Update in Rheumatoid Arthritis Gregory Gardner M D




- Slides: 58
Update in Rheumatoid Arthritis Gregory Gardner, M. D. Gilliland-Henderson Professor of Medicine Division of Rheumatology University of Washington
Outline of Discussion n Pathophysiology n Clinical Features n Treatment Update n Perioperative Management
Rheumatoid Arthritis Pathophysiology
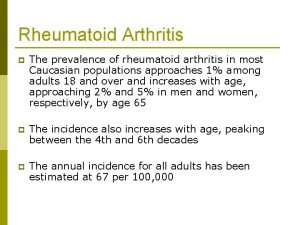
Rheumatoid arthritis demographics n Autoimmune disease n Affects 1 -2% of US population n 1 st degree relative has double the risk n Women: Men 3: 1 n Occurs in two peaks: -Women during child bearing years -Men and women after age 60
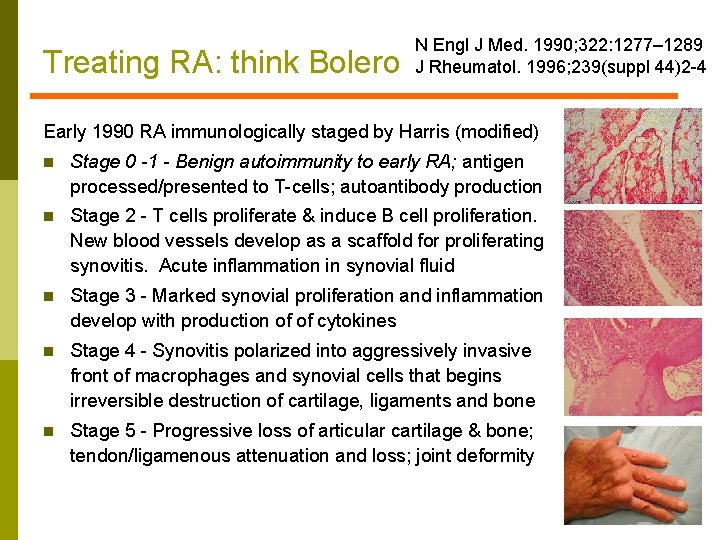
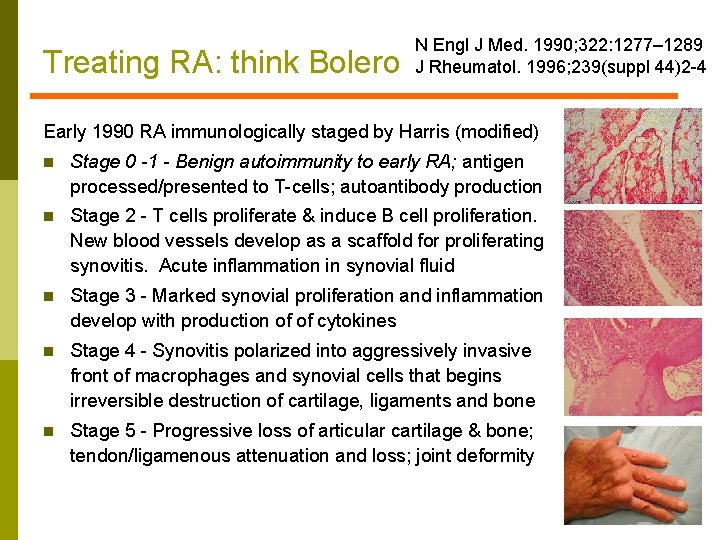
Treating RA: think Bolero N Engl J Med. 1990; 322: 1277– 1289 J Rheumatol. 1996; 239(suppl 44)2 -4 Early 1990 RA immunologically staged by Harris (modified) n Stage 0 -1 - Benign autoimmunity to early RA; antigen processed/presented to T-cells; autoantibody production n Stage 2 - T cells proliferate & induce B cell proliferation. New blood vessels develop as a scaffold for proliferating synovitis. Acute inflammation in synovial fluid n Stage 3 - Marked synovial proliferation and inflammation develop with production of of cytokines n Stage 4 - Synovitis polarized into aggressively invasive front of macrophages and synovial cells that begins irreversible destruction of cartilage, ligaments and bone n Stage 5 - Progressive loss of articular cartilage & bone; tendon/ligamenous attenuation and loss; joint deformity
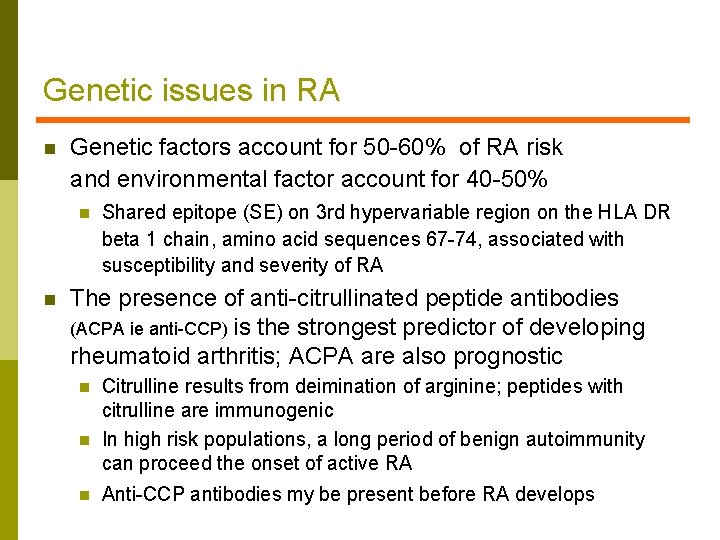
Genetic issues in RA n Genetic factors account for 50 -60% of RA risk and environmental factor account for 40 -50% n n Shared epitope (SE) on 3 rd hypervariable region on the HLA DR beta 1 chain, amino acid sequences 67 -74, associated with susceptibility and severity of RA The presence of anti-citrullinated peptide antibodies (ACPA ie anti-CCP) is the strongest predictor of developing rheumatoid arthritis; ACPA are also prognostic n n n Citrulline results from deimination of arginine; peptides with citrulline are immunogenic In high risk populations, a long period of benign autoimmunity can proceed the onset of active RA Anti-CCP antibodies my be present before RA develops
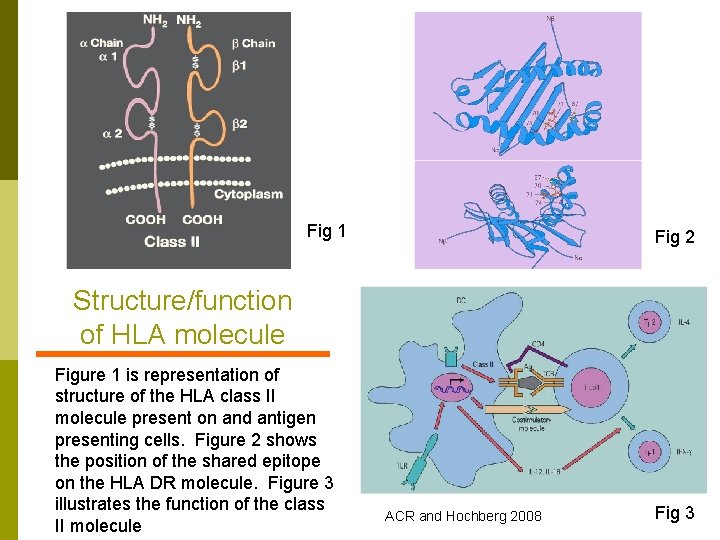
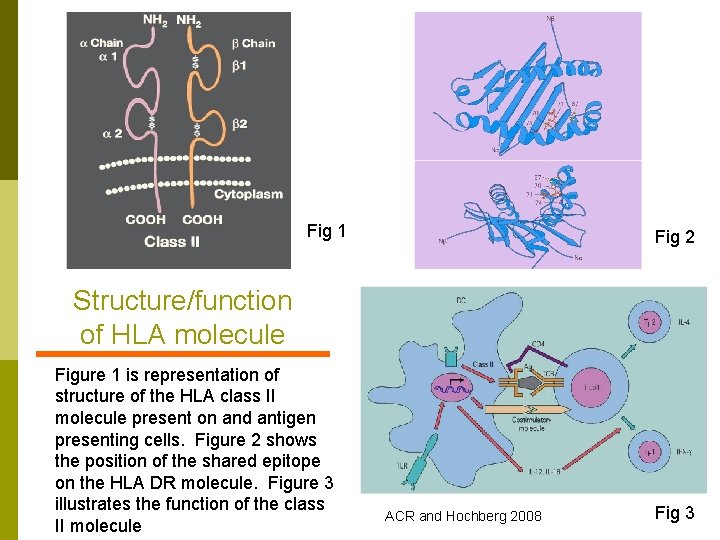
Fig 1 Fig 2 Structure/function of HLA molecule Figure 1 is representation of structure of the HLA class II molecule present on and antigen presenting cells. Figure 2 shows the position of the shared epitope on the HLA DR molecule. Figure 3 illustrates the function of the class II molecule ACR and Hochberg 2008 Fig 3
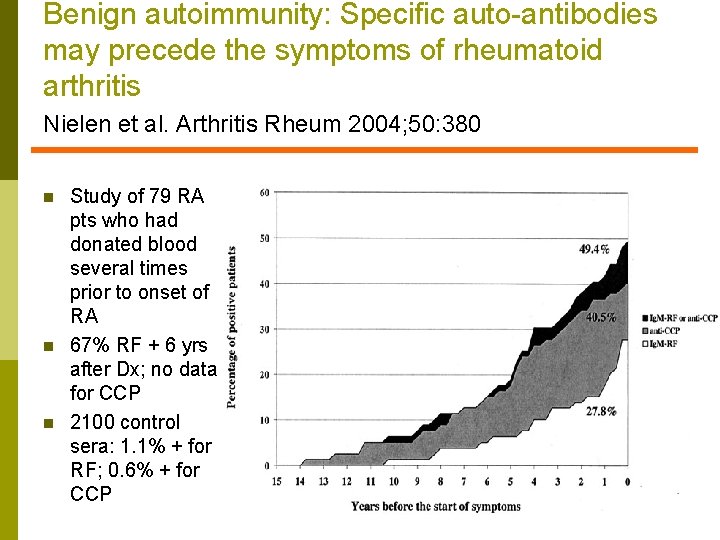
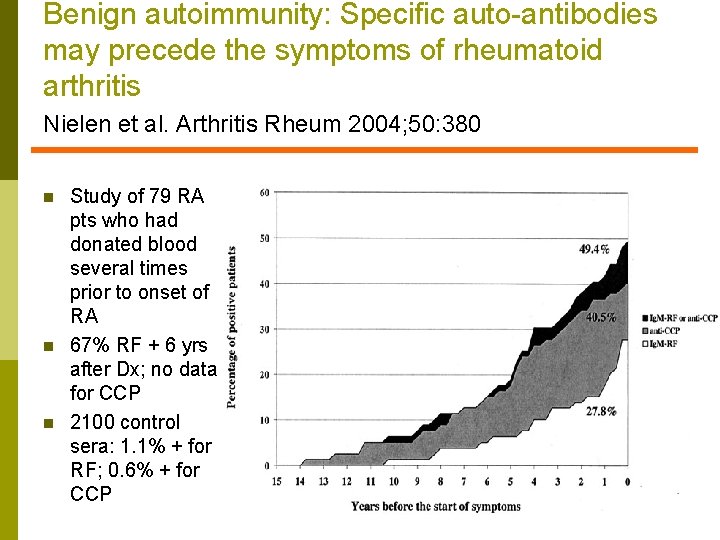
Benign autoimmunity: Specific auto-antibodies may precede the symptoms of rheumatoid arthritis Nielen et al. Arthritis Rheum 2004; 50: 380 n n n Study of 79 RA pts who had donated blood several times prior to onset of RA 67% RF + 6 yrs after Dx; no data for CCP 2100 control sera: 1. 1% + for RF; 0. 6% + for CCP
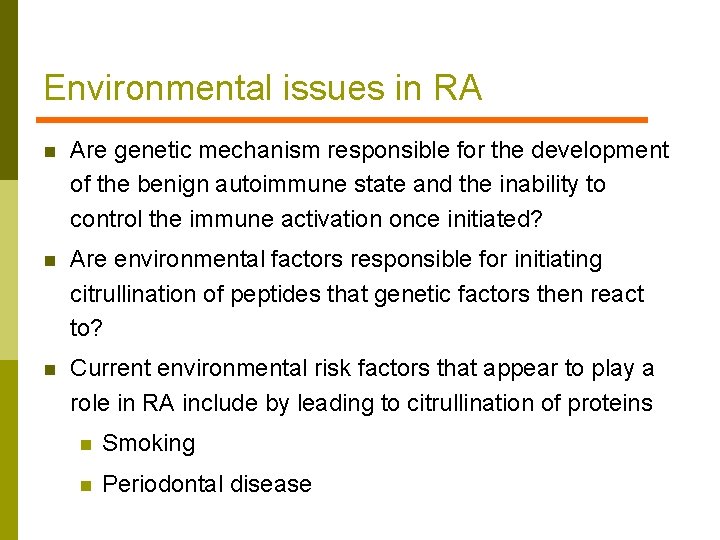
Environmental issues in RA n Are genetic mechanism responsible for the development of the benign autoimmune state and the inability to control the immune activation once initiated? n Are environmental factors responsible for initiating citrullination of peptides that genetic factors then react to? n Current environmental risk factors that appear to play a role in RA include by leading to citrullination of proteins n Smoking n Periodontal disease
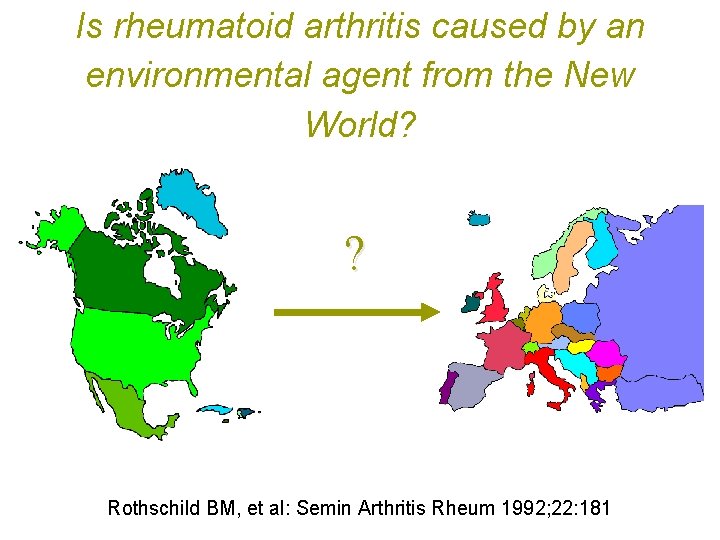
Is rheumatoid arthritis caused by an environmental agent from the New World? ? Rothschild BM, et al: Semin Arthritis Rheum 1992; 22: 181
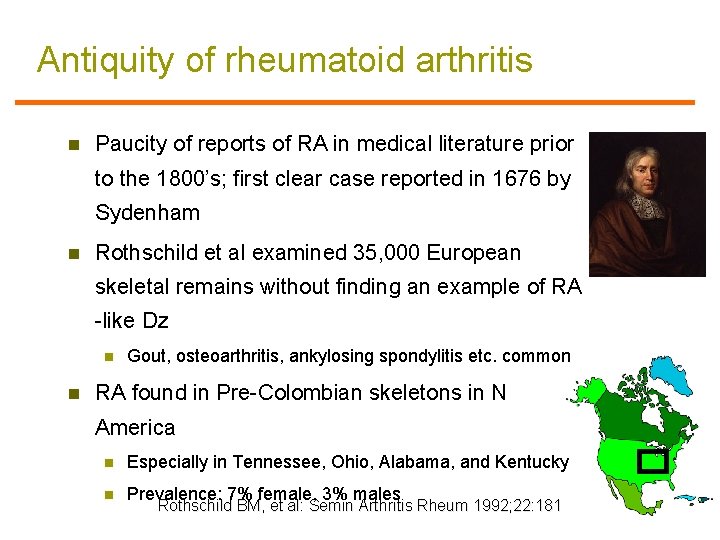
Antiquity of rheumatoid arthritis n Paucity of reports of RA in medical literature prior to the 1800’s; first clear case reported in 1676 by Sydenham n Rothschild et al examined 35, 000 European skeletal remains without finding an example of RA -like Dz n n Gout, osteoarthritis, ankylosing spondylitis etc. common RA found in Pre-Colombian skeletons in N America n Especially in Tennessee, Ohio, Alabama, and Kentucky n Prevalence: 7% female, 3% males Rothschild BM, et al: Semin Arthritis Rheum 1992; 22: 181
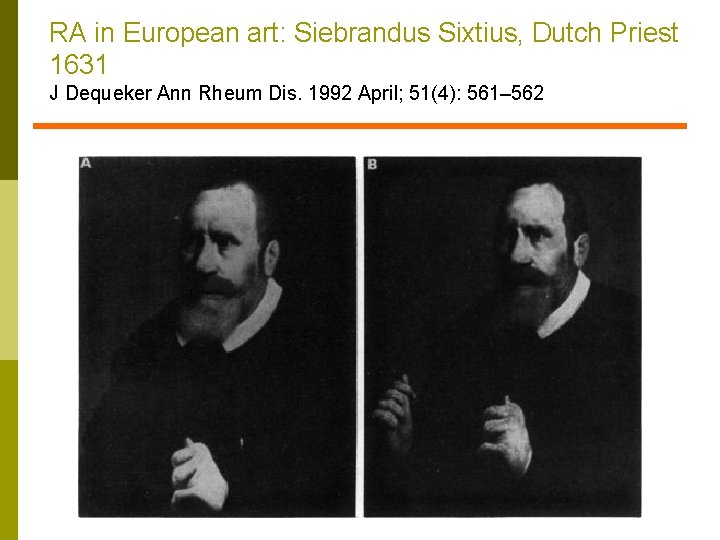
RA in European art: Siebrandus Sixtius, Dutch Priest 1631 J Dequeker Ann Rheum Dis. 1992 April; 51(4): 561– 562
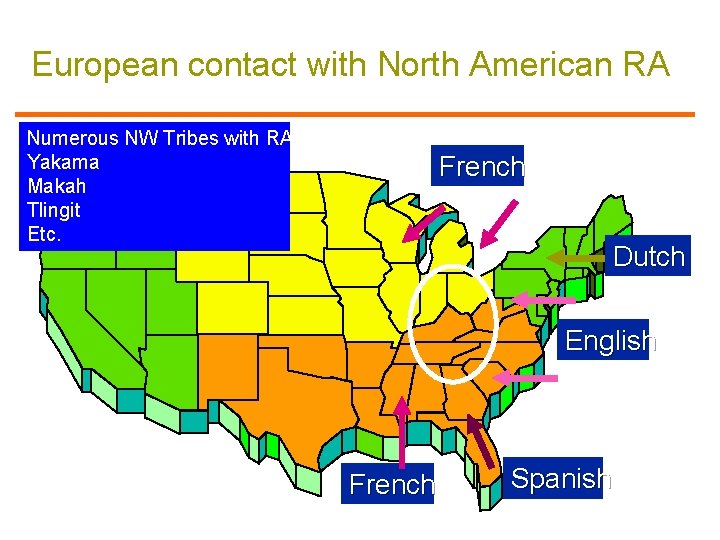
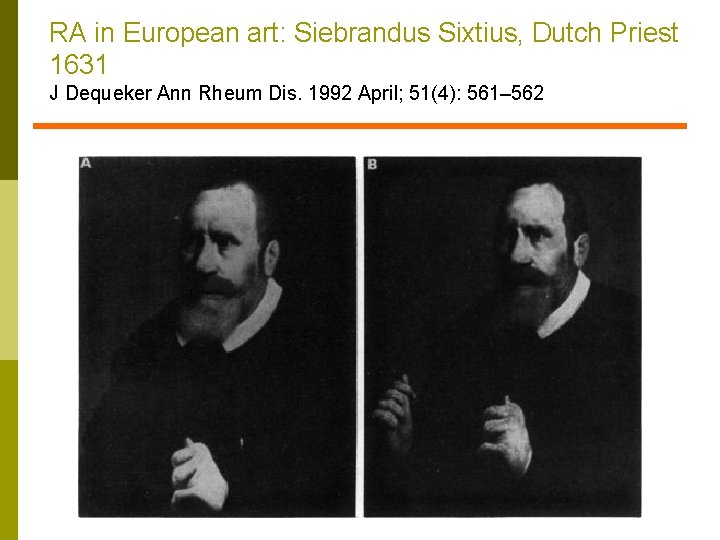
European contact with North American RA Numerous NW Tribes with RA Yakama Makah Tlingit Etc. French Dutch English French Spanish
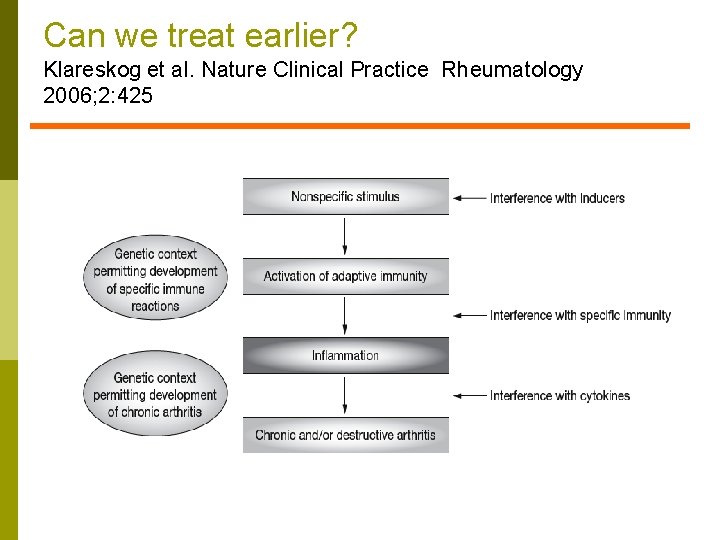
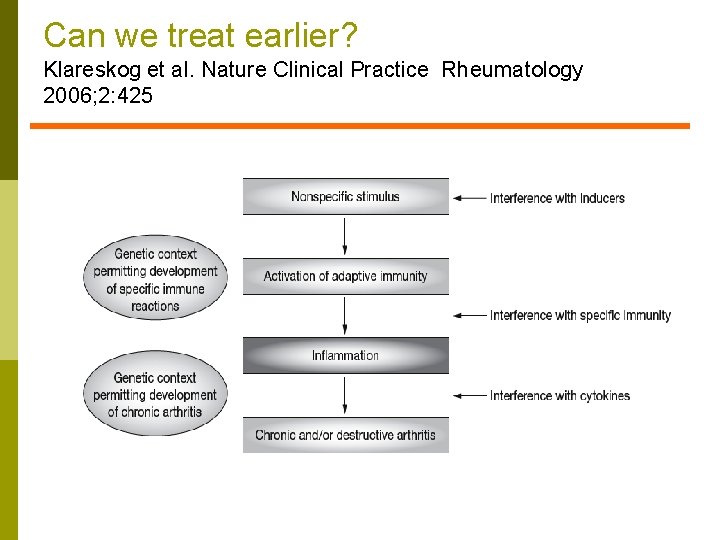
Can we treat earlier? Klareskog et al. Nature Clinical Practice Rheumatology 2006; 2: 425
Rheumatoid Arthritis Clinical Features
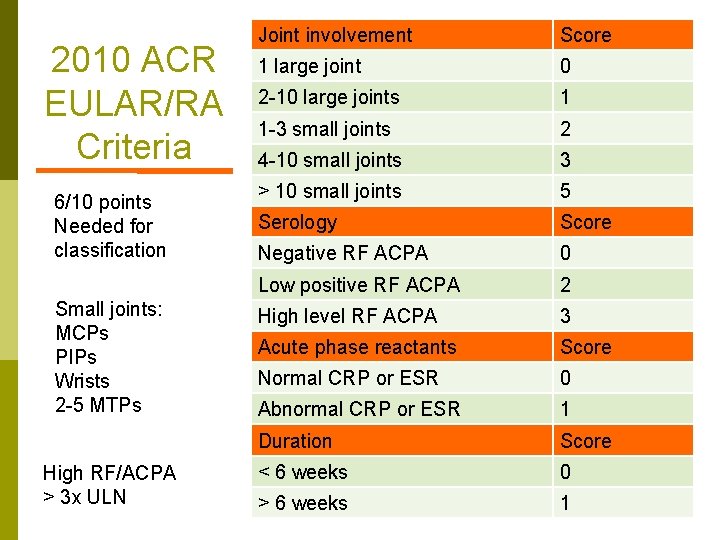
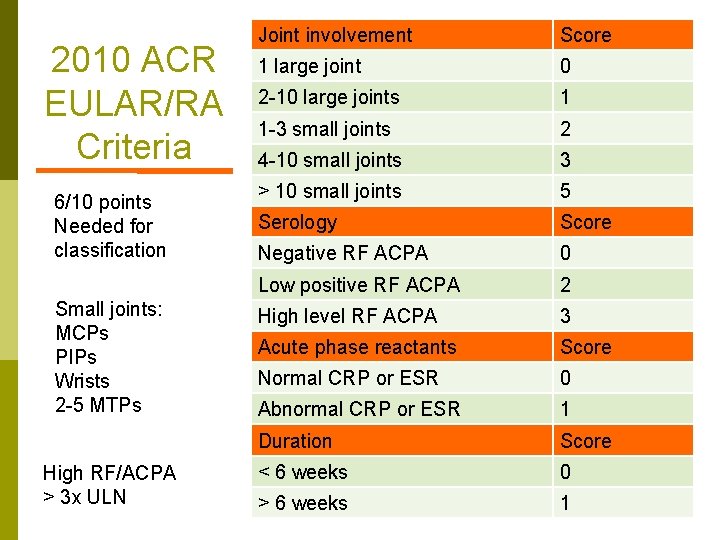
2010 ACR EULAR/RA Criteria 6/10 points Needed for classification Small joints: MCPs PIPs Wrists 2 -5 MTPs High RF/ACPA > 3 x ULN Joint involvement Score 1 large joint 0 2 -10 large joints 1 1 -3 small joints 2 4 -10 small joints 3 > 10 small joints 5 Serology Score Negative RF ACPA 0 Low positive RF ACPA 2 High level RF ACPA 3 Acute phase reactants Score Normal CRP or ESR 0 Abnormal CRP or ESR 1 Duration Score < 6 weeks 0 > 6 weeks 1
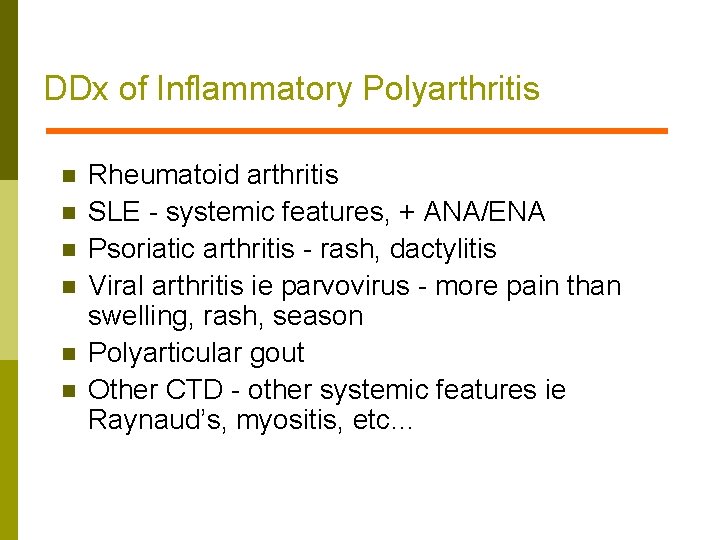
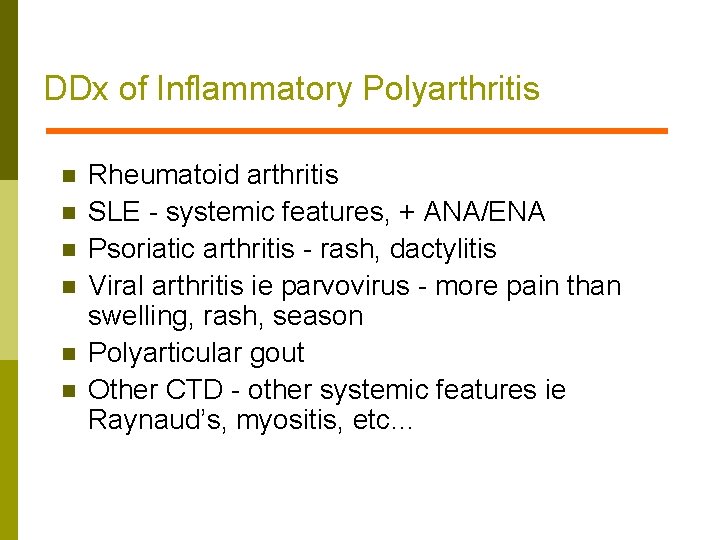
DDx of Inflammatory Polyarthritis n n n Rheumatoid arthritis SLE - systemic features, + ANA/ENA Psoriatic arthritis - rash, dactylitis Viral arthritis ie parvovirus - more pain than swelling, rash, season Polyarticular gout Other CTD - other systemic features ie Raynaud’s, myositis, etc…
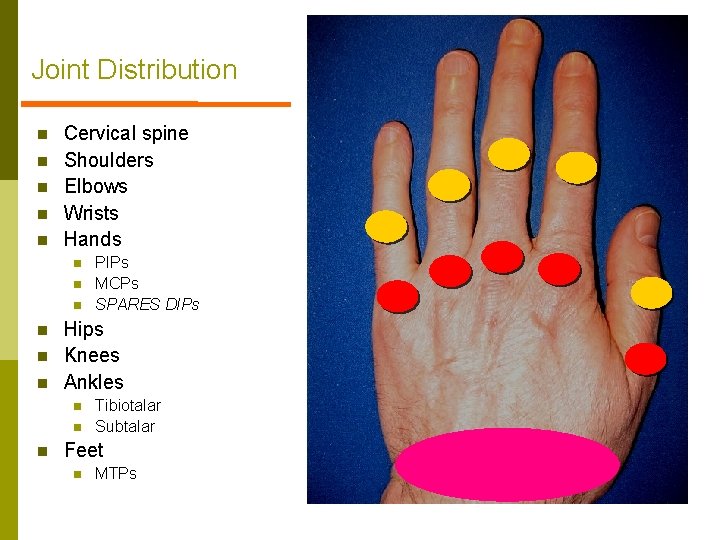
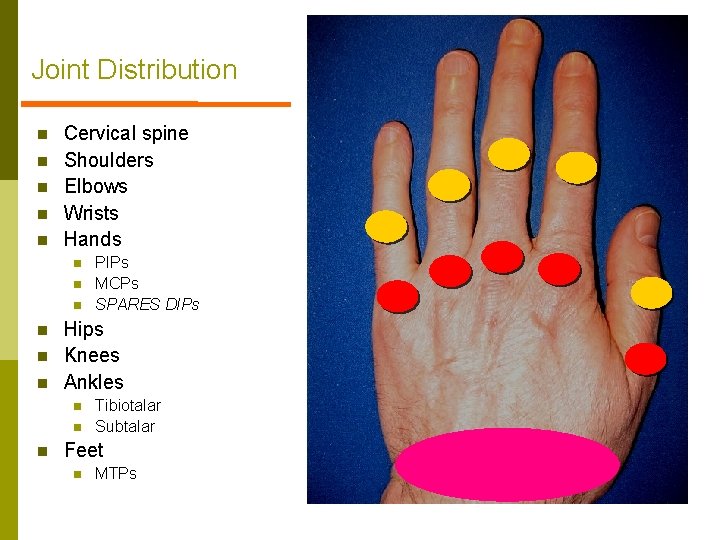
Joint Distribution n n Cervical spine Shoulders Elbows Wrists Hands n n n Hips Knees Ankles n n n PIPs MCPs SPARES DIPs Tibiotalar Subtalar Feet n MTPs

Earliest RA

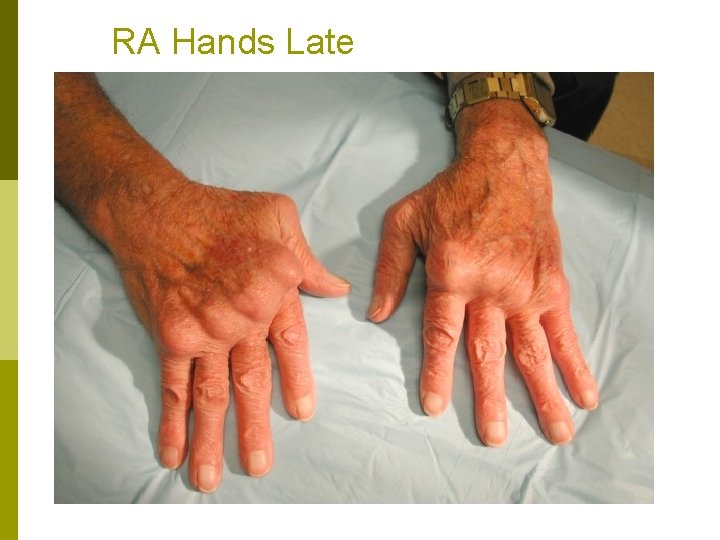
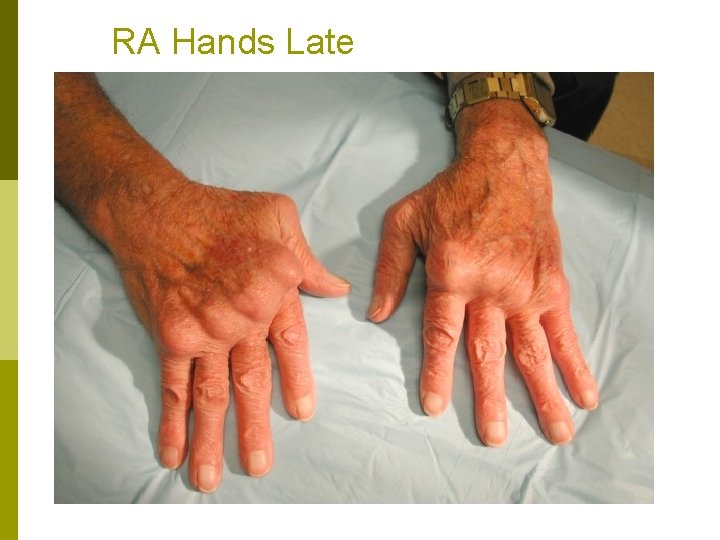
RA Hands Late

RA Feet
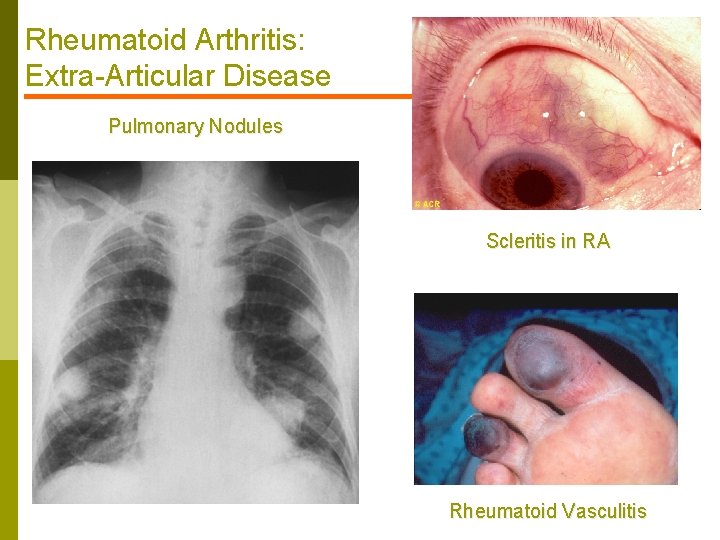
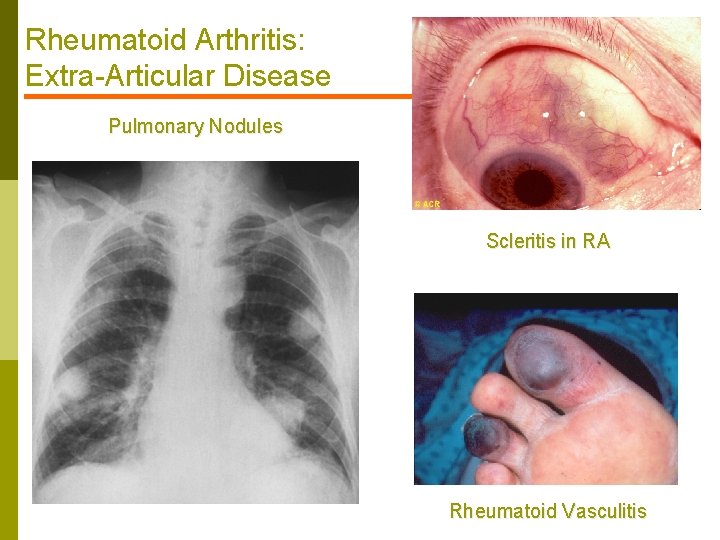
Rheumatoid Arthritis: Extra-Articular Disease Pulmonary Nodules Scleritis in RA Rheumatoid Vasculitis
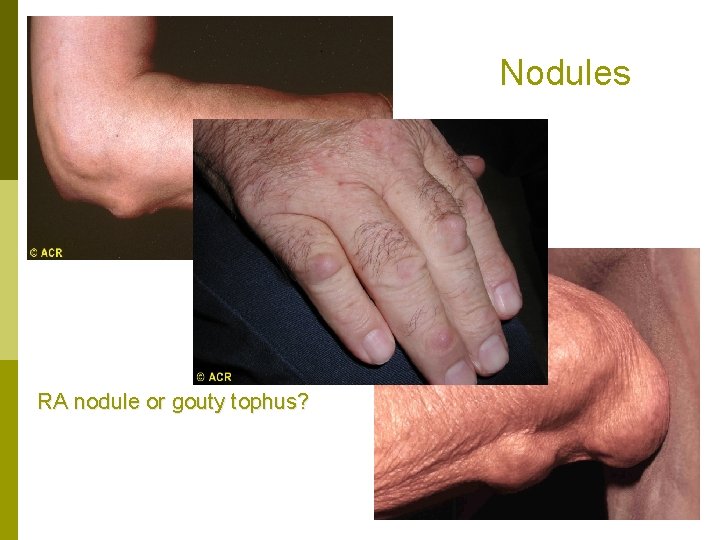
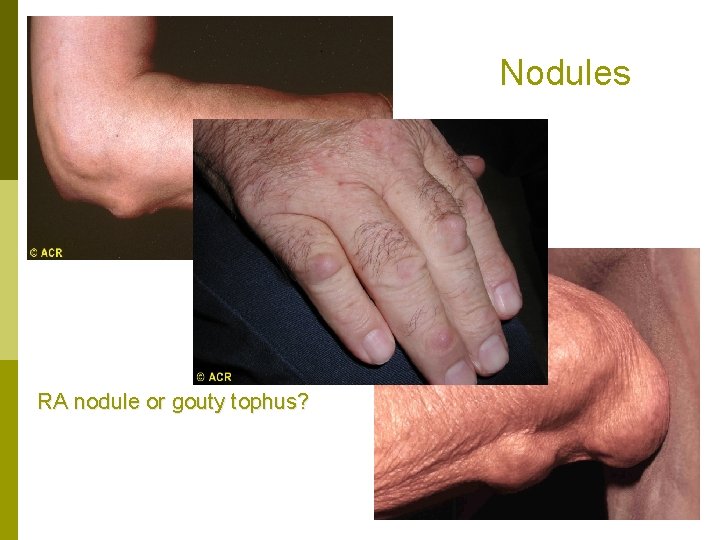
Nodules RA nodule or gouty tophus?
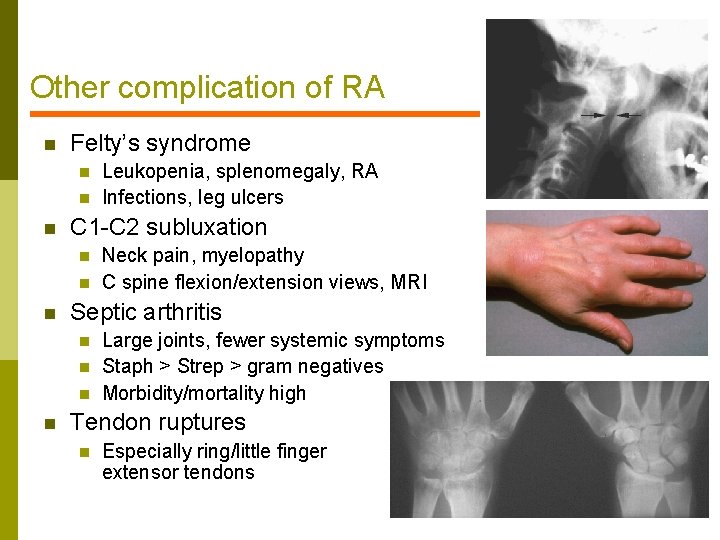
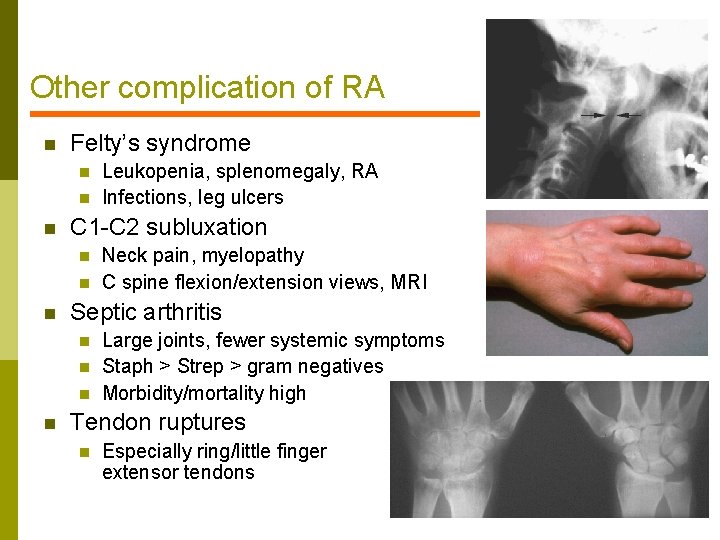
Other complication of RA n Felty’s syndrome n n n C 1 -C 2 subluxation n Neck pain, myelopathy C spine flexion/extension views, MRI Septic arthritis n n Leukopenia, splenomegaly, RA Infections, leg ulcers Large joints, fewer systemic symptoms Staph > Strep > gram negatives Morbidity/mortality high Tendon ruptures n Especially ring/little finger extensor tendons
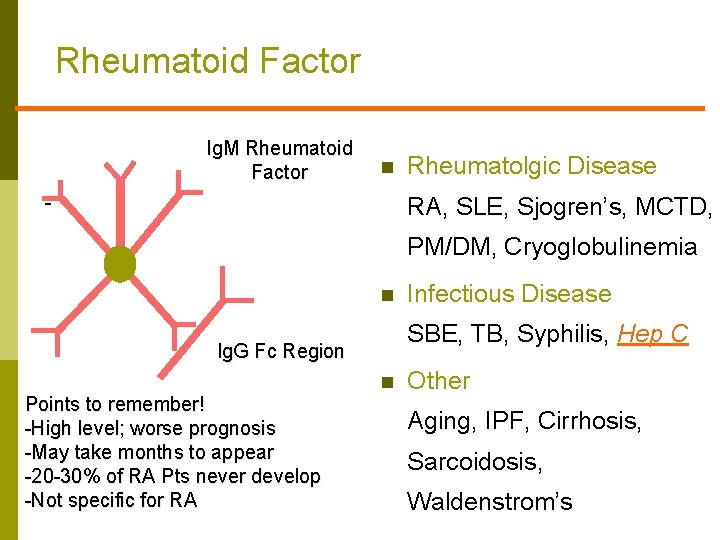
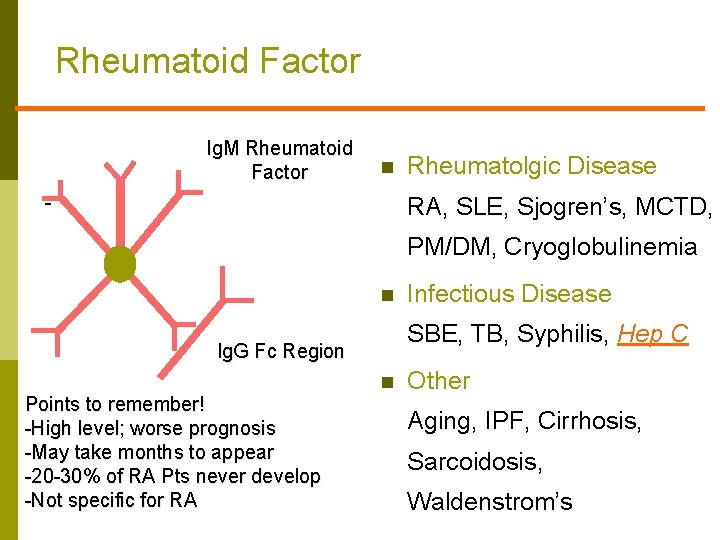
Rheumatoid Factor Ig. M Rheumatoid Factor n Rheumatolgic Disease RA, SLE, Sjogren’s, MCTD, PM/DM, Cryoglobulinemia n SBE, TB, Syphilis, Hep C Ig. G Fc Region Points to remember! -High level; worse prognosis -May take months to appear -20 -30% of RA Pts never develop -Not specific for RA Infectious Disease n Other Aging, IPF, Cirrhosis, Sarcoidosis, Waldenstrom’s
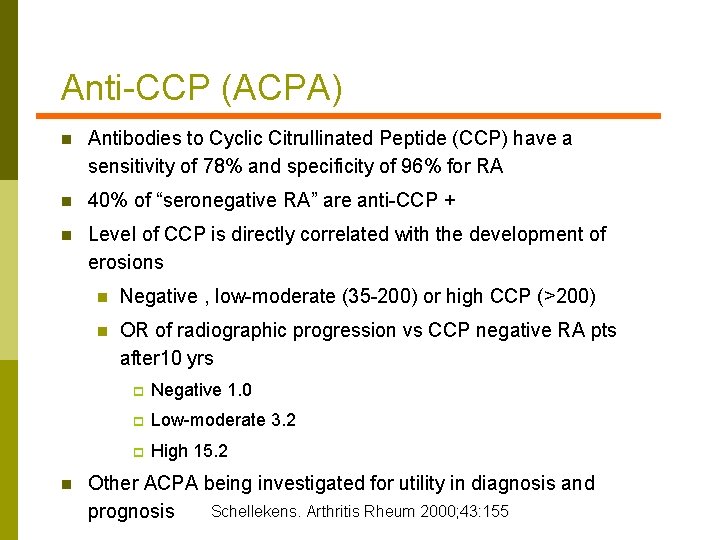
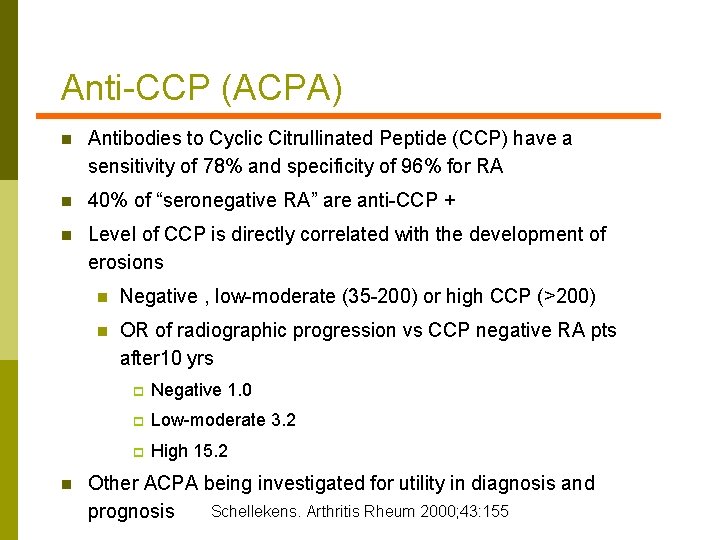
Anti-CCP (ACPA) n Antibodies to Cyclic Citrullinated Peptide (CCP) have a sensitivity of 78% and specificity of 96% for RA n 40% of “seronegative RA” are anti-CCP + n Level of CCP is directly correlated with the development of erosions n n Negative , low-moderate (35 -200) or high CCP (>200) n OR of radiographic progression vs CCP negative RA pts after 10 yrs p Negative 1. 0 p Low-moderate 3. 2 p High 15. 2 Other ACPA being investigated for utility in diagnosis and Schellekens. Arthritis Rheum 2000; 43: 155 prognosis
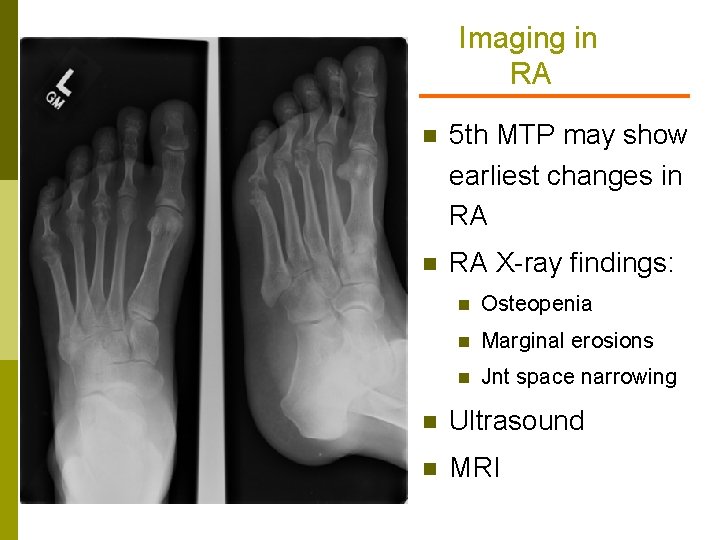
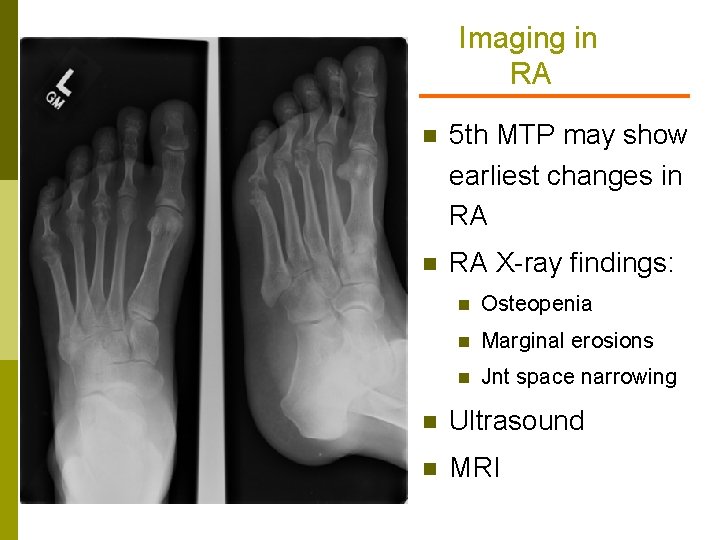
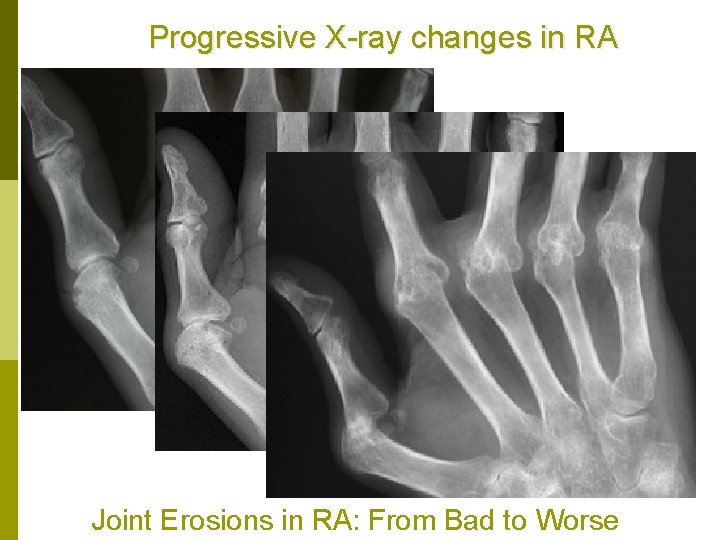
Imaging in RA n 5 th MTP may show earliest changes in RA X-ray findings: n Osteopenia n Marginal erosions n Jnt space narrowing n Ultrasound n MRI
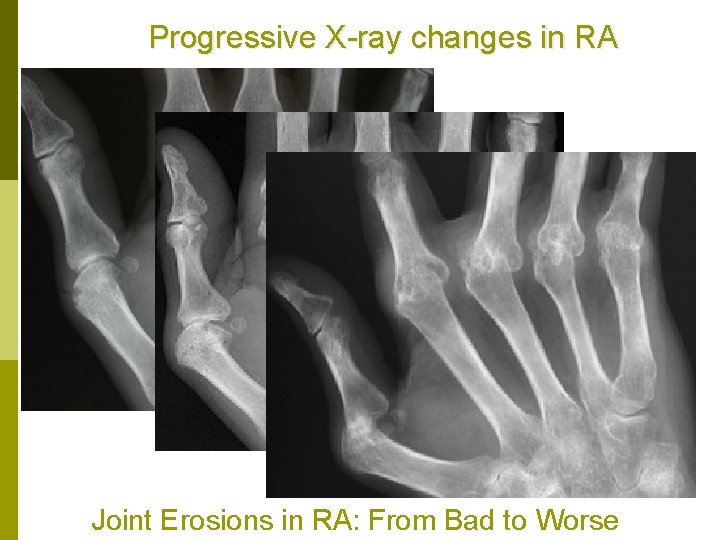
Progressive X-ray changes in RA Joint Erosions in RA: From Bad to Worse
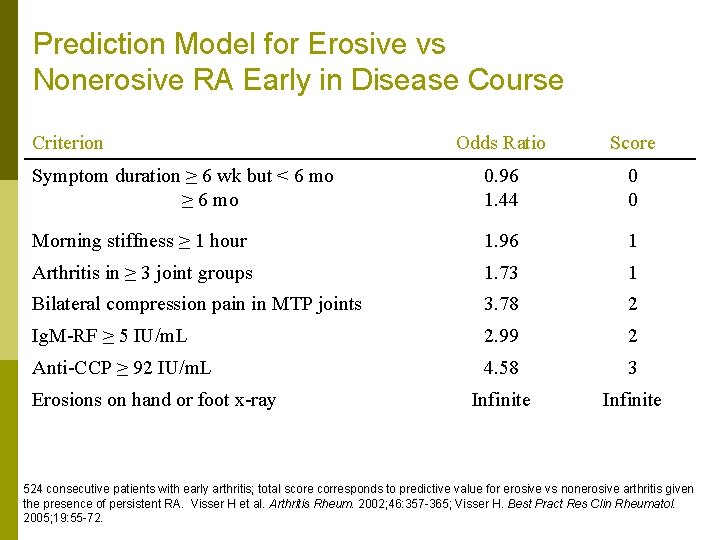
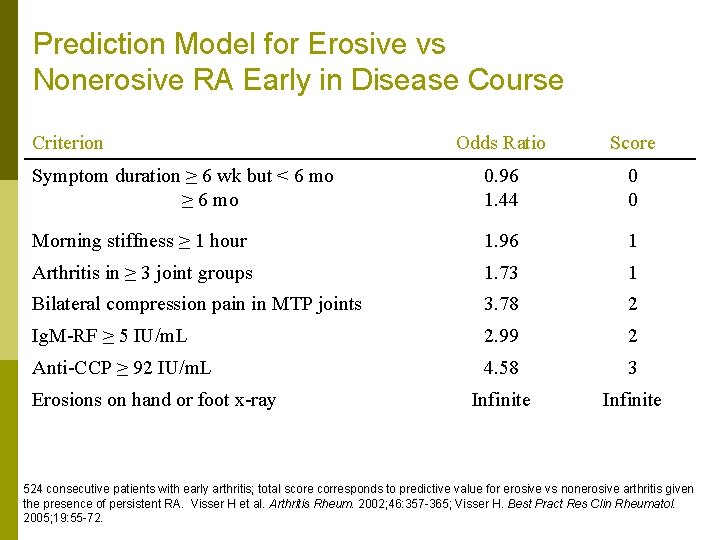
Prediction Model for Erosive vs Nonerosive RA Early in Disease Course Criterion Odds Ratio Score Symptom duration ≥ 6 wk but < 6 mo ≥ 6 mo 0. 96 1. 44 0 0 Morning stiffness ≥ 1 hour 1. 96 1 Arthritis in ≥ 3 joint groups 1. 73 1 Bilateral compression pain in MTP joints 3. 78 2 Ig. M-RF ≥ 5 IU/m. L 2. 99 2 Anti-CCP ≥ 92 IU/m. L 4. 58 3 Infinite Erosions on hand or foot x-ray 524 consecutive patients with early arthritis; total score corresponds to predictive value for erosive vs nonerosive arthritis given the presence of persistent RA. Visser H et al. Arthritis Rheum. 2002; 46: 357 -365; Visser H. Best Pract Res Clin Rheumatol. 2005; 19: 55 -72.
Rheumatoid Arthritis Treatment Issues
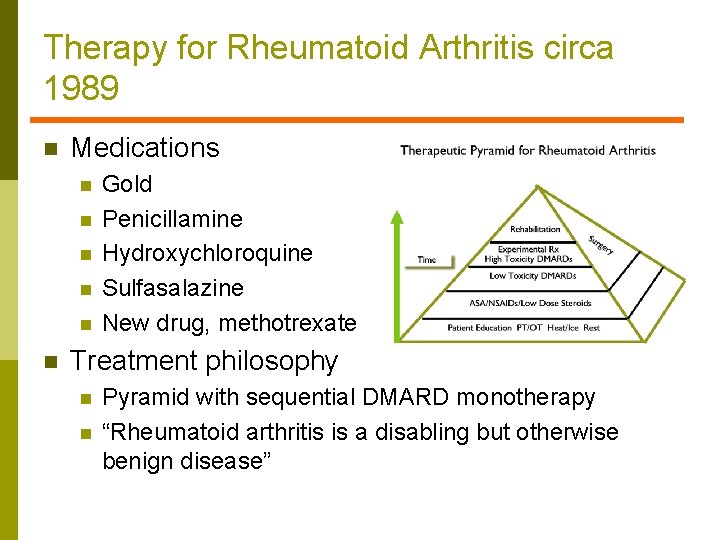
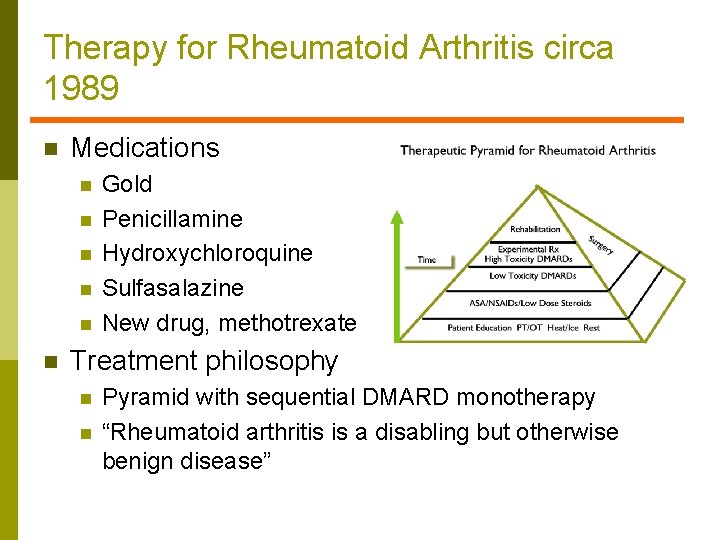
Therapy for Rheumatoid Arthritis circa 1989 n Medications n n n Gold Penicillamine Hydroxychloroquine Sulfasalazine New drug, methotrexate Treatment philosophy n n Pyramid with sequential DMARD monotherapy “Rheumatoid arthritis is a disabling but otherwise benign disease”
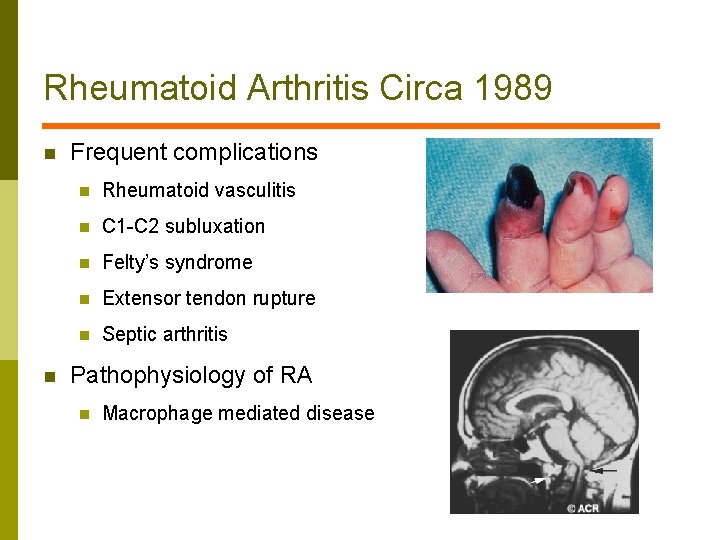
Rheumatoid Arthritis Circa 1989 n n Frequent complications n Rheumatoid vasculitis n C 1 -C 2 subluxation n Felty’s syndrome n Extensor tendon rupture n Septic arthritis Pathophysiology of RA n Macrophage mediated disease
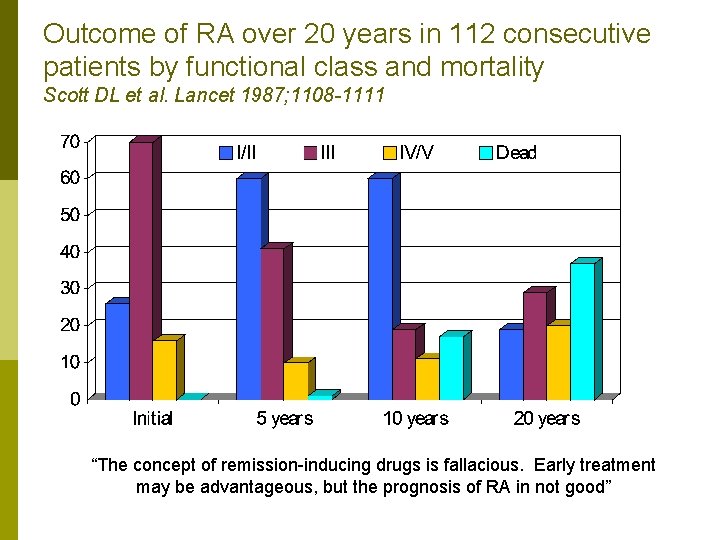
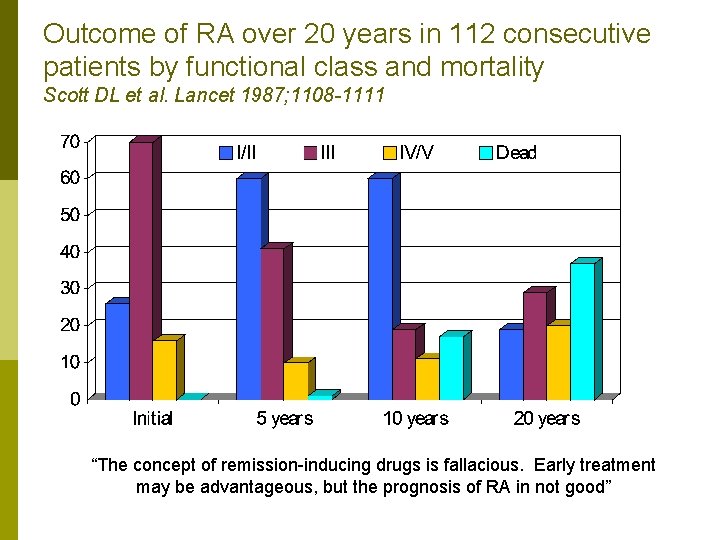
Outcome of RA over 20 years in 112 consecutive patients by functional class and mortality Scott DL et al. Lancet 1987; 1108 -1111 “The concept of remission-inducing drugs is fallacious. Early treatment may be advantageous, but the prognosis of RA in not good”
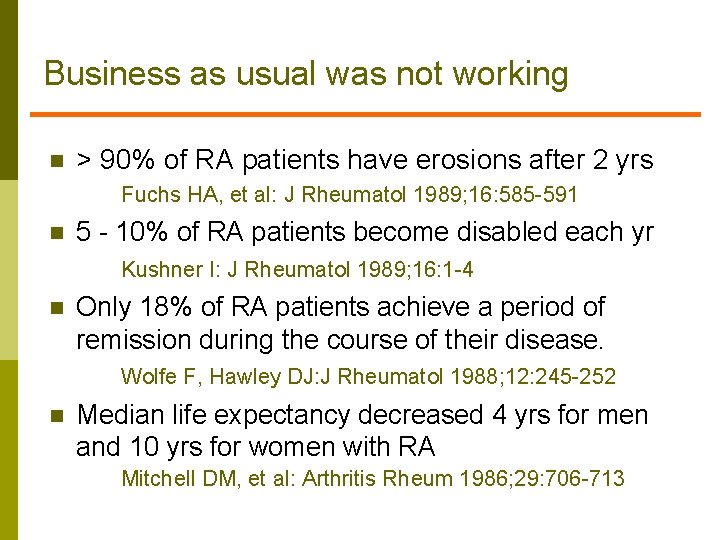
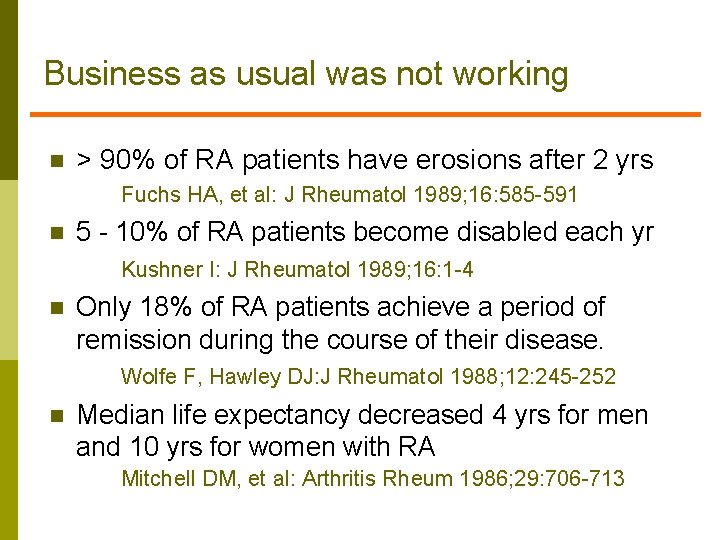
Business as usual was not working n > 90% of RA patients have erosions after 2 yrs Fuchs HA, et al: J Rheumatol 1989; 16: 585 -591 n 5 - 10% of RA patients become disabled each yr Kushner I: J Rheumatol 1989; 16: 1 -4 n Only 18% of RA patients achieve a period of remission during the course of their disease. Wolfe F, Hawley DJ: J Rheumatol 1988; 12: 245 -252 n Median life expectancy decreased 4 yrs for men and 10 yrs for women with RA Mitchell DM, et al: Arthritis Rheum 1986; 29: 706 -713
Irving Kushner, M. D. J Rheumatol 1989; 16: 1 -4 “What we need in RA is a drug for which one does not need a statistician to see the beneficial effects”
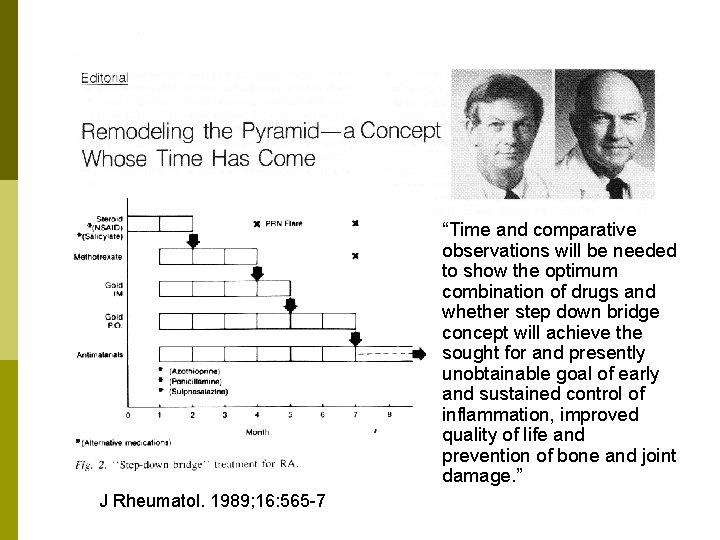
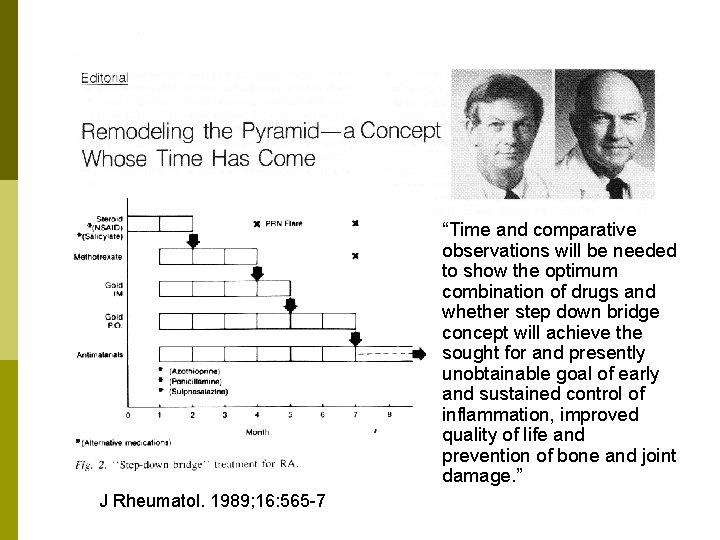
“Time and comparative observations will be needed to show the optimum combination of drugs and whether step down bridge concept will achieve the sought for and presently unobtainable goal of early and sustained control of inflammation, improved quality of life and prevention of bone and joint damage. ” J Rheumatol. 1989; 16: 565 -7
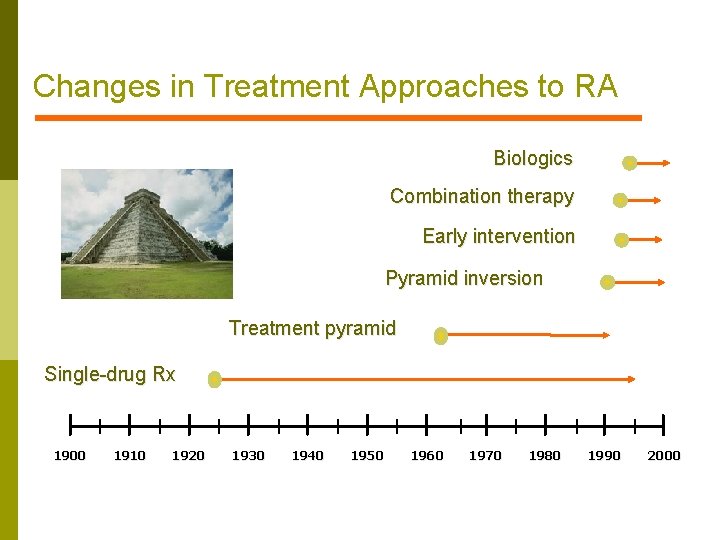
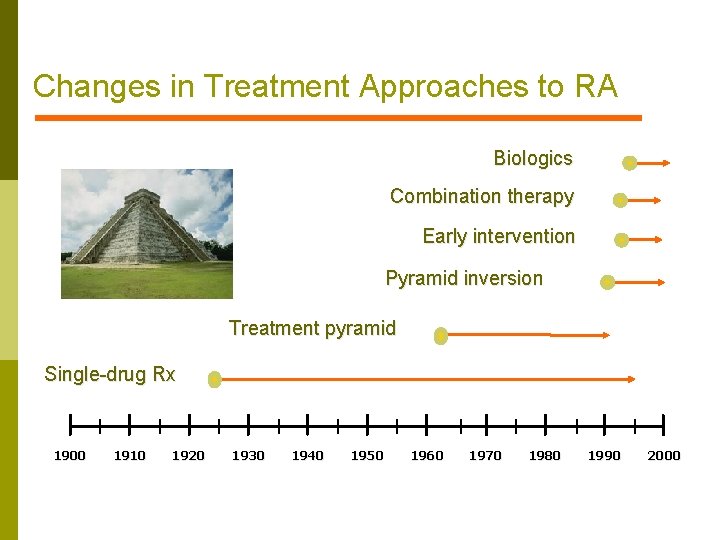
Changes in Treatment Approaches to RA Biologics Combination therapy Early intervention Pyramid inversion Treatment pyramid Single-drug Rx 1900 1910 1920 1930 1940 1950 1960 1970 1980 1990 2000
RA treatment themes 2011 n Early recognition, early institution of therapy especially with those with poor prognostic markers n Presence of erosions n High titer anti-CCP/RF n Treat to DAS (disease activity score) or some other measure of disease activity (SDAI, CDAI etc) n Methotrexate mainstay in most pts; dose to 15 -20 mg/week n Consider early institution of biologic therapy n Strategies for using biologics under study ie initial therapy with subsequent withdrawl vs add (discussed below)
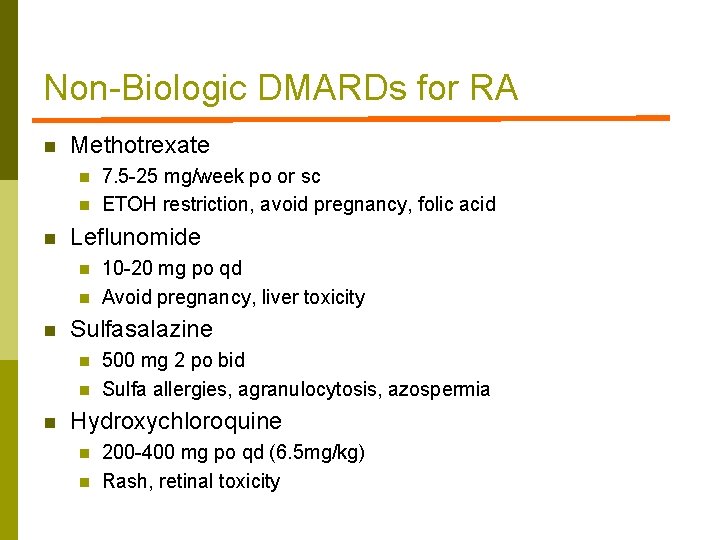
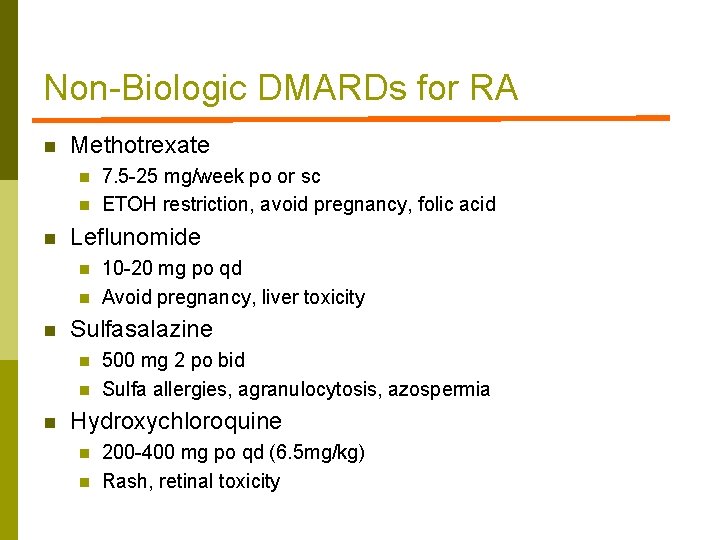
Non-Biologic DMARDs for RA n Methotrexate n n n Leflunomide n n n 10 -20 mg po qd Avoid pregnancy, liver toxicity Sulfasalazine n n n 7. 5 -25 mg/week po or sc ETOH restriction, avoid pregnancy, folic acid 500 mg 2 po bid Sulfa allergies, agranulocytosis, azospermia Hydroxychloroquine n n 200 -400 mg po qd (6. 5 mg/kg) Rash, retinal toxicity

Biologic Therapies 2011 n Anti-TNF agents n n n Etanercept Adalimumab Infliximab Certozilumab Golimumab Anti-B cell agent n Rituximab n Anti-T cell agent n n Anti-IL-6 receptor antagonist n n Abatacept Tocilizumab Coming attractions n n Jak-2 inhibitors Anti-IL-17 therapy
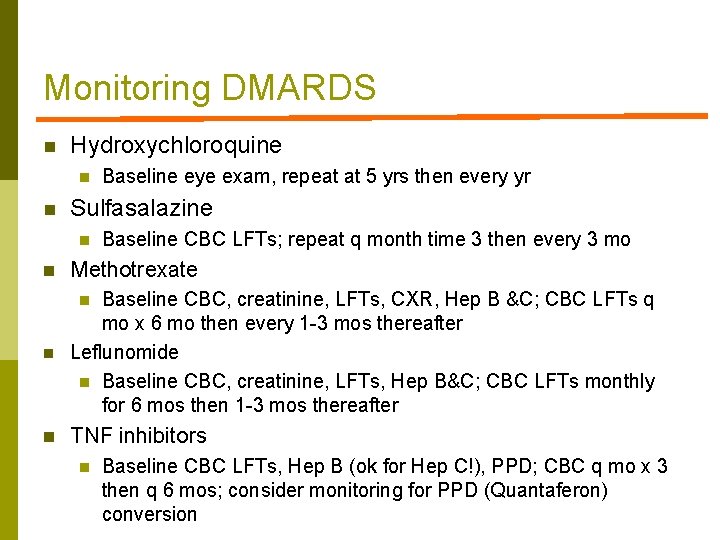
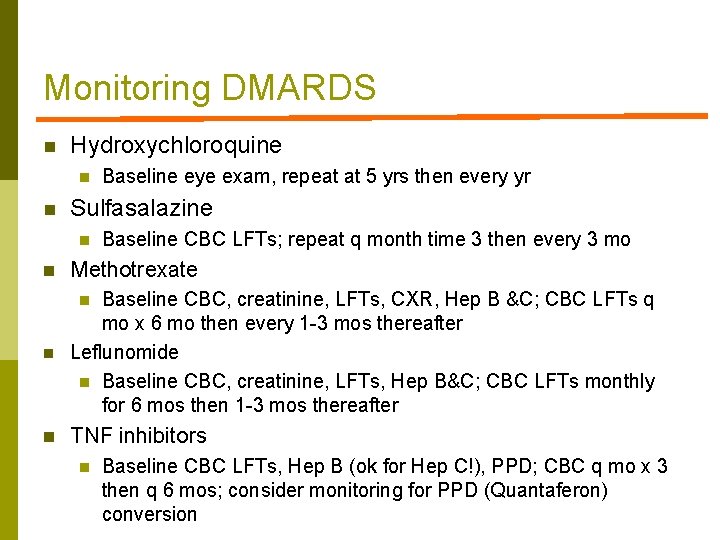
Monitoring DMARDS n Hydroxychloroquine n n Baseline eye exam, repeat at 5 yrs then every yr Sulfasalazine n Baseline CBC LFTs; repeat q month time 3 then every 3 mo n Methotrexate n Baseline CBC, creatinine, LFTs, CXR, Hep B &C; CBC LFTs q mo x 6 mo then every 1 -3 mos thereafter Leflunomide n Baseline CBC, creatinine, LFTs, Hep B&C; CBC LFTs monthly for 6 mos then 1 -3 mos thereafter n TNF inhibitors n n Baseline CBC LFTs, Hep B (ok for Hep C!), PPD; CBC q mo x 3 then q 6 mos; consider monitoring for PPD (Quantaferon) conversion
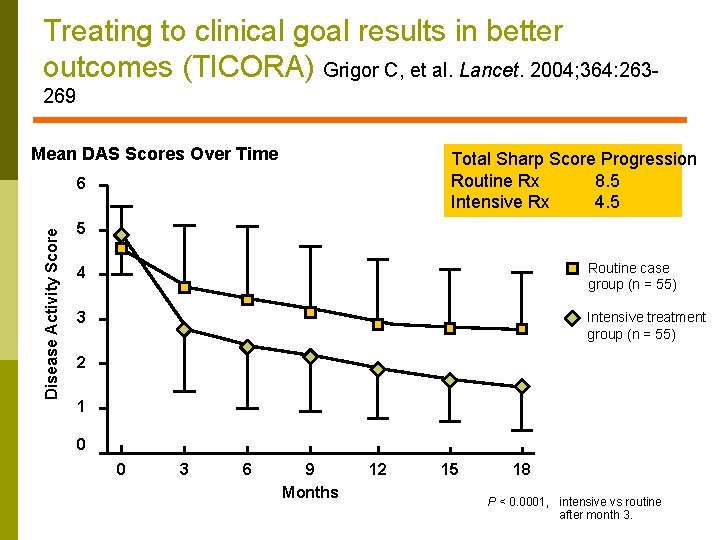
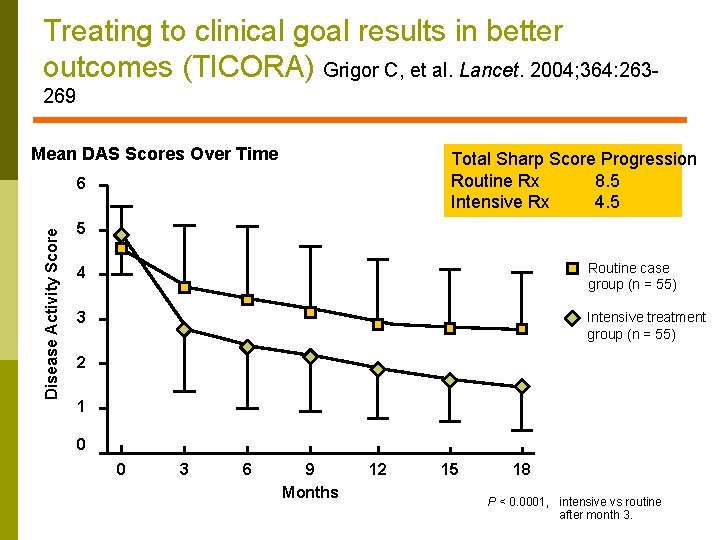
Treating to clinical goal results in better outcomes (TICORA) Grigor C, et al. Lancet. 2004; 364: 263269 Mean DAS Scores Over Time Total Sharp Score Progression Routine Rx 8. 5 Intensive Rx 4. 5 Disease Activity Score 6 5 4 Routine case group (n = 55) 3 Intensive treatment group (n = 55) 2 1 0 0 3 6 9 Months 12 15 18 P < 0. 0001, intensive vs routine after month 3.
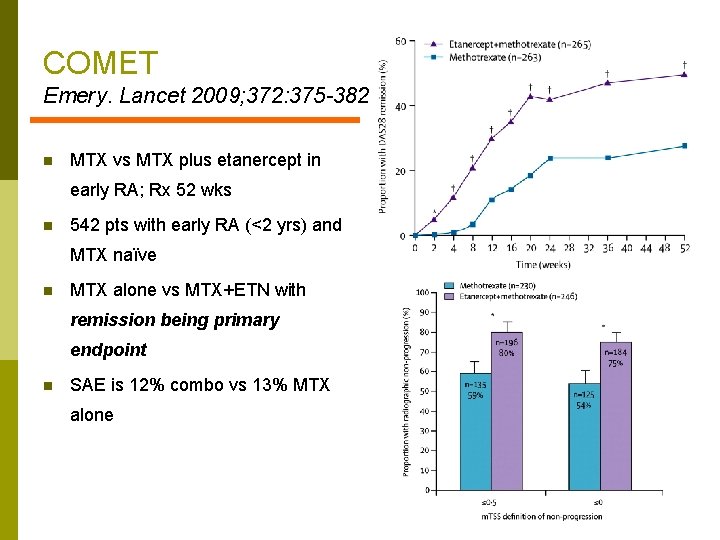
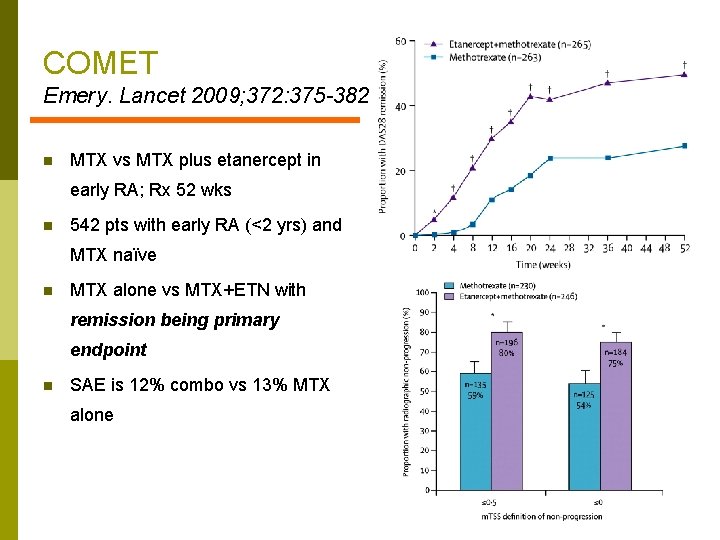
COMET Emery. Lancet 2009; 372: 375 -382 n MTX vs MTX plus etanercept in early RA; Rx 52 wks n 542 pts with early RA (<2 yrs) and MTX naïve n MTX alone vs MTX+ETN with remission being primary endpoint n SAE is 12% combo vs 13% MTX alone
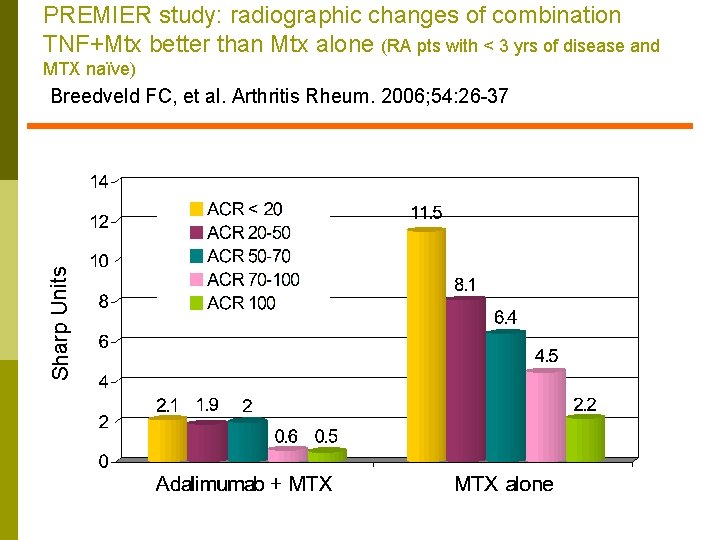
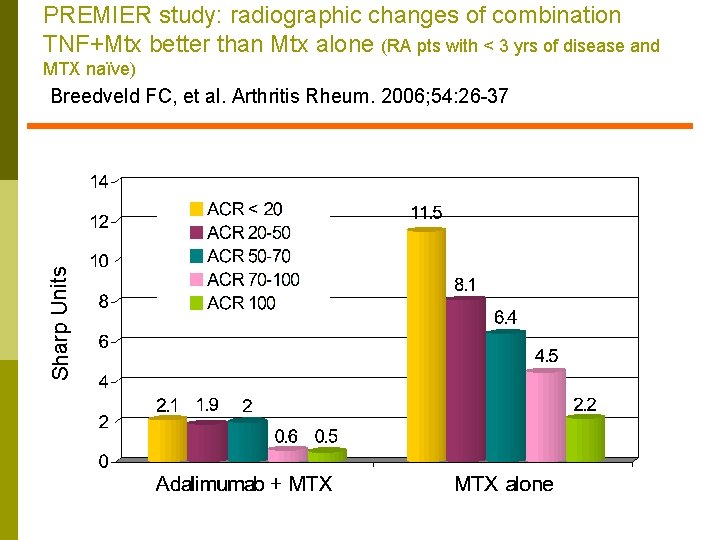
PREMIER study: radiographic changes of combination TNF+Mtx better than Mtx alone (RA pts with < 3 yrs of disease and MTX naïve) Sharp Units Breedveld FC, et al. Arthritis Rheum. 2006; 54: 26 -37
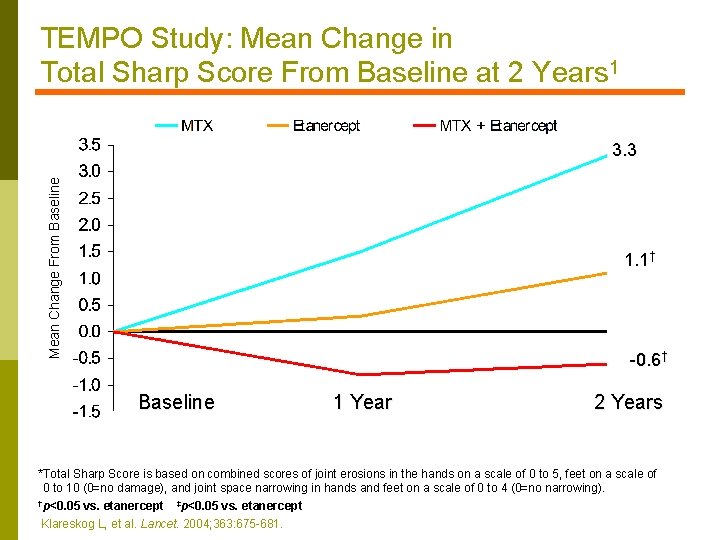
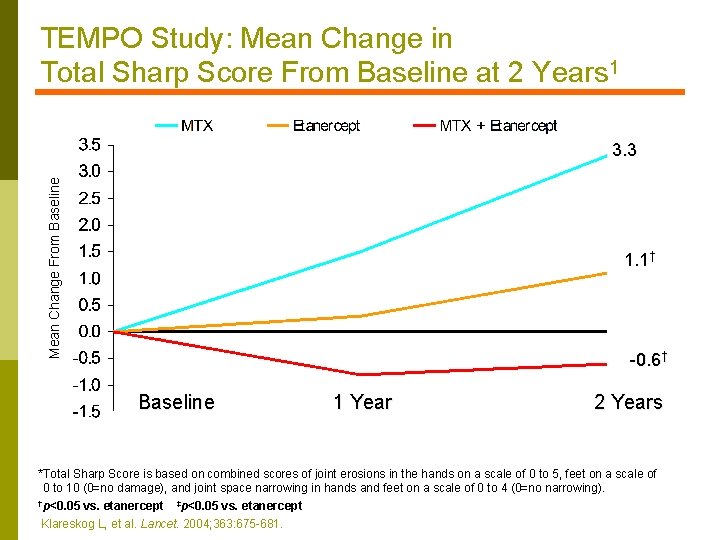
TEMPO Study: Mean Change in Total Sharp Score From Baseline at 2 Years 1 Mean Change From Baseline 3. 3 1. 1† -0. 6† Baseline Inhibition 1 Year 2 Years *Total Sharp Score is based on combined scores of joint erosions in the hands on a scale of 0 to 5, feet on a scale of 0 to 10 (0=no damage), and joint space narrowing in hands and feet on a scale of 0 to 4 (0=no narrowing). †p<0. 05 vs. etanercept ‡p<0. 05 vs. etanercept Klareskog L, et al. Lancet. 2004; 363: 675 -681.
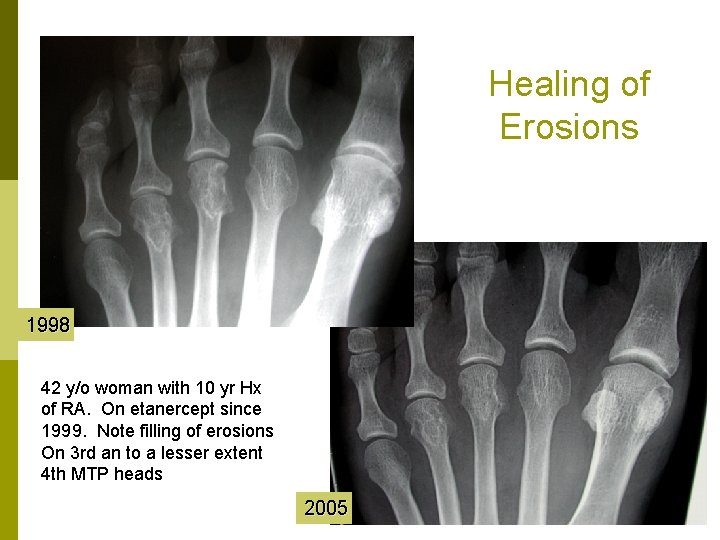
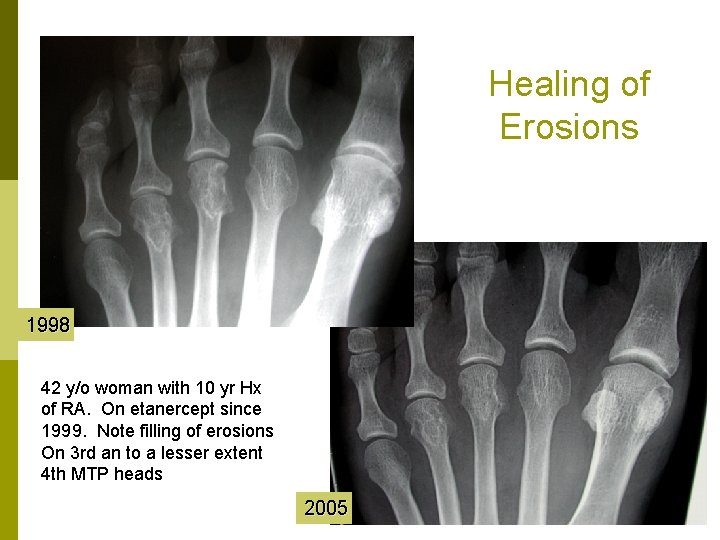
Healing of Erosions 1998 42 y/o woman with 10 yr Hx of RA. On etanercept since 1999. Note filling of erosions On 3 rd an to a lesser extent 4 th MTP heads 2005
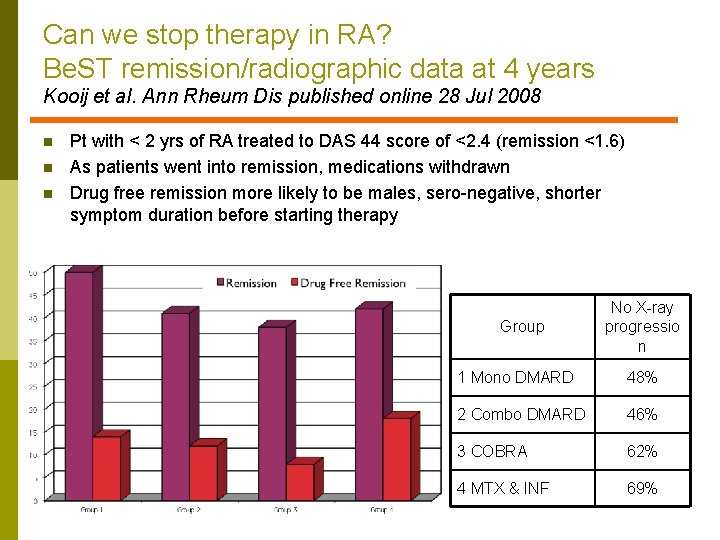
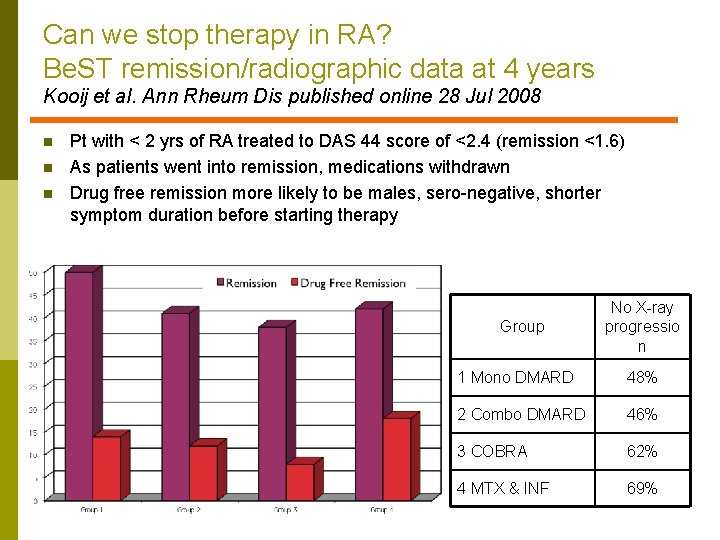
Can we stop therapy in RA? Be. ST remission/radiographic data at 4 years Kooij et al. Ann Rheum Dis published online 28 Jul 2008 n n n Pt with < 2 yrs of RA treated to DAS 44 score of <2. 4 (remission <1. 6) As patients went into remission, medications withdrawn Drug free remission more likely to be males, sero-negative, shorter symptom duration before starting therapy Group No X-ray progressio n 1 Mono DMARD 48% 2 Combo DMARD 46% 3 COBRA 62% 4 MTX & INF 69%
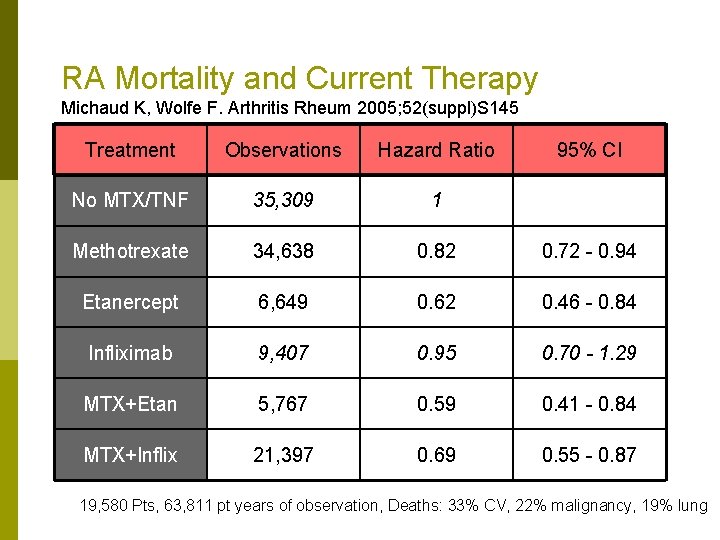
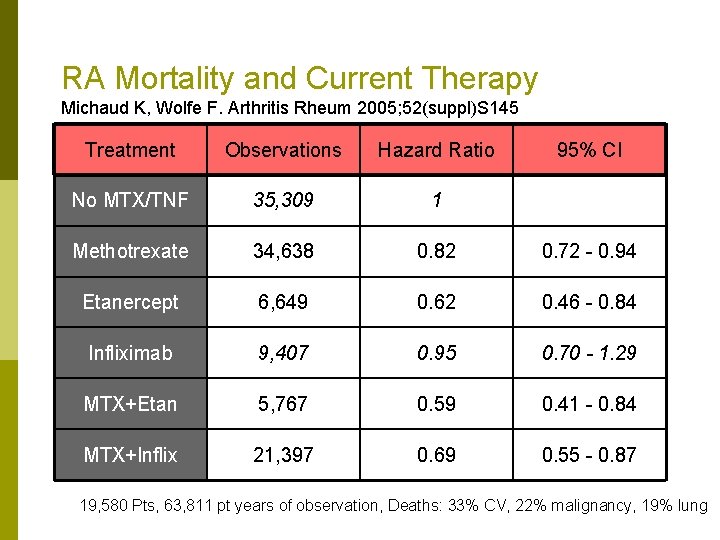
RA Mortality and Current Therapy Michaud K, Wolfe F. Arthritis Rheum 2005; 52(suppl)S 145 Treatment Observations Hazard Ratio 95% CI No MTX/TNF 35, 309 1 Methotrexate 34, 638 0. 82 0. 72 - 0. 94 Etanercept 6, 649 0. 62 0. 46 - 0. 84 Infliximab 9, 407 0. 95 0. 70 - 1. 29 MTX+Etan 5, 767 0. 59 0. 41 - 0. 84 MTX+Inflix 21, 397 0. 69 0. 55 - 0. 87 19, 580 Pts, 63, 811 pt years of observation, Deaths: 33% CV, 22% malignancy, 19% lung
DL Scott on Early Aggressive Therapy Scott DL. British Medical Bulletin 2007 81 -82(1): 97 -114 “At present, it seems sensible to focus on trying to rapidly identify patients with the most severe early RA, particularly patients who are seropositive for rheumatoid factor and have early erosive damage, and give them intensive treatment. There is some evidence, albeit incomplete, that combination therapy using TNFinhibitors is most effective. ”
Rheumatoid Arthritis Perioperative Management
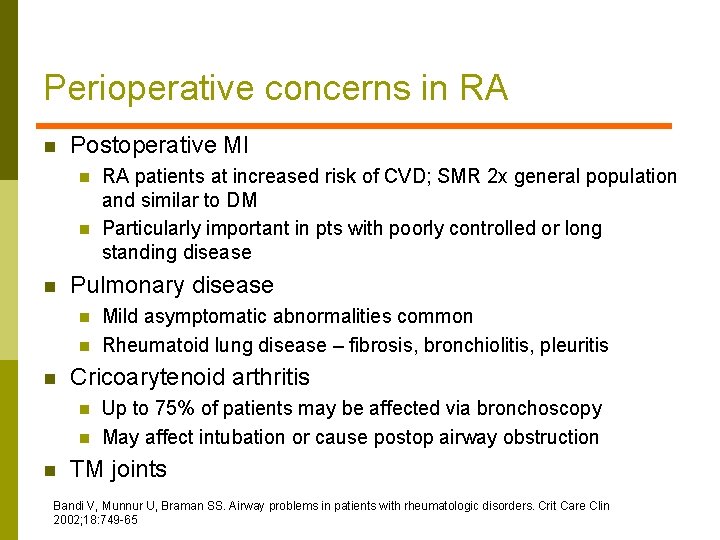
Perioperative concerns in RA n Postoperative MI n n n Pulmonary disease n n n Mild asymptomatic abnormalities common Rheumatoid lung disease – fibrosis, bronchiolitis, pleuritis Cricoarytenoid arthritis n n n RA patients at increased risk of CVD; SMR 2 x general population and similar to DM Particularly important in pts with poorly controlled or long standing disease Up to 75% of patients may be affected via bronchoscopy May affect intubation or cause postop airway obstruction TM joints Bandi V, Munnur U, Braman SS. Airway problems in patients with rheumatologic disorders. Crit Care Clin 2002; 18: 749 -65
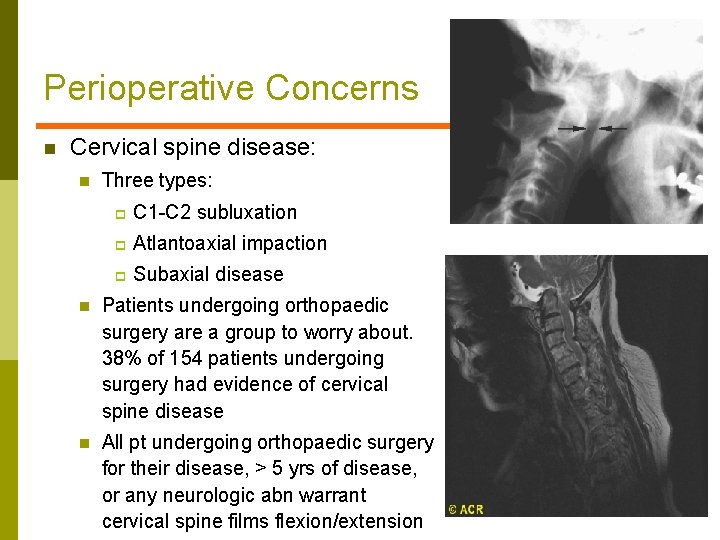
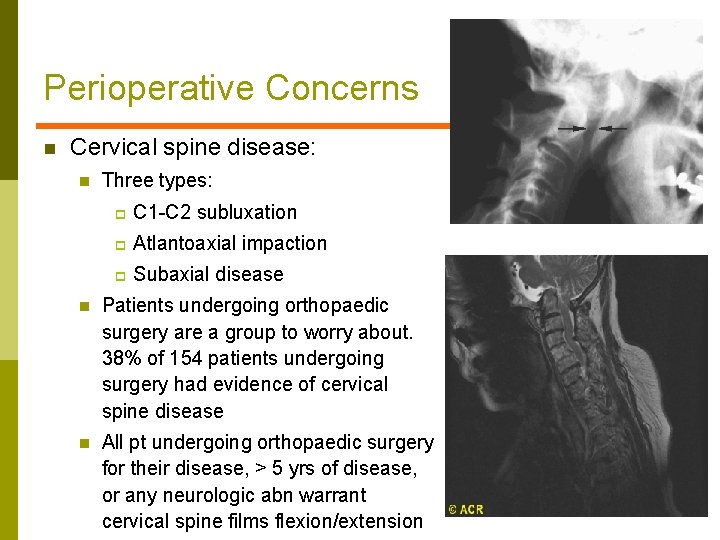
Perioperative Concerns n Cervical spine disease: n Three types: p C 1 -C 2 subluxation p Atlantoaxial impaction p Subaxial disease n Patients undergoing orthopaedic surgery are a group to worry about. 38% of 154 patients undergoing surgery had evidence of cervical spine disease n All pt undergoing orthopaedic surgery for their disease, > 5 yrs of disease, or any neurologic abn warrant cervical spine films flexion/extension
NSAIDs n n Not utilized as intensely as in years gone by Use puts patient at risk for intraop bleeding and postop GI bleeding n n n Sponge weights and suction volumes indicate that NSAID use up to the time of surgery increase blood loss by factor of two and increases transfusion requirements (mortality? ) Recommendation is to stop NSAIDs 5 half-lives before surgery ASA should be stopped 10 -14 days before surgery n What about primary and secondary prophylaxis? Hi risk?
Methotrexate n Continue for most surgeries n n Consider temporary stop for: n n n Grennan demonstrated fewer infections and flares in group of RA patients who continued Mtx perioperatively Rising creatinine Post op infection Long period of NPO Patients over 70 yrs Toxiciy: bone marrow suppression, severe stomatitis n Rx with folinic acid po or IV
Other Non-Biologic DMARDs n Leflunomide n n Sulfasalazine – no reason to stop except for NPO n n Half-life of 2 weeks 2 studies with opposite conclusions regarding wound healing issues Consider stopping 1 month before surgery where large wounds expected May be protective against infection Hydroxychloroquine – no reason to stop n Used as postop anticoagulant in years gone by
TNF Agents n n Suggest holding for now TNF agent for moderate to intense procedures; continue for minor Hold based on half-life; hold at least 2 half lives n n n Etanercept – half life 3. 5 -5. 5 days Adalimumab – half life 10 -20 days Infliximab – half life 9. 5 days Certolizumab– half life 14 days Golumimab – half life 14 days Restart 10 -14 days postop
Summary n n Exciting changes in the treatment of RA over the last 20 years; most patients will never know how sick they could be! Remember themes n n Early recognition, early therapy Treat to objective – low disease activity/remission Early institution of biologics/combination therapy Treatments and treatment schemes evolving
 Nursing diagnosis for gouty arthritis
Nursing diagnosis for gouty arthritis Polyarticular arthritis
Polyarticular arthritis Rheumatoid arthritis
Rheumatoid arthritis What is esr
What is esr Osteoarthritis vs rheumatoid arthritis
Osteoarthritis vs rheumatoid arthritis Anti tnf mechanism of action
Anti tnf mechanism of action Abatacept
Abatacept Pathology of rheumatoid arthritis
Pathology of rheumatoid arthritis Steinbrocker stage rheumatoid arthritis
Steinbrocker stage rheumatoid arthritis Spondyloarthropathy
Spondyloarthropathy Radial head fractire
Radial head fractire Haart side effects
Haart side effects Nursing management of arthritis
Nursing management of arthritis B t cells
B t cells Rheumatoid arthritis extra-articular manifestations
Rheumatoid arthritis extra-articular manifestations Gardner and gardner 1969
Gardner and gardner 1969 Gregory gardner md
Gregory gardner md Backup and recovery techniques
Backup and recovery techniques Rheumatoid factor range
Rheumatoid factor range Seronegative arthritis
Seronegative arthritis Haemophilus influenzae septic arthritis
Haemophilus influenzae septic arthritis Caprine arthritis encefalitis
Caprine arthritis encefalitis Gonorrhea symptoms female
Gonorrhea symptoms female Narbentypen
Narbentypen Reactive arthritis pathophysiology
Reactive arthritis pathophysiology Kode icd 10 osteoarthritis genu
Kode icd 10 osteoarthritis genu Allergies and arthritis
Allergies and arthritis Septic arthritis antibiotics
Septic arthritis antibiotics Ans
Ans Sacroiliitis grade 3
Sacroiliitis grade 3 Flitting and fleeting arthritis
Flitting and fleeting arthritis Icd 10 muscle
Icd 10 muscle Anatomi fisiologi asam urat
Anatomi fisiologi asam urat Jean luc meynard
Jean luc meynard Gardening with arthritis
Gardening with arthritis Viral arthritis
Viral arthritis Reiter's syndrome
Reiter's syndrome Arthritis foundation indiana
Arthritis foundation indiana Poststreptococcal reactive arthritis
Poststreptococcal reactive arthritis Infusion therapy for arthritis
Infusion therapy for arthritis Septic arthritis workup
Septic arthritis workup Haemophilus influenzae
Haemophilus influenzae Septic arthritis complications
Septic arthritis complications Arthritis and food allergies
Arthritis and food allergies Carol maury
Carol maury Peripheral arthritis
Peripheral arthritis Is gout like arthritis
Is gout like arthritis Septic arthritis complications
Septic arthritis complications Septic arthritis
Septic arthritis Gossec
Gossec Rehaklinik psoriasis arthritis
Rehaklinik psoriasis arthritis Arthritis treatment
Arthritis treatment Example of gram negative cocci
Example of gram negative cocci Septic arthritis antibiotics
Septic arthritis antibiotics Psoriasis arthritis nhs
Psoriasis arthritis nhs Was will smith homeless
Was will smith homeless Multiple intelligences musical
Multiple intelligences musical Spleen examination
Spleen examination Gardner theory of intelligence slideshare
Gardner theory of intelligence slideshare