Update on eczema and food allergy Associate Professor





















- Slides: 70
Update on eczema and food allergy Associate Professor Rohan Ameratunga
Update on food allergy • Food allergen update incl cross-reactivity • Epidemiology • Case history: diagnosis including testing • Type 1 reactions incl anaphylaxis • Prevention of food allergy • FA studies in NZ

Adverse Reactions to Food Toxic (eg. Ciguatera) Immune (Food Allergy) Ig. E Non Toxic Non Immune (Food Intolerance) Non-Ig. E Enzymatic Chemical Pharmacologic (eg eczema) (eg celiac) Unknown (lactase) (eg. salicylate) (histamine) Food Aversion

Pathogenesis Ig. E Non-Ig. E Anaphylaxis/angioedema Gastrointestinal anaphylaxis Oral Allergy Syndrome Eczema Allergic Eosinophilic Esophagitis, Gastritis & Gastroenteritis Dietary protein colitis, proctitis and enteropathy [Celiac Disease]
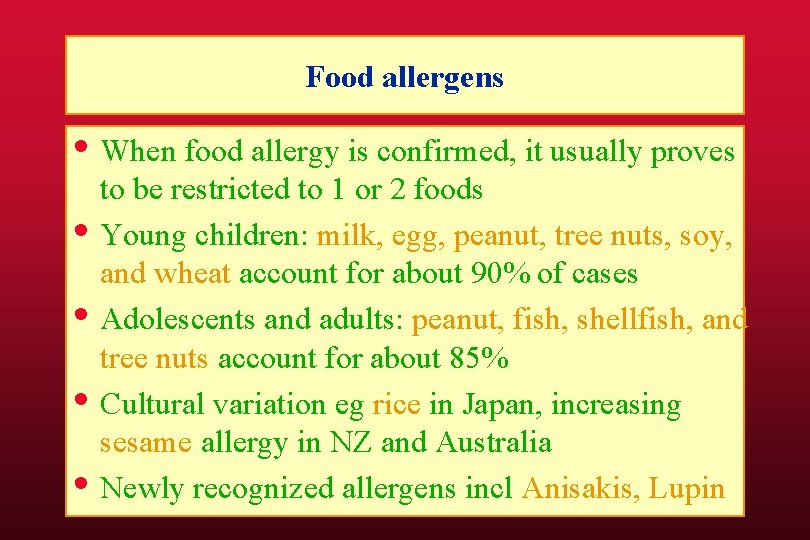
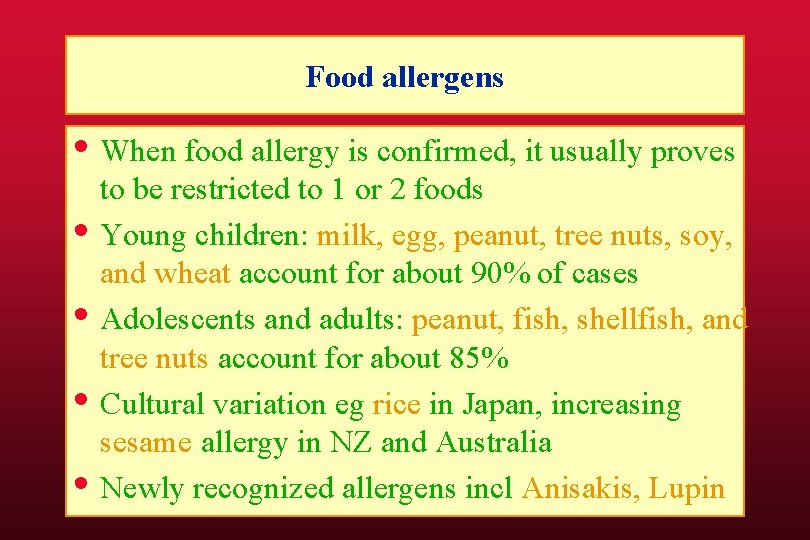
Food allergens • When food allergy is confirmed, it usually proves • • to be restricted to 1 or 2 foods Young children: milk, egg, peanut, tree nuts, soy, and wheat account for about 90% of cases Adolescents and adults: peanut, fish, shellfish, and tree nuts account for about 85% Cultural variation eg rice in Japan, increasing sesame allergy in NZ and Australia Newly recognized allergens incl Anisakis, Lupin

Multiple food allergy • Food contamination • Cross reactivity • Food chemical sensitivity • True multiple food allergy
Food cross-reactivity
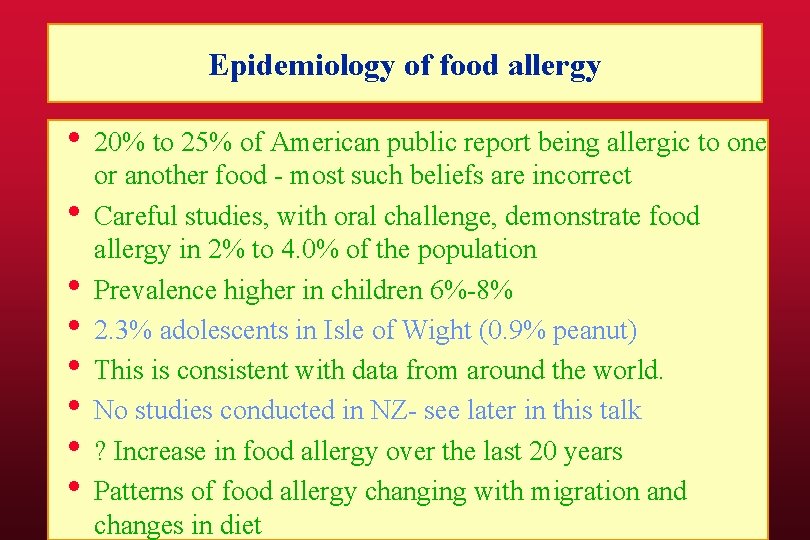
Epidemiology of food allergy • 20% to 25% of American public report being allergic to one • • or another food - most such beliefs are incorrect Careful studies, with oral challenge, demonstrate food allergy in 2% to 4. 0% of the population Prevalence higher in children 6%-8% 2. 3% adolescents in Isle of Wight (0. 9% peanut) This is consistent with data from around the world. No studies conducted in NZ- see later in this talk ? Increase in food allergy over the last 20 years Patterns of food allergy changing with migration and changes in diet

The prevalence of food allergy: A meta-analysis Rona et al JACI Sep 2007 • Papers selected from the literature • Categorised according to methodology • Cochrane methodology • Stringent criteria for inclusion • Divided according to age group • Unselected population papers, not enriched populations such as clinic patients

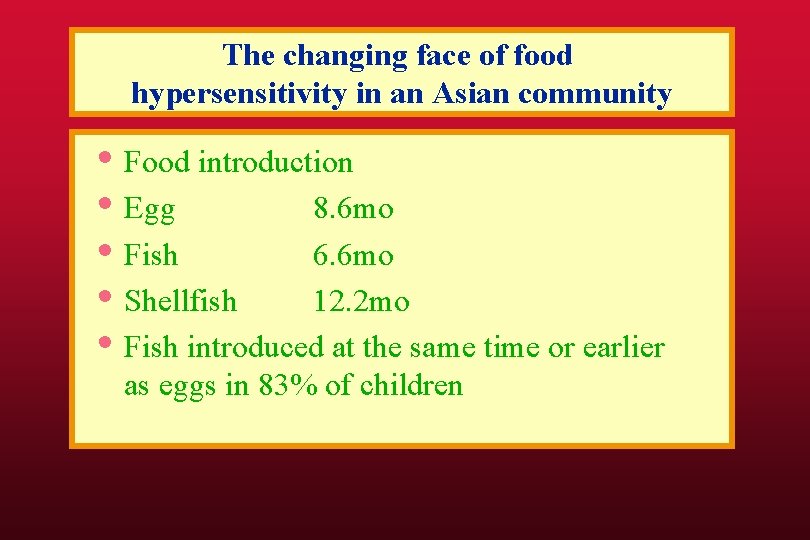
The changing face of food hypersensitivity in an Asian community Chiang et al Clin Exp Allergy 2007 • Very little data on food allergy in Asia • Different diets • Ethnic makeup Chinese, Indian, Malays, • • • Eurasian Melting pot: Rapidly changing lifestyle Increasing westernisation of diet Previous data indicates Chinese have major issues with fish and shellfish
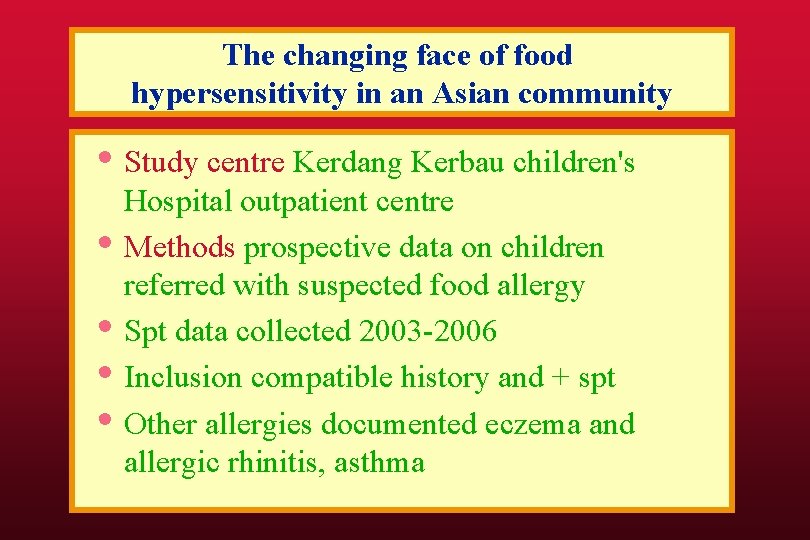
The changing face of food hypersensitivity in an Asian community • Study centre Kerdang Kerbau children's • • Hospital outpatient centre Methods prospective data on children referred with suspected food allergy Spt data collected 2003 -2006 Inclusion compatible history and + spt Other allergies documented eczema and allergic rhinitis, asthma
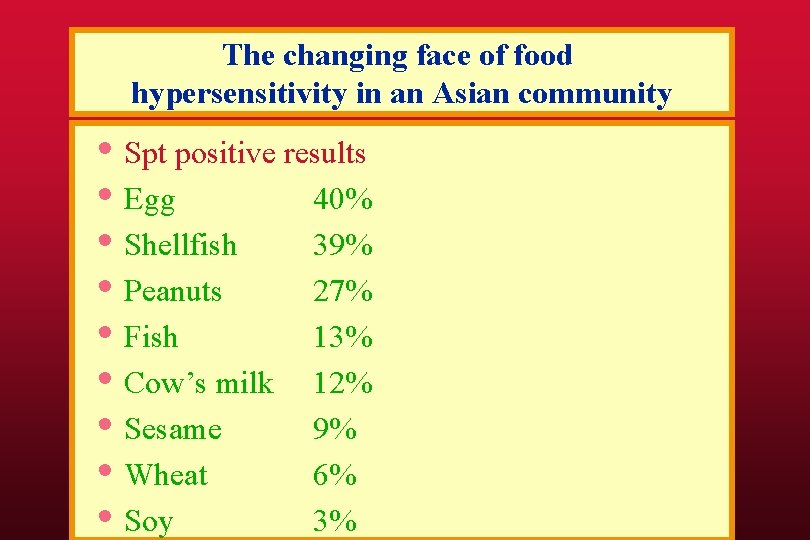
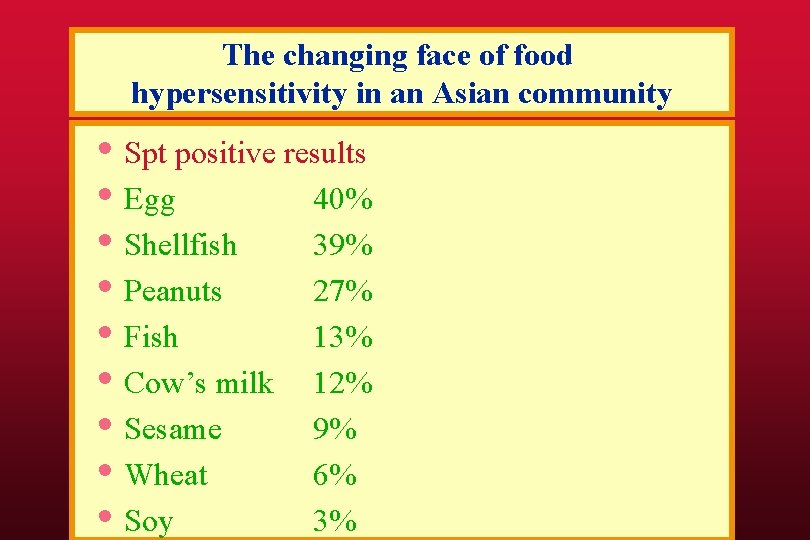
The changing face of food hypersensitivity in an Asian community • Spt positive results • Egg 40% • Shellfish 39% • Peanuts 27% • Fish 13% • Cow’s milk 12% • Sesame 9% • Wheat 6% • Soy 3%
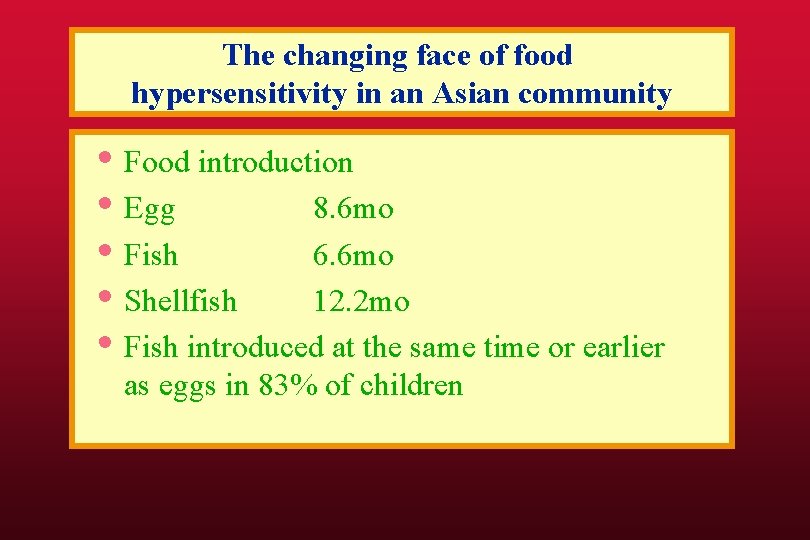
The changing face of food hypersensitivity in an Asian community • Food introduction • Egg 8. 6 mo • Fish 6. 6 mo • Shellfish 12. 2 mo • Fish introduced at the same time or earlier as eggs in 83% of children
Update on food allergy • Epidemiology • Food allergen update incl cross-reactivity • Case history: diagnosis including testing • Type 1 reactions incl anaphylaxis • Prevention of food allergy • FA studies in NZ
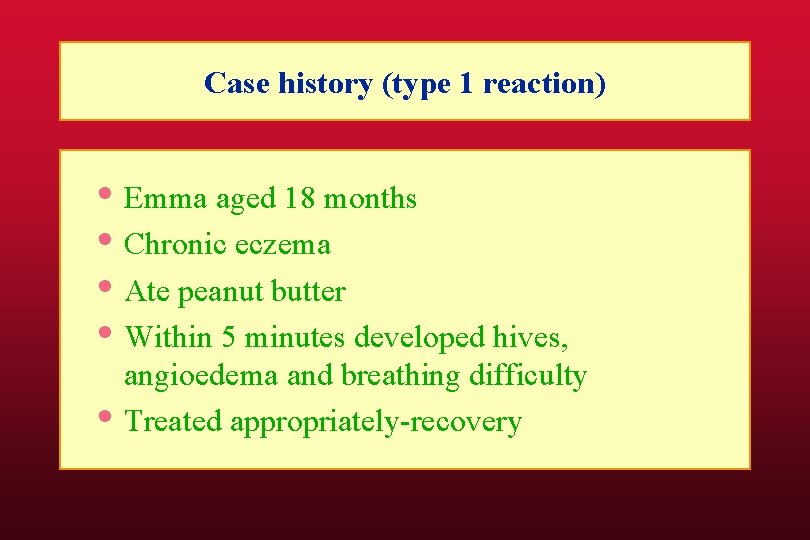
Case history (type 1 reaction) • Emma aged 18 months • Chronic eczema • Ate peanut butter • Within 5 minutes developed hives, • angioedema and breathing difficulty Treated appropriately-recovery
Case history (type 1 reaction) • Managing anaphylaxis • Useful diagnostic procedures • Long term management plan • What is her long-term prognosis? • How common is this problem? • Is there any specific treatment? • What is known about FA in NZ? • Can this problem be prevented?
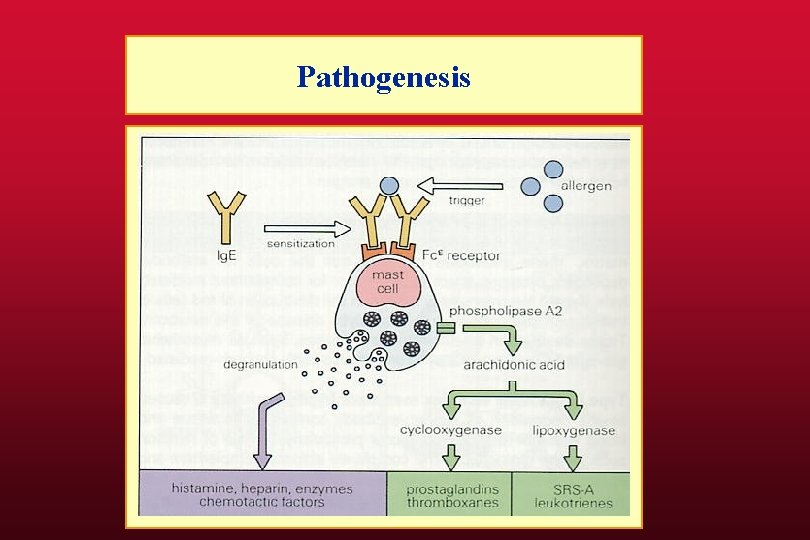
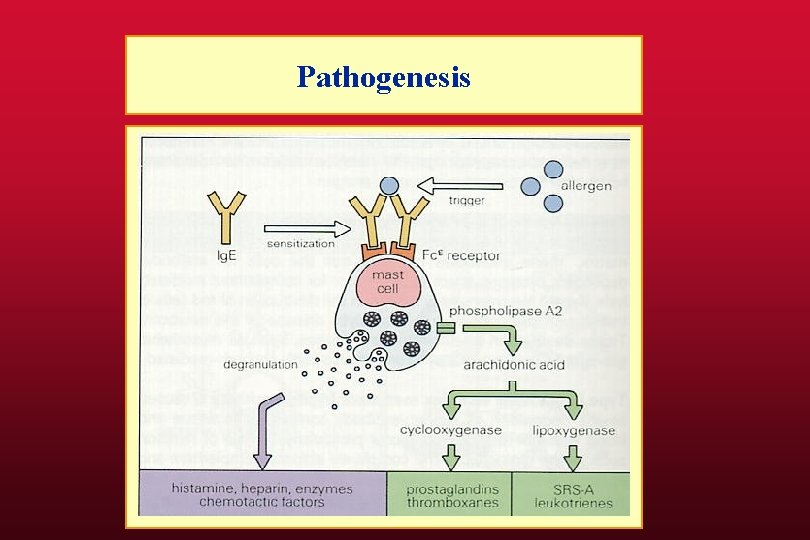
Pathogenesis

Spectrum of Ig. E mediated food allergy • • • Anaphylaxis, urticaria, angioedema: classical anaphylactic reaction Gastrointestinal anaphylaxis: no cutaneous symptoms Food-dependent exercise induced anaphylaxis Oral allergy syndrome: include itching of the mouth, and swelling of the tongues and lips - associated with eating FRESH apple, carrots, hazelnut, bananas, melons Eczema: Up to 50% of young children with eczema may have a food allergy trigger Milk-allergy has been associated with nausea, vomiting, diarrhea, bloating, early satiety, reflux, esophagitis, gastritis, malabsoption, abdominal pain, and bloody stool

Treatment of anaphylaxis • Keep patient lying flat- risk of sudden death • Elevate legs to assist venous return • Risk of late reactions • Patients should be admitted/observed for at • • least 6 hours Serum tryptase 1 -2 h after reaction Fill out ACC form
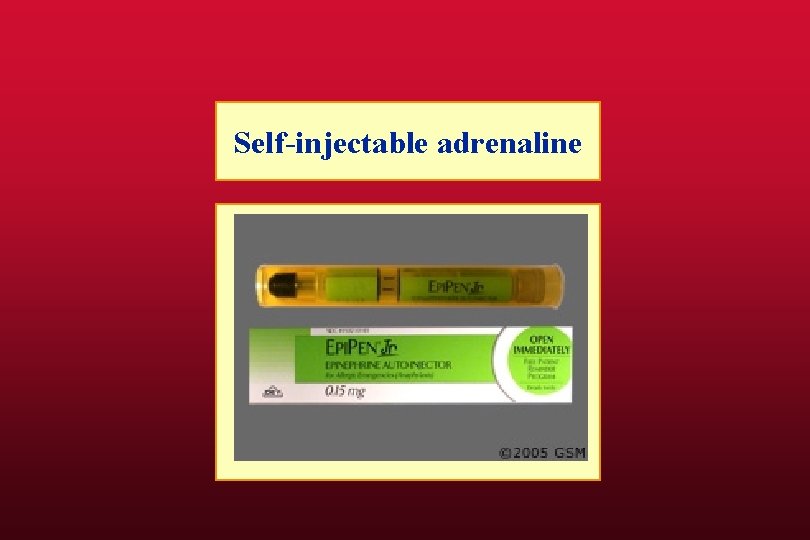
Adrenaline • Dose • • • Adults 0. 3 -0. 5 mg Children 0. 01 ml/kg 1: 1000 ie 10 µg/Kg EPI-PEN 0. 3 mg EPI-PEN Jr 0. 15 mg (8 -20 Kg) Syringe, needle and vial of adrenaline Adrenaline Inhaler- potential problems IV adrenaline only for cardiac arrest Twinject- new device
Individuals at increased risk • Patients with asthma • Antihypertensives esp blockers • MAO inhibitors • Cardiovascular disease • Pregnancy
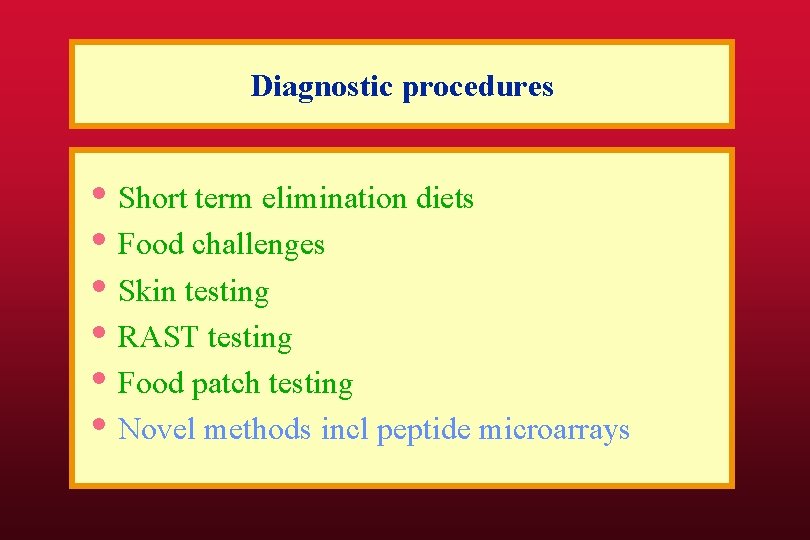
Diagnostic procedures • Short term elimination diets • Food challenges • Skin testing • RAST testing • Food patch testing • Novel methods incl peptide microarrays
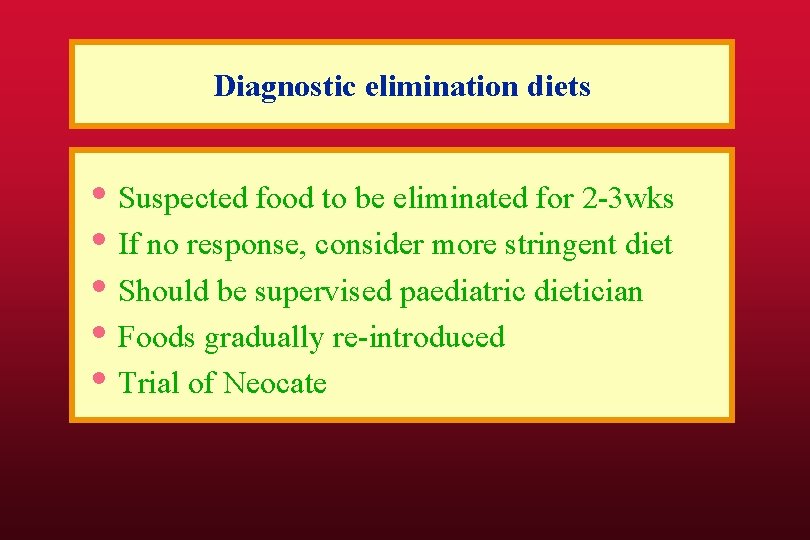
Diagnostic elimination diets • Suspected food to be eliminated for 2 -3 wks • If no response, consider more stringent diet • Should be supervised paediatric dietician • Foods gradually re-introduced • Trial of Neocate
Skin testing

Skin testing
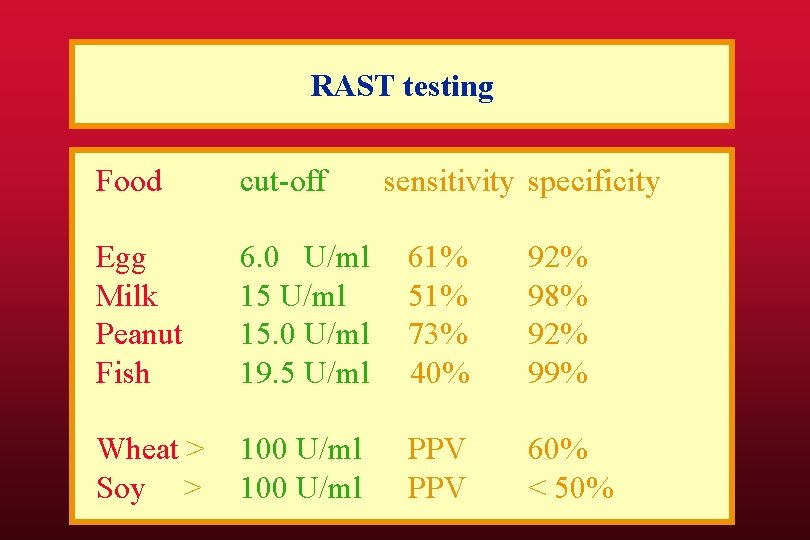
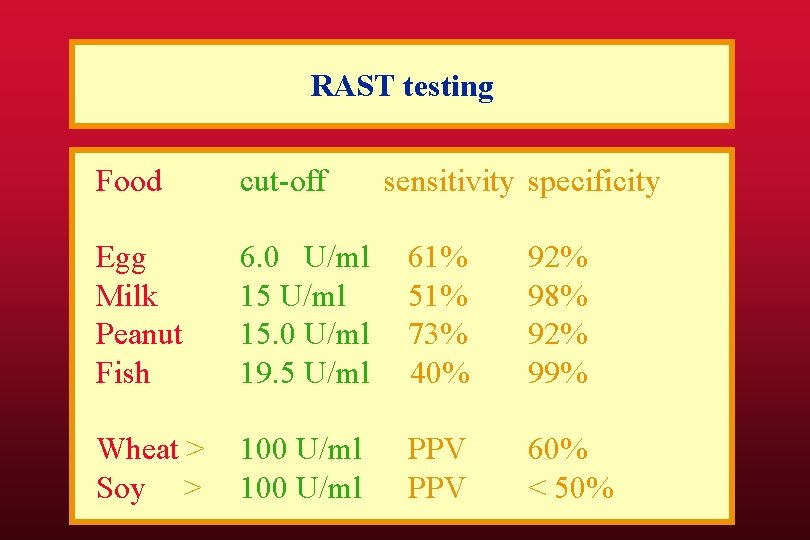
RAST testing Food cut-off sensitivity specificity Egg Milk Peanut Fish 6. 0 U/ml 15. 0 U/ml 19. 5 U/ml 61% 51% 73% 40% 92% 98% 92% 99% Wheat > Soy > 100 U/ml PPV 60% < 50%

Determinants of the severity of a reaction • Sensitivity (food specific Ig. E) • Amount of food consumed • Digestion: use of antacids • Absorption rate (slowed by charcoal) • Co-factors (aspirin, exercise, alcohol) • Sensitivity can increase with subsequent exposures (memory)
Update on food allergy • Epidemiology • Food allergen update incl cross-reactivity • Diagnosis including testing • Type 1 reactions incl anaphylaxis • Prevention of food allergy • FA studies in NZ

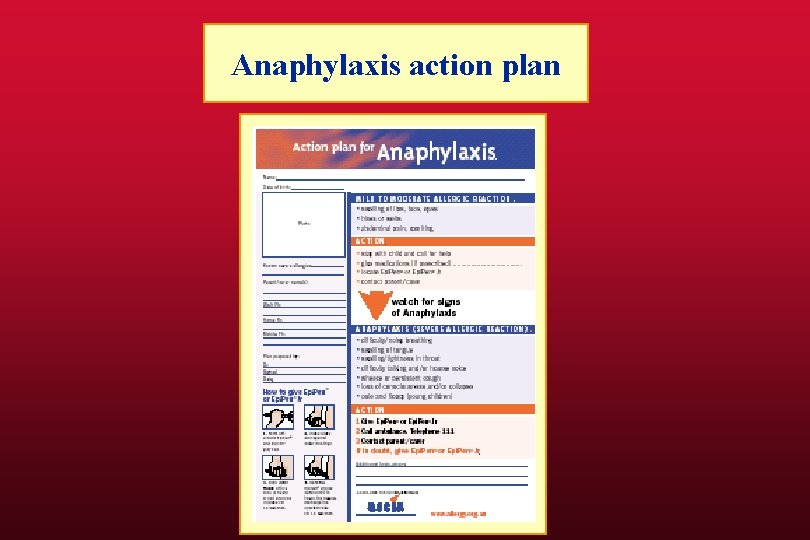
Food allergy management plan • Education re foods and avoidance-dietician • Written action plan • MEDIC-ALERT emblem-velcro • Public Health nurses to visit school/daycare • Anaphylaxis video (Allergy NZ) • Follow up RAST testing 6 -12 monthly • Food challenge if RAST becomes negative
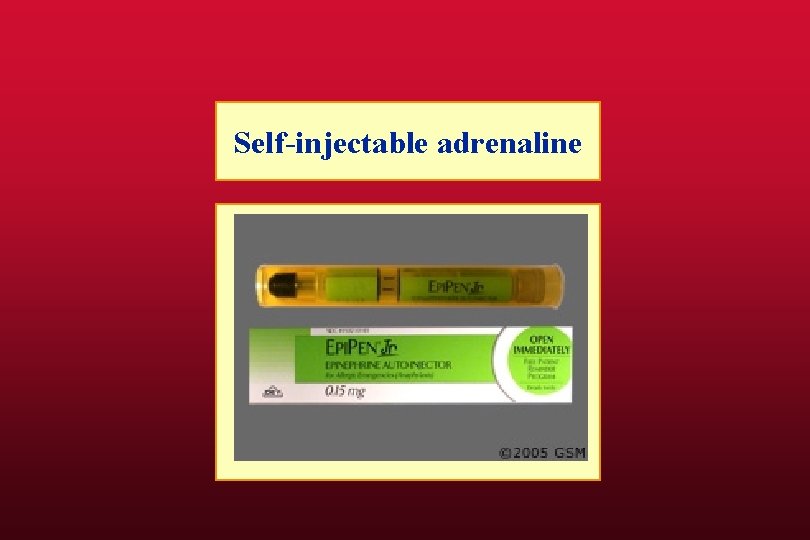
Self-injectable adrenaline

Self-injectable adrenaline
Self-injectable adrenaline
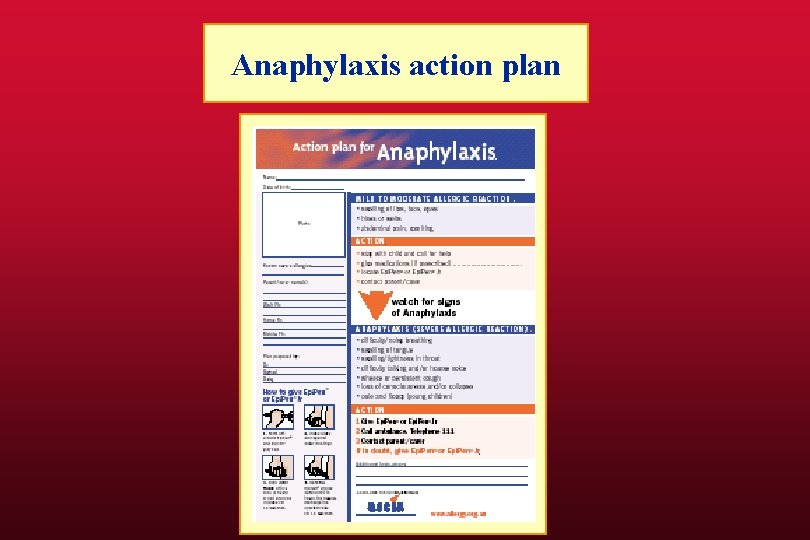
Anaphylaxis action plan

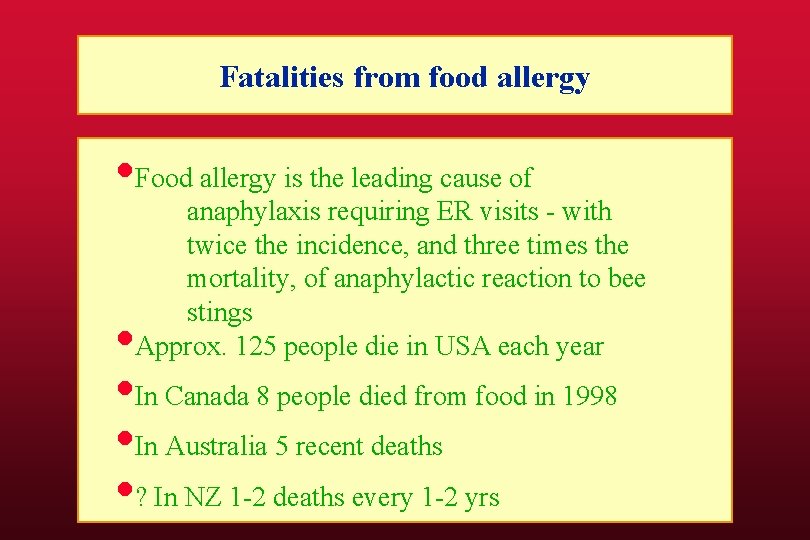
Fatalities from food allergy • Food allergy is the leading cause of anaphylaxis requiring ER visits - with twice the incidence, and three times the mortality, of anaphylactic reaction to bee stings Approx. 125 people die in USA each year • • In Canada 8 people died from food in 1998 • In Australia 5 recent deaths • ? In NZ 1 -2 deaths every 1 -2 yrs
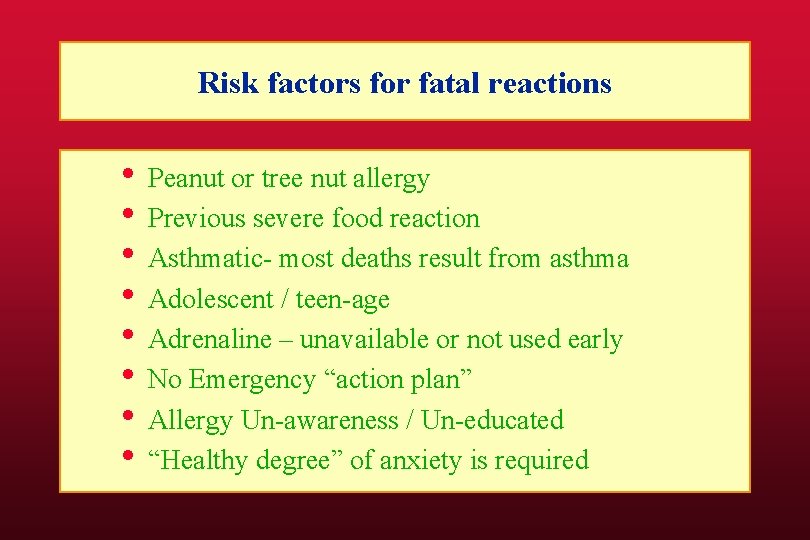
Risk factors for fatal reactions • Peanut or tree nut allergy • Previous severe food reaction • Asthmatic- most deaths result from asthma • Adolescent / teen-age • Adrenaline – unavailable or not used early • No Emergency “action plan” • Allergy Un-awareness / Un-educated • “Healthy degree” of anxiety is required
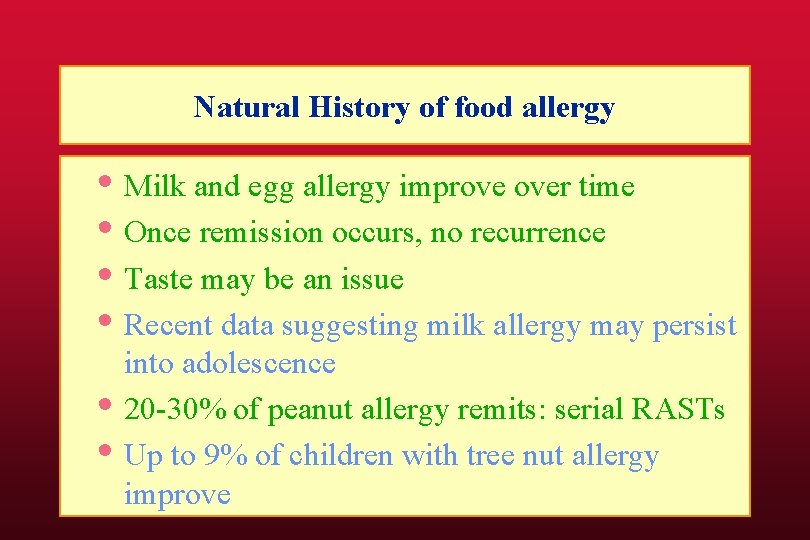
Natural History of food allergy • Milk and egg allergy improve over time • Once remission occurs, no recurrence • Taste may be an issue • Recent data suggesting milk allergy may persist • • into adolescence 20 -30% of peanut allergy remits: serial RASTs Up to 9% of children with tree nut allergy improve
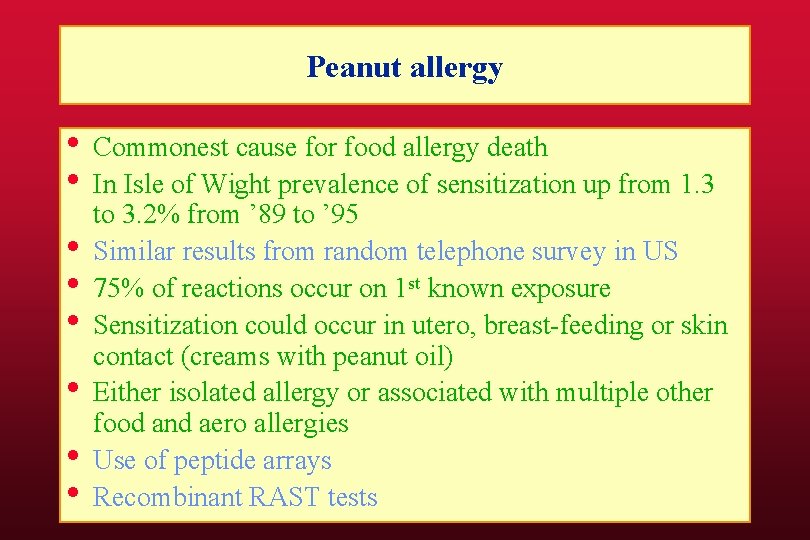
Peanut allergy • Commonest cause for food allergy death • In Isle of Wight prevalence of sensitization up from 1. 3 • • • to 3. 2% from ’ 89 to ’ 95 Similar results from random telephone survey in US 75% of reactions occur on 1 st known exposure Sensitization could occur in utero, breast-feeding or skin contact (creams with peanut oil) Either isolated allergy or associated with multiple other food and aero allergies Use of peptide arrays Recombinant RAST tests
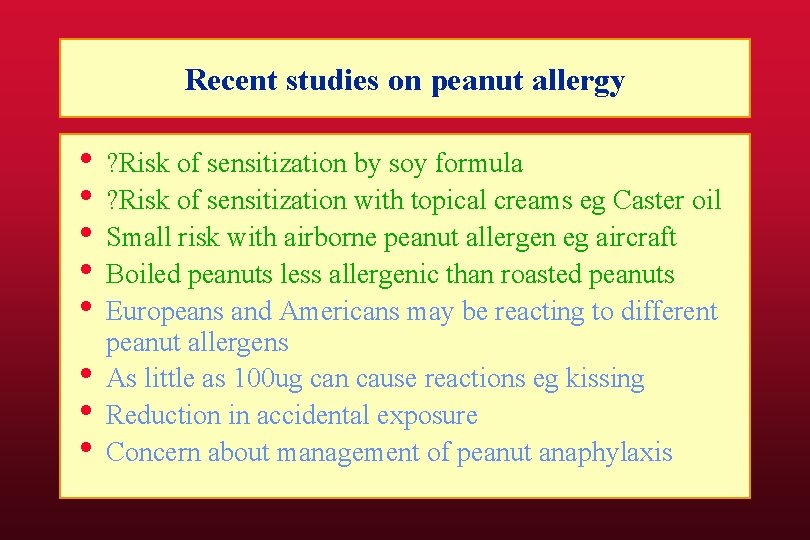
Recent studies on peanut allergy • ? Risk of sensitization by soy formula • ? Risk of sensitization with topical creams eg Caster oil • Small risk with airborne peanut allergen eg aircraft • Boiled peanuts less allergenic than roasted peanuts • Europeans and Americans may be reacting to different • • • peanut allergens As little as 100 ug can cause reactions eg kissing Reduction in accidental exposure Concern about management of peanut anaphylaxis
Recent studies on peanut allergy • Up to 20 -30% of peanut allergic children remit • Remission more likely with lower peanut Ig. E levels • Higher risk of recurrence with infrequent peanut • • ingestion Cross-reactivity with other nuts (or co-sensitization) Chinese herbal preparation: protection against murine peanut anaphylaxis

Anti-Ig. E therapy • Recent study with TNX 901 showed anti-Ig. E therapy • • • can markedly improve peanut allergy Threshold doses increased from 1/2 peanut to 8 peanuts Lawsuit- project discontinued Currently phase 2 study of Omalizumab (Xolair) Leung et al NEJM 2004
Recent studies on peanut allergy • Peanut desensitisation • Two studies Cambridge and Durham NC • ?
Update on food allergy • Epidemiology • Food allergen update incl cross-reactivity • Case history: diagnosis including testing • Type 1 reactions incl anaphylaxis • Prevention of food allergy • FA studies in NZ
The changing epidemiology of food allergy Proposed food allergy studies in NZ
Questions • • What is the burden of food allergy? Can food allergy be prevented? What services are utilised by patients What are the gaps in services What is the response of Gov’t agencies? Are there any unusual food allergies in NZ? What is the natural history of food allergy?

Agencies involved in food allergy • • • Ministry of health ARPHS DHBNZ Ministry of Education PHARMAC MEDSAFE ACC Ministry of Trade and Industry FSANZ NZFSA IGA

Lack of food allergy data in New Zealand • Currently little data specific to food allergy • May be similar to overseas? ? • However ethnic makeup different • Ethnic makeup rapidly changing • Role of genetics • Feeding practices may be different • Available foods are different eg shellfish
Lack of food allergy Research in New Zealand • Lack of data is hindering medical services • No public food allergy service in south • Island for children Epipens unfunded
Lack of food allergy Research in New Zealand • Ad hoc approach in schools • Issues with preschools

Lack of food allergy Research in New Zealand • Risk management issues for food industry • • • and hospitality industry Important for food export industry Public not aware of the problem Impact on quality of life not appreciated
Is there an ideal method to determine food allergy prevalence? • Large scale unselected cohort • Regular clinical review and testing • DBPCFC for patients with Sx or +ve tests • But. . .
Is there an ideal method? • Time dependent data • Risk of food challenges • Expense of studies • No data on adults • Change in demographics • Change in feeding practices • Changes in available foods • Likely to be different to others parts of NZ
Difficulties with food allergy Epidemiology • Symptoms vary according to age • Symptoms not confined to one organ system • Delayed reactions • Patients may not be aware a food is • • • triggering symptoms The need for lab tests Survey instruments are not well established Therefore FA studies are expensive
Difficulties with FA studies in NZ • Funding agencies • Food industry unaware/ denial of risk
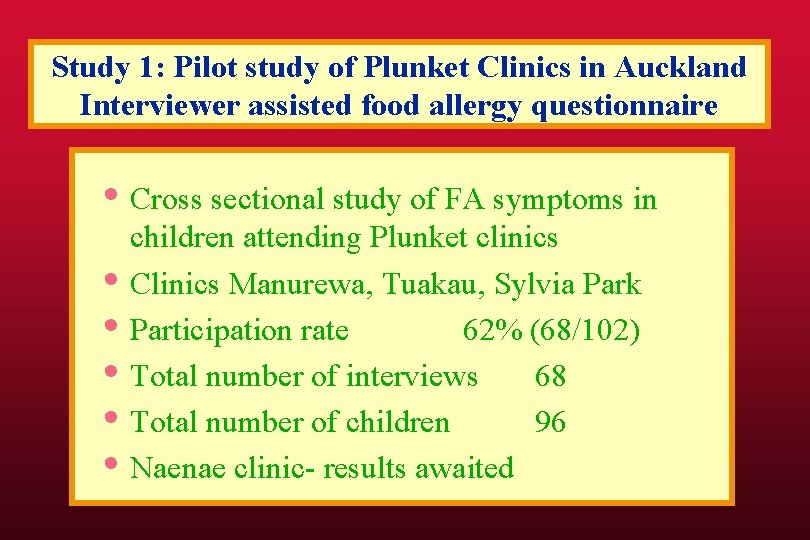
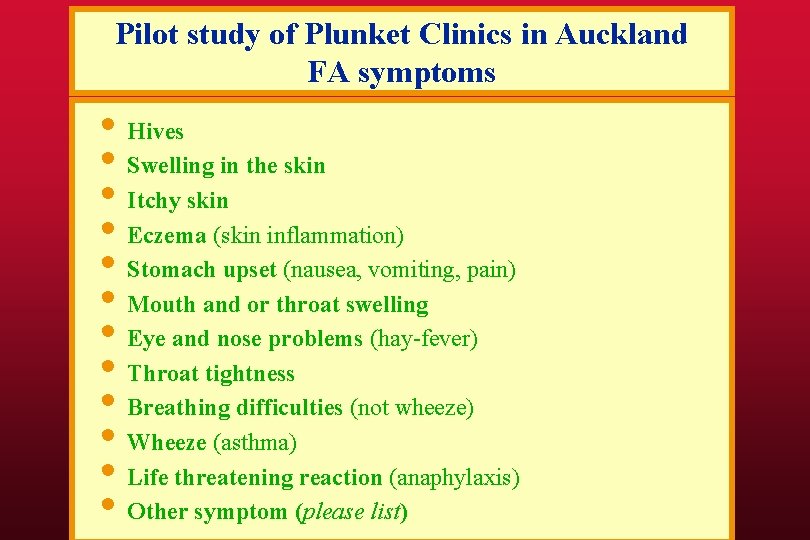
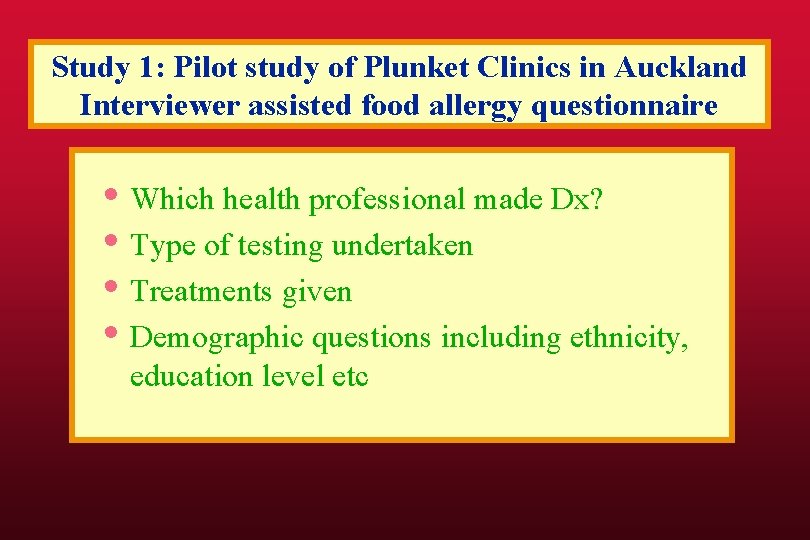
Study 1: Pilot study of Plunket Clinics in Auckland Interviewer assisted food allergy questionnaire • Cross sectional study of FA symptoms in • • • children attending Plunket clinics Clinics Manurewa, Tuakau, Sylvia Park Participation rate 62% (68/102) Total number of interviews 68 Total number of children 96 Naenae clinic- results awaited
Pilot study of Plunket Clinics in Auckland FA symptoms • Hives • Swelling in the skin • Itchy skin • Eczema (skin inflammation) • Stomach upset (nausea, vomiting, pain) • Mouth and or throat swelling • Eye and nose problems (hay-fever) • Throat tightness • Breathing difficulties (not wheeze) • Wheeze (asthma) • Life threatening reaction (anaphylaxis) • Other symptom (please list)
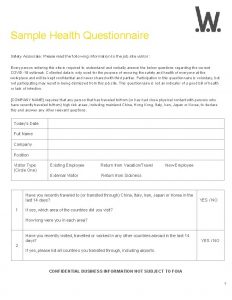
Study 1: Pilot study of Plunket Clinics in Auckland Interviewer assisted food allergy questionnaire • Which health professional made Dx? • Type of testing undertaken • Treatments given • Demographic questions including ethnicity, education level etc

Pilot study of Plunket Clinics in Auckland FA symptoms: hives
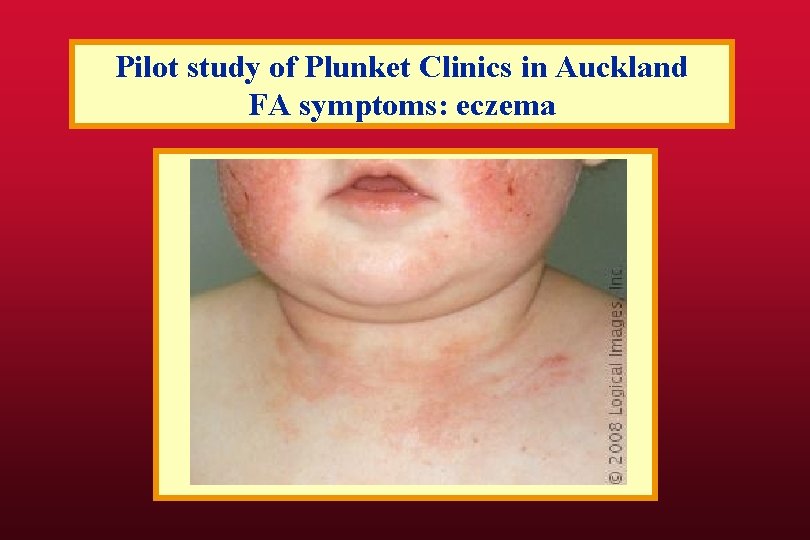
Pilot study of Plunket Clinics in Auckland FA symptoms: eczema
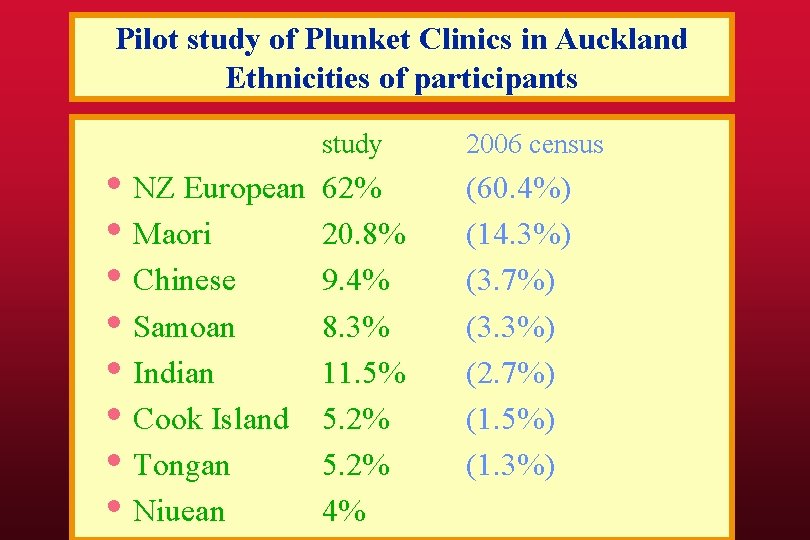
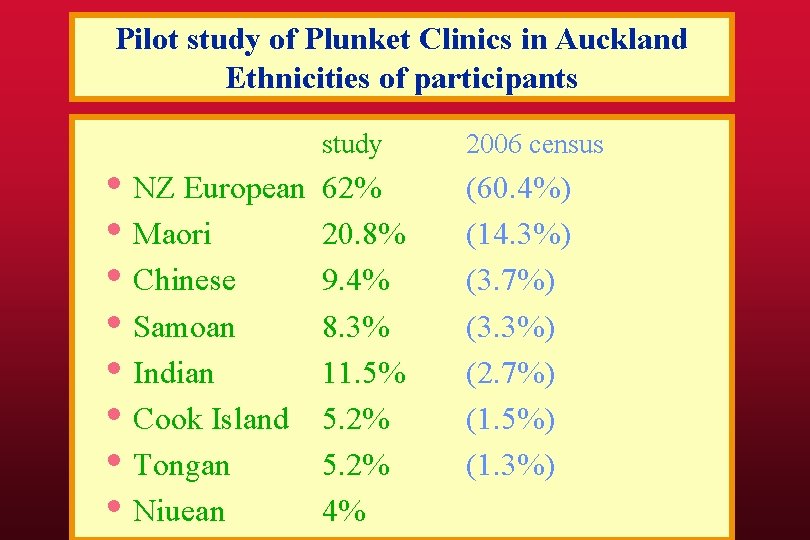
Pilot study of Plunket Clinics in Auckland Ethnicities of participants • NZ European • Maori • Chinese • Samoan • Indian • Cook Island • Tongan • Niuean study 2006 census 62% 20. 8% 9. 4% 8. 3% 11. 5% 5. 2% 4% (60. 4%) (14. 3%) (3. 7%) (3. 3%) (2. 7%) (1. 5%) (1. 3%)
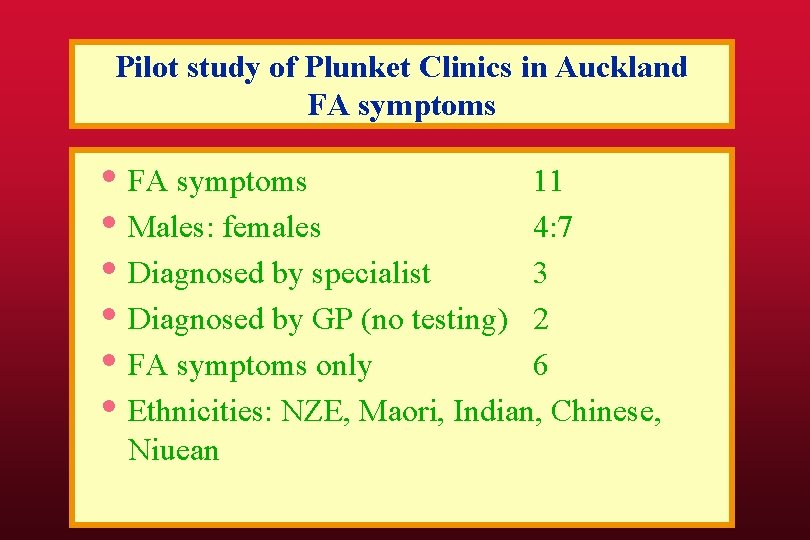
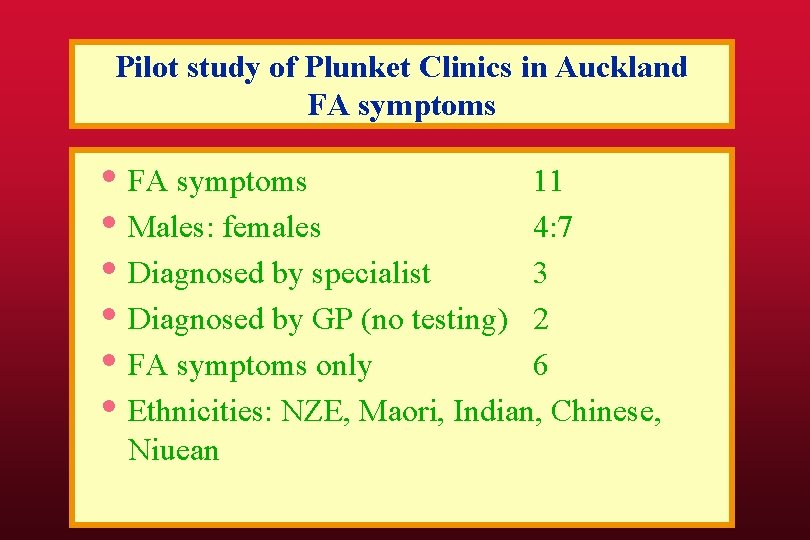
Pilot study of Plunket Clinics in Auckland FA symptoms • FA symptoms 11 • Males: females 4: 7 • Diagnosed by specialist 3 • Diagnosed by GP (no testing) 2 • FA symptoms only 6 • Ethnicities: NZE, Maori, Indian, Chinese, Niuean
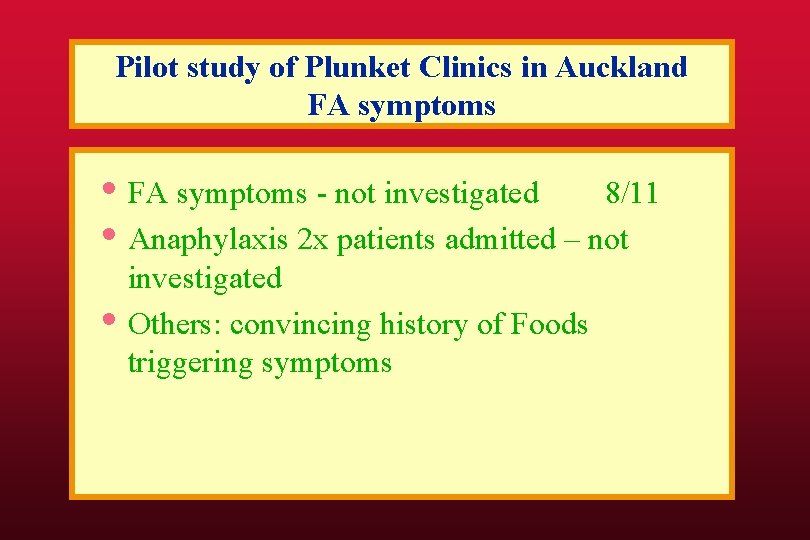
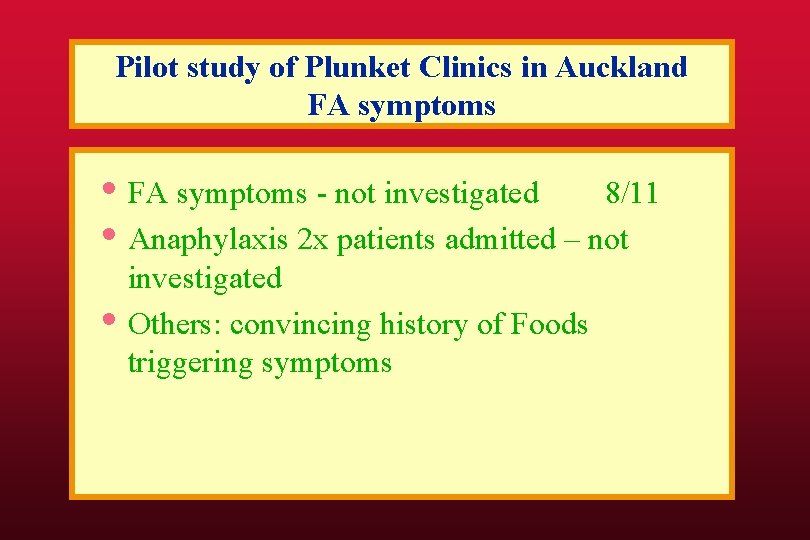
Pilot study of Plunket Clinics in Auckland FA symptoms • FA symptoms - not investigated 8/11 • Anaphylaxis 2 x patients admitted – not • investigated Others: convincing history of Foods triggering symptoms

Pilot study of Plunket Clinics in Auckland Eczema • Eczema 30% • Treated by GP 17% • NZ Health survey 14% with eczema • Some mothers changed own diet while breast feeding and found eczema improved.
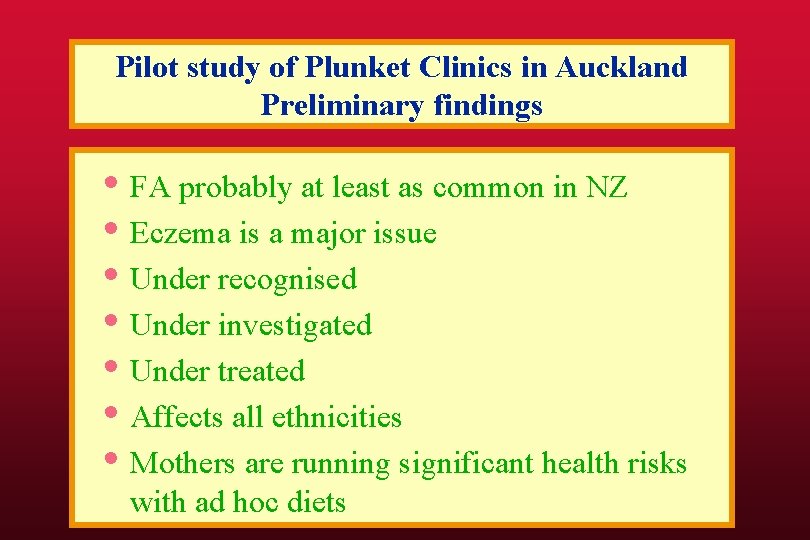
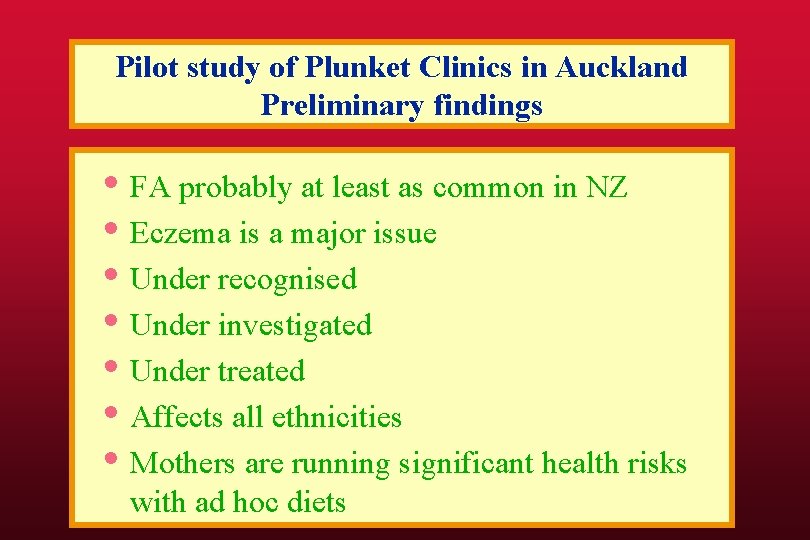
Pilot study of Plunket Clinics in Auckland Preliminary findings • FA probably at least as common in NZ • Eczema is a major issue • Under recognised • Under investigated • Under treated • Affects all ethnicities • Mothers are running significant health risks with ad hoc diets

Study 2 Larger cross-sectional study of FA • Larger study of FA symptoms in Auckland • Practical issues • Interview room ? Mobile office • Languages • Working with Plunket • Funding
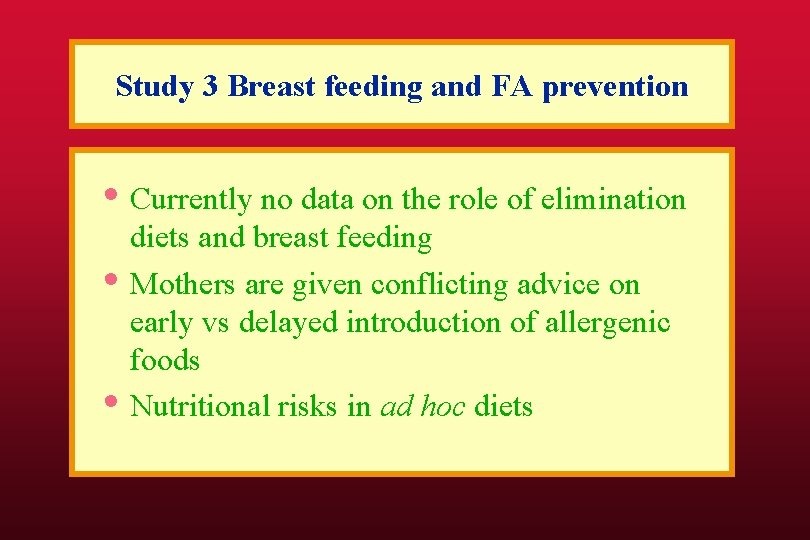
Study 3 Breast feeding and FA prevention • Currently no data on the role of elimination • • diets and breast feeding Mothers are given conflicting advice on early vs delayed introduction of allergenic foods Nutritional risks in ad hoc diets
Study 3 Breast feeding and FA prevention Eligibility • Have an older child with proven FA • Pregnant- 34/40+ • Regular FA questionnaire • Regular dietary assessment • RAST testing cord blood and 5 months • Prelude to a longer cohort study

Funding: unrestricted grants • ADHB Charitable trust • Allergy New Zealand • ASCIA • Australian Laboratory Sciences • Nutricia • William and Lois Manchester trust

Food Allergy Research Group • Christine Crooks (Lab. Plus) • Maia Brewerton (Wellington Hospital) • • • Penny Jorgensen (Allergy New Zealand) Steve Buetow (University of Auckland) Claire Wall (University of Auckland) Shannon Brothers (Starship) Allen Liang Allergy Specialist Rohan Ameratunga (Lab. Plus, Chair)
Paediatric food allergy/ eczema clinic JHU Prof Robert Wood Prof Hugh Sampson Prof Ken Schurberth
 Promotion from associate professor to professor
Promotion from associate professor to professor Alternative of log based recovery
Alternative of log based recovery Maia brewerton
Maia brewerton Eczema dysidrosique
Eczema dysidrosique Kode icd 10 pityriasis rosea
Kode icd 10 pityriasis rosea Dr bogdan zrnic
Dr bogdan zrnic Freederm hc eczema cream
Freederm hc eczema cream Dr lemer nyc
Dr lemer nyc Closcript topical cream
Closcript topical cream Nummular eczema
Nummular eczema Nummular eczema
Nummular eczema Eczema herpetico tratamiento
Eczema herpetico tratamiento Sharon hulley
Sharon hulley Jennerian vesicle
Jennerian vesicle Eczema impetiginizzato
Eczema impetiginizzato Food and beverage knowledge
Food and beverage knowledge Surgical prep
Surgical prep American academy of allergy asthma and immunology 2018
American academy of allergy asthma and immunology 2018 Unit 2 food food food
Unit 2 food food food Eltonian pyramid
Eltonian pyramid The allergy guy
The allergy guy Latex in outlook
Latex in outlook Latex fruit allergy
Latex fruit allergy Allergy wise
Allergy wise Weights of the backpacks of first graders on a school bus.
Weights of the backpacks of first graders on a school bus. Latex food syndrome
Latex food syndrome Macaulay allergy
Macaulay allergy Allergic rhinitis treatment guidelines
Allergic rhinitis treatment guidelines Allergic crease adalah
Allergic crease adalah Allergic rhinitis treatment guidelines
Allergic rhinitis treatment guidelines Allergy
Allergy Anegdotal
Anegdotal Allergy
Allergy Allergic reaction icd 9 code
Allergic reaction icd 9 code Allergy rates
Allergy rates Rhinitis allergy
Rhinitis allergy Allergy board review course
Allergy board review course Rhinitis allergy
Rhinitis allergy Allergy
Allergy Acr contrast reaction card
Acr contrast reaction card Erythroblastosis
Erythroblastosis Penicillin allergy cme
Penicillin allergy cme World allergy organ j
World allergy organ j Keva immunorich
Keva immunorich Eu food information for consumers regulation
Eu food information for consumers regulation Sensitization hypersensitivity
Sensitization hypersensitivity Allergy asthma immunol res impact factor
Allergy asthma immunol res impact factor Bcs professional membership
Bcs professional membership Tecniche associate al pensiero computazionale:
Tecniche associate al pensiero computazionale: The pyramid at chichen itza is most closely associate with
The pyramid at chichen itza is most closely associate with Lone star college nursing program reviews
Lone star college nursing program reviews Incose asep certification
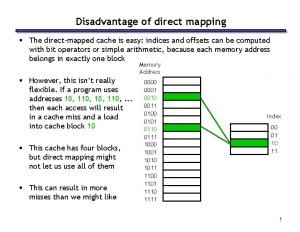
Incose asep certification Direct mapping cache
Direct mapping cache Project associate cern
Project associate cern Associate degree netherlands
Associate degree netherlands Laser alignment
Laser alignment Jeannie watkins
Jeannie watkins Rcog cpd portfolio
Rcog cpd portfolio Kosten tio hbo
Kosten tio hbo Analyst hierarchy
Analyst hierarchy Harper college international students
Harper college international students Iter project associate
Iter project associate Michelin aad program
Michelin aad program Lahc verify my fafsa
Lahc verify my fafsa Why critical reading is an active process of discovery
Why critical reading is an active process of discovery Delta chi flag
Delta chi flag Associate degree rmit
Associate degree rmit Cumsa certificate
Cumsa certificate Cincinnati state associate degrees
Cincinnati state associate degrees Safety associate
Safety associate Associate warden
Associate warden