Urinary system Aids homeostasis by removing cellular wastes
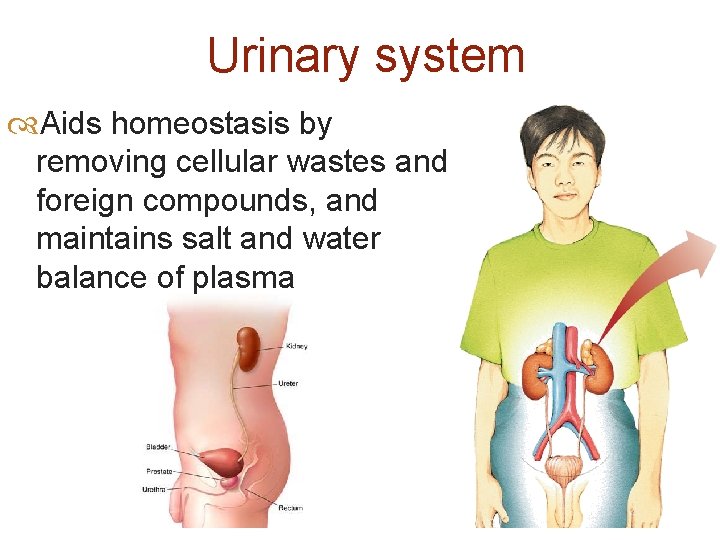
Urinary system Aids homeostasis by removing cellular wastes and foreign compounds, and maintains salt and water balance of plasma
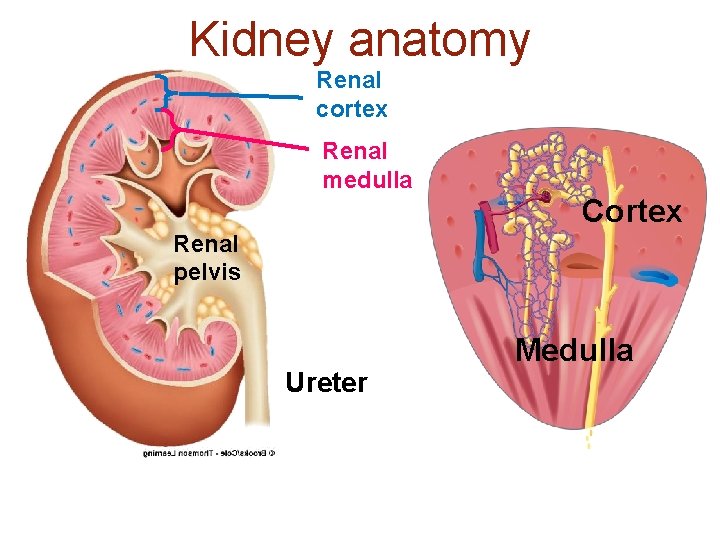
Kidney anatomy Renal cortex Renal medulla Cortex Renal pelvis Ureter Medulla
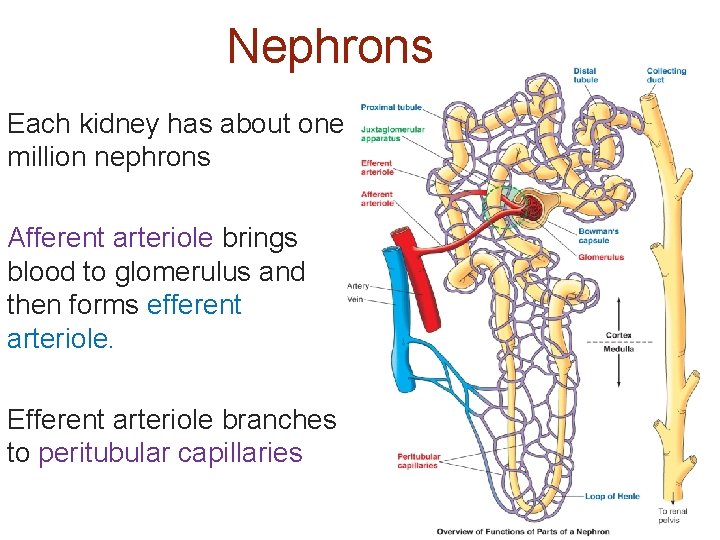
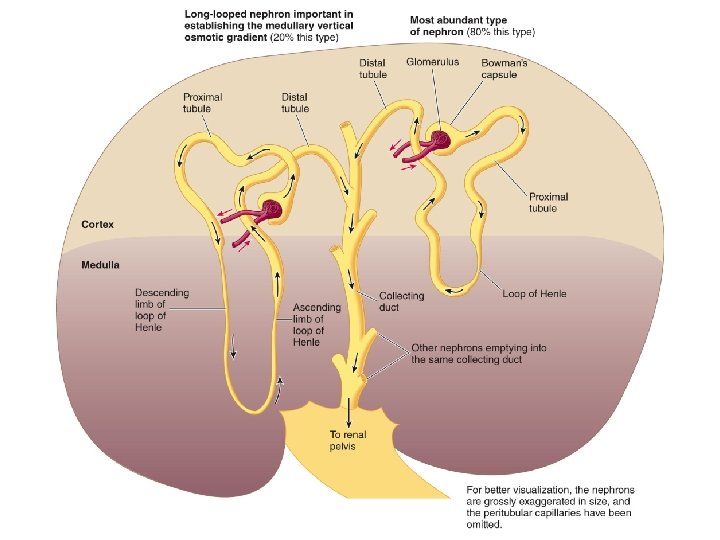
Nephrons Each kidney has about one million nephrons Afferent arteriole brings blood to glomerulus and then forms efferent arteriole. Efferent arteriole branches to peritubular capillaries
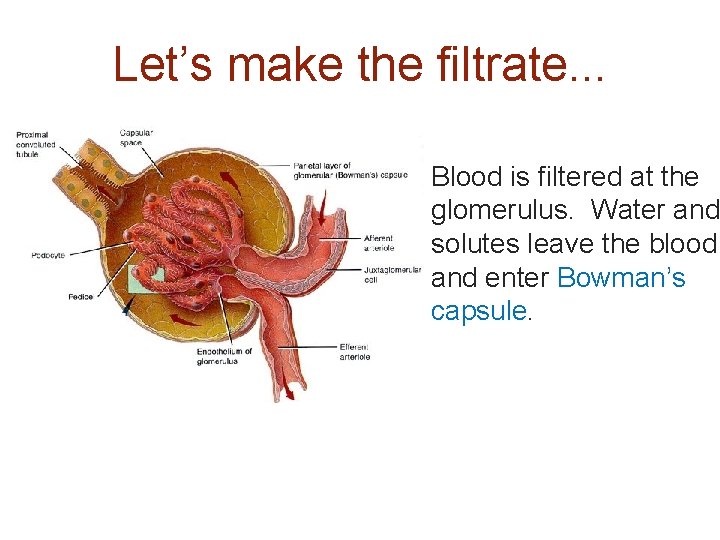
Let’s make the filtrate. . . Blood is filtered at the glomerulus. Water and solutes leave the blood and enter Bowman’s capsule.
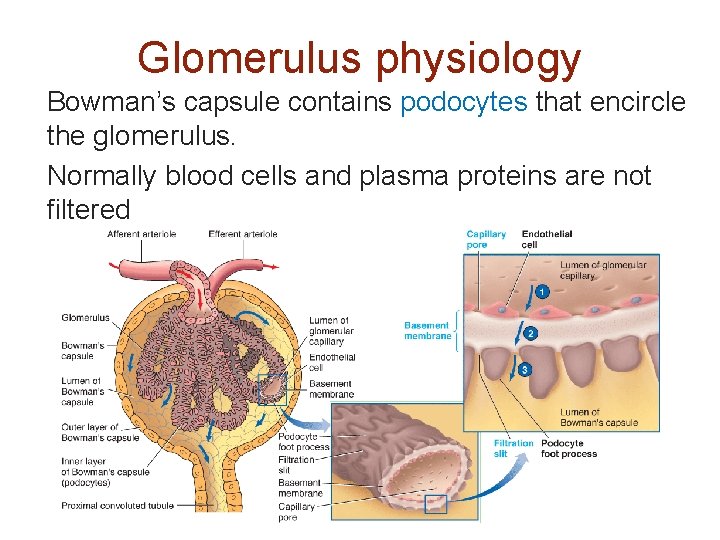
Glomerulus physiology Bowman’s capsule contains podocytes that encircle the glomerulus. Normally blood cells and plasma proteins are not filtered
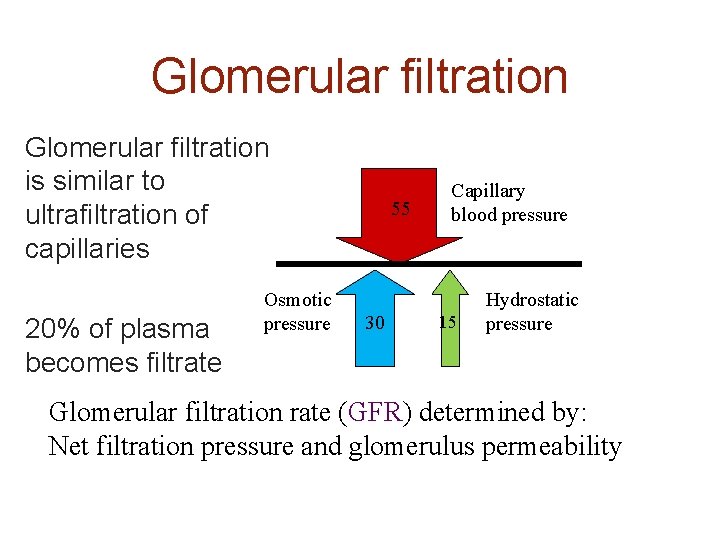
Glomerular filtration is similar to ultrafiltration of capillaries 20% of plasma becomes filtrate Osmotic pressure 55 30 Capillary blood pressure 15 Hydrostatic pressure Glomerular filtration rate (GFR) determined by: Net filtration pressure and glomerulus permeability
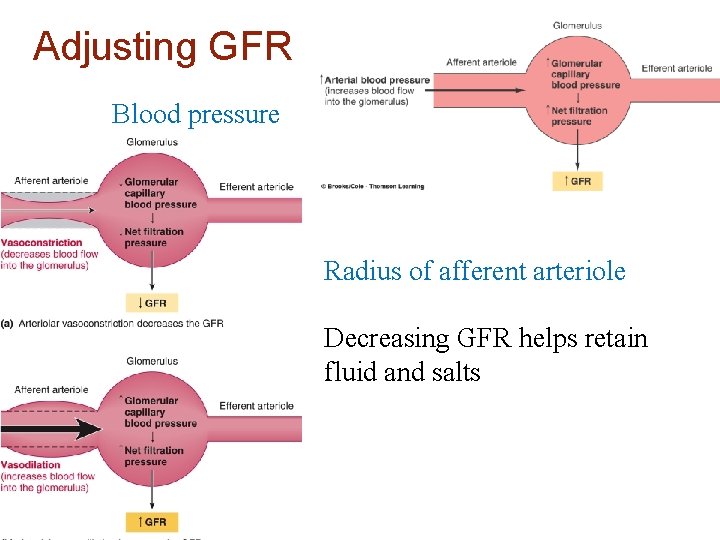
Adjusting GFR Blood pressure Radius of afferent arteriole Decreasing GFR helps retain fluid and salts
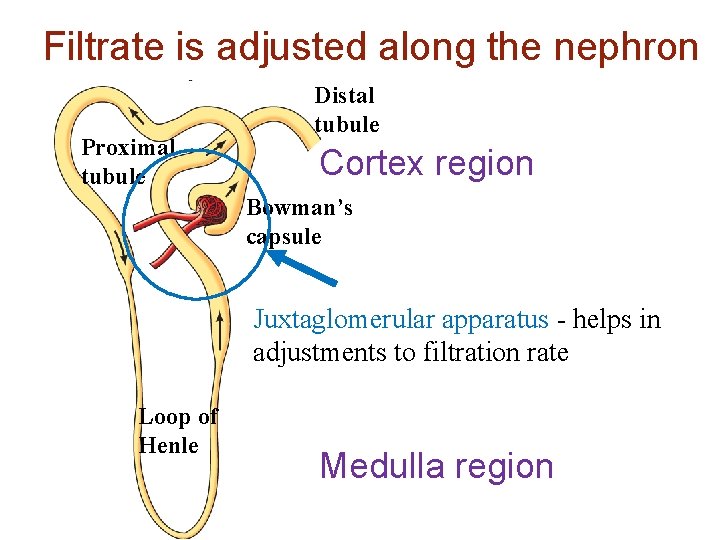
Filtrate is adjusted along the nephron Proximal tubule Distal tubule Cortex region Bowman’s capsule Juxtaglomerular apparatus - helps in adjustments to filtration rate Loop of Henle Medulla region
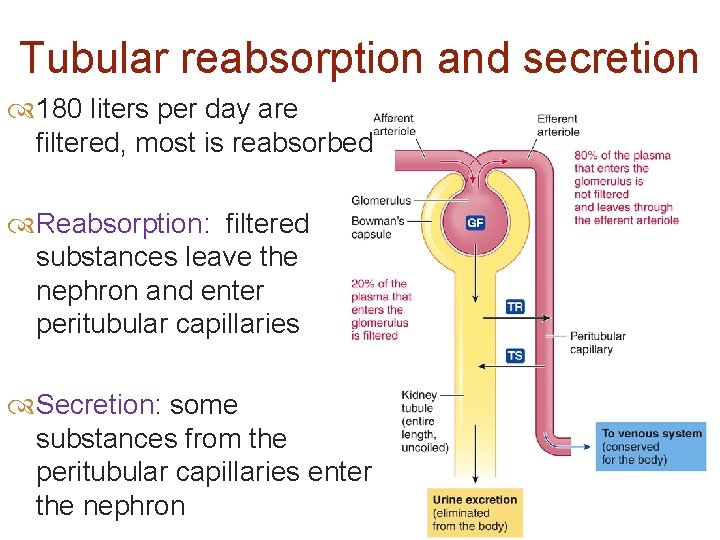
Tubular reabsorption and secretion 180 liters per day are filtered, most is reabsorbed Reabsorption: filtered substances leave the nephron and enter peritubular capillaries Secretion: some substances from the peritubular capillaries enter the nephron
So what is urine, then? Everything in the nephron that does not get reabsorbed into the blood leaves as …. urine!!!
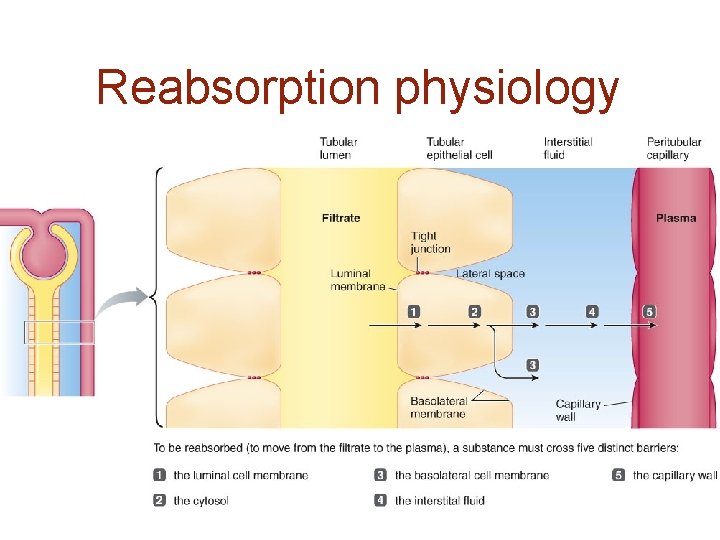
Reabsorption physiology
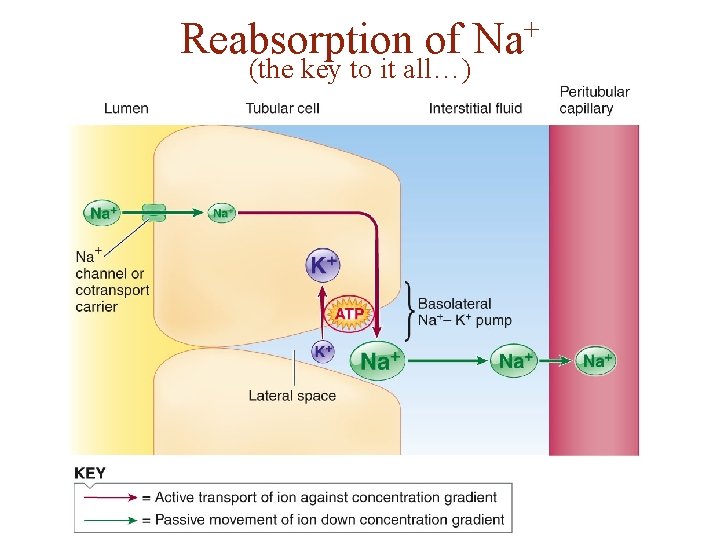
Reabsorption of (the key to it all…) + Na
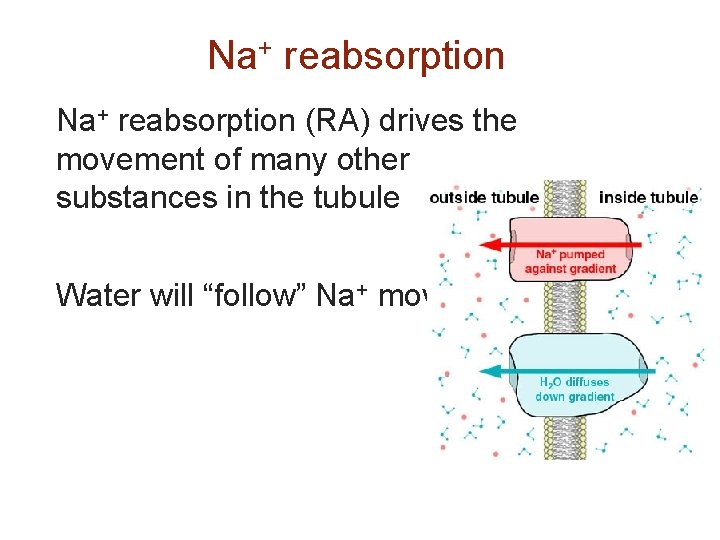
Na+ reabsorption (RA) drives the movement of many other substances in the tubule Water will “follow” Na+ movement
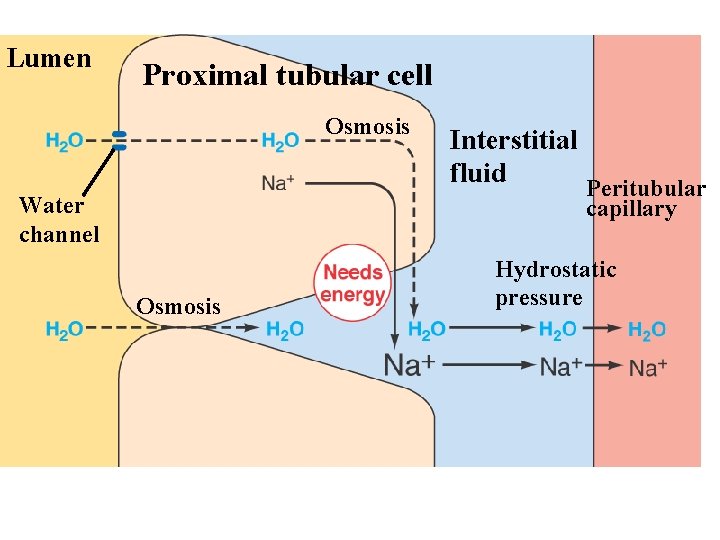
Lumen Page 533 Proximal tubular cell Osmosis Water channel Interstitial fluid Peritubular capillary Osmosis Hydrostatic pressure
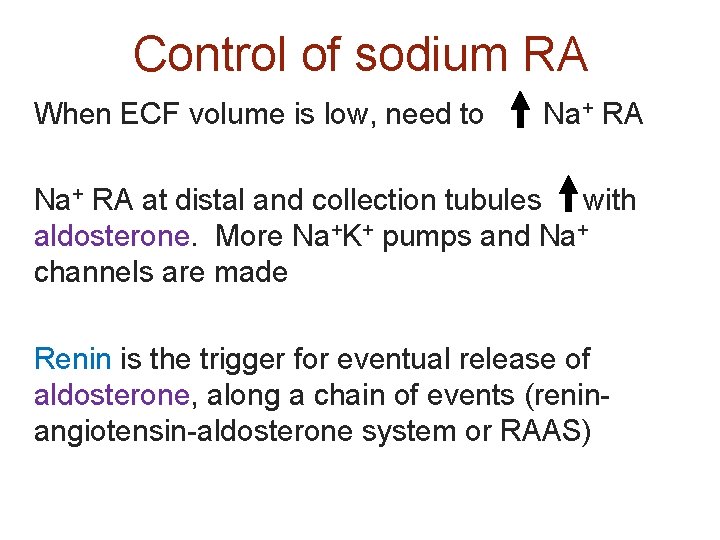
Control of sodium RA When ECF volume is low, need to Na+ RA at distal and collection tubules with aldosterone. More Na+K+ pumps and Na+ channels are made Renin is the trigger for eventual release of aldosterone, along a chain of events (reninangiotensin-aldosterone system or RAAS)
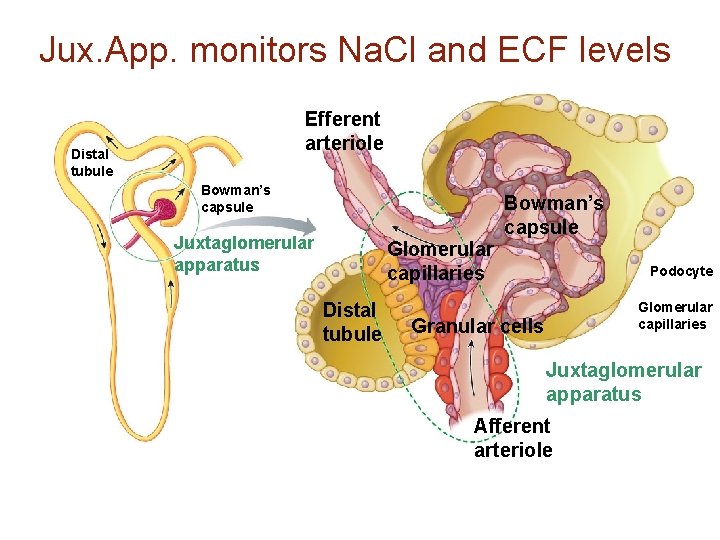
Jux. App. monitors Na. Cl and ECF levels Efferent arteriole Distal tubule Bowman’s capsule Juxtaglomerular apparatus Glomerular capillaries Distal tubule Bowman’s capsule Podocyte Glomerular capillaries Granular cells Juxtaglomerular apparatus Afferent arteriole
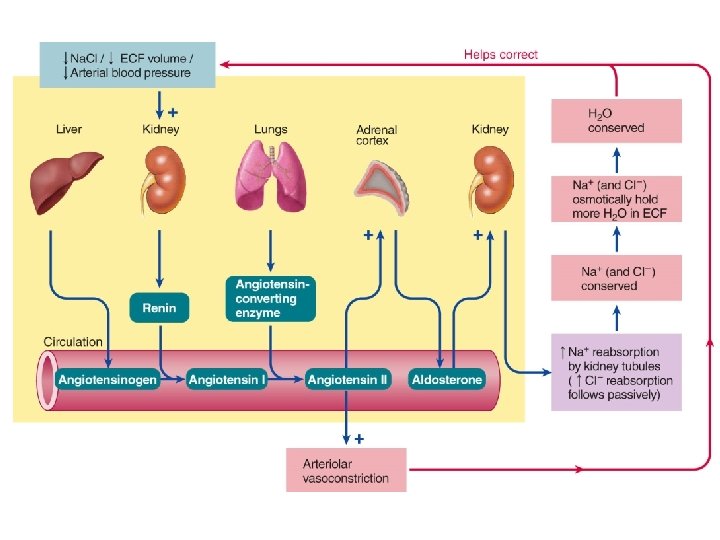
Hypertension can be due to increased renin leading to more plasma and thus high blood pressure
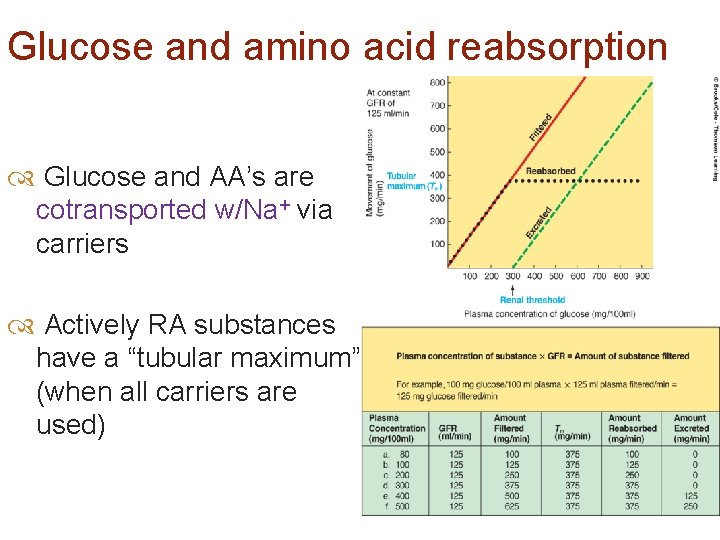
Glucose and amino acid reabsorption Glucose and AA’s are cotransported w/Na+ via carriers Actively RA substances have a “tubular maximum” (when all carriers are used)
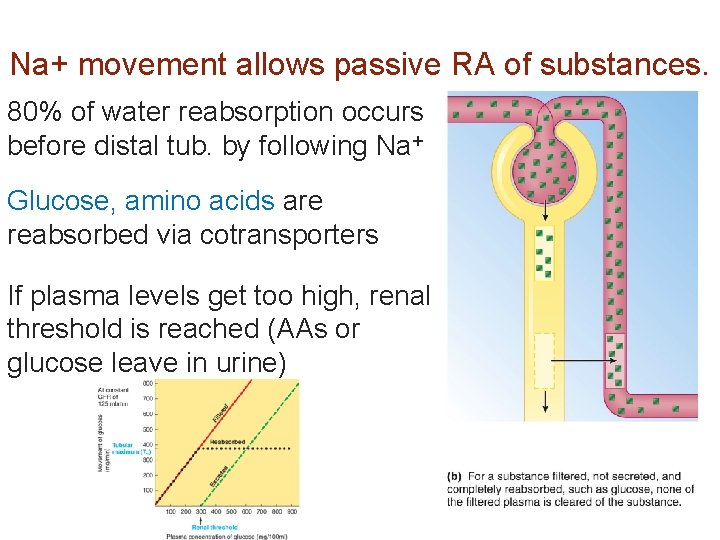
Na+ movement allows passive RA of substances. 80% of water reabsorption occurs before distal tub. by following Na+ Glucose, amino acids are reabsorbed via cotransporters If plasma levels get too high, renal threshold is reached (AAs or glucose leave in urine)
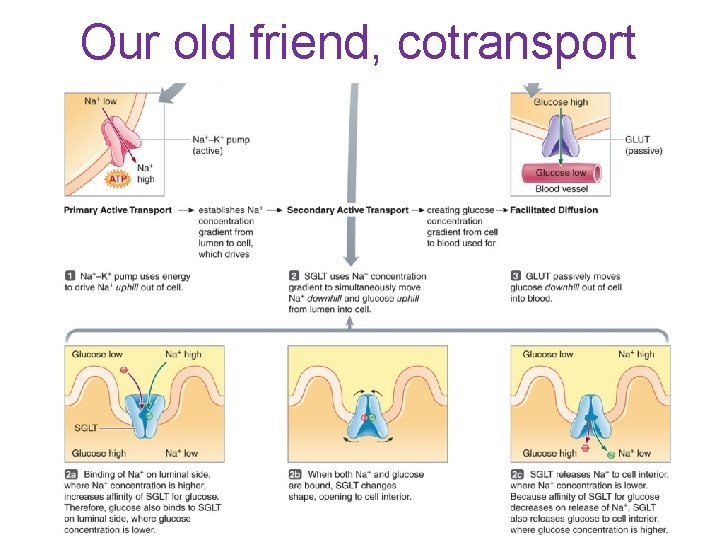
Our old friend, cotransport
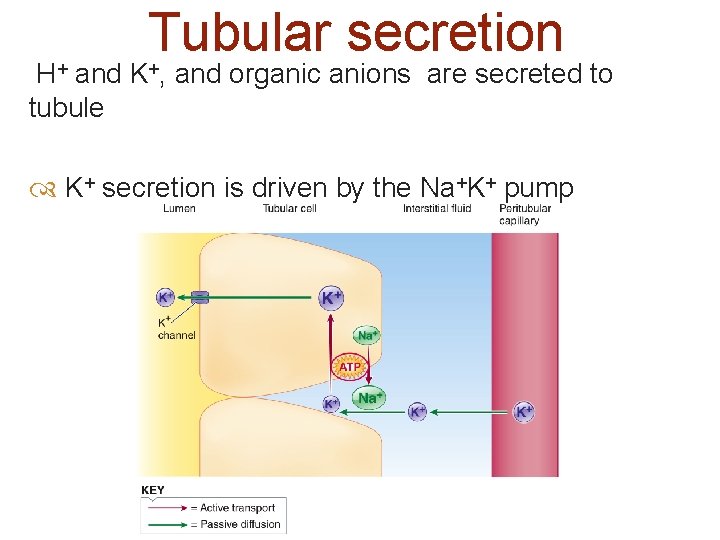
Tubular secretion H+ and K+, and organic anions are secreted to tubule K+ secretion is driven by the Na+K+ pump
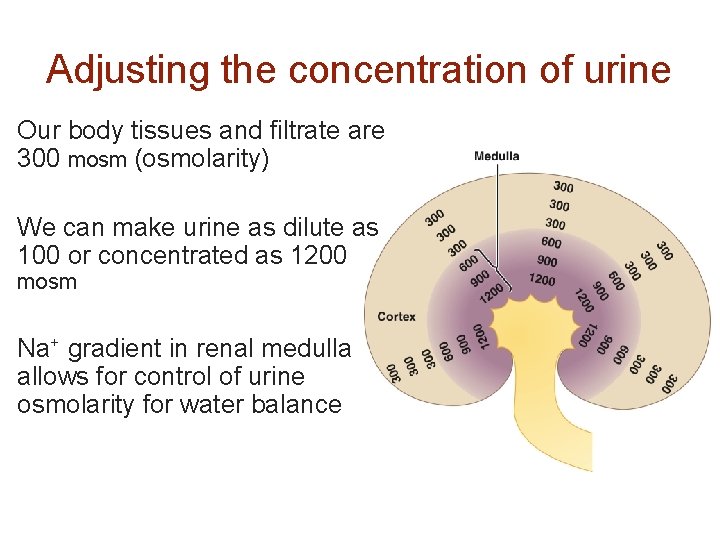
Adjusting the concentration of urine Our body tissues and filtrate are 300 mosm (osmolarity) We can make urine as dilute as 100 or concentrated as 1200 mosm Na+ gradient in renal medulla allows for control of urine osmolarity for water balance
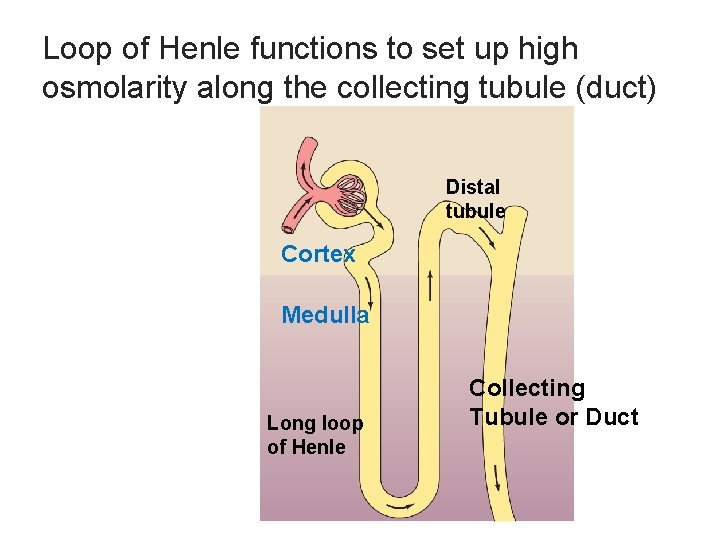
Loop of Henle functions to set up high osmolarity along the collecting tubule (duct) Distal tubule Cortex Medulla Long loop of Henle Collecting Tubule or Duct
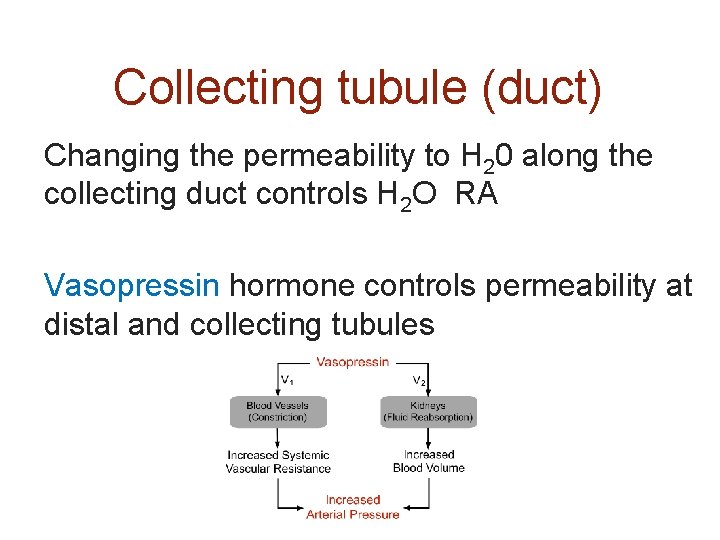
Collecting tubule (duct) Changing the permeability to H 20 along the collecting duct controls H 2 O RA Vasopressin hormone controls permeability at distal and collecting tubules
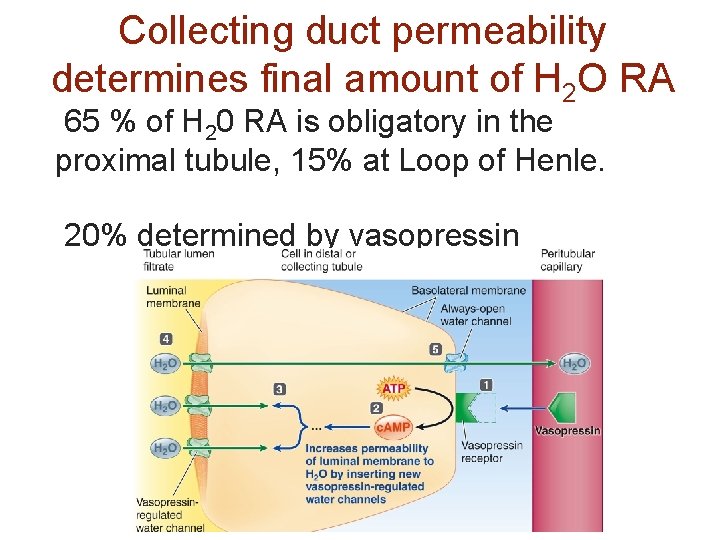
Collecting duct permeability determines final amount of H 2 O RA 65 % of H 20 RA is obligatory in the proximal tubule, 15% at Loop of Henle. 20% determined by vasopressin
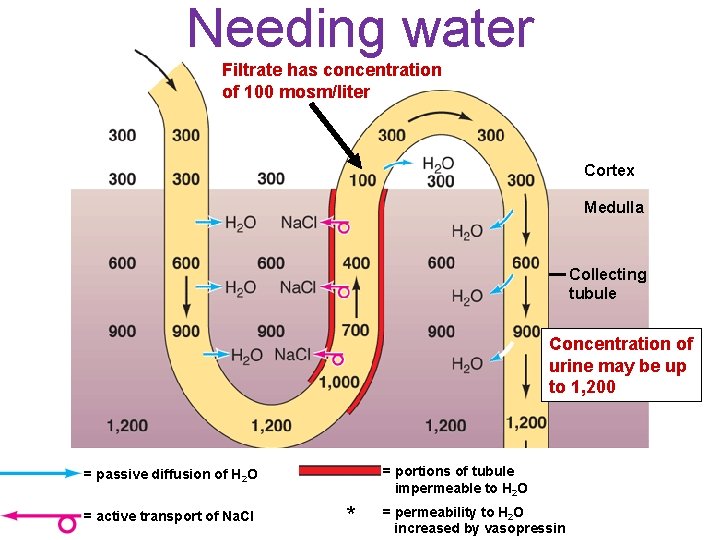
Needing water Filtrate has concentration of 100 mosm/liter Cortex Medulla Collecting tubule Concentration of urine may be up to 1, 200 = portions of tubule impermeable to H 2 O = passive diffusion of H 2 O = active transport of Na. Cl * = permeability to H 2 O increased by vasopressin
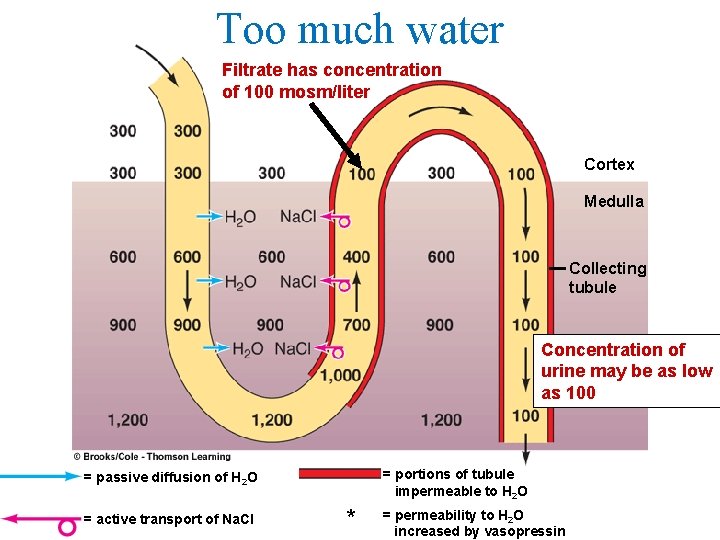
Too much water Filtrate has concentration of 100 mosm/liter Cortex Medulla Collecting tubule Concentration of urine may be as low as 100 = portions of tubule impermeable to H 2 O = passive diffusion of H 2 O = active transport of Na. Cl * = permeability to H 2 O increased by vasopressin
Why increased urination from alcohol? Alcohol inhibits vasopressin It can also temporarily reduce blood glucose (via liver effects)
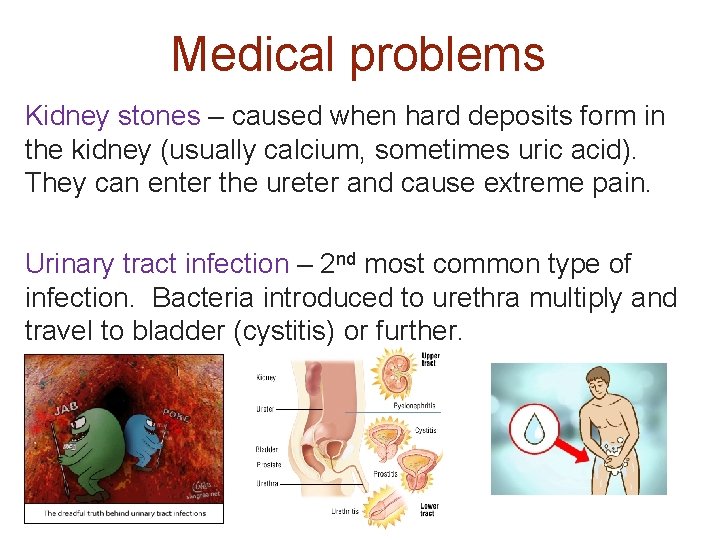
Medical problems Kidney stones – caused when hard deposits form in the kidney (usually calcium, sometimes uric acid). They can enter the ureter and cause extreme pain. Urinary tract infection – 2 nd most common type of infection. Bacteria introduced to urethra multiply and travel to bladder (cystitis) or further.
End of exam 4 material
Things I’m assuming you know: Know layers found throughout alimentary canal (mucosa, submucosa, muscular layers) and the term lumen Accessory structures (pancreas, liver, salivary glands, other exocrine glands) are a part of the digestive system
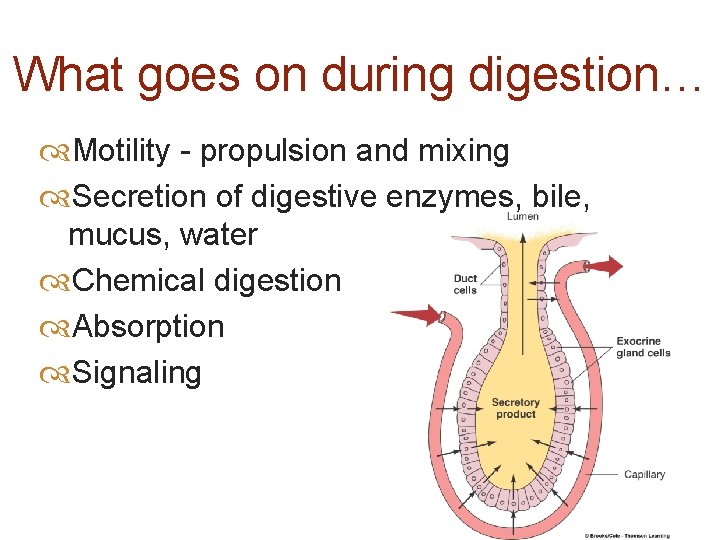
What goes on during digestion… Motility - propulsion and mixing Secretion of digestive enzymes, bile, mucus, water Chemical digestion Absorption Signaling
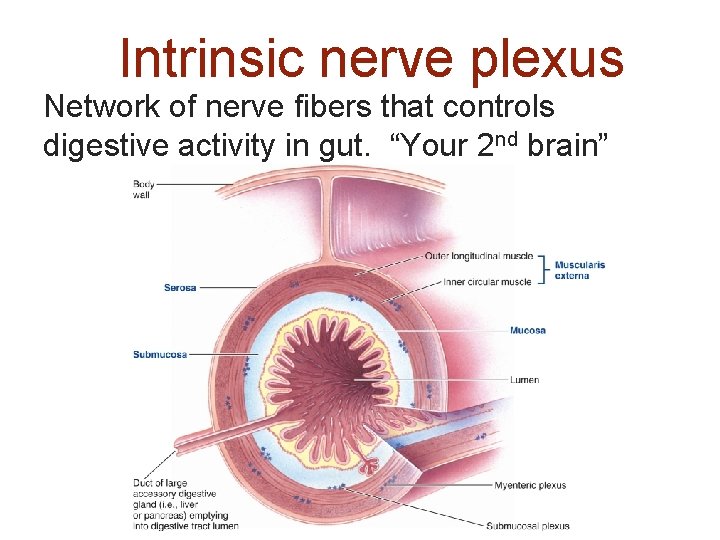
Intrinsic nerve plexus Network of nerve fibers that controls digestive activity in gut. “Your 2 nd brain”
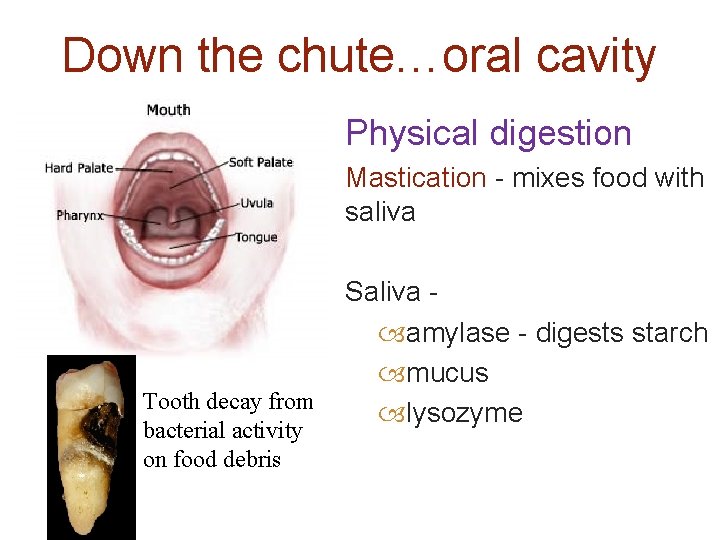
Down the chute…oral cavity Physical digestion Mastication - mixes food with saliva Tooth decay from bacterial activity on food debris Saliva amylase - digests starch mucus lysozyme
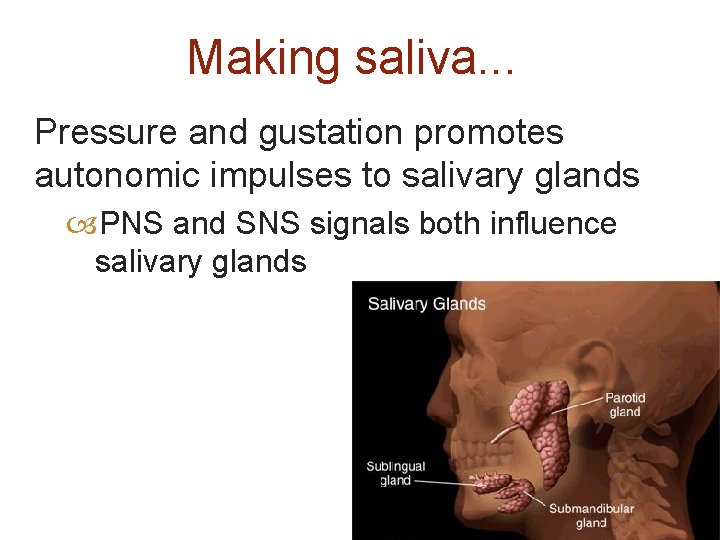
Making saliva. . . Pressure and gustation promotes autonomic impulses to salivary glands PNS and SNS signals both influence salivary glands
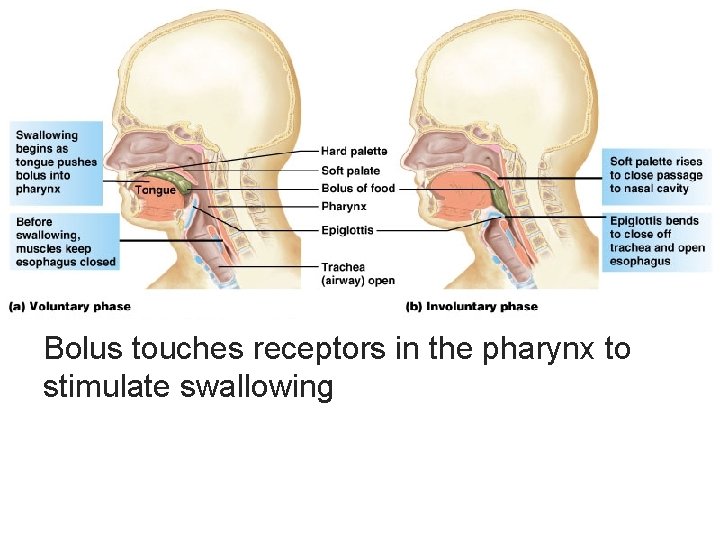
Bolus touches receptors in the pharynx to stimulate swallowing
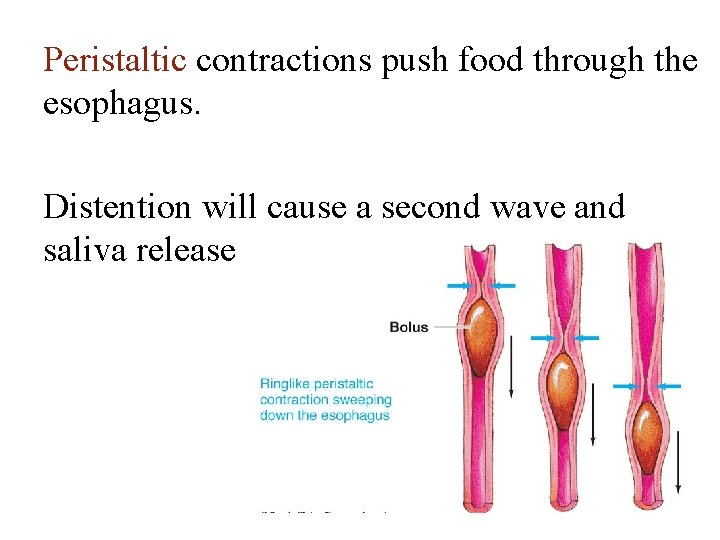
Peristaltic contractions push food through the esophagus. Distention will cause a second wave and saliva release
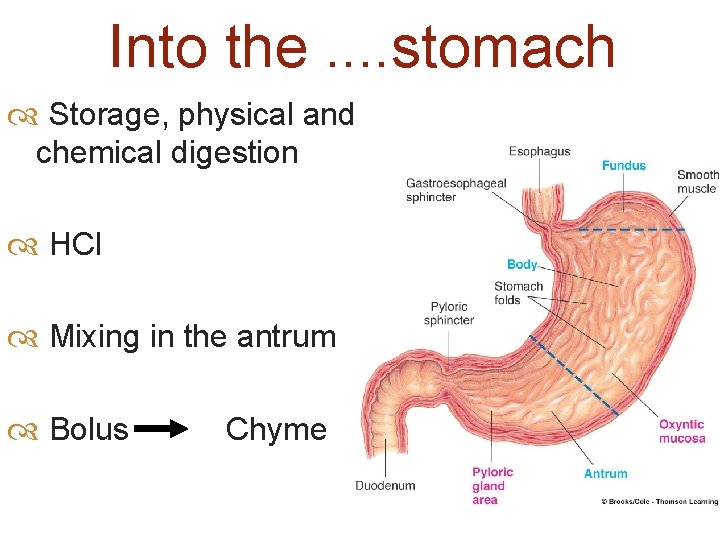
Into the. . stomach Storage, physical and chemical digestion HCl Mixing in the antrum Bolus Chyme
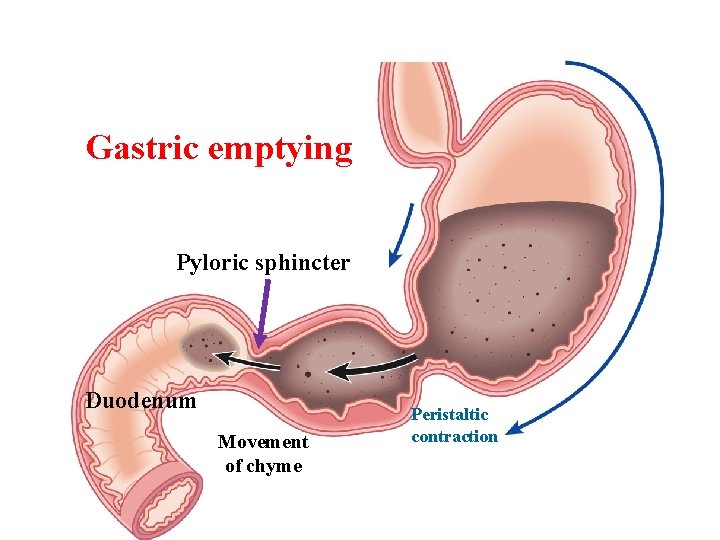
Gastric emptying Pyloric sphincter Duodenum Movement of chyme Peristaltic contraction
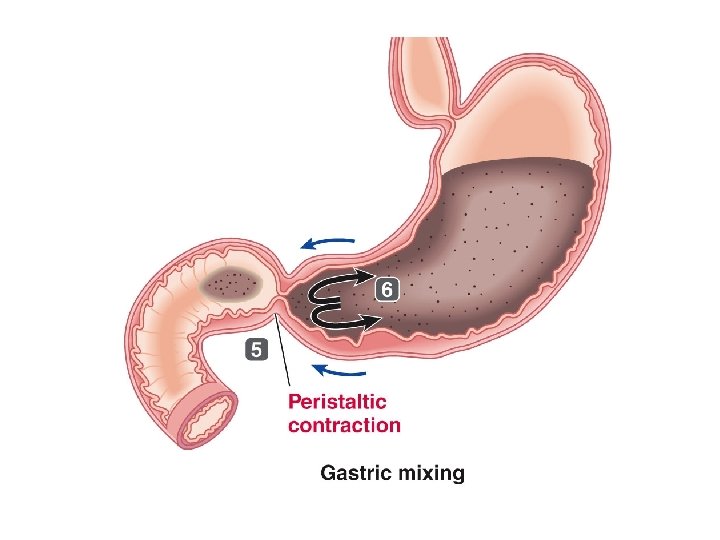
Peristaltic contraction
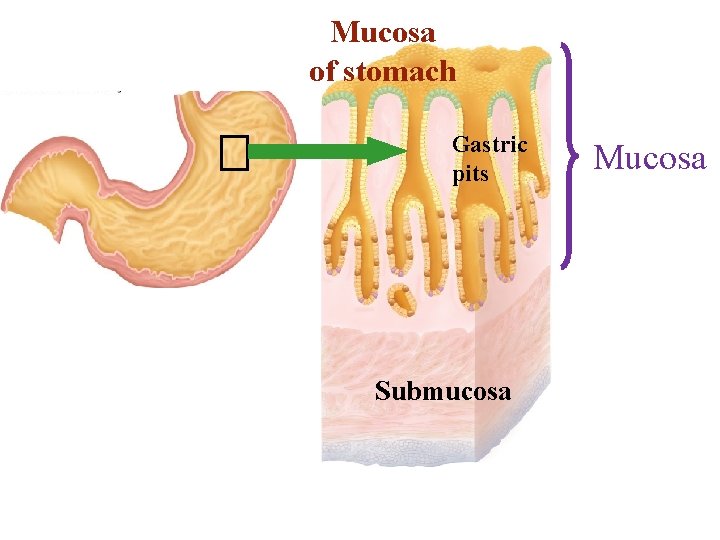
Mucosa of stomach Gastric pits Submucosa Mucosa
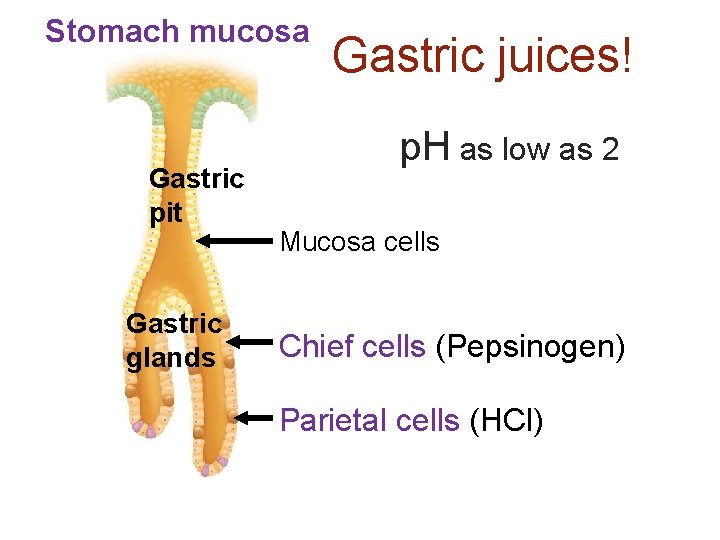
Stomach mucosa Gastric pit Gastric glands Gastric juices! p. H as low as 2 Mucosa cells Chief cells (Pepsinogen) Parietal cells (HCl)
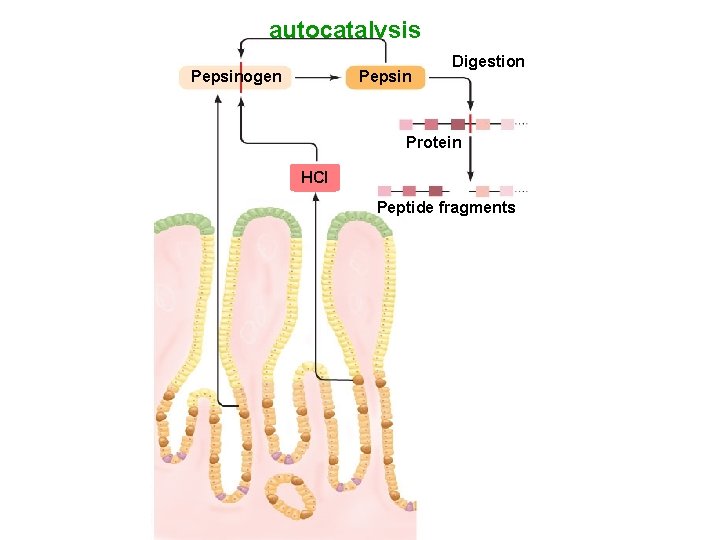
autocatalysis Pepsinogen Pepsin Digestion Protein HCI Peptide fragments
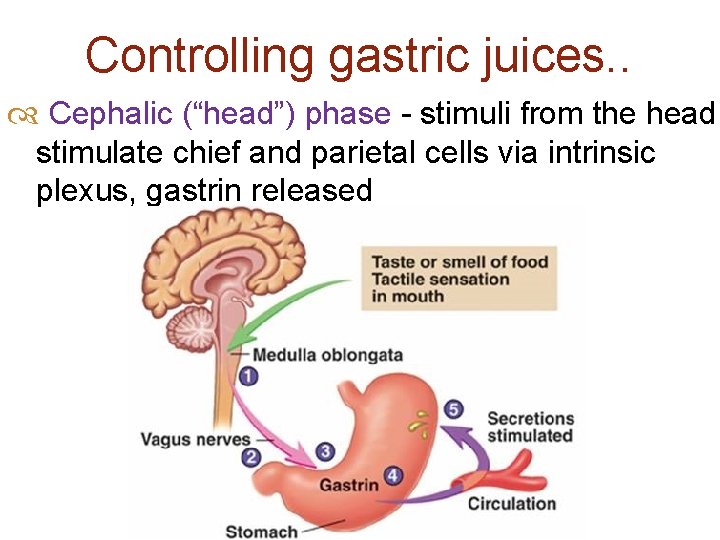
Controlling gastric juices. . Cephalic (“head”) phase - stimuli from the head stimulate chief and parietal cells via intrinsic plexus, gastrin released
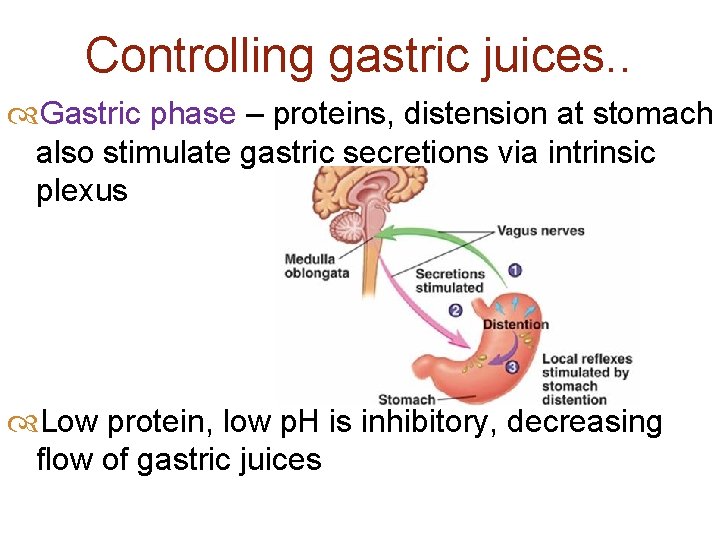
Controlling gastric juices. . Gastric phase – proteins, distension at stomach also stimulate gastric secretions via intrinsic plexus Low protein, low p. H is inhibitory, decreasing flow of gastric juices
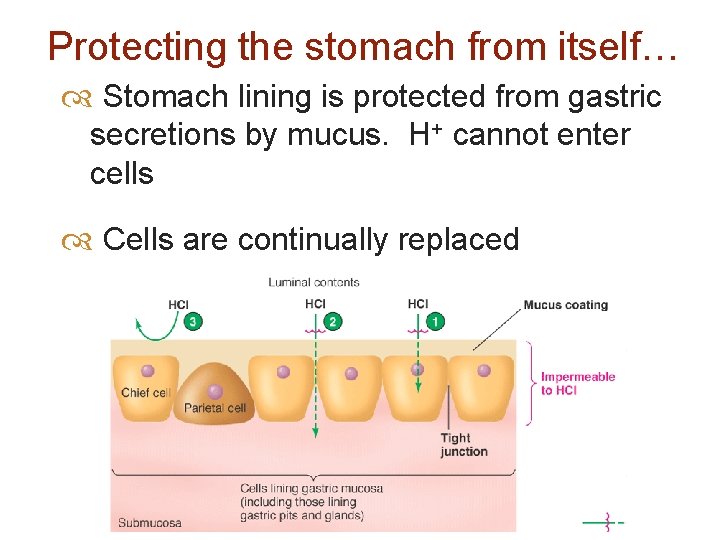
Protecting the stomach from itself… Stomach lining is protected from gastric secretions by mucus. H+ cannot enter cells Cells are continually replaced
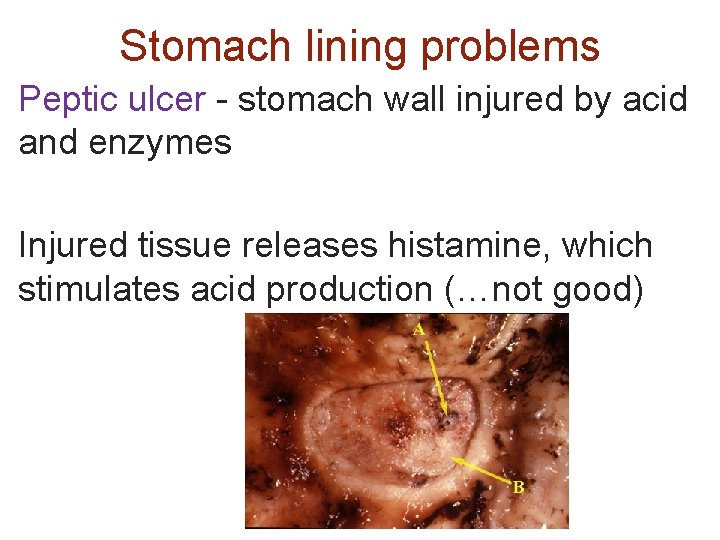
Stomach lining problems Peptic ulcer - stomach wall injured by acid and enzymes Injured tissue releases histamine, which stimulates acid production (…not good)
Leaving the stomach… Emptying controlled by duodenum and stomach Chyme volume promotes emptying Acid and fats in duodenum prevent gastric emptying
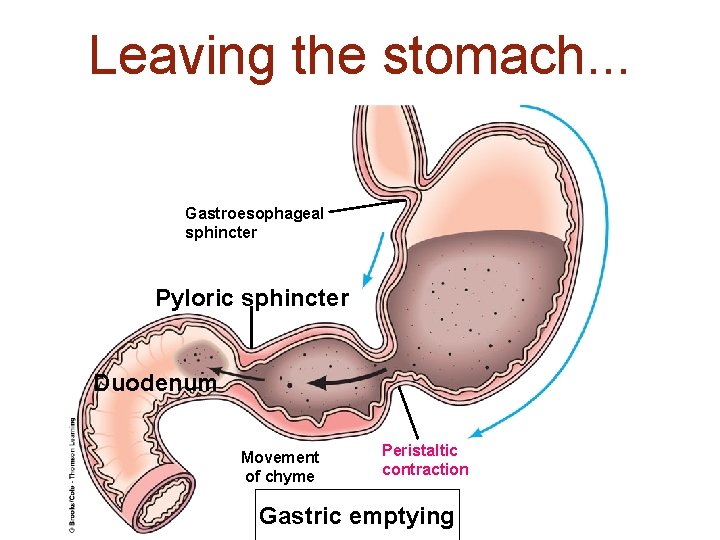
Leaving the stomach. . . Gastroesophageal sphincter Pyloric sphincter Duodenum Movement of chyme Peristaltic contraction Gastric emptying
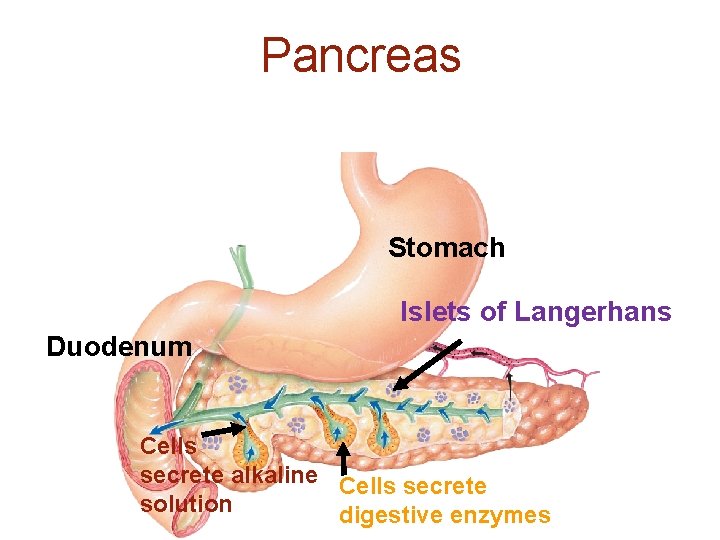
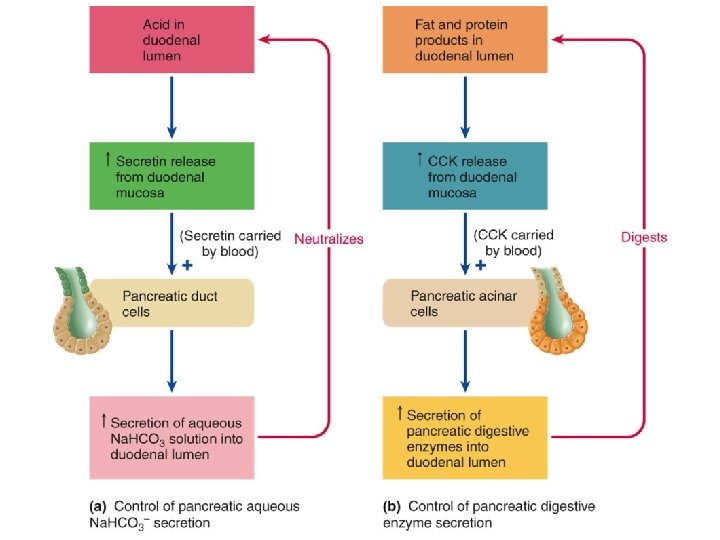
Pancreas Stomach Islets of Langerhans Duodenum Cells secrete alkaline Cells secrete solution digestive enzymes
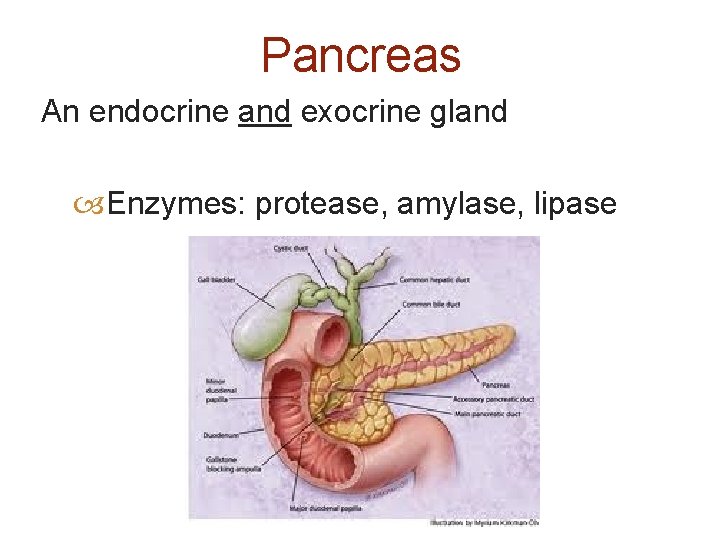
Pancreas An endocrine and exocrine gland Enzymes: protease, amylase, lipase
- Slides: 54