Update on Primary Care Networks Dr Dianne Aitken



- Slides: 7

Update on Primary Care Networks Dr Dianne Aitken – Governing Body Member, NHS Lambeth CCG
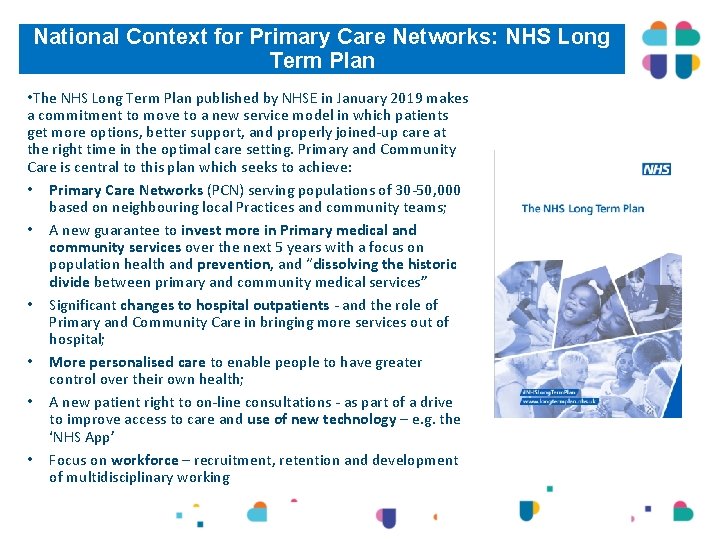
National Context for Primary Care Networks: NHS Long Term Plan • The NHS Long Term Plan published by NHSE in January 2019 makes a commitment to move to a new service model in which patients get more options, better support, and properly joined-up care at the right time in the optimal care setting. Primary and Community Care is central to this plan which seeks to achieve: • Primary Care Networks (PCN) serving populations of 30 -50, 000 based on neighbouring local Practices and community teams; • A new guarantee to invest more in Primary medical and community services over the next 5 years with a focus on population health and prevention, and “dissolving the historic divide between primary and community medical services” • Significant changes to hospital outpatients - and the role of Primary and Community Care in bringing more services out of hospital; • More personalised care to enable people to have greater control over their own health; • A new patient right to on-line consultations - as part of a drive to improve access to care and use of new technology – e. g. the ‘NHS App’ • Focus on workforce – recruitment, retention and development of multidisciplinary working

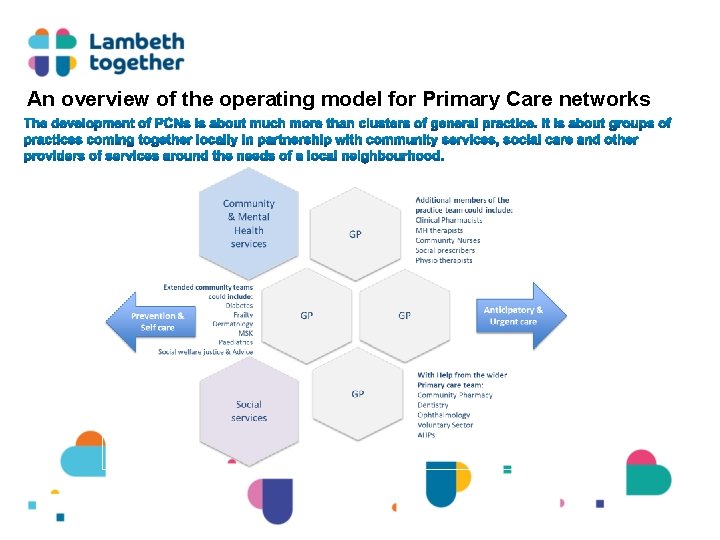
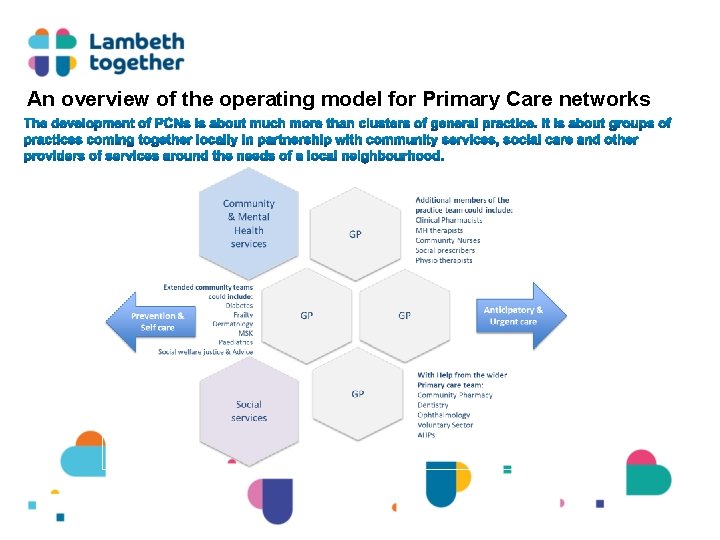
An overview of the operating model for Primary Care networks

New Workforce for PCNs The five reimbursable roles are: • • • clinical pharmacists (from 2019) social prescribing link workers (from 2019) physician associates (from 2020) first contact physiotherapists (from 2020) first contact community paramedics (from 2021)
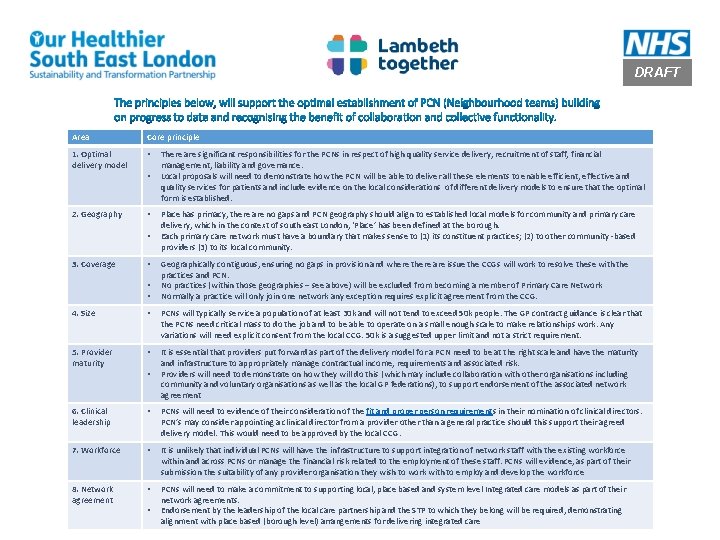
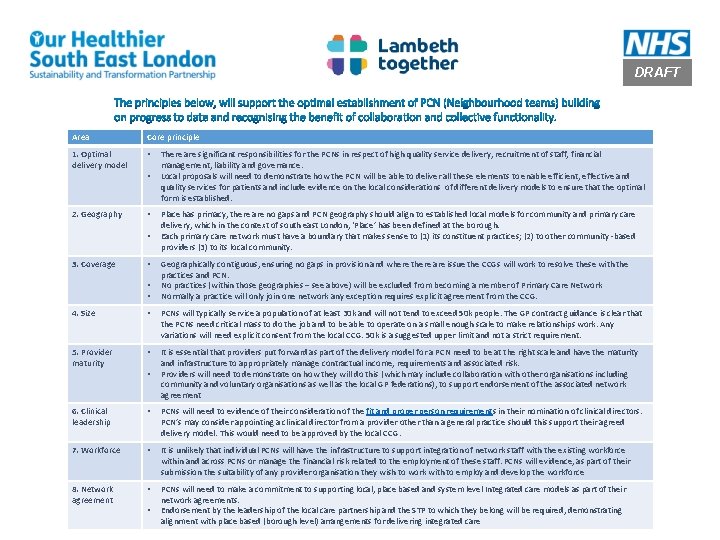
DRAFT Area Core principle 1. Optimal delivery model • 2. Geography • • • 3. Coverage • • • There are significant responsibilities for the PCNs in respect of high quality service delivery, recruitment of staff, financial management, liability and governance. Local proposals will need to demonstrate how the PCN will be able to deliver all these elements to enable efficient, effective and quality services for patients and include evidence on the local considerations of different delivery models to ensure that the optimal form is established. Place has primacy, there are no gaps and PCN geography should align to established local models for community and primary care delivery, which in the context of south east London, ‘Place’ has been defined at the borough. Each primary care network must have a boundary that makes sense to (1) its constituent practices; (2) to other community -based providers (3) to its local community. Geographically contiguous, ensuring no gaps in provision and where there are issue the CCGs will work to resolve these with the practices and PCN. No practices (within those geographies – see above) will be excluded from becoming a member of Primary Care Network Normally a practice will only join one network any exception requires explicit agreement from the CCG. 4. Size • PCNs will typically service a population of at least 30 k and will not tend to exceed 50 k people. The GP contract guidance is clear that the PCNs need critical mass to do the job and to be able to operate on a small enough scale to make relationships work. Any variations will need explicit consent from the local CCG. 50 k is a suggested upper limit and not a strict requirement. 5. Provider maturity • It is essential that providers put forward as part of the delivery model for a PCN need to be at the right scale and have the maturity and infrastructure to appropriately manage contractual income, requirements and associated risk. Providers will need to demonstrate on how they will do this (which may include collaboration with other organisations including community and voluntary organisations as well as the local GP federations), to support endorsement of the associated network agreement 6. Clinical leadership • PCNs will need to evidence of their consideration of the fit and proper person requirements in their nomination of clinical directors. PCN’s may consider appointing a clinical director from a provider other than a general practice should this support their agreed delivery model. This would need to be approved by the local CCG. 7. Workforce • It is unlikely that individual PCNs will have the infrastructure to support integration of network staff with the existing workforce within and across PCNs or manage the financial risk related to the employment of these staff. PCNs will evidence, as part of 7 their submission the suitability of any provider organisation they wish to work with to employ and develop the workforce 8. Network agreement • PCNs will need to make a commitment to supporting local, place based and system level Integrated care models as part of their network agreements. Endorsement by the leadership of the local care partnership and the STP to which they belong will be required, demonstrating alignment with place based (borough level) arrangements for delivering integrated care • •