Unmet Need for Hepatitis C PCR Testing New


- Slides: 24
Unmet Need for Hepatitis C PCR Testing, New York City, 2009 -2010 Emily Mc. Gibbon, MPH June 2011 CSTE Annual Conference
Hepatitis C (HCV) – the basics • Bloodborne virus • Main modes of transmission: • • Injection drug use Transfusion before 1992 Perinatal transmission rate = 6% Sexual transmission low; conflicting data in literature
HCV – the basics cont’d • No test for acute infection • Usually leads to chronic infection • In 10 -15% infection spontaneously resolves • Patients asymptomatic or have mild illness for years • 15 -20% with chronic HCV develop liver cirrhosis
HCV antibody test • Screening test • Positive EIA (with high signal-to-cutoff ratio) or RIBA reportable to NYC DOHMH • If positive, could indicate: • Either acute or chronic infection • Resolved infection • False positive • If resolved infection, antibody positive for life but does not confer immunity to reinfection
HCV NAT test • Positive Nucleic Acid Test (NAT), e. g. PCR, reportable to NYC DOHMH • Indicates current HCV infection • Fewer labs perform this test • $$$ compared to antibody test
Patients with positive HCV antibody need PCR test • About 10 -15% of antibody-positive patients are not infected • Without PCR, patients do not know infection status • Unclear what clinicians are telling patients when antibody positive and PCR not done
HCV in New York City • About 10, 000 patients newly reported per year 1 • High volume and limited staff • No routine investigation (unless acute) • Limited data on epi of HCV in NYC 1) http: //www. nyc. gov/html/doh/downloads/pdf/cd/cd-hepabc-surveillance-report-08 -09. pdf
Enhanced HCV surveillance methods • On-going enhanced surveillance – July 2009 • Sample 20 patients every 2 months • Newly reported • NYC residents or unknown address • DOB known • Physician questionnaire (fax or phone) • • • Demographics Risk factors Reasons for testing Treatment, hepatitis A and B vaccination Counseling on transmission and alcohol use
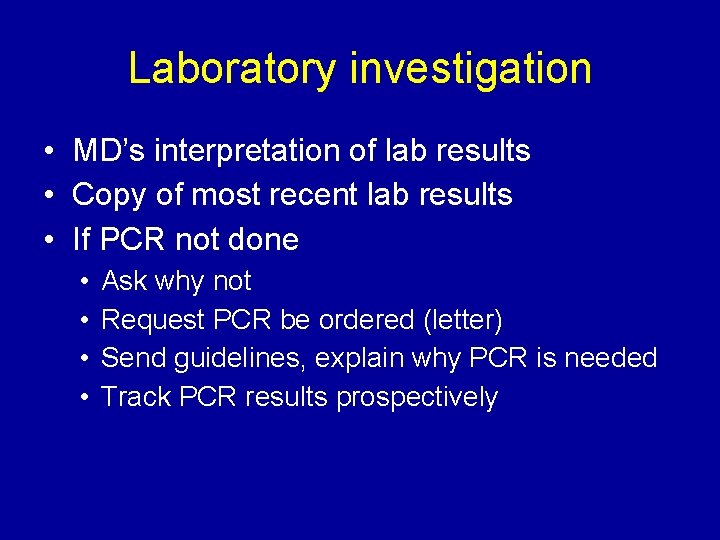
Laboratory investigation • MD’s interpretation of lab results • Copy of most recent lab results • If PCR not done • • Ask why not Request PCR be ordered (letter) Send guidelines, explain why PCR is needed Track PCR results prospectively
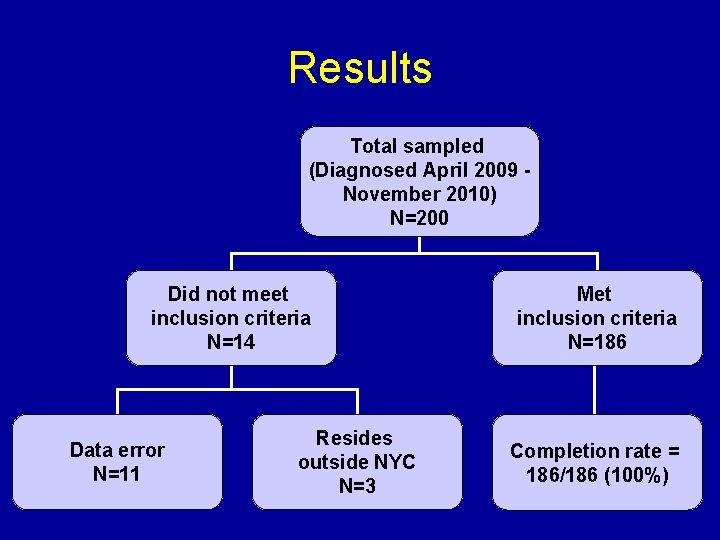
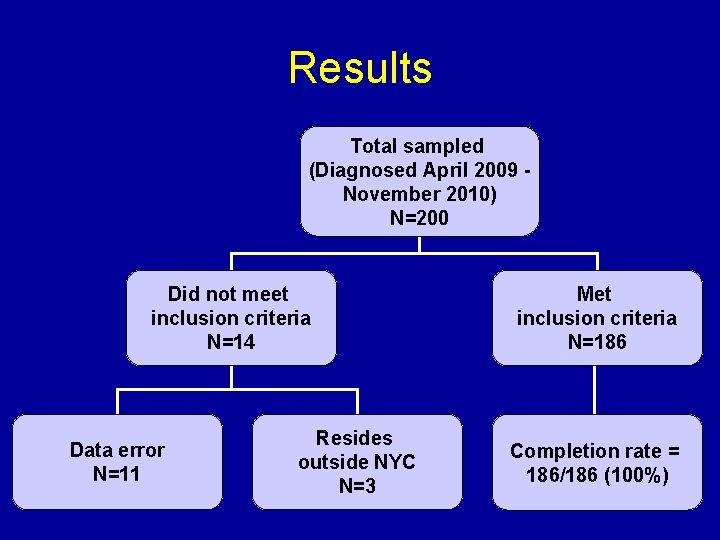
Results Total sampled (Diagnosed April 2009 November 2010) N=200 Did not meet inclusion criteria N=14 Data error N=11 Resides outside NYC N=3 Met inclusion criteria N=186 Completion rate = 186/186 (100%)
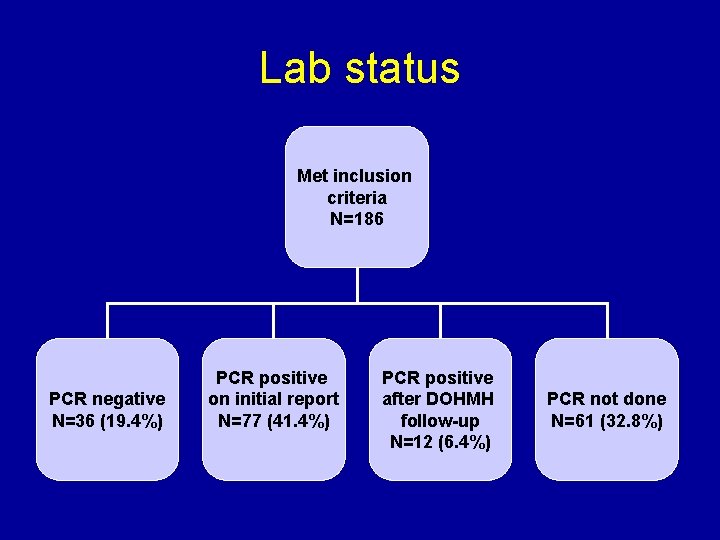
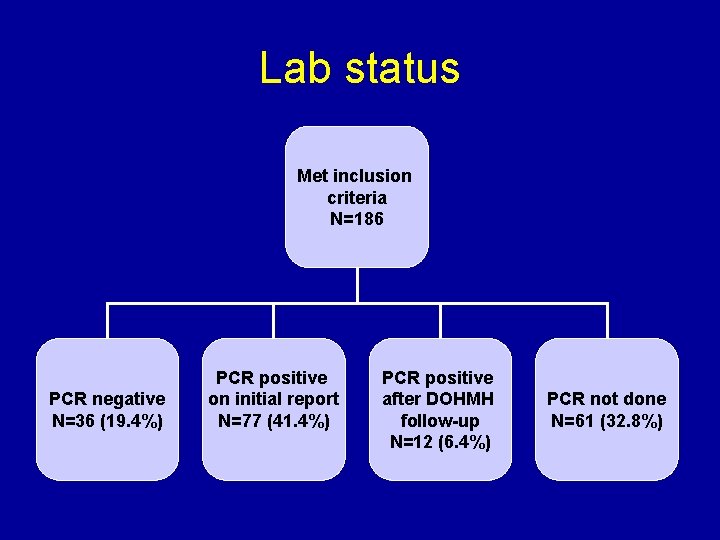
Lab status Met inclusion criteria N=186 PCR negative N=36 (19. 4%) PCR positive on initial report N=77 (41. 4%) PCR positive after DOHMH follow-up N=12 (6. 4%) PCR not done N=61 (32. 8%)
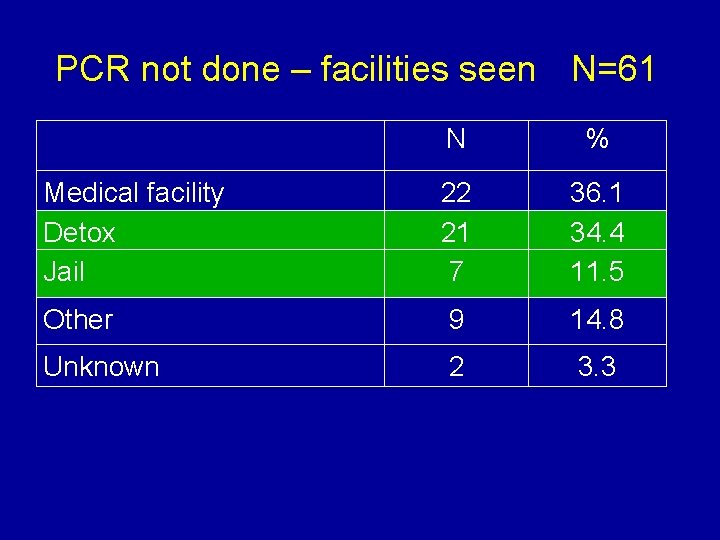
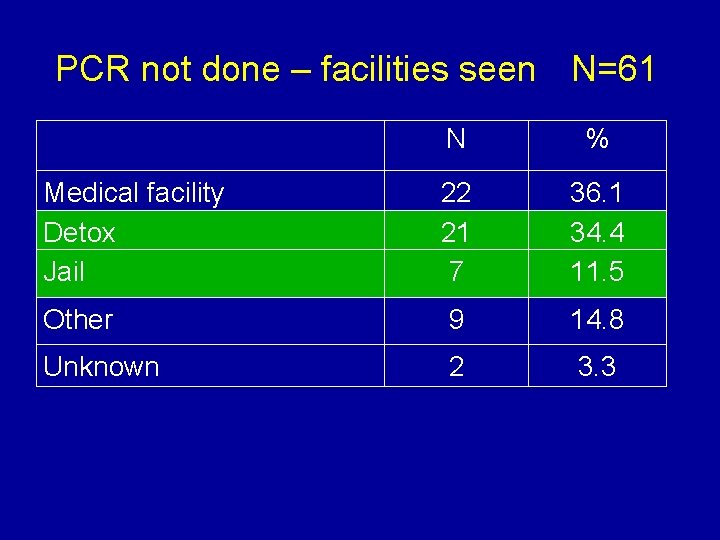
PCR not done – facilities seen N=61 N % Medical facility Detox Jail 22 21 7 36. 1 34. 4 11. 5 Other 9 14. 8 Unknown 2 3. 3
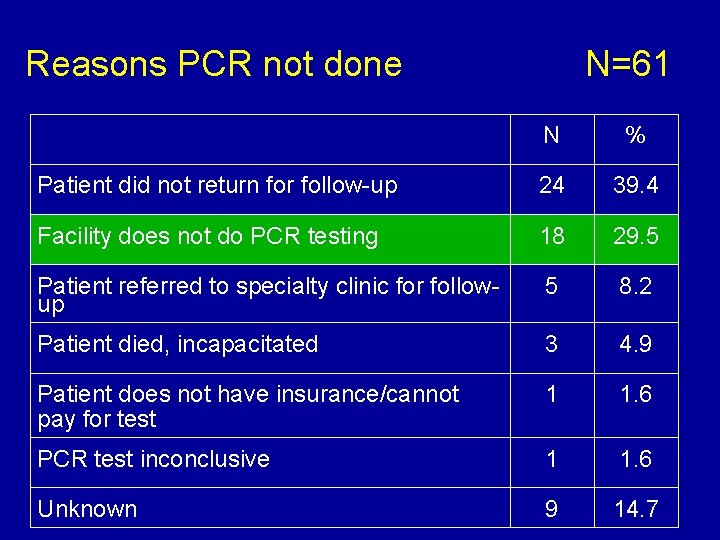
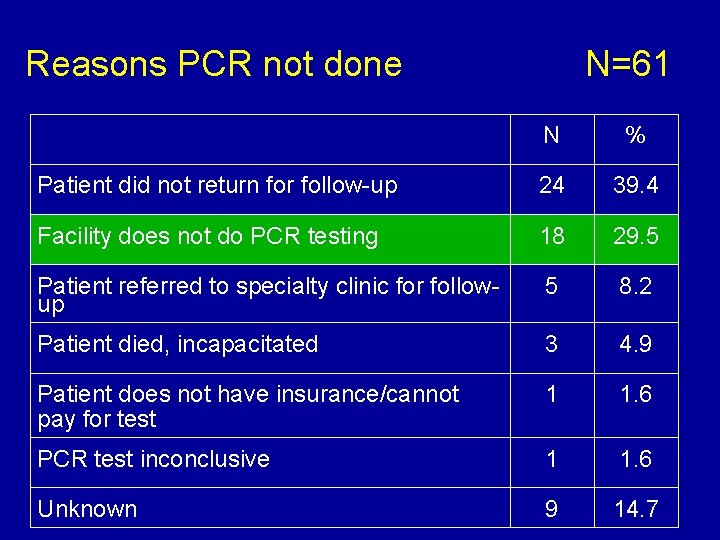
Reasons PCR not done N=61 N % Patient did not return for follow-up 24 39. 4 Facility does not do PCR testing 18 29. 5 Patient referred to specialty clinic for followup 5 8. 2 Patient died, incapacitated 3 4. 9 Patient does not have insurance/cannot pay for test 1 1. 6 PCR test inconclusive 1 1. 6 Unknown 9 14. 7
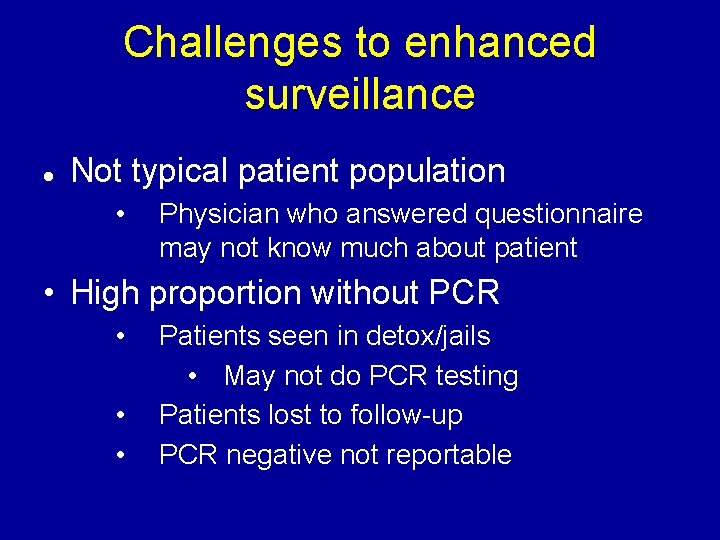
Challenges to enhanced surveillance Not typical patient population • Physician who answered questionnaire may not know much about patient • High proportion without PCR • • • Patients seen in detox/jails • May not do PCR testing Patients lost to follow-up PCR negative not reportable
Patient #1 • Tested antibody positive while in detox • Facility does not do PCR testing • Referred patient to specialist for follow-up (standard practice) • No positive PCR ever reported
Patient #2 • 23 year-old student, tested antibody positive as screening for school • Only risk factor is immigrating from Ukraine (high-prevalence country) in 1993 • MD told him he had HCV • Patient did not go back to initial MD as far as we know • No PCR as far as we can tell
Patient #3 • 5 reports of antibody positive results from different detox facilities • No PCR as far as we can tell
Patient #4 • Antibody positive this year, reported to us for first time • Had prior positive antibody test in 2005, tested PCR negative in 2006 • Likely had HCV in past but resolved infection • Should not have been retested for antibody!
Conclusions • If PCR not done: • Infection status for patients often remains unknown • Difficult to assess patients’ needs • Difficult to know when to stop investigating • Of 200 sampled: • 36 were PCR negative • Meet case definition for chronic/resolved HCV • Probably not infected
Health Department response • Interview multiple providers if learn about another MD who may know patient better • Developed clinical bulletin about HCV diagnosis and care, emphasizing need for PCR • Started additional follow-up for patients where PCR not done

PCR follow-up project Select patients whose enhanced surveillance investigations were closed >9 months prior Patients where PCR not done (N=61) Contact all known clinicians Was PCR ever done? Started project Feb 23, 2011 – 37 cases to follow up on
Next steps? • Continue educating providers about importance of PCR testing • Clinical staff • Detox, jail staff: social workers, counselors • Lobby to make PCR test more available/affordable for detox and jails

Acknowledgements • • • Ellen Gee Duyang Kim Bianca Malcolm Grace Malonga Meredith Rossi Allan Uribe Tim Wen Janette Yung Sharon Balter Jennifer Baumgartner Katherine Bornschlegel