Urethral Injuries Ahmed S Zugail Urology House Officer






























- Slides: 56
Urethral Injuries Ahmed S. Zugail Urology House Officer
Case: • 26 year old . • Medically free. • Sudanese. • MVC (pedestrian). • ER 16/11. • Urethral meatus bleeding. • Lower abdominal pain. • Acute urinary retention.

• No past medical or surgical history. • Smoker. • Jeddah. • ABCDE. • Surgical and orthopedic consultation. • O/E • Vitally normal. • Blood at meatus. • Suprapubic tenderness.
• CXR, Pelvic X-ray & CT. • Retrograde urethrogram. • Suprapubic catheter. • Admission on 16/10. • Passed clots with small amount of urine 17/10.







• CT 19/10: • Cystogram. • Arterial phase. • Delayed phase.




• Flexible cystoscopy with urethral catheter insertion. • Dischared Home 22/10 • F/U Retrograde urethrogram 22/11. • Remove catheter in OR then cystoscopy 3/1/2012.




Etiology: • • • Well-defined events. Major blunt trauma 90%. 1 Penetrating injuries. Straddle injuries. Iatrogenic injury. Dixon CM. Diagnosis and acute management of posterior urethral disruptions. In: Mc. Aninch JW, ed. Traumatic and Reconstructive Urology. Philadelphia, Pa: WB Saunders; 1996: 347 -55. 1

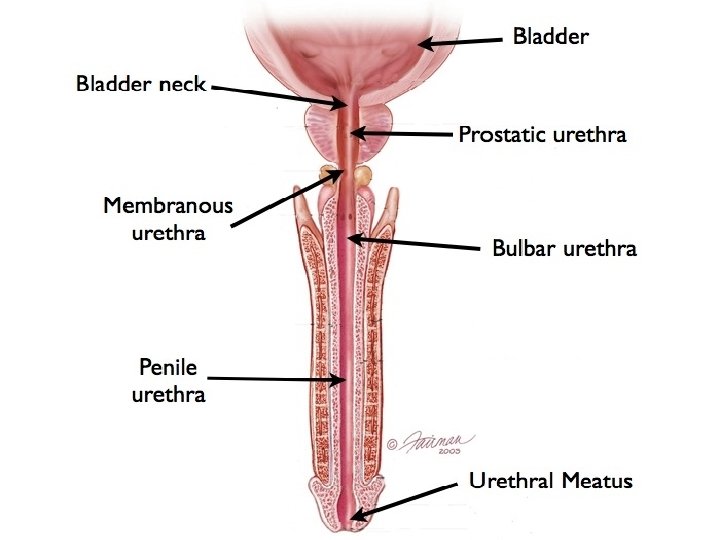
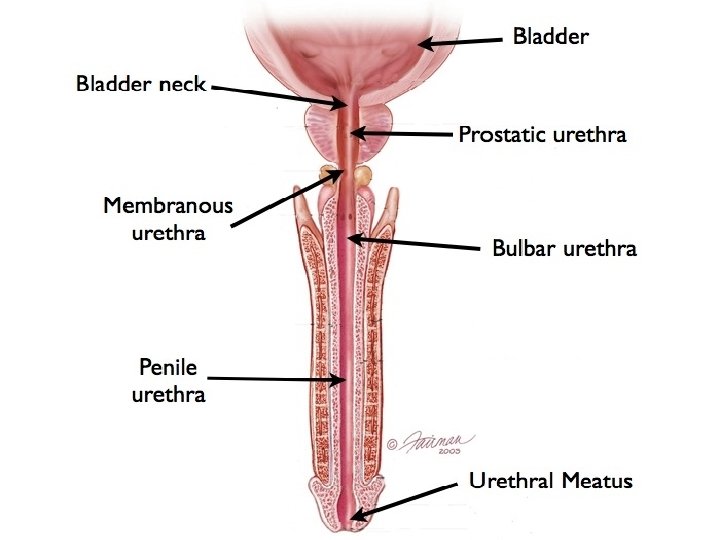
• The Bulbomembranous junction is more vulnerable to injury during pelvic fracture than is the prostatomembranous junction (Colapinto and Mc. Callum, 1977; Brandes and Borelli, 2001).
• In children, injuries are more likely to extend proximally to the bladder neck because of the rudimentary nature of the prostate (Devine et al, 1989; Al. Rifaei et al, 1991; Boone et al, 1992).

Iatrogenic injury to the urethra: • The majority of iatrogenic lesions are the result of improper or prolonged catheterization. • They are surprisingly common and account for 32% of urethral strictures. Of these, 52% affect the bulbar and/or prostatic urethra. 2 2 Fenton AS, Morey AF, Aviles R, Garcia CR. Anterior urethral stricture: etiology and characteristics. Urology 2005 Jun; 65(6): 1055 -8 (level of evidence 3).
• Iatrogenic urethral trauma caused by transurethral surgery Transurethral procedures, especially transurethral resection of the prostate (TUR-P), are the second most common cause of iatrogenic urethral lesions. 3 3 Vicente J, Rosales A, Montlleó M, Caffaratti J. Value of electrical dispersion as a cause of urethral stenosis after endoscopic surgery. Eur Urol 1992; 21(4): 280 -3.

Frequency: • Posterior urethral injuries’ incidence is 510% associated with pelvic fracture with an annual rate of 20: 100000. 4 Dixon CM. Diagnosis and acute management of posterior urethral disruptions. In: Mc. Aninch JW, ed. Traumatic and Reconstructive Urology. Philadelphia, Pa: WB Saunders; 1996: 347 -55. 4

• The male posterior urethra is injured in 4 -19% and the female urethra in 0 -6% of all pelvic fractures. 5 5 Koraitim MM, Marzouk ME, Atta MA, Orabi SS. Risk factors and mechanism of urethral injury in pelvic fractures. Br J Urol 1996 Jun; 77(6): 876 -80 (level of evidence: 2 b).
• Anterior urethral injuries actual incidence is difficult to determine because they are seldom diagnosed emergently. • Penetrating injury to the urethra is rare.
Presentation: • Blood at the meatus. • Inability to urinate. • Palpably full bladder. • High-riding prostate. • Perineal hematoma. • Vulvar edema. • Blood at the vaginal introitus. • Failure to pass a foley catheter.

• Blood at the meatus is present in 3793% of patients with posterior urethral injury 6, and in at least 75% of patients with anterior urethral injury. 7 Lim PH, Chng HC. Initial management of acute urethral injuries. Br J Urol 1989 Aug; 64(2): 165 -8 (level of evidence: 3). 7 Mc. Aninch JW. Traumatic injuries to the urethra. J Trauma 1981 Apr; 21(4): 291 -7 (level of evidence: 3). 6
• Blood at the vaginal introitus is present in more than 80% of female patients with pelvic fractures and co-existing urethral injuries. 8
• The symptoms of urethral injury caused by improper catheterisation or use of instruments are: • Penile and/or perineal pain (100%) • Urethral bleeding (86%). 8 8 Perry MO, Husmann DA. Urethral injuries in female subjects following pelvic fractures. J Urol 1992 Jan; 147(1): 139 -43 (level of evidence 2 b).

Imaging Studies: 1 - Retrograde urethrography: It is performed using gentle injection of 2030 m. L of contrast into the urethra. Examination is made for extravasation, which pinpoints the existence and location of the urethral tear.
• Direct inspection by urethroscopy is suggested in lieu of urethrography in females with suspected urethral injury (Perry and Husmann, 1992; Koraitim, 1999).
2 - Cystography: • Exclude bladder injury in the acute setting (static cystography). • Voiding cystography (performed through the suprapubic catheter) demonstrates the bladder neck and prostatic urethral anatomy when a delayed repair is being considered and for surgical planning.
3 - Computerized tomography: may miss lower urinary tract injuries and thus missing the suspicion for further evaluating studies of urethral injuries. 9 9 Lawson CM, Daley BJ, Ormsby CD, Enderson B. Missed injuries in the era of the trauma scan. J Trauma. Feb, 2011; 70: 452 -6.
4 - Magnetic Resonance Imaging: has been used successfully to define defect length and to determine the extent and direction of urethral dislocation and the extent of prostatic displacement, and it may help in planning the surgical approach. (Dixon et al, 1992) and (Koraitim and Reda, 2007).

Diagnostic Procedure: Cystoscopy: • A valuable tool in the evaluation of a male urethral injury. • The feasibility of early endoscopic realignment can be determined especially in the acute setting.
• The combination of the imaging studies “up and down-o-gram” and cystoscopy gives a more accurate estimation of the stricture length which facilitates decisions in operative strategy.

Management

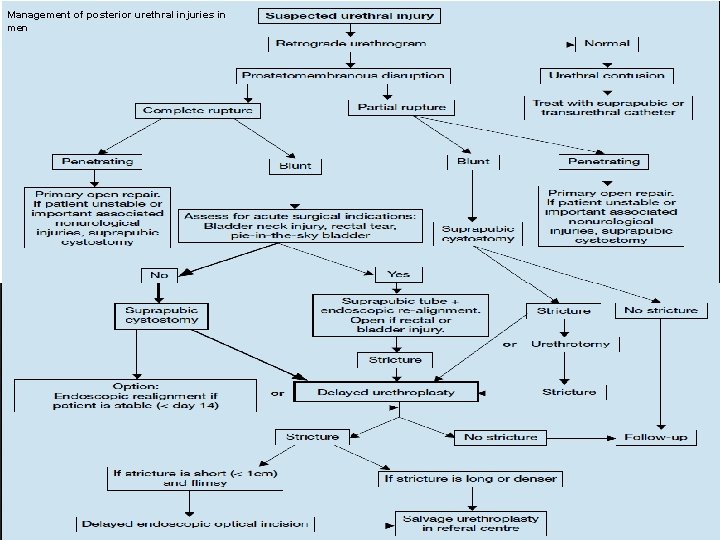
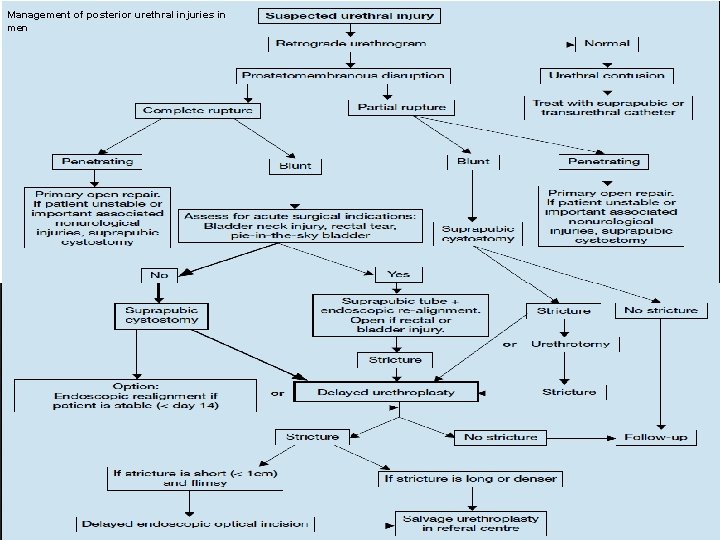
Management of posterior urethral injuries in men
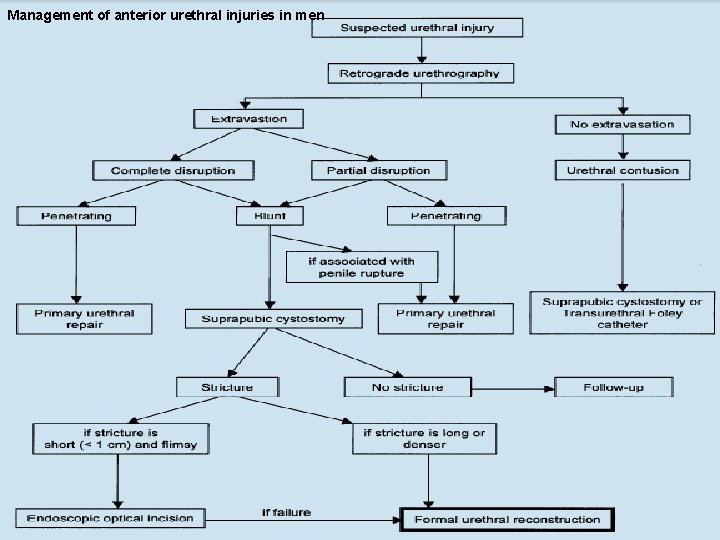
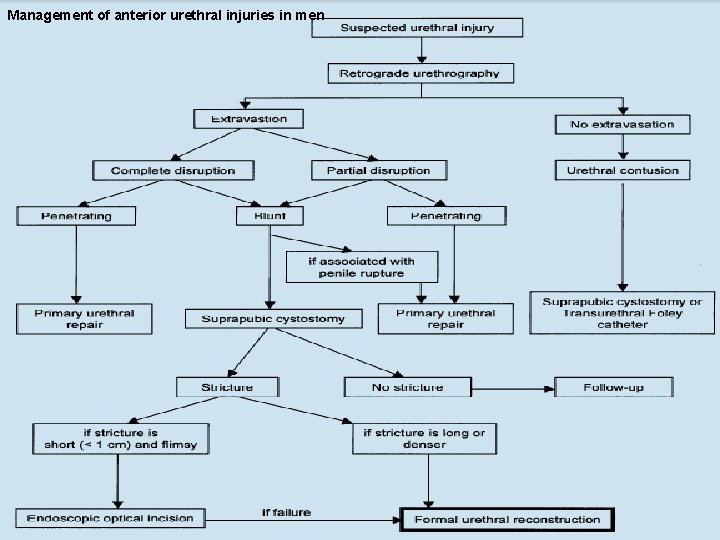
Management of anterior urethral injuries in men

Management of urethral injuries in women

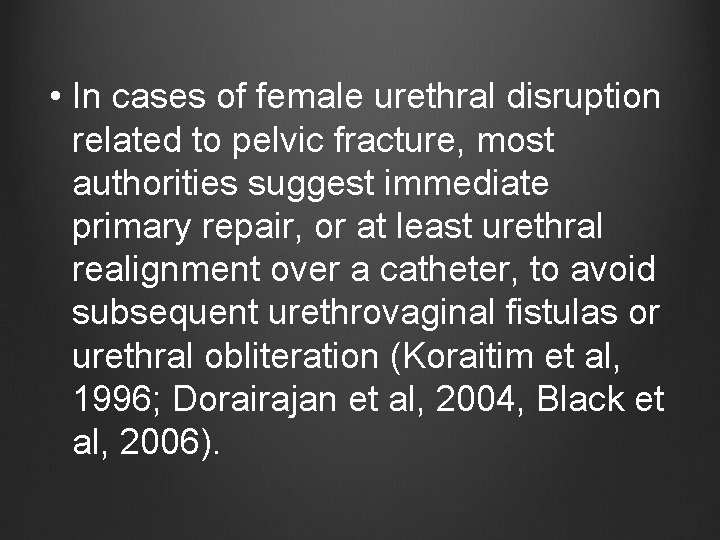
• In cases of female urethral disruption related to pelvic fracture, most authorities suggest immediate primary repair, or at least urethral realignment over a catheter, to avoid subsequent urethrovaginal fistulas or urethral obliteration (Koraitim et al, 1996; Dorairajan et al, 2004, Black et al, 2006).
• Incomplete urethral tears are best treated by stenting with a urethral catheter. The authors and others (Al-Ali and Husain, 1983; Mundy, 1991; Kotkin and Koch, 1996) have not seen any evidence that a gentle attempt to place a urethral catheter can convert an incomplete into a complete transection.
Complications: • Erectile Dysfunction. • Recurrent Stenosis/Stricture. • Incontinence.

• Some degree of impotence is noted in up to 82% of patients with pelvic fracture and urethral distraction injury (Flynn et al, 2003). • Although the average reported rate is approximately 50% (Corriere et al, 1994; Routt et al, 1996; Elliott and Barrett, 1997; Asci et al, 1999; Koraitim, 2005).

• The etiology is multifactorial and variably attributed to cavernous nerve injury, arterial insufficiency, venous leak, and direct corporeal injury (Narumi et al, 1993; Munarriz et al, 1995; Shenfeld et al, 2003).
• The risk of impotence caused by delayed urethroplasty is about 5% and the rate of incontinence is about 4%.

Thank you
 Ahmed muhudiin ahmed
Ahmed muhudiin ahmed Erythema urethral meatus
Erythema urethral meatus External urethral orifice
External urethral orifice Gram positive cocci in urethral discharge
Gram positive cocci in urethral discharge External urethral orifice
External urethral orifice Urethral sphincter
Urethral sphincter Erythema urethral meatus
Erythema urethral meatus V
V Uterus perimetrium
Uterus perimetrium Metaphyseal
Metaphyseal Priapisml
Priapisml Vas deferens
Vas deferens Shape of urethral suppository
Shape of urethral suppository Urogenital sinus
Urogenital sinus L
L Suppository types
Suppository types Refhelp urology
Refhelp urology Urology match
Urology match Srmc urology
Srmc urology Hidrocele y varicocele
Hidrocele y varicocele Pediatric urologist salary
Pediatric urologist salary Urology match
Urology match Usc
Usc Dr donaldson urology
Dr donaldson urology Urology coding cheat sheet
Urology coding cheat sheet Rpug in urology
Rpug in urology Hymen
Hymen Laura oakley
Laura oakley Ubc urology
Ubc urology Children urology
Children urology Sports injuries angus, on
Sports injuries angus, on Miniscus replacement
Miniscus replacement Climatic injury
Climatic injury 17:4 providing first aid for shock
17:4 providing first aid for shock The hunger games chapter 24 questions and answers
The hunger games chapter 24 questions and answers Hunger games comprehension questions
Hunger games comprehension questions Injuries first aid
Injuries first aid Chapter 13 worksheet recognizing different sports injuries
Chapter 13 worksheet recognizing different sports injuries Chapter 13:2 preventing accidents and injuries
Chapter 13:2 preventing accidents and injuries Kristen wilson injuries
Kristen wilson injuries Human crutch/two-person drag
Human crutch/two-person drag Tendon injuries clinton
Tendon injuries clinton Biomechanics throwing football
Biomechanics throwing football Preventing hand injuries
Preventing hand injuries Define intentional fallacy
Define intentional fallacy Jsp539
Jsp539 Emr chapter 15 injuries to muscles and bones
Emr chapter 15 injuries to muscles and bones Sentinel injuries in infants are
Sentinel injuries in infants are How are sports injuries classified and managed
How are sports injuries classified and managed Characters of firearm injuries
Characters of firearm injuries Chapter 4 basics of tissue injuries
Chapter 4 basics of tissue injuries Pallet jack injuries
Pallet jack injuries Chapter 11 injuries to the shoulder region
Chapter 11 injuries to the shoulder region A short backboard or vest-style immobilization
A short backboard or vest-style immobilization Why does atticus ask bob ewell to write his name?
Why does atticus ask bob ewell to write his name? Beck weathers injuries
Beck weathers injuries Injury prevention safety and first aid
Injury prevention safety and first aid