Update on hypertension complications and HTN management Prof





- Slides: 38
Update on hypertension complications and HTN management Prof. Vang Chu MD. , Ph. D. , FAs. CC, FACC, FESC Director of the Lao-Luxembourg Heart Centre President of the Lao Cardiac Society
Lecture Contents Ø Burden of hypertension and its complications Ø Update on hypertension management
Lecture Contents Ø Burden of hypertension and its complications
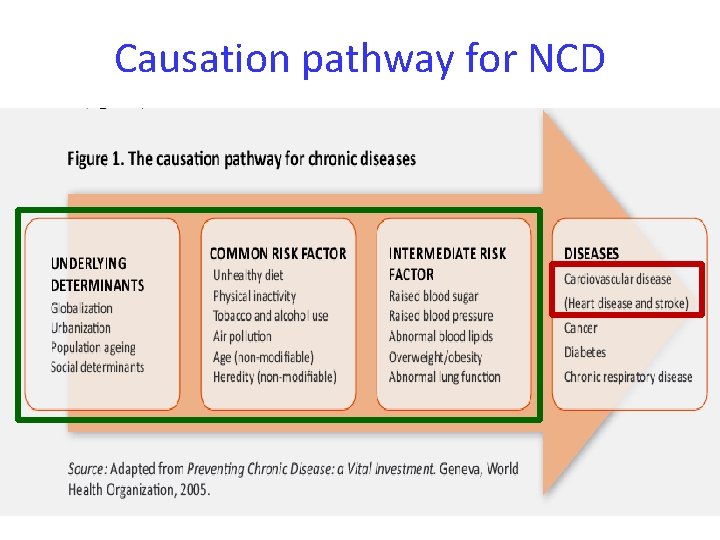
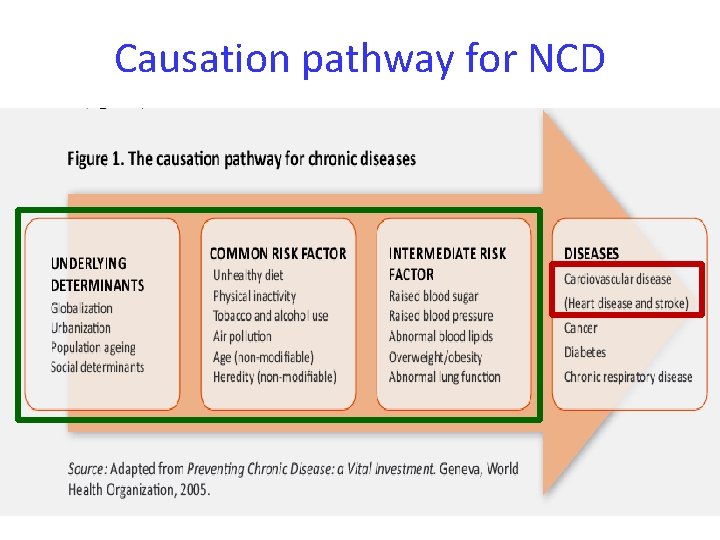
Causation pathway for NCD
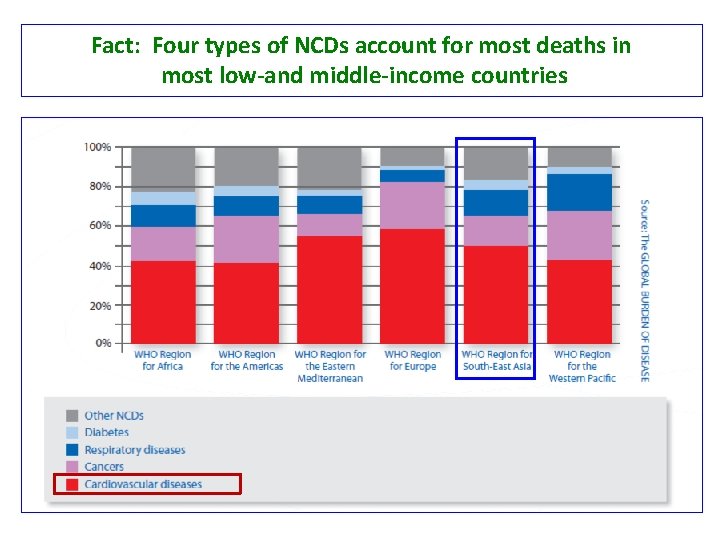
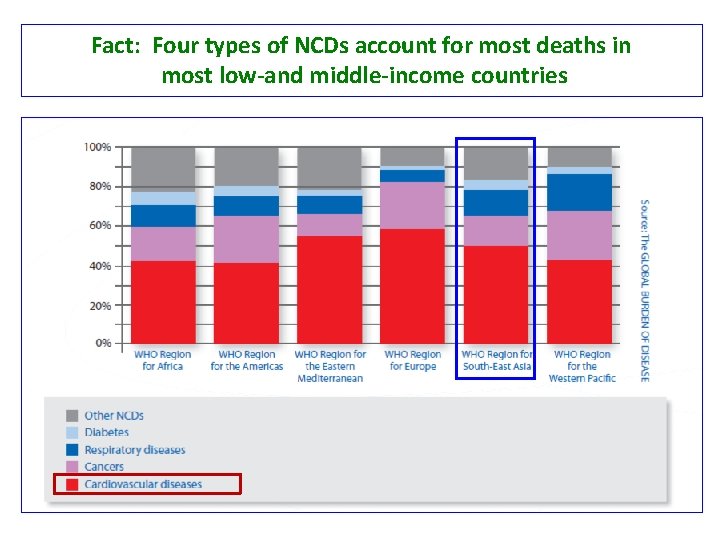
Fact: Four types of NCDs account for most deaths in most low-and middle-income countries
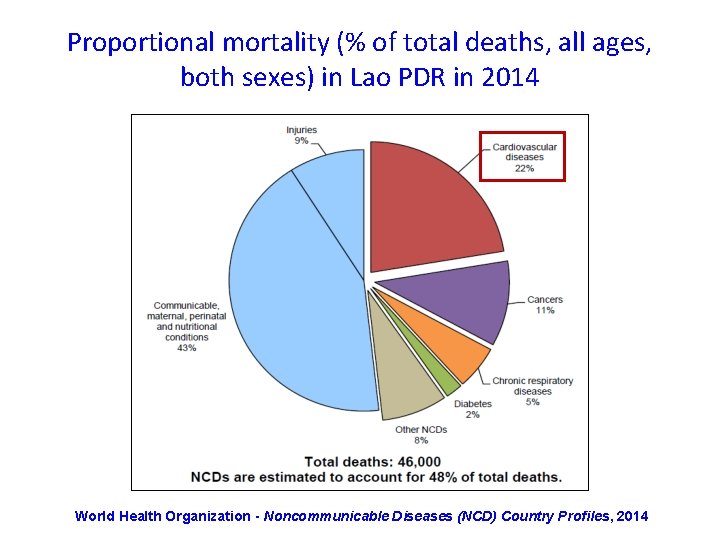
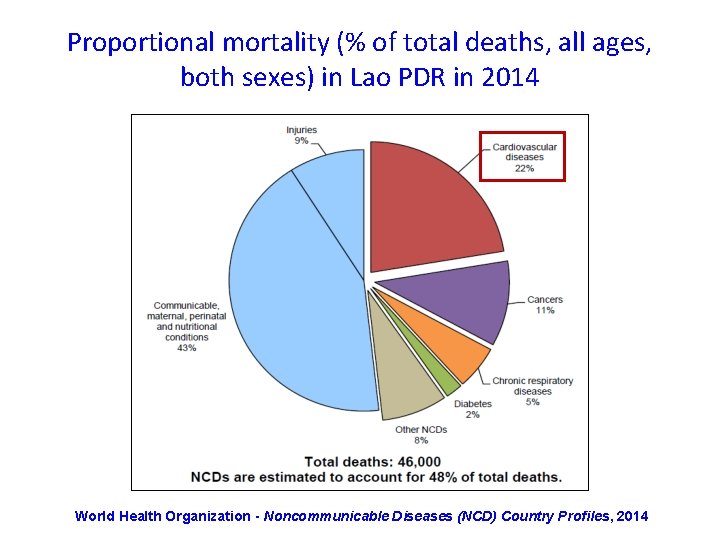
Proportional mortality (% of total deaths, all ages, both sexes) in Lao PDR in 2014 World Health Organization - Noncommunicable Diseases (NCD) Country Profiles, 2014
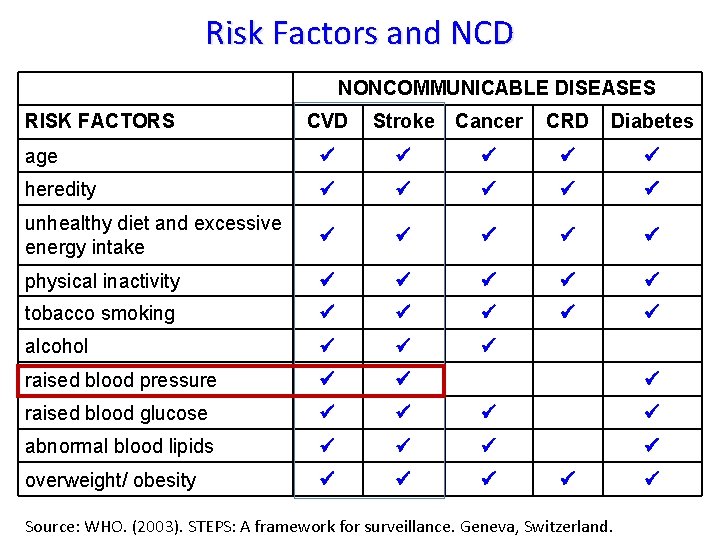
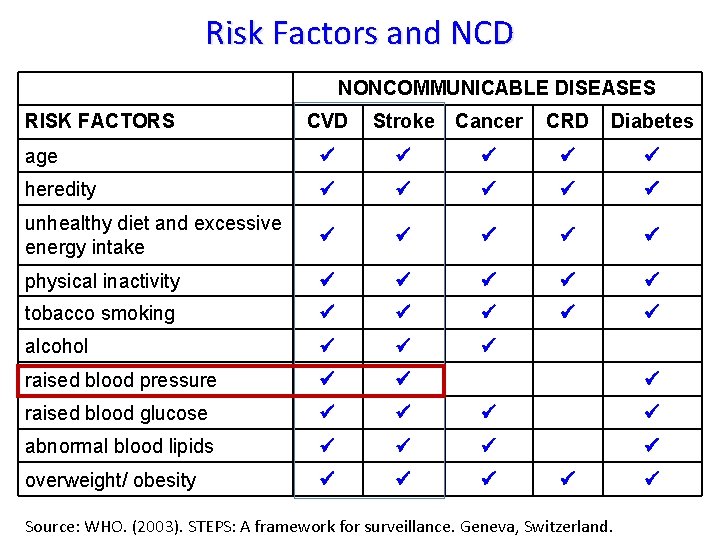
Risk Factors and NCD NONCOMMUNICABLE DISEASES RISK FACTORS CVD Stroke Cancer CRD Diabetes age heredity unhealthy diet and excessive energy intake physical inactivity tobacco smoking alcohol raised blood pressure raised blood glucose abnormal blood lipids overweight/ obesity Source: WHO. (2003). STEPS: A framework for surveillance. Geneva, Switzerland.
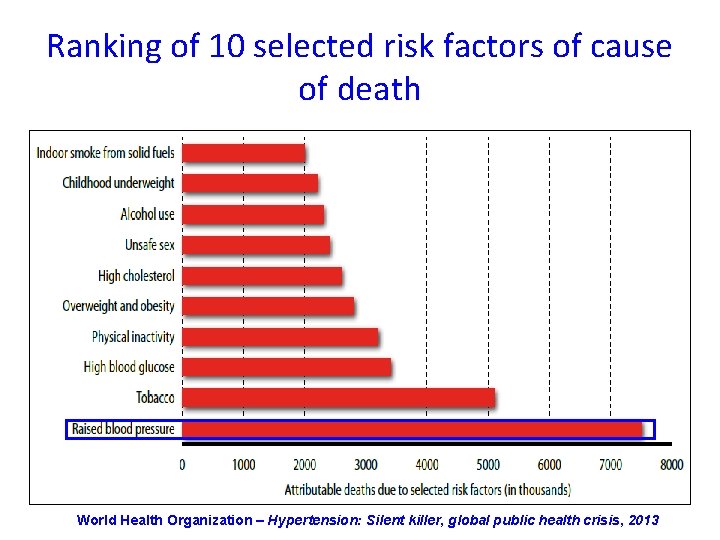
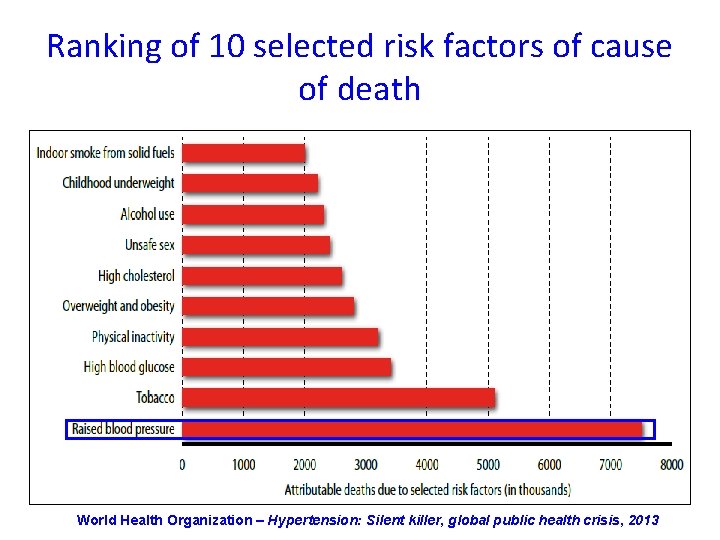
Ranking of 10 selected risk factors of cause of death World Health Organization – Hypertension: Silent killer, global public health crisis, 2013
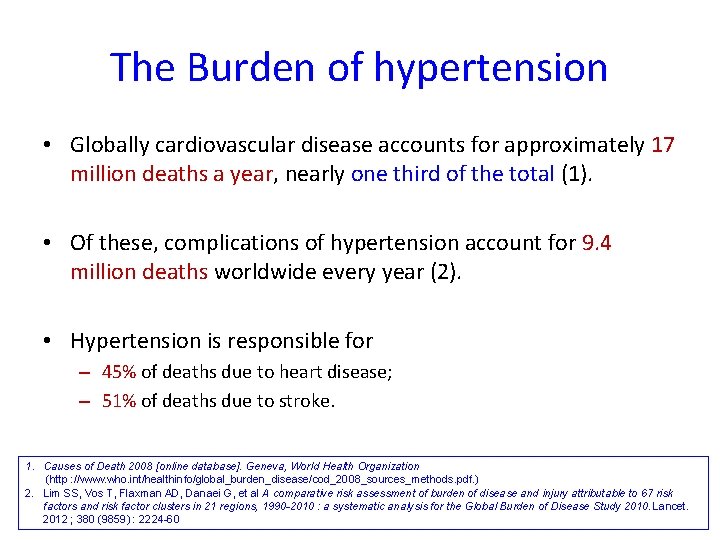
The Burden of hypertension • Globally cardiovascular disease accounts for approximately 17 million deaths a year, nearly one third of the total (1). • Of these, complications of hypertension account for 9. 4 million deaths worldwide every year (2). • Hypertension is responsible for – 45% of deaths due to heart disease; – 51% of deaths due to stroke. 1. Causes of Death 2008 [online database]. Geneva, World Health Organization (http : //www. who. int/healthinfo/global_burden_disease/cod_2008_sources_methods. pdf. ) 2. Lim SS, Vos T, Flaxman AD, Danaei G, et al A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990 -2010 : a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012 ; 380 (9859) : 2224 -60
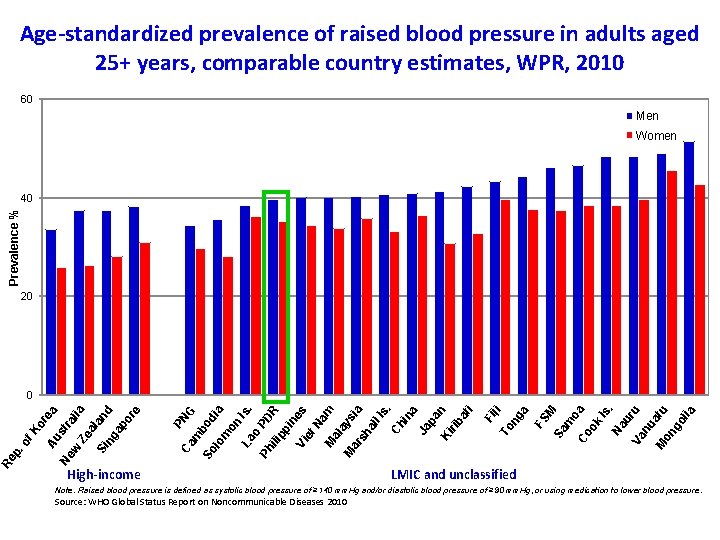
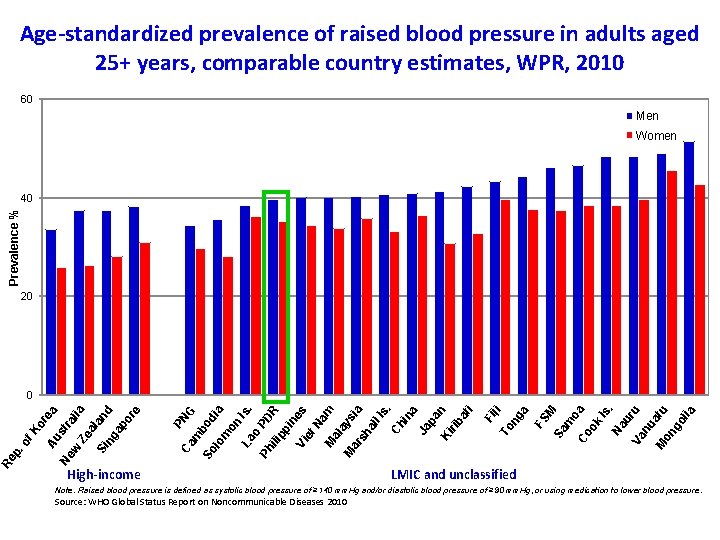
Age-standardized prevalence of raised blood pressure in adults aged 25+ years, comparable country estimates, WPR, 2010 60 Men Women Prevalence % 40 20 High-income FS M Sa m o Co a ok Is. Na u Va ru nu at M on u go lia a ng ji Ph ili To Fi pp in es Vi et Na m M al ay M si ar sh a al l. I s. Ch in a Ja pa Ki n rib at i Is. PD R o La So l om on di a G bo m PN Ca Ze ia a Si land ng ap or e ra l w st Au Ne Re p. of Ko re a 0 LMIC and unclassified Note: Raised blood pressure is defined as systolic blood pressure of ≥ 140 mm. Hg and/or diastolic blood pressure of ≥ 90 mm. Hg, or using medication to lower blood pressure. Source: WHO Global Status Report on Noncommunicable Diseases 2010
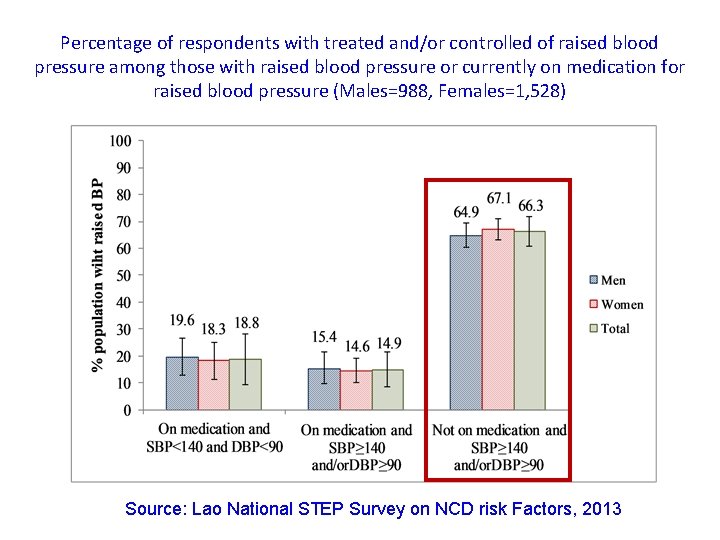
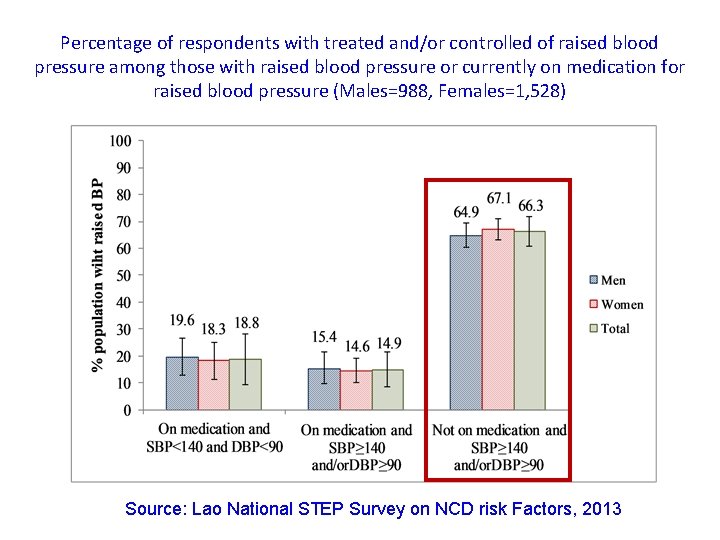
Percentage of respondents with treated and/or controlled of raised blood pressure among those with raised blood pressure or currently on medication for raised blood pressure (Males=988, Females=1, 528) Source: Lao National STEP Survey on NCD risk Factors, 2013

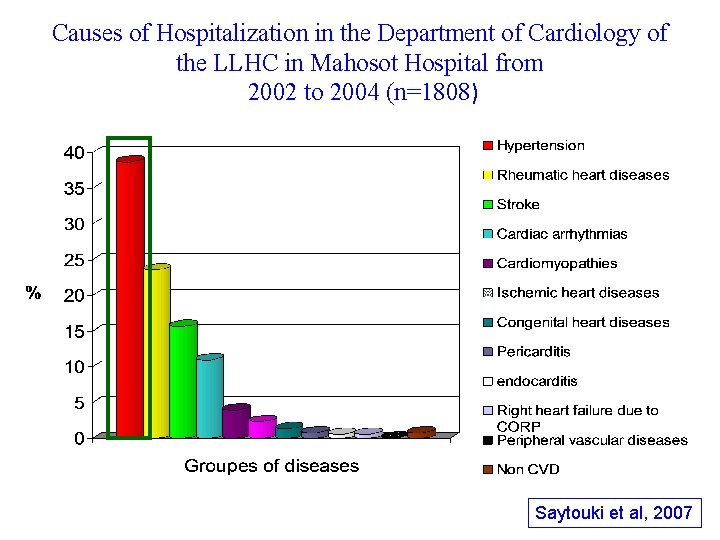
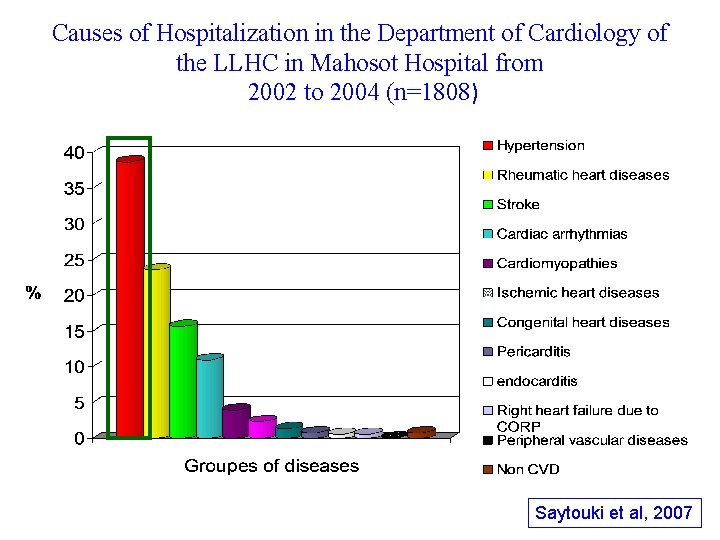
Causes of Hospitalization in the Department of Cardiology of the LLHC in Mahosot Hospital from 2002 to 2004 (n=1808) Saytouki et al, 2007

Is the current hospital admission due to hypertension complications ? (n= 329) 23% Yes 77% Yang N & Vang C, 2013 No
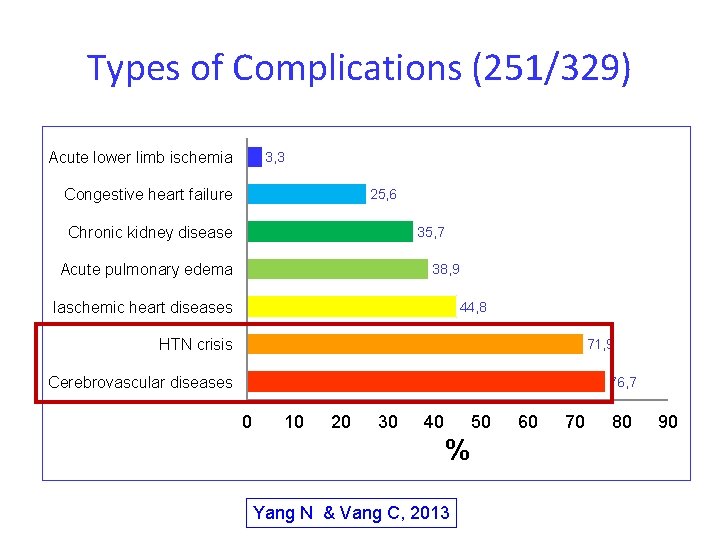
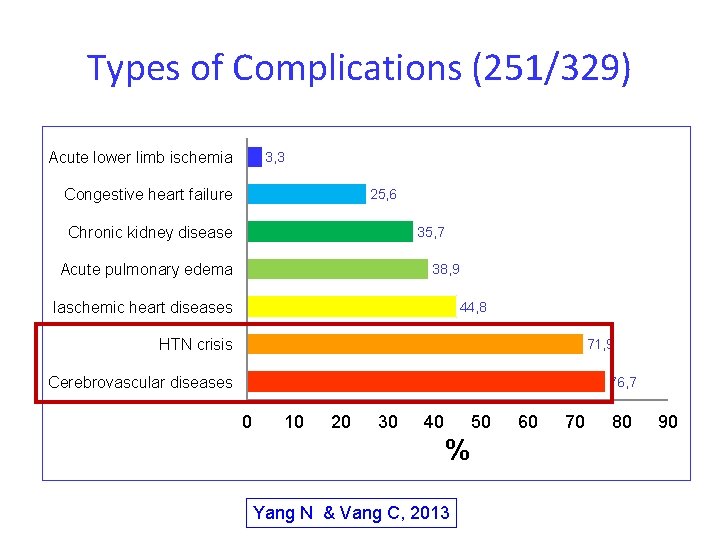
Types of Complications (251/329) Acute lower limb ischemia 3, 3 Congestive heart failure 25, 6 Chronic kidney disease 35, 7 Acute pulmonary edema 38, 9 Iaschemic heart diseases 44, 8 HTN crisis 71, 9 Cerebrovascular diseases 76, 7 0 10 20 30 40 50 % Yang N & Vang C, 2013 60 70 80 90
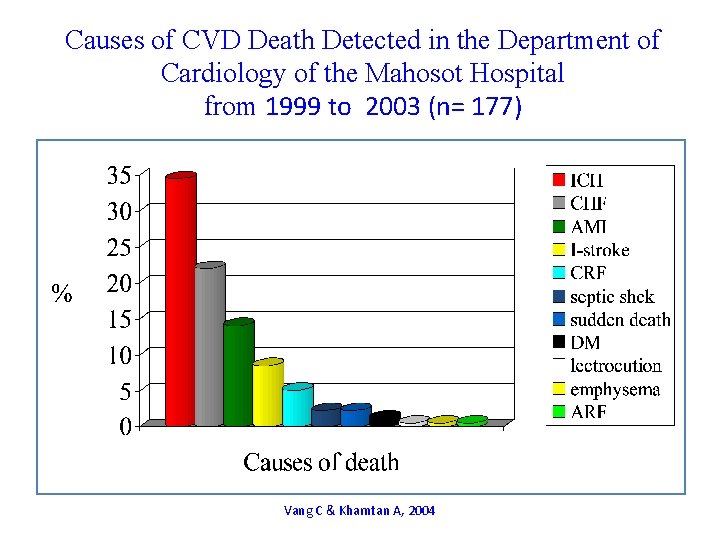
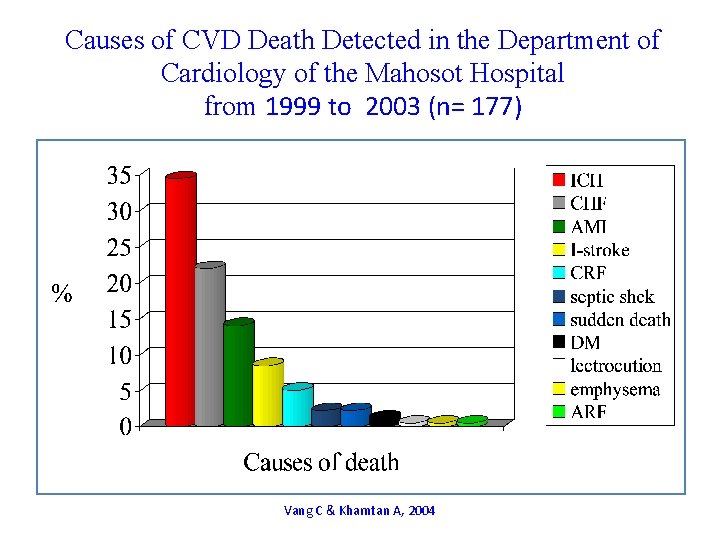
Causes of CVD Death Detected in the Department of Cardiology of the Mahosot Hospital from 1999 to 2003 (n= 177) Vang C & Khamtan A, 2004
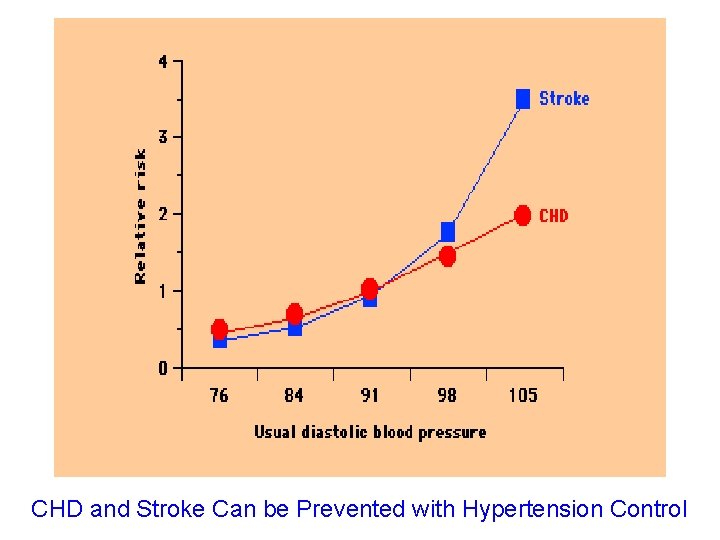
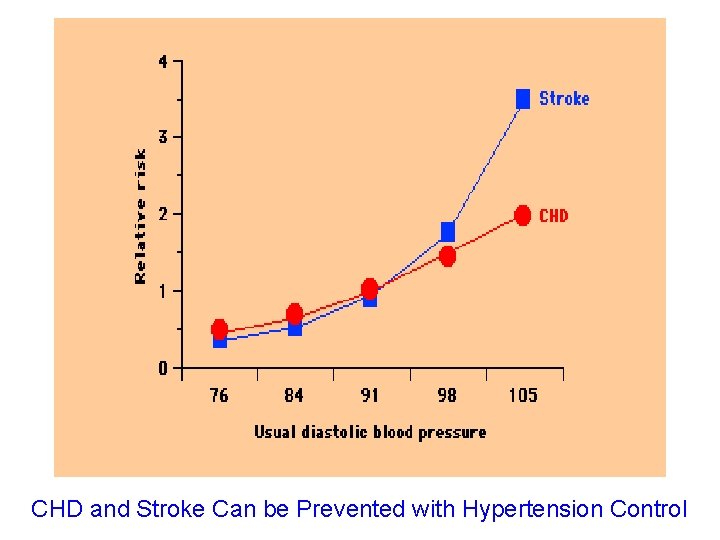
CHD and Stroke Can be Prevented with Hypertension Control
Lecture Contents Ø Update on hypertension management

World Heart Day 2013: Hypertension- A silent killer, global public health crisis
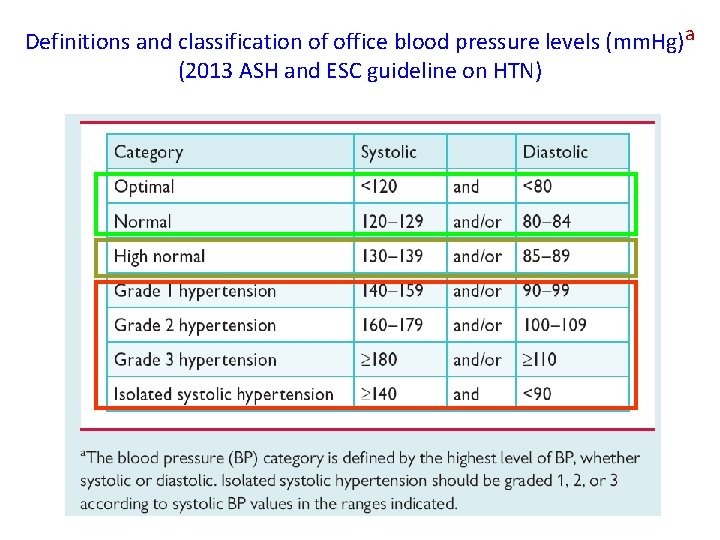
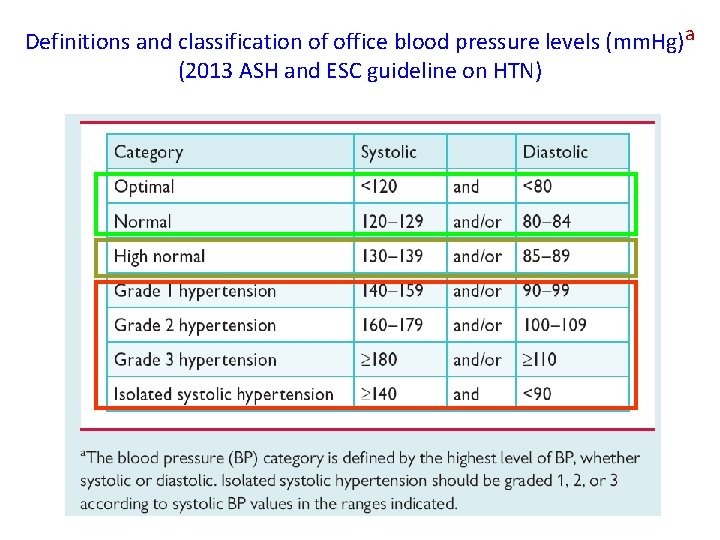
Definitions and classification of office blood pressure levels (mm. Hg)a (2013 ASH and ESC guideline on HTN)
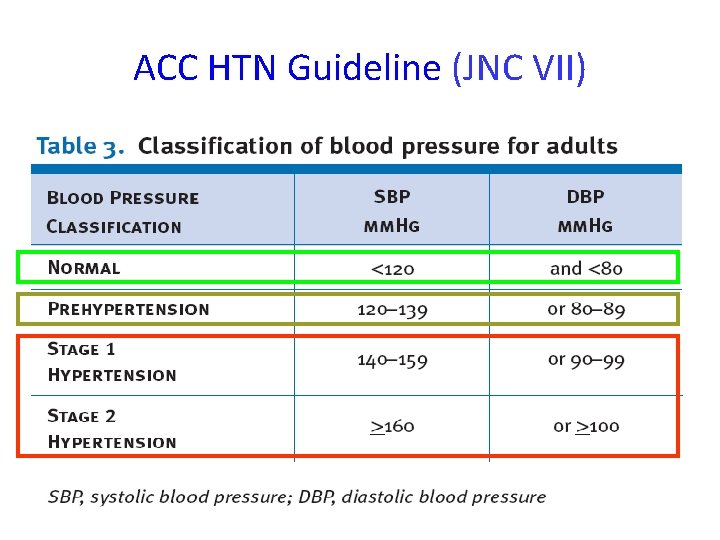
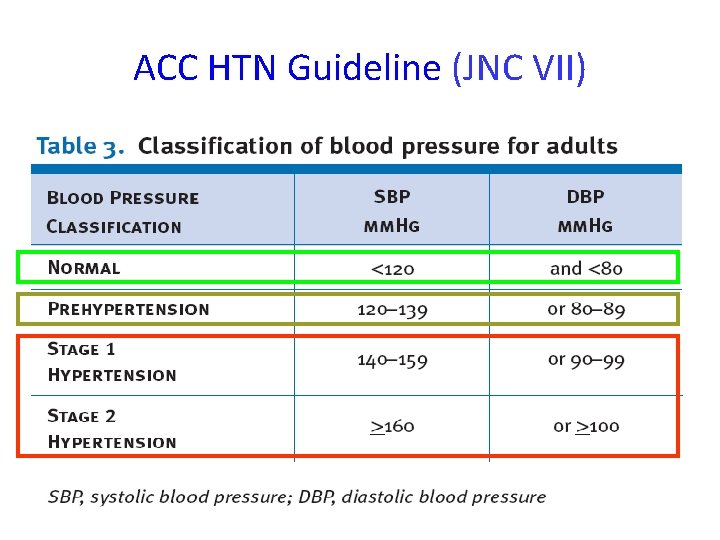
ACC HTN Guideline (JNC VII)
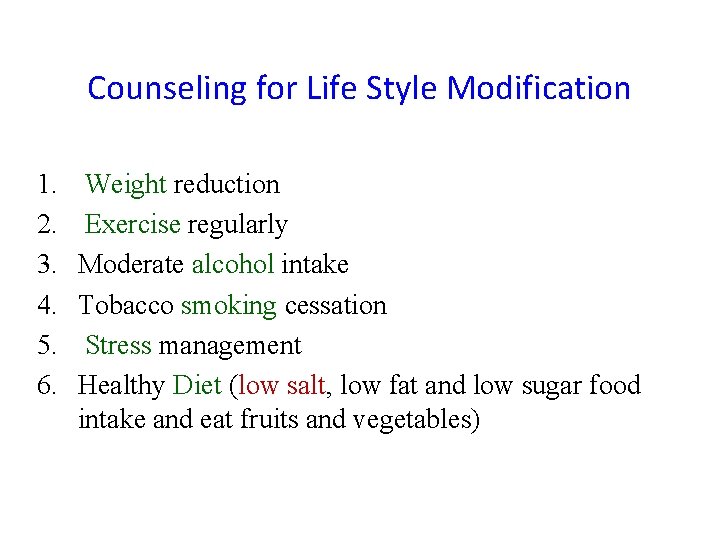
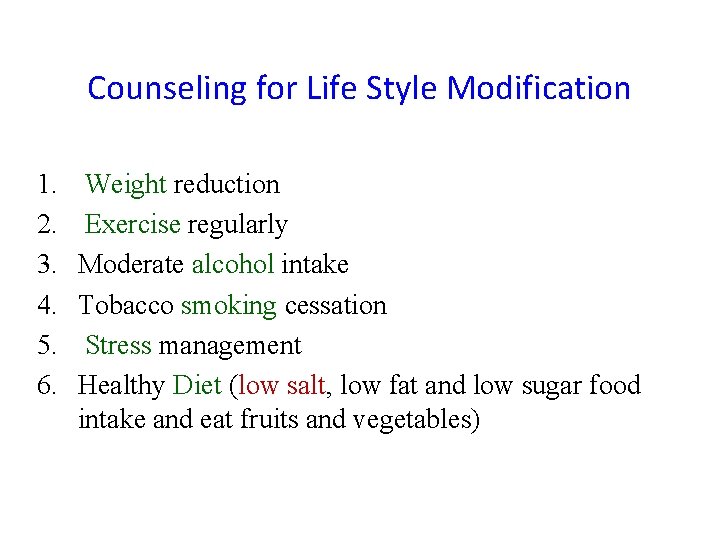
Counseling for Life Style Modification 1. 2. 3. 4. 5. 6. Weight reduction Exercise regularly Moderate alcohol intake Tobacco smoking cessation Stress management Healthy Diet (low salt, low fat and low sugar food intake and eat fruits and vegetables)
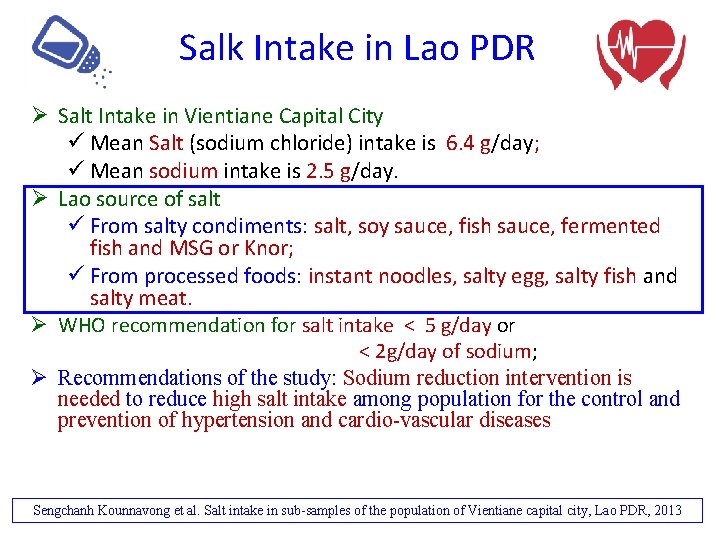
Salk Intake in Lao PDR Ø Salt Intake in Vientiane Capital City ü Mean Salt (sodium chloride) intake is 6. 4 g/day; ü Mean sodium intake is 2. 5 g/day. Ø Lao source of salt ü From salty condiments: salt, soy sauce, fish sauce, fermented fish and MSG or Knor; ü From processed foods: instant noodles, salty egg, salty fish and salty meat. Ø WHO recommendation for salt intake < 5 g/day or < 2 g/day of sodium; Ø Recommendations of the study: Sodium reduction intervention is needed to reduce high salt intake among population for the control and prevention of hypertension and cardio-vascular diseases Sengchanh Kounnavong et al. Salt intake in sub-samples of the population of Vientiane capital city, Lao PDR, 2013
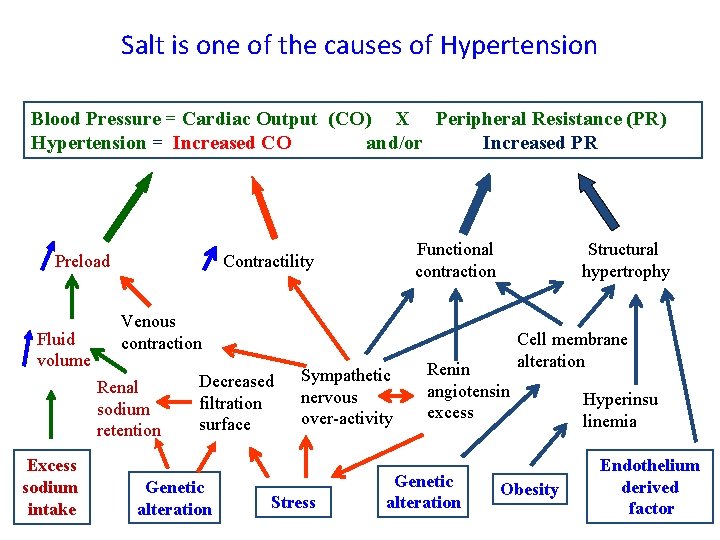
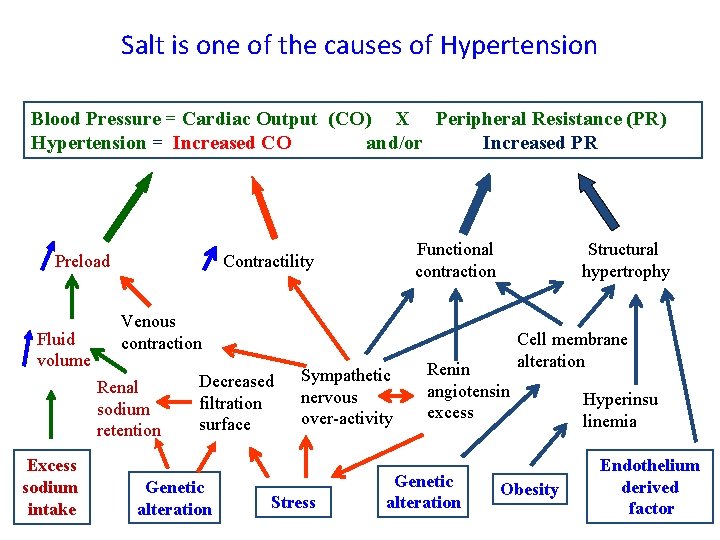
Salt is one of the causes of Hypertension Blood Pressure = Cardiac Output (CO) X Peripheral Resistance (PR) Hypertension = Increased CO and/or Increased PR Preload Fluid volume Structural hypertrophy Venous contraction Renal sodium retention Excess sodium intake Functional contraction Contractility Decreased filtration surface Genetic alteration Sympathetic nervous over-activity Stress Renin angiotensin excess Genetic alteration Cell membrane alteration Obesity Hyperinsu linemia Endothelium derived factor
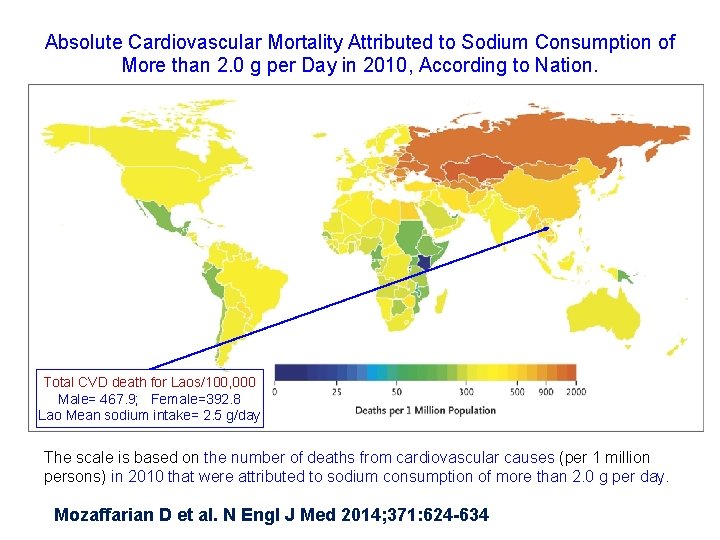
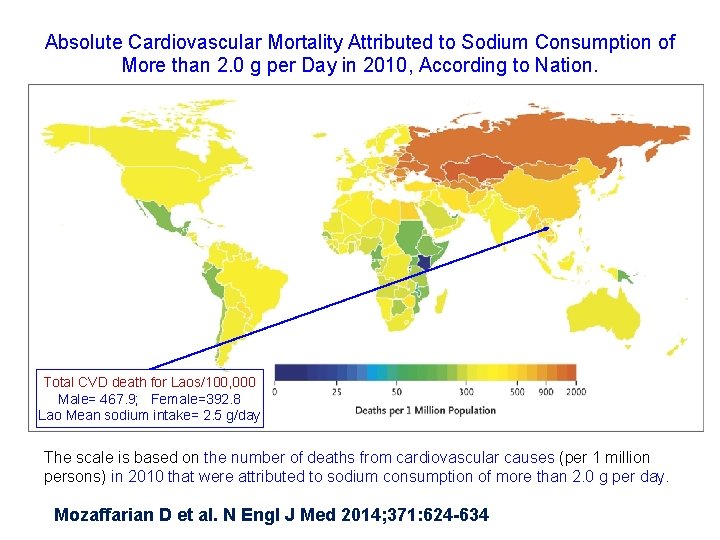
Absolute Cardiovascular Mortality Attributed to Sodium Consumption of More than 2. 0 g per Day in 2010, According to Nation. Total CVD death for Laos/100, 000 Male= 467. 9; Female=392. 8 Lao Mean sodium intake= 2. 5 g/day The scale is based on the number of deaths from cardiovascular causes (per 1 million persons) in 2010 that were attributed to sodium consumption of more than 2. 0 g per day. Mozaffarian D et al. N Engl J Med 2014; 371: 624 -634
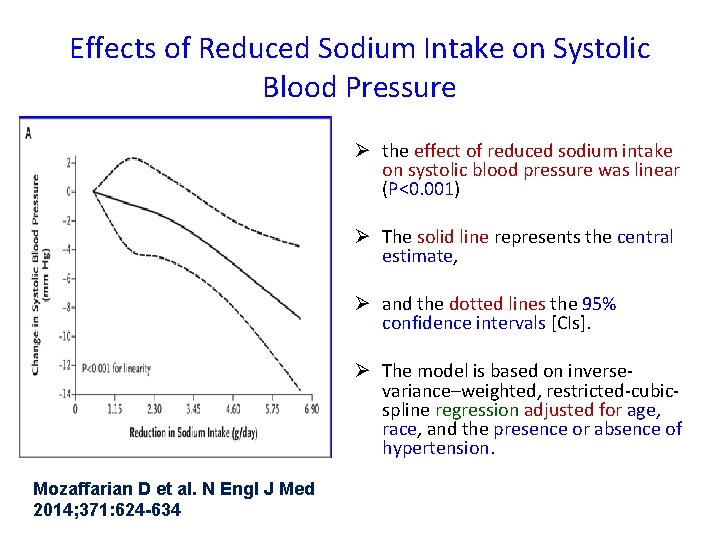
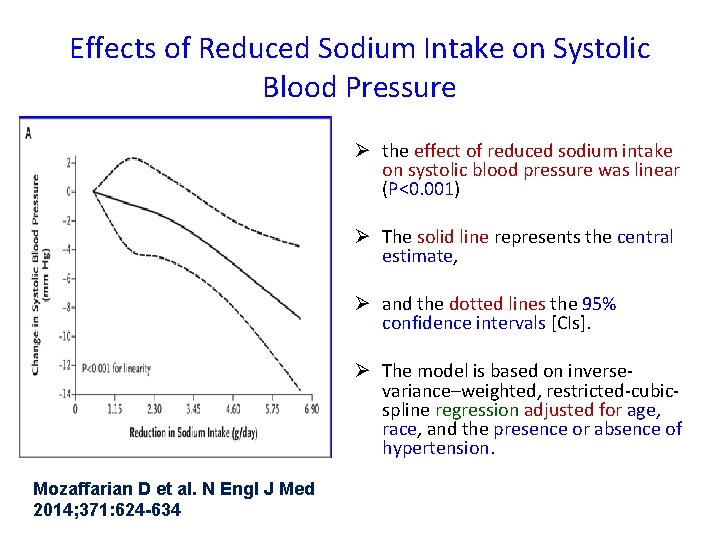
Effects of Reduced Sodium Intake on Systolic Blood Pressure Ø the effect of reduced sodium intake on systolic blood pressure was linear (P<0. 001) Ø The solid line represents the central estimate, Ø and the dotted lines the 95% confidence intervals [CIs]. Ø The model is based on inversevariance–weighted, restricted-cubicspline regression adjusted for age, race, and the presence or absence of hypertension. Mozaffarian D et al. N Engl J Med 2014; 371: 624 -634

Less salt please! Ø Worldwide salt intake is 10 g/day Ø WHO’s recommendation for salt intake is < 5 g/day or < 1 teaspoon /day
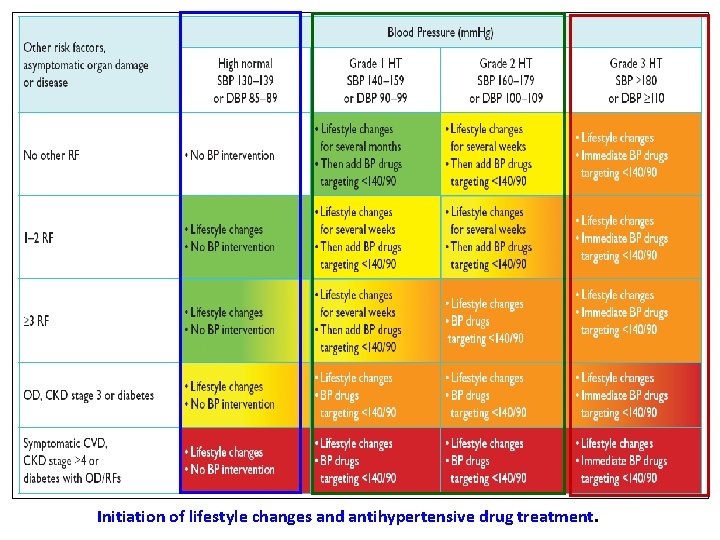
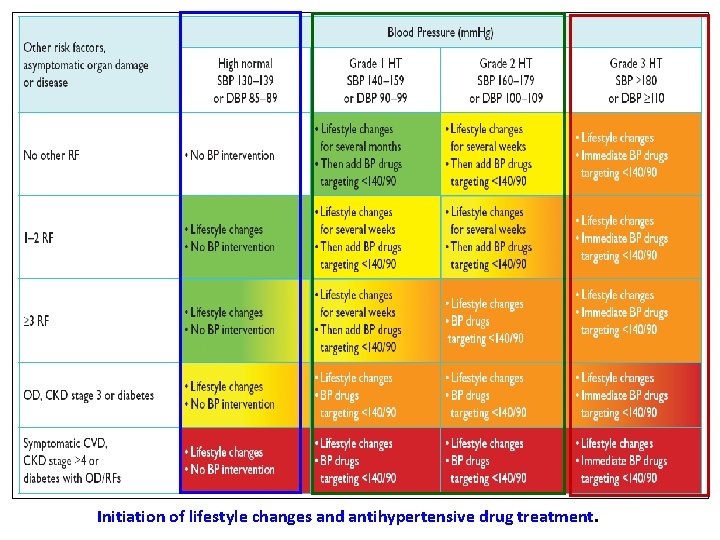
Initiation of lifestyle changes and antihypertensive drug treatment.
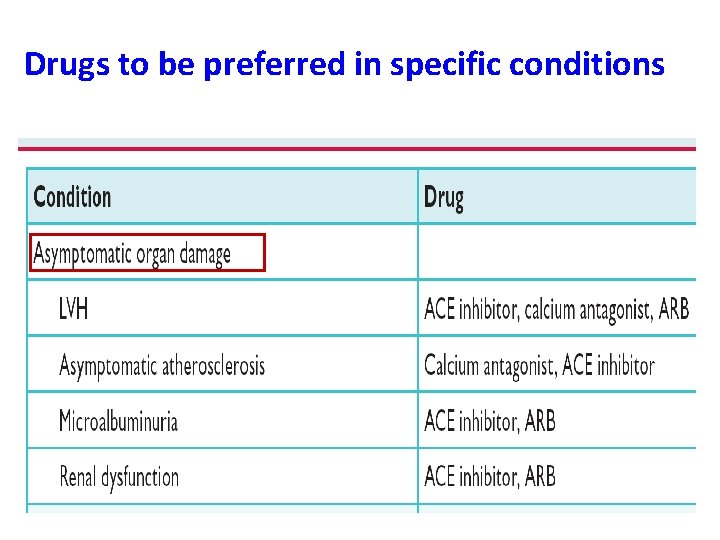
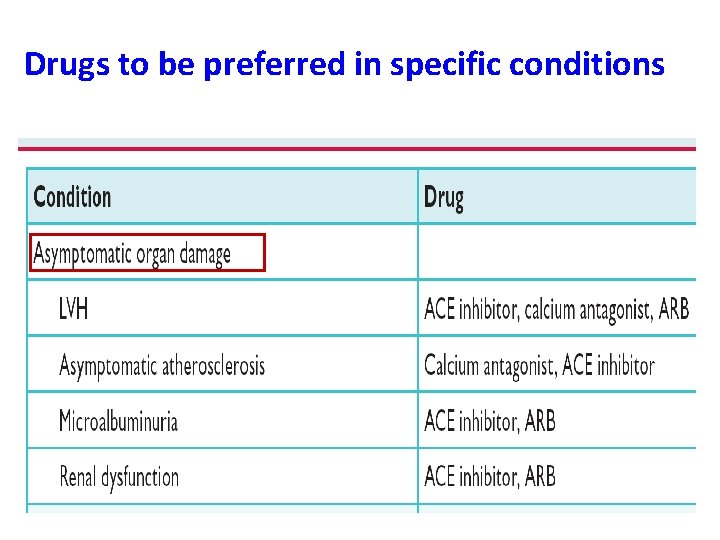
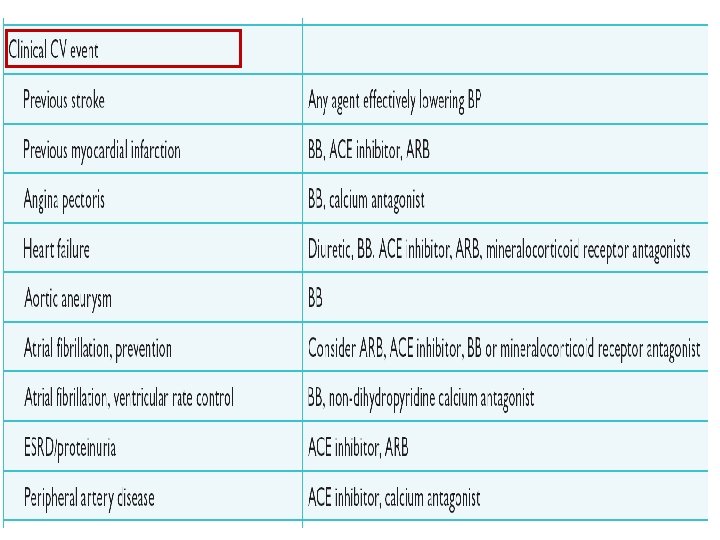
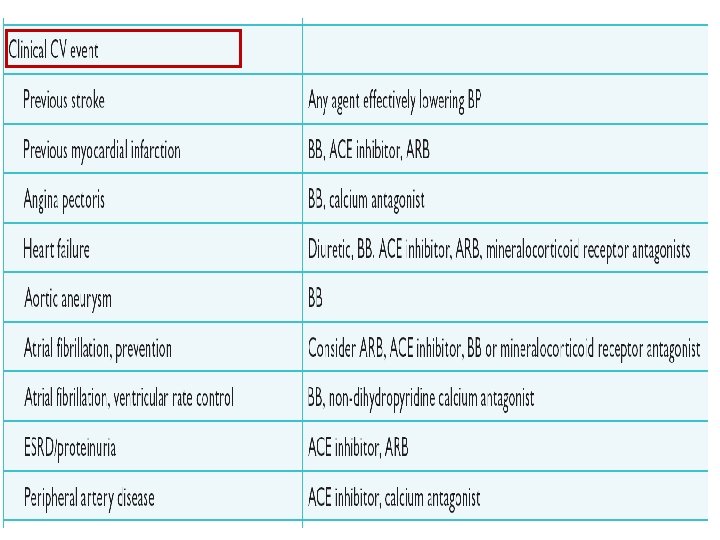
Drugs to be preferred in specific conditions

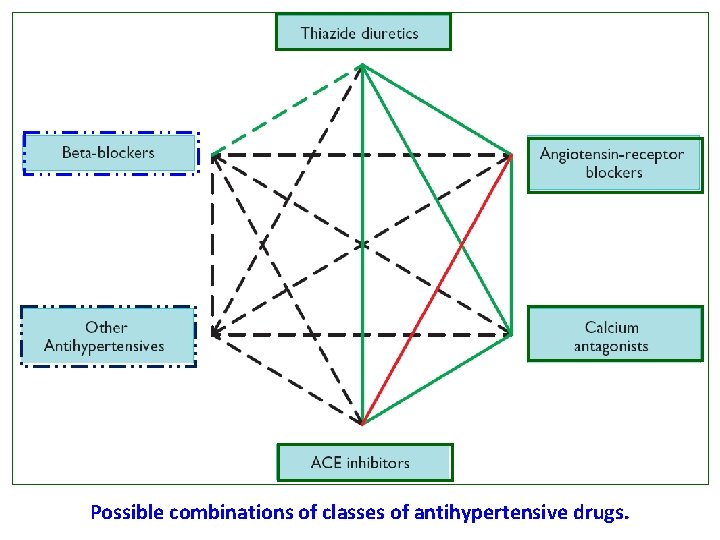
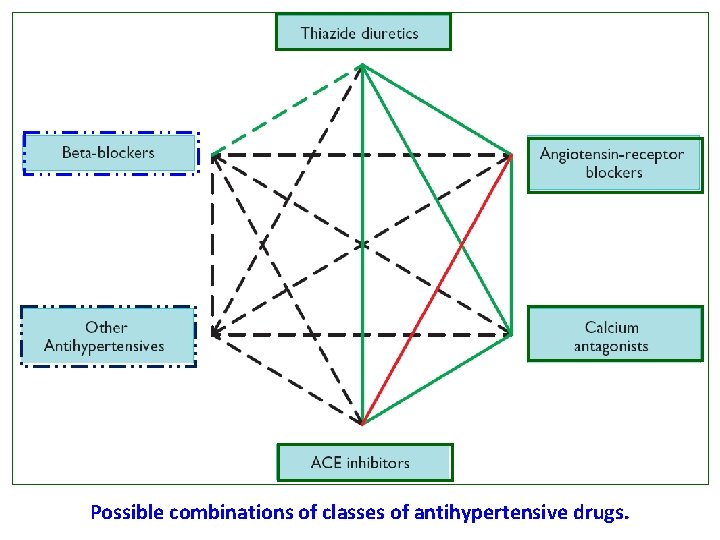
Possible combinations of classes of antihypertensive drugs.
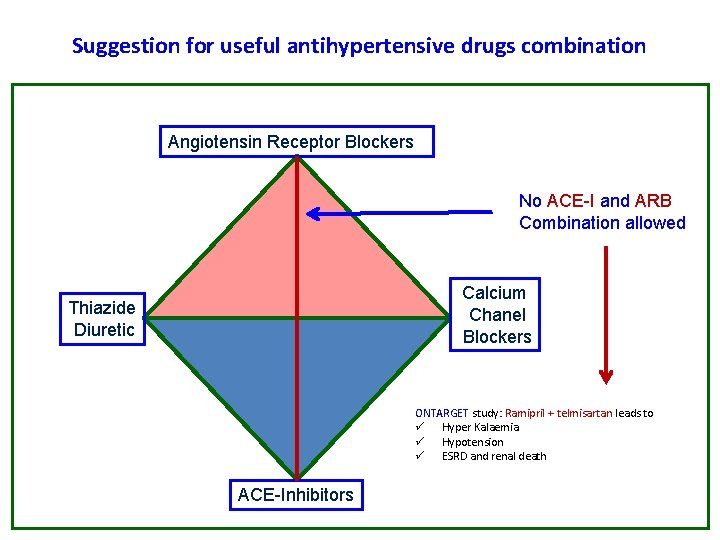
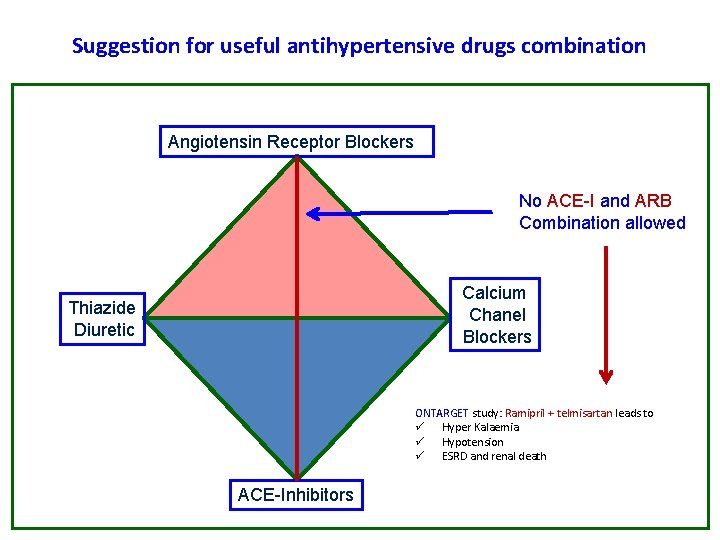
Suggestion for useful antihypertensive drugs combination Angiotensin Receptor Blockers No ACE-I and ARB Combination allowed Calcium Chanel Blockers Thiazide Diuretic ONTARGET study: Ramipril + telmisartan leads to ü Hyper Kalaemia ü Hypotension ü ESRD and renal death ACE-Inhibitors
Beta Blockers indication • • • Stable angina Previous MI Atrial fibrillation, Ventricular rate control Heart failure Excitation by sympathetic nerve (e. g. Hyperthyroidism, anxiety neurosis)
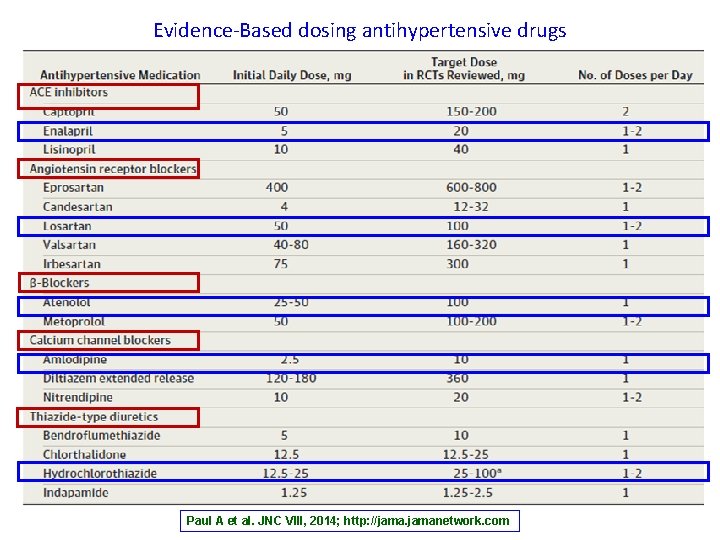
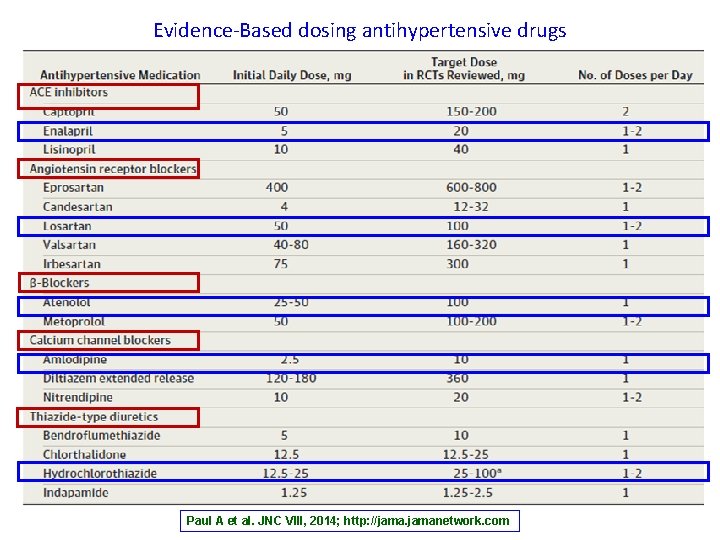
Evidence-Based dosing antihypertensive drugs Paul A et al. JNC VIII, 2014; http: //jamanetwork. com
Take Home Messages Ø Cardiovascular diseases is the leading cause of mortality worldwide Ø Cardiovascular diseases: Prevention is better than care Ø Hypertension is the most common cardiovascular disease that you have to learn how to manage it appropriately
Any Questions ?
More Information available in: 1. United Nations General Assembly resolution 66/2 (http: //www. who. int/nmh/events/un_ncd_summit 2011/political_declaratio n. pdf) 2. Global Action Plan for the Prevention and Control of Noncommunicable Diseases (2013 -2020) Appendix 3/Corr. 1 3. 2013 ESH/ESC Guidelines for the management of arterial hypertension. European Heart Journal 2013; 10: 1093 -1151. 4. Paul A et al. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report From the Panel Members Appointed to the Eighth Joint National Committee (JNC 8) (http: //jamanetwork. com) 5. ONTARGET Investigators. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med 2008; 358: 1547– 1559.