Urinary Incontinence Kathleen Pace Murphy Ph D MS


- Slides: 21
Urinary Incontinence Kathleen Pace Murphy, Ph. D, MS, APRN Assistant Professor, UT Medical School Geriatric and Palliative Medicine
Prevalence �Increases with age and affects women more than men (2: 1) until age 80 � 15 -30% in community dwellers age 65 and older � 60 -70% in older adults age 65 and older in long term care �Significantly impairs quality of life
Risk Factors �Obesity �Functional impairment �Dementia �Medications �Environmental barriers to toilet access
Age related LUT changes �Bladder contractility decreases �Uninhibited bladder contractions increase �Diurnal urine output occurse later in day �Bladder capacity decreases �Sphincteric striated muscle attenuates �PVR increases
Age related LUT changes- Women �In addition to the physiologic changes already discussed: �Urethral closure pressure decreases �Vaginal mucosal atrophy
Age related LUT changes- Men �In addition to the physiologic changes already discussed: �Benign prostatic hyperplasia �Prostate hypertrophy
LUT Pathophysiology in UI Urge UI �Urge UI with detrusor overactivity (uninhibited bladder contractions) � 40% on urodynamic testing �Suggest detrusor overactivity PLUS impaired compensatory mechanisms. �Idiopathic, age-related, secondary to lesions in cerebral and spinal pathways. �Due to bladder outlet obstruction or bladder irritation (infection, stones, tumor)
LUT Pathophysiology in UI Stress UI �Etiology �Damage to the pelvic floor supports �Sphincter failure �Leakage associated with coughing, sneezing, laughing, physical activity �Second most common form in women �Seen in men after prostectomy
LUT Pathophysiology in UI Mixed UI with both detrusor overactivity and impaired sphincter support �Leakage occurs with both urgency and activity �Seen in women
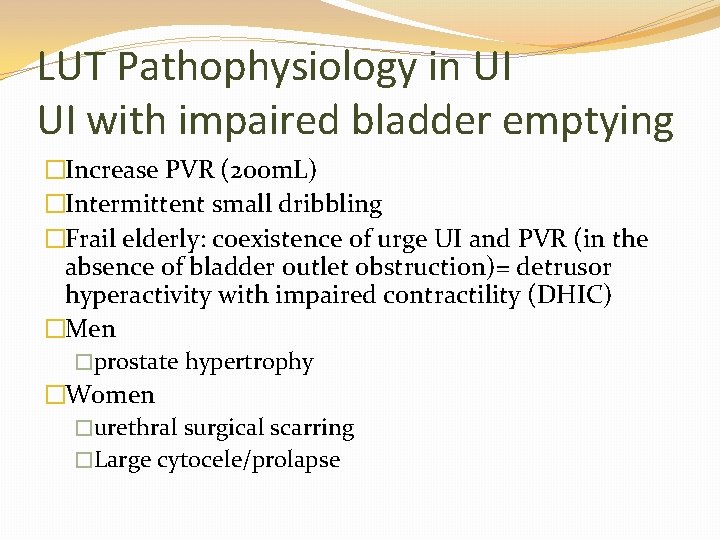
LUT Pathophysiology in UI UI with impaired bladder emptying �Increase PVR (200 m. L) �Intermittent small dribbling �Frail elderly: coexistence of urge UI and PVR (in the absence of bladder outlet obstruction)= detrusor hyperactivity with impaired contractility (DHIC) �Men �prostate hypertrophy �Women �urethral surgical scarring �Large cytocele/prolapse
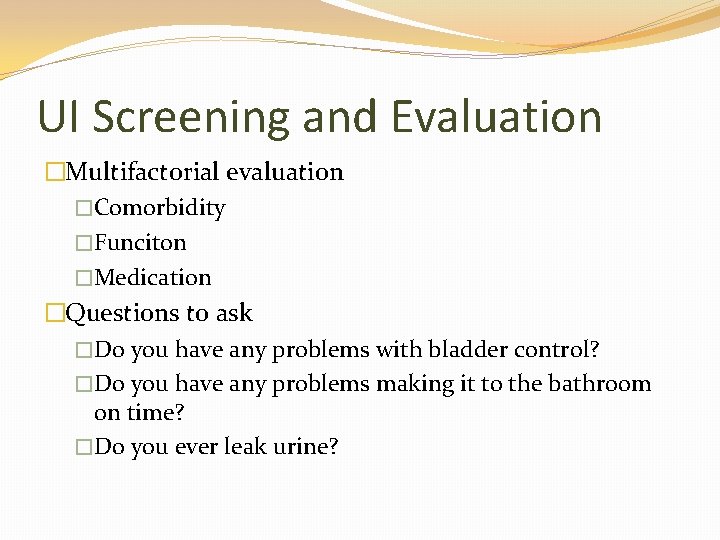
UI Screening and Evaluation �Multifactorial evaluation �Comorbidity �Funciton �Medication �Questions to ask �Do you have any problems with bladder control? �Do you have any problems making it to the bathroom on time? �Do you ever leak urine?

Medications Associated with UI � Alcohol � Alpha-adrenergic agonists � Alpha-adrenergic blockers � ACE Inhibitors � Anticholinergic � Antipsychotics � CCB � Cholinesterase inhibitors � Estrogen � Gabapentin � Loop diuretics � Narcotics � NSAIDs � Sedative hypnotics � Thiazolidinediones � TCA

UI Red Flags �Abrupt onset �Pelvic pain (constant, worsened, or improve with voiding) �Hematuria
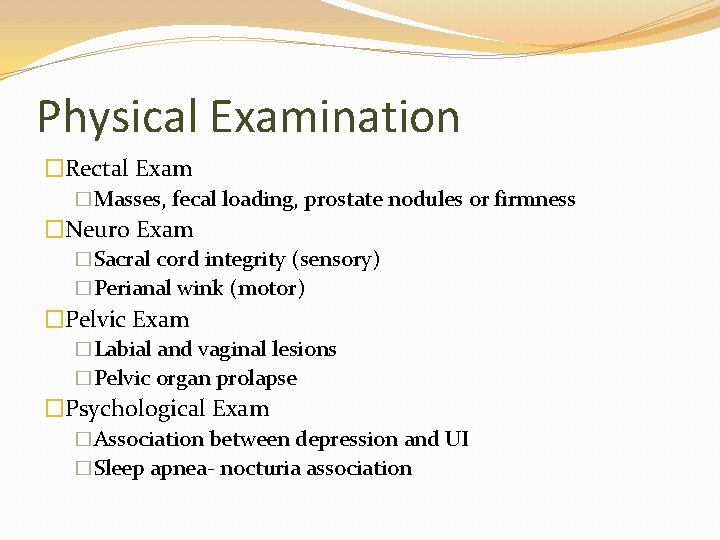
Physical Examination �Rectal Exam �Masses, fecal loading, prostate nodules or firmness �Neuro Exam �Sacral cord integrity (sensory) �Perianal wink (motor) �Pelvic Exam �Labial and vaginal lesions �Pelvic organ prolapse �Psychological Exam �Association between depression and UI �Sleep apnea- nocturia association
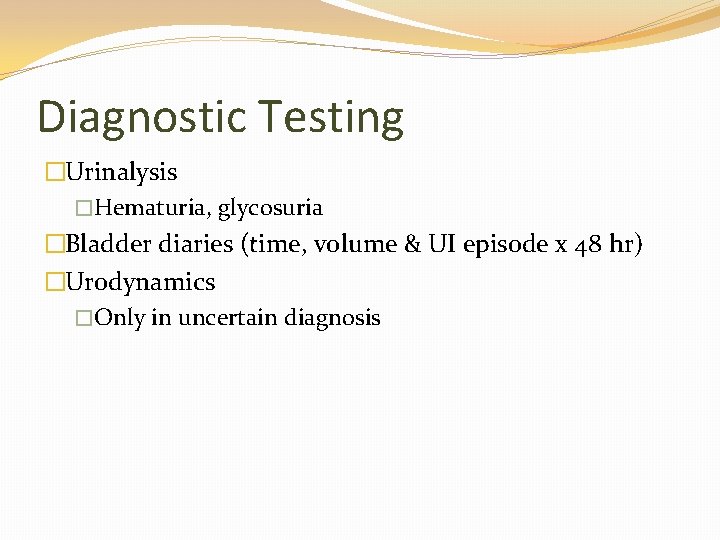
Diagnostic Testing �Urinalysis �Hematuria, glycosuria �Bladder diaries (time, volume & UI episode x 48 hr) �Urodynamics �Only in uncertain diagnosis
UI Treatment and Management �Lifestyle Management �Weight loss (SOE=A) �Extreme fluid intake �Limit caffinated beverages �Limit ETOH �Limit evening fluid intake �Quit smoking (stress UI)
UI Treatment and Management �Behavioral Therapies �A. Bladder training and pelvic muscle exercises � 1. Effective urge, mixed, and stress UI (SOE=A) �B. Prompt timed voiding in cognitively impaired �C. Biofeedback for PME � 1. Medicare covers (SOE=Unkown)
Medications Anti Muscarinics � MOA � Increase bladder capacity by decreasing basal excretion of Ach from urothelium � Contraindicated � Narrow angle glaucoma � Impaired gastric emptying � Known urinary retention � Patient taking cholinesterase inhibitor � Drugs � Oxybutynin � Tolterodine � Fesoterodine � Trospium � Darifenacin � Solifenacin
Medications �Rx UI and OAB �MOA �Stimulation of beta 3 receptors in the detruor mediates bladder relaxation: �Myrbetriq 25 -50 mg QD �ADE �Increase blood pressure �Prescribe carefully in patient with renal and hepatic impairment �Many drug-drug AE like muscarins
Other Treatments �Intravesical injection of botulinum toxin �Sacral nerve neuromodulation �Surgery (stress UI) �Colpsuspension (Burch Operation) �Slings (synthetic mesh, or autologus or cadaveric fascia)
References � Flaherty E & Resnick B Geriatric Nursing Review Syllabus (4 th Ed). New York: American Geriatric Society; 2014. � Gulur DM, Mevcha AM, Drake MJ. Nocturia as a manifestation of systemic disease. BJU Int. 2011; 107 (50): 702 -13. � Ham, RJ, Sloan, PD, Warshaw, GA, Potter, JE & Flaherty E. Primary Care Geriatrics: A case-based approach (6 th Ed. ). 2014. Philadelphia: Elsevier Saunders. � Holroyd-Leduc JM, Tannenbaum C, Thorpe KE, Strauss SE. What type of urinariy incontinence does this woman have? JAMA, 2008 : 299: 1446 -56. � Landefeld CS, Bowers BJ, Feld AD et al. NIH state-of-the-scienceconference statement: Prevention of fecal and urinary incontinence in adults. Ann Intern Med 2008: 148: 449 -58. � Shamliyan T, Wyman J, Kane RL. Benefits and harms of pharmacologic treatment for UI in women: A systematic review. Ann Intern Med 2012: 156(12): 861 -74.