Updates in Pulmonary Function Testing A Deeper Dive
- Slides: 25
Updates in Pulmonary Function Testing: A Deeper Dive into Spirometry in COPD Timothy Scialla, MD Assistant Professor Division of Pulmonary and Critical Care Duke University 09/07/2017
COI disclosure slide ♦ I am a co-investigator for on-site clinical research trials sponsored by: ♦ GSK ♦ Astra. Zeneca ♦ Sanofi ♦ Genentech ♦ NHLBI
Overview of Talk ♦ Standardization of Spirometry ♦ COPD diagnosis ♦ Lower Limit of Normal (LLN) vs: ♦ FEV 1/FVC < 0. 70 (Fixed Ratio [FR]) ♦ Bronchodilator Reversibility in COPD
Practice makes permanent! Standards for Spirometry ♦ Proper Calibration ♦ Volume test ♦ Leak test ♦ Test Procedure ♦ Maximal inspiration ♦ “Blast” of exhalation ♦ Complete exhalation till end of test Miller et al. Standardisation of spirometry. ERS. 2005
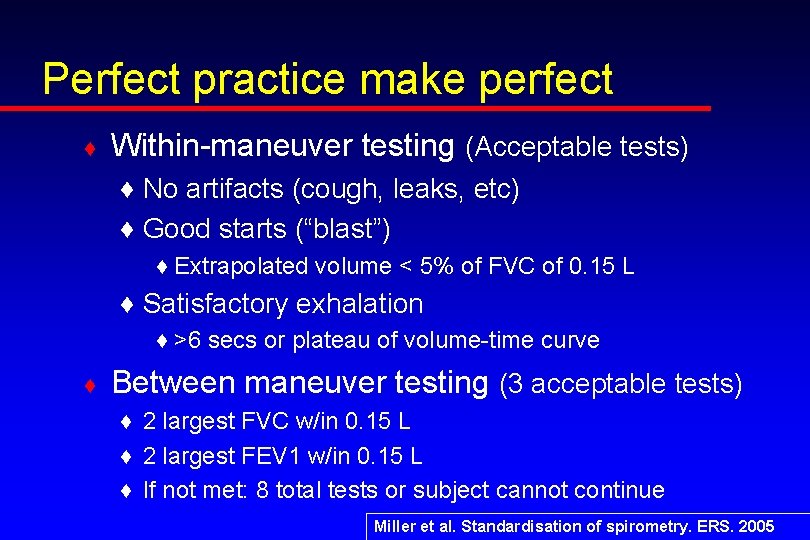
Perfect practice make perfect ♦ Within-maneuver testing (Acceptable tests) ♦ No artifacts (cough, leaks, etc) ♦ Good starts (“blast”) ♦ Extrapolated volume < 5% of FVC of 0. 15 L ♦ Satisfactory exhalation ♦ >6 secs or plateau of volume-time curve ♦ Between maneuver testing (3 acceptable tests) ♦ 2 largest FVC w/in 0. 15 L ♦ 2 largest FEV 1 w/in 0. 15 L ♦ If not met: 8 total tests or subject cannot continue Miller et al. Standardisation of spirometry. ERS. 2005
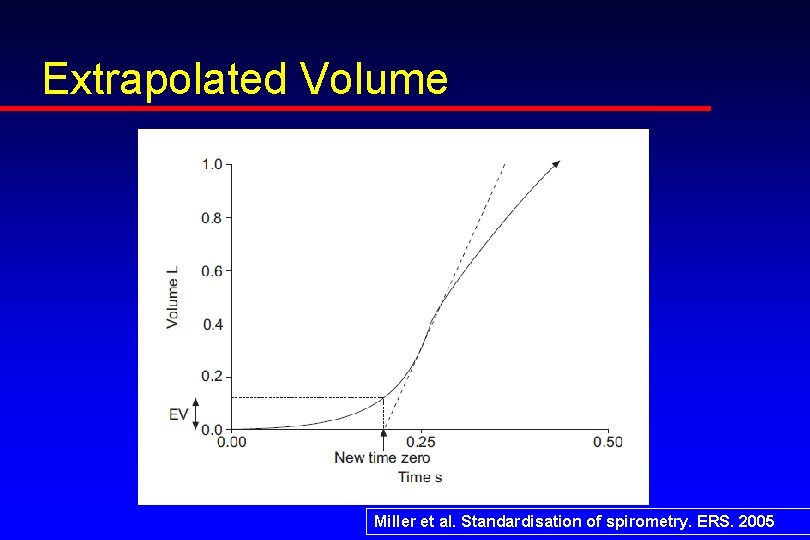
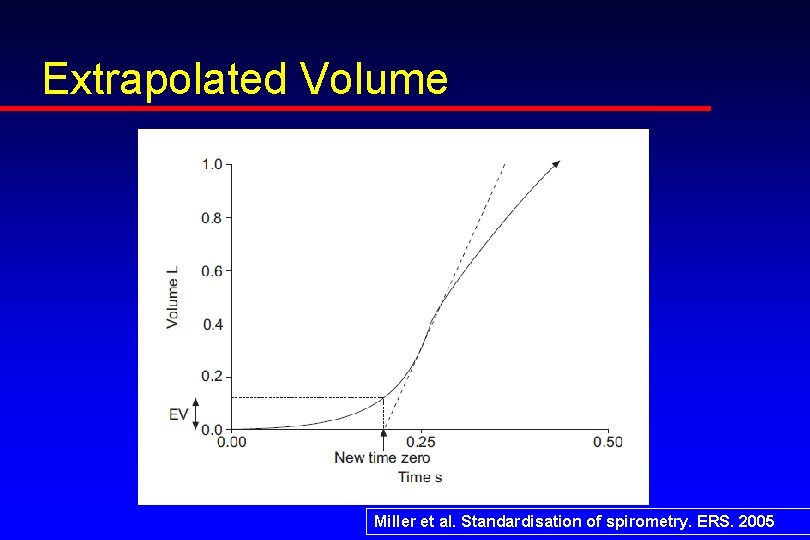
Extrapolated Volume Miller et al. Standardisation of spirometry. ERS. 2005
Spirometry integral to the diagnosis of COPD ♦ Definition of COPD ♦ Airflow limitation that is NOT fully reversible ♦ What are the “Gold Standards” to diagnose? ♦ Airflow Limitation ♦ Reversibility There are none
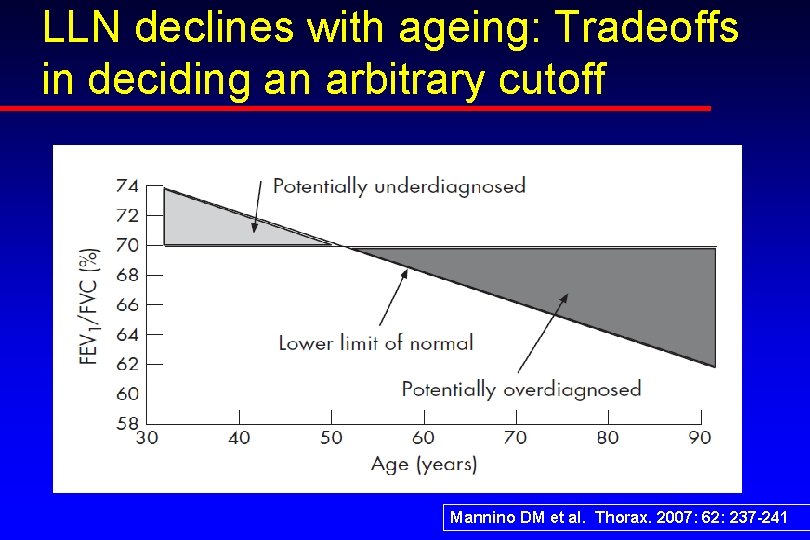
Airflow Limitation Definition ♦ Issue getting air OUT of the lungs ♦ Obstruction defined by FEV 1/FVC ♦ FEV 1/FVC steadily declines with aging ♦ Natural loss of elasticity ♦ Fixed ratio vs lower limit of normal (LLN) ♦ Severity of Obstruction ♦ Determined by FEV 1 (% predicted) ♦ FVC ♦ Clues about restriction vs. air trapping
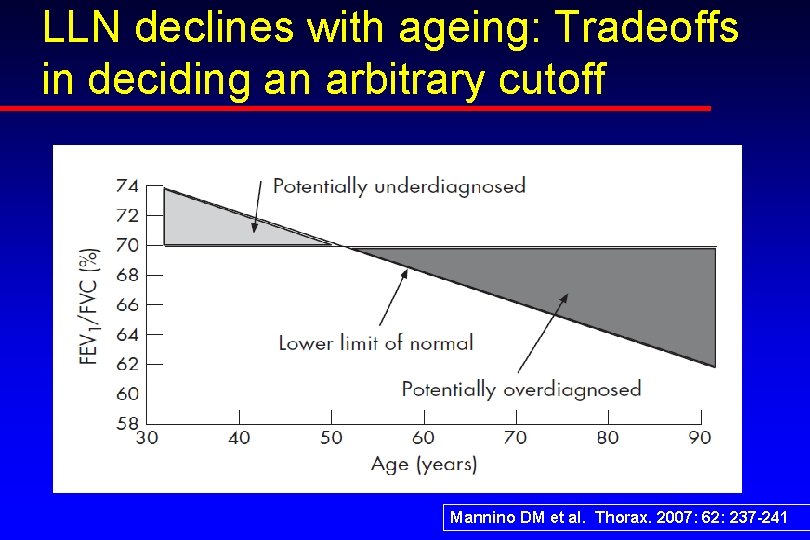
LLN declines with ageing: Tradeoffs in deciding an arbitrary cutoff Mannino DM et al. Thorax. 2007: 62: 237 -241
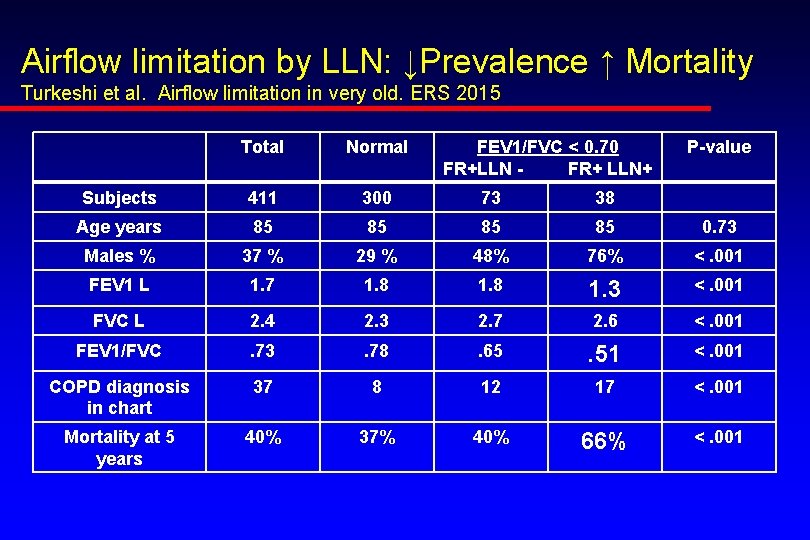
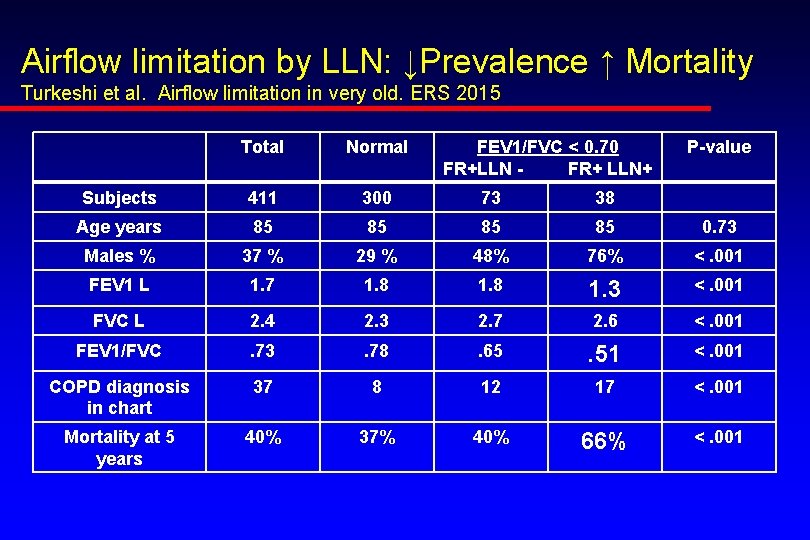
Airflow limitation by LLN: ↓Prevalence ↑ Mortality Turkeshi et al. Airflow limitation in very old. ERS 2015 Total Normal FEV 1/FVC < 0. 70 FR+LLN FR+ LLN+ P-value Subjects 411 300 73 38 Age years 85 85 0. 73 Males % 37 % 29 % 48% 76% <. 001 FEV 1 L 1. 7 1. 8 1. 3 <. 001 FVC L 2. 4 2. 3 2. 7 2. 6 <. 001 FEV 1/FVC . 73 . 78 . 65 . 51 <. 001 COPD diagnosis in chart 37 8 12 17 <. 001 Mortality at 5 years 40% 37% 40% 66% <. 001
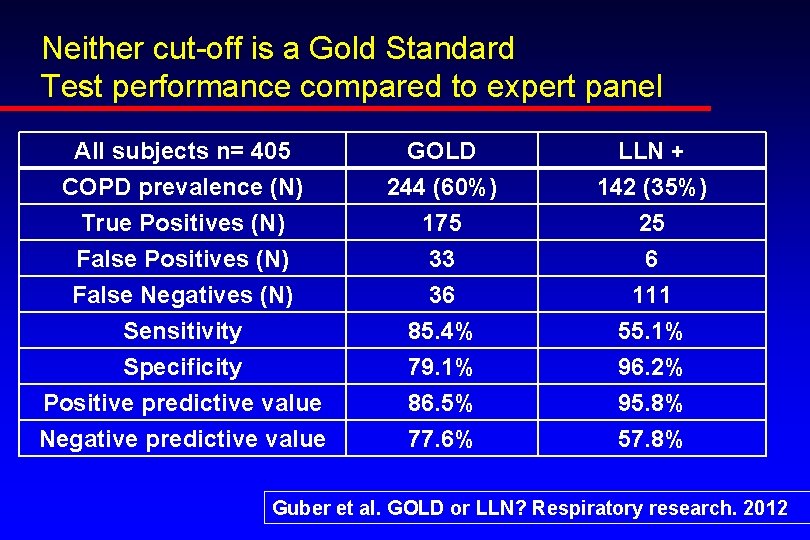
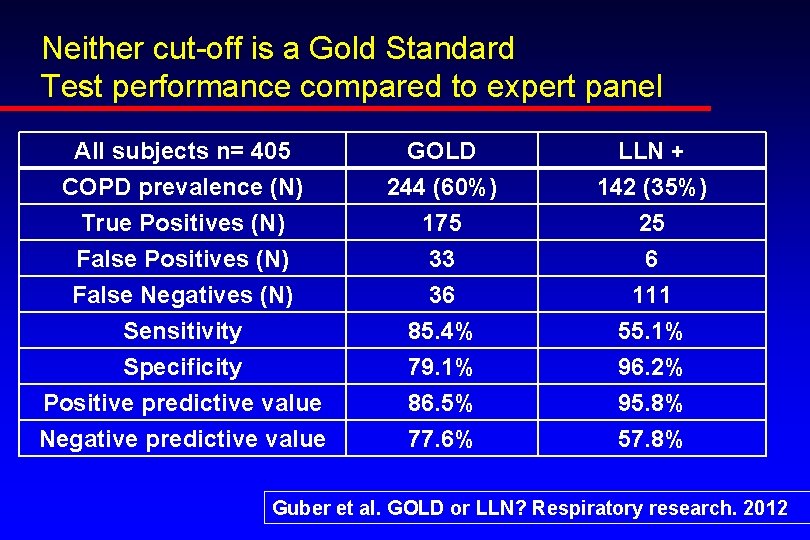
Neither cut-off is a Gold Standard Test performance compared to expert panel All subjects n= 405 COPD prevalence (N) True Positives (N) False Positives (N) GOLD 244 (60%) 175 33 LLN + 142 (35%) 25 6 False Negatives (N) Sensitivity Specificity Positive predictive value Negative predictive value 36 85. 4% 79. 1% 86. 5% 77. 6% 111 55. 1% 96. 2% 95. 8% 57. 8% Guber et al. GOLD or LLN? Respiratory research. 2012
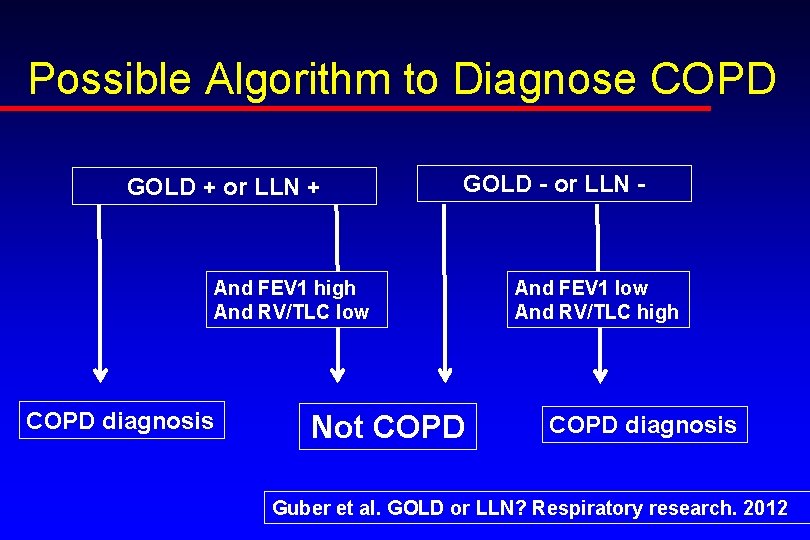
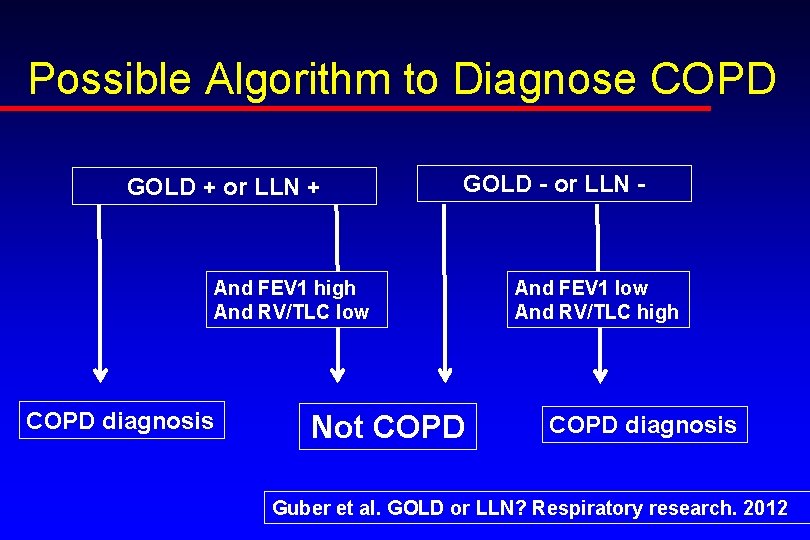
Possible Algorithm to Diagnose COPD GOLD + or LLN + GOLD - or LLN - And FEV 1 high And RV/TLC low COPD diagnosis Not COPD And FEV 1 low And RV/TLC high COPD diagnosis Guber et al. GOLD or LLN? Respiratory research. 2012
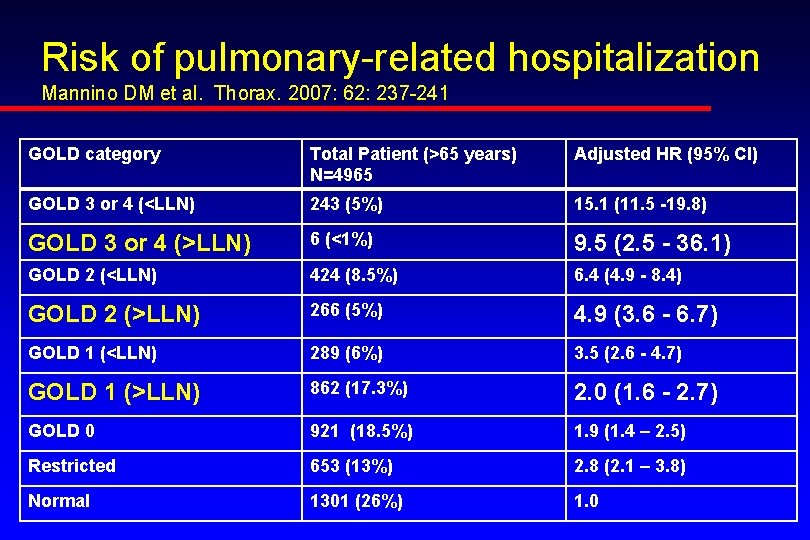
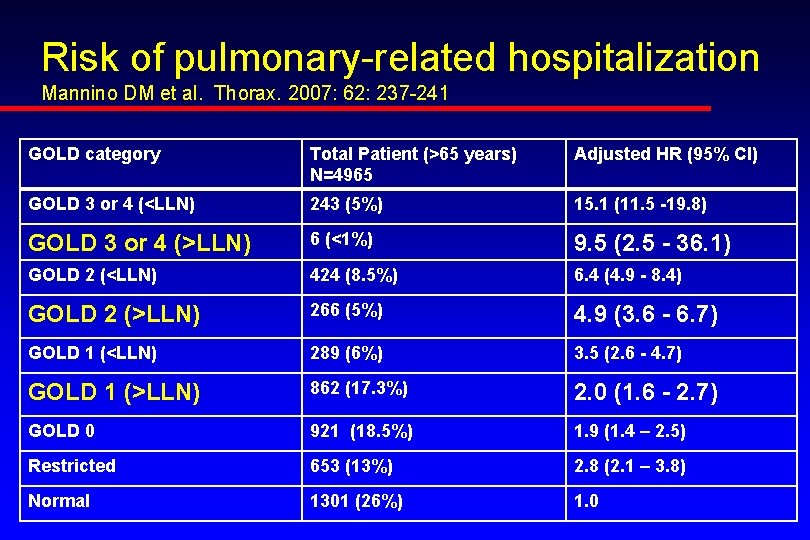
Risk of pulmonary-related hospitalization Mannino DM et al. Thorax. 2007: 62: 237 -241 GOLD category Total Patient (>65 years) N=4965 Adjusted HR (95% CI) GOLD 3 or 4 (<LLN) 243 (5%) 15. 1 (11. 5 -19. 8) GOLD 3 or 4 (>LLN) 6 (<1%) 9. 5 (2. 5 - 36. 1) GOLD 2 (<LLN) 424 (8. 5%) 6. 4 (4. 9 - 8. 4) GOLD 2 (>LLN) 266 (5%) 4. 9 (3. 6 - 6. 7) GOLD 1 (<LLN) 289 (6%) 3. 5 (2. 6 - 4. 7) GOLD 1 (>LLN) 862 (17. 3%) 2. 0 (1. 6 - 2. 7) GOLD 0 921 (18. 5%) 1. 9 (1. 4 – 2. 5) Restricted 653 (13%) 2. 8 (2. 1 – 3. 8) Normal 1301 (26%) 1. 0
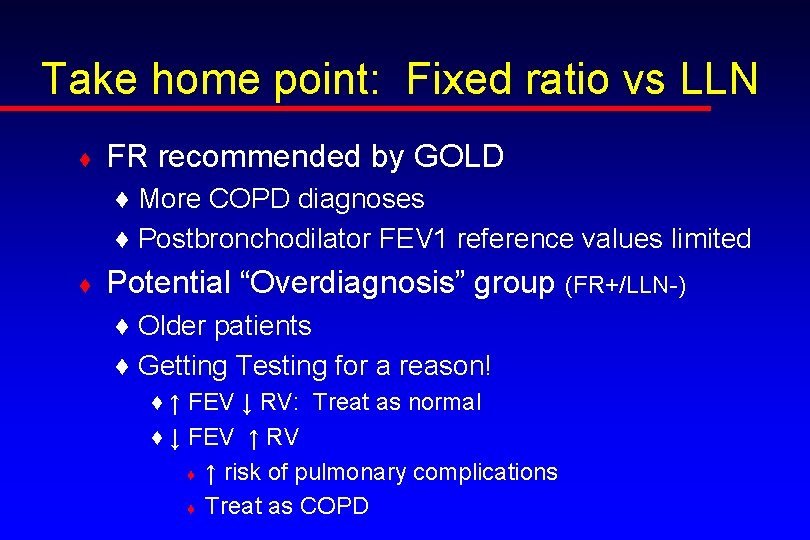
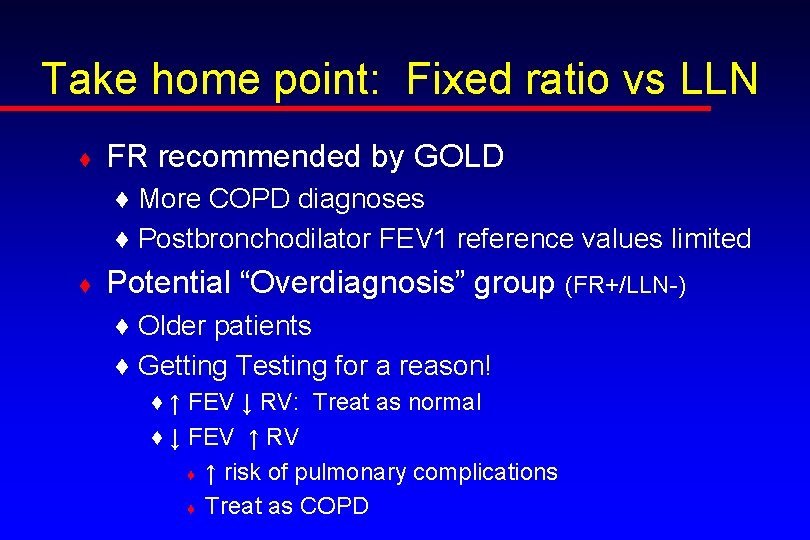
Take home point: Fixed ratio vs LLN ♦ FR recommended by GOLD ♦ More COPD diagnoses ♦ Postbronchodilator FEV 1 reference values limited ♦ Potential “Overdiagnosis” group (FR+/LLN-) ♦ Older patients ♦ Getting Testing for a reason! ♦ ↑ FEV ↓ RV: Treat as normal ♦ ↓ FEV ↑ RV ♦ ↑ risk of pulmonary complications ♦ Treat as COPD
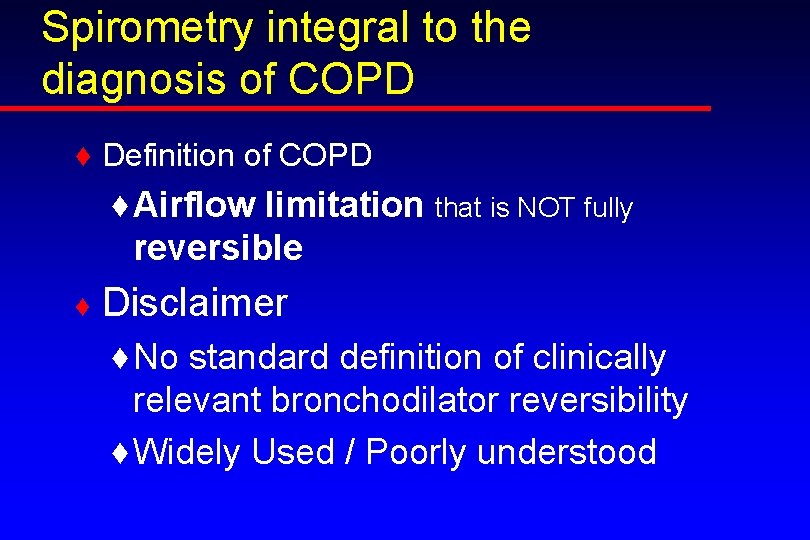
Spirometry integral to the diagnosis of COPD ♦ Definition of COPD ♦ Airflow limitation that is NOT fully reversible ♦ Disclaimer ♦ No standard definition of clinically relevant bronchodilator reversibility ♦ Widely Used / Poorly understood
Common Misconceptions about Reversibility Testing ♦ Reversibility distinguishes asthma from COPD ♦ Reversibility clearly linked to better clinical outcomes ♦ Reversibility effects choice of specific bronchodilator used in chronic management ♦ Reversibility testing is consistently reproducible
Factors affecting Reversibility Testing ♦ ♦ ♦ Criteria used to interpret Baseline FEV 1 (much less likely with ↓ FEV 1) Dose and type of bronchodilator Timing of test after drug administration Delivery technique Last dose of bronchodilator ♦ Short-acting ♦ Long-acting Hanania et al. Bronchodilator Reversibility in COPD. CHEST 2011
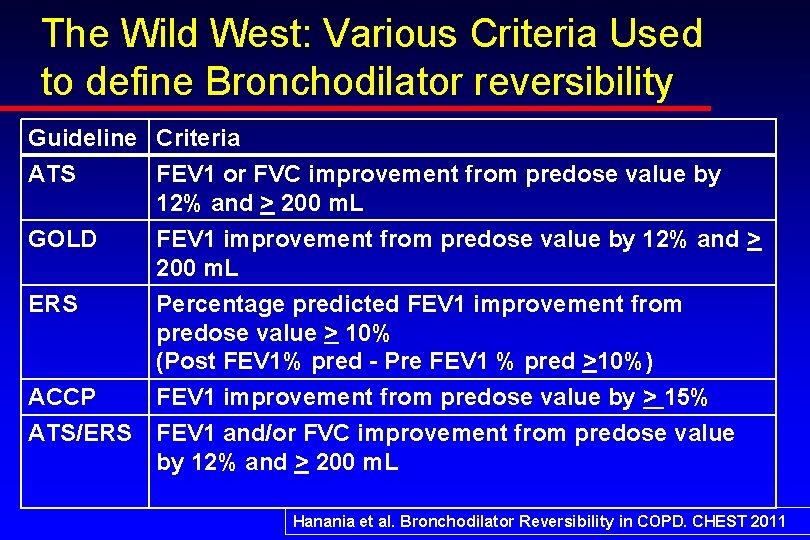
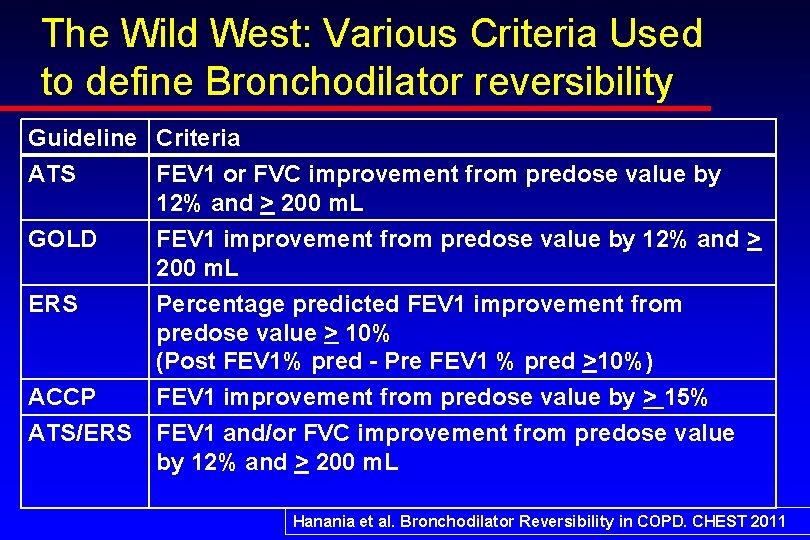
The Wild West: Various Criteria Used to define Bronchodilator reversibility Guideline Criteria ATS FEV 1 or FVC improvement from predose value by 12% and > 200 m. L GOLD FEV 1 improvement from predose value by 12% and > 200 m. L ERS Percentage predicted FEV 1 improvement from predose value > 10% (Post FEV 1% pred - Pre FEV 1 % pred >10%) ACCP FEV 1 improvement from predose value by > 15% ATS/ERS FEV 1 and/or FVC improvement from predose value by 12% and > 200 m. L Hanania et al. Bronchodilator Reversibility in COPD. CHEST 2011
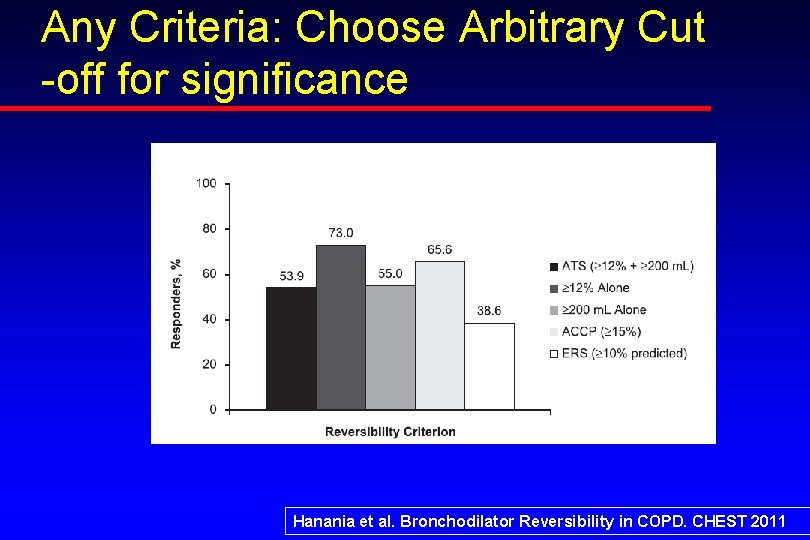
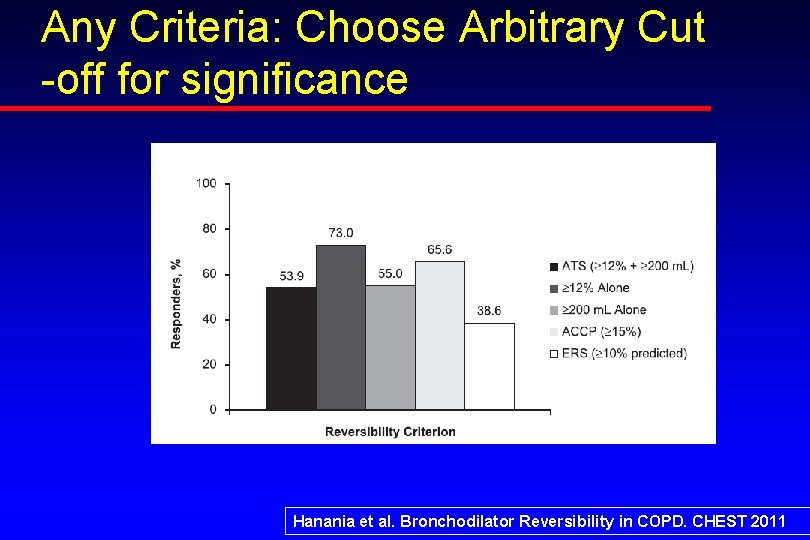
Any Criteria: Choose Arbitrary Cut -off for significance Hanania et al. Bronchodilator Reversibility in COPD. CHEST 2011
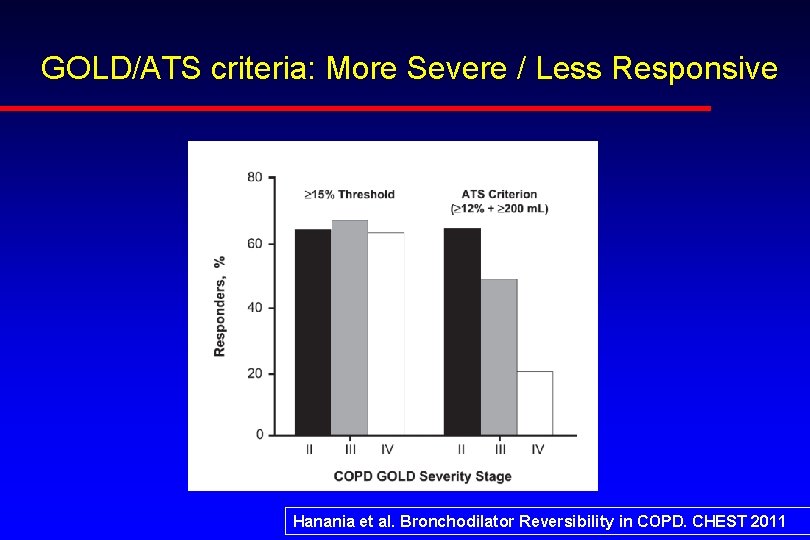
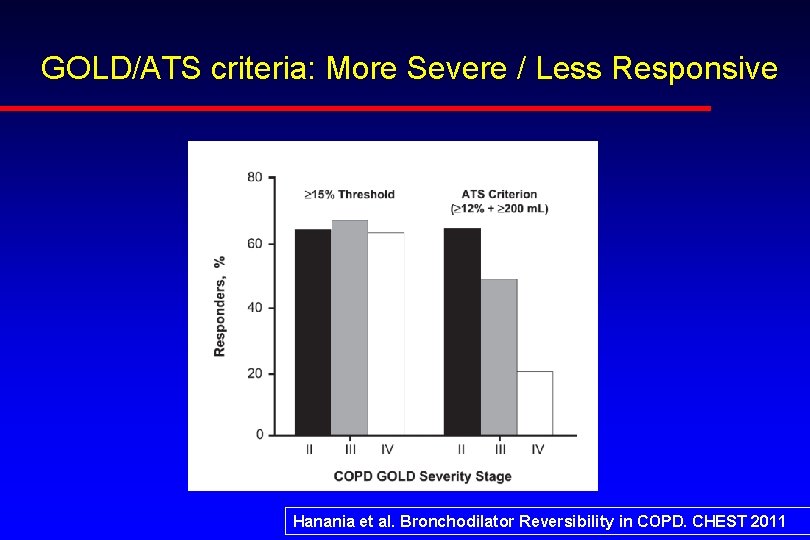
GOLD/ATS criteria: More Severe / Less Responsive Hanania et al. Bronchodilator Reversibility in COPD. CHEST 2011
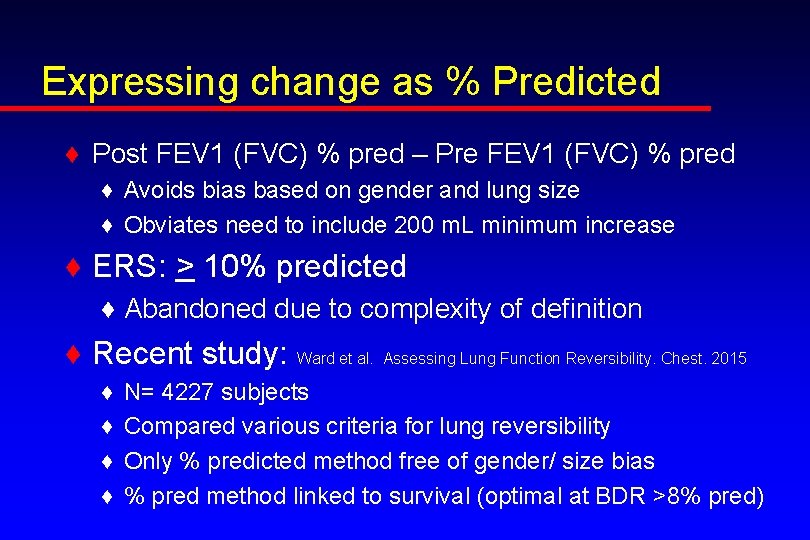
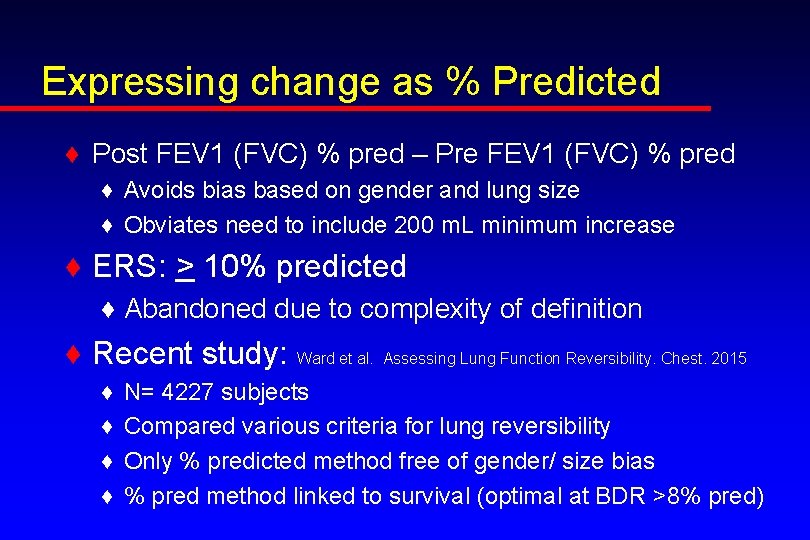
Expressing change as % Predicted ♦ Post FEV 1 (FVC) % pred – Pre FEV 1 (FVC) % pred ♦ Avoids bias based on gender and lung size ♦ Obviates need to include 200 m. L minimum increase ♦ ERS: > 10% predicted ♦ Abandoned due to complexity of definition ♦ Recent study: Ward et al. Assessing Lung Function Reversibility. Chest. 2015 ♦ ♦ N= 4227 subjects Compared various criteria for lung reversibility Only % predicted method free of gender/ size bias % pred method linked to survival (optimal at BDR >8% pred)
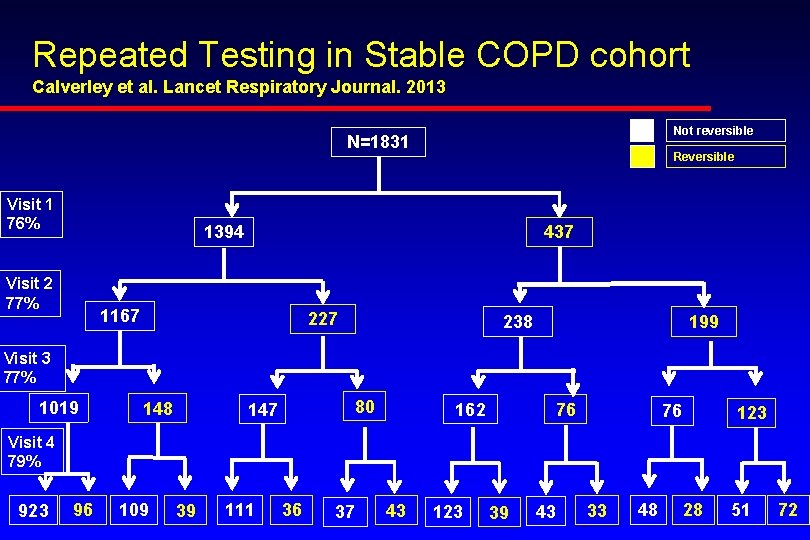
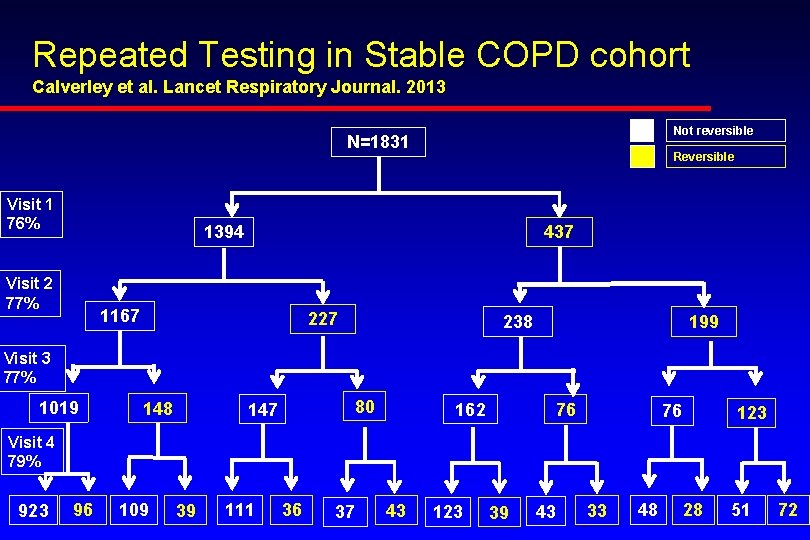
Repeated Testing in Stable COPD cohort Calverley et al. Lancet Respiratory Journal. 2013 Not reversible N=1831 Visit 1 76% Reversible 1394 Visit 2 77% 437 1167 227 238 199 Visit 3 77% 1019 148 80 147 162 76 76 123 Visit 4 79% 923 96 109 39 111 36 37 43 123 39 43 33 48 28 51 72
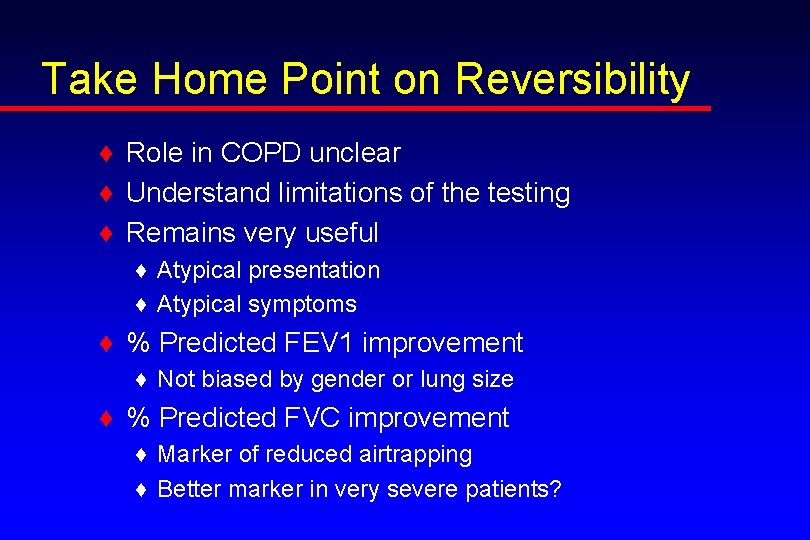
Take Home Point on Reversibility ♦ Role in COPD unclear ♦ Understand limitations of the testing ♦ Remains very useful ♦ Atypical presentation ♦ Atypical symptoms ♦ % Predicted FEV 1 improvement ♦ Not biased by gender or lung size ♦ % Predicted FVC improvement ♦ Marker of reduced airtrapping ♦ Better marker in very severe patients?
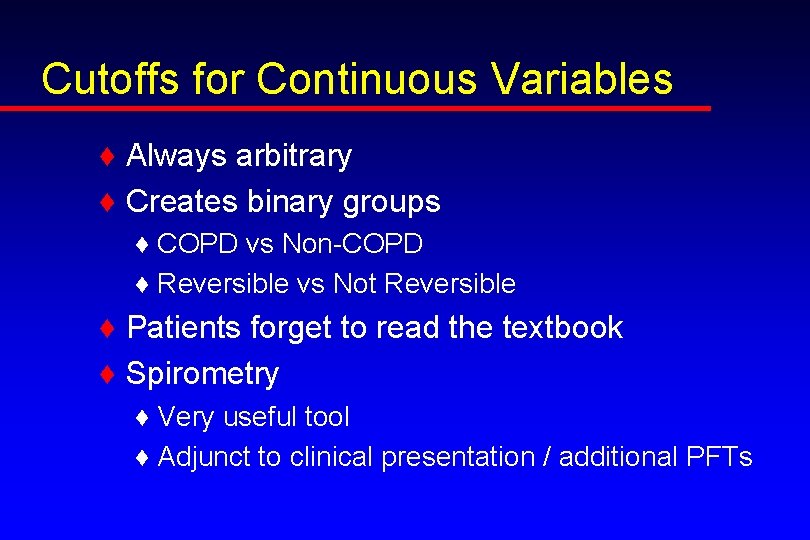
Cutoffs for Continuous Variables ♦ Always arbitrary ♦ Creates binary groups ♦ COPD vs Non-COPD ♦ Reversible vs Not Reversible ♦ Patients forget to read the textbook ♦ Spirometry ♦ Very useful tool ♦ Adjunct to clinical presentation / additional PFTs
Questions