URINARY CATHETERS DEPARTMENT OF UROLOGY 2006 DIAN L

- Slides: 18
URINARY CATHETERS DEPARTMENT OF UROLOGY 2006 DIAN L KIRSTEIN
CATHETERS • Size • Shape • Material • Retaining mechanism • Lumens
SIZES • Different size systems (External catheter diameter) • Most common: French (F) (Charriere) • 0. 33 mm = 1 F • 3 F = 1 mm, 30 F = 10 mm
CATHETER TYPES • Non self-retaining (Jaques, Robinson, Nelaton) • Self-retaining (Pezzer, Malecot) • Self-retaining 2/3 way balloon Foley Catheter • Postoperative haematuria catheter (rigid)
CONDOM CATHETERS • Men without outflow obstruction and intact voiding reflex pathways • Restricted to selected patients where other measures are unsuccessful

TYPES OF MATERIAL • Latex • Plastic • Silicone coated latex • Silicone • Hydromers (biocath) • Silver-inpregnated • Antibiotic coated
INDICATIONS FOR USE OF URINARY CATHETERS • Diagnostic • Therapeutic • Short-term • Long-term
SHORT-TERM CATHETERIZATION • Acute urinary retention • Urine collection (U mcs, residual volume) • Urologic surgery • Surgery on contiguous structures • Urine output (medical, surgical) • Urodynamic studies • Radiology ( cystogram) • Installation of antibiotics, immunotherapy etc
LONG-TERM CATHETERIZATION • Refractory urine retention – not correctable medically or surgically • Neurogenic bladder – some • Incontinence – non-responders to specific treatment – terminally ill, severely impaired – intractable skin breakdown
TECHNIQUE • Inform patient - explain procedure • NB aseptic • Prepare • Indication • Size: “narrowest, softest tube that will serve the purpose”
PREPARATION • Position patient • Expose • Open set using sterile technique • Wash hands and don sterile gloves • Test catheter balloon • Attach drainage bag to catheter • Lubricate catheter (local anesthetic lubricant) • Clean
CATHETERIZATION • Aseptic • Place catheter (urine? ) • Inflate balloon (5 ml) • Gently pull back on catheter • Tape tubing to thigh • Position bag to facilitate drainage by gravity • NB: retract foreskin
CLOSED DRAINAGE SYSTEM • “Open drainage system”: – 95% bacteriuria prevalence in 4 days • “Closed”: – 5% per day risk, 40% by day 10 • Risk increases: – changing the catheter bags – taking urine samples – bladder washout regimes
SUPRAPUBIC CATHETER INDICATIONS • Failed urethral catheterization • Urethral disruption • Long-term bladder drainage
SUPRAPUBIC CATHETER CONTRA-INDICATIONS • Non-palpable bladder • Previous lower abdominal surgery • Coagulopathy • Known bladder tumour • Clot retention
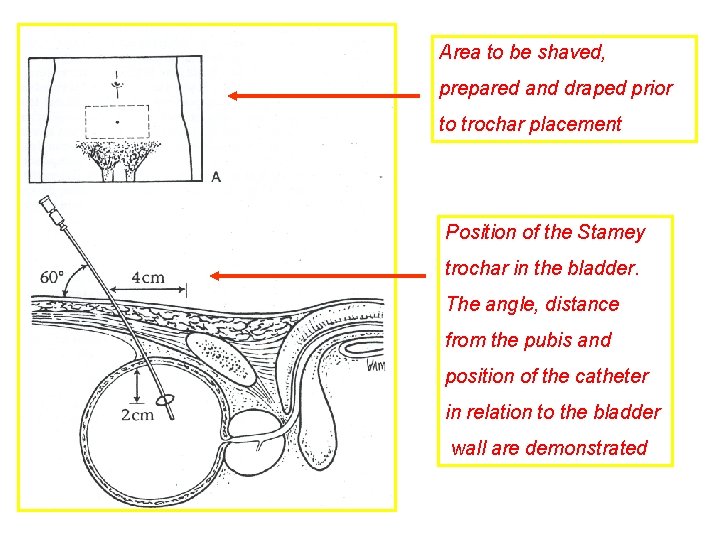
SUPRAPUBIC CATHETER TECHNIQUE • Informed consent • Supine position • Confirm full bladder • Prepare suprapubic area • Anesthetize: skin, sub-cutaneous tissue to the anterior bladder wall • Confirm distance to full bladder by aspiration
TECHNIQUE • Plan angle and depth of puncture • Stab wound • Cystostomy trocar • Fixate catheter
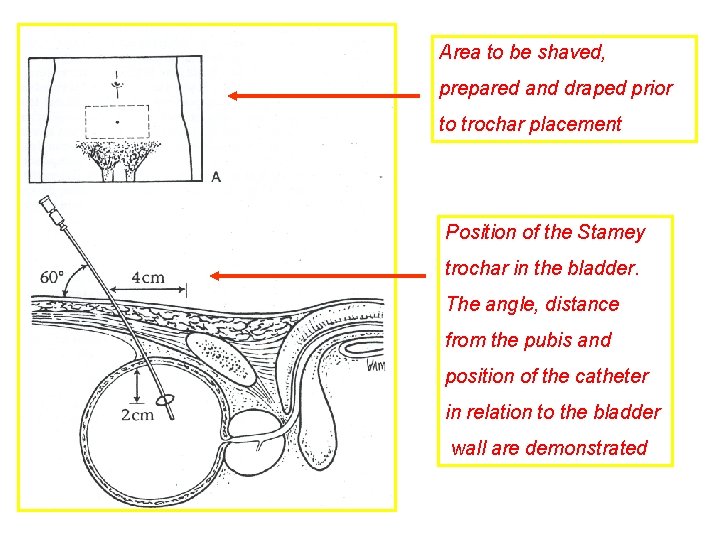
Area to be shaved, prepared and draped prior to trochar placement Position of the Stamey trochar in the bladder. The angle, distance from the pubis and position of the catheter in relation to the bladder wall are demonstrated