URINARY INCONTINENCE For Practicing Physicians Take Away Points


- Slides: 79
URINARY INCONTINENCE For Practicing Physicians
Take Away Points l l UI is a common and a serious problem among your patients A careful history and a brief exam can help identify the type(s) of UI Behavioral treatments are underutilized Anticholinergic drugs are indicated only for urge incontinence
Definition -- International l Involuntary loss of urine l Generally in an undesirable place l Creating a social, hygienic problem
Prevalence. . . What percentage of YOUR patients present with urinary incontinence? l Mostly men or women? l What age group? l How often do you address this concern? l
What percentage of communityliving older adults have UI? 1. 2. 3. 4. 5. 10% 30% 50% 70% 90%
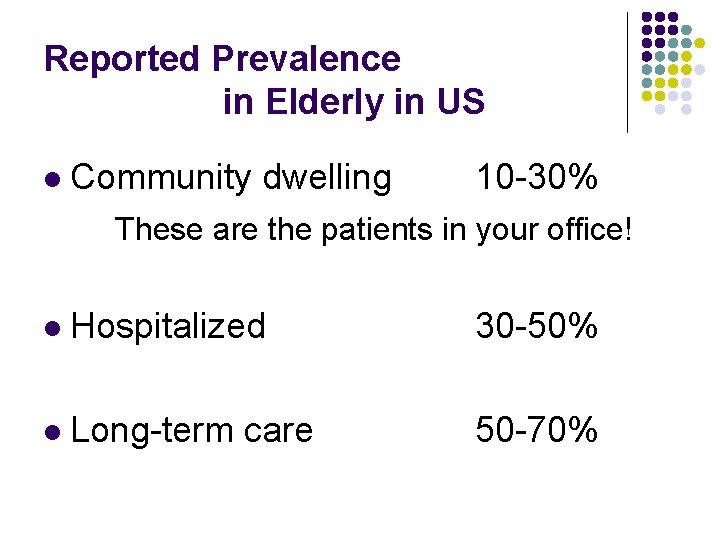
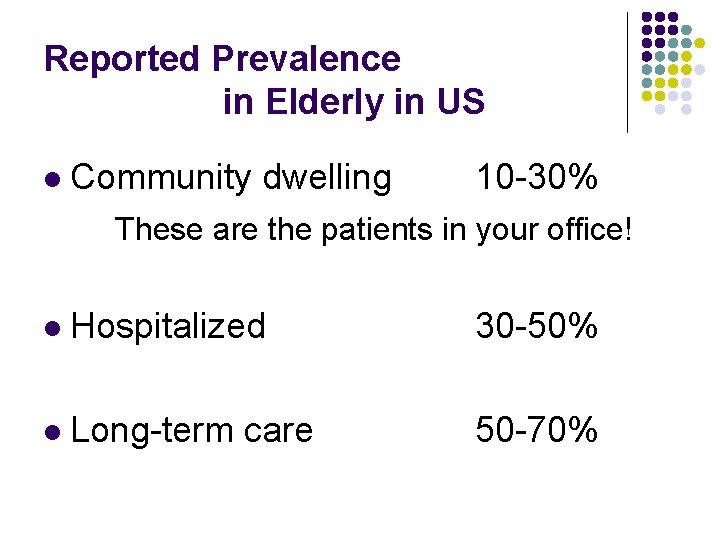
Reported Prevalence in Elderly in US l Community dwelling 10 -30% These are the patients in your office! l Hospitalized 30 -50% l Long-term care 50 -70%
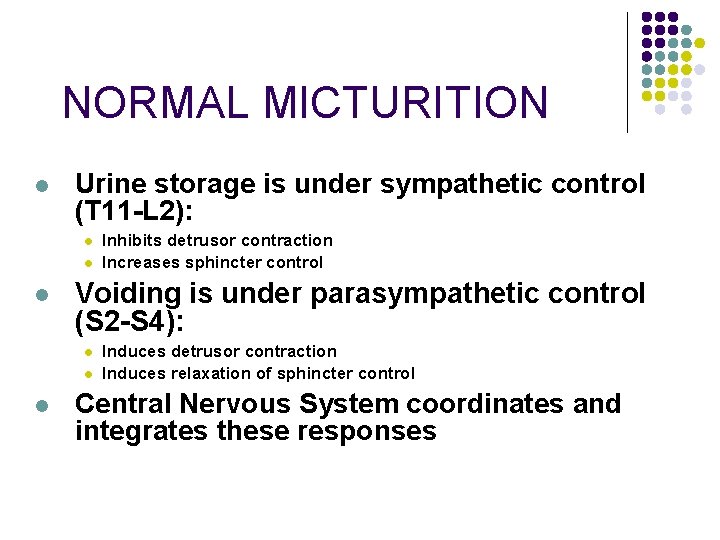
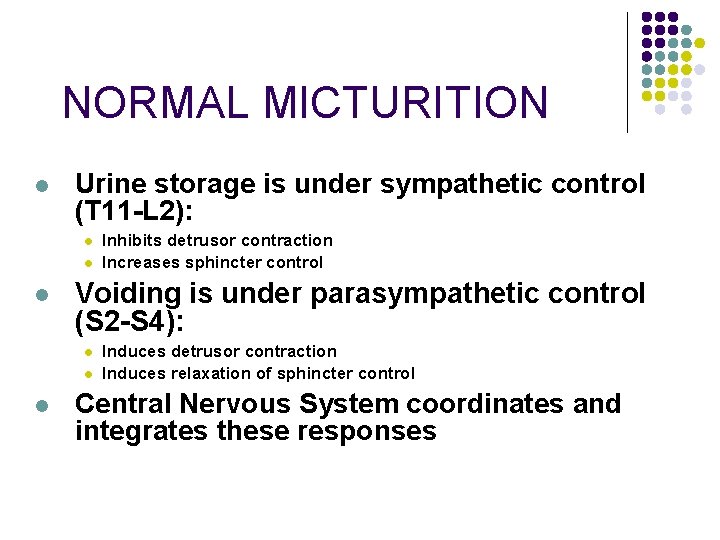
NORMAL MICTURITION l Urine storage is under sympathetic control (T 11 -L 2): l l l Voiding is under parasympathetic control (S 2 -S 4): l l l Inhibits detrusor contraction Increases sphincter control Induces detrusor contraction Induces relaxation of sphincter control Central Nervous System coordinates and integrates these responses
What changes occur with the aging process which can contribute to urinary incontinence? 1. 2. 3. 4. 5. 6. Decreased mobility Inability to postpone voiding Prostate hypertrophy Urethral dysfunction Increased night time urine volume All of the above
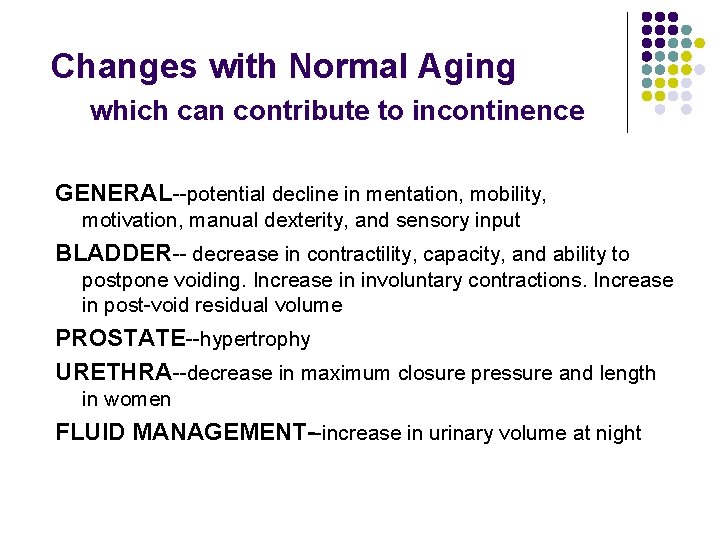
Changes with Normal Aging which can contribute to incontinence GENERAL--potential decline in mentation, mobility, motivation, manual dexterity, and sensory input BLADDER-- decrease in contractility, capacity, and ability to postpone voiding. Increase in involuntary contractions. Increase in post-void residual volume PROSTATE--hypertrophy URETHRA--decrease in maximum closure pressure and length in women FLUID MANAGEMENT--increase in urinary volume at night
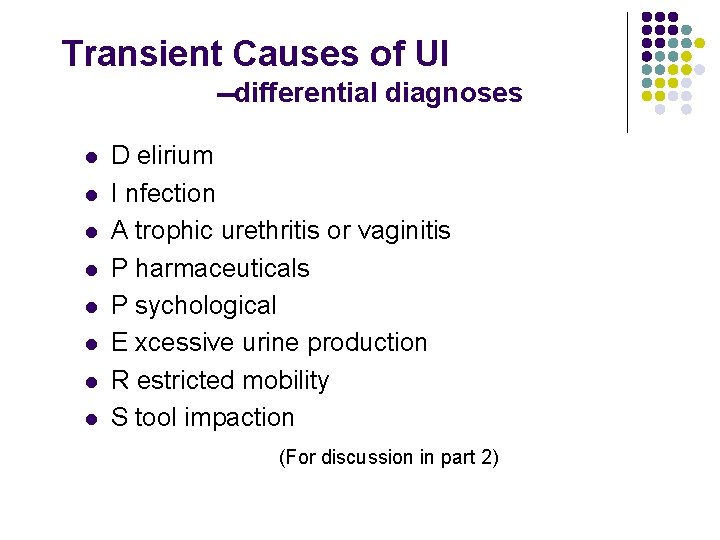
Transient Causes of UI --differential diagnoses l l l l D elirium I nfection A trophic urethritis or vaginitis P harmaceuticals P sychological E xcessive urine production R estricted mobility S tool impaction (For discussion in part 2)
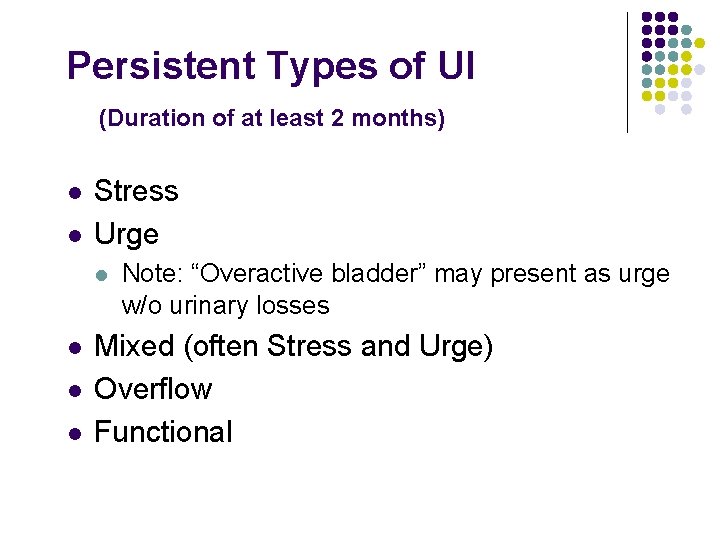
Persistent Types of UI (Duration of at least 2 months) l l Stress Urge l l Note: “Overactive bladder” may present as urge w/o urinary losses Mixed (often Stress and Urge) Overflow Functional
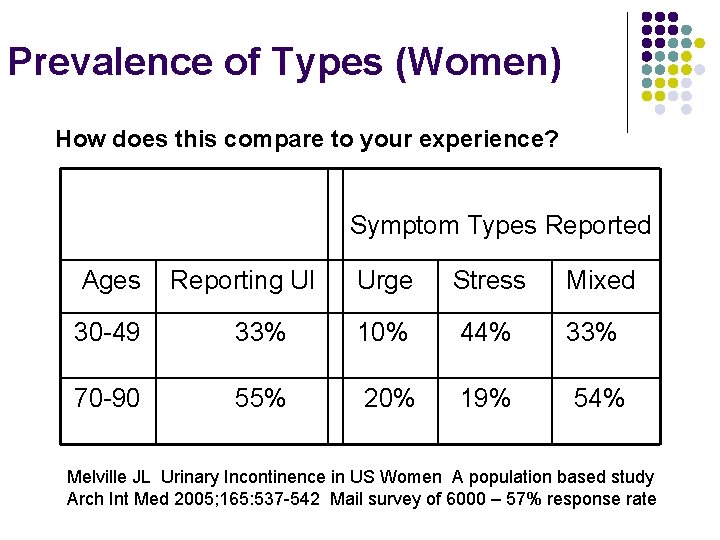
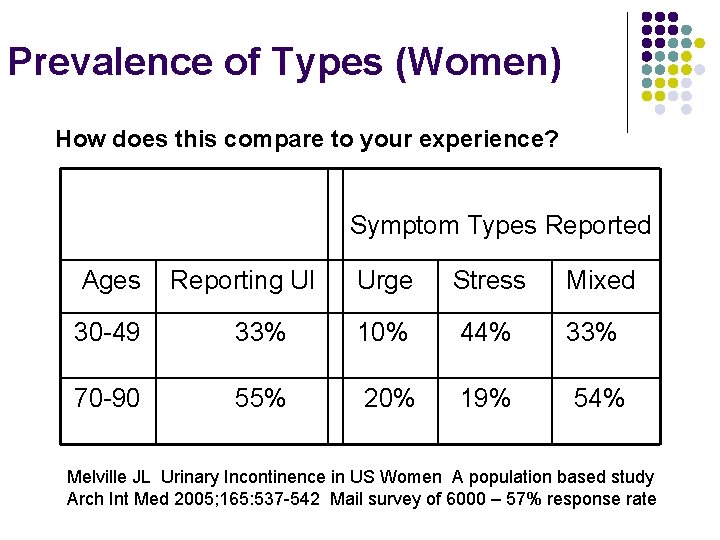
Prevalence of Types (Women) How does this compare to your experience? Symptom Types Reported Ages Reporting UI Urge Stress Mixed 30 -49 33% 10% 44% 33% 70 -90 55% 20% 19% 54% Melville JL Urinary Incontinence in US Women A population based study Arch Int Med 2005; 165: 537 -542 Mail survey of 6000 – 57% response rate

Prevalence Data from JH Incontinence Program 403 patients, 85% female, age 78. 4+/-8. 22 Urge 254 total (35 urge alone) Stress 185 total (42 stress alone) Urge and Stress together 138 total Overflow 34 total (17 overflow alone) Functional 160 total (10 functional alone) Most cases had 2 or 3 types of incontinence
Workup in Primary Care --Persistent incontinence l History—including medications, supplemented by bladder records or voiding diaries. Quality of life concerns. l Focused physical—mental and neurologic, abdomen, pelvic and rectal l Office Testing—Urinalysis, routine lab tests, postvoid residual
Case 1 Mrs. Leeky l l A 78 year old woman with urinary incontinence: urgency, nocturia and leakage enroute to BR Duration >2 mos. Also losses with coughing. Wears pads. No significant GU history. The pt has CHF, GERD, glaucoma, and osteoporosis. Meds: enalapril, furosemide, K+, timolol eyedrops, calcium, ranitidine. More
Case 1 continued l l PE: Ambulatory, cognitively intact. Normal CV and neurologic findings. 2+ ankle edema. Abd neg. Pelvic--no inflammation, grade 2 cystocele, no masses. Rectal nl. Coughing produces drops of urine at the meatus. The patient voids 325 ml of urine when she develops a normal sense of micturition and is then catheterized for 60 ml. Urinalysis is normal.
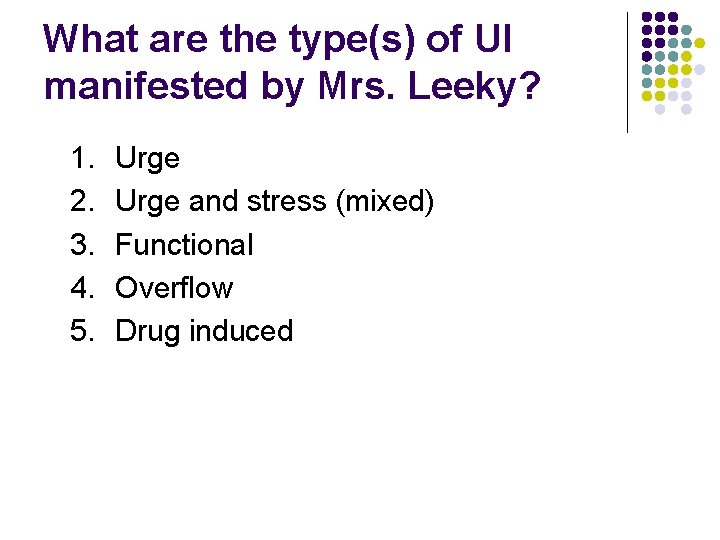
What are the type(s) of UI manifested by Mrs. Leeky? 1. 2. 3. 4. 5. Urge and stress (mixed) Functional Overflow Drug induced
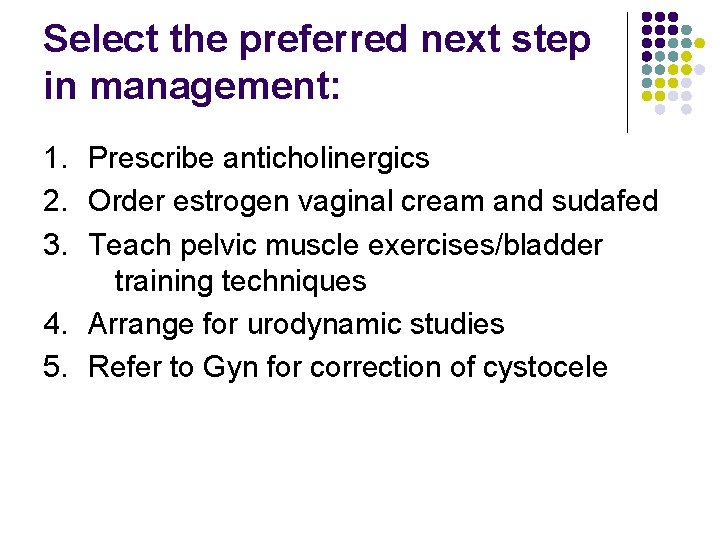
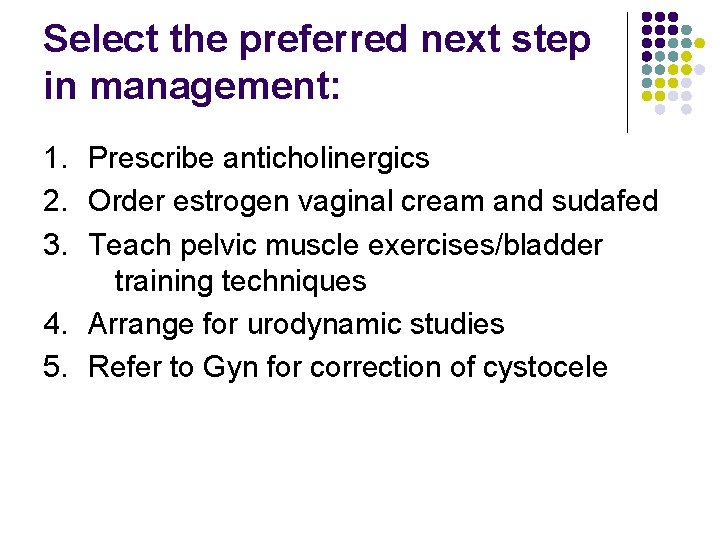
Select the preferred next step in management: 1. Prescribe anticholinergics 2. Order estrogen vaginal cream and sudafed 3. Teach pelvic muscle exercises/bladder training techniques 4. Arrange for urodynamic studies 5. Refer to Gyn for correction of cystocele
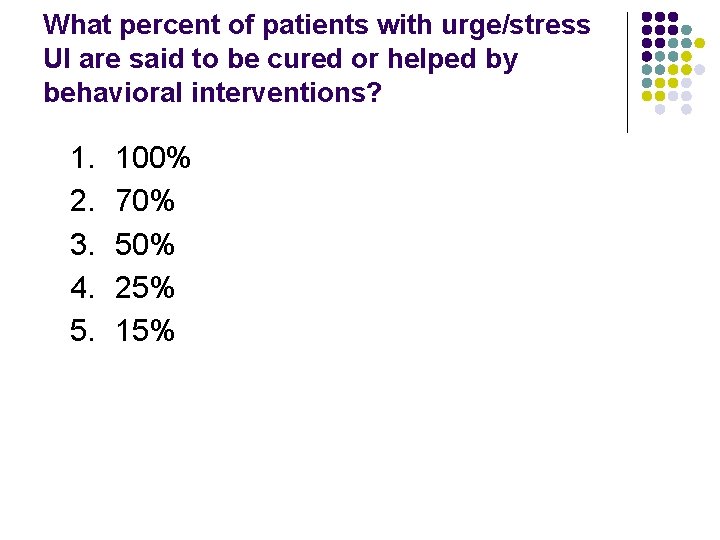
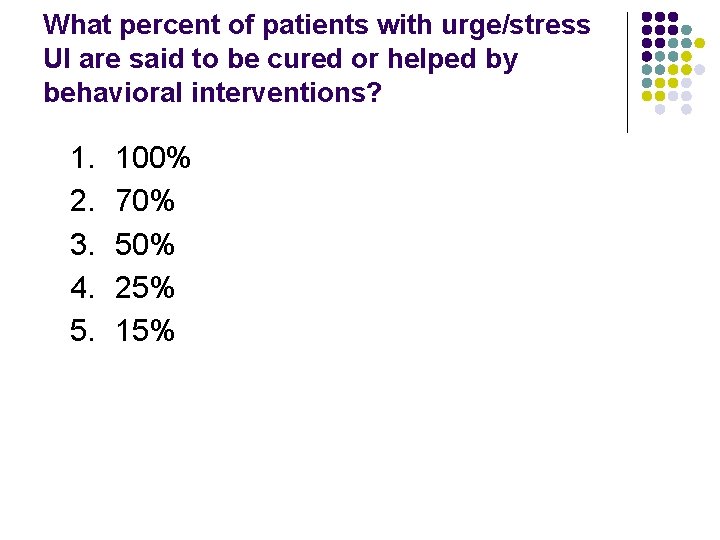
What percent of patients with urge/stress UI are said to be cured or helped by behavioral interventions? 1. 2. 3. 4. 5. 100% 70% 50% 25% 15%

Stress Incontinence l Definition Loss of urine due to pressure on the bladder exceeding ability of sphincter to control l Causes Relative incompetence of sphincter Weakness of supporting structures Malposition of bladder/urethra
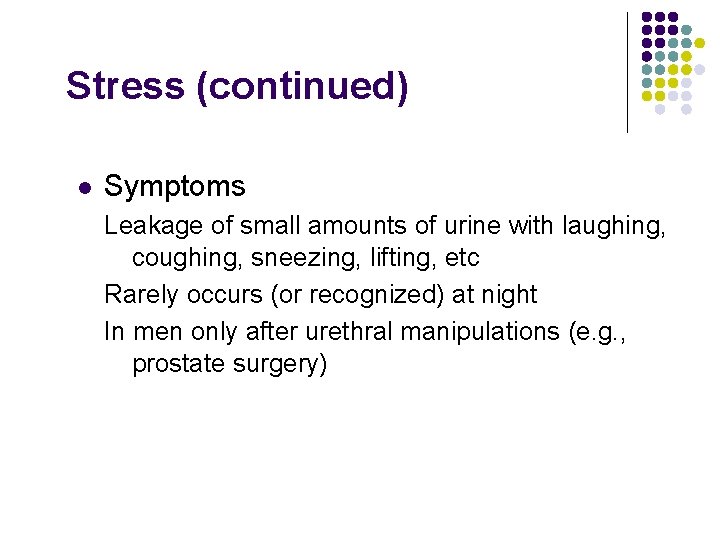
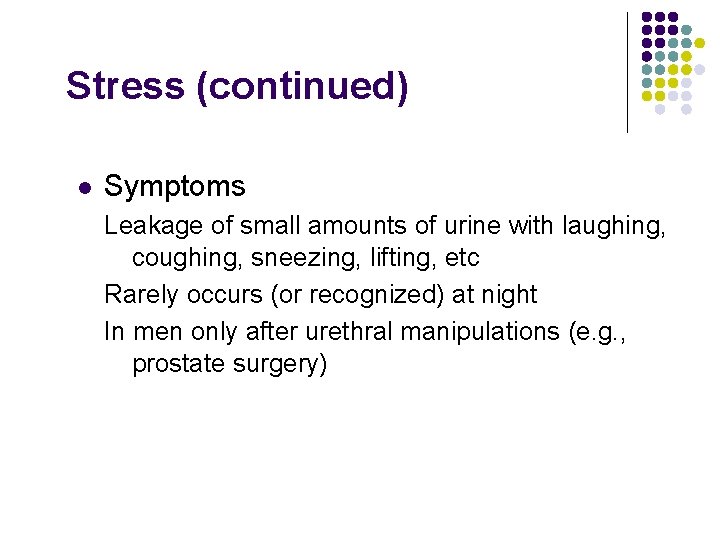
Stress (continued) l Symptoms Leakage of small amounts of urine with laughing, coughing, sneezing, lifting, etc Rarely occurs (or recognized) at night In men only after urethral manipulations (e. g. , prostate surgery)
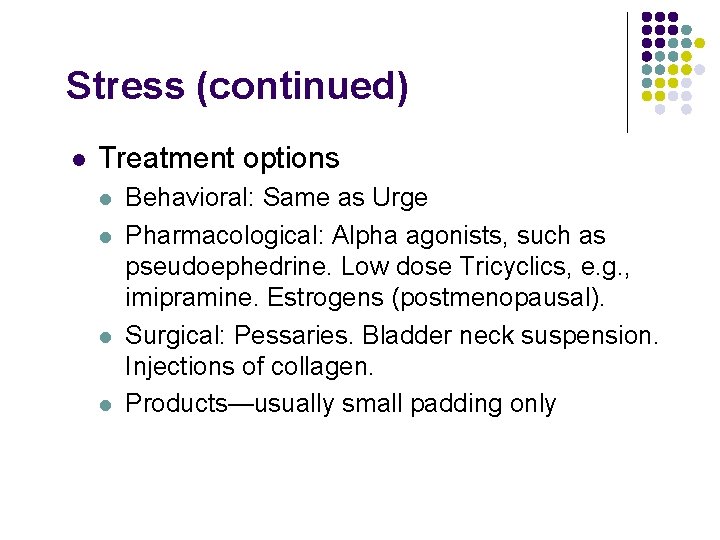
Stress (continued) l Treatment options l l Behavioral: Same as Urge Pharmacological: Alpha agonists, such as pseudoephedrine. Low dose Tricyclics, e. g. , imipramine. Estrogens (postmenopausal). Surgical: Pessaries. Bladder neck suspension. Injections of collagen. Products—usually small padding only
Urge Incontinence Definition Involuntary loss of urine due to uncontrollable contraction of bladder, with and without warning Causes GU changes of aging Irritative/neurologic condition, such as infections, diabetes mellitus, bladder stones, tumors, stroke or dementia, and increased intraabdominal pressure changes
Urge (continued) Signs and Symptoms Losses of variable (often large) amounts Little or no warning time Associated frequency Occurs both day and night
Urge – Behavioral Treatment l l l Bladder training Kegel exercises Prompted voiding; scheduled voiding Biofeedback Electrical stimulation
Urge – Drug Treatment l Nonspecific anticholinergics: l Oxybutynin (Ditropan or Oxytrol) l Tolterodine (Detrol) l Trospium (Sanctura)
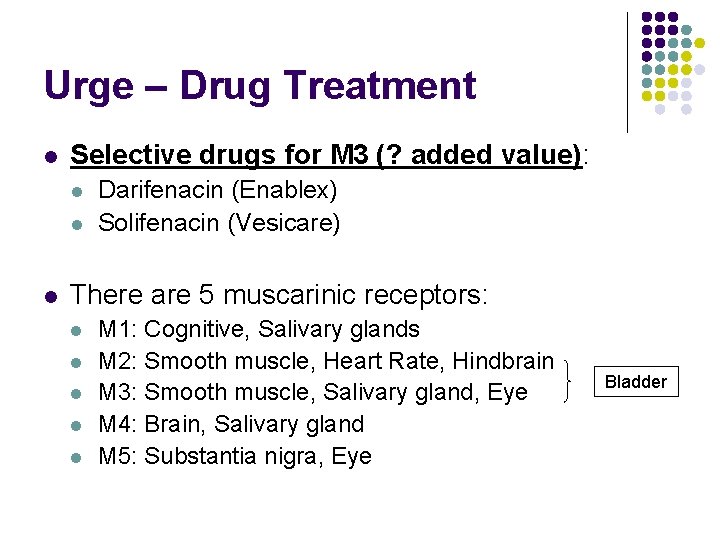
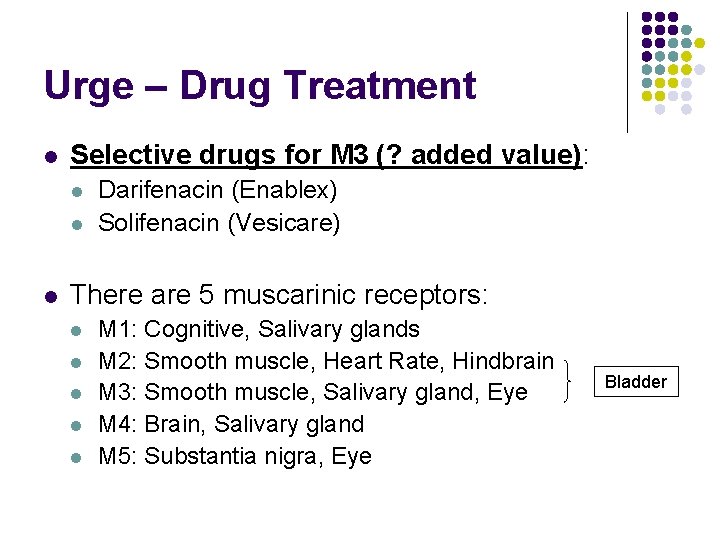
Urge – Drug Treatment l Selective drugs for M 3 (? added value): l l l Darifenacin (Enablex) Solifenacin (Vesicare) There are 5 muscarinic receptors: l l l M 1: Cognitive, Salivary glands M 2: Smooth muscle, Heart Rate, Hindbrain M 3: Smooth muscle, Salivary gland, Eye M 4: Brain, Salivary gland M 5: Substantia nigra, Eye Bladder
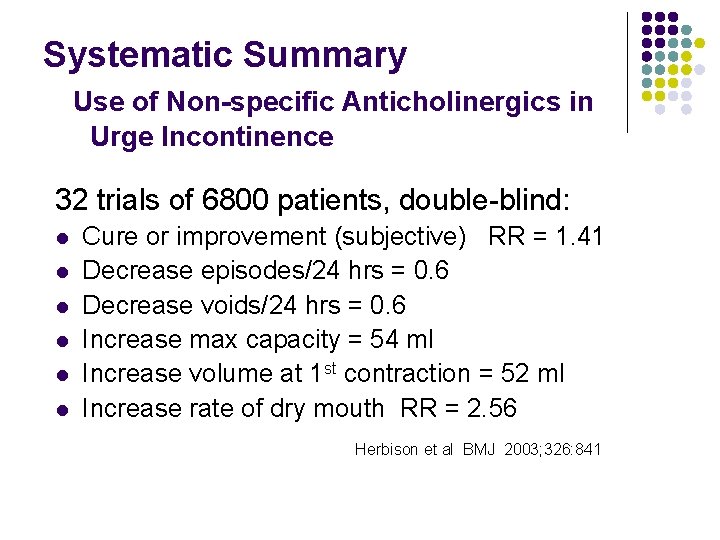
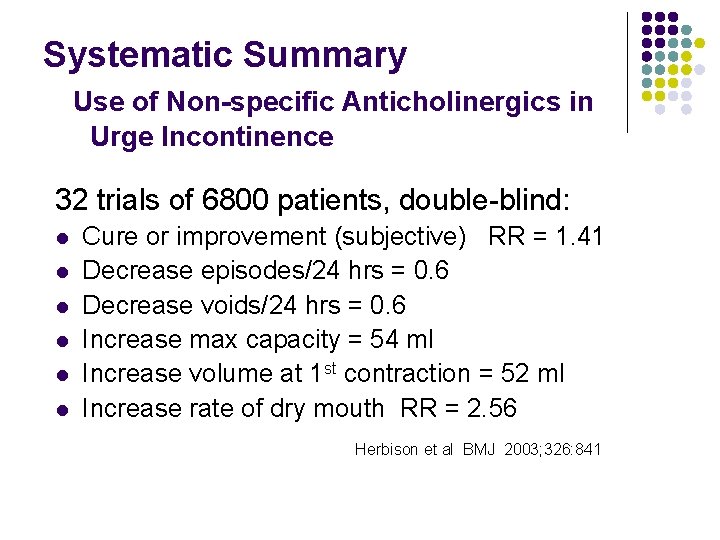
Systematic Summary Use of Non-specific Anticholinergics in Urge Incontinence 32 trials of 6800 patients, double-blind: l l l Cure or improvement (subjective) RR = 1. 41 Decrease episodes/24 hrs = 0. 6 Decrease voids/24 hrs = 0. 6 Increase max capacity = 54 ml Increase volume at 1 st contraction = 52 ml Increase rate of dry mouth RR = 2. 56 Herbison et al BMJ 2003; 326: 841
Urge - Treatment Options Surgical: Sacral nerve neuromodulation Augmentation cystoplasty Palliative: Appropriate products
Product--example Super Brief Medium (34"-47") packaged 28/bag - 56/case Capacity 5. 6 cups Large (48"-59") packaged 28/bag - 56/case Capacity: 7. 6 cups Costs: 45 to 70 cents each
Case 2 Mr. Holdner l l l A 78 -year-old man has longstanding urinary frequency and urgency that has worsened in past month. He often cannot reach the toilet in time and must change clothes once or twice a day. A tremor of the left hand has worsened in the past 2 months. His wife reports that he is lazy and “hardly moves around any more. ” His medical history includes hypertension, hyperlipidemia and coronary artery disease. More
Case 2 continued He has masked facies, diminished arm swing, normal gait, and increased muscle tone and resting tremor on left side l Abdomen and genitalia are normal l Rectal exam shows brown stool in the vault and no evidence of impaction. The prostate seems slightly large, with partial obliteration of the median sulcus, but without nodules or masses l Urinalysis is normal l Plasma glucose and serum calcium levels are normal; serum creatinine is 1. 2 mg/dl l
Which of the following tests is the most appropriate next step in evaluating Mr. Holdner? 1. 2. 3. 4. 5. Urine cytology Serum prostate-specific antigen (PSA) Postvoid residual volume (PVR) Cystometry Voiding diary
Case 2 continued Mr. Holder is found to have a post void residual of 350 ml.
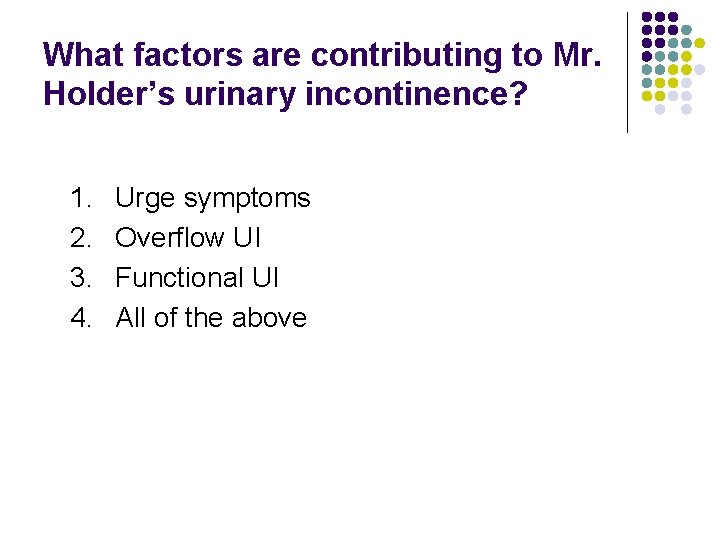
What factors are contributing to Mr. Holder’s urinary incontinence? 1. 2. 3. 4. Urge symptoms Overflow UI Functional UI All of the above
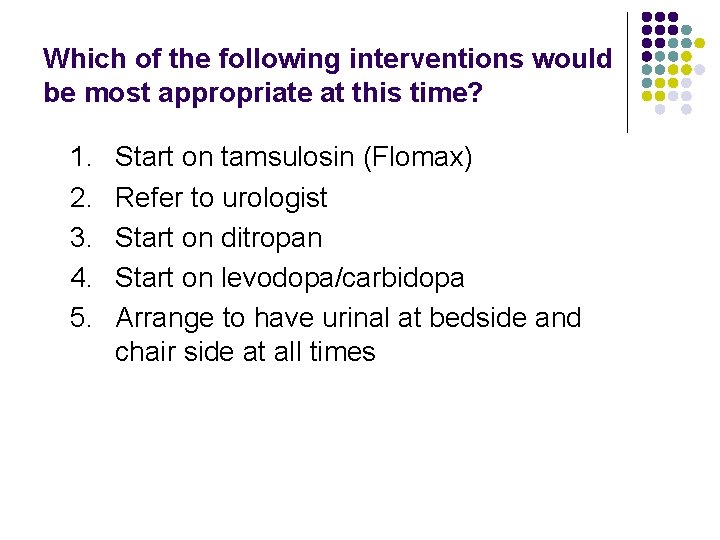
Which of the following interventions would be most appropriate at this time? 1. 2. 3. 4. 5. Start on tamsulosin (Flomax) Refer to urologist Start on ditropan Start on levodopa/carbidopa Arrange to have urinal at bedside and chair side at all times
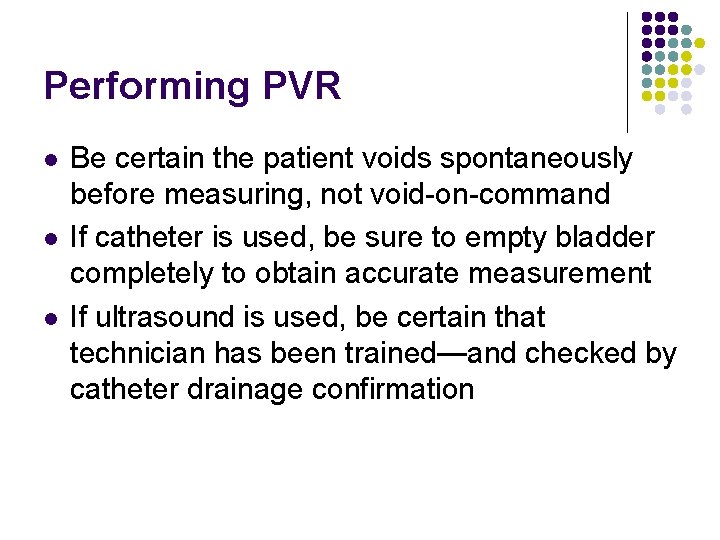
Performing PVR l l l Be certain the patient voids spontaneously before measuring, not void-on-command If catheter is used, be sure to empty bladder completely to obtain accurate measurement If ultrasound is used, be certain that technician has been trained—and checked by catheter drainage confirmation
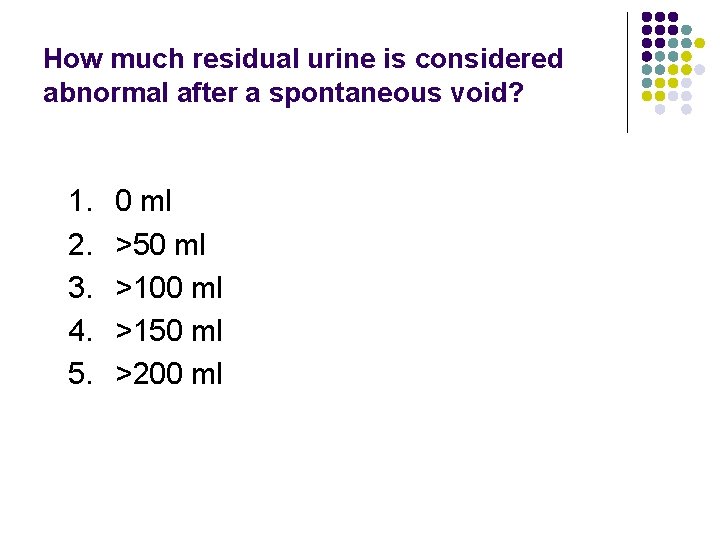
How much residual urine is considered abnormal after a spontaneous void? 1. 2. 3. 4. 5. 0 ml >50 ml >100 ml >150 ml >200 ml
Overflow Incontinence Definition Unpredictable involuntary losses of urine due to overdistention of the bladder Causes Obstructive l Prostatic hypertrophy; urethral stenosis Neurogenic l Spinal cord injury; neuropathy (e. g. , diabetes)
Overflow (continued) Signs and Symptoms l l Involuntary losses of urine, including dribbling, urge and stress symptoms Palpable bladder; large residual volume Treatment l Obstructive: l l Surgical intervention Neurogenic: l l Cholinergic drugs, e. g. , bethanechol (Urecholine) – Rarely effective Intermittent catheterization
Functional Incontinence l Definition Inappropriate urination despite normally functioning bladder and sphincter l Causes Cognitive or emotional: dementia, behavioral Musculoskeletal limitations: strokes, arthritis Environmental barriers: restraints
Functional (continued) l Treatment options for l l Cognitive: routine toileting, habit retraining, behavior modification Non-motivated/depressed: reinforcers, rewards Musculoskeletal: assistance, assistive devices, commode placement Environmental: removal of barriers and restraints, lighting, commode placement
Overview of Management for Urinary Incontinence l Goal: relieve the most bothersome aspect(s) l Correct underlying medical illnesses and medications that may contribute to UI Manage fluid intake: avoid caffeine, alcohol; minimize evening intake Reduce constipation Start with least invasive treatments: l l l behavior - medications - palliation - surgery
Take Away Points l l UI is a common and a serious problem among your patients A careful history and a brief exam can help identify the cause Behavioral treatments are underutilized Anticholinergic drugs are indicated only for urge incontinence
URINARY INCONTINENCE For Practicing Physicians: Part 2 Variables and Pitfalls
Take Away Points l l l Inquiring about incontinence should be included in the review of systems Overactive Bladder Syndrome is common even in the absence of incontinence Drugs used for other purposes may affect the voiding mechanisms Transient causes of incontinence can be distinguished from established types Only selected cases of UI require referral to specialists
Reprise: Persistent Types l l Stress Urge l l Note: “Overactive bladder” may present as urge w/o urinary losses Mixed (often Stress and Urge) Overflow Functional
Transient Causes of UI l History l l l Physical exam l l Drugs Delirium Recent prostatectomy Excessive fluid intake Atrophic vaginitis Fecal impaction Impaired mobility Urinalysis l l Urinary infection Glycosuria
Which of the following medications can contribute to UI? 1. 2. 3. 4. 5. Tamsulosin (Flomax) Diphenhydramine (Benadryl) Pseudoephedrine (Sudafed) Benztropine (Cogentin) All of the above (See accompanying list)
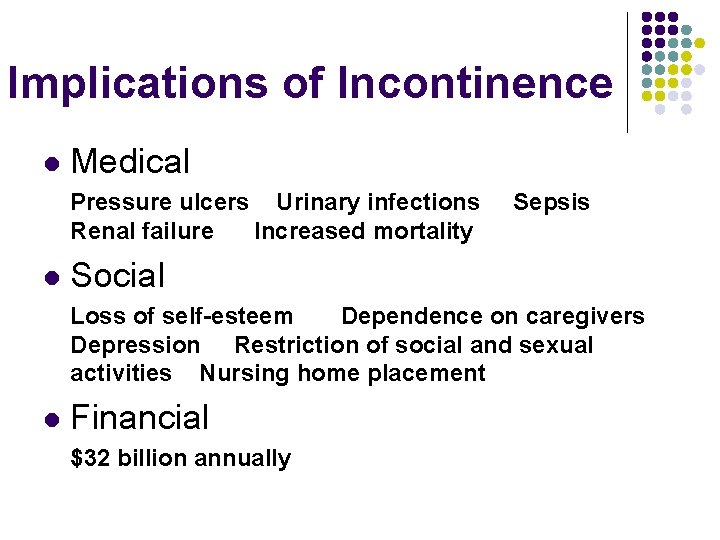
Implications of Incontinence l Medical Pressure ulcers Urinary infections Renal failure Increased mortality l Sepsis Social Loss of self-esteem Dependence on caregivers Depression Restriction of social and sexual activities Nursing home placement l Financial $32 billion annually
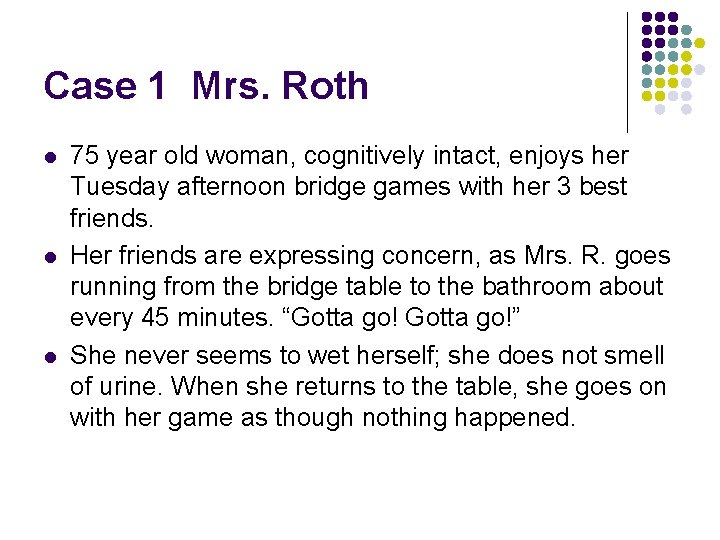
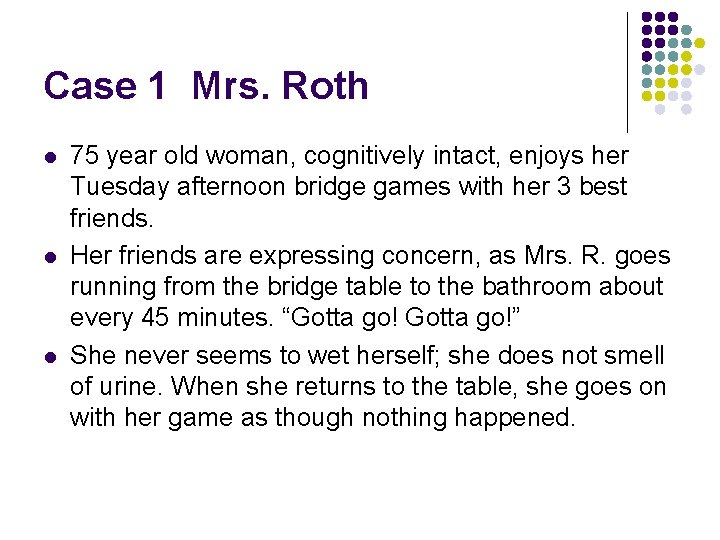
Case 1 Mrs. Roth l l l 75 year old woman, cognitively intact, enjoys her Tuesday afternoon bridge games with her 3 best friends. Her friends are expressing concern, as Mrs. R. goes running from the bridge table to the bathroom about every 45 minutes. “Gotta go!” She never seems to wet herself; she does not smell of urine. When she returns to the table, she goes on with her game as though nothing happened.
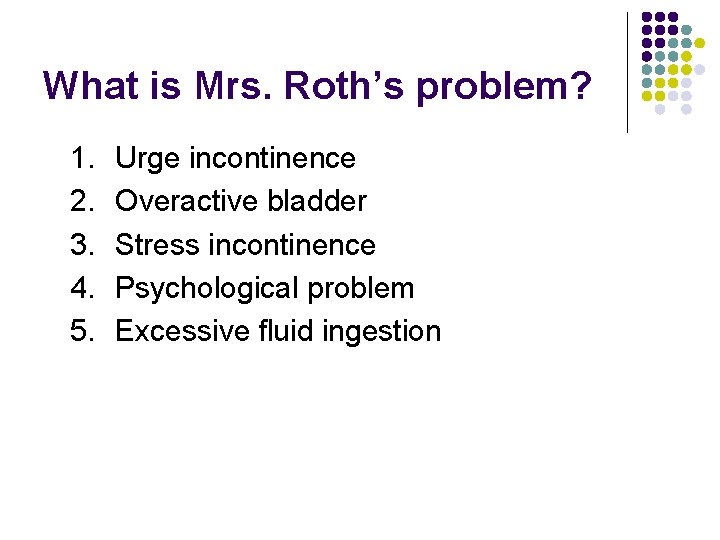
What is Mrs. Roth’s problem? 1. 2. 3. 4. 5. Urge incontinence Overactive bladder Stress incontinence Psychological problem Excessive fluid ingestion
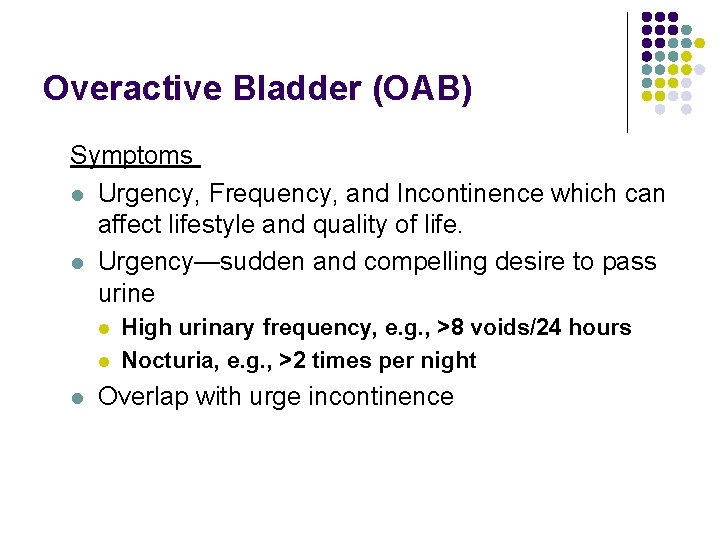
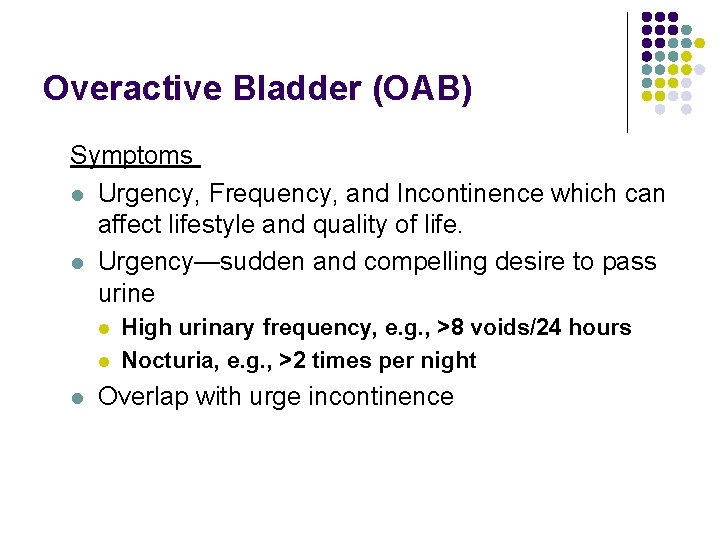
Overactive Bladder (OAB) Symptoms l Urgency, Frequency, and Incontinence which can affect lifestyle and quality of life. l Urgency—sudden and compelling desire to pass urine l l l High urinary frequency, e. g. , >8 voids/24 hours Nocturia, e. g. , >2 times per night Overlap with urge incontinence
Overactive Bladder Your experiences: Are you having many complaints regarding this issue, especially since the direct-to-consumer advertisements have made it so apparent? How do you manage these cases? What kind of results are you having?
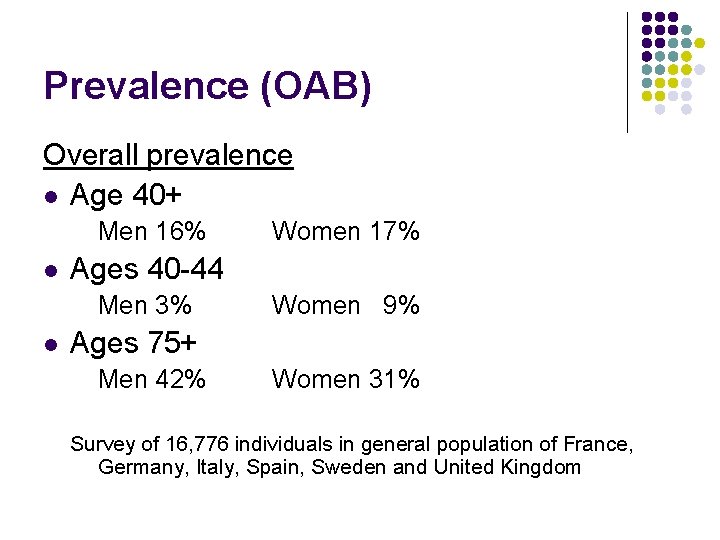
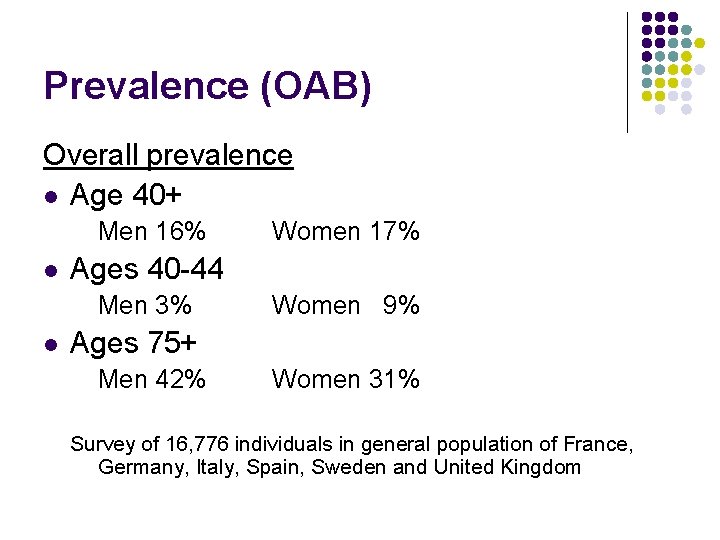
Prevalence (OAB) Overall prevalence l Age 40+ Men 16% l Ages 40 -44 Men 3% l Women 17% Women 9% Ages 75+ Men 42% Women 31% Survey of 16, 776 individuals in general population of France, Germany, Italy, Spain, Sweden and United Kingdom
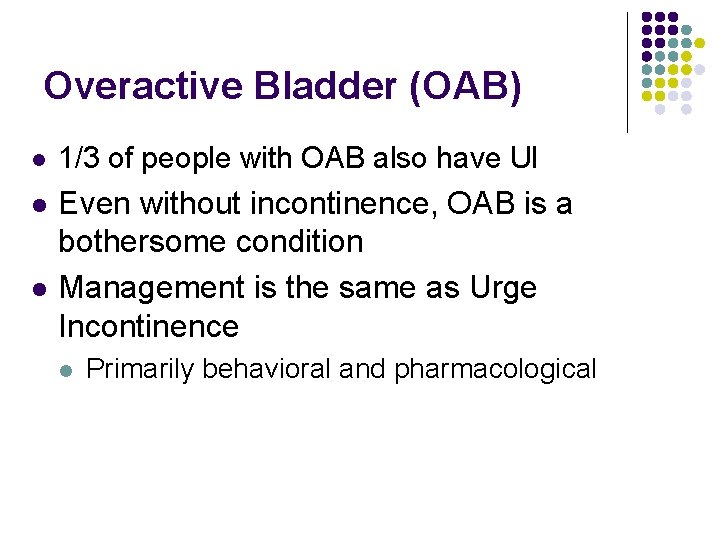
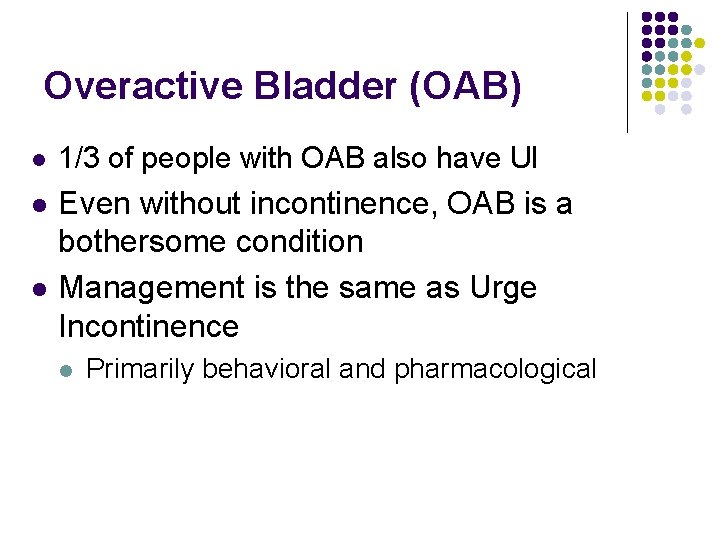
Overactive Bladder (OAB) l 1/3 of people with OAB also have UI l Even without incontinence, OAB is a bothersome condition Management is the same as Urge Incontinence l l Primarily behavioral and pharmacological
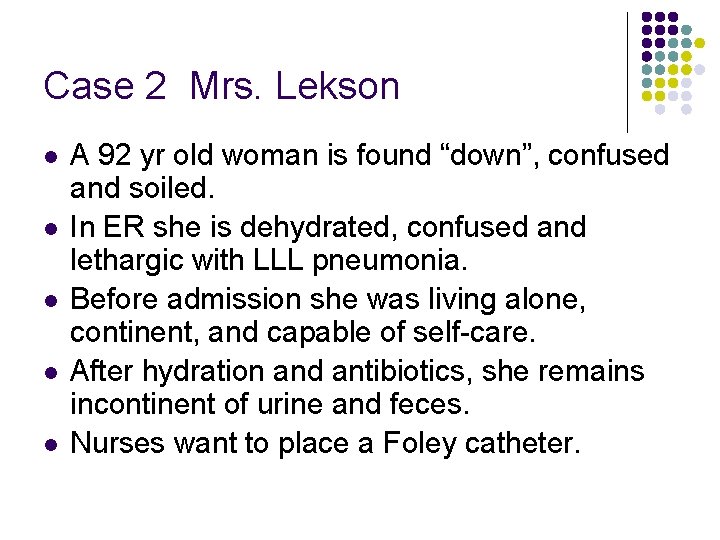
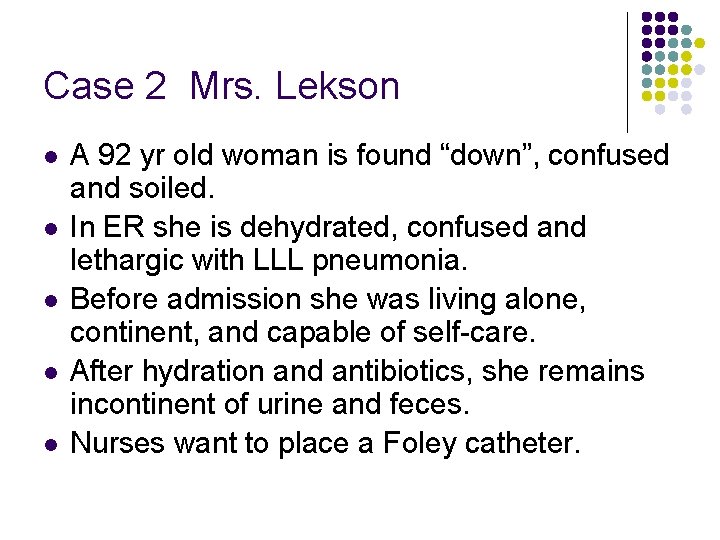
Case 2 Mrs. Lekson l l l A 92 yr old woman is found “down”, confused and soiled. In ER she is dehydrated, confused and lethargic with LLL pneumonia. Before admission she was living alone, continent, and capable of self-care. After hydration and antibiotics, she remains incontinent of urine and feces. Nurses want to place a Foley catheter.
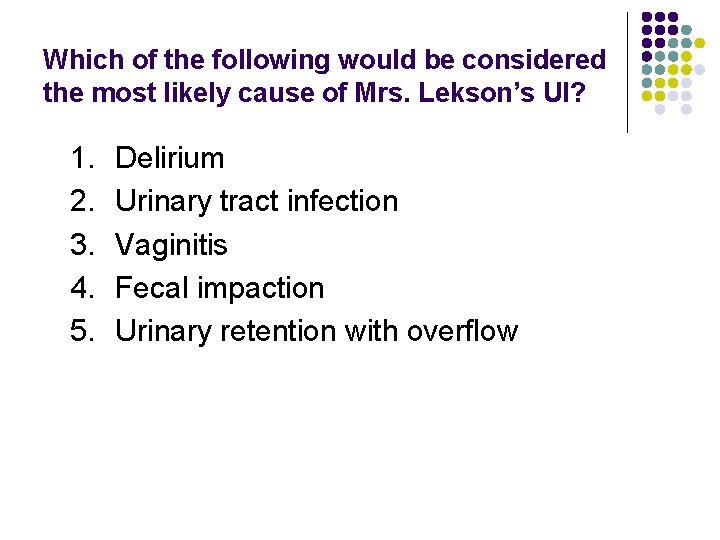
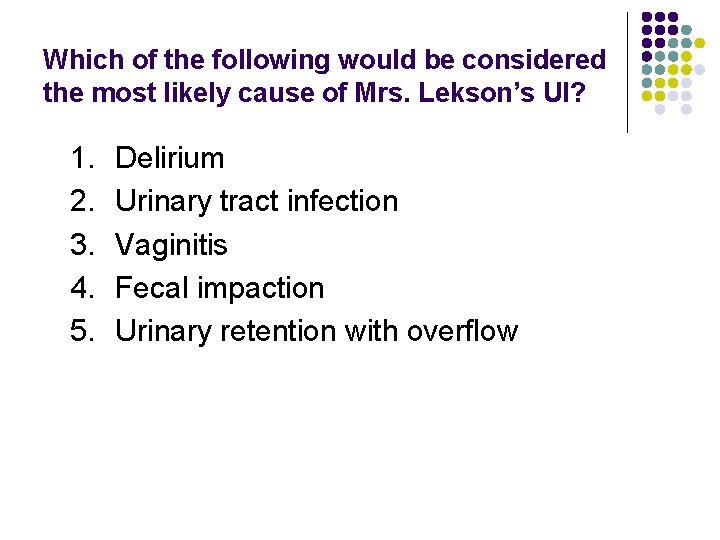
Which of the following would be considered the most likely cause of Mrs. Lekson’s UI? 1. 2. 3. 4. 5. Delirium Urinary tract infection Vaginitis Fecal impaction Urinary retention with overflow
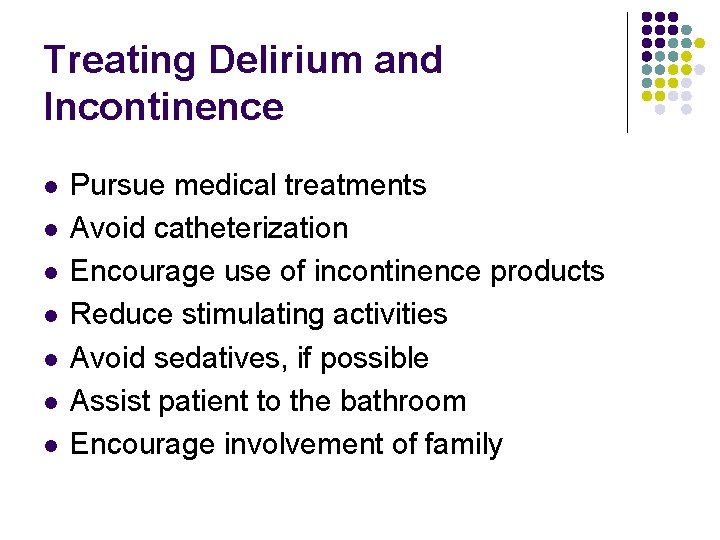
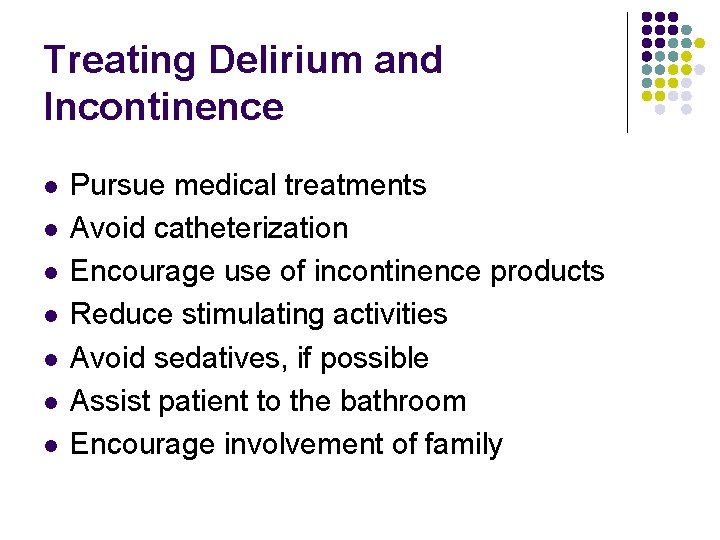
Treating Delirium and Incontinence l l l l Pursue medical treatments Avoid catheterization Encourage use of incontinence products Reduce stimulating activities Avoid sedatives, if possible Assist patient to the bathroom Encourage involvement of family
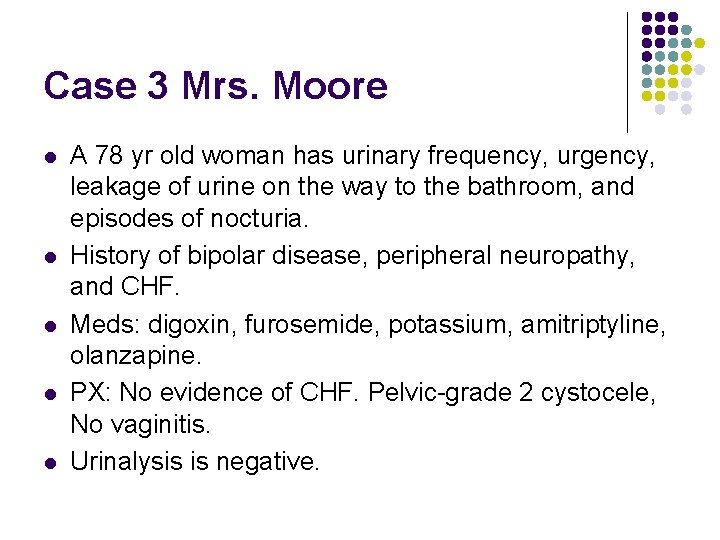
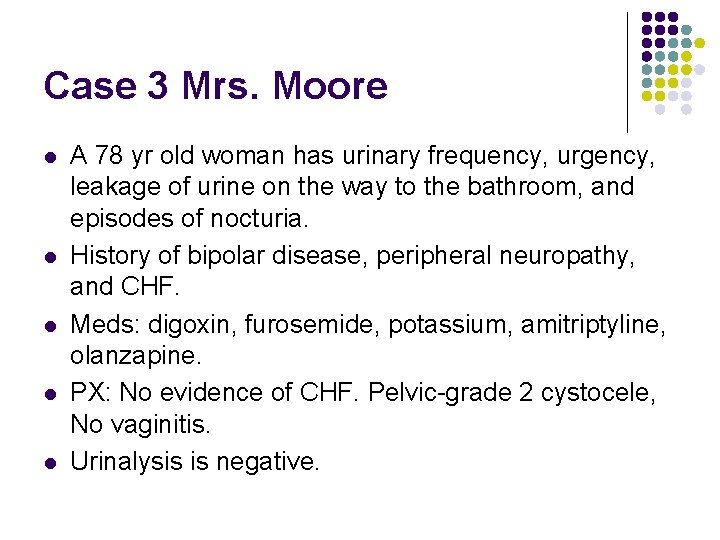
Case 3 Mrs. Moore l l l A 78 yr old woman has urinary frequency, urgency, leakage of urine on the way to the bathroom, and episodes of nocturia. History of bipolar disease, peripheral neuropathy, and CHF. Meds: digoxin, furosemide, potassium, amitriptyline, olanzapine. PX: No evidence of CHF. Pelvic-grade 2 cystocele, No vaginitis. Urinalysis is negative.
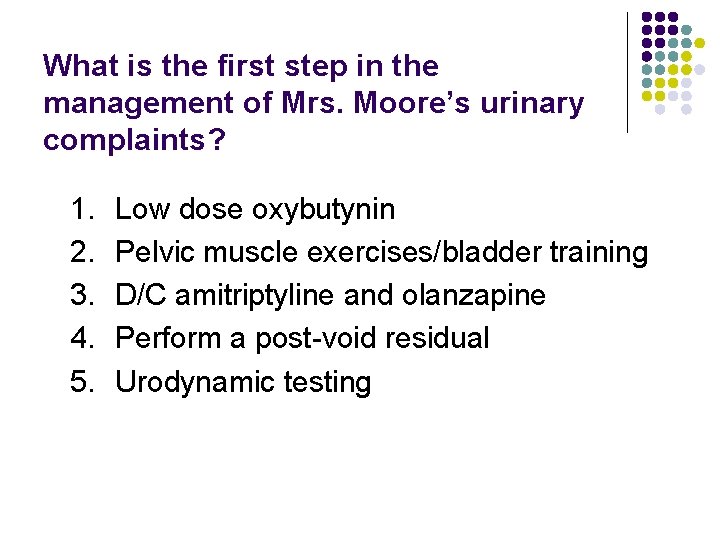
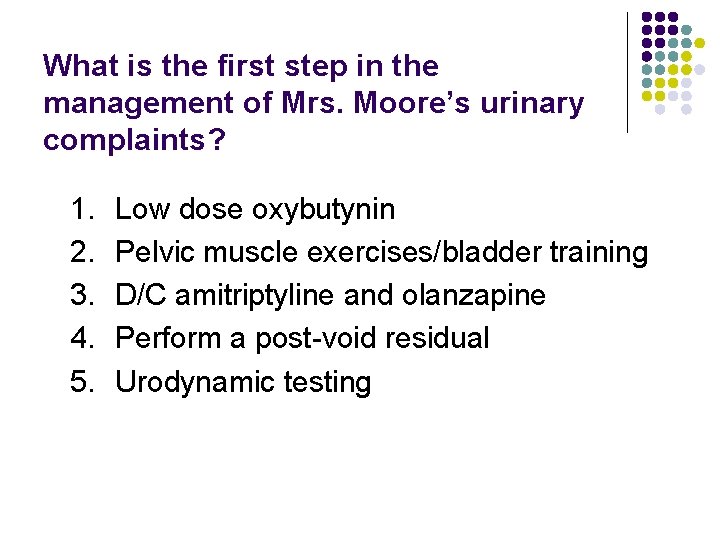
What is the first step in the management of Mrs. Moore’s urinary complaints? 1. 2. 3. 4. 5. Low dose oxybutynin Pelvic muscle exercises/bladder training D/C amitriptyline and olanzapine Perform a post-void residual Urodynamic testing
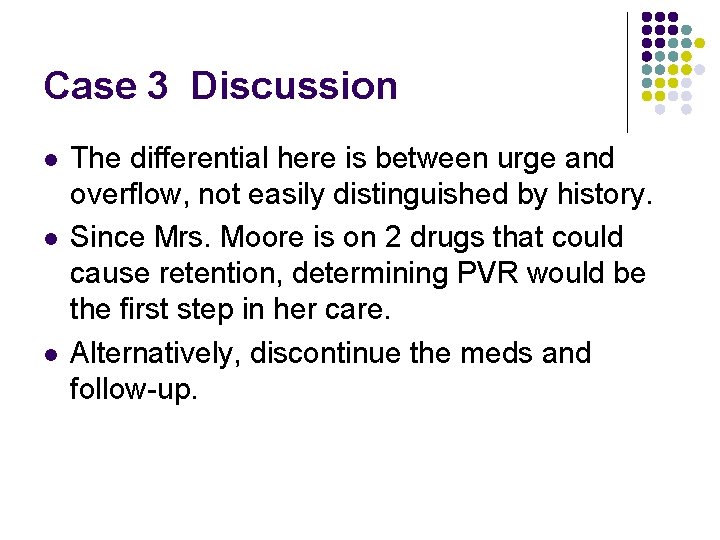
Case 3 Discussion l l l The differential here is between urge and overflow, not easily distinguished by history. Since Mrs. Moore is on 2 drugs that could cause retention, determining PVR would be the first step in her care. Alternatively, discontinue the meds and follow-up.
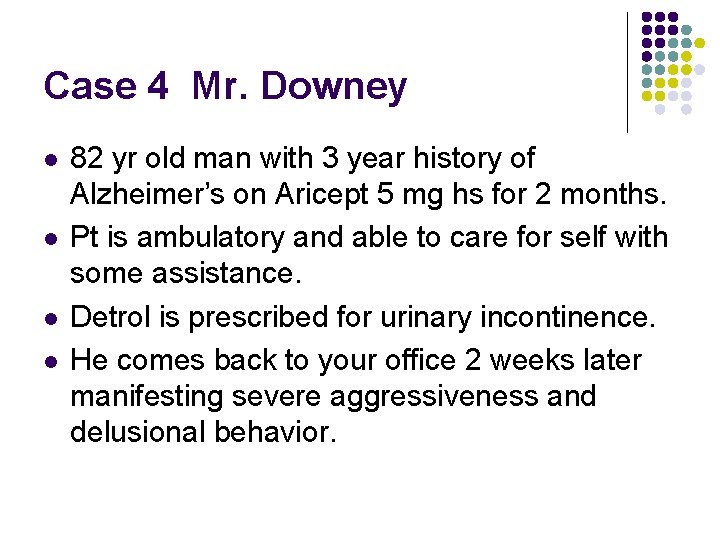
Case 4 Mr. Downey l l 82 yr old man with 3 year history of Alzheimer’s on Aricept 5 mg hs for 2 months. Pt is ambulatory and able to care for self with some assistance. Detrol is prescribed for urinary incontinence. He comes back to your office 2 weeks later manifesting severe aggressiveness and delusional behavior.
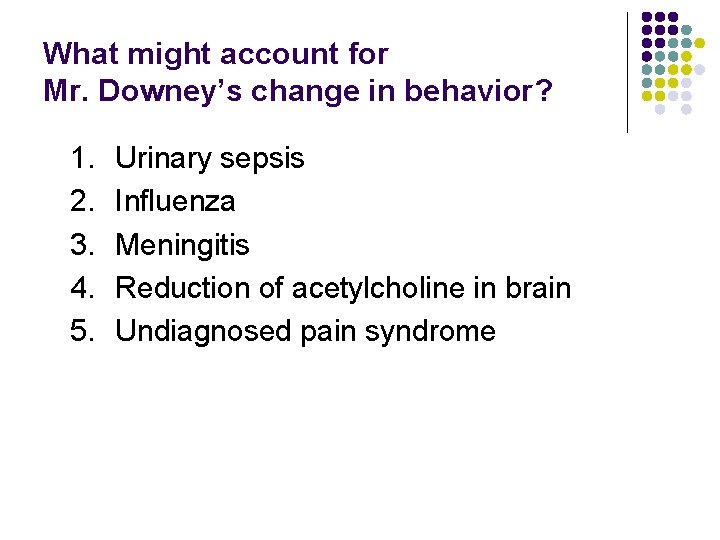
What might account for Mr. Downey’s change in behavior? 1. 2. 3. 4. 5. Urinary sepsis Influenza Meningitis Reduction of acetylcholine in brain Undiagnosed pain syndrome
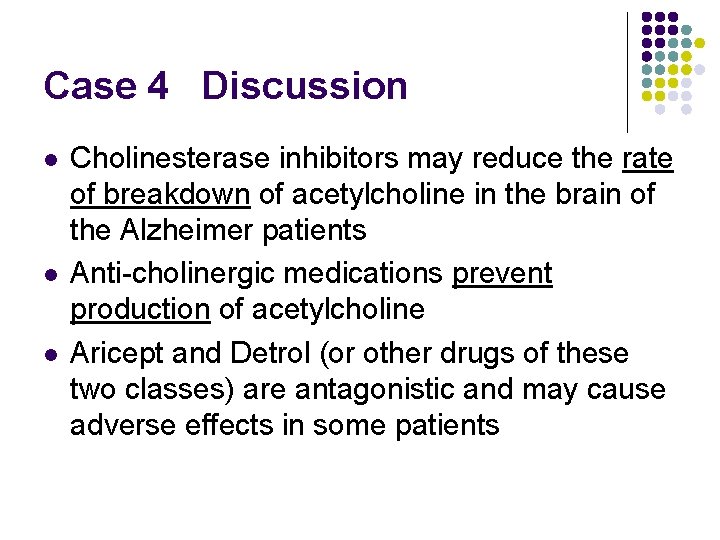
Case 4 Discussion l l l Cholinesterase inhibitors may reduce the rate of breakdown of acetylcholine in the brain of the Alzheimer patients Anti-cholinergic medications prevent production of acetylcholine Aricept and Detrol (or other drugs of these two classes) are antagonistic and may cause adverse effects in some patients
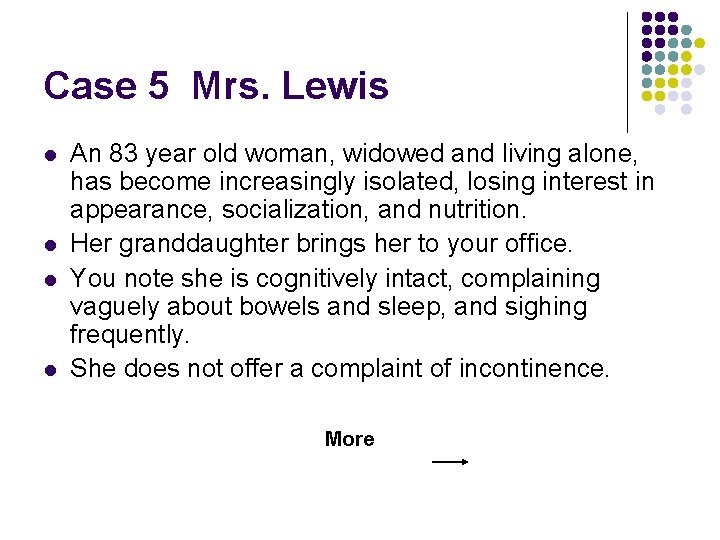
Case 5 Mrs. Lewis l l An 83 year old woman, widowed and living alone, has become increasingly isolated, losing interest in appearance, socialization, and nutrition. Her granddaughter brings her to your office. You note she is cognitively intact, complaining vaguely about bowels and sleep, and sighing frequently. She does not offer a complaint of incontinence. More
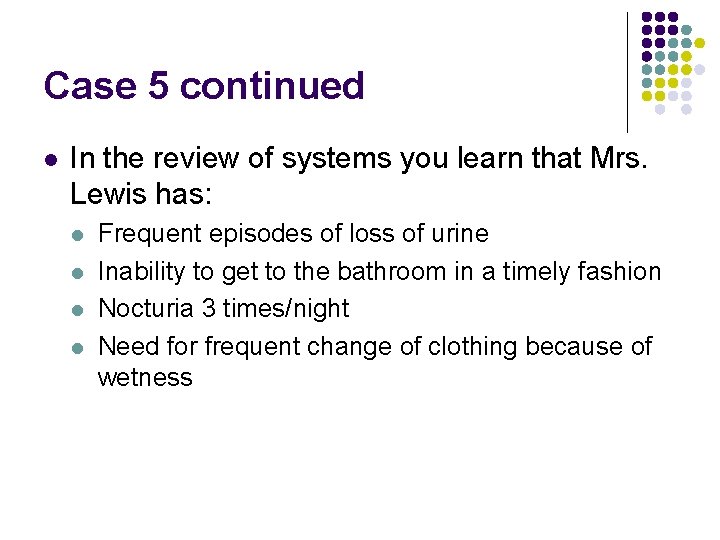
Case 5 continued l In the review of systems you learn that Mrs. Lewis has: l l Frequent episodes of loss of urine Inability to get to the bathroom in a timely fashion Nocturia 3 times/night Need for frequent change of clothing because of wetness
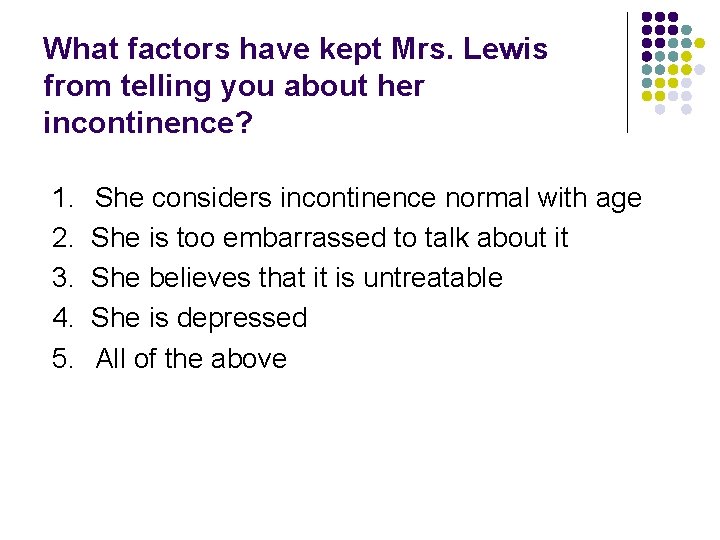
What factors have kept Mrs. Lewis from telling you about her incontinence? 1. 2. 3. 4. 5. She considers incontinence normal with age She is too embarrassed to talk about it She believes that it is untreatable She is depressed All of the above
How would you manage her isolation and depression? 1. 2. 3. 4. 5. Offer antidepressants Offer drug treatment for incontinence Encourage use of urinary products Explain that UI is common and treatable All of the above
Case 6 Mr. Burton An 83 year old man who has: Frequency, urge incontinence and nocturia persisting two months after transurethral resection of the prostate for benign prostatic hypertrophy.
Which of these drugs should be offered? 1. 2. 3. 4. 5. Pseudoephedrine Imipramine Oxybutynin Bethanechol Tamsulosin (Flomax)
Mr. Burton Discussion l l The aging bladder, in both genders, becomes more irritable The prostate, with its “irritative” symptoms, adds a second reason for urgency In this case, the “obstructive” concerns have been relieved, but the urgency persists Treat with appropriate anticholinergics for symptom control
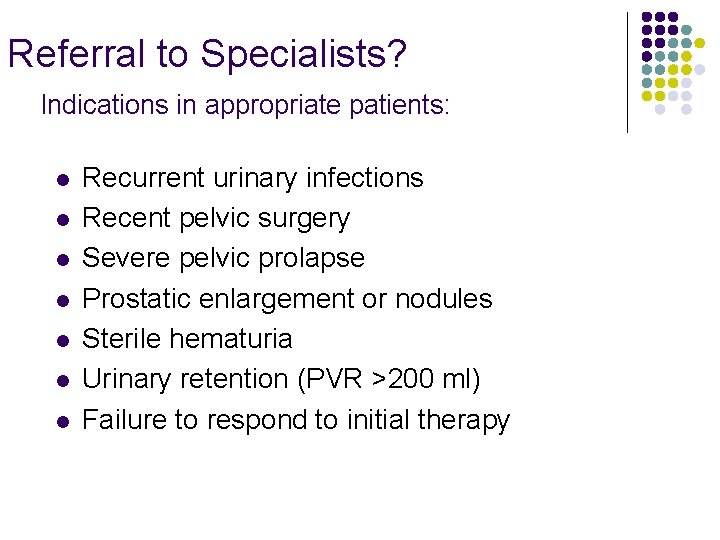
Referral to Specialists? Indications in appropriate patients: l l l l Recurrent urinary infections Recent pelvic surgery Severe pelvic prolapse Prostatic enlargement or nodules Sterile hematuria Urinary retention (PVR >200 ml) Failure to respond to initial therapy
Take Away Points l l l Inquiring about incontinence should be included in the review of systems Overactive Bladder Syndrome is a frequent issue, even in the absence of incontinence Drugs used for other purposes may affect the voiding mechanisms Transient causes of incontinence can be distinguished from established types Only selected cases of UI require referral to specialists
Future considerations in UI l l l Improved diagnostic techniques Better understanding of cellular, myogenic and neurogenic mechanisms Evaluation of newer bladder-specific drugs: l l M 3 specific blockers Resiniferitoxin (RTX)--ultrapotent capsaicin analog for direct instillation into bladder
URINARY INCONTINENCE IS NOT A DIAGNOSIS. . . BUT RATHER IS A SYMPTOM OF AN UNDERLYING PROBLEM.
THE TERMS DEFINING TYPES OF PERSISTENT INCONTINENCE. . . ARE DESCRIPTIVE, AND NOT DIAGNOSTIC
URINARY INCONTINENCE IS NOT SIMPLY A PART OF NORMAL AGING. . . …BUT AGE-RELATED CHANGES PREDISPOSE TO ITS OCCURRENCE.