UPPER RESPIRATORY TRACT INFECTION Dr Sarika Gupta MD


- Slides: 15

UPPER RESPIRATORY TRACT INFECTION Dr Sarika Gupta (MD, Ph. D); Asst. Professor
v v v v v 1. Croup 2. Epiglottitis 3. Bacterial tracheitis 4. Acute infectious laryngitis 5. Spasmodic croup 6. Common Cold 7. Otitis Media 8. Sinusitis 9. Pharyngitis/Tonsillitis
CROUP v v v v Laryngotracheobronchitis Early childhood viral syndrome Most common age group is 3 m – 5 years , peak in 2 nd year Boys Winter season The parainfluenza viruses (type 1, 2 and 3) account for 75% others – influenza A, B , adenovirus , measles , RSV, rhinovirus, coronavirus and human metapneumovirus.
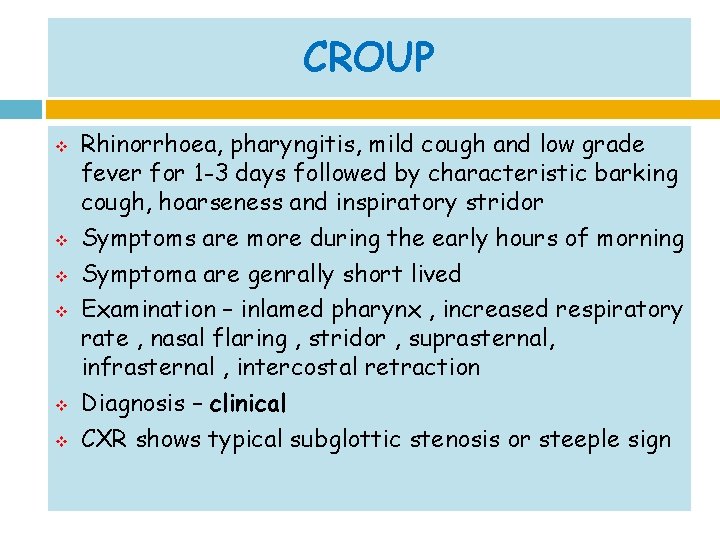
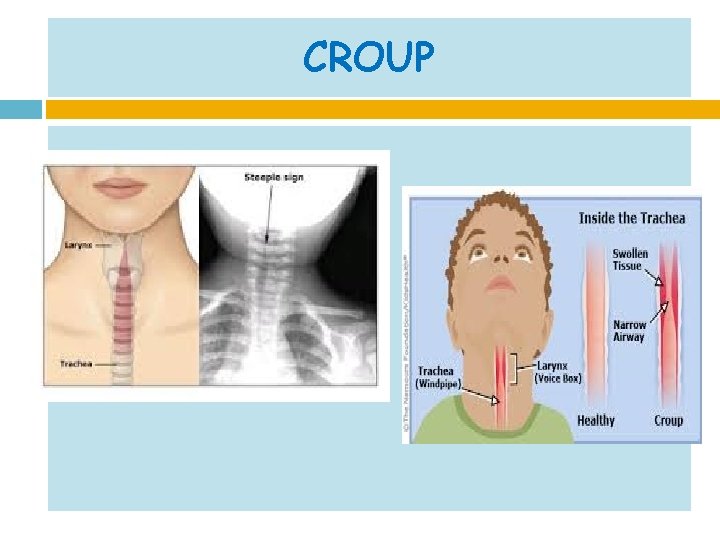
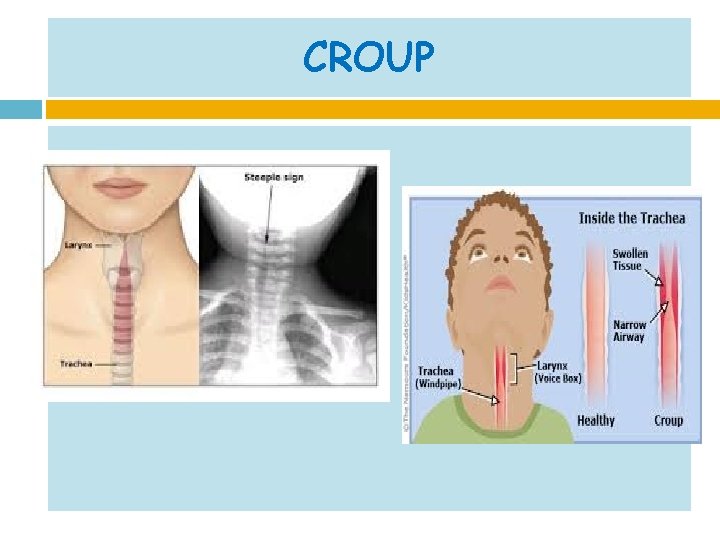
CROUP v v v Rhinorrhoea, pharyngitis, mild cough and low grade fever for 1 -3 days followed by characteristic barking cough, hoarseness and inspiratory stridor Symptoms are more during the early hours of morning Symptoma are genrally short lived Examination – inlamed pharynx , increased respiratory rate , nasal flaring , stridor , suprasternal, infrasternal , intercostal retraction Diagnosis – clinical CXR shows typical subglottic stenosis or steeple sign
CROUP
CROUP v v v Differential diagnosis: 1. Reteropharyngeal or peritonsillar abscess 2. Angioneurotic edema 3. Allergic reaction 4. Foreign body 5. Laryngeal diphtheria
CROUP v v v Treatment: 1. Reduce agitation 2. Airway management 3. Treatment of hypoxia- BLOW by oxygen 4. Single dose of 0. 6 mg/kg of oral / im dexamethasone 5. Nebulised epinephrine
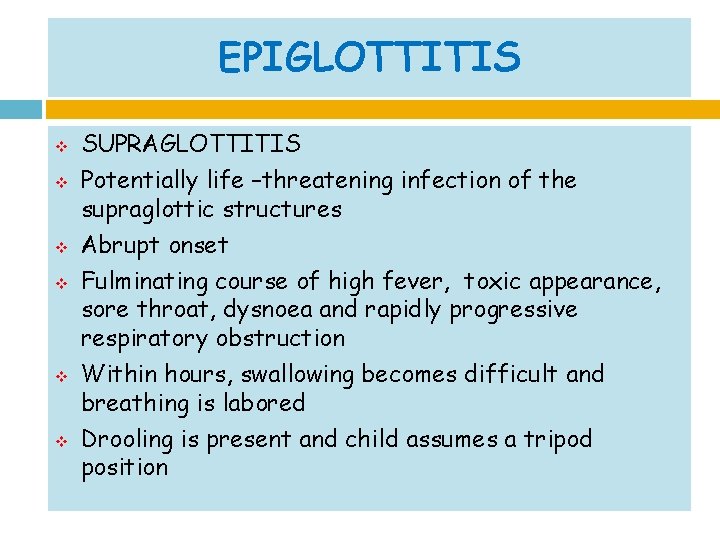
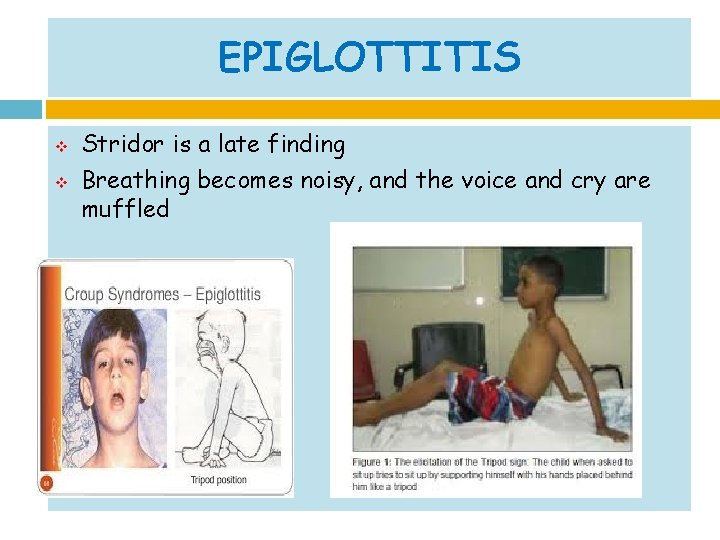
EPIGLOTTITIS v v v SUPRAGLOTTITIS Potentially life –threatening infection of the supraglottic structures Abrupt onset Fulminating course of high fever, toxic appearance, sore throat, dysnoea and rapidly progressive respiratory obstruction Within hours, swallowing becomes difficult and breathing is labored Drooling is present and child assumes a tripod position
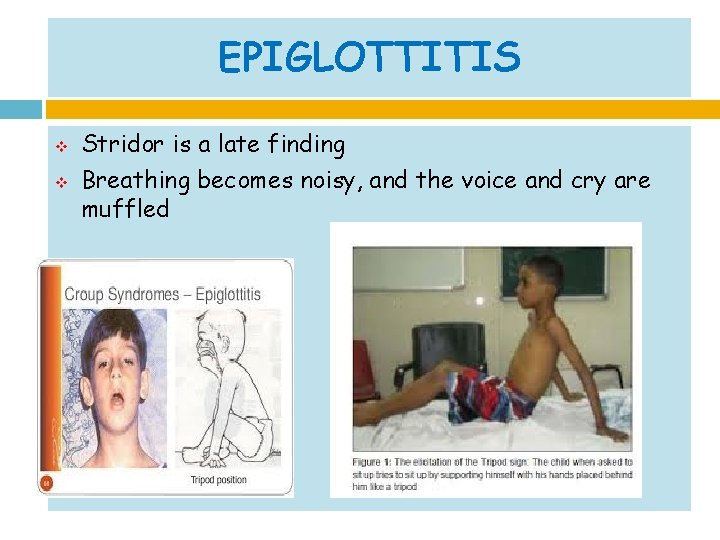
EPIGLOTTITIS v v Stridor is a late finding Breathing becomes noisy, and the voice and cry are muffled
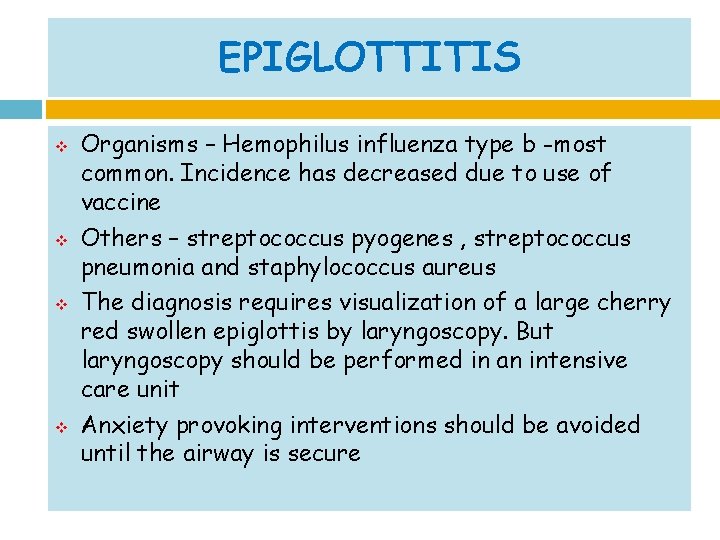
EPIGLOTTITIS v v Organisms – Hemophilus influenza type b -most common. Incidence has decreased due to use of vaccine Others – streptococcus pyogenes , streptococcus pneumonia and staphylococcus aureus The diagnosis requires visualization of a large cherry red swollen epiglottis by laryngoscopy. But laryngoscopy should be performed in an intensive care unit Anxiety provoking interventions should be avoided until the airway is secure
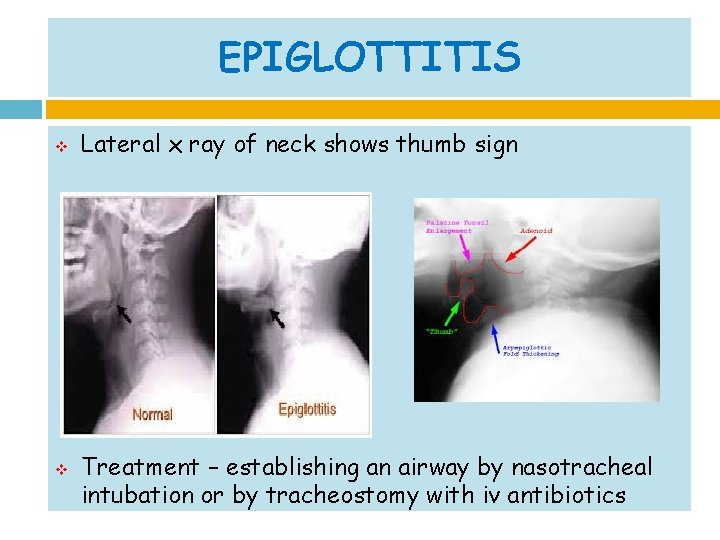
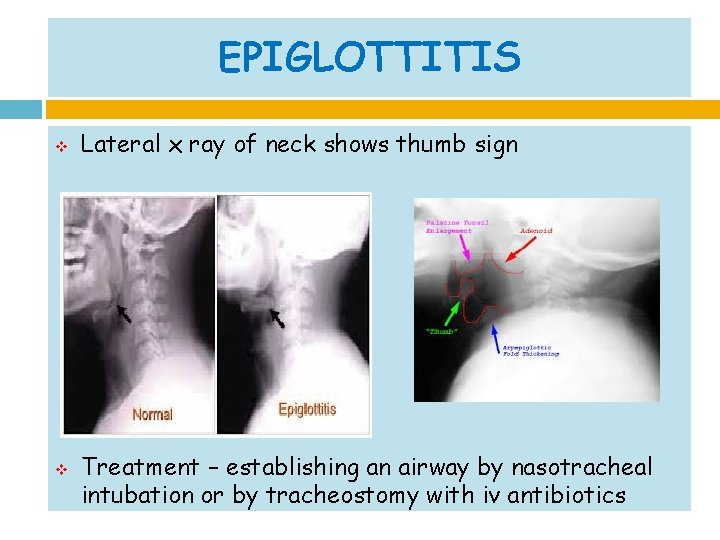
EPIGLOTTITIS v v Lateral x ray of neck shows thumb sign Treatment – establishing an airway by nasotracheal intubation or by tracheostomy with iv antibiotics
BACTERIAL TRACHEITIS v v v v Acute bacterial infection of upper airway Life threatening Often a complication of viral croup Most common organism – staphylococcus aureus Children with bacterial tracheitis tend to be older compared with those with viral croup High fever , toxicity with respiratory distress Diagnosis – clinical, purulent material is noted below the cords during endotracheal intubation
BACTERIAL TRACHEITIS v v Treatment: 1. establishing an airway by nasotracheal intubation or by tracheostomy 2. Antibiotics Complications: toxic shock syndrome, septic shock, post intubation pulmonary edema, ARDS and subglottic stenosis

Summary v v The differential diagnosis for stridous breathing should include croup, epiglottitis and bacterial tracheitis Most patients with croup can be managed as outpatients with corticosteroids If epiglottitis is suspected, the child should be admitted Children who have croup tend to have sudden onset of hoarseness and barking cough, but do not appear toxic, as compared to those who have epiglottitis and bacterial tracheitis
 Classification of upper respiratory tract infection
Classification of upper respiratory tract infection Conclusion of respiratory tract infection
Conclusion of respiratory tract infection Protective reflexes
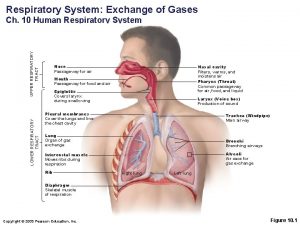
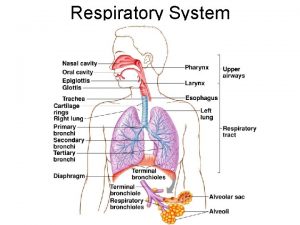
Protective reflexes Anatomy of the upper respiratory tract
Anatomy of the upper respiratory tract Upper respiratory tract anatomy
Upper respiratory tract anatomy Ophthalmootorhinolaryngology
Ophthalmootorhinolaryngology Anatomy of upper respiratory tract
Anatomy of upper respiratory tract Upper respiratory tract
Upper respiratory tract Upper and lower respiratory tract
Upper and lower respiratory tract What is the major function of the respiratory system
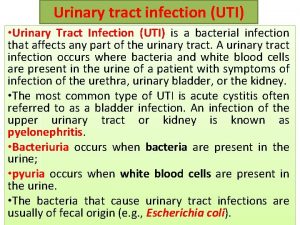
What is the major function of the respiratory system Urinary tract infection in pregnancy ppt
Urinary tract infection in pregnancy ppt Nursing management for urinary tract infection
Nursing management for urinary tract infection Complicated uti symptoms
Complicated uti symptoms Sexually transmitted diseases
Sexually transmitted diseases Uti symptoms men
Uti symptoms men Complicated urinary tract infection
Complicated urinary tract infection