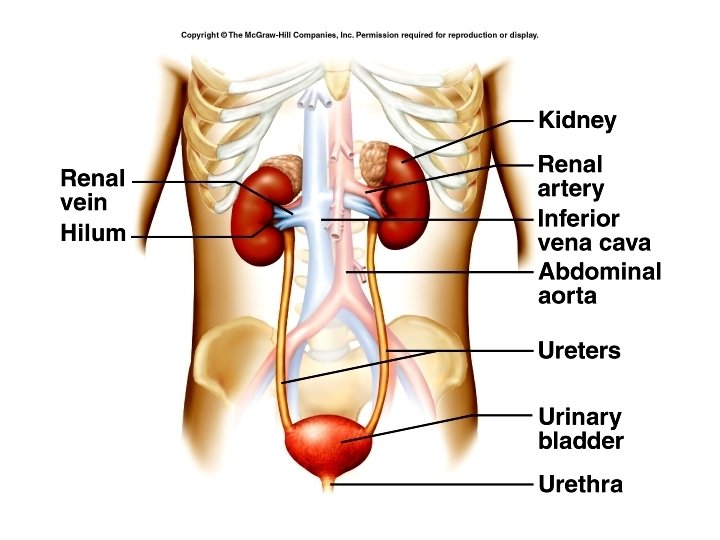
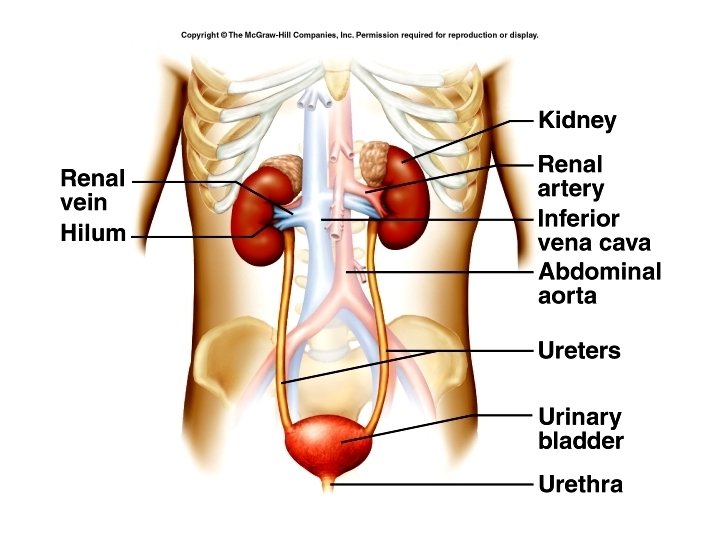
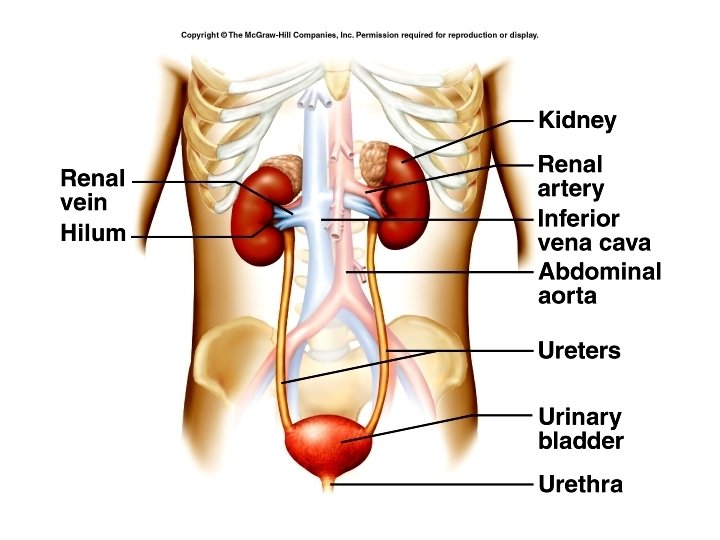
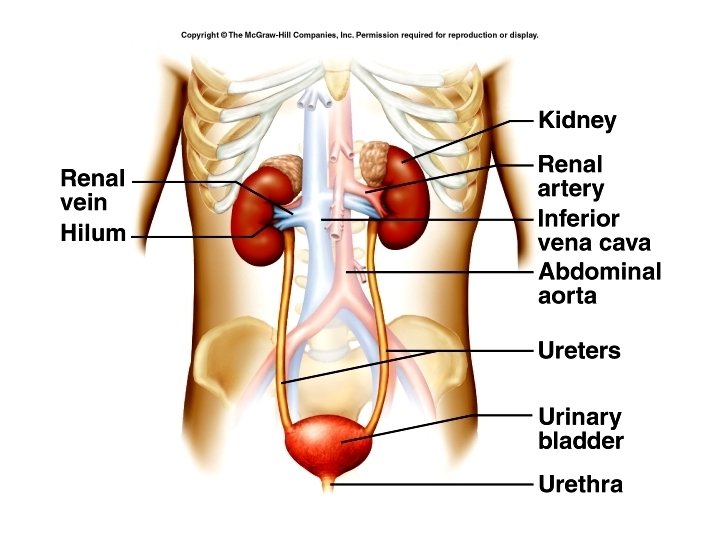
Organs of the Urinary System • • • 2 kidneys Urinary bladder 2 ureters Urethra Primary function is to filter blood, and reabsorb water and needed substances back into blood. Remaining water and wastes are removed in urine.
• • Regulate blood volume and composition Regulate blood p. H Regulate blood pressure Contribute to metabolism – Calcitriol – Erythropoietin – Gluconeogenesis
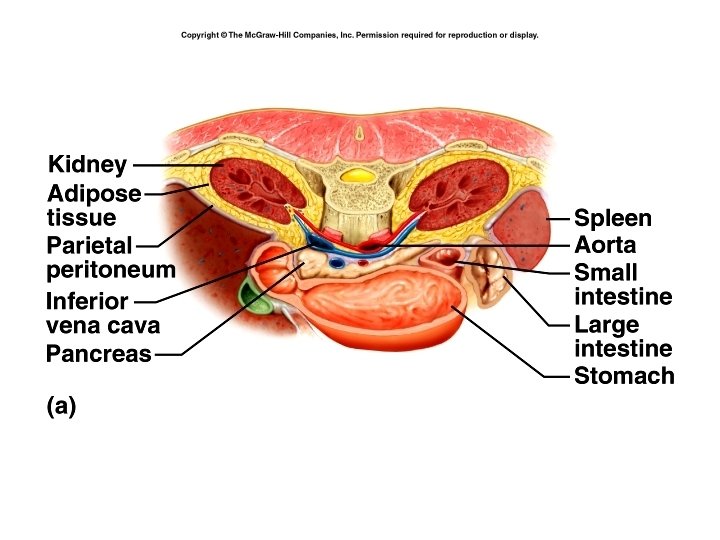
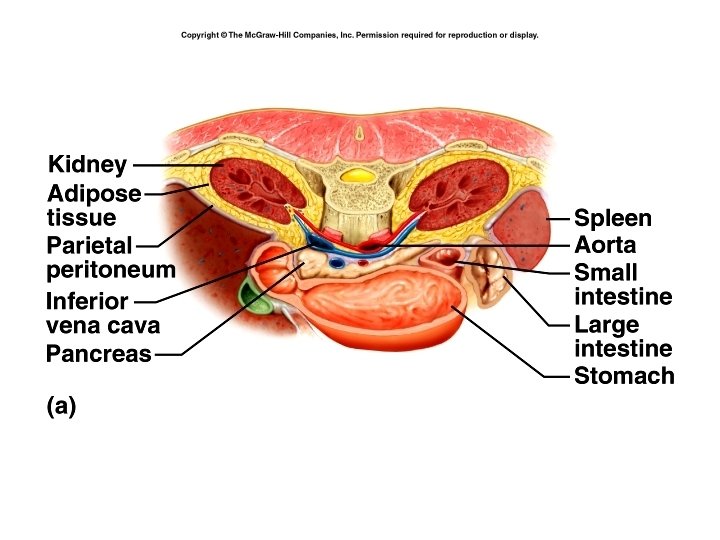
Location of kidneys • • • Between T 12 and L 3 Partially protected by 11 th and 12 th ribs Right kidney is lower than left Kidneys and ureters are retroperitoneal Protected by three layers: – Renal capsule – Adipose capsule – Renal fascia
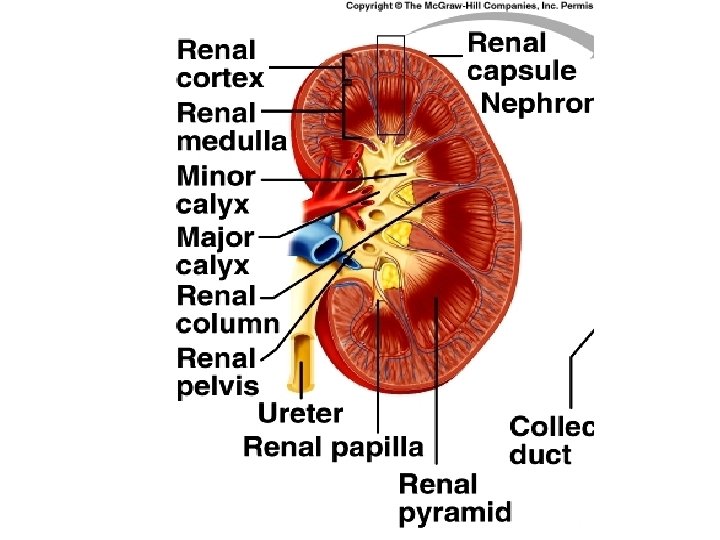
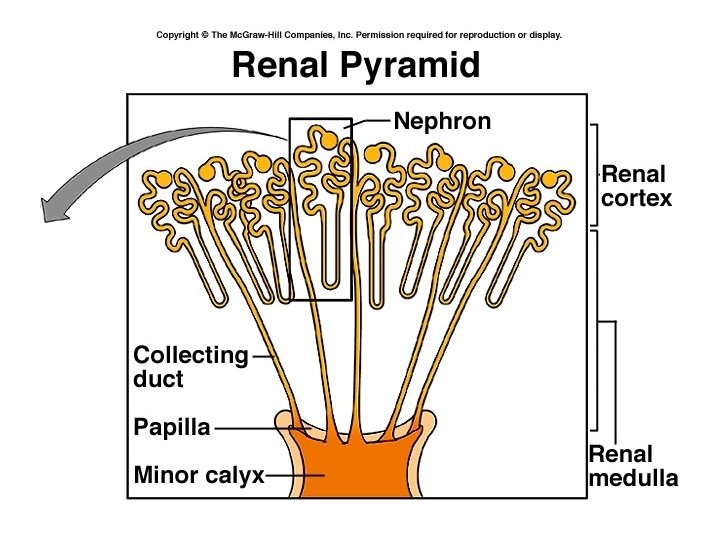
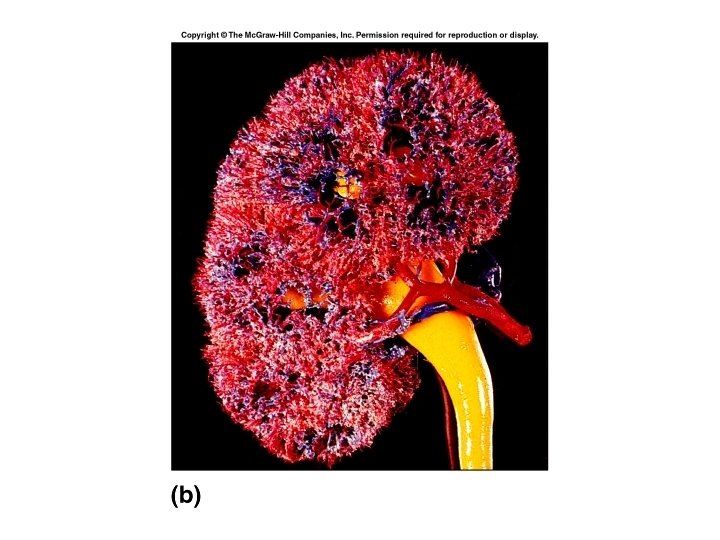
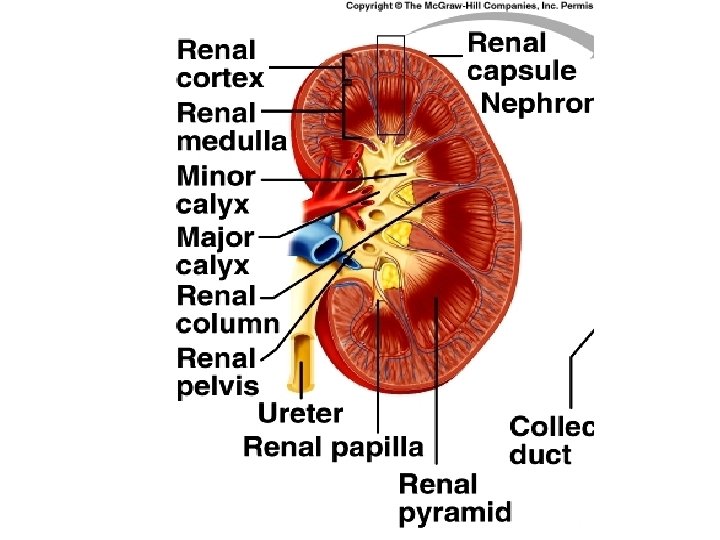
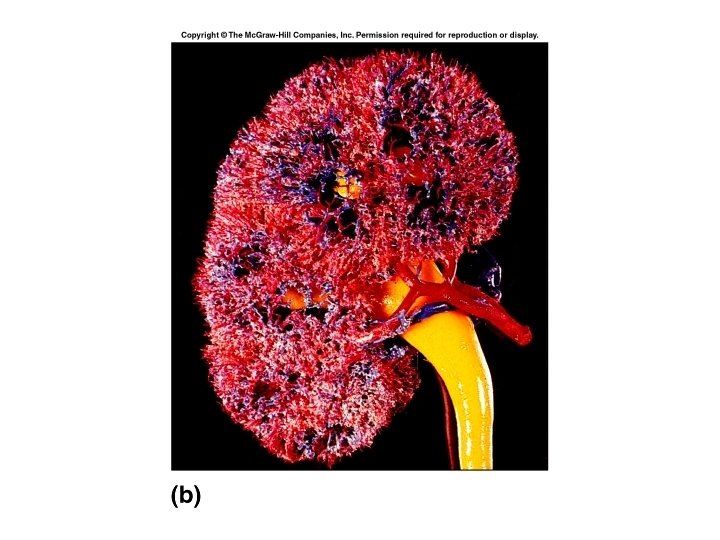
Anatomy • Renal hilum – ureter, blood and lymphatic vessels • Renal sinus • Renal cortex • Renal medulla – Renal pyramids – Renal papilla • Renal columns
Nephron • • Functional unit of kidney Number constant from birth Can function on 2/3 of one kidney Forms the urine
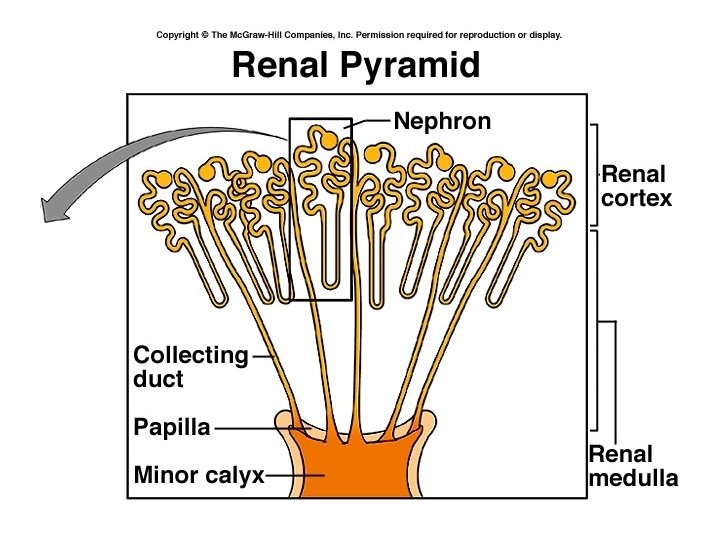
Duct system • • • Minor calyces Major calyces Renal pelvis Ureter Urine is not changed after it leaves the collecting duct
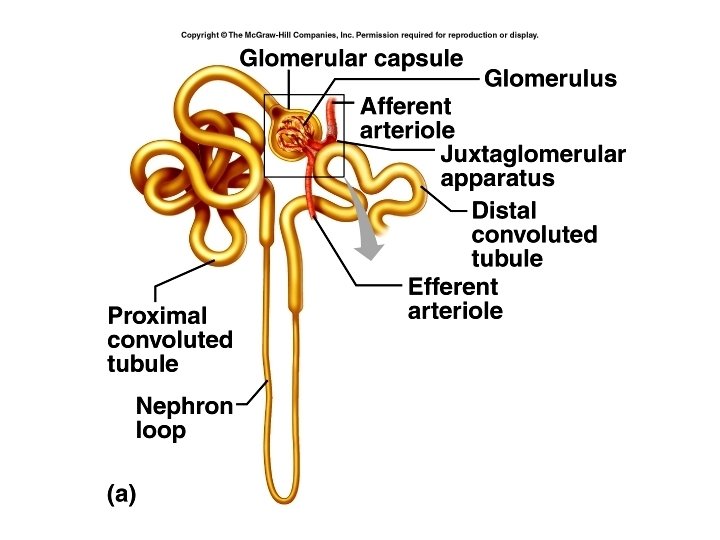
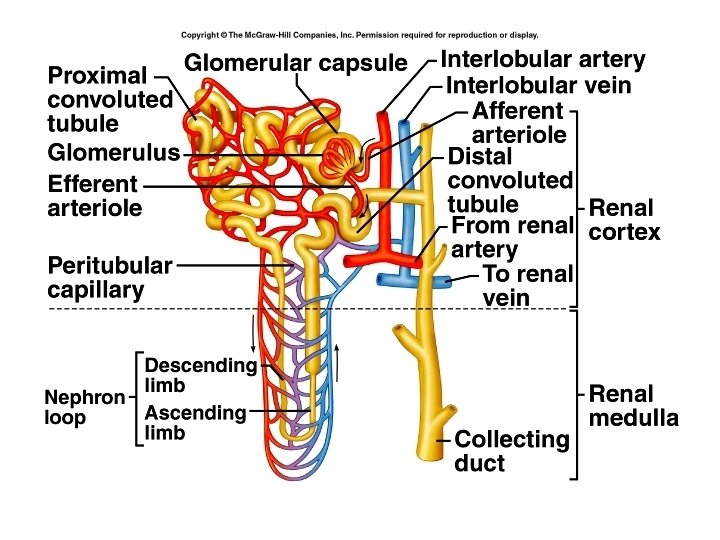
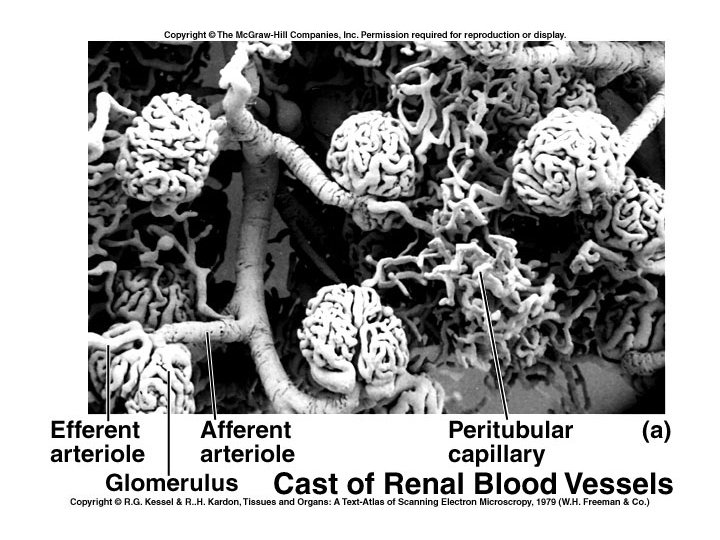
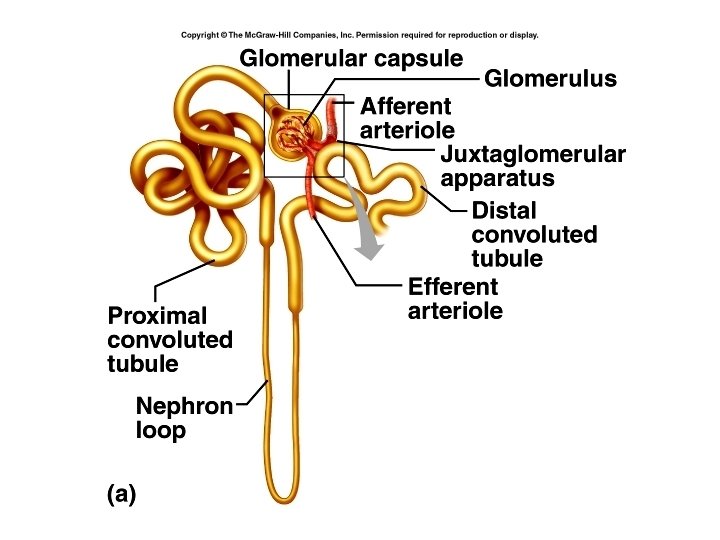
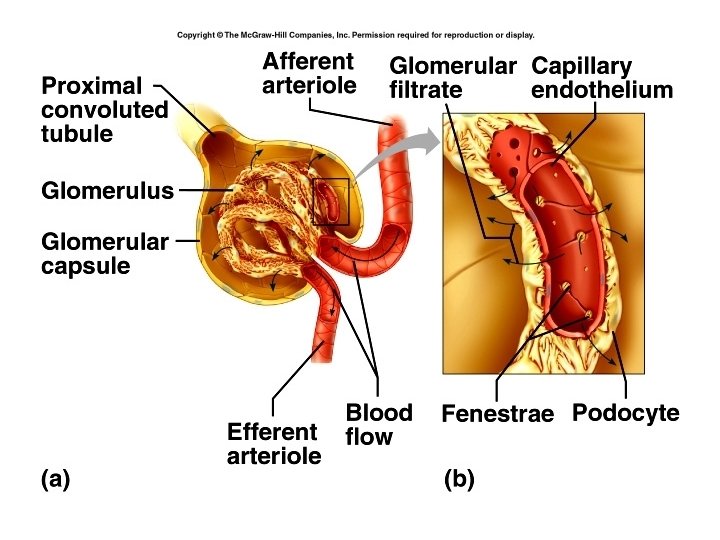
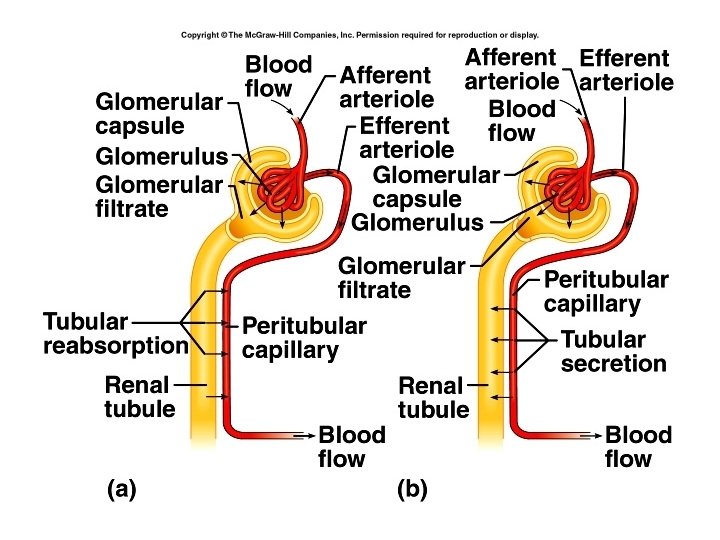
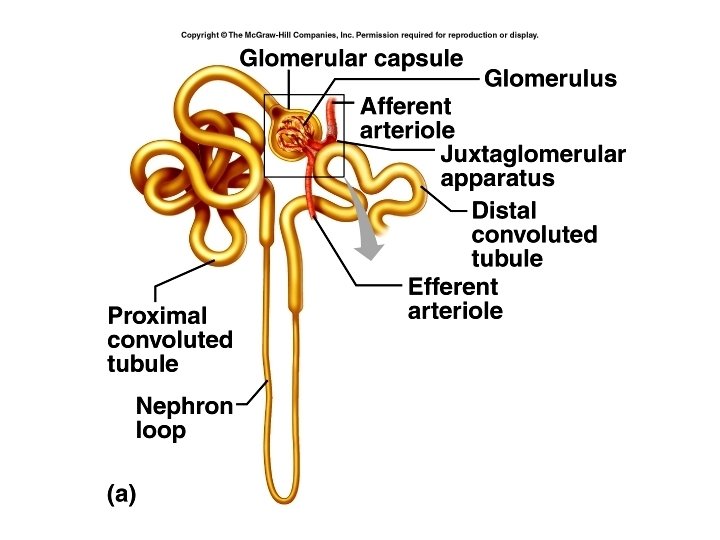
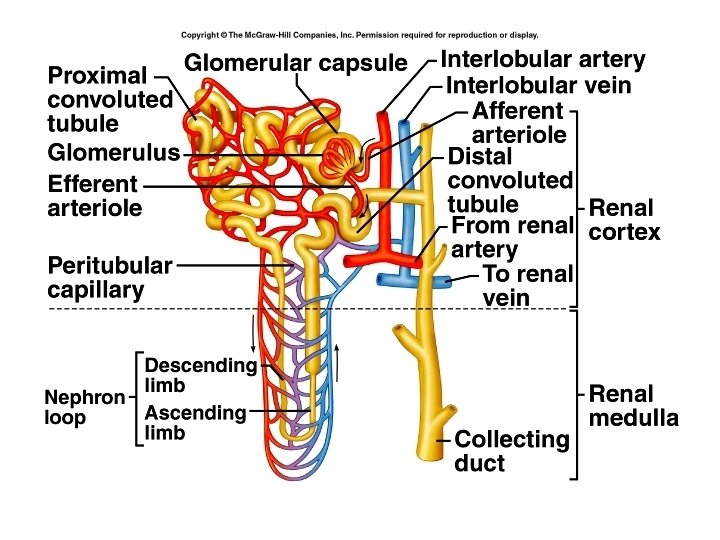
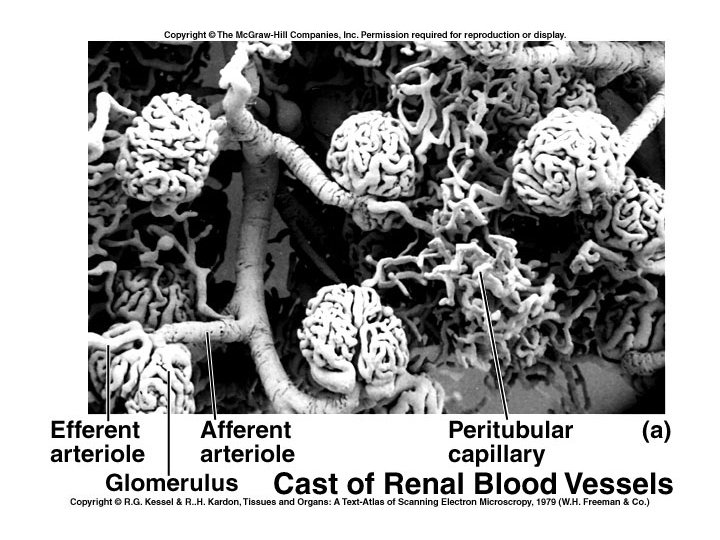
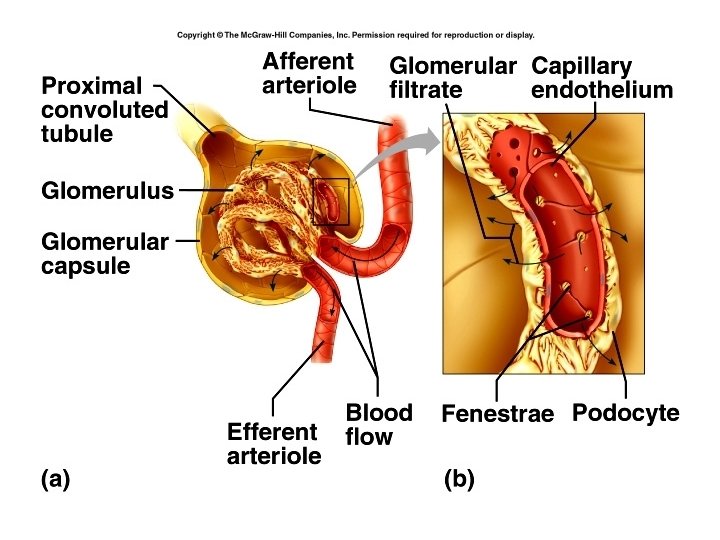
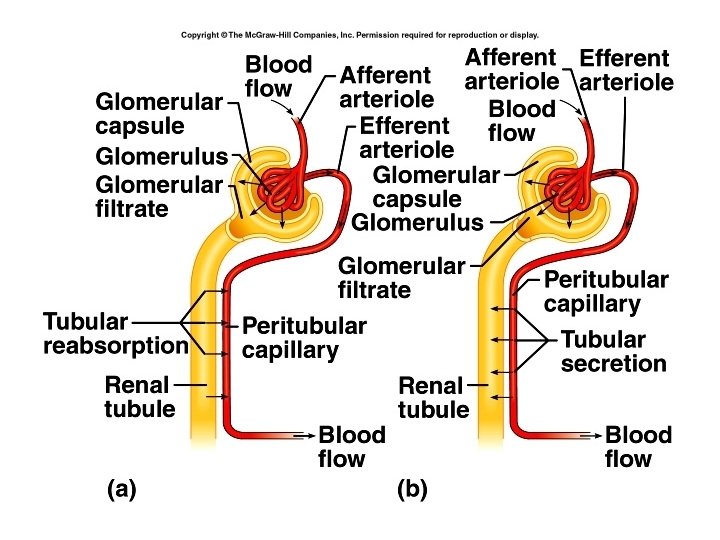
• • Kidneys = 1% of body mass Receive 15 -30 % of blood flow Blood supplied to kidney by renal artery Afferent arteriole divides into ball shaped capillary network called the glomerulus. • Capillaries rejoin to form efferent arteriole, then peritubular capillaries • Vasa recta
Functions of the Nephron • Filtration • Tubular reabsorption • Tubular secretion
Structure of a nephron • Renal corpuscle – Glomerulus – Glomerular capsule or Bowman’s capsule • Renal tubule – Proximal convoluted tubule – Nephron loop or loop of Henle – Distal convoluted tubule – Collecting duct
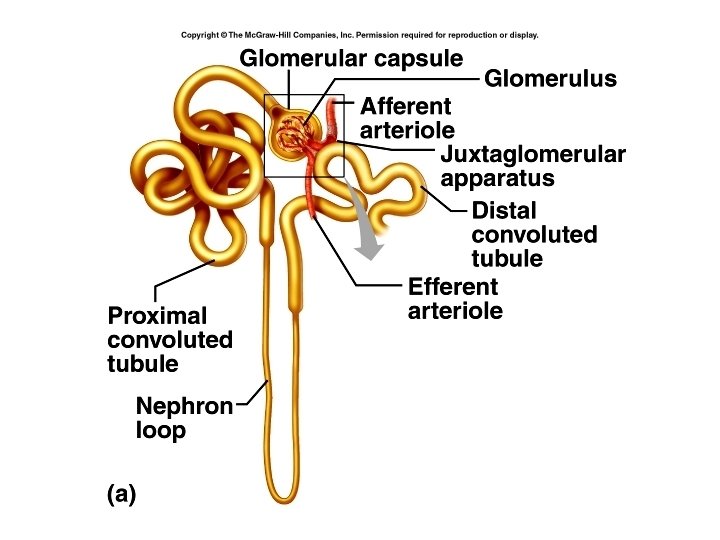
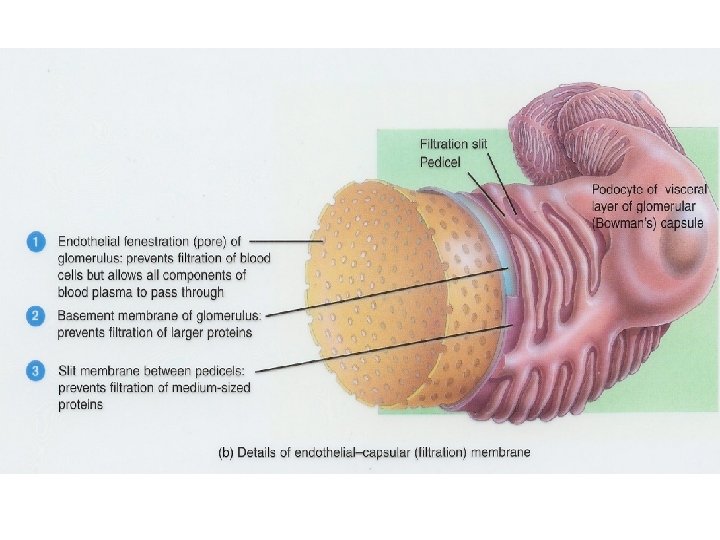
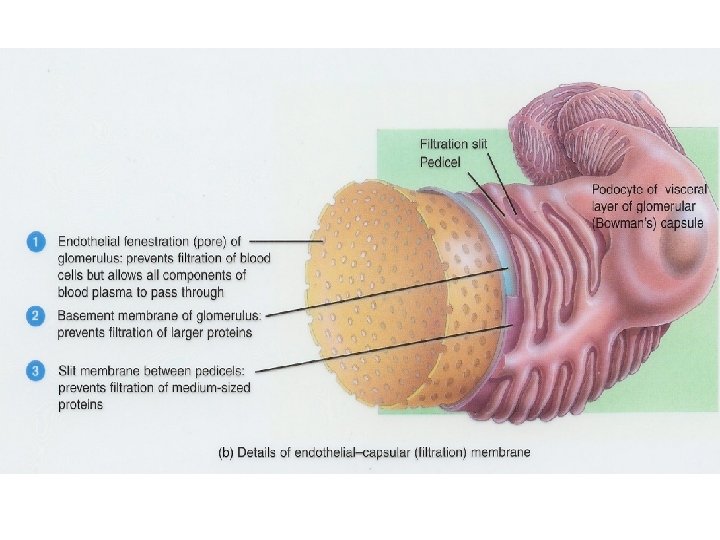
Bowman’s capsule • Outer layer - simple squamous epithelium • Inner layer – modified simple squamous epi. – Cells called podocytes – Projections are pedicels • Endothelium of capillary and podocytes form the endothelial-capsular (filtration) membrane.
Filtration membrane 1. Fenestrated endothelium – prevents the passage of cells 2. Basement membrane of glomerulus – prevents passage of large proteins 3. Slit membrane (between pedicels) – prevents the passage of medium sized proteins
• Wall of renal tubules made up of single layer of epithelial cells and a basement membrane. • Proximal convoluted tubule – cells are cuboidal and have microvilli. • About 65 % of water and 100 % of some solutes are reabsorbed here.
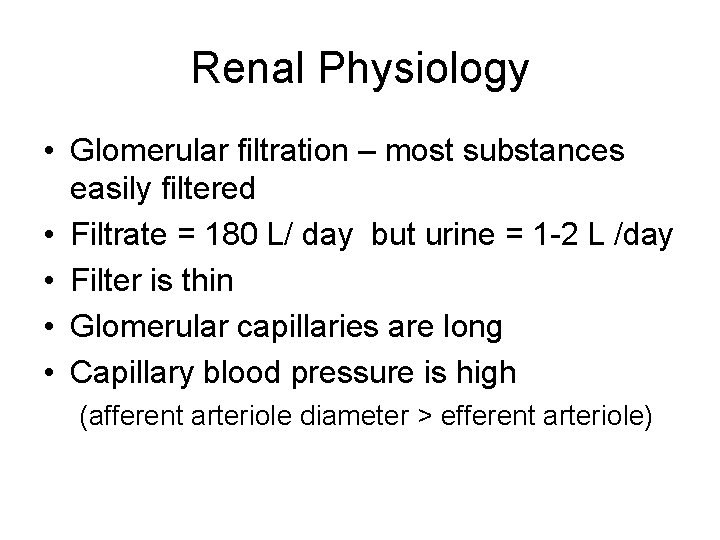
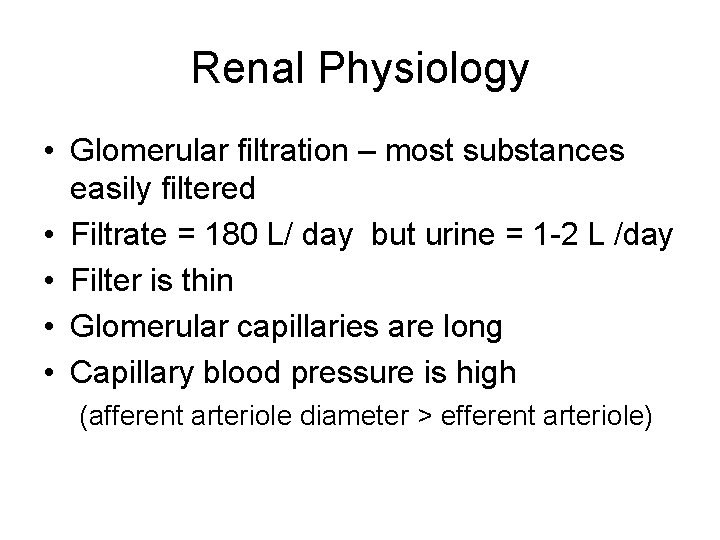
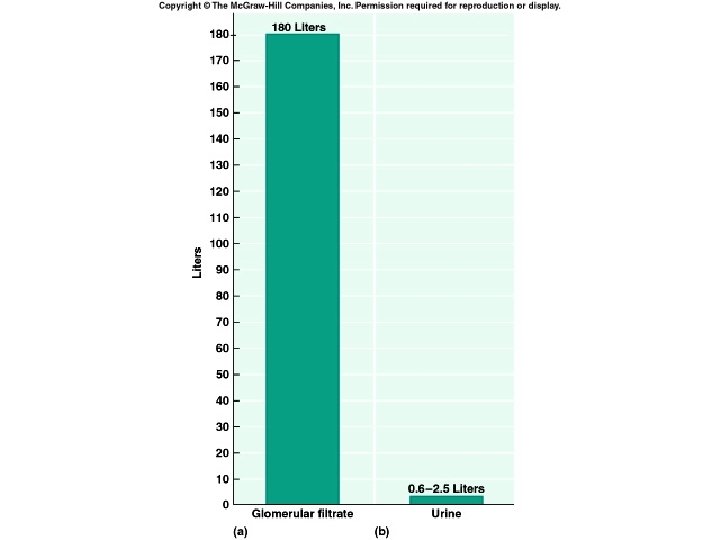
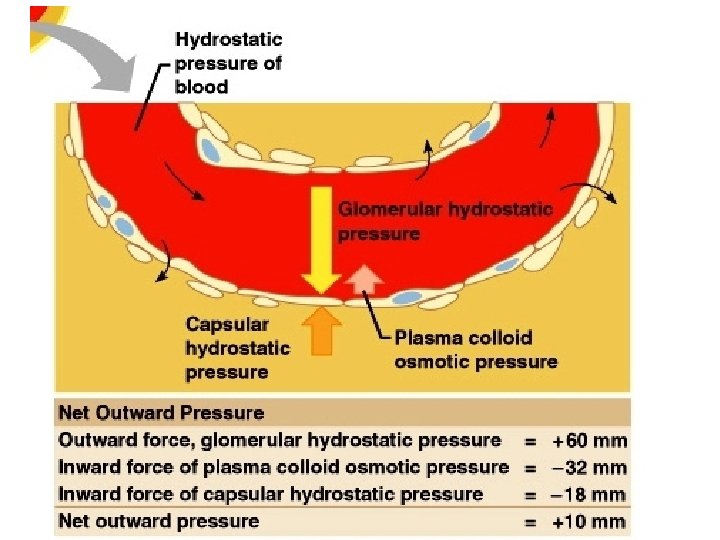
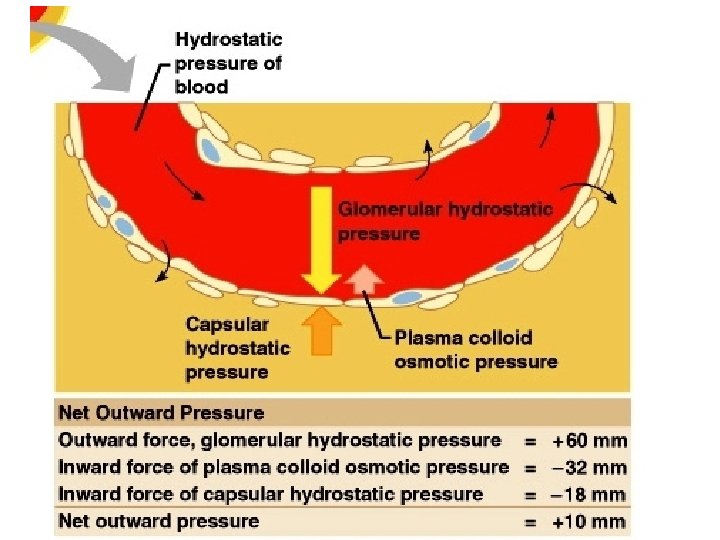
Renal Physiology • Glomerular filtration – most substances easily filtered • Filtrate = 180 L/ day but urine = 1 -2 L /day • Filter is thin • Glomerular capillaries are long • Capillary blood pressure is high (afferent arteriole diameter > efferent arteriole)
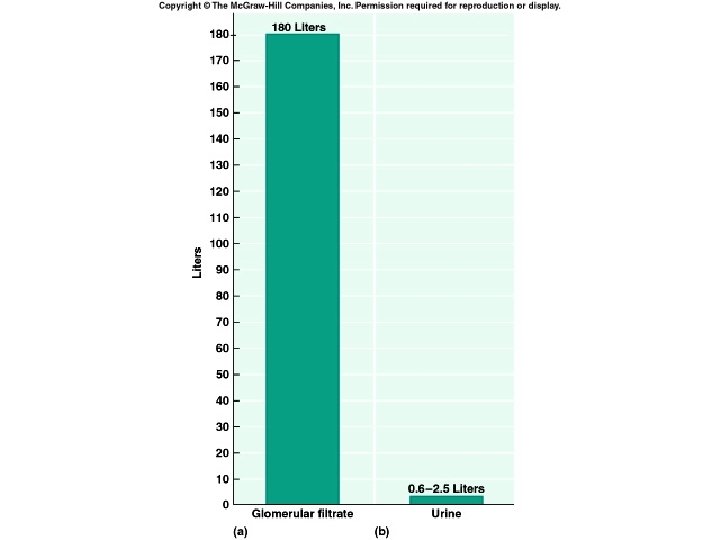
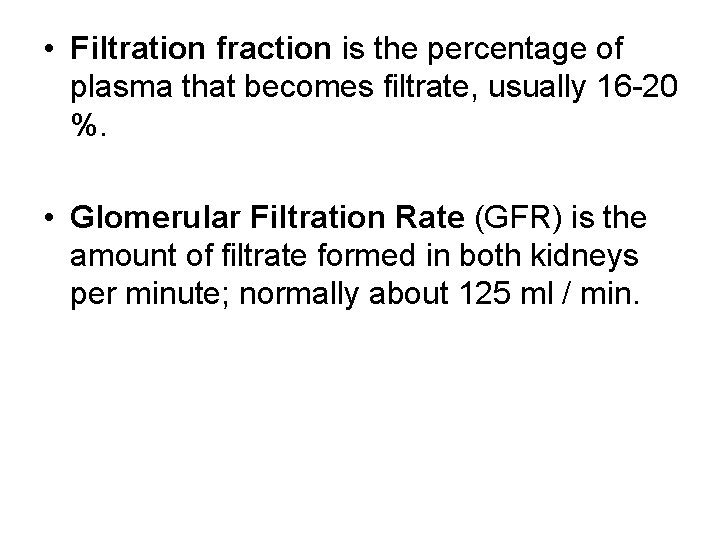
• Filtration fraction is the percentage of plasma that becomes filtrate, usually 16 -20 %. • Glomerular Filtration Rate (GFR) is the amount of filtrate formed in both kidneys per minute; normally about 125 ml / min.
Renal autoregulation • JGA senses Na+, Cl- and water • When these ↓, JGA dilates afferent arteriole, ↑ blood pressure in glomerulus
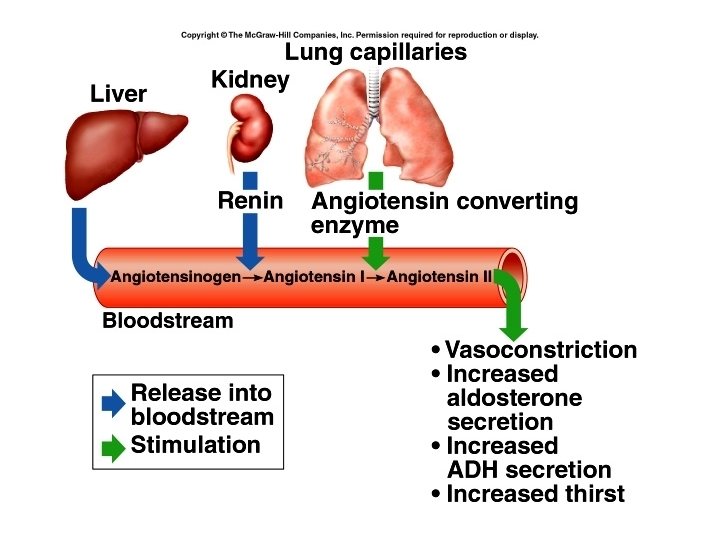
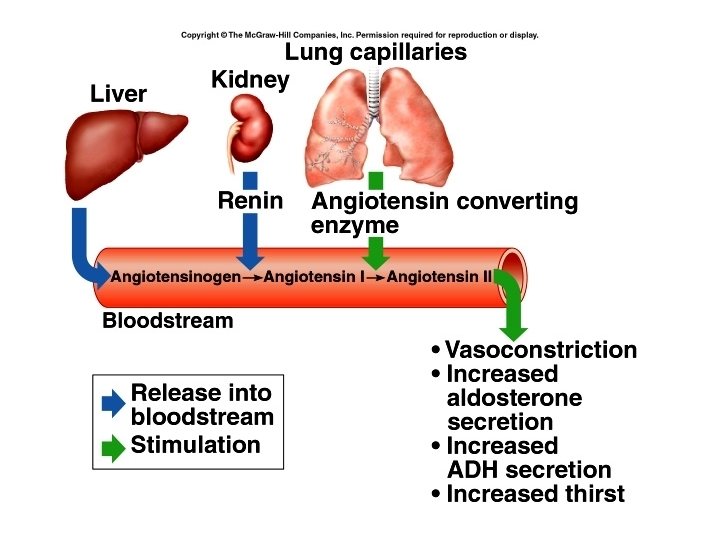
Hormonal regulation • When BP ↓, JGA secretes renin which converts angiotensinogen to angiotensin I, angiotensin I is converted to angiotensin II in the lungs. Angiotensin II is a potent vasoconstrictor. It also stimulates the release of aldosterone, and stimulates the thirst center in the hypothalamus and release of ADH from the posterior pituitary gland.
Tubular reabsorption • Volume of fluid that enters the proximal convoluted tubule in ½ an hour > total plasma volume. • Reabsorb water, glucose, amino acids, urea and ions, esp. Na+, Cl- and K+ • Na+ diffuses into cells, but is actively pumped out into interstitial fluid • Promotes reabsorption of water
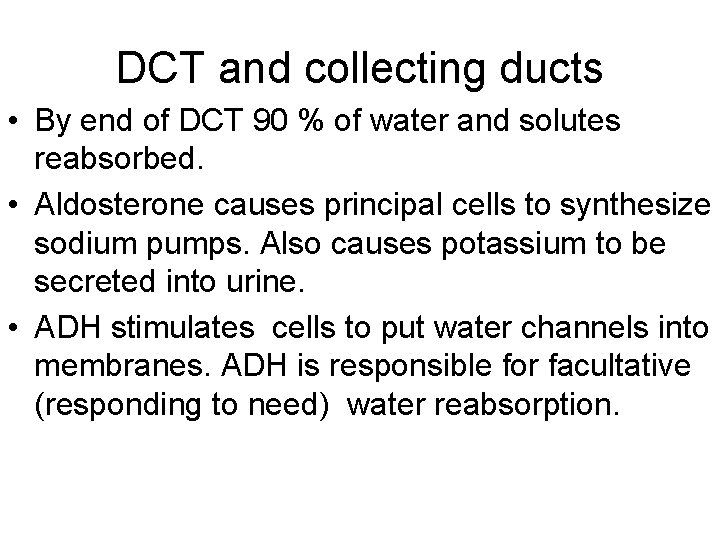
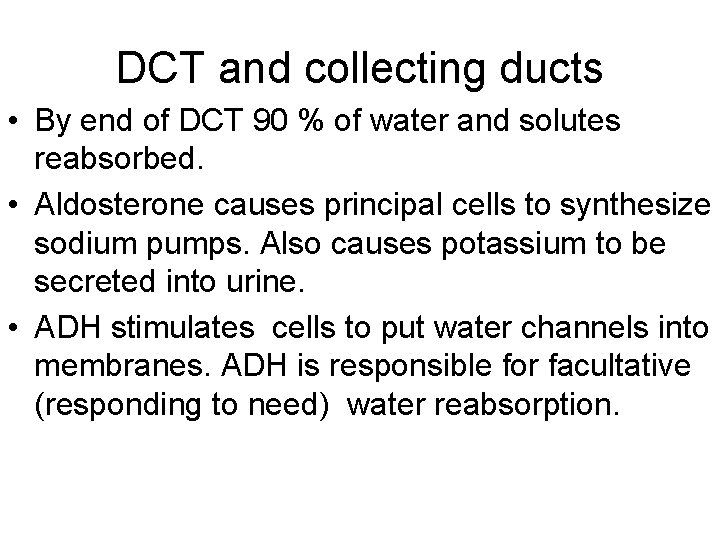
DCT and collecting ducts • By end of DCT 90 % of water and solutes reabsorbed. • Aldosterone causes principal cells to synthesize sodium pumps. Also causes potassium to be secreted into urine. • ADH stimulates cells to put water channels into membranes. ADH is responsible for facultative (responding to need) water reabsorption.
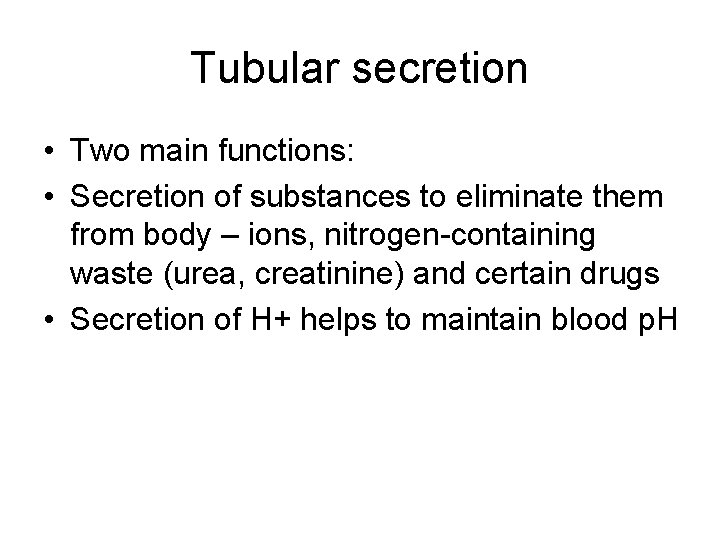
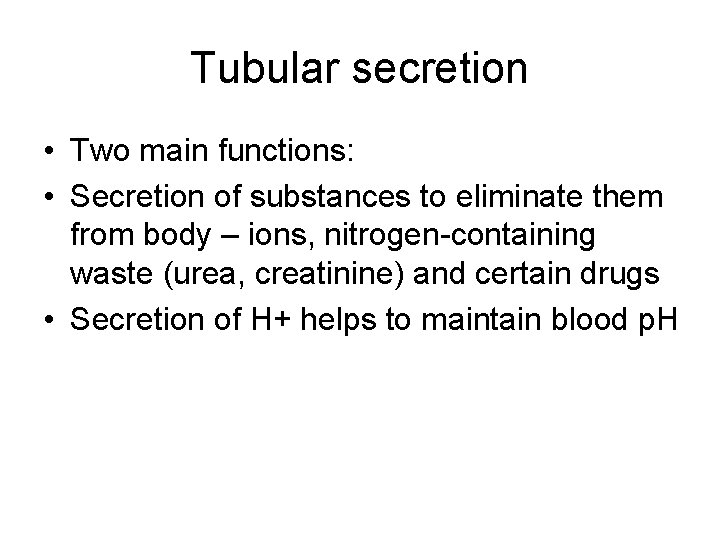
Tubular secretion • Two main functions: • Secretion of substances to eliminate them from body – ions, nitrogen-containing waste (urea, creatinine) and certain drugs • Secretion of H+ helps to maintain blood p. H
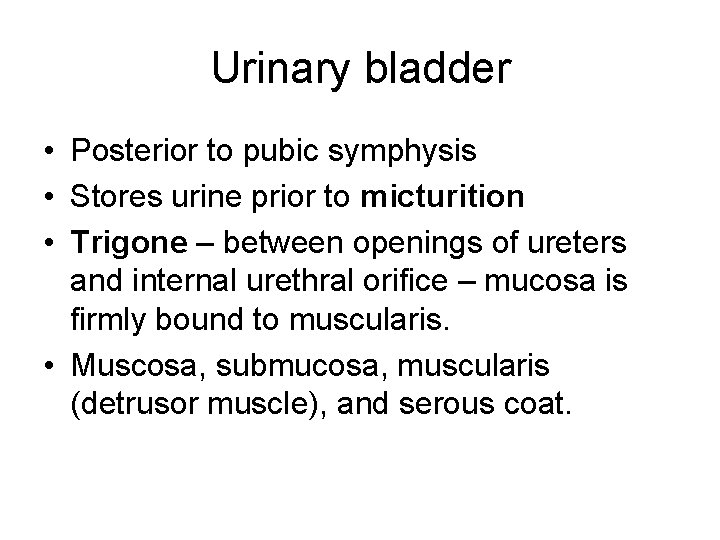
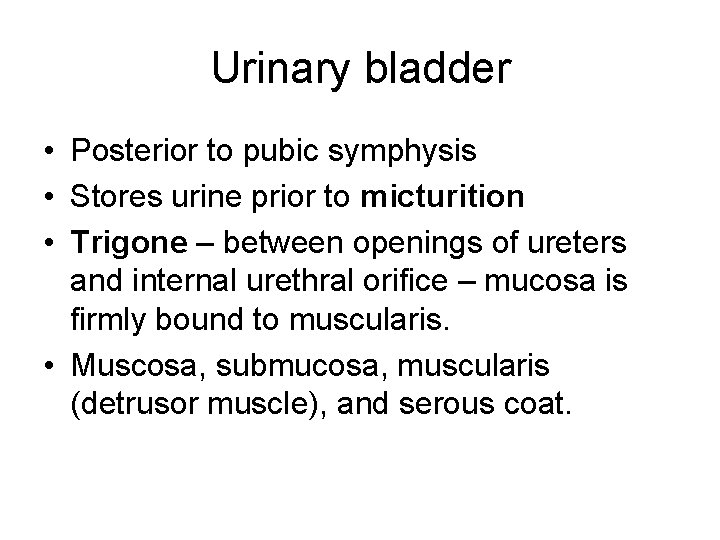
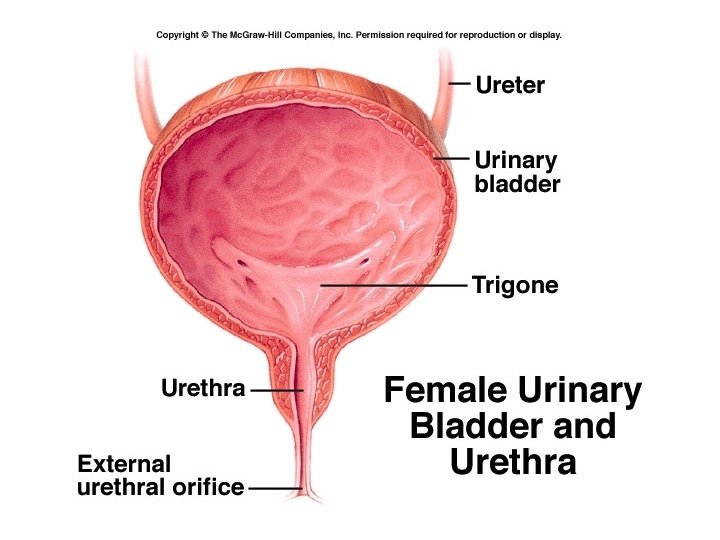
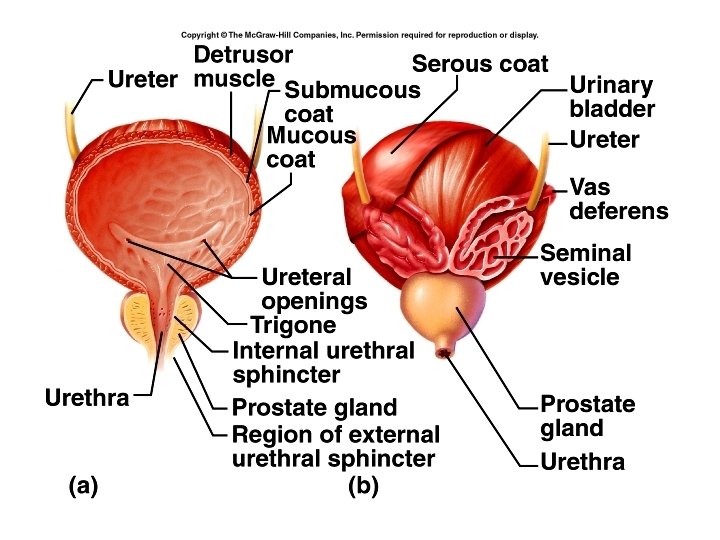
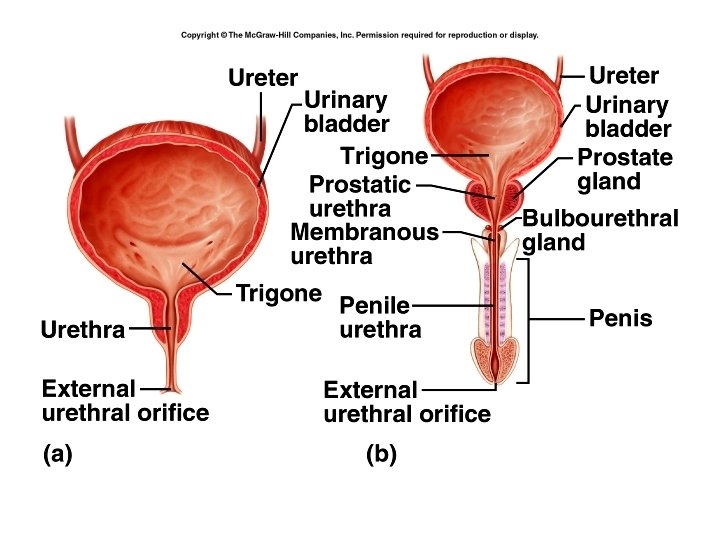
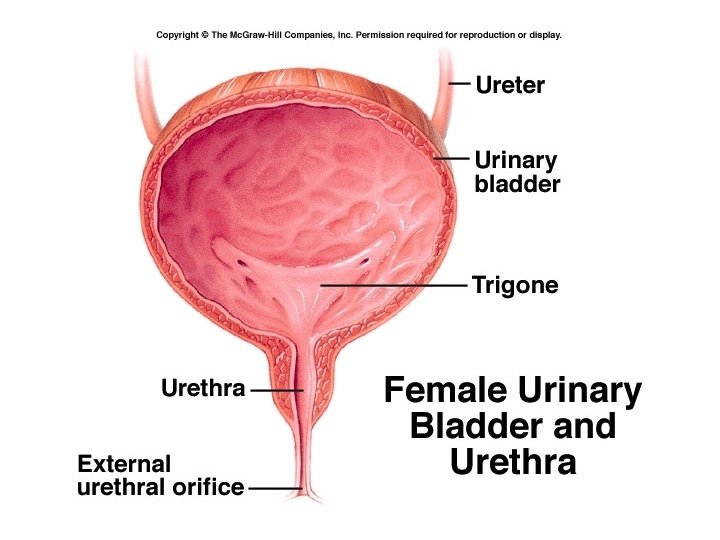
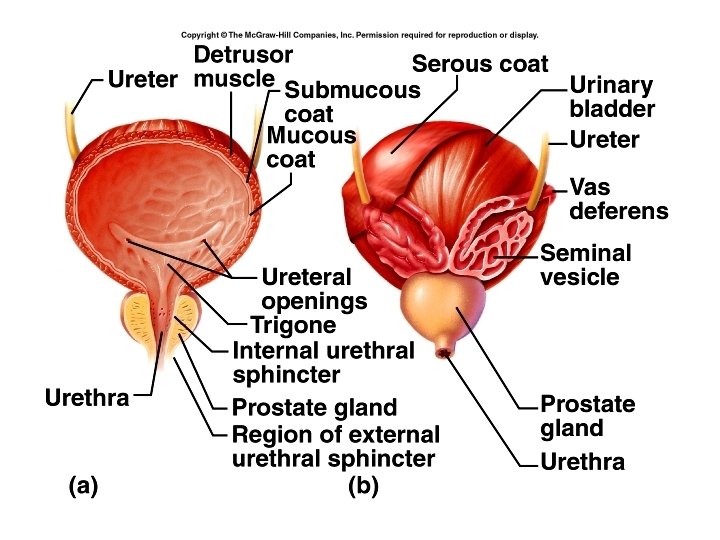
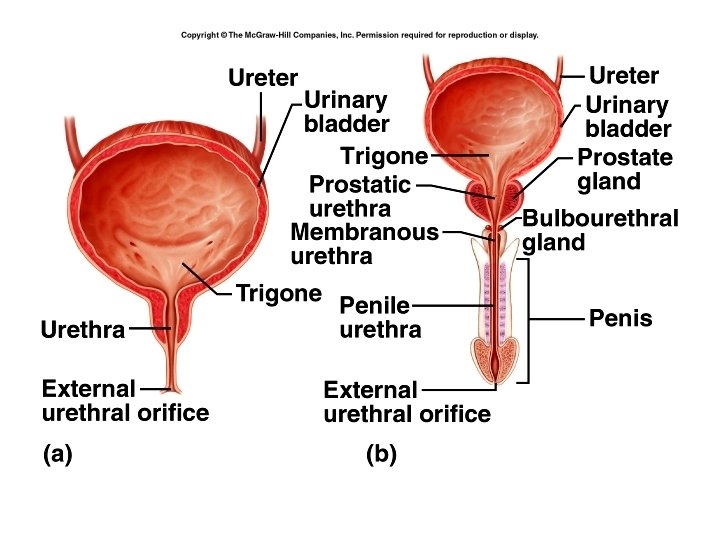
Urinary bladder • Posterior to pubic symphysis • Stores urine prior to micturition • Trigone – between openings of ureters and internal urethral orifice – mucosa is firmly bound to muscularis. • Muscosa, submucosa, muscularis (detrusor muscle), and serous coat.
Evaluation of kidney function • Blood Urea Nitrogen (BUN) – urea is a breakdown product of proteins – Influenced by diet • Creatinine – end product of muscle metabolism – Normally constant – Can determine creatinine clearance
Normal urine • Transparent yellow • Contains ions : Na+, Cl-, K+ ; nitrogenous wastes: ammonia, creatinine, urea and uric acid; and foreign chemicals: drugs, pesticides, food additives, etc. • Suspended solids in trace amounts: bacteria, blood cells, casts.
Not normally present • Albumin • Glucose, Acetone– diabetes mellitus • Bile – liver disease, obstruction of bile ducts, hemolytic disease • p. H 4. 6 -8. 0
Specific gravity • 1. 001 -1. 035 • Damage to tubules , s. g. fixed at 1. 010 = filtrate • Diabetes insipidus (lack of ADH) – 1. 003 • Diabetes mellitus – “sugar diabetes” – 1. 030 osmotic diuresis • Emesis or fever – – 1. 040