Update from education committee Train the trainercontent reviewed

- Slides: 15
Update from education committee • Train the trainer—content reviewed from Extended Time Window for Acute Stroke Intervention “First Tuesdays” Lecture Series
Introduction and Goal of “First Tuesdays” • Sabreena Slavin MD – Vascular Neurologist and Neurohospitalist at KU School of Medicine • Craig Bloom RN, BSN, MBA – Senior Clinical Specialist Lytics, Genentech, Inc. • Didactic lecture series as part of the Kansas Initiative for Stroke Survival • Updates in Practice and FAQ’s on Acute Stroke Care • 20 minute didactic, 10 minutes for questions/discussion.
Review of Acute Stroke Interventions • IV alteplase (t. PA) for all patients who have disabling symptoms of acute stroke • Mechanical thrombectomy: only for large vessel occlusions (LVO). Only hospitals with capabilities (eg: comprehensive stroke center) can perform thrombectomy. – A higher NIHSS (10 or more) can be indicative of a large vessel occlusion. – Diagnosed with CTA head/neck
Extended Time Window • Time limit for IV t. PA: 4. 5 hours from last known normal. This is unchanged. • Time limit for mechanical thrombectomy: Previously was up to 6 hours from last known normal. Now can take up to 24 hours from last known normal. This is a new change in recommendation based on recent studies.
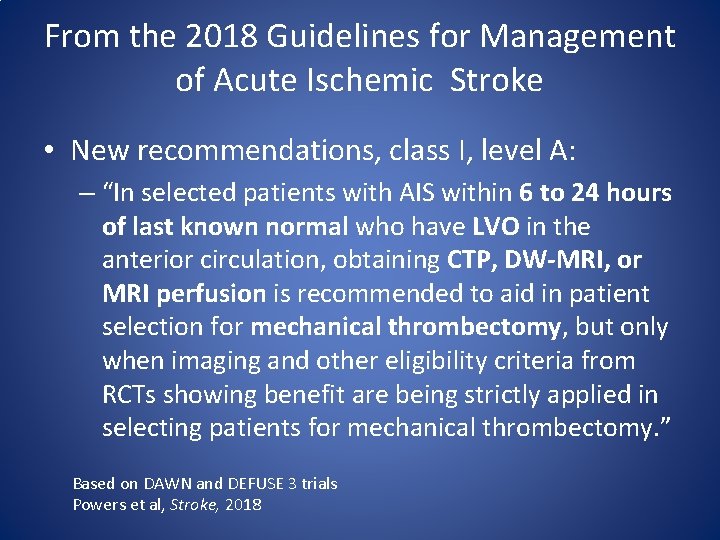
From the 2018 Guidelines for Management of Acute Ischemic Stroke • New recommendations, class I, level A: – “In selected patients with AIS within 6 to 24 hours of last known normal who have LVO in the anterior circulation, obtaining CTP, DW-MRI, or MRI perfusion is recommended to aid in patient selection for mechanical thrombectomy, but only when imaging and other eligibility criteria from RCTs showing benefit are being strictly applied in selecting patients for mechanical thrombectomy. ” Based on DAWN and DEFUSE 3 trials Powers et al, Stroke, 2018

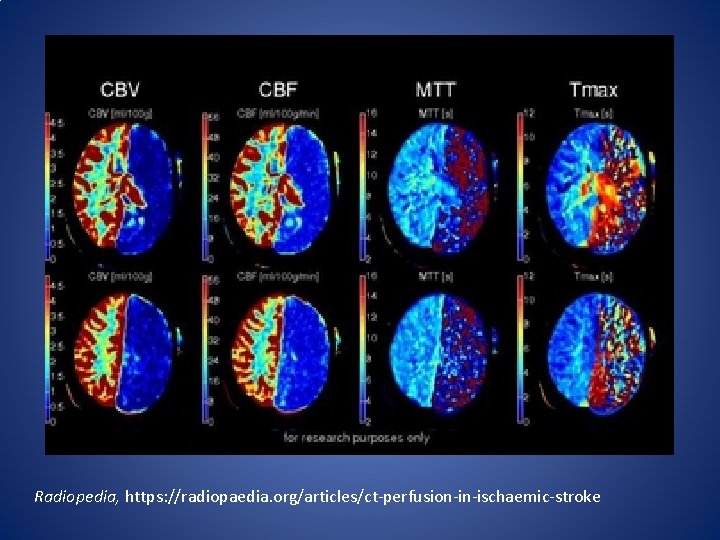
Perfusion Imaging • CT perfusion and MR perfusion imaging is used to find a mismatch between ischemic core (area already damaged) and ischemic penumbra (area at risk of damage). • Measures of core: cerebral blood volume, cerebral blood flow • Measures of penumbra: mean transit time (ratio cerebral blood flow/cerebral blood volume), time to peak, time to drain, and Tmax (measures of contrast arrival time to tissue).
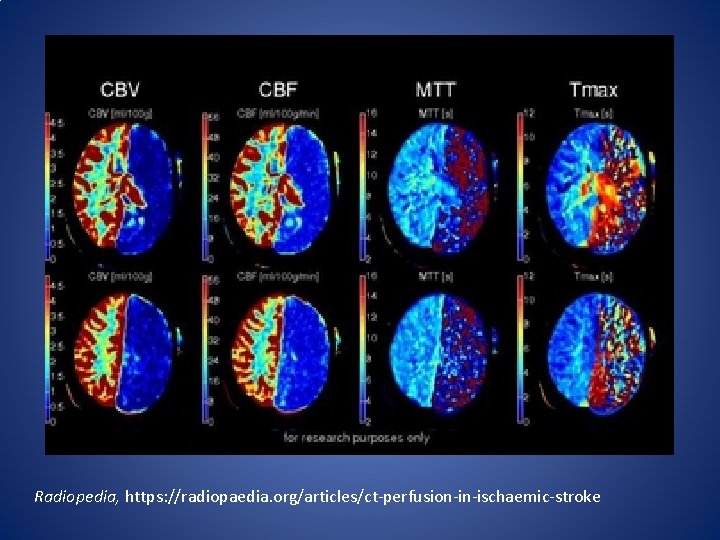
Radiopedia, https: //radiopaedia. org/articles/ct-perfusion-in-ischaemic-stroke
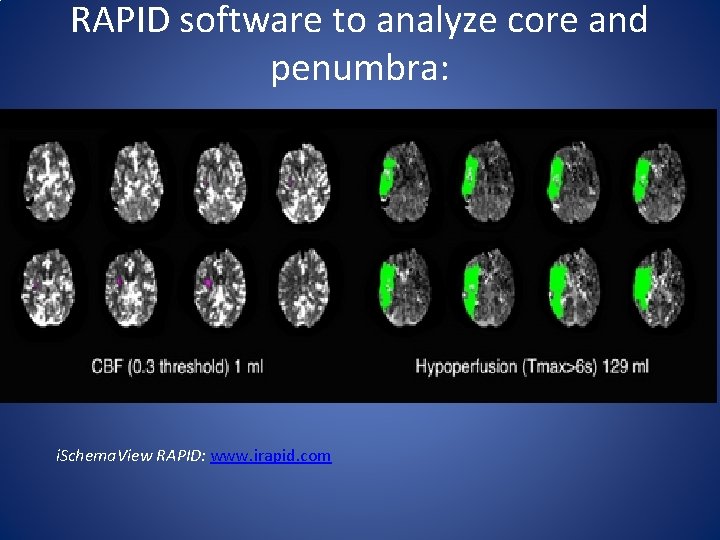
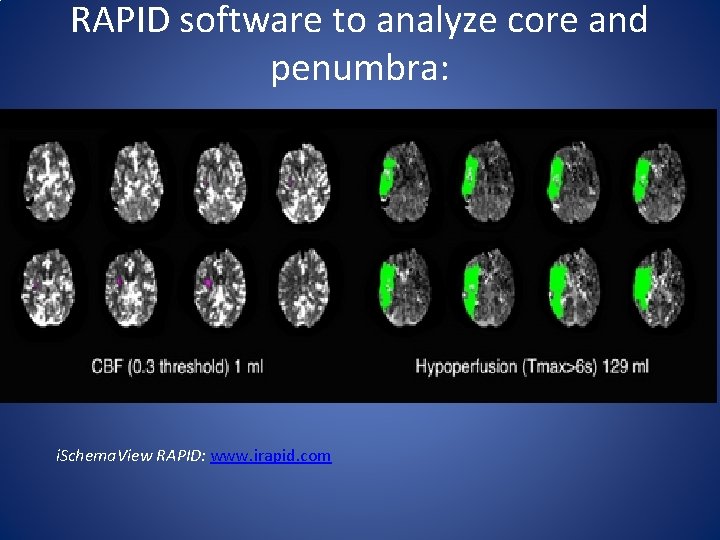
RAPID software to analyze core and penumbra: i. Schema. View RAPID: www. irapid. com
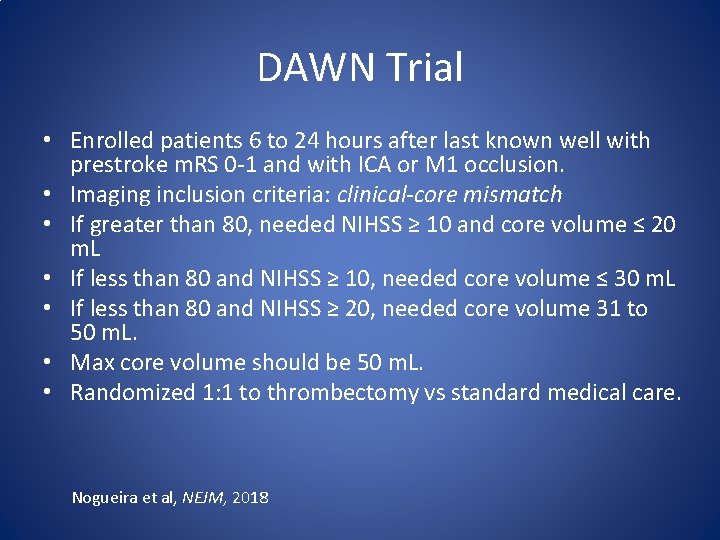
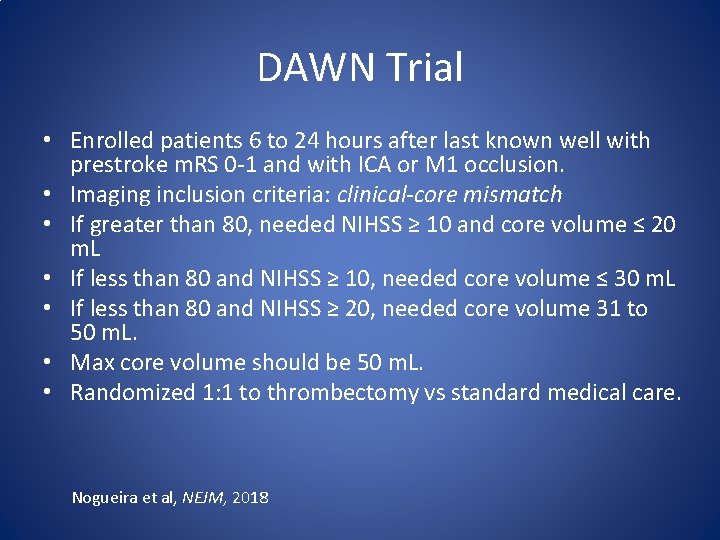
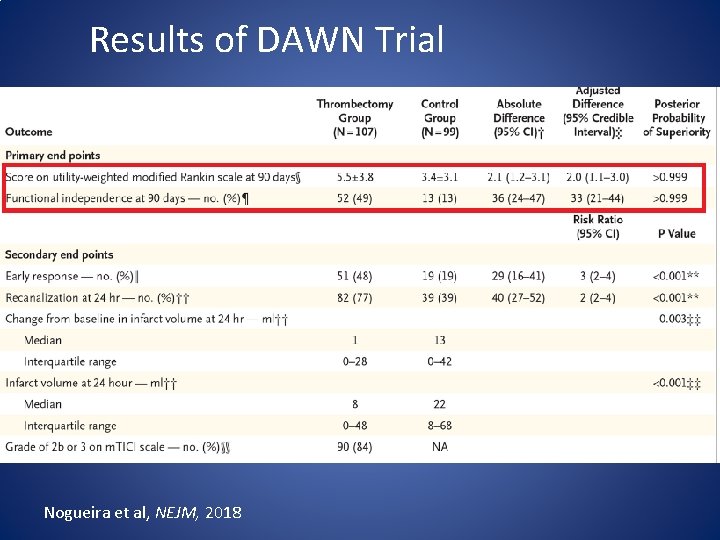
DAWN Trial • Enrolled patients 6 to 24 hours after last known well with prestroke m. RS 0 -1 and with ICA or M 1 occlusion. • Imaging inclusion criteria: clinical-core mismatch • If greater than 80, needed NIHSS ≥ 10 and core volume ≤ 20 m. L • If less than 80 and NIHSS ≥ 10, needed core volume ≤ 30 m. L • If less than 80 and NIHSS ≥ 20, needed core volume 31 to 50 m. L. • Max core volume should be 50 m. L. • Randomized 1: 1 to thrombectomy vs standard medical care. Nogueira et al, NEJM, 2018
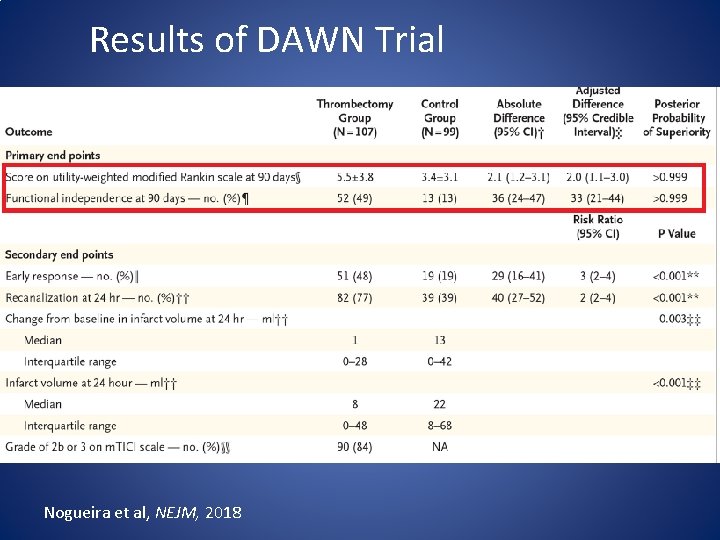
Results of DAWN Trial Nogueira et al, NEJM, 2018
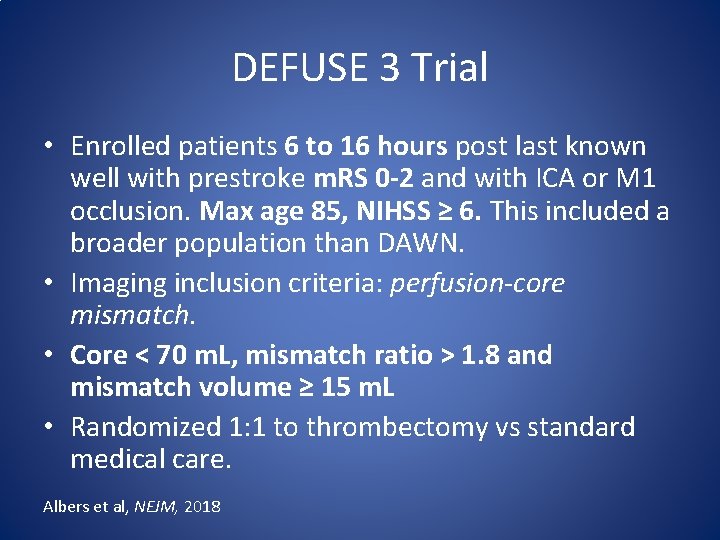
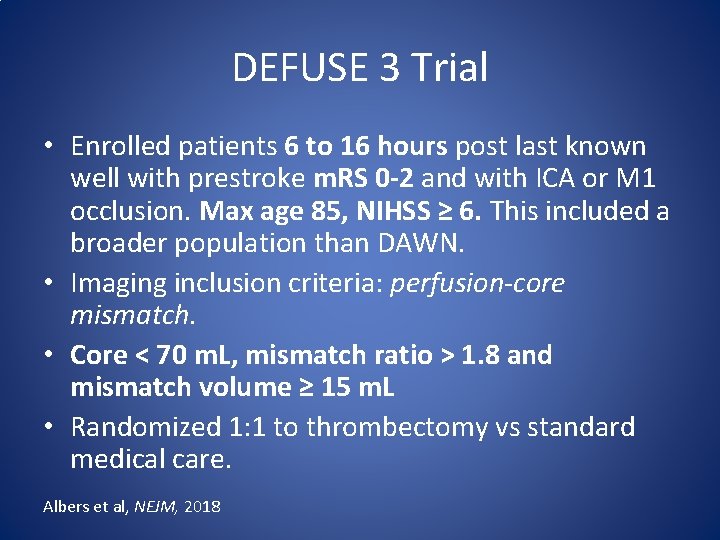
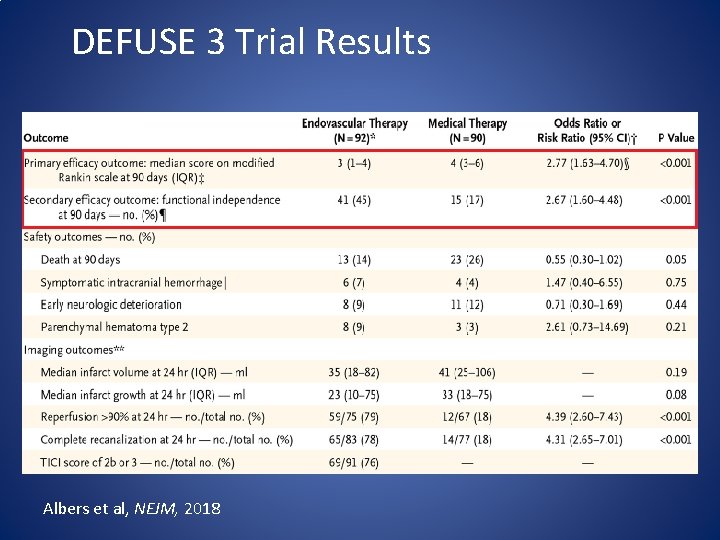
DEFUSE 3 Trial • Enrolled patients 6 to 16 hours post last known well with prestroke m. RS 0 -2 and with ICA or M 1 occlusion. Max age 85, NIHSS ≥ 6. This included a broader population than DAWN. • Imaging inclusion criteria: perfusion-core mismatch. • Core < 70 m. L, mismatch ratio > 1. 8 and mismatch volume ≥ 15 m. L • Randomized 1: 1 to thrombectomy vs standard medical care. Albers et al, NEJM, 2018
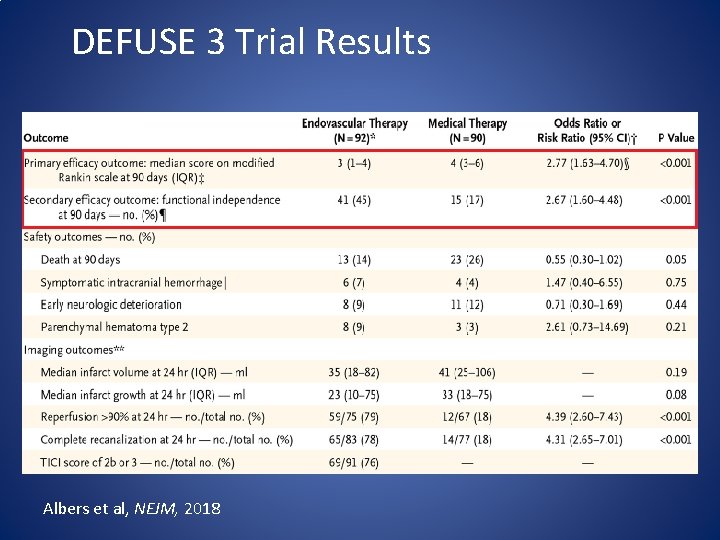
DEFUSE 3 Trial Results Albers et al, NEJM, 2018
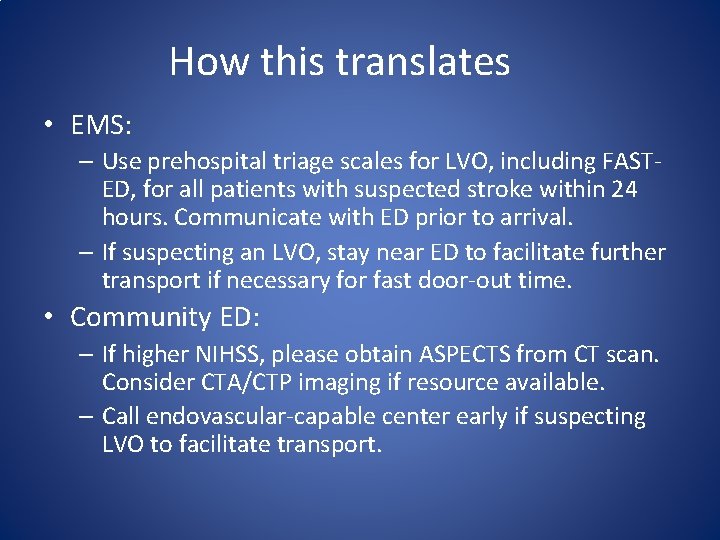
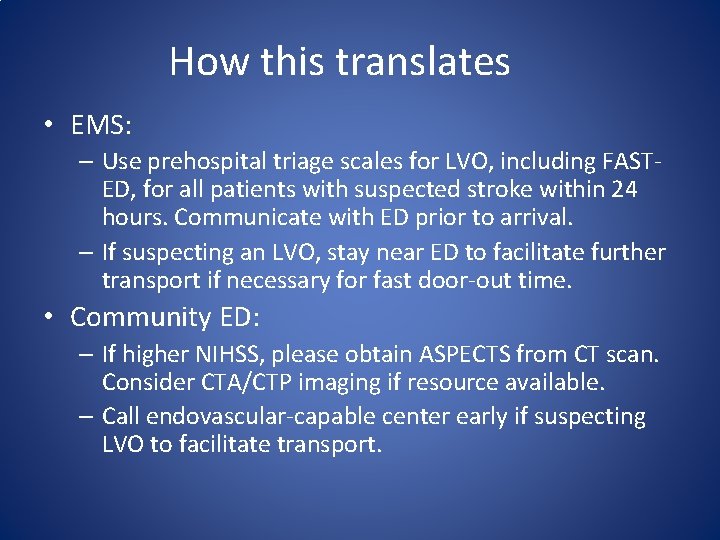
How this translates • EMS: – Use prehospital triage scales for LVO, including FASTED, for all patients with suspected stroke within 24 hours. Communicate with ED prior to arrival. – If suspecting an LVO, stay near ED to facilitate further transport if necessary for fast door-out time. • Community ED: – If higher NIHSS, please obtain ASPECTS from CT scan. Consider CTA/CTP imaging if resource available. – Call endovascular-capable center early if suspecting LVO to facilitate transport.
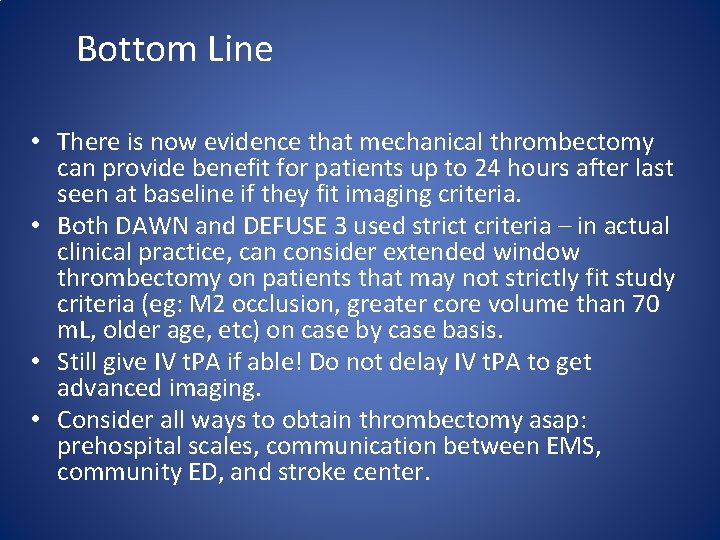
Bottom Line • There is now evidence that mechanical thrombectomy can provide benefit for patients up to 24 hours after last seen at baseline if they fit imaging criteria. • Both DAWN and DEFUSE 3 used strict criteria – in actual clinical practice, can consider extended window thrombectomy on patients that may not strictly fit study criteria (eg: M 2 occlusion, greater core volume than 70 m. L, older age, etc) on case by case basis. • Still give IV t. PA if able! Do not delay IV t. PA to get advanced imaging. • Consider all ways to obtain thrombectomy asap: prehospital scales, communication between EMS, community ED, and stroke center.
Questions? • Call for help anytime! • http: //www. kissnetwork. us/ • KU BAT phone: 913 -588 -3727