Update from Recent Trials Professor Kausik Ray Professor











- Slides: 42
Update from Recent Trials Professor Kausik Ray Professor of Cardiovascular Disease Prevention BSc (hons), MBCh. B, MD, Mphil (Cantab), FRCP, FACC, FESC, FAHA 2014
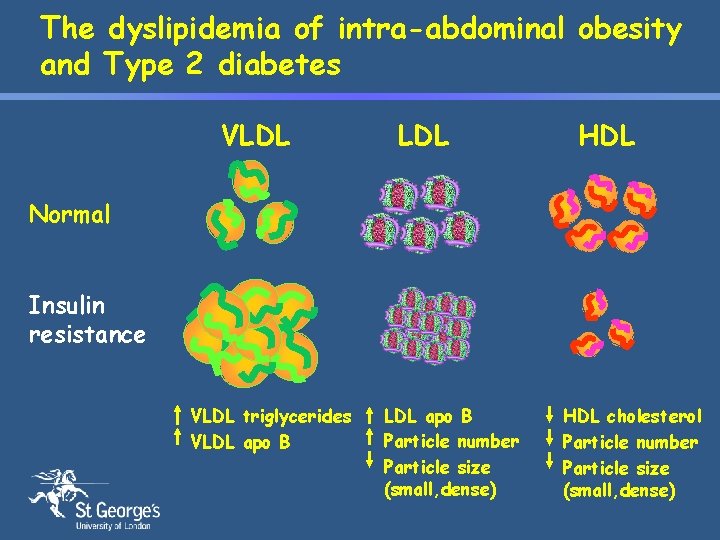
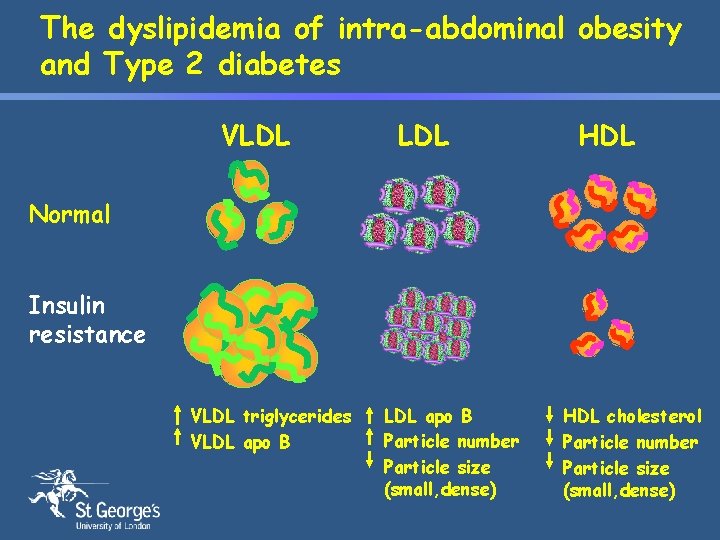
The dyslipidemia of intra-abdominal obesity and Type 2 diabetes VLDL HDL Normal Insulin resistance VLDL triglycerides VLDL apo B Particle number Particle size (small, dense) HDL cholesterol Particle number Particle size (small, dense)
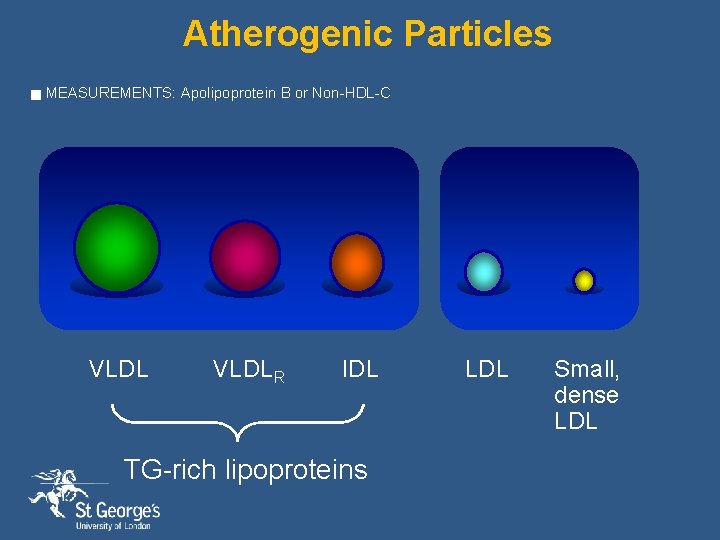
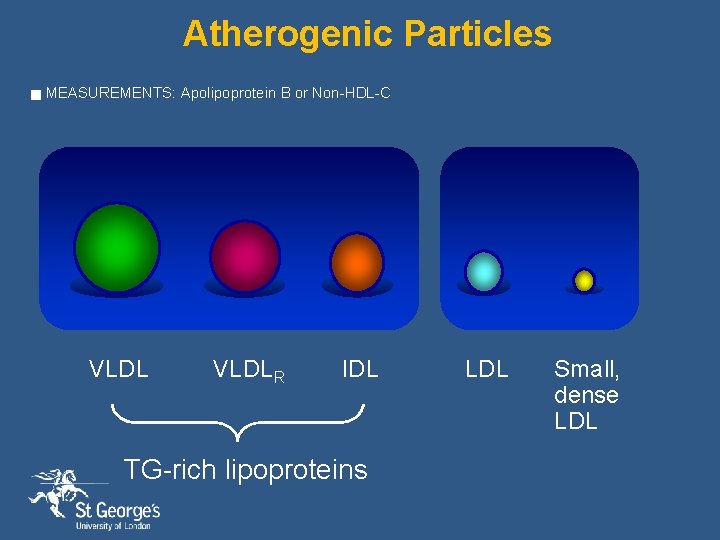
Atherogenic Particles g MEASUREMENTS: Apolipoprotein B or Non-HDL-C VLDLR IDL TG-rich lipoproteins LDL Small, dense LDL
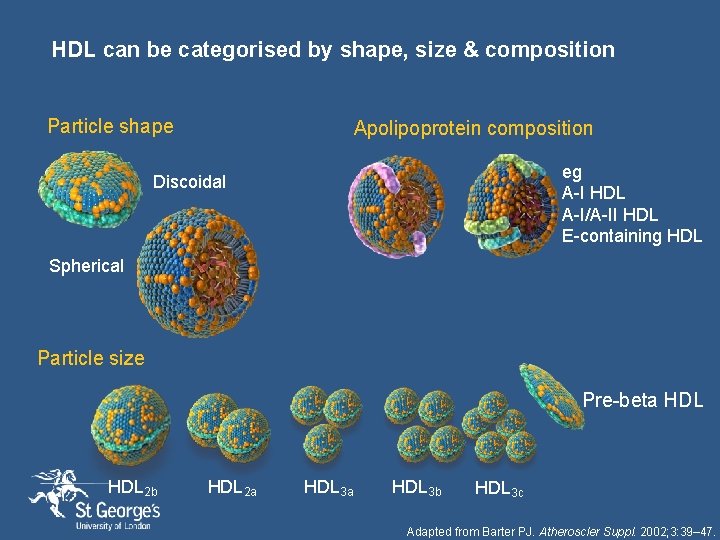
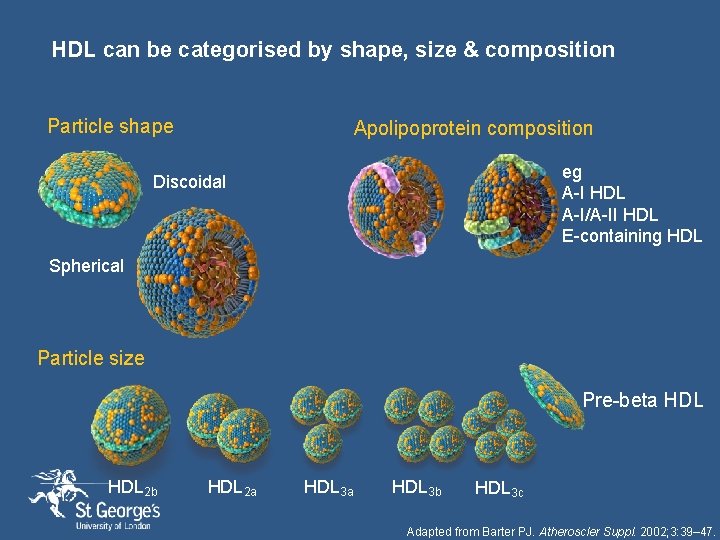
HDL can be categorised by shape, size & composition Particle shape Apolipoprotein composition eg A-I HDL A-I/A-II HDL E-containing HDL Discoidal Spherical Particle size Pre-beta HDL 2 b HDL 2 a HDL 3 b HDL 3 c Adapted from Barter PJ. Atheroscler Suppl. 2002; 3: 39– 47.
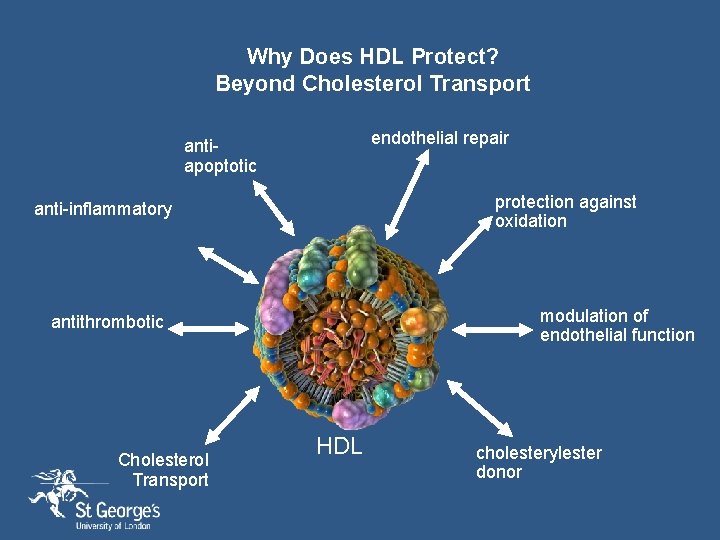
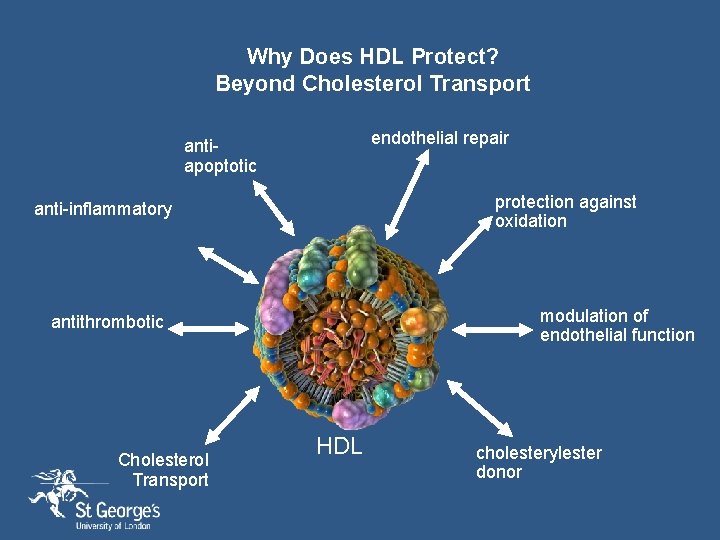
Why Does HDL Protect? Beyond Cholesterol Transport endothelial repair antiapoptotic protection against oxidation anti-inflammatory modulation of endothelial function antithrombotic Cholesterol Transport HDL cholesterylester donor

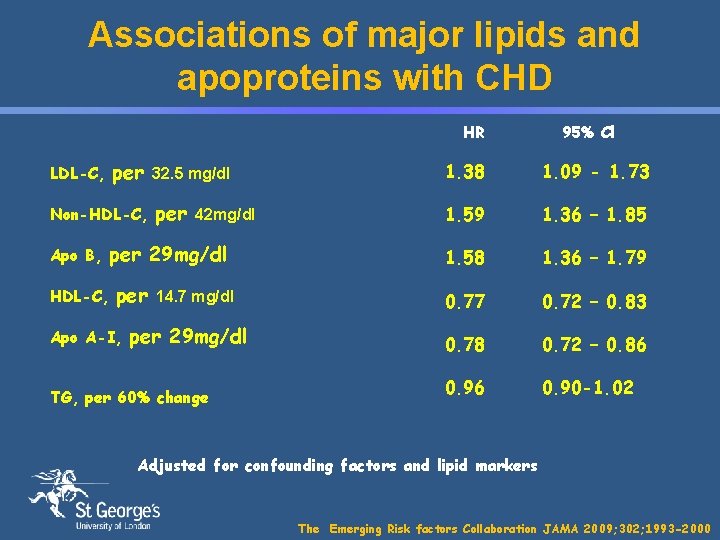
What is the best measure of atherogenic risk LDL-C, Non-HDLC or apo B
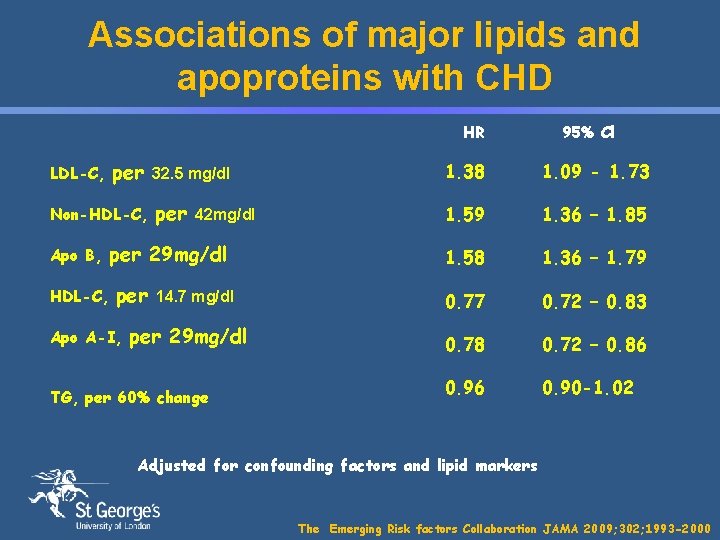
Associations of major lipids and apoproteins with CHD HR LDL-C, per Non-HDL-C, Apo B, HDL-C, 32. 5 mg/dl 1. 38 1. 09 - 1. 73 per 1. 59 1. 36 – 1. 85 1. 58 1. 36 – 1. 79 0. 77 0. 72 – 0. 83 0. 78 0. 72 – 0. 86 0. 90 -1. 02 42 mg/dl per 29 mg/dl per Apo A-I, 95% Cl 14. 7 mg/dl per 29 mg/dl TG, per 60% change Adjusted for confounding factors and lipid markers The Emerging Risk factors Collaboration JAMA 2009; 302; 1993 -2000
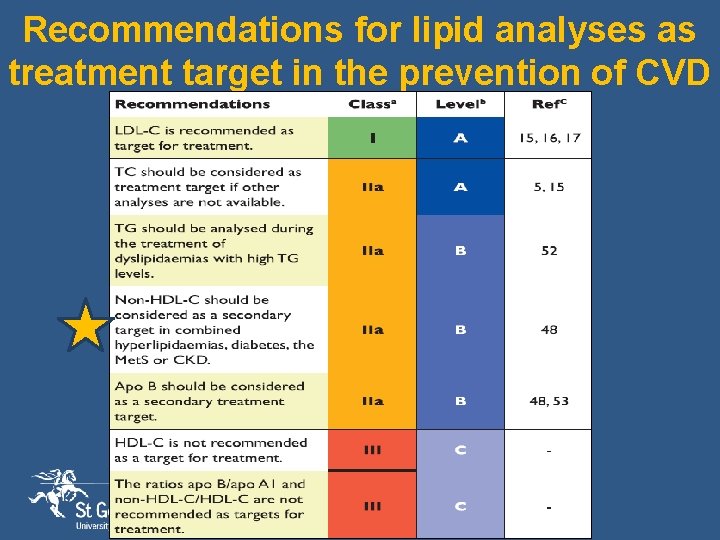
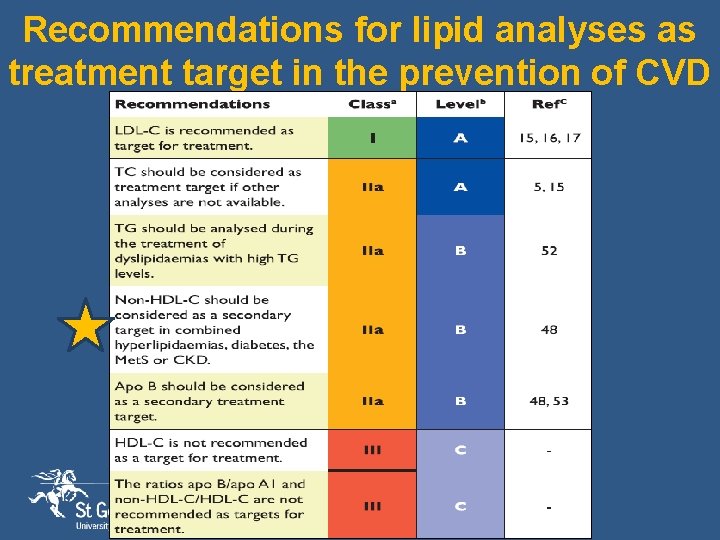
Recommendations for lipid analyses as treatment target in the prevention of CVD

STATINS VARY IN CHEMICAL STRUCTURES Simvastatin Pravastatin Atorvastatin • Ose L Clin Lipidol 2010; 5(3): 309– 323. Fluvastatin Ca 2+ 2 2 Pitavastatin Rosuvastatin
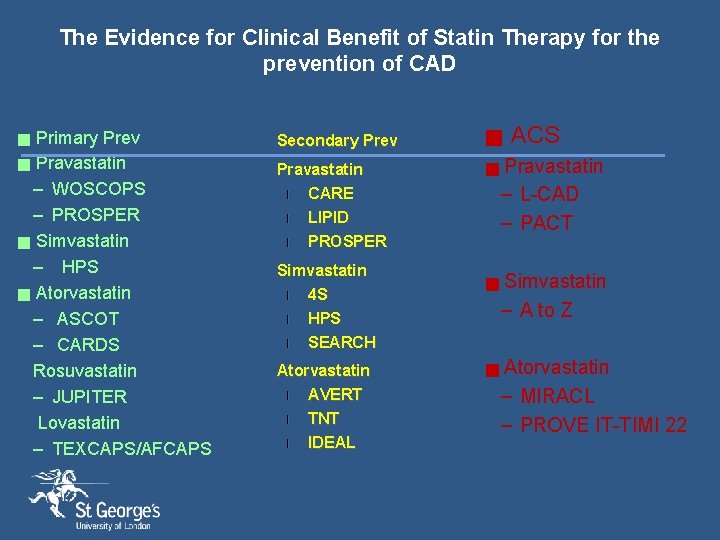
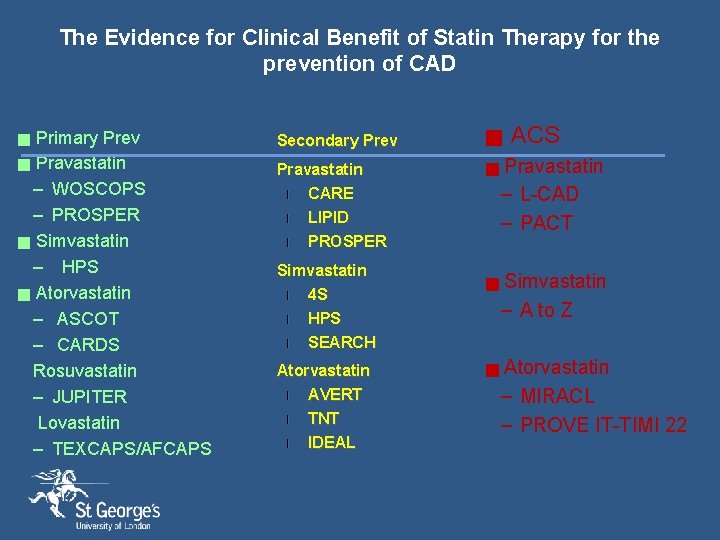
The Evidence for Clinical Benefit of Statin Therapy for the prevention of CAD Primary Prev g Pravastatin – WOSCOPS – PROSPER g Simvastatin – HPS g Atorvastatin – ASCOT – CARDS Rosuvastatin – JUPITER Lovastatin – TEXCAPS/AFCAPS g Secondary Prev g Pravastatin l CARE g l l LIPID PROSPER Simvastatin l 4 S l HPS l SEARCH Atorvastatin l AVERT l TNT l IDEAL g g ACS Pravastatin – L-CAD – PACT Simvastatin – A to Z Atorvastatin – MIRACL – PROVE IT-TIMI 22
How low should we go with LDL-C lowering
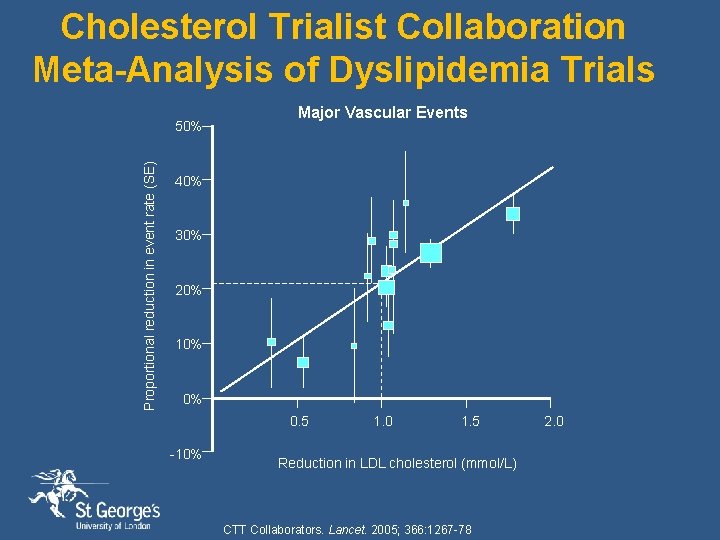
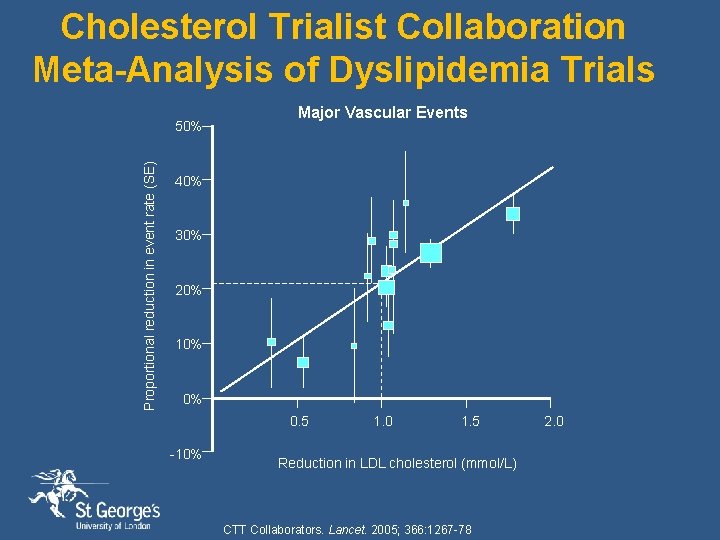
Cholesterol Trialist Collaboration Meta-Analysis of Dyslipidemia Trials Proportional reduction in event rate (SE) 50% Major Vascular Events 40% 30% 20% 10% 0% 0. 5 -10% 1. 0 1. 5 Reduction in LDL cholesterol (mmol/L) CTT Collaborators. Lancet. 2005; 366: 1267 -78 2. 0

CTT Collaboration Effects on Major Coronary Events per mmol/L LDL Cholesterol Reduction Subdivided by Baseline Lipid Values Groups (mmol/L) Events (%) Treatment Control Heterogeneity/trend RR & CI (Treatment : Control) p-value Total cholesterol: ≤ 5. 2 -6. 5 >6. 5 748 (6· 9) 1678 (7· 0) 896 (8· 8) 940 (8· 6) 2246 (9· 4) 1220 (12· 1) LDL cholesterol: ≤ 3. 5 -4. 5 >4. 5 1130 (6· 8) 1374 (7· 3) 801 (9· 3) 1443 (8· 7) 1814 (9· 6) 1120 (12· 9) p = 0· 5 HDL cholesterol: ≤ 0. 9 -1. 1 >1. 1 1167 (9· 3) 939 (7· 4) 1207 (6· 2) 1538 (12· 1) 1270 (10· 2) 1595 (8· 1) p = 0· 8 Triglycerides: ≤ 1. 4 -2. 0 >2. 0 1162 (7· 3) 937 (7· 1) 1217 (7· 9) 1521 (9· 6) 1304 (9· 8) 1564 (10· 2) p = 0· 6 Overall 3337 (7· 4) 4420 (9· 8) p = 0· 77 (0· 74 – 0· 80) p < 0· 00001 1· 5 v 23% risk reduction per 39 mg/dl lowering of 0· 5 LDL-C 1· 0 - irrespective of Treatment Control base line lipid levels better v Starting statin therpay early in patients proves beneficial CTT Collaborators. Lancet. 2005; 366: 1267 -78
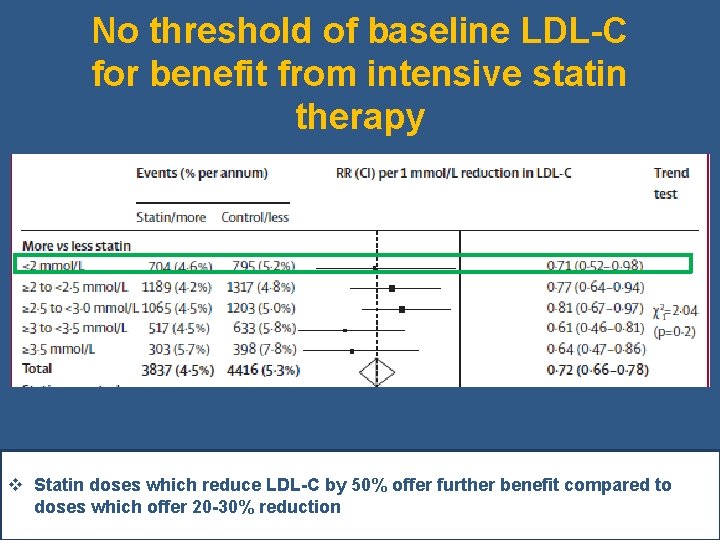
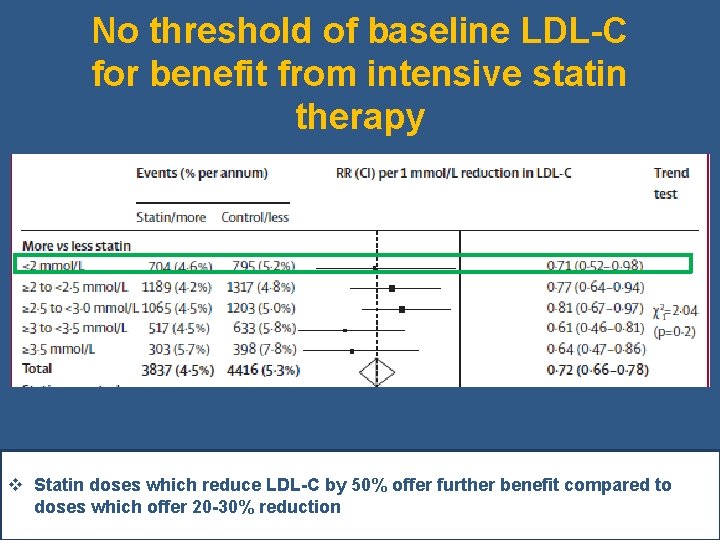
No threshold of baseline LDL-C for benefit from intensive statin therapy v Statin doses which reduce LDL-C by 50% offer further benefit compared to doses which offer 20 -30% reduction CTT 2 – Lancet 2010
Recent Guidelines
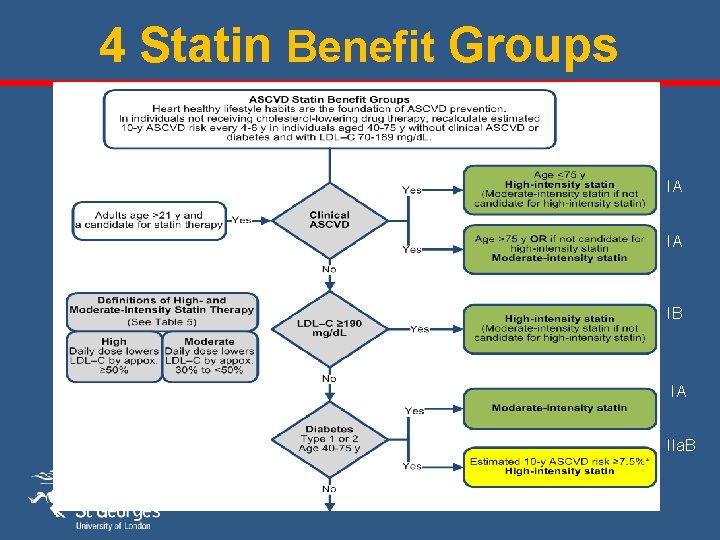
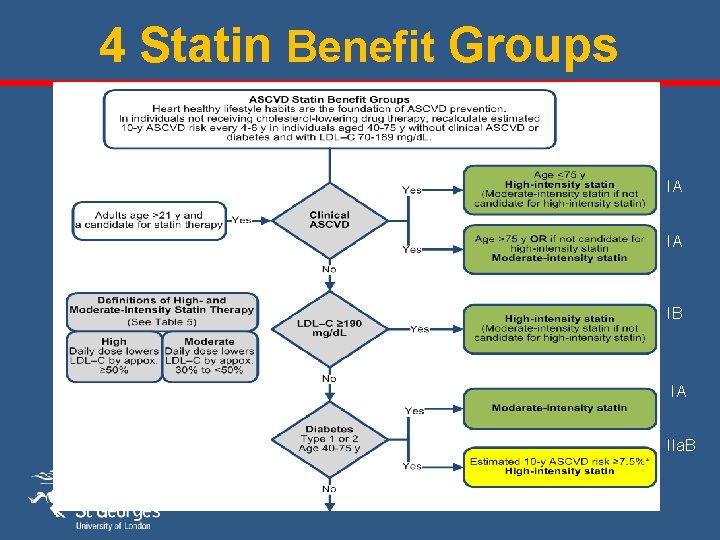
4 Statin Benefit Groups IA IA IB IA IIa. B
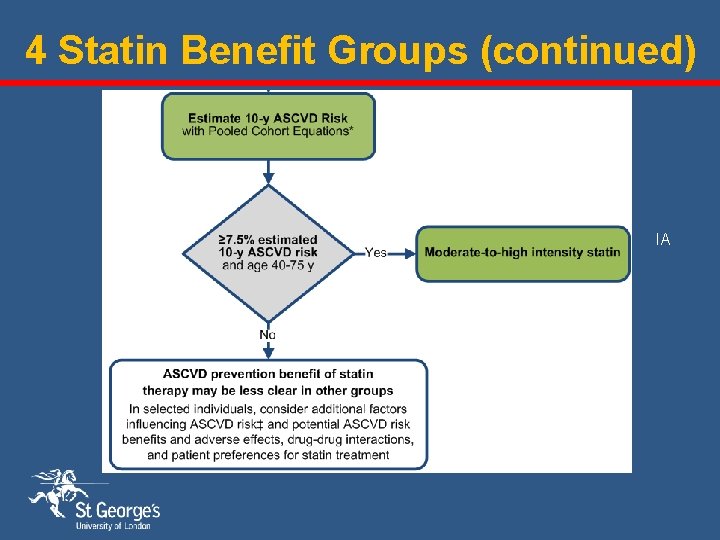
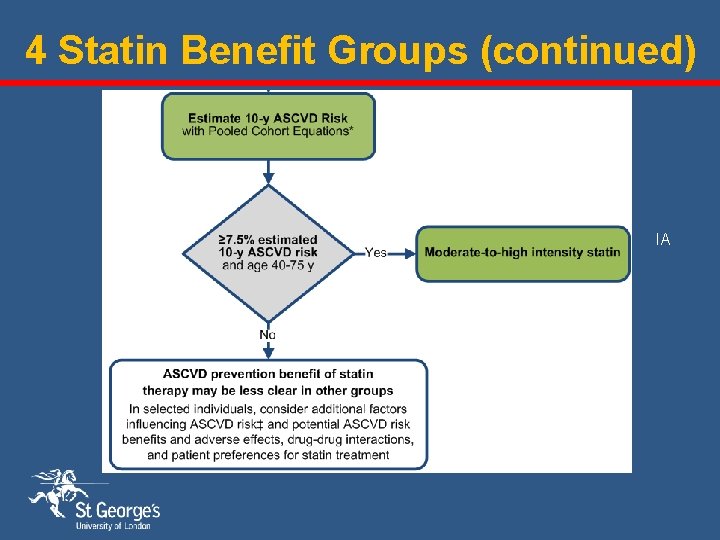
4 Statin Benefit Groups (continued) IA IA *10 -year ASCVD Risk Calculator online

2013 ACC/AHA Essentially recommend either high intensity or moderate intensity statin treatment. High intensity statin treatment reduces LDL-C by around 50% (Atorvastatin 40 or 80 mg, Rosuvastatin 20/40 mg) Moderate intensity statin treatment reduces LDL-c by 30 -50% (Atorvastatin 10 mg, Simvastatin 20 or 40 mg, Pravastatin 40 mg, Fluvastatin 40 mg bd, Rosuvastatin 5 and 10 mg) Considered risk reduction with either high or moderate intensity statin regimes with estimates of adverse events ▪ new onset DM (0. 1/100 patient years with moderate intensity and 0. 3/100 patient years with high intensity) ▪ myopathy ▪ haemorrhagic stroke No evidence of statin benefit if NYHA Class II-IV heart failure, or if on haemodialysis.

2011 ESC/EAS Treatment Targets Primary target: on treatment LDL-c Very high risk LDL-c < 70 MG/d. L and or 50% ↓ in LDL-c when target level cannot be reached (Class I, Level A) High risk LDL-c < 100 mg/d. L should be considered (Class IIa, Level A) Moderate risk LDL-c < 130 mg/d. L should be considered (Class IIa, Level C) Secondary targets: non-HDL-c Very high risk High risk < 100 mg/d. L < 140 mg/d. L Apo B-100 Very high risk High risk < 80 mg/d. L < 100 mg/d. L

Do statins work in low risk primary prevention ?
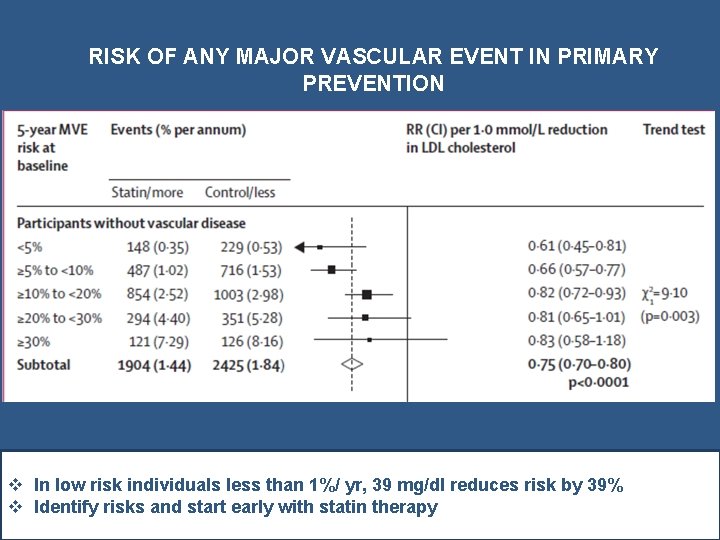
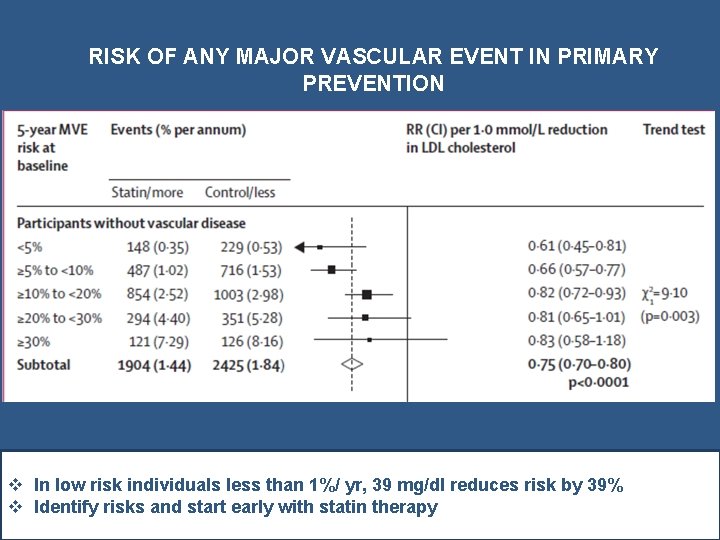
RISK OF ANY MAJOR VASCULAR EVENT IN PRIMARY PREVENTION v In low risk individuals less than 1%/ yr, 39 mg/dl reduces risk by 39% v Identify risks and start early with statin therapy CTT Lancet 2012

Early Initiation
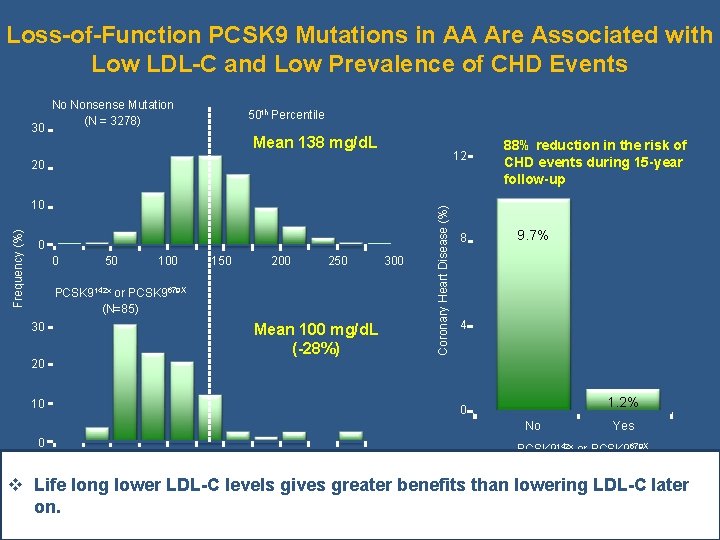
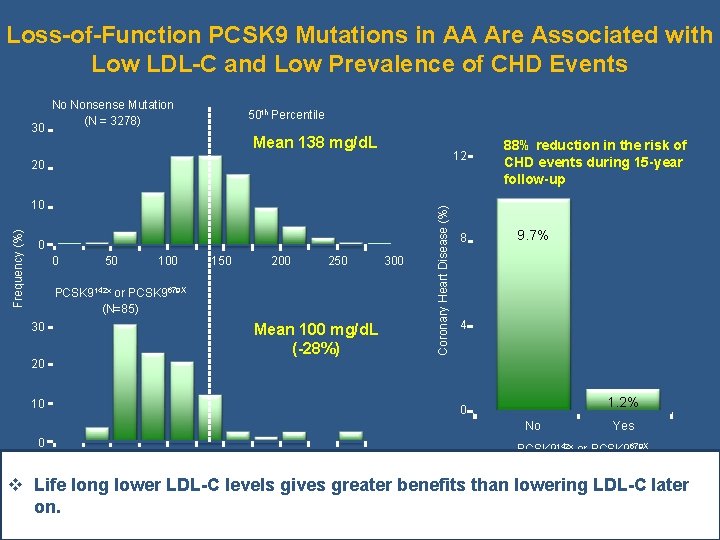
Loss-of-Function PCSK 9 Mutations in AA Are Associated with Low LDL-C and Low Prevalence of CHD Events 30 No Nonsense Mutation (N = 3278) 50 th Percentile Mean 138 mg/d. L 12 Frequency (%) 10 0 0 50 100 150 200 250 300 PCSK 9142 x or PCSK 9679 X (N=85) 30 Mean 100 mg/d. L (-28%) Coronary Heart Disease (%) 20 8 88% reduction in the risk of CHD events during 15 -year follow-up 9. 7% 4 20 10 1. 2% 0 No 0 0 50 100 150 200 250 Plasma LDL Cholesterol in Black Subjects (mg/d. L) 300 Yes PCSK 9142 x or PCSK 9679 X v Life long lower LDL-C levels gives greater benefits than lowering LDL-C later Adapted from Cohen JC. N Engl J Med 2006; 354: 1264 -72 ARIC=Atherosclerosis Risk in the Community on.
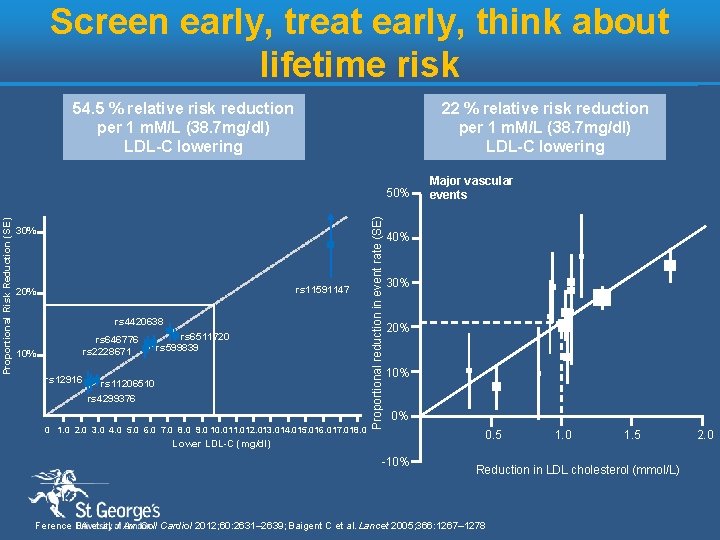
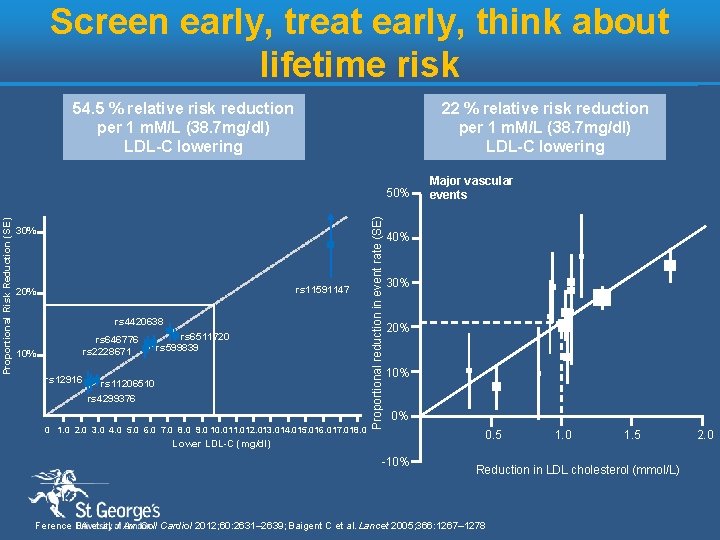
Screen early, treat early, think about lifetime risk 54. 5 % relative risk reduction per 1 m. M/L (38. 7 mg/dl) LDL-C lowering 22 % relative risk reduction per 1 m. M/L (38. 7 mg/dl) LDL-C lowering 30% rs 11591147 20% rs 4420638 rs 646776 rs 2228671 10% rs 12916 rs 6511720 rs 599839 rs 11206510 rs 4299376 0 1. 0 2. 0 3. 0 4. 0 5. 0 6. 0 7. 0 8. 0 9. 0 10. 011. 012. 013. 014. 015. 016. 017. 018. 0 Proportional reduction in event rate (SE) Proportional Risk Reduction (SE) 50% Major vascular events 40% 30% 20% 10% 0% Lower LDL-C (mg/dl) -10% 0. 5 1. 0 1. 5 Reduction in LDL cholesterol (mmol/L) Ference BA et al. J Am Coll Cardiol 2012; 60: 2631– 2639; Baigent C et al. Lancet 2005; 366: 1267– 1278 2. 0

Safety
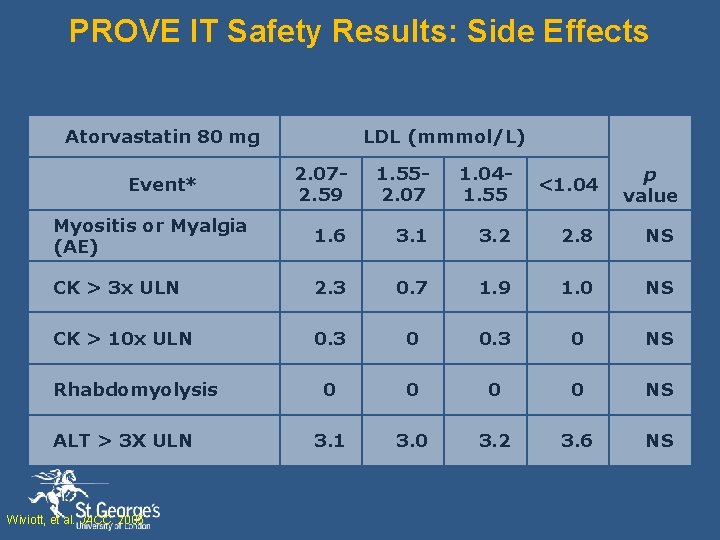
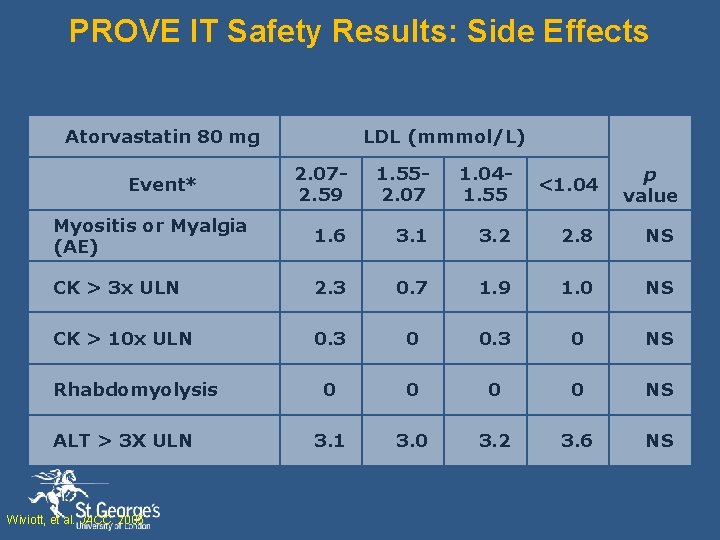
PROVE IT Safety Results: Side Effects Atorvastatin 80 mg LDL (mmmol/L) 2. 072. 59 1. 552. 07 1. 041. 55 <1. 04 p value Myositis or Myalgia (AE) 1. 6 3. 1 3. 2 2. 8 NS CK > 3 x ULN 2. 3 0. 7 1. 9 1. 0 NS CK > 10 x ULN 0. 3 0 NS 0 0 NS 3. 1 3. 0 3. 2 3. 6 NS Event* Rhabdomyolysis ALT > 3 X ULN Wiviott, et al. JACC. 2005
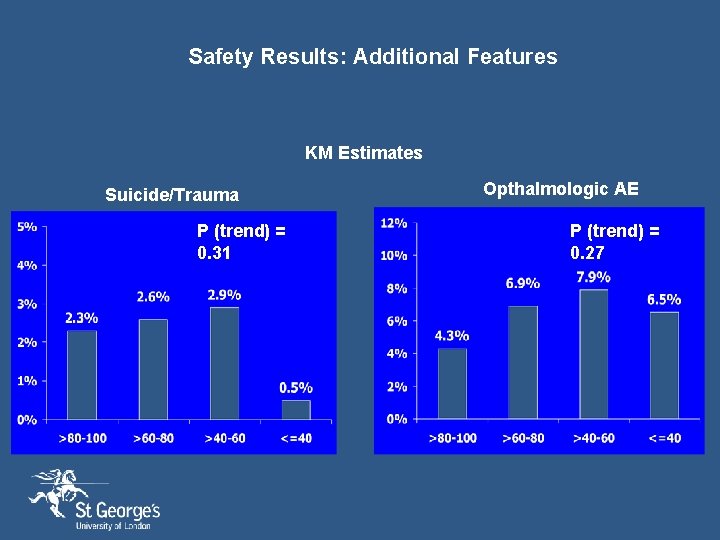
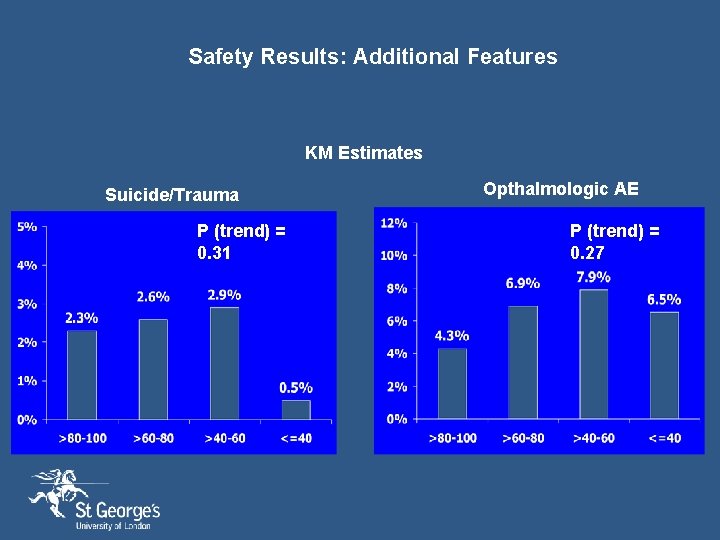
Safety Results: Additional Features KM Estimates Suicide/Trauma P (trend) = 0. 31 Opthalmologic AE P (trend) = 0. 27

Relative Risk of Onset of Cancer from the Cholesterol Treatment Trialists' (CTT) Meta. Analysis of Statin Trials, According to Year of Onset Peto R et al. N Engl J Med 2008; 359: 1357 -1366
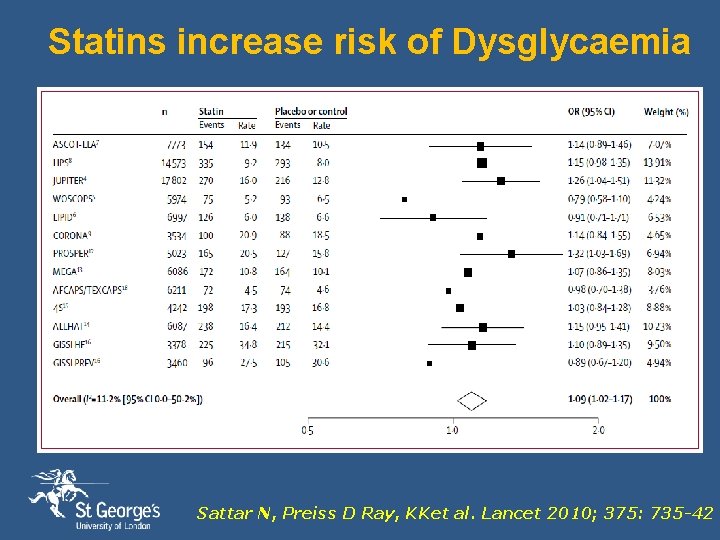
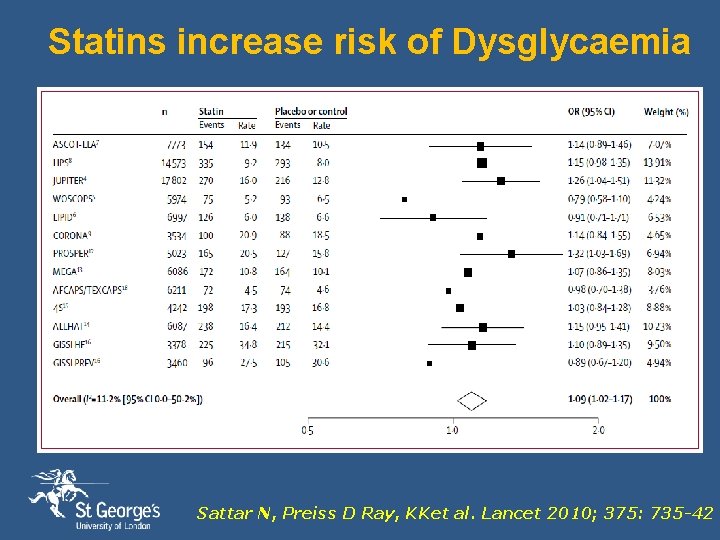
Statins increase risk of Dysglycaemia Sattar N, Preiss D Ray, KKet al. Lancet 2010; 375: 735 -42
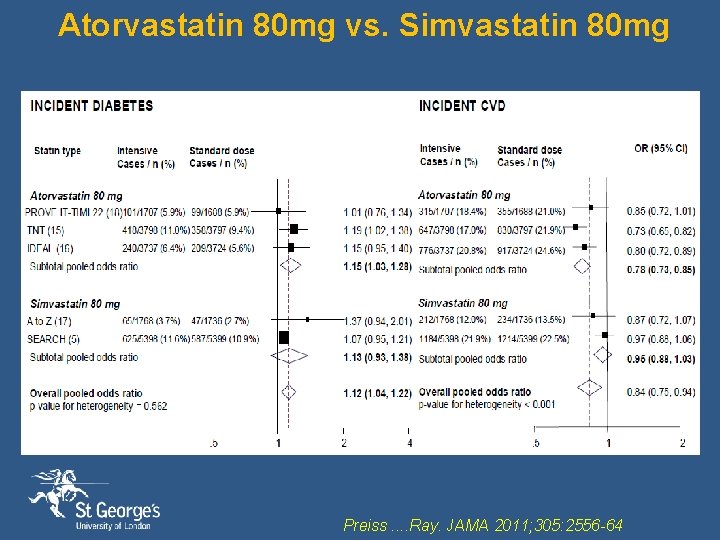
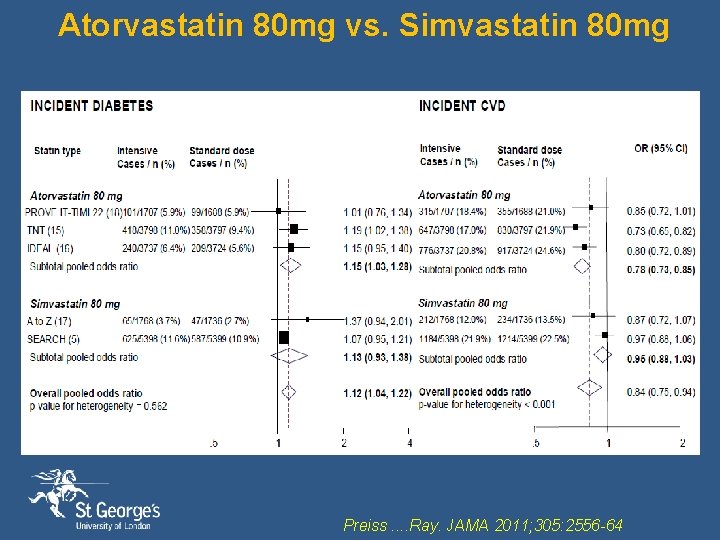
Atorvastatin 80 mg vs. Simvastatin 80 mg Preiss. . Ray. JAMA 2011; 305: 2556 -64
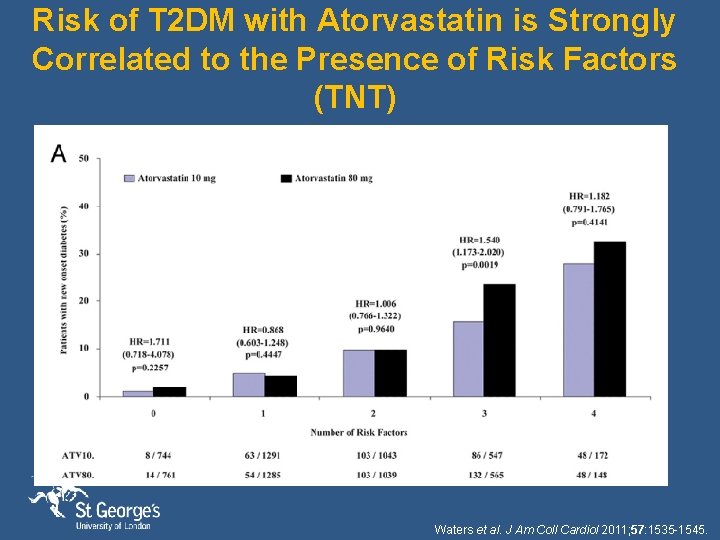
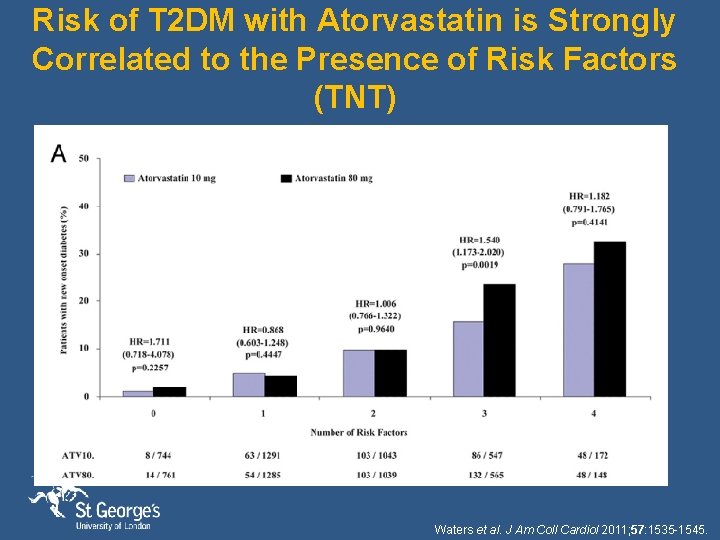
Risk of T 2 DM with Atorvastatin is Strongly Correlated to the Presence of Risk Factors (TNT) Waters et al. J Am Coll Cardiol 2011; 57: 1535 -1545.
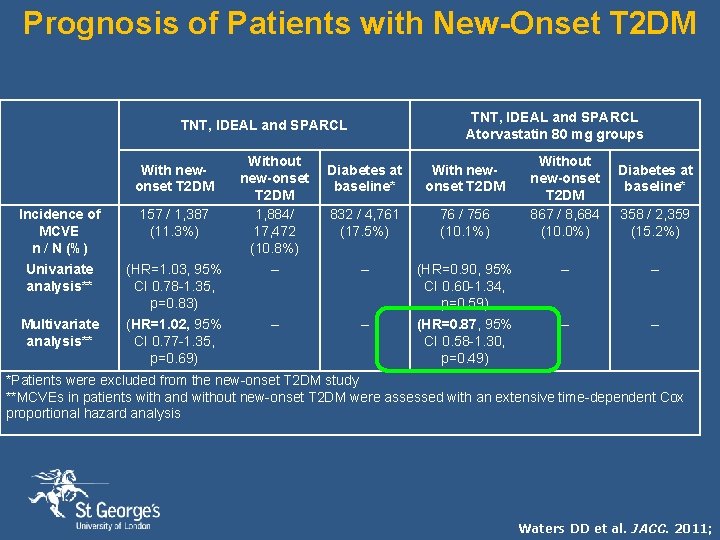
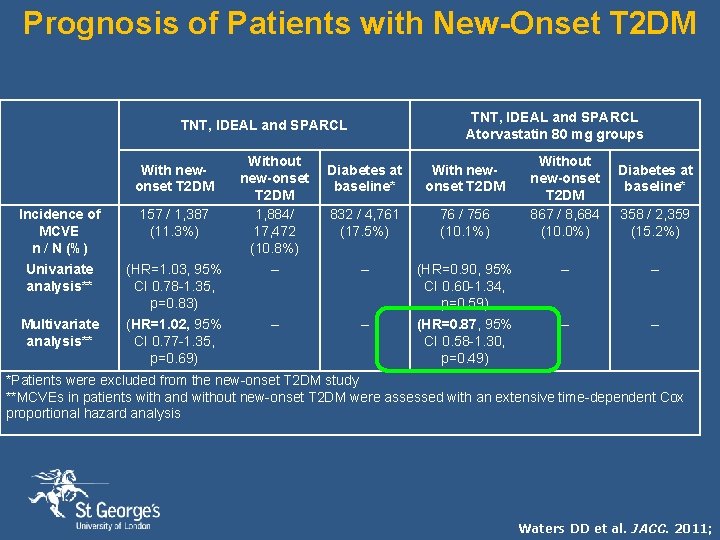
Prognosis of Patients with New-Onset T 2 DM TNT, IDEAL and SPARCL Atorvastatin 80 mg groups TNT, IDEAL and SPARCL With newonset T 2 DM Without new-onset T 2 DM 1, 884/ 17, 472 (10. 8%) Diabetes at baseline* With newonset T 2 DM 832 / 4, 761 (17. 5%) 76 / 756 (10. 1%) Without new-onset T 2 DM 867 / 8, 684 (10. 0%) Diabetes at baseline* Incidence of MCVE n / N (%) 157 / 1, 387 (11. 3%) 358 / 2, 359 (15. 2%) Univariate analysis** (HR=1. 03, 95% CI 0. 78 -1. 35, p=0. 83) – – (HR=0. 90, 95% CI 0. 60 -1. 34, p=0. 59) – – Multivariate analysis** (HR=1. 02, 95% CI 0. 77 -1. 35, p=0. 69) – – (HR=0. 87, 95% CI 0. 58 -1. 30, p=0. 49) – – *Patients were excluded from the new-onset T 2 DM study **MCVEs in patients with and without new-onset T 2 DM were assessed with an extensive time-dependent Cox proportional hazard analysis Waters DD et al. JACC. 2011;
Residual Risk

Absolute risk of cardiovascular disease over 5 years in patients by systolic blood pressure at specified levels of other risk factors 44% Incremental Risk Diabetic, Smoker, Male, 60 yrs, TC : 240 mg/dl and HDL: 40 MG/DL 33% Reference 24% Non Diabetic, Non Smoker, female, 50 yrs, TC : 160 MG/dl and HDL: 60 MG/DL 18% 12% 3% 6%
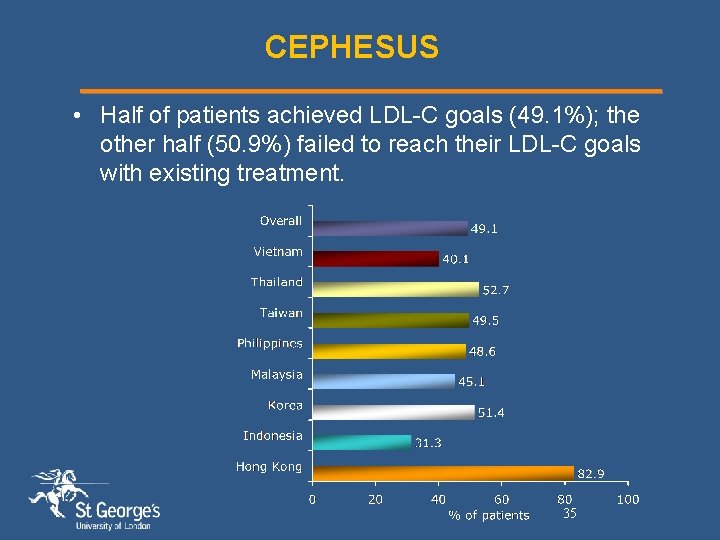
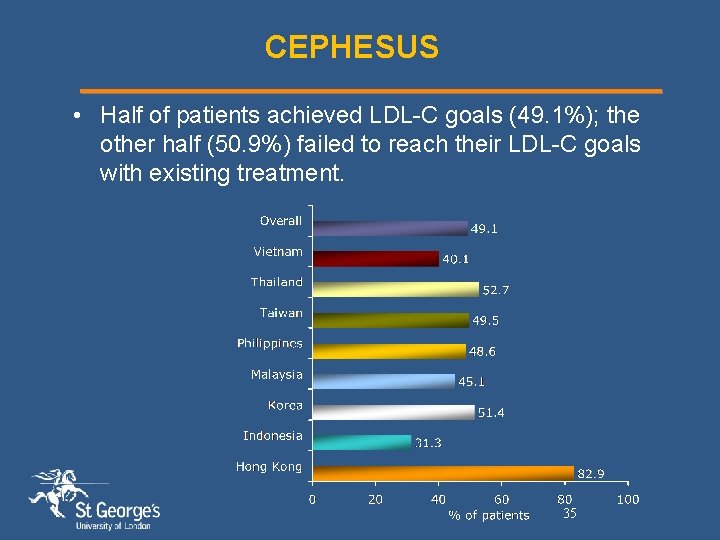
CEPHESUS • Half of patients achieved LDL-C goals (49. 1%); the other half (50. 9%) failed to reach their LDL-C goals with existing treatment. 35
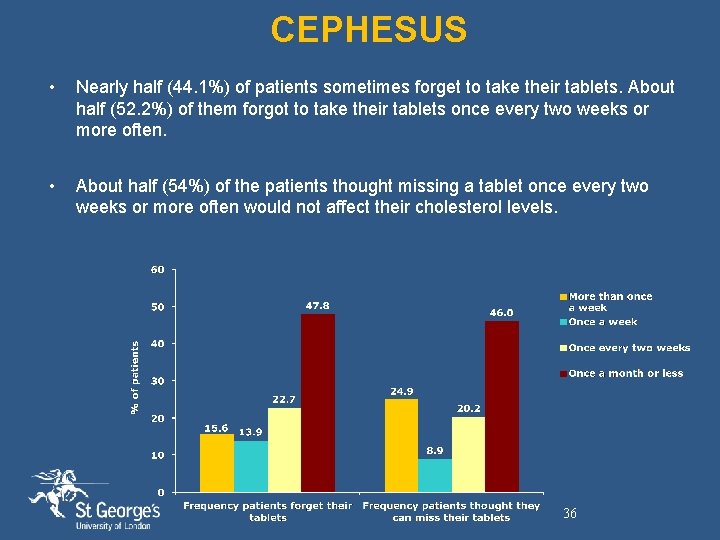
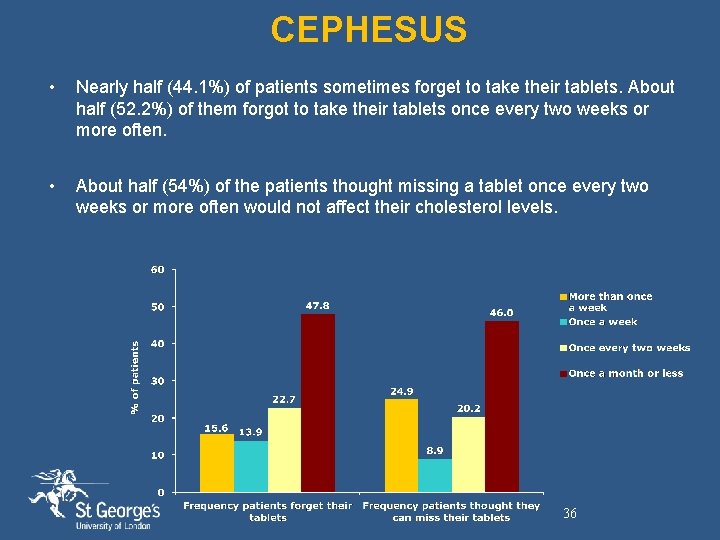
CEPHESUS • Nearly half (44. 1%) of patients sometimes forget to take their tablets. About half (52. 2%) of them forgot to take their tablets once every two weeks or more often. • About half (54%) of the patients thought missing a tablet once every two weeks or more often would not affect their cholesterol levels. 36
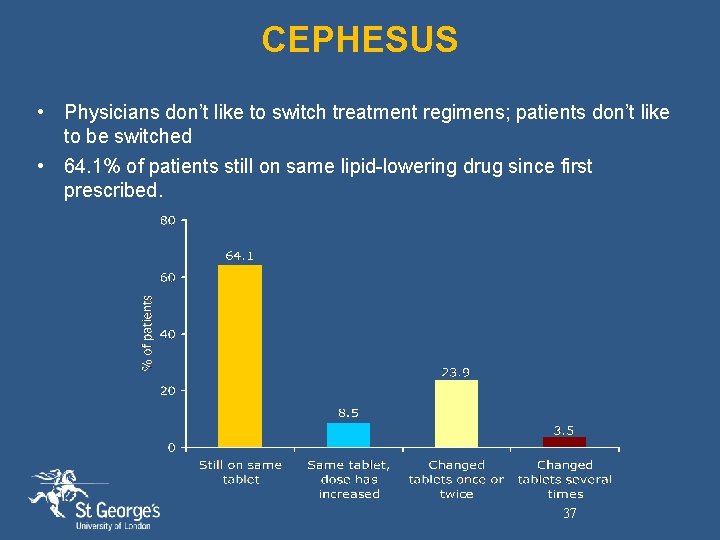
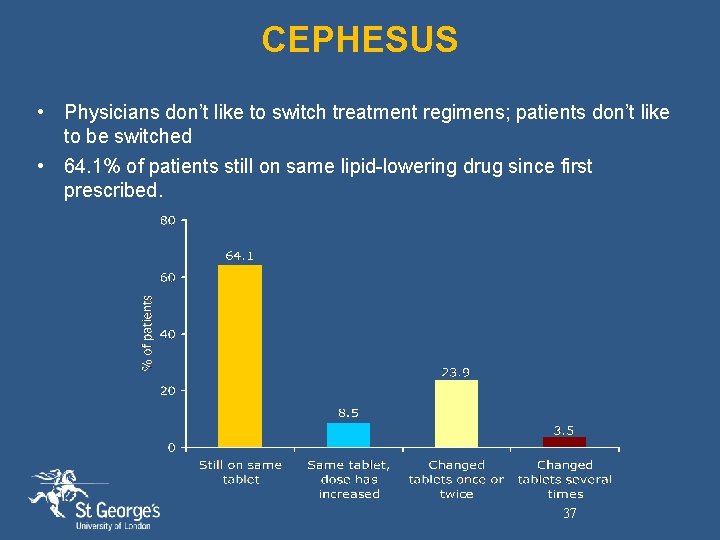
CEPHESUS • Physicians don’t like to switch treatment regimens; patients don’t like to be switched • 64. 1% of patients still on same lipid-lowering drug since first prescribed. 37
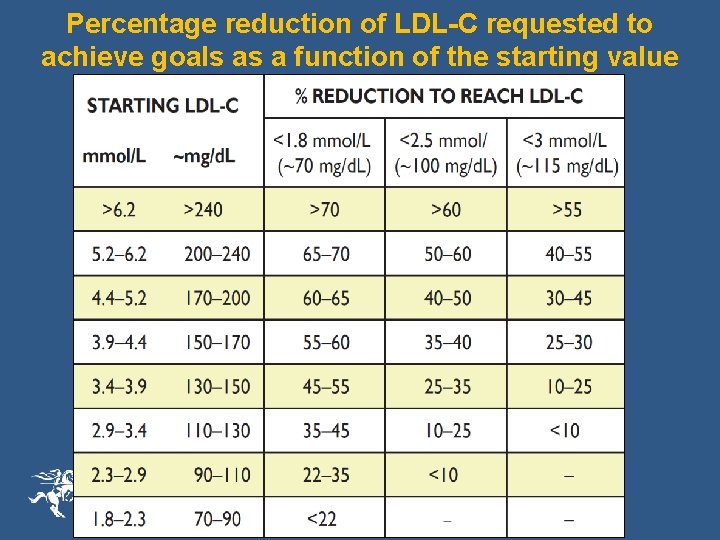
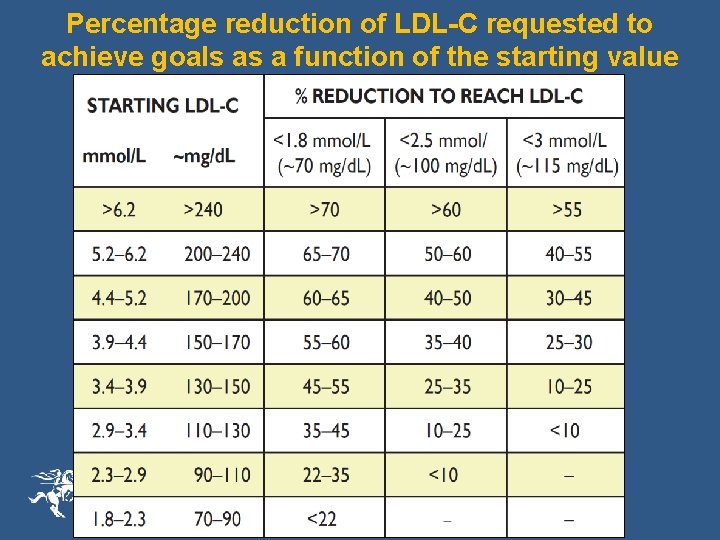
Percentage reduction of LDL-C requested to achieve goals as a function of the starting value
Atheroma Progression
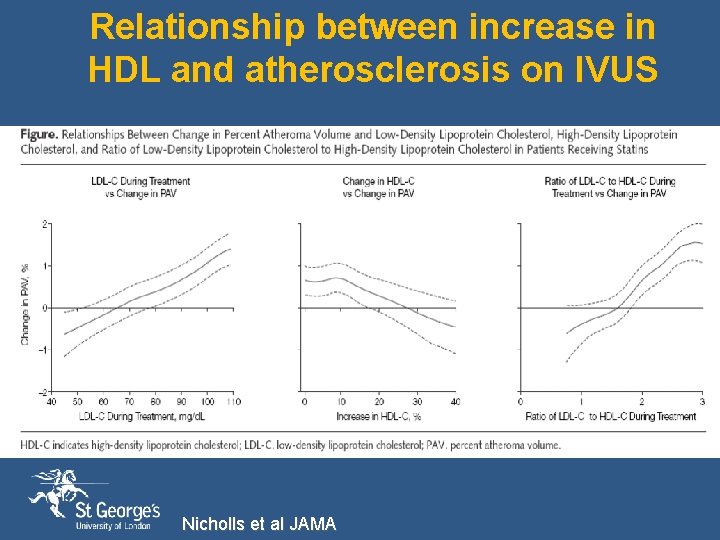
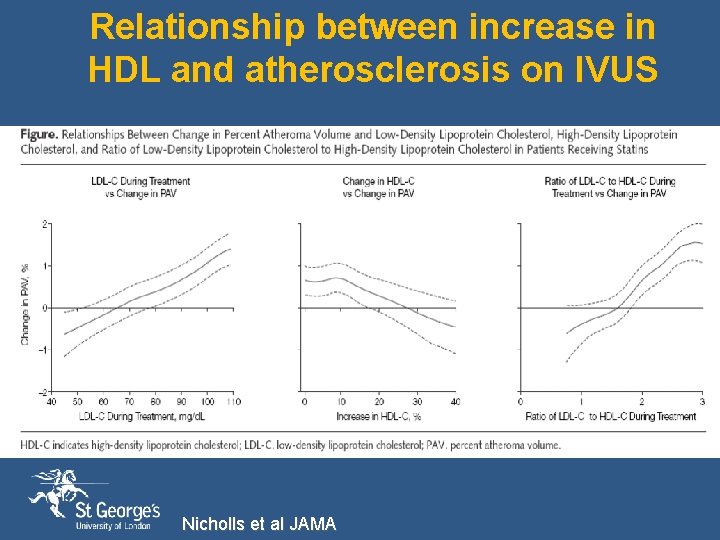
Relationship between increase in HDL and atherosclerosis on IVUS Nicholls et al JAMA
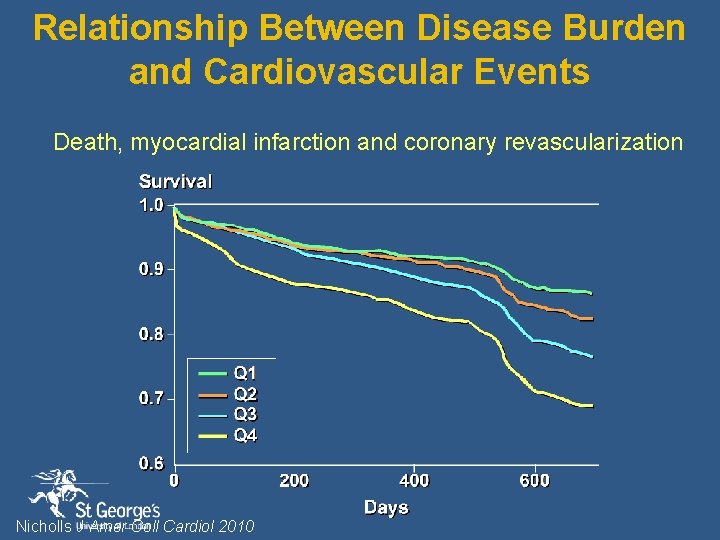
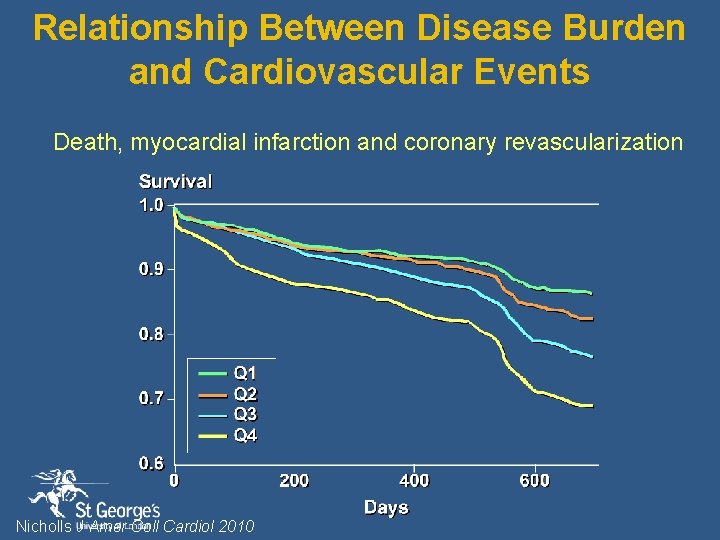
Relationship Between Disease Burden and Cardiovascular Events Death, myocardial infarction and coronary revascularization Nicholls J Amer Coll Cardiol 2010

Summary § ESC guidelines identify 5 groups for CVD, DM, FH, high global risk § LDL-C targets depend on hisk with lower targets for those at highest risk § Statins are safe and currently the most effective treatments and pitavastatin has an excellent profile on LDL-C and HDL-C § Statins as a class seam to raise blood glucose in some but the benefits outweigh the risks. Pitavastatin may be the most glucose “gentle” in that regard