Upper Extremity Fractures and Dislocations Clavicle Fracture Epidemiology









- Slides: 43
Upper Extremity Fractures and Dislocations
Clavicle Fracture • Epidemiology: – Clavicle fractures account for 2. 6% to 12% of all fractures and for 44% to 66% of fractures about the shoulder. – Middle third fractures account for 80% of all clavicle fractures, whereas fractures of the lateral and medial third of the clavicle account for 15% and 5%, respectively. • Anatomy: – The clavicle is the first bone to ossify (fifth week of gestation) and the last ossification center (sternal end) to fuse, at 22 to 25 years of age. – The clavicle is S-shaped, with the medial end convex forward and the lateral end concave forward. – The junction between the two cross-sectional configurations occurs in the middle third and constitutes a vulnerable area to fracture, especially with axial loading. Moreover, the middle third lacks reinforcement by muscles or ligaments distal to the subclavius insertion, resulting in additional vulnerability.
Clavicle Fracture • Mechanism of injury: – Falls onto the affected shoulder account for most (87%) of clavicular fractures, with direct impact accounting for only 7% and falls onto an outstretched hand accounting for 6%.
Clavicle Fracture • Clinical Evaluation – Patients usually present with splinting of the affected extremity, with the arm adducted across the chest and supported by the contralateral hand to unload the injured shoulder. – A careful neurovascular examination is necessary to assess the integrity of neural and vascular elements lying posterior to the clavicle. – The proximal fracture end is usually prominent and may tent the skin. Assessment of skin integrity is essential to rule out open fracture.
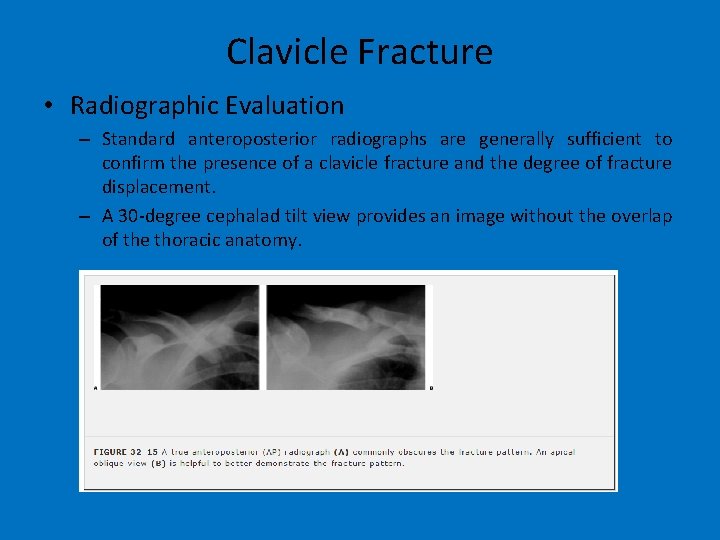
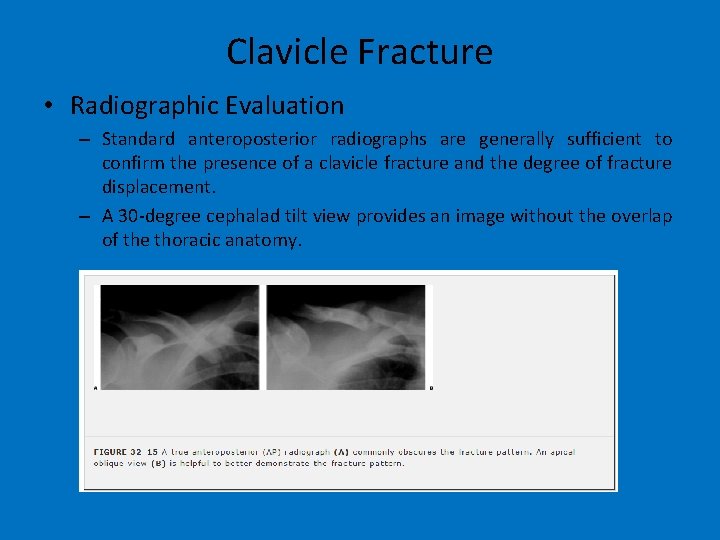
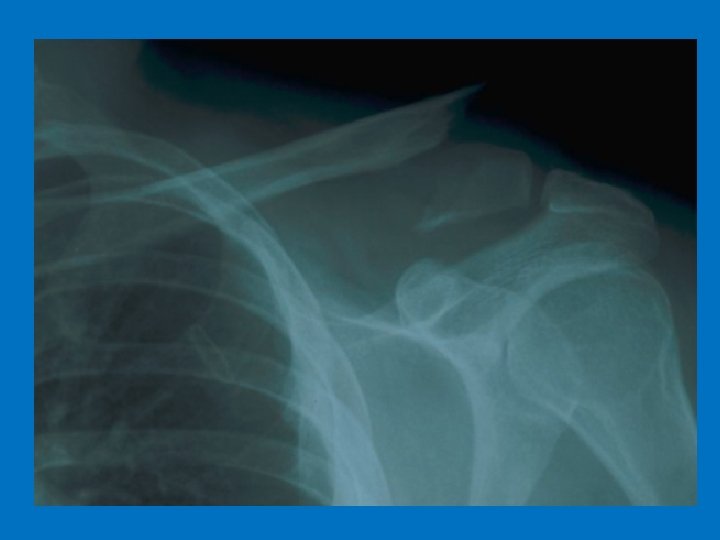
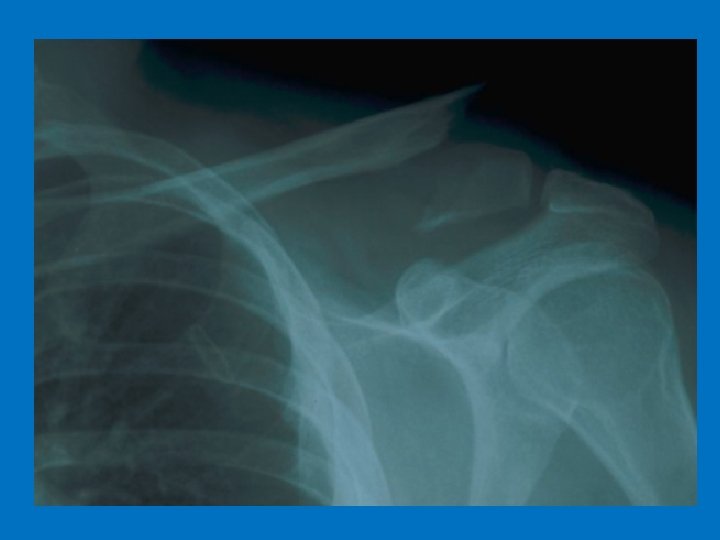
Clavicle Fracture • Radiographic Evaluation – Standard anteroposterior radiographs are generally sufficient to confirm the presence of a clavicle fracture and the degree of fracture displacement. – A 30 -degree cephalad tilt view provides an image without the overlap of the thoracic anatomy.
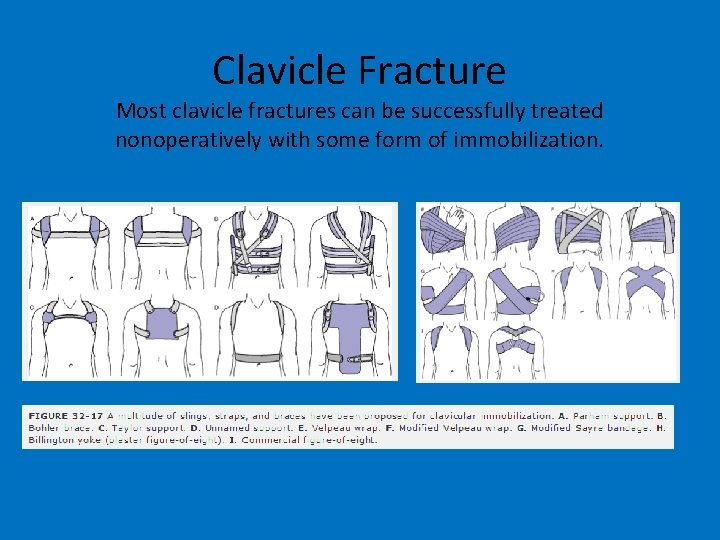
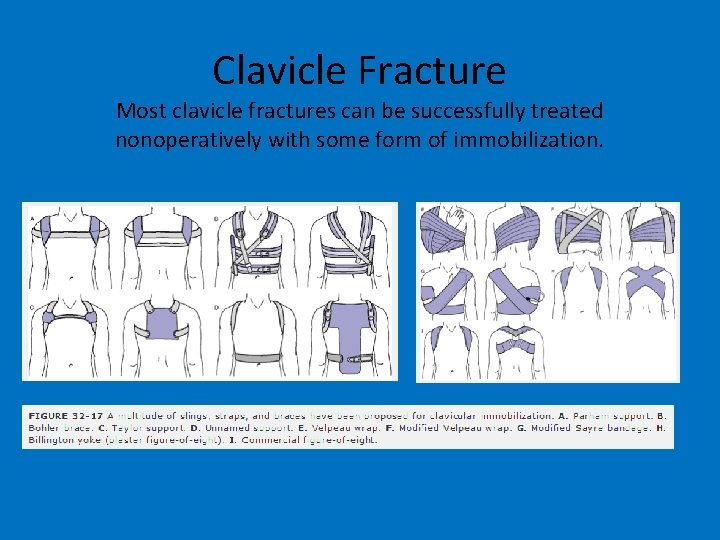
Clavicle Fracture Most clavicle fractures can be successfully treated nonoperatively with some form of immobilization.
Glenohumeral Dislocation • Epidemiology – The shoulder is the most commonly dislocated major joint of the body, accounting for up to 45% of dislocations. – Most shoulder dislocations are anterior; this occurs between eight and nine times more frequently than posterior dislocation, the second most common direction of dislocation. – Inferior and superior shoulder dislocations are rare.
Anterior glenohumeral dislocation represent 90% of shoulder dislocations • Mechanism of Injury – Anterior glenohumeral dislocation may occur as a result of trauma, secondary to either direct or indirect forces. – Indirect trauma to the upper extremity with the shoulder in abduction, extension, and external rotation is the most common mechanism. – Direct, anteriorly directed impact to the posterior shoulder may produce an anterior dislocation. – Convulsive mechanisms and electrical shock typically produce posterior shoulder dislocations, but they may also result in an anterior dislocation.
Glenohumeral Dislocation • Clinical Evaluation – The patient typically presents with the injured shoulder held in slight abduction and external rotation. The acutely dislocated shoulder is painful, with muscular spasm. – Examination typically reveals squaring of the shoulder owing to a relative prominence of the acromion, a relative hollow beneath the acromion posteriorly, and a palpable mass anteriorly. – A careful neurovascular examination is important, with attention to axillary nerve integrity. Deltoid muscle testing is usually not possible, but sensation over the deltoid may be assessed. Deltoid atony may be present and should not be confused with axillary nerve injury. Musculocutaneous nerve integrity can be assessed by the presence of sensation on the anterolateral forearm.
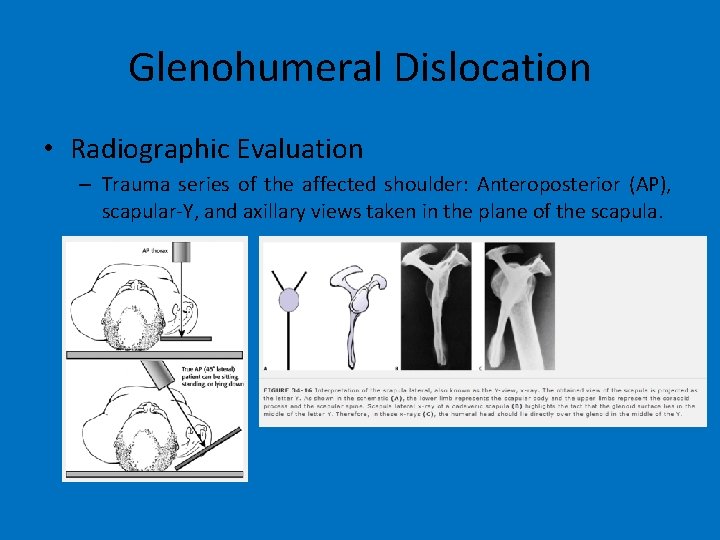
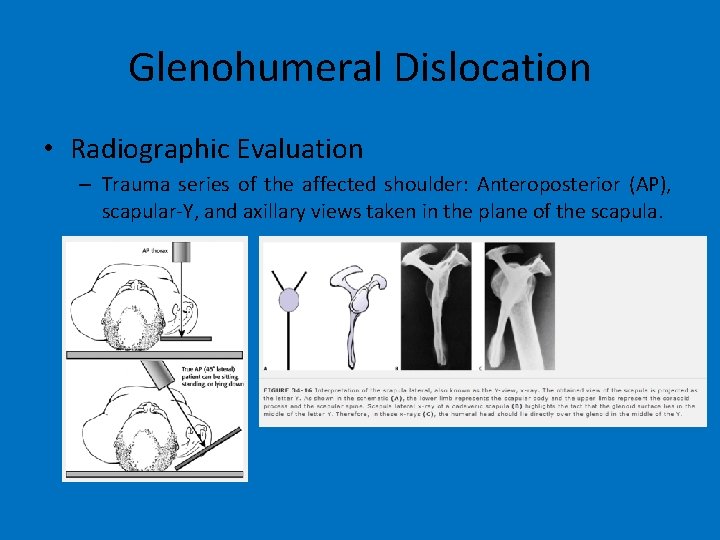
Glenohumeral Dislocation • Radiographic Evaluation – Trauma series of the affected shoulder: Anteroposterior (AP), scapular-Y, and axillary views taken in the plane of the scapula.

Glenohumeral Dislocation
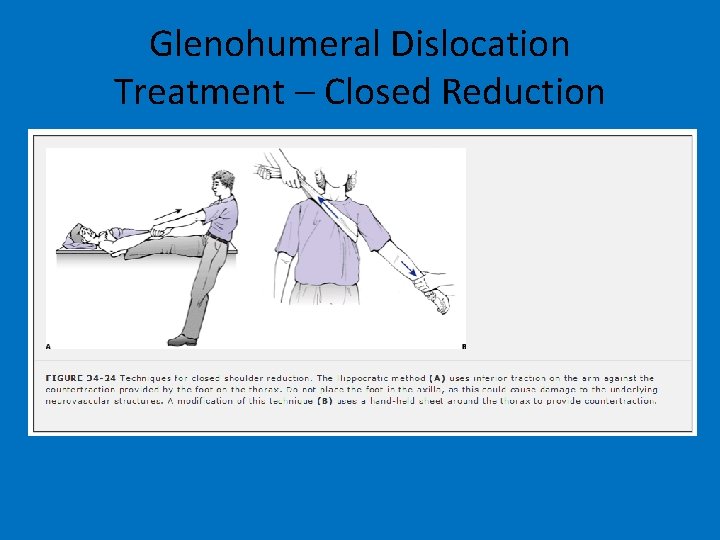
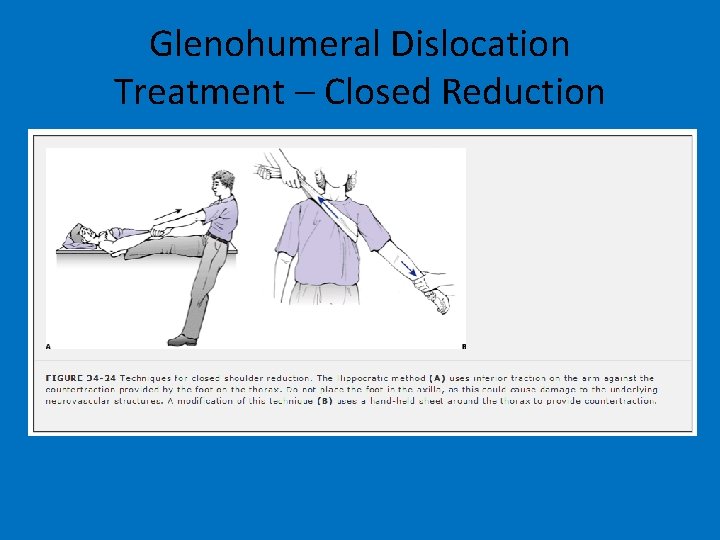
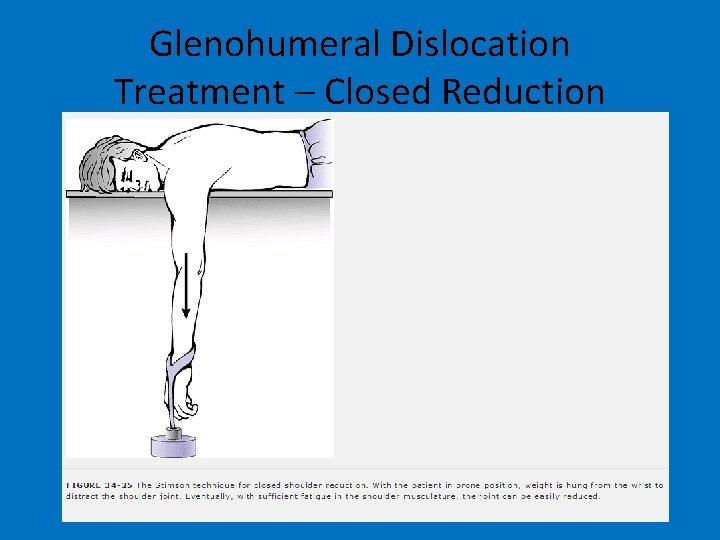
Glenohumeral Dislocation Treatment – Closed Reduction
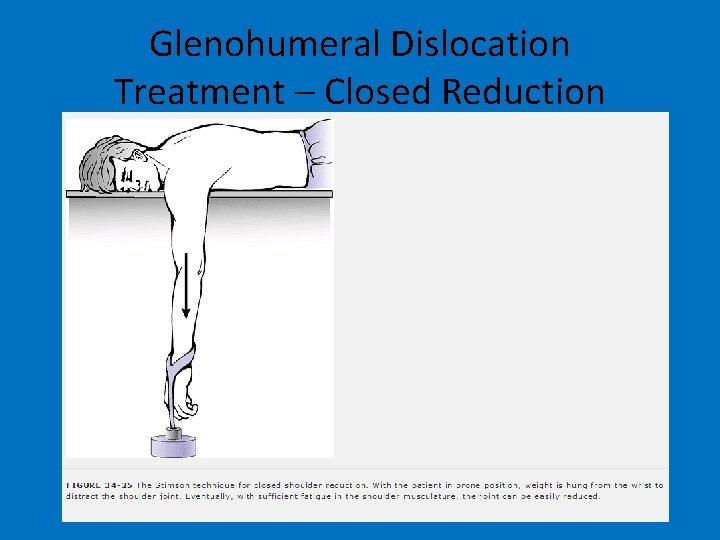
Glenohumeral Dislocation Treatment – Closed Reduction
Humeral Shaft Fracture • Mechanism of injury: – Direct (most common): Direct trauma to the arm from a blow or motor vehicle accident results in transverse or comminuted fractures. – Indirect: A fall on an outstretched arm results in spiral or oblique fractures, especially in elderly patients. Uncommonly, throwing injuries with extreme muscular contraction have been reported to cause humeral shaft fractures. – Fracture pattern depends on the type of force applied: • • Compressive: proximal or distal humeral fractures Bending: transverse fractures of the humeral shaft Torsional: spiral fractures of the humeral shaft Torsional and bending: oblique fracture, often accompanied by a butterfly fragment
Humeral Shaft Fracture • Clinical Evaluation: – Patients with humeral shaft fractures typically present with pain, swelling, deformity, and shortening of the affected arm. – A careful neurovascular examination is essential, with particular attention to radial nerve function. In cases of extreme swelling, serial neurovascular examinations are indicated with possible measurement of compartment pressures. – Physical examination frequently reveals gross instability with crepitus on gentle manipulation. – Soft tissue abrasions and minor lacerations must be differentiated from open fractures.
Humeral Shaft Fracture • Radiographic Evaluation: – AP and lateral radiographs of the humerus should be obtained, including the shoulder and elbow joints on each view. To obtain views at 90° from each other, the patient, NOT the arm, should be rotated, as manipulation of the injured extremity will typically result in distal fragment rotation only. – Radiographs of the contralateral humerus may aid in preoperative planning.

Humeral Shaft Fracture
Humeral Shaft Fracture • Treatment: – The goal is to establish union with an acceptable humeral alignment and to restore the patient to preinjury level of function. – Both patient and fracture characteristics, including patient age and functional level, presence of associated injuries, soft tissue status, and fracture pattern, need to be considered when selecting an appropriate treatment option.
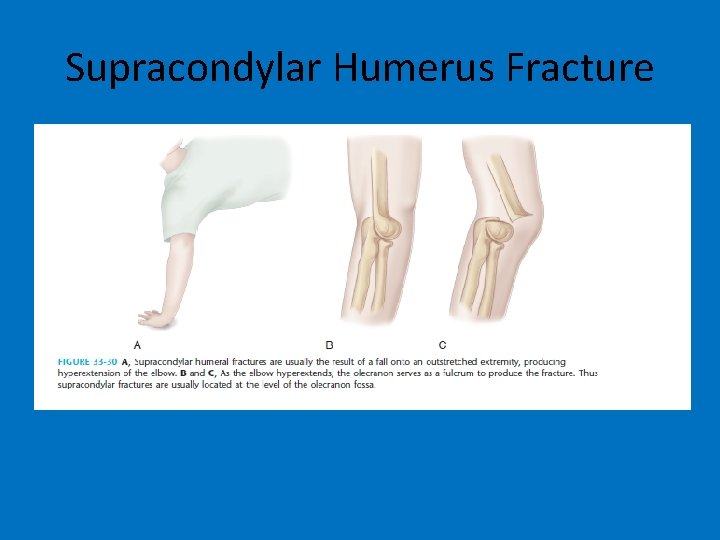
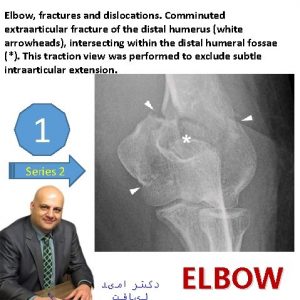
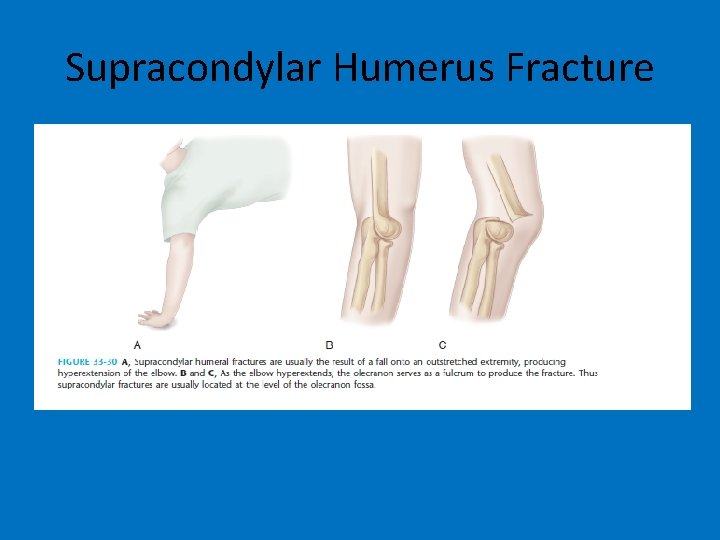
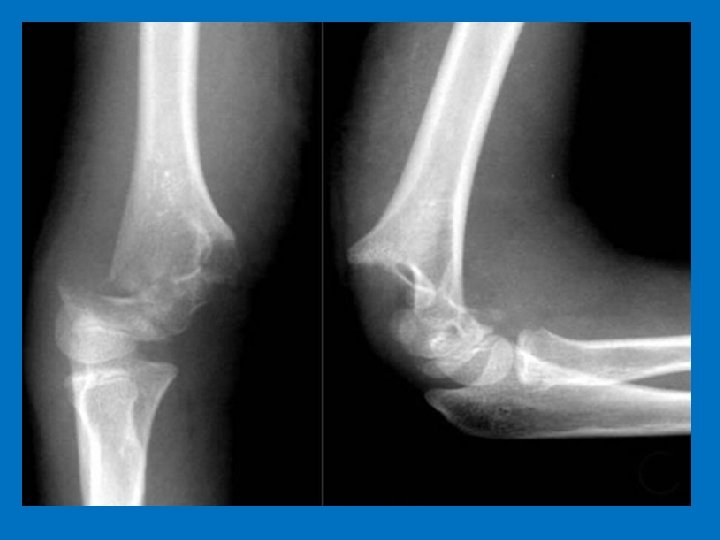
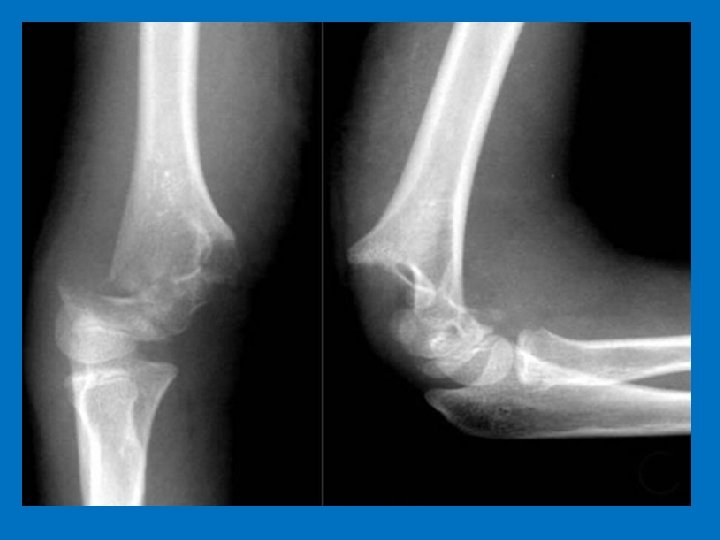
Supracondylar Humerus Fracture

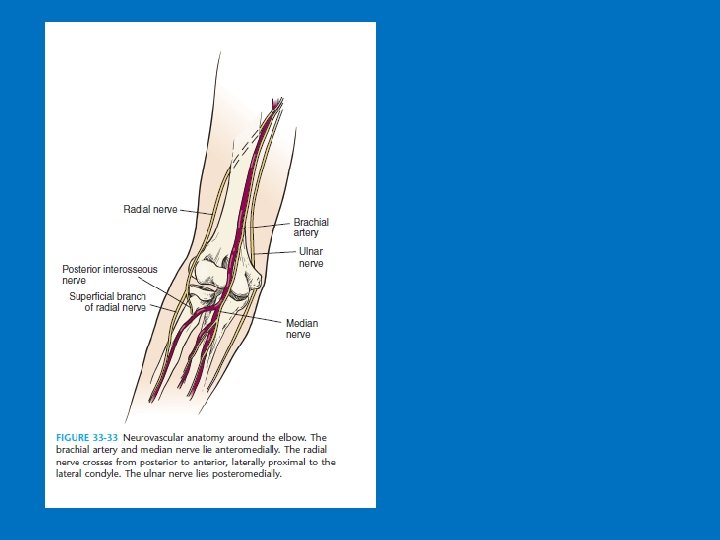


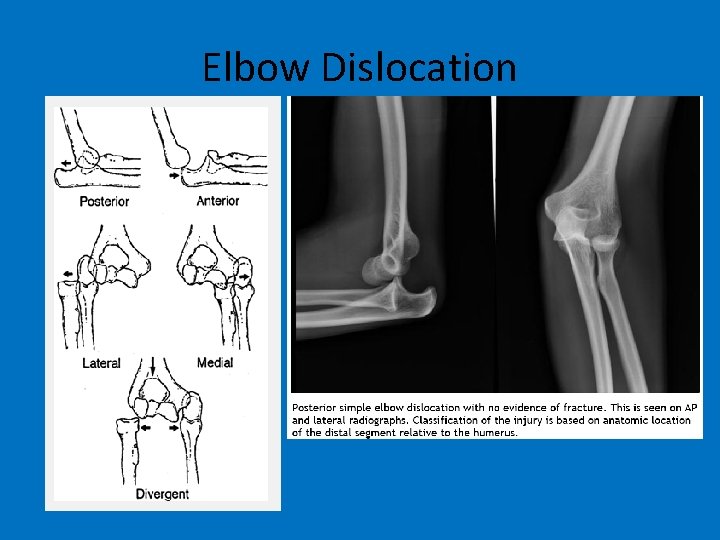
Elbow Dislocation • Epidemiology: – Accounts for 11% to 28% of injuries to the elbow. – Posterior dislocation is most common. – Simple dislocations are those without fracture. – Complex dislocations are those that occur with an associated fracture and represent just under 50% of elbow dislocations. – Highest incidence in the 10 - to 20 -year old age group associated with sports injuries, although recurrent dislocation is uncommon.
Elbow Dislocation • Mechanism of injury: – Most commonly, injury is caused by a fall onto an outstretched hand or elbow, resulting in a levering force to unlock the olecranon from the trochlea combined with translation of the articular surfaces to produce the dislocation. – Posterior dislocation: This is a combination of elbow hyperextension, valgus stress, arm abduction, and forearm supination.

Elbow Dislocation • Mechanism of injury: – Most commonly, injury is caused by a fall onto an outstretched hand or elbow, resulting in a levering force to unlock the olecranon from the trochlea combined with translation of the articular surfaces to produce the dislocation. – Posterior dislocation: This is a combination of elbow hyperextension, valgus stress, arm abduction, and forearm supination.
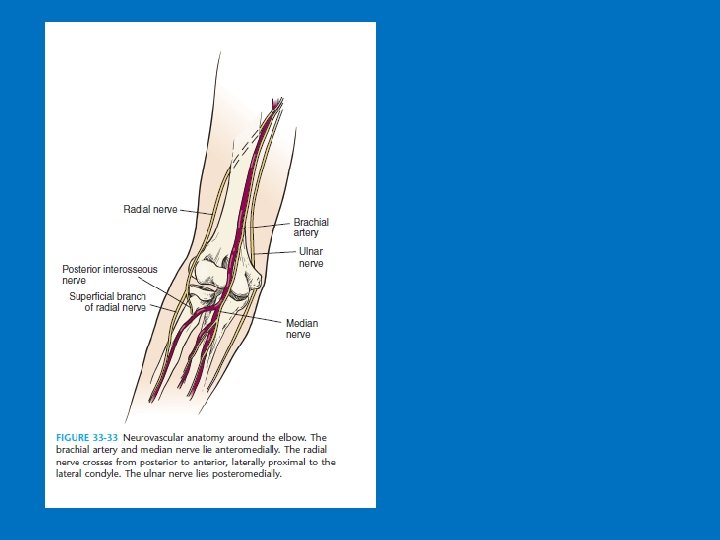
Elbow Dislocation • Clinical Evaluation: – Patients typically guard the injured upper extremity, which shows variable gross instability and swelling. – A careful neurovascular examination is essential and should be performed before radiography or manipulation. – Following manipulation or reduction, repeat neurovascular examination should be performed to assess neurovascular status. – Serial neurovascular examinations should be performed when massive antecubital swelling exists or when the patient is felt to be at risk for compartment syndrome.
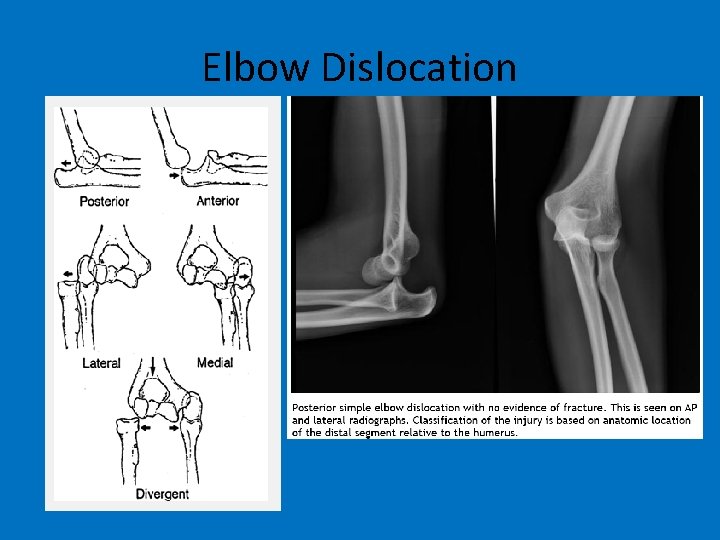
Elbow Dislocation
Elbow Dislocation • Treatment: – Acute simple elbow dislocations should undergo closed reduction with the patient under sedation and adequate analgesia. Alternatively, general or regional anesthesia may be used. – Correction of medial or lateral displacement followed by longitudinal traction and flexion is usually successful for posterior dislocations. – For posterior dislocations, reduction should be performed with the elbow flexed while providing distal traction. – Neurovascular status should be reassessed, followed by evaluation of stable range of elbow motion. – Postreduction radiographs are essential. – Postreduction management should consist of a posterior splint at 90 degrees and elevation. – Early, gentle, active range of elbow motion is associated with better long-term results. Prolonged immobilization is associated with unsatisfactory results and greater flexion contracture. – Recovery of motion and strength may require 3 to 6 months.
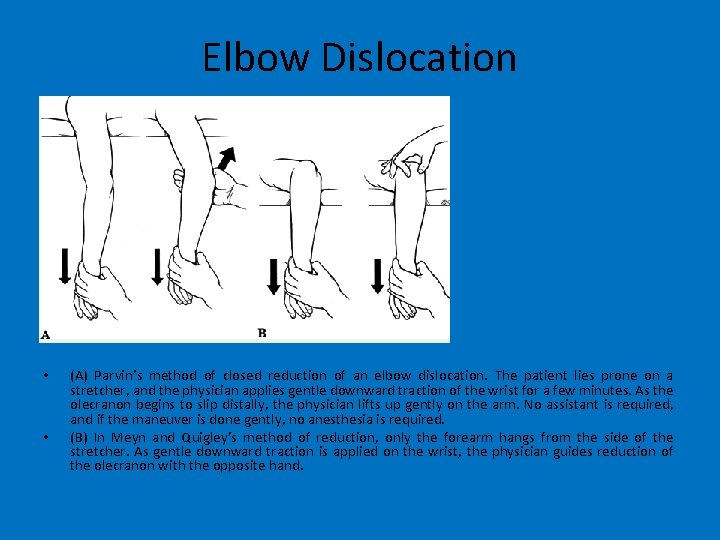
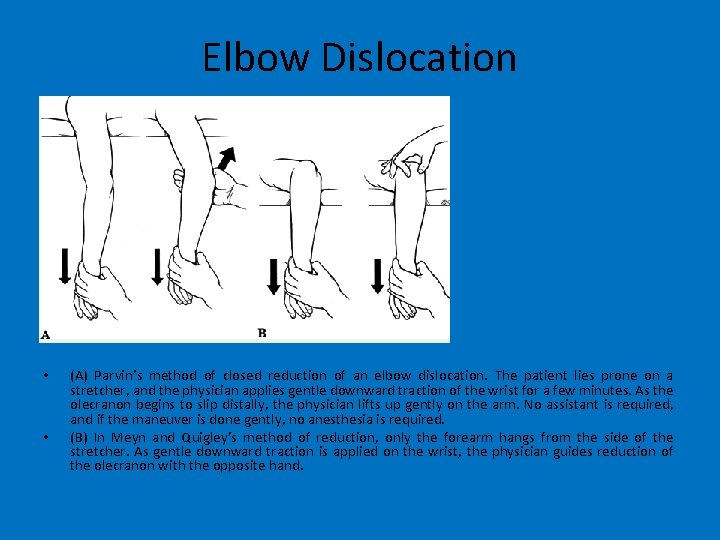
Elbow Dislocation • • (A) Parvin’s method of closed reduction of an elbow dislocation. The patient lies prone on a stretcher, and the physician applies gentle downward traction of the wrist for a few minutes. As the olecranon begins to slip distally, the physician lifts up gently on the arm. No assistant is required, and if the maneuver is done gently, no anesthesia is required. (B) In Meyn and Quigley’s method of reduction, only the forearm hangs from the side of the stretcher. As gentle downward traction is applied on the wrist, the physician guides reduction of the olecranon with the opposite hand.
Radius and ulna shaft fracture • Clinical Evaluation: – Patients typically present with gross deformity of the involved forearm, pain, swelling, and loss of hand forearm function. – A careful neurovascular examination is essential, with assessment of radial and ulnar pulses, as well as median, radial, and ulnar nerve function. – One must carefully assess open wounds because the ulna border is subcutaneous, and even superficial wounds can expose the bone.
Radius and ulna shaft fracture • Operative treatment: – Open reduction and internal fixation is the procedure of choice for displaced forearm fractures involving the radius and ulna in adults. – Internal fixation involves use of compression plating (3. 5 -mm dynamic compression plate) with or without bone grafting. – Principles of plate fixation: • Restore ulnar and radial length (prevents subluxation of either the proximal or distal radioulnar joint). • Restore rotational alignment. • Restore radial bow (essential for rotational function of the forearm). – External fixation may be used in cases with severe bone or soft tissue loss, gross contamination, infected nonunion, or in cases of open elbow fracture-dislocations with soft tissue loss.


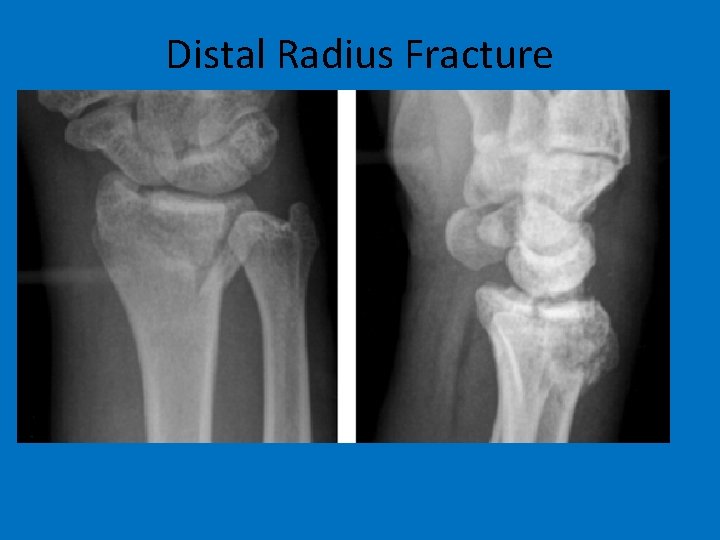
Distal Radius Fracture • Epidemiology: – Distal radius fractures are among the most common fractures of the upper extremity. – Fractures of the distal radius represent approximately onesixth of all fractures treated in emergency departments. – The incidence of distal radius fractures in the elderly correlates with osteopenia and rises in incidence with increasing age, nearly in parallel with the increased incidence of hip fractures. – Risk factors for fractures of the distal radius in the elderly include decreased bone mineral density, female sex, white race, family history, and early menopause.
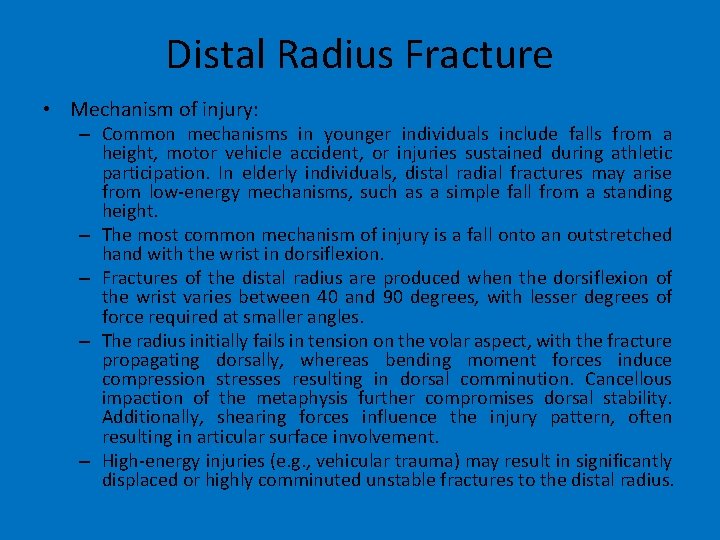
Distal Radius Fracture • Mechanism of injury: – Common mechanisms in younger individuals include falls from a height, motor vehicle accident, or injuries sustained during athletic participation. In elderly individuals, distal radial fractures may arise from low-energy mechanisms, such as a simple fall from a standing height. – The most common mechanism of injury is a fall onto an outstretched hand with the wrist in dorsiflexion. – Fractures of the distal radius are produced when the dorsiflexion of the wrist varies between 40 and 90 degrees, with lesser degrees of force required at smaller angles. – The radius initially fails in tension on the volar aspect, with the fracture propagating dorsally, whereas bending moment forces induce compression stresses resulting in dorsal comminution. Cancellous impaction of the metaphysis further compromises dorsal stability. Additionally, shearing forces influence the injury pattern, often resulting in articular surface involvement. – High-energy injuries (e. g. , vehicular trauma) may result in significantly displaced or highly comminuted unstable fractures to the distal radius.
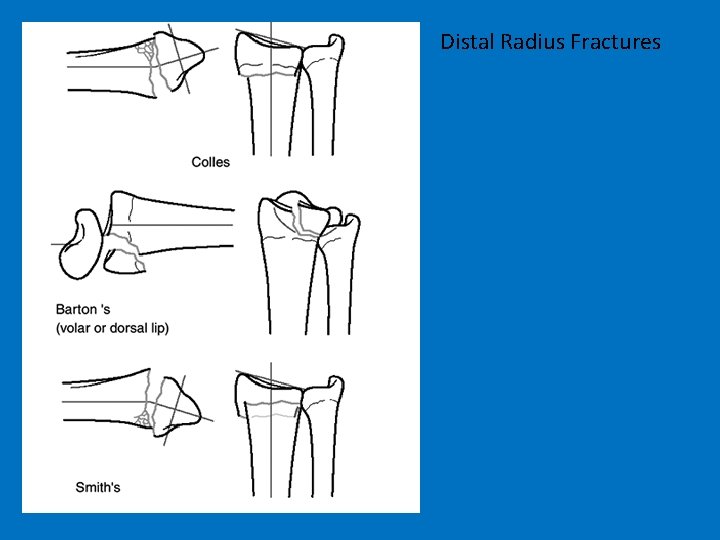
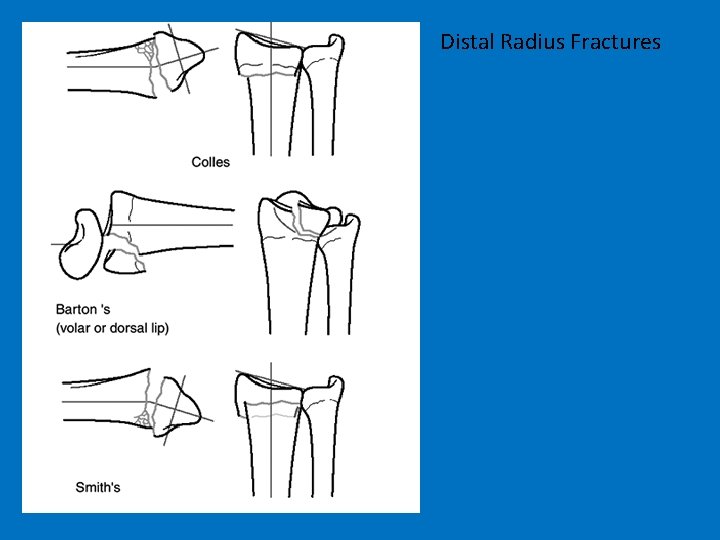
Distal Radius Fractures
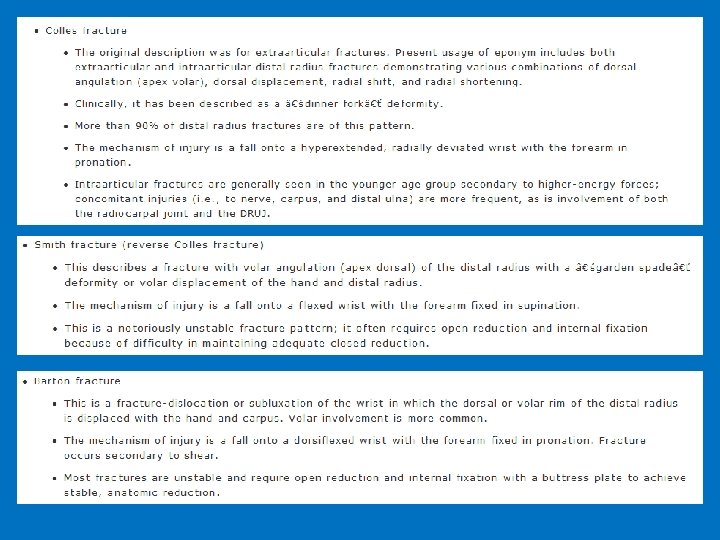
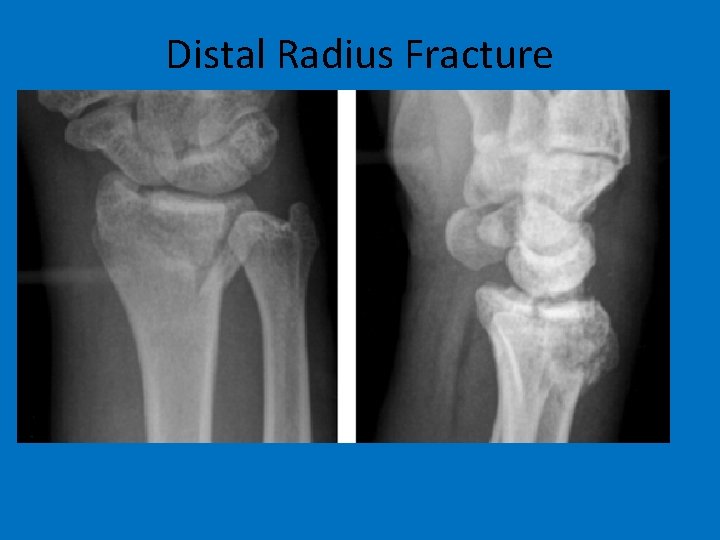
Distal Radius Fracture

Distal Radius Fracture • Treatment: – All fractures should undergo closed reduction, even if it is expected that surgical management will be needed. • Fracture reduction helps to limit postinjury swelling, provides pain relief, and relieves compression on the median nerve. – Cast immobilization is indicated for: • Nondisplaced or minimally displaced fractures. • Displaced fractures with a stable fracture pattern which can be expected to unite within acceptable radiographic parameters. • Low-demand elderly patients in whom future functional impairment is less of a priority than immediate health concerns and/or operative risks. – Hematoma block with supplemental intravenous sedation, Bier block, or conscious sedation can be used to provide analgesia for closed reduction.
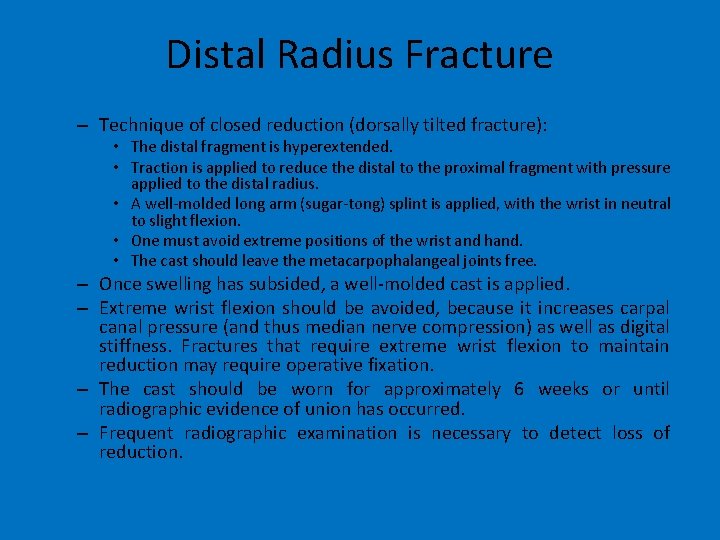
Distal Radius Fracture – Technique of closed reduction (dorsally tilted fracture): • The distal fragment is hyperextended. • Traction is applied to reduce the distal to the proximal fragment with pressure applied to the distal radius. • A well-molded long arm (sugar-tong) splint is applied, with the wrist in neutral to slight flexion. • One must avoid extreme positions of the wrist and hand. • The cast should leave the metacarpophalangeal joints free. – Once swelling has subsided, a well-molded cast is applied. – Extreme wrist flexion should be avoided, because it increases carpal canal pressure (and thus median nerve compression) as well as digital stiffness. Fractures that require extreme wrist flexion to maintain reduction may require operative fixation. – The cast should be worn for approximately 6 weeks or until radiographic evidence of union has occurred. – Frequent radiographic examination is necessary to detect loss of reduction.
 Victorian paediatric orthopaedic network
Victorian paediatric orthopaedic network Subclavian artery location
Subclavian artery location Upper extremity pnf patterns
Upper extremity pnf patterns Closed chain kinematics
Closed chain kinematics Orrin franko md
Orrin franko md The biomechanics of the human upper extremity
The biomechanics of the human upper extremity Upper extremity dermatomes
Upper extremity dermatomes Dislocations in crystals
Dislocations in crystals Consider two edge dislocations of opposite sign
Consider two edge dislocations of opposite sign Boneframework
Boneframework Right hip bone
Right hip bone Hyperresonance sound
Hyperresonance sound Epitrochlear lymph nodes
Epitrochlear lymph nodes New ballard score
New ballard score Cat clavicle
Cat clavicle Ductile failure vs brittle failure
Ductile failure vs brittle failure Femoral artery pulse
Femoral artery pulse Radial and concentric fractures
Radial and concentric fractures Activity 14-1 glass fracture patterns answer key
Activity 14-1 glass fracture patterns answer key Pnf d1 flexion
Pnf d1 flexion Left lower extremity
Left lower extremity Mummy restraint
Mummy restraint Muscles of thigh cross section
Muscles of thigh cross section Branches of popliteal artery
Branches of popliteal artery Regio plantar pedis
Regio plantar pedis Extremity
Extremity Patient wristband colors
Patient wristband colors Introduction of lifting and transferring of patients
Introduction of lifting and transferring of patients Rigidity vs spasticity
Rigidity vs spasticity Skeletal system
Skeletal system Thesourceagents
Thesourceagents Advantages and disadvantages of nutritional epidemiology
Advantages and disadvantages of nutritional epidemiology Descriptive vs analytical epidemiology
Descriptive vs analytical epidemiology Incidence vs prevalence
Incidence vs prevalence Certification board of infection control and epidemiology
Certification board of infection control and epidemiology Epidemiology person place time
Epidemiology person place time Irving tennis elbow
Irving tennis elbow Ao classification of fractures
Ao classification of fractures Fracture sus et intercondylienne du coude
Fracture sus et intercondylienne du coude Les ischions
Les ischions What is water seal chest tube
What is water seal chest tube Primary bone vs secondary bone
Primary bone vs secondary bone Panfacial fractures sequencing
Panfacial fractures sequencing Classification of open fractures
Classification of open fractures