Unmet Need and Challenges in Vasculitis Scottish Systemic


- Slides: 60
Unmet Need and Challenges in Vasculitis Scottish Systemic Vasculitis Network December 12, 2019 Dr Neil Basu University of Glasgow
Disclosures • Research funding: Pfizer, GSK, Novartis, Vifor • Non-promotional speaking fees: Roche, Vifor, Lilly, Abbvie • Consultancies: Pfizer, MSD, Lilly
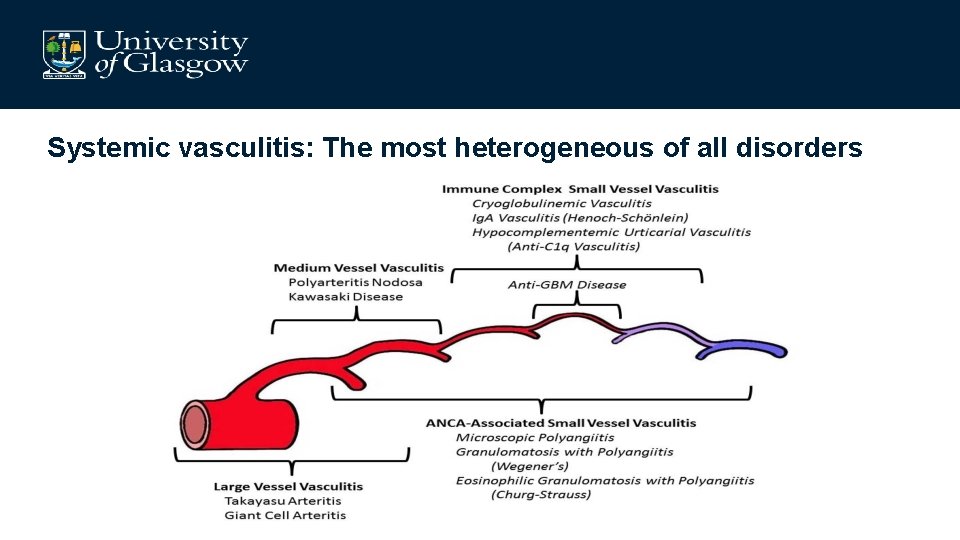
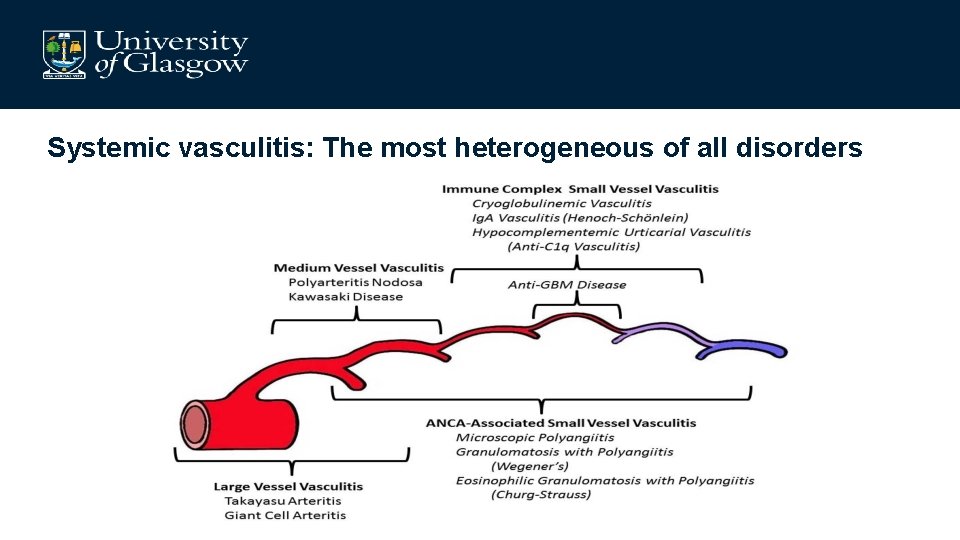
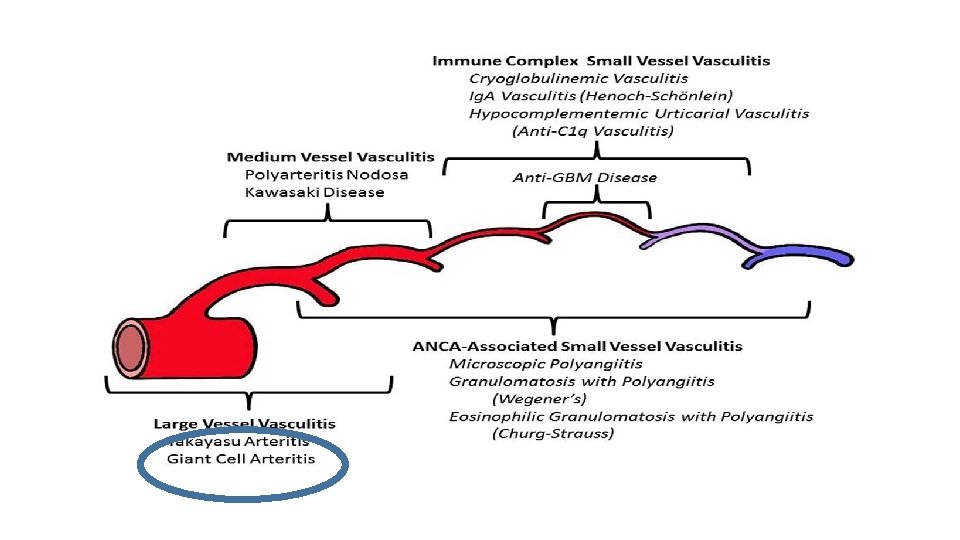
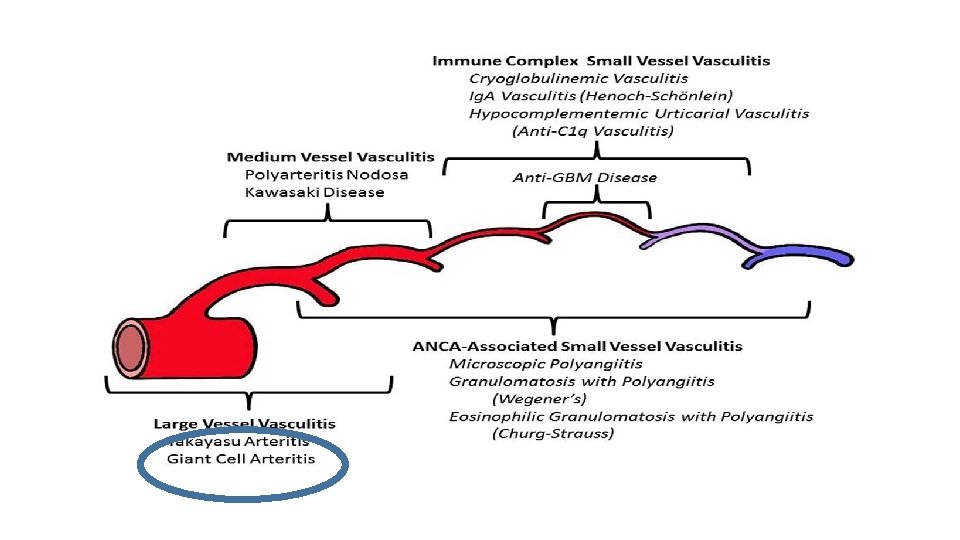
Systemic vasculitis: The most heterogeneous of all disorders
Patient LM: 45 year old male architect • Presenting complaint – 3/12 Ear discharge, hearing loss – 2/12 Arthralgia – Nasal bridge pain • No significant PMHx, Medications • Urine – blood ++ protein ++ • Normal renal excretory function • PR 3 -ANCA positive
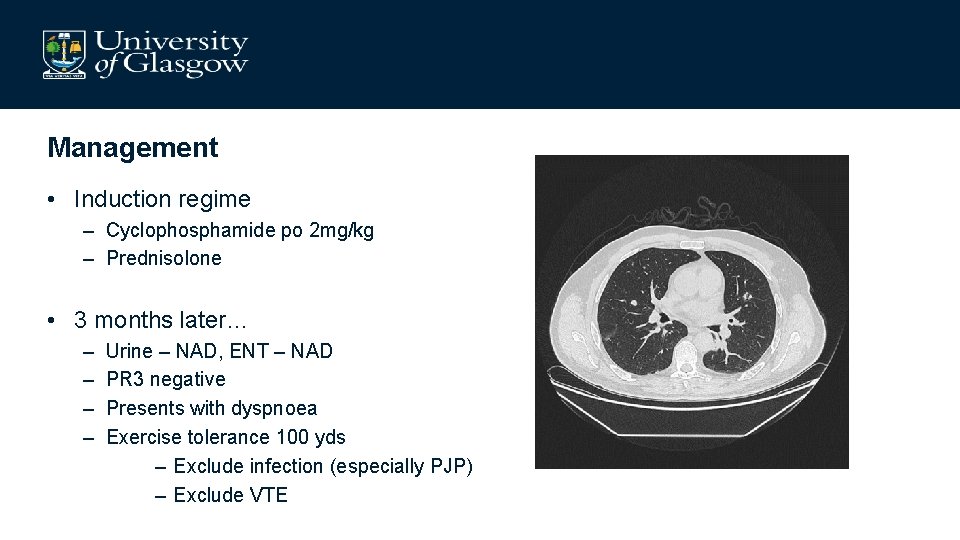
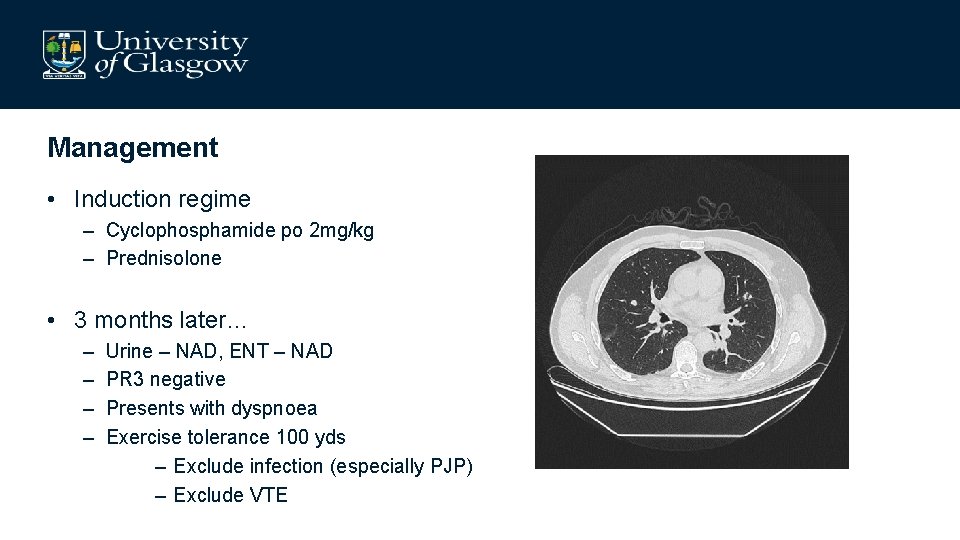
Management • Induction regime – Cyclophosphamide po 2 mg/kg – Prednisolone • 3 months later… – – Urine – NAD, ENT – NAD PR 3 negative Presents with dyspnoea Exercise tolerance 100 yds – Exclude infection (especially PJP) – Exclude VTE
Induction toolkit • Cyclophosphamide (po/iv) • Rituximab • Methotrexate • Mycophenolate
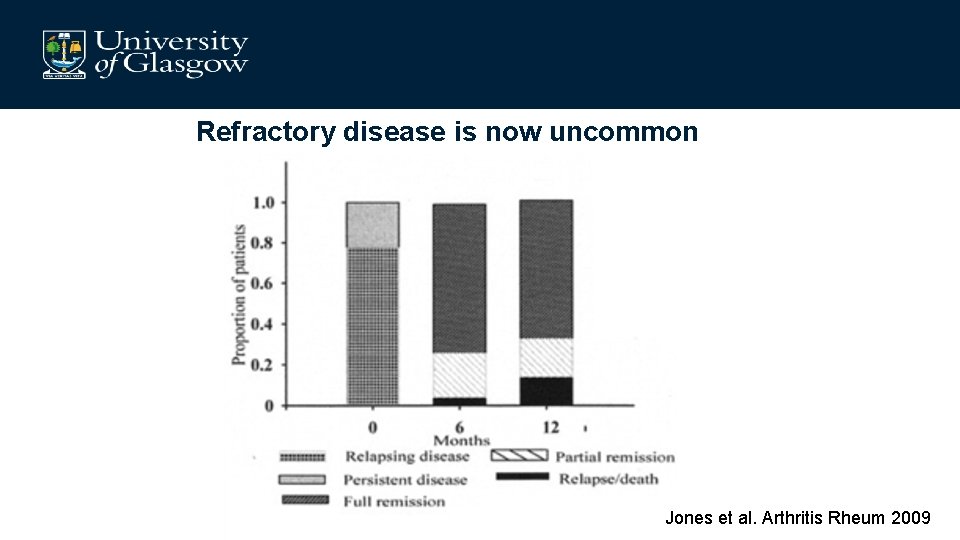
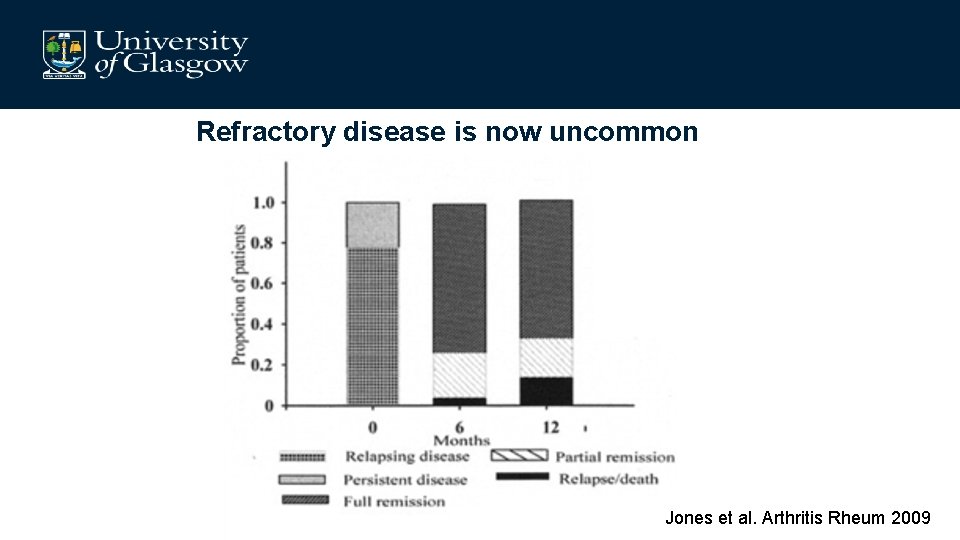
Refractory disease is now uncommon Jones et al. Arthritis Rheum 2009
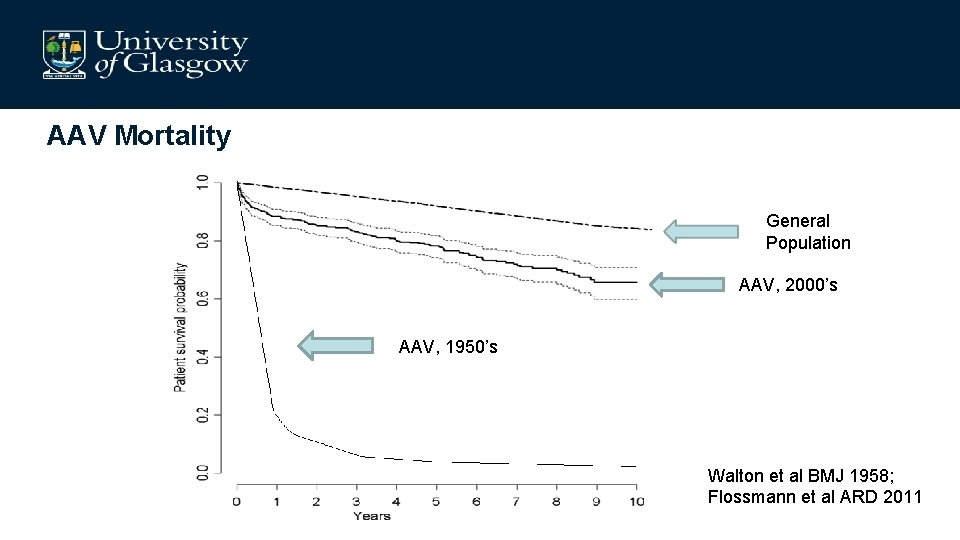
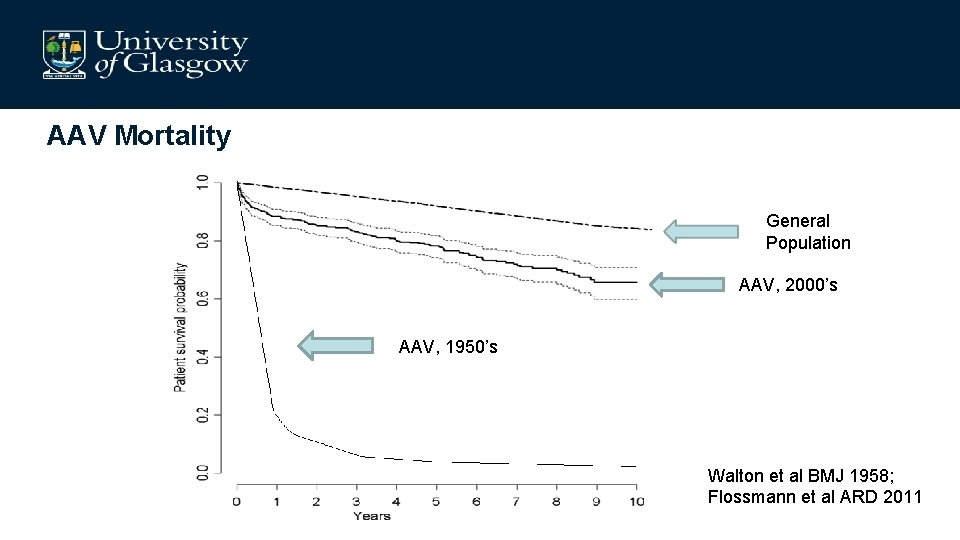
AAV Mortality General Population AAV, 2000’s AAV, 1950’s Walton et al BMJ 1958; Flossmann et al ARD 2011
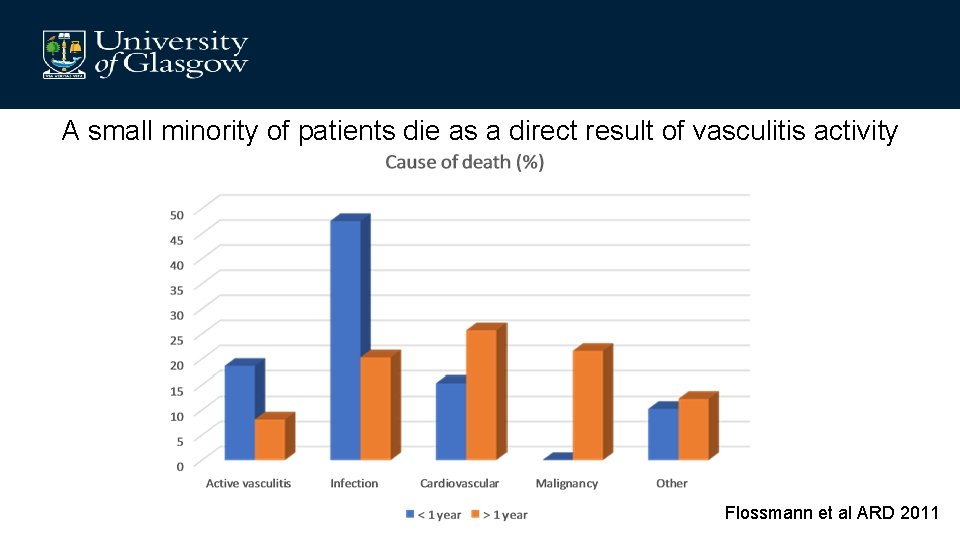
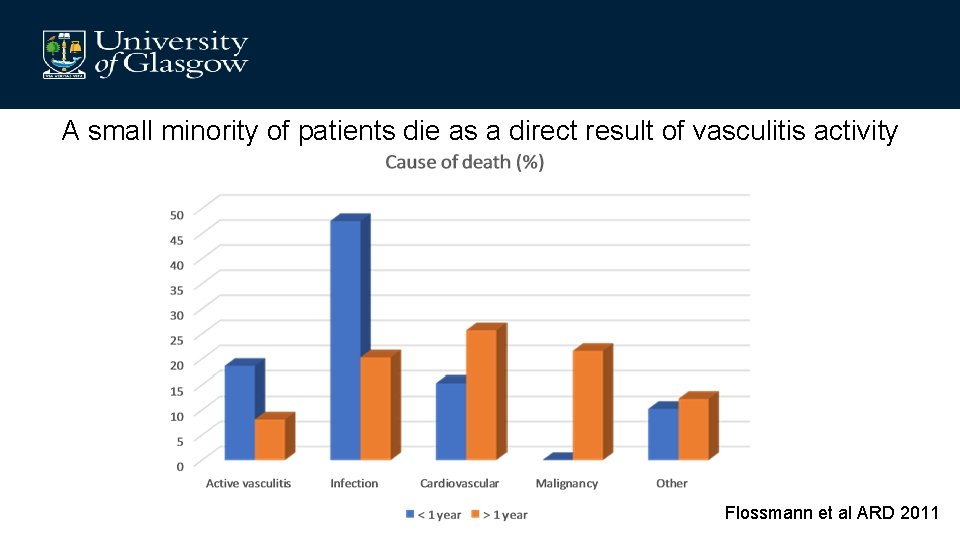
A small minority of patients die as a direct result of vasculitis activity Flossmann et al ARD 2011
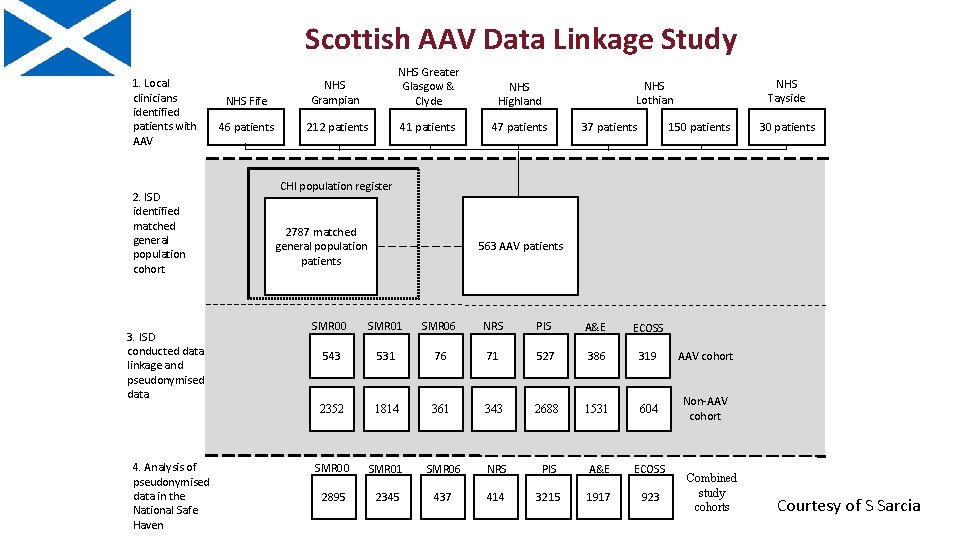
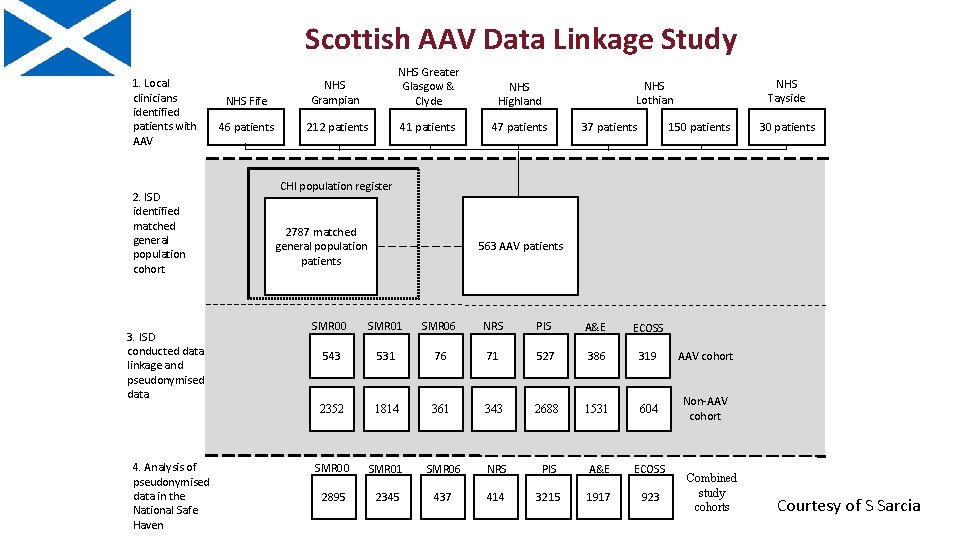
Scottish AAV Data Linkage Study 1. Local clinicians identified patients with AAV 2. ISD identified matched general population cohort 3. ISD conducted data linkage and pseudonymised data 4. Analysis of pseudonymised data in the National Safe Haven NHS Fife NHS Grampian NHS Greater Glasgow & Clyde NHS Highland 46 patients 212 patients 41 patients 47 patients NHS Tayside NHS Lothian 150 patients 37 patients 30 patients CHI population register 2787 matched general population patients 563 AAV patients SMR 00 SMR 01 SMR 06 NRS PIS A&E ECOSS 543 531 76 71 527 386 319 AAV cohort 2352 1814 361 343 2688 1531 604 Non-AAV cohort SMR 00 SMR 01 SMR 06 NRS PIS A&E ECOSS 2895 2345 437 414 3215 1917 923 Combined study cohorts Courtesy of S Sarcia
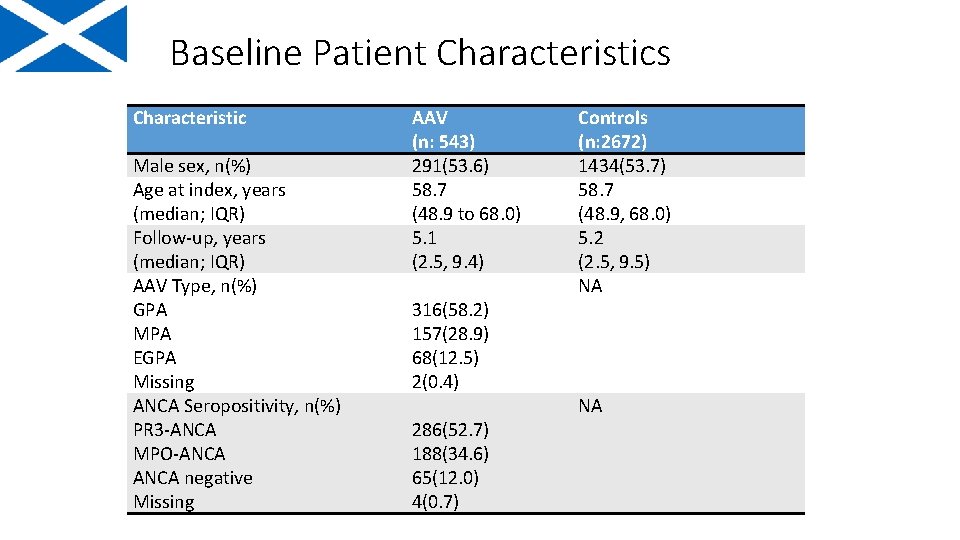
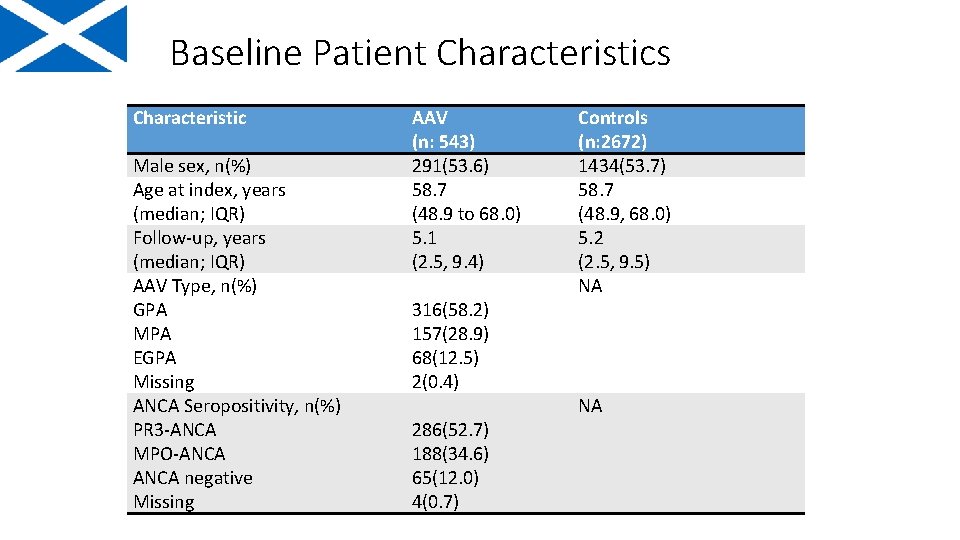
Baseline Patient Characteristics Characteristic Male sex, n(%) Age at index, years (median; IQR) Follow-up, years (median; IQR) AAV Type, n(%) GPA MPA EGPA Missing ANCA Seropositivity, n(%) PR 3 -ANCA MPO-ANCA negative Missing AAV (n: 543) 291(53. 6) 58. 7 (48. 9 to 68. 0) 5. 1 (2. 5, 9. 4) 316(58. 2) 157(28. 9) 68(12. 5) 2(0. 4) 286(52. 7) 188(34. 6) 65(12. 0) 4(0. 7) Controls (n: 2672) 1434(53. 7) 58. 7 (48. 9, 68. 0) 5. 2 (2. 5, 9. 5) NA NA
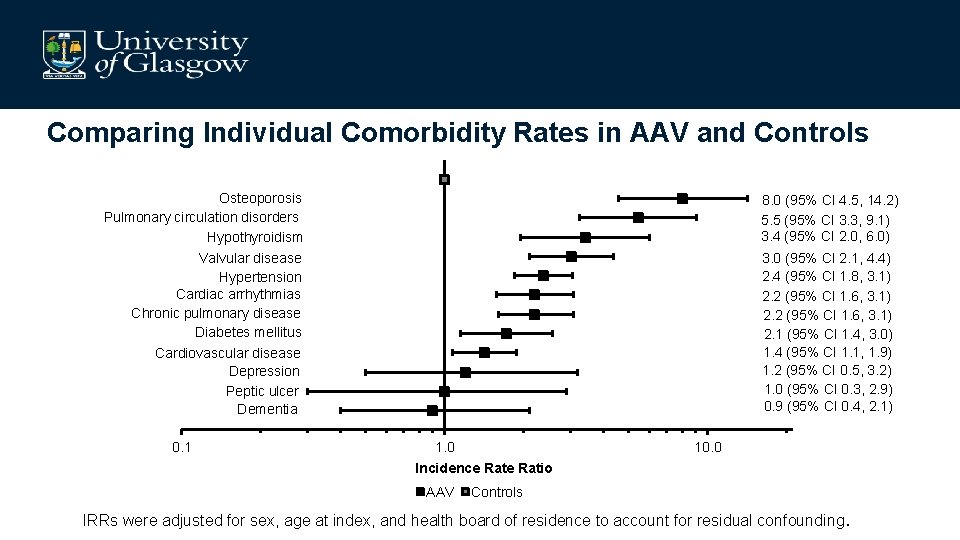
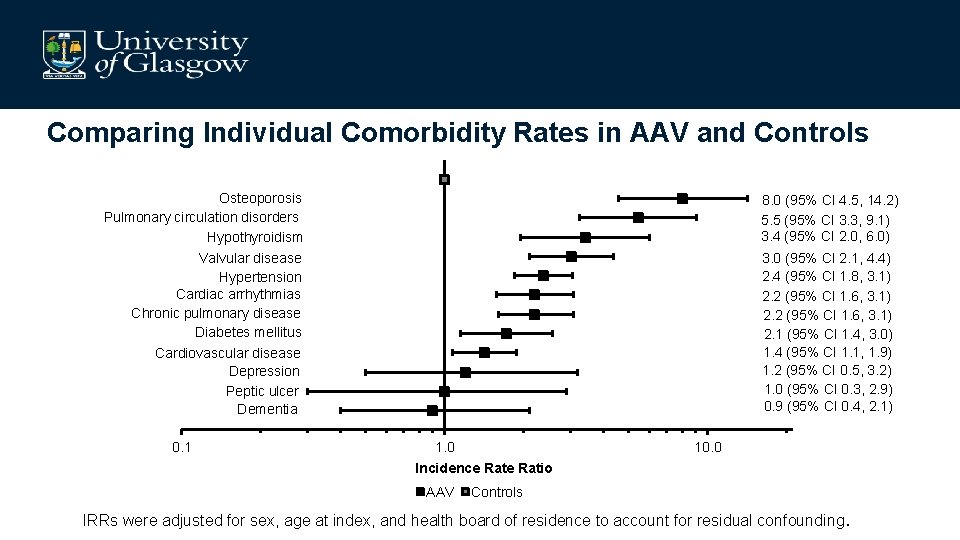
Comparing Individual Comorbidity Rates in AAV and Controls Osteoporosis Pulmonary circulation disorders Hypothyroidism Valvular disease Hypertension Cardiac arrhythmias Chronic pulmonary disease Diabetes mellitus Cardiovascular disease Depression Peptic ulcer Dementia 0. 1 8. 0 (95% CI 4. 5, 14. 2) 5. 5 (95% CI 3. 3, 9. 1) 3. 4 (95% CI 2. 0, 6. 0) 3. 0 (95% CI 2. 1, 4. 4) 2. 4 (95% CI 1. 8, 3. 1) 2. 2 (95% CI 1. 6, 3. 1) 2. 1 (95% CI 1. 4, 3. 0) 1. 4 (95% CI 1. 1, 1. 9) 1. 2 (95% CI 0. 5, 3. 2) 1. 0 (95% CI 0. 3, 2. 9) 0. 9 (95% CI 0. 4, 2. 1) 1. 0 Incidence Ratio AAV 10. 0 Controls IRRs were adjusted for sex, age at index, and health board of residence to account for residual confounding.
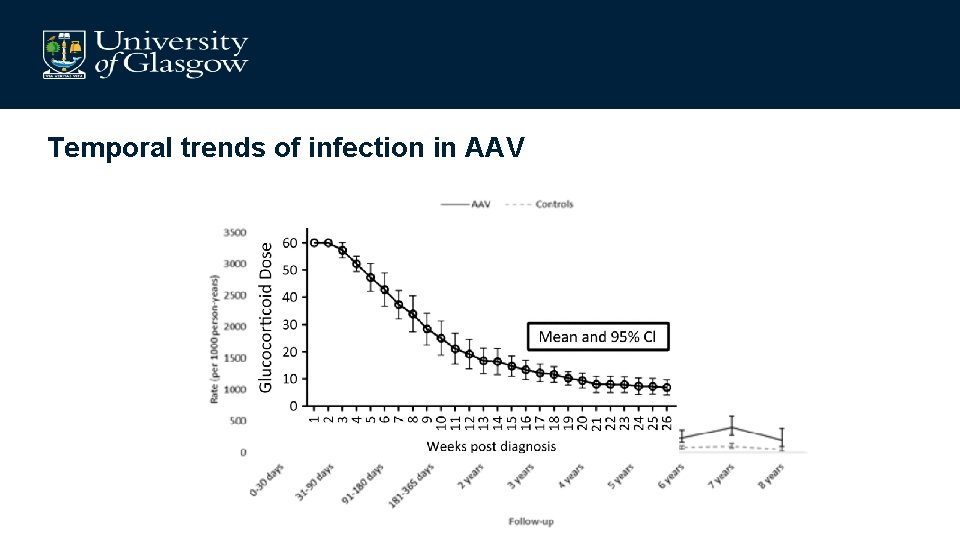
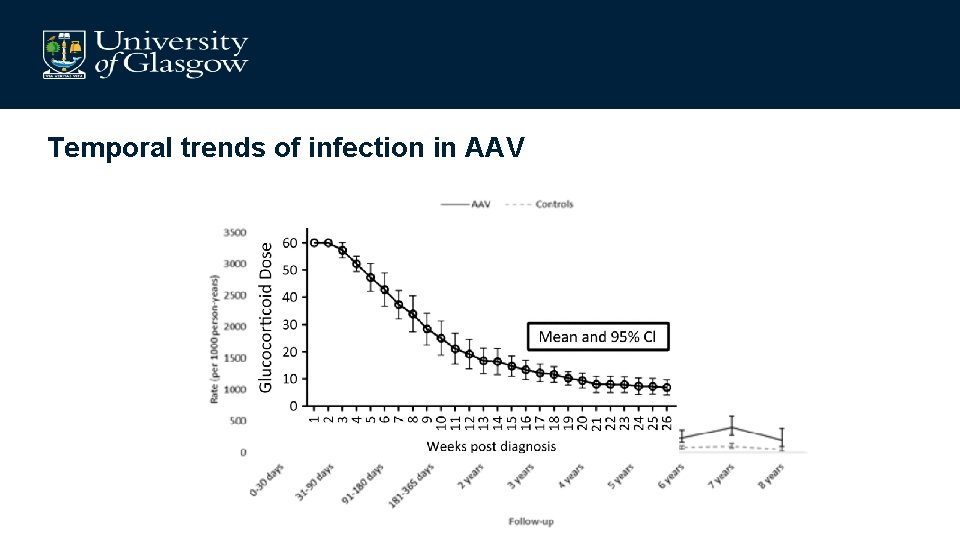
Temporal trends of infection in AAV
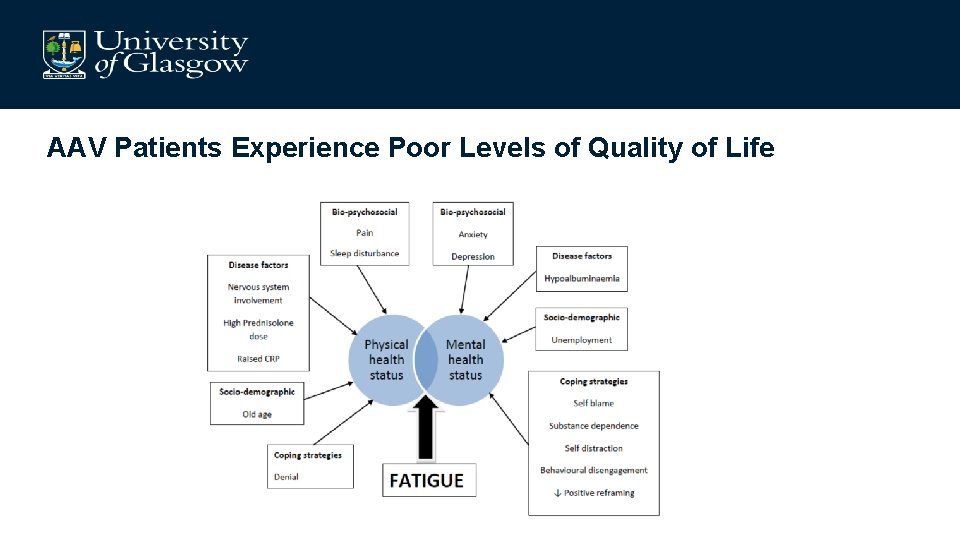
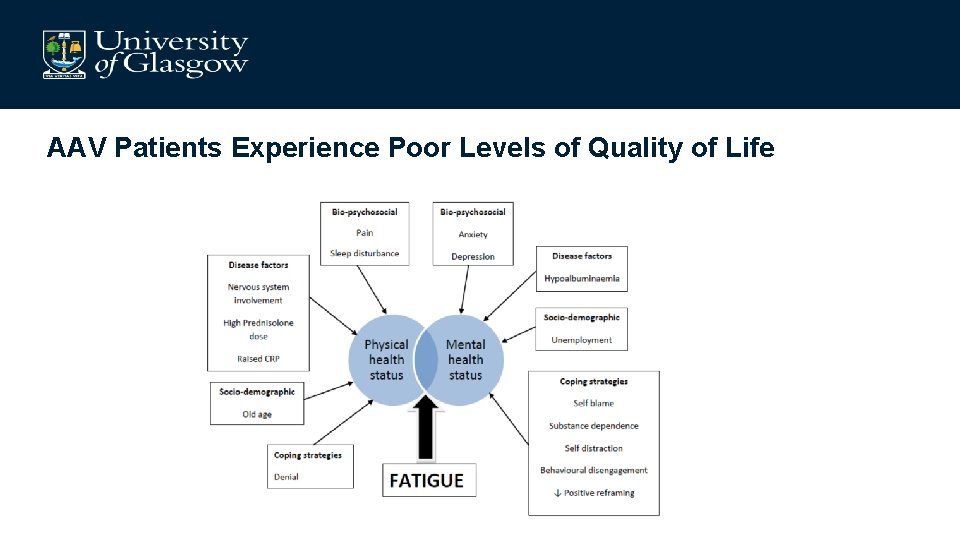
AAV Patients Experience Poor Levels of Quality of Life
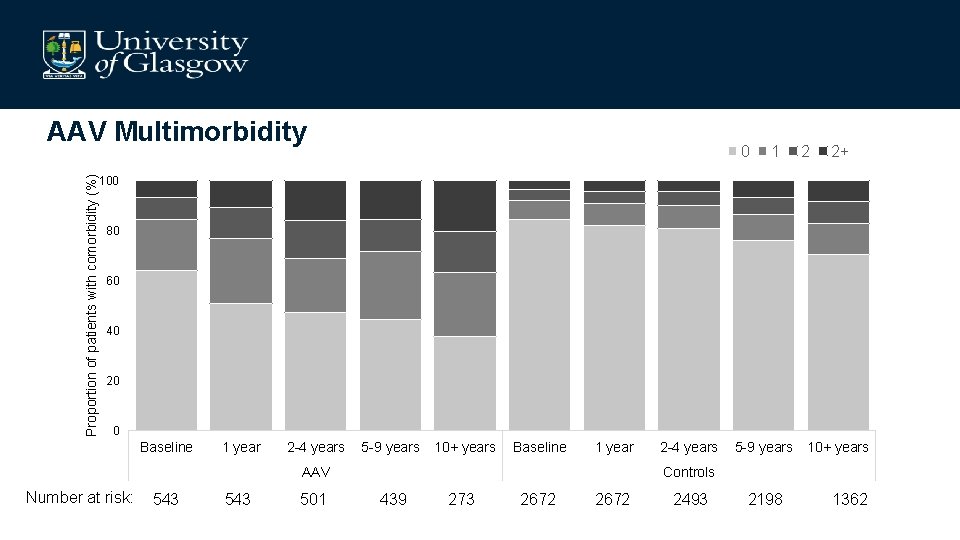
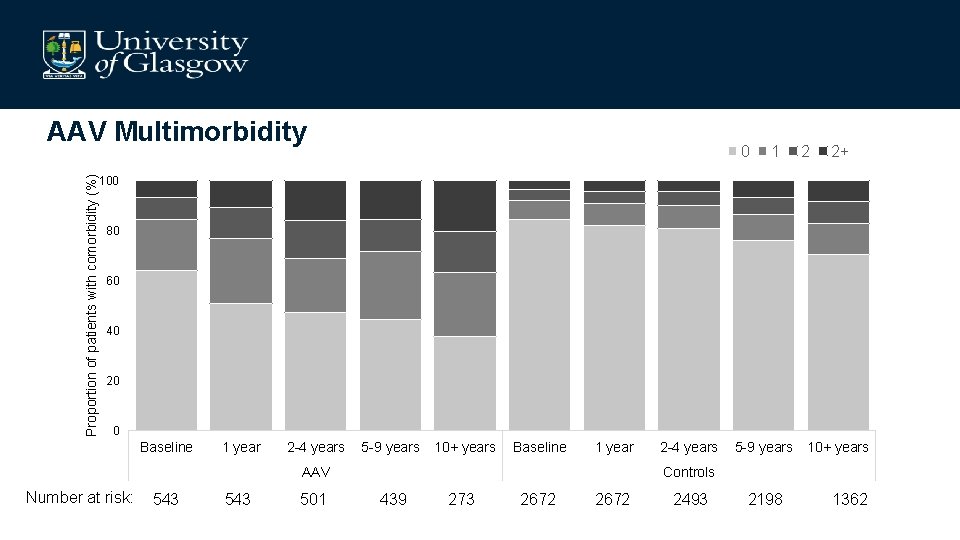
Proportion of patients with comorbidity (%) AAV Multimorbidity 0 1 2 2+ 100 80 60 40 20 0 Baseline 1 year 2 -4 years 5 -9 years 10+ years Baseline 1 year AAV Number at risk: 543 501 2 -4 years 5 -9 years 10+ years Controls 439 273 2672 2493 2198 1362
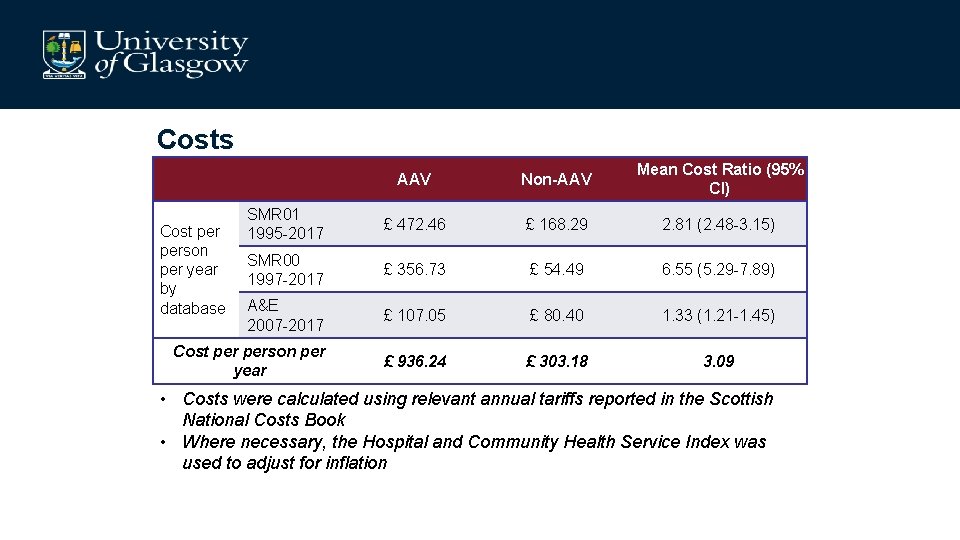
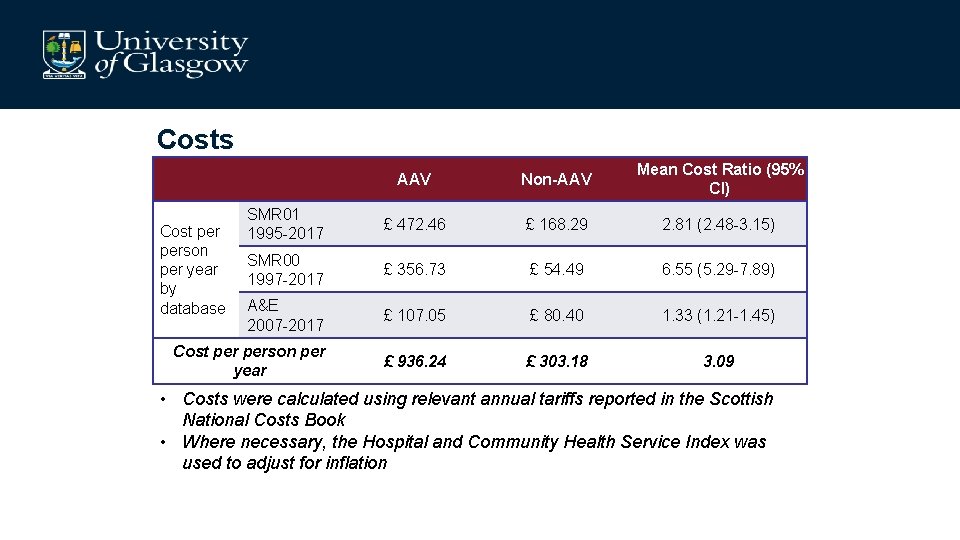
Costs AAV Non-AAV Mean Cost Ratio (95% CI) SMR 01 1995 -2017 £ 472. 46 £ 168. 29 2. 81 (2. 48 -3. 15) SMR 00 1997 -2017 £ 356. 73 £ 54. 49 6. 55 (5. 29 -7. 89) A&E 2007 -2017 £ 107. 05 £ 80. 40 1. 33 (1. 21 -1. 45) Cost person per year £ 936. 24 £ 303. 18 3. 09 Cost person per year by database • Costs were calculated using relevant annual tariffs reported in the Scottish National Costs Book • Where necessary, the Hospital and Community Health Service Index was used to adjust for inflation
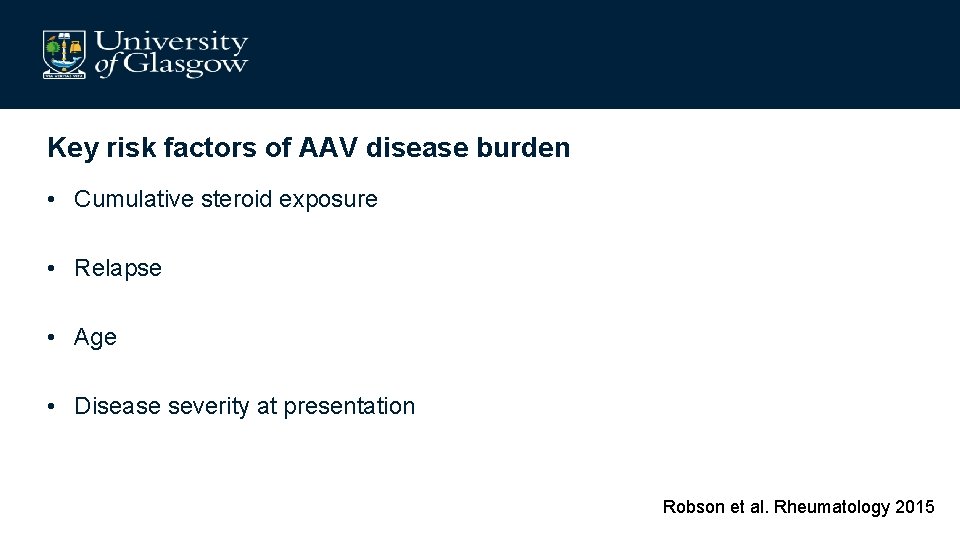
Key risk factors of AAV disease burden • Cumulative steroid exposure • Relapse • Age • Disease severity at presentation Robson et al. Rheumatology 2015
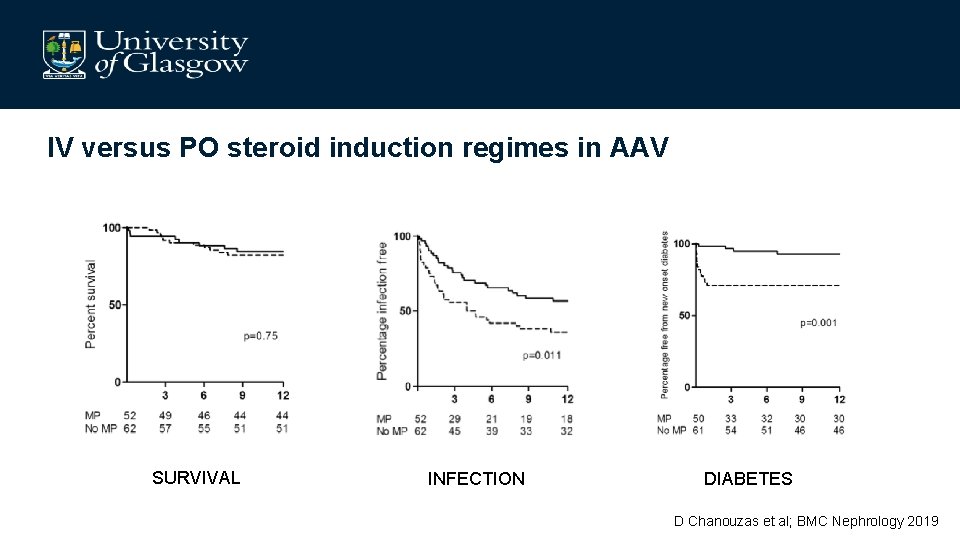
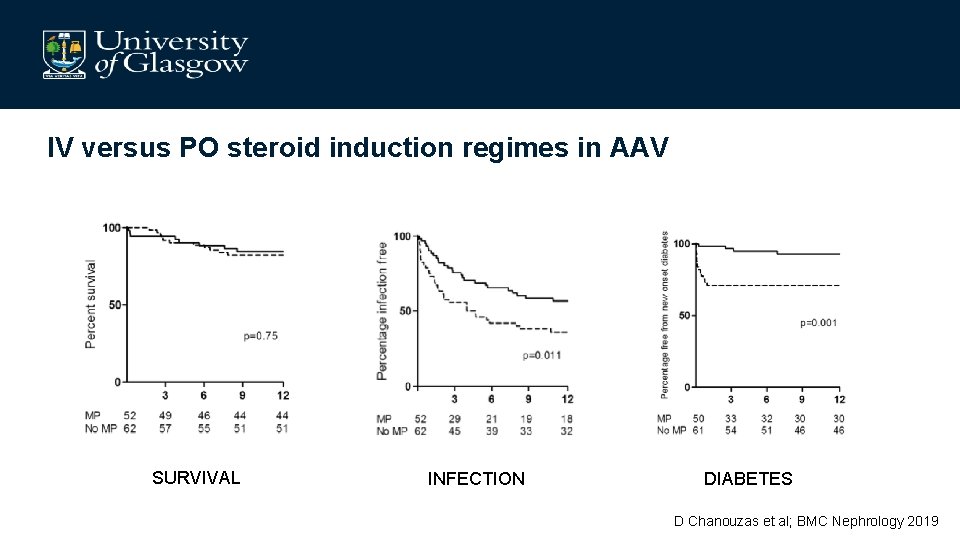
IV versus PO steroid induction regimes in AAV SURVIVAL INFECTION DIABETES D Chanouzas et al; BMC Nephrology 2019
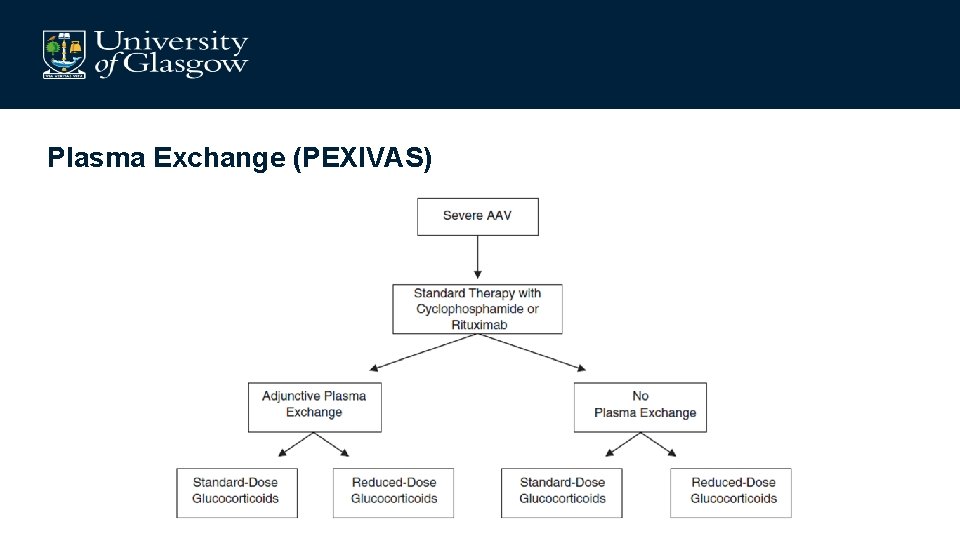
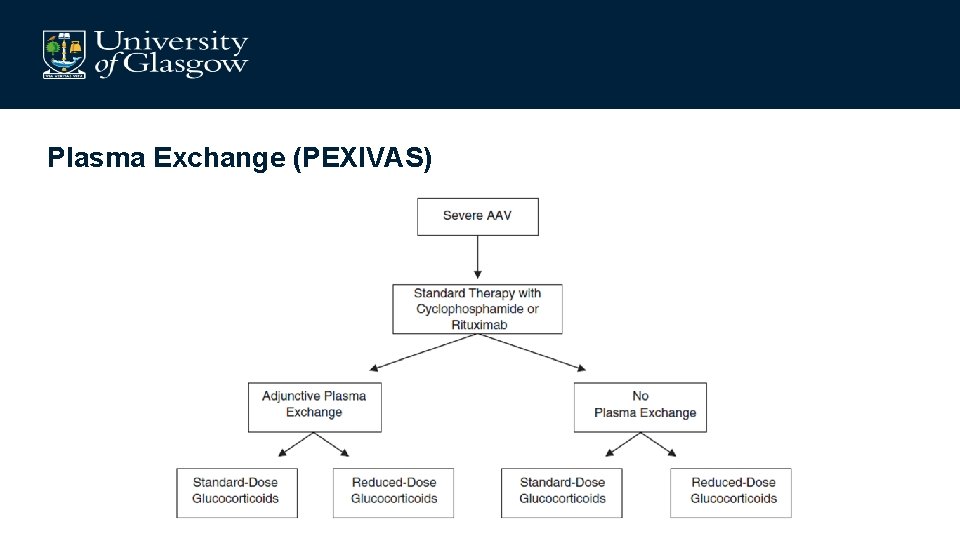
Plasma Exchange (PEXIVAS)
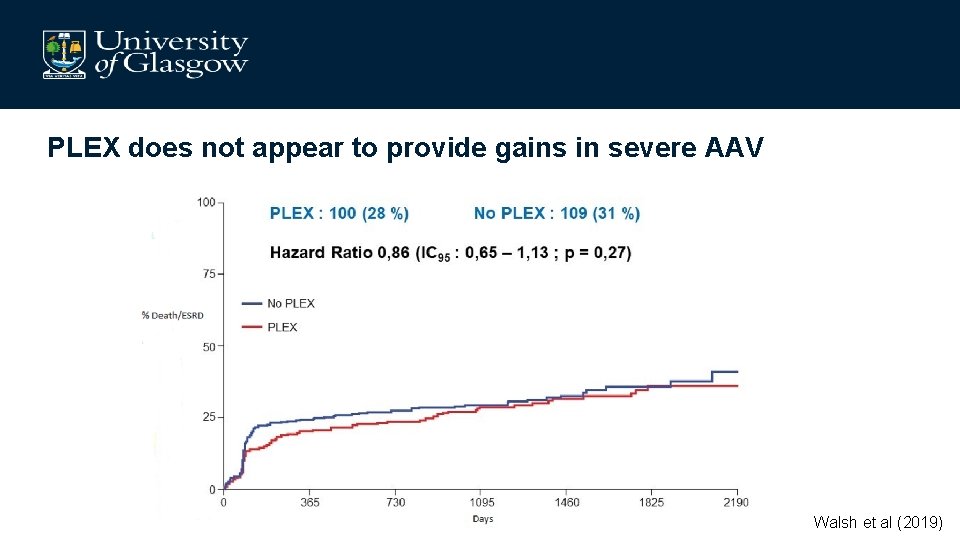
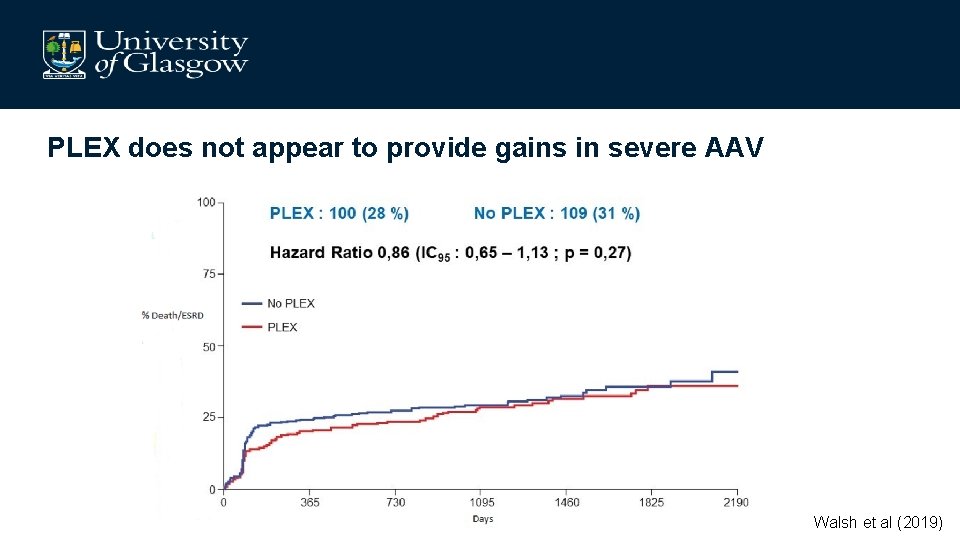
PLEX does not appear to provide gains in severe AAV Walsh et al (2019)
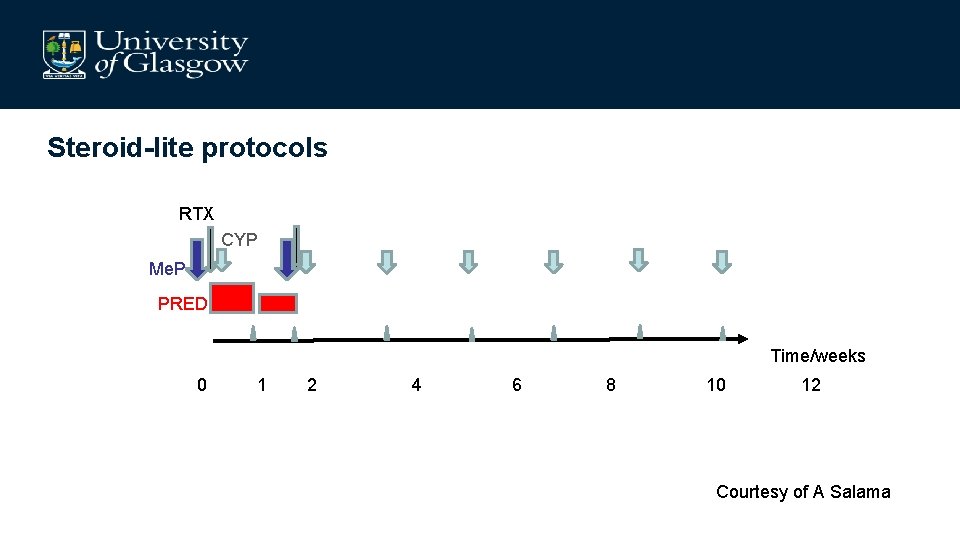
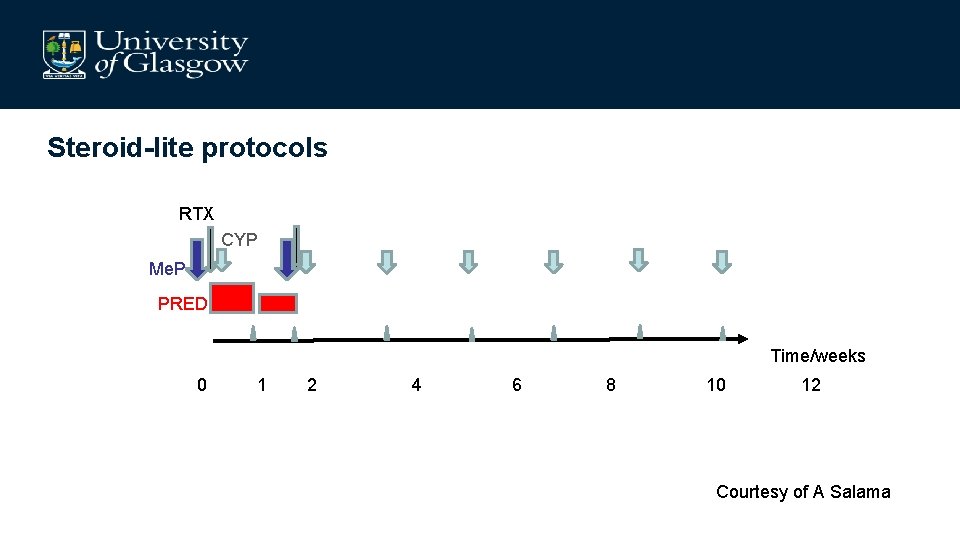
Steroid-lite protocols RTX CYP Me. P PRED Time/weeks 0 1 2 4 6 8 10 12 Courtesy of A Salama
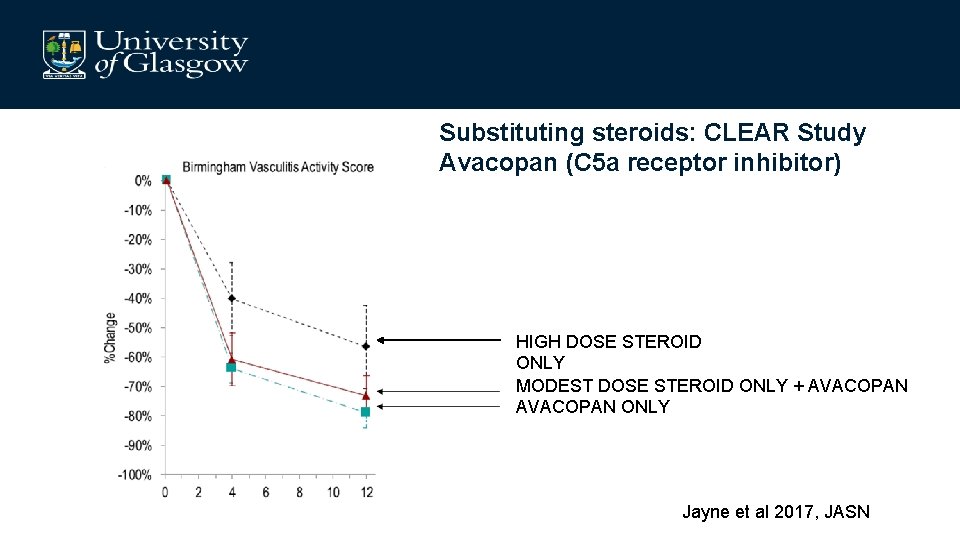
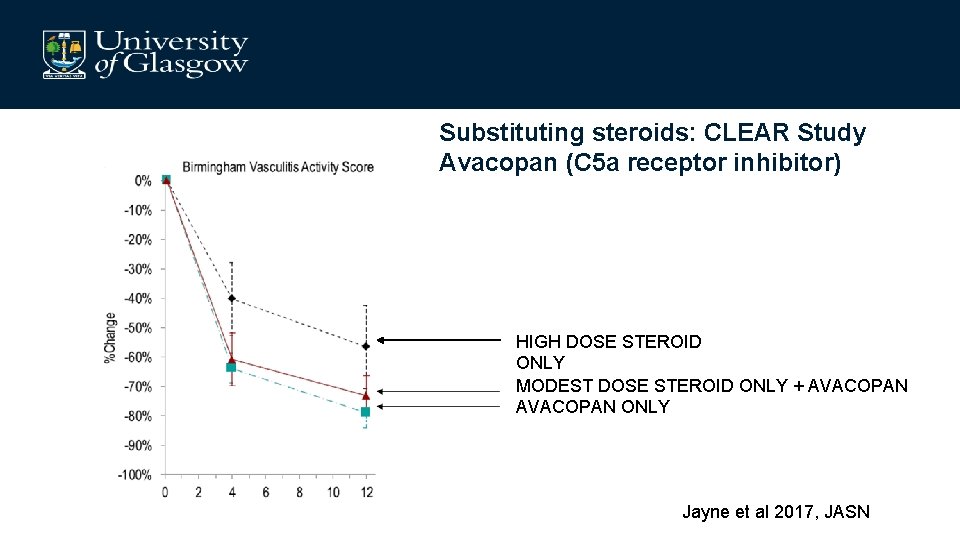
Substituting steroids: CLEAR Study Avacopan (C 5 a receptor inhibitor) HIGH DOSE STEROID ONLY MODEST DOSE STEROID ONLY + AVACOPAN ONLY Jayne et al 2017, JASN
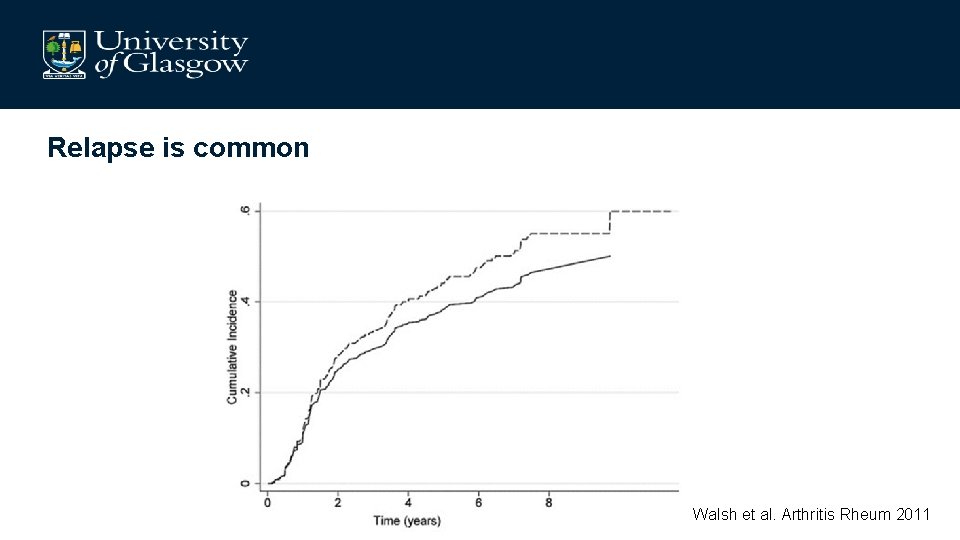
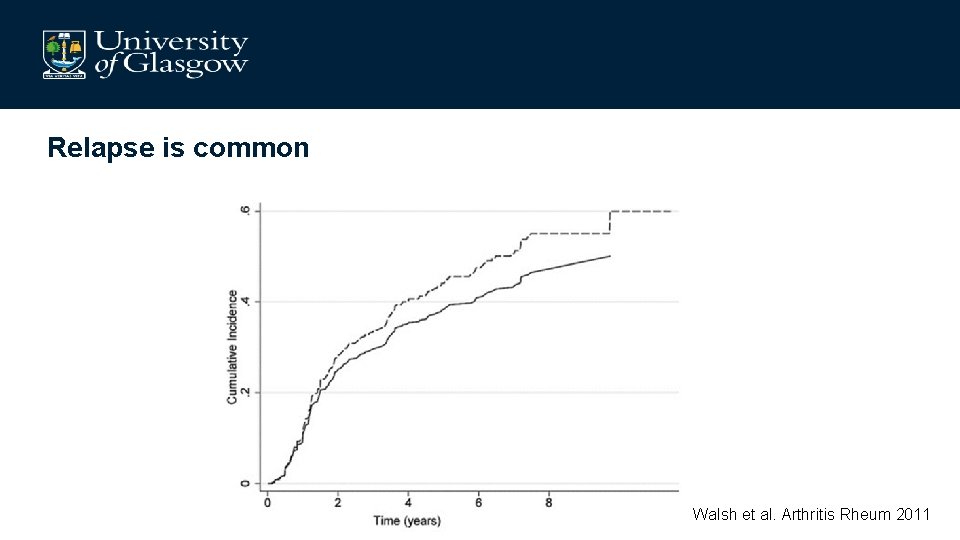
Relapse is common Walsh et al. Arthritis Rheum 2011
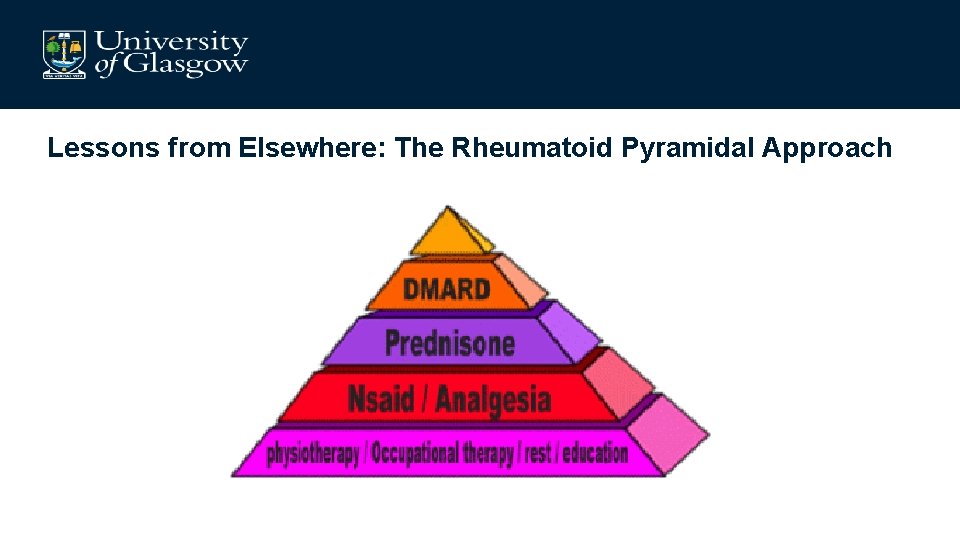
Lessons from Elsewhere: The Rheumatoid Pyramidal Approach
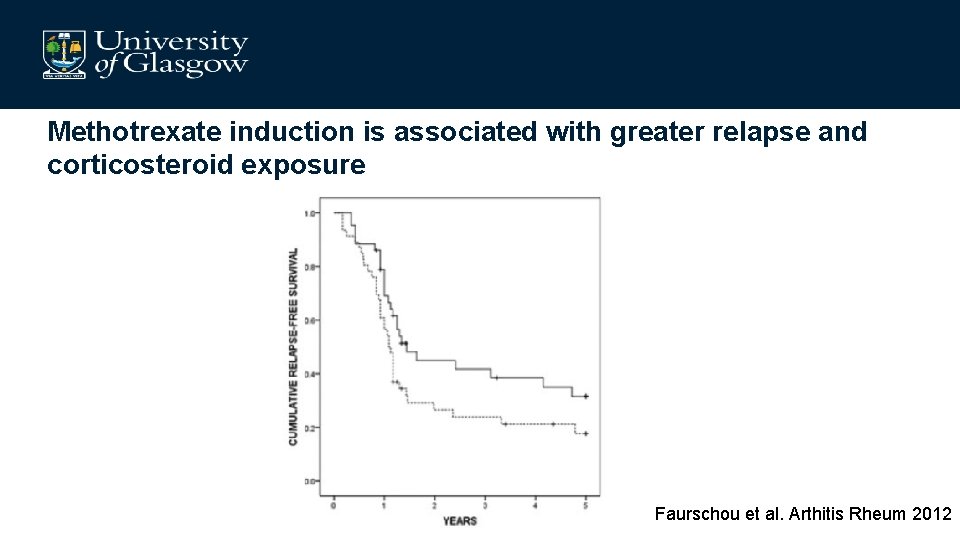
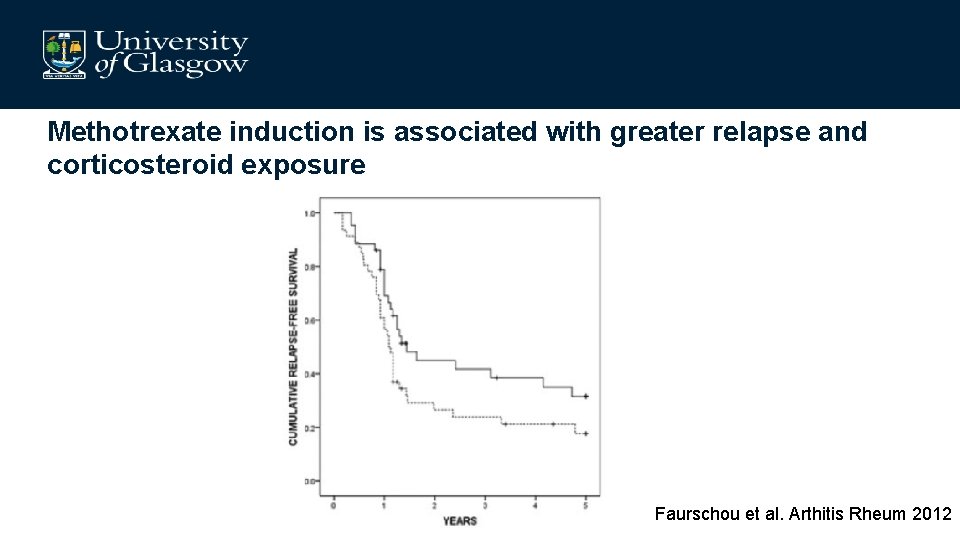
Methotrexate induction is associated with greater relapse and corticosteroid exposure Faurschou et al. Arthitis Rheum 2012
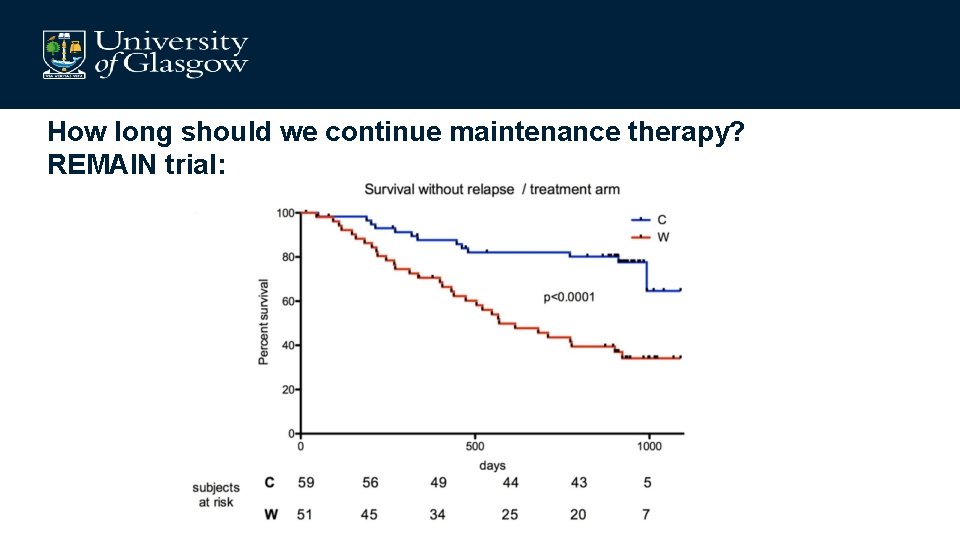
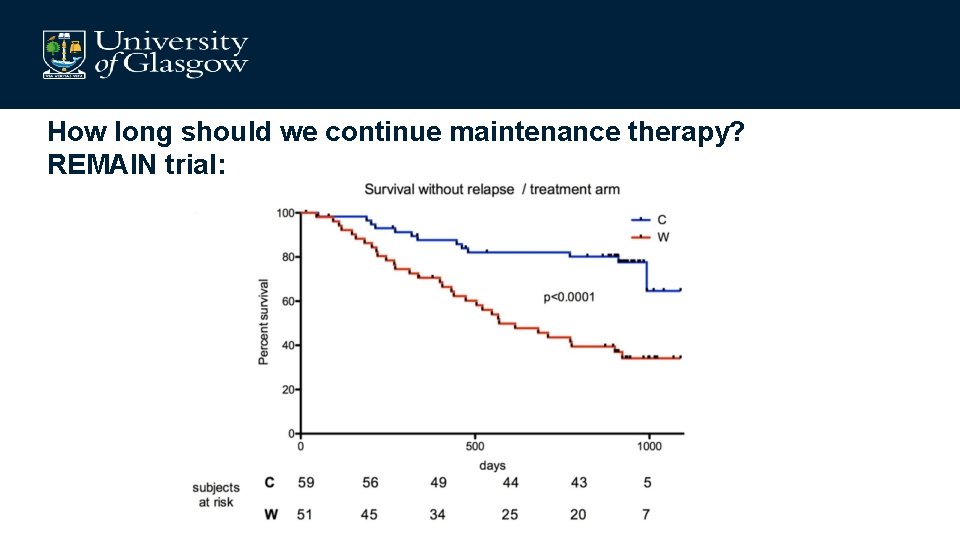
How long should we continue maintenance therapy? REMAIN trial:
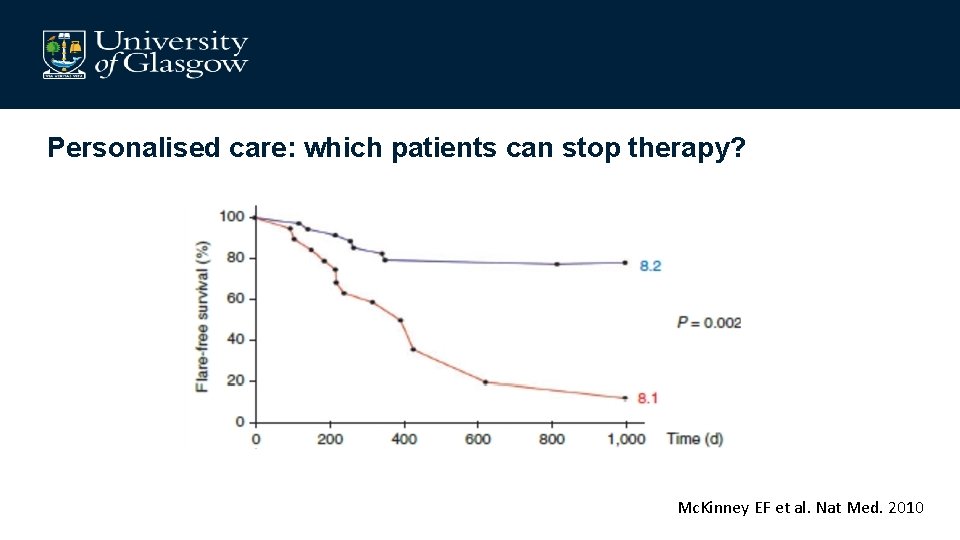
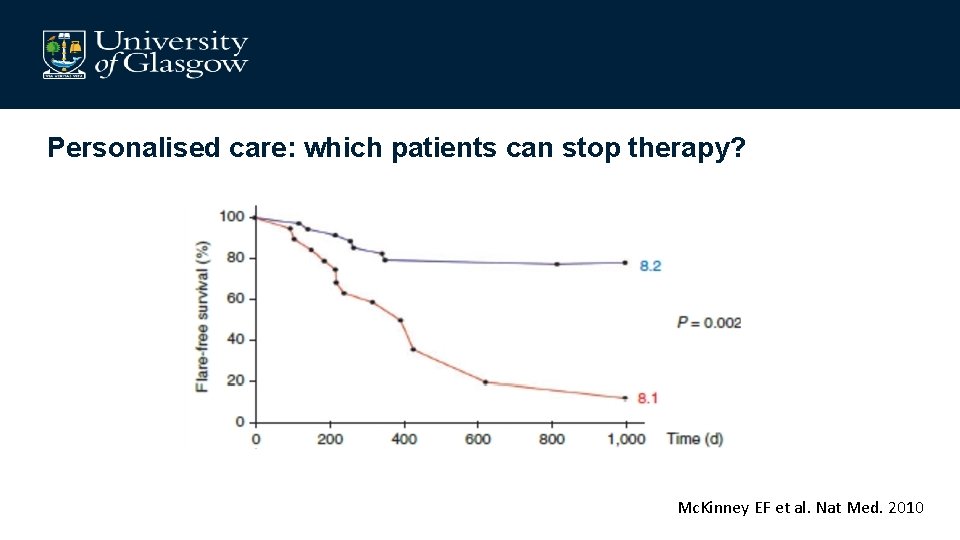
Personalised care: which patients can stop therapy? Mc. Kinney EF et al. Nat Med. 2010
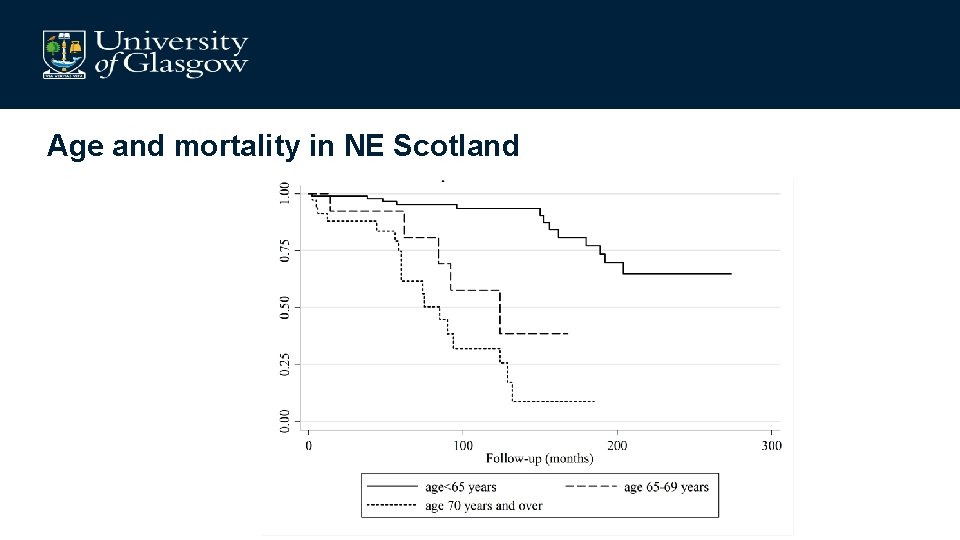
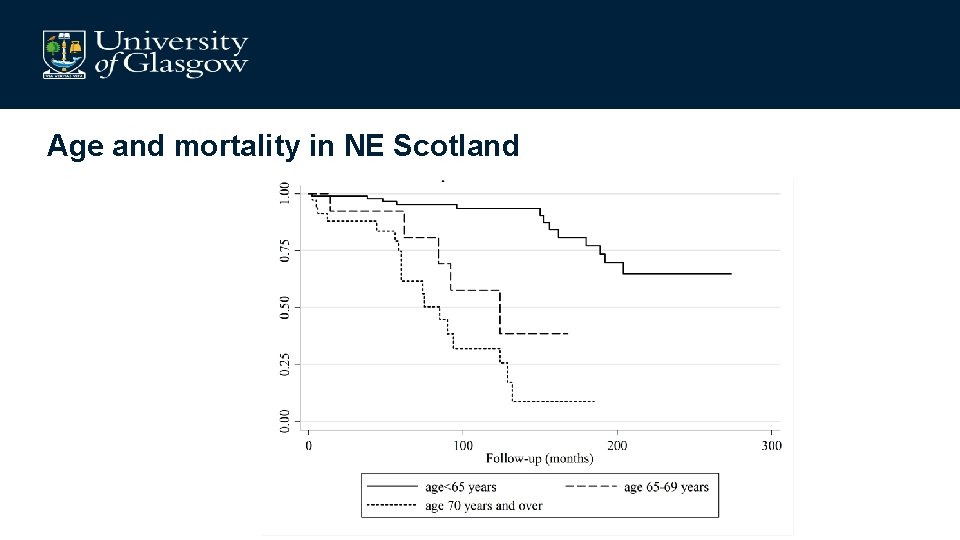
Age and mortality in NE Scotland
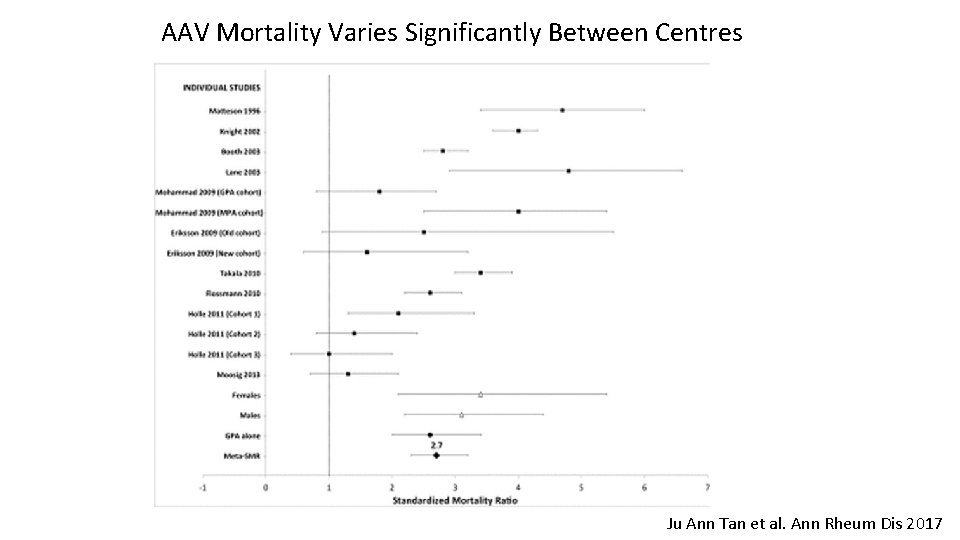
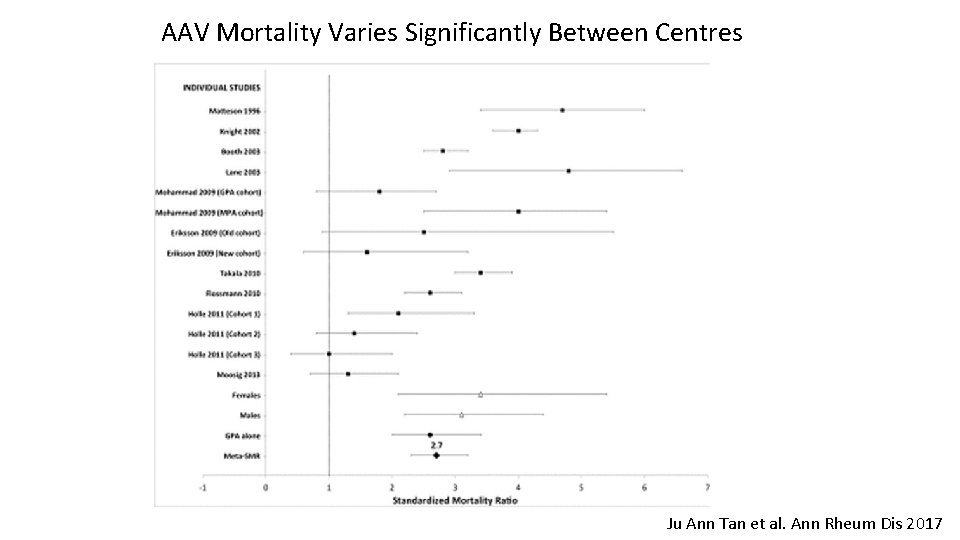
AAV Mortality Varies Significantly Between Centres Ju Ann Tan et al. Ann Rheum Dis 2017
AAV take aways • Refractory disease is unusual • Premature mortality remains an issue but is not primarily driven by active vasculitis • Comorbidities impact mortality and quality of life • Outcomes could be enhanced by: – – Minimising steroid exposure Reducing relapses Personalised management Optimising health service care pathways
Mr GS, 77 year old retired surveyor • PHx – Seronegative inflammatory arthritis controlled with MTX – Hypertension – Ex-smoker • 16 April ‘ 19 – Admitted with LRT-I – H. influenza and strep. pneumonia cultured from sputum – Discharged fit after 5/7
• 2 May’ 19, Ophthalmology review – Reduced visual acuity – Diplopia ? IV nerve palsy • 12 June ‘ 19, Neurology review – – – Mild R temple headache Jaw claudication PMR Night sweats ESR 130
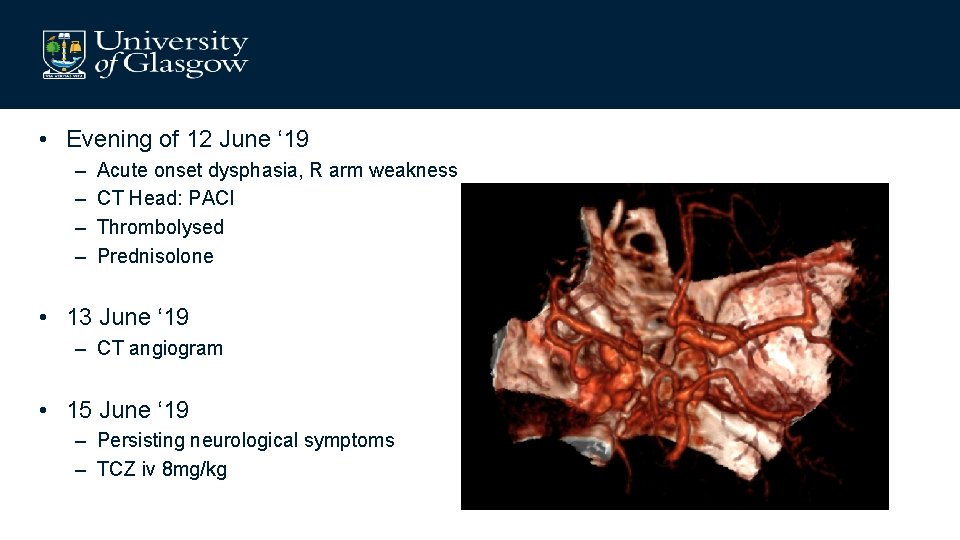
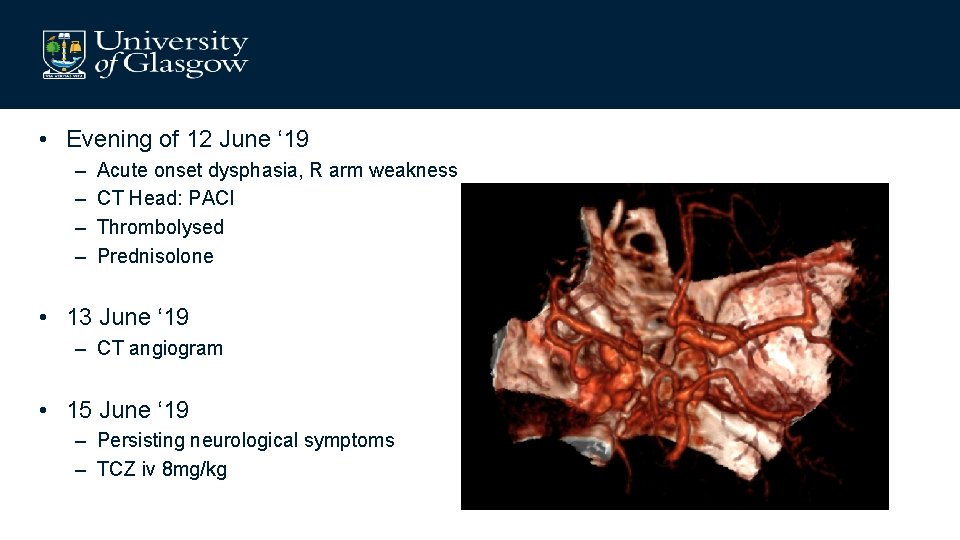
• Evening of 12 June ‘ 19 – – Acute onset dysphasia, R arm weakness CT Head: PACI Thrombolysed Prednisolone • 13 June ‘ 19 – CT angiogram • 15 June ‘ 19 – Persisting neurological symptoms – TCZ iv 8 mg/kg
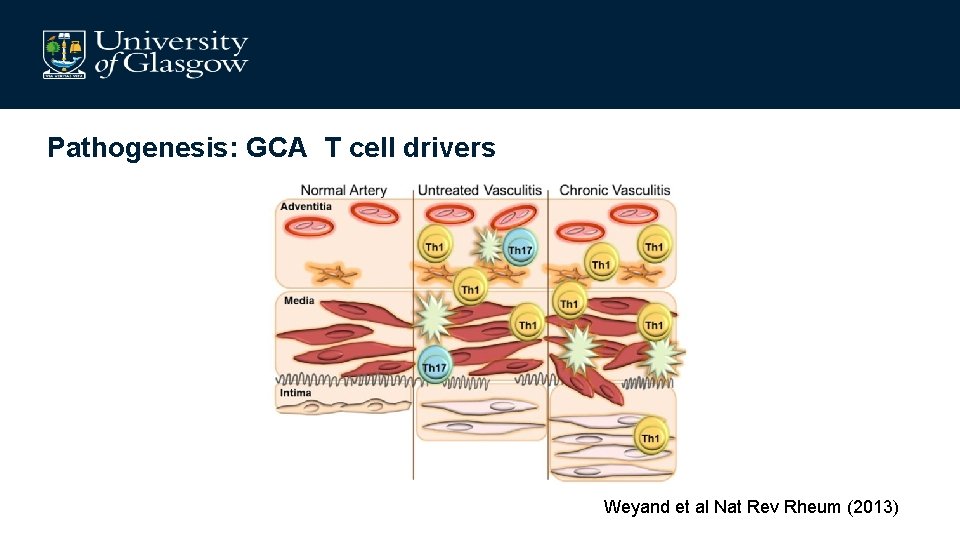
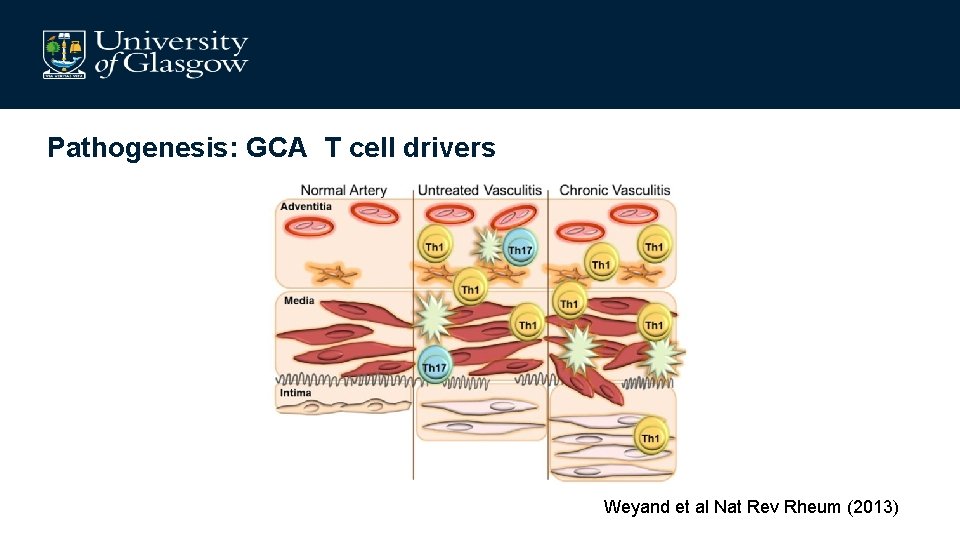
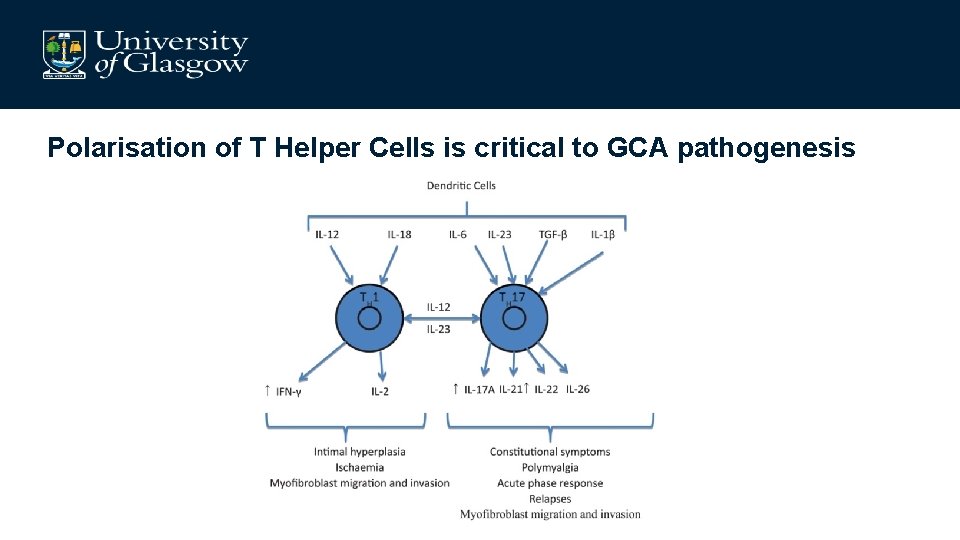
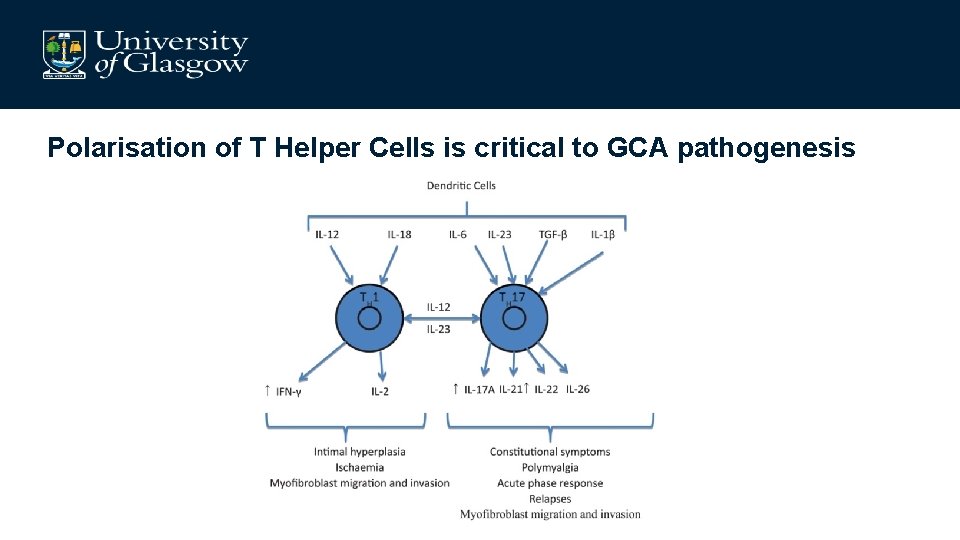
Pathogenesis: GCA T cell drivers Weyand et al Nat Rev Rheum (2013)
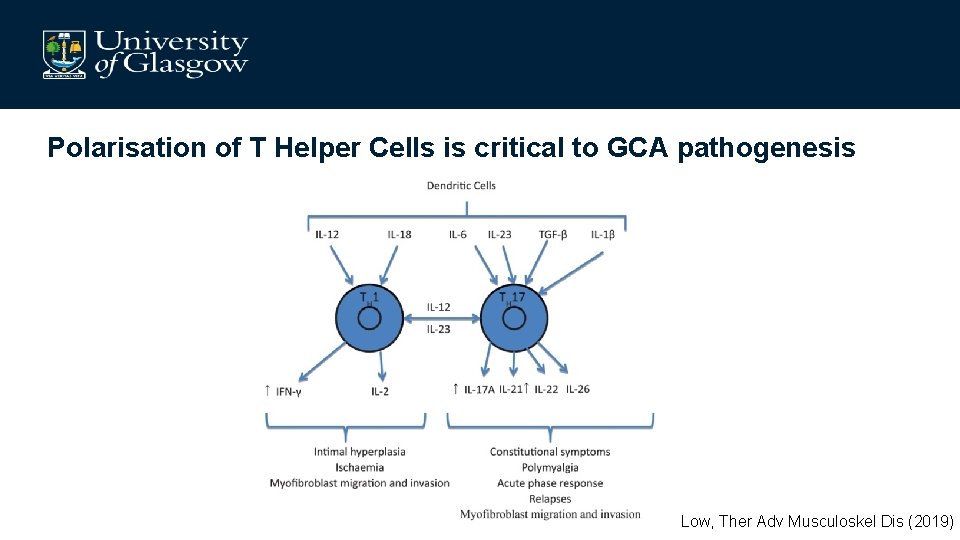
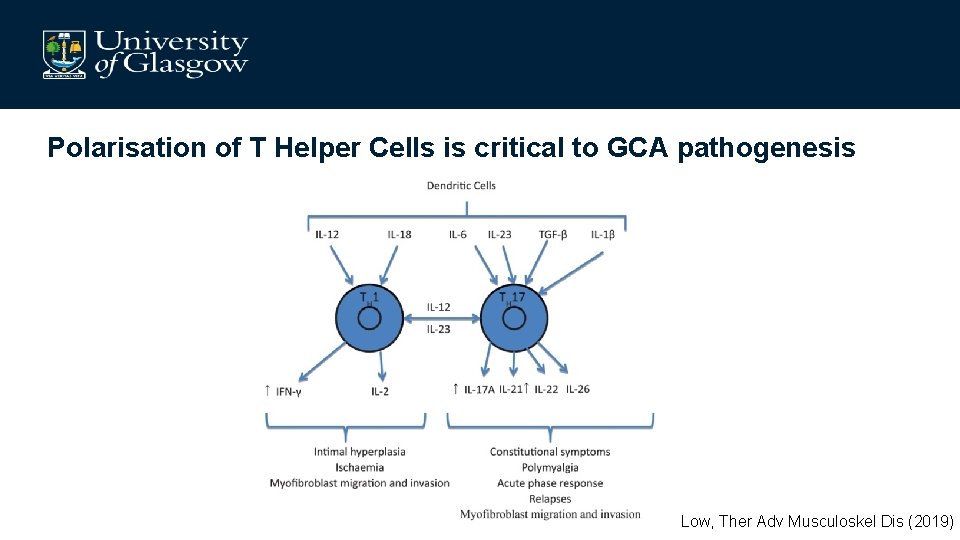
Polarisation of T Helper Cells is critical to GCA pathogenesis Low, Ther Adv Musculoskel Dis (2019)

Draft Giant Cell Arteritis Classification Criteria Inclusion Criteria: The following must be met to be considered for classification q Diagnosis of vasculitis q ≥ 50 years of age at time of diagnosis Criteria: ≥ 6 points meets threshold for classification Laboratory Findings Clinical Features Morning stiffness in shoulders or neck Sudden visual loss Jaw or tongue claudication New temporal headache Scalp tenderness +2 +2 +2 Temporal Vascular Exam Artery Exam Findings Reduced pulse, ‘cord-like’, or tenderness +1 ESR ≥ 50 mm/hour or CRP ≥ 10 mg/L +3 Temporal Artery Biopsy Definite vasculitis +5 Imaging Findings Temporal artery halo sign (US) Bilateral axillary involvement FDG-PET activity throughout aorta +5 +3 +3
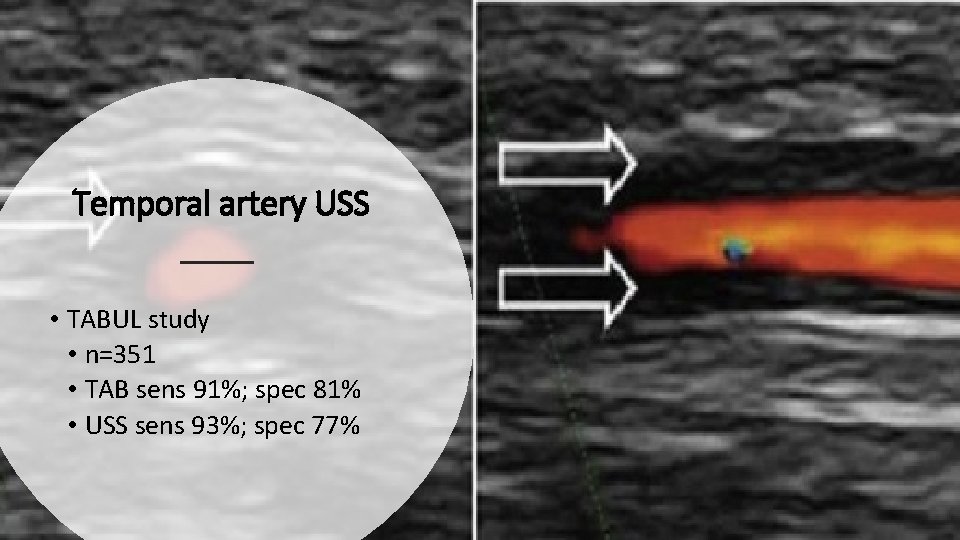
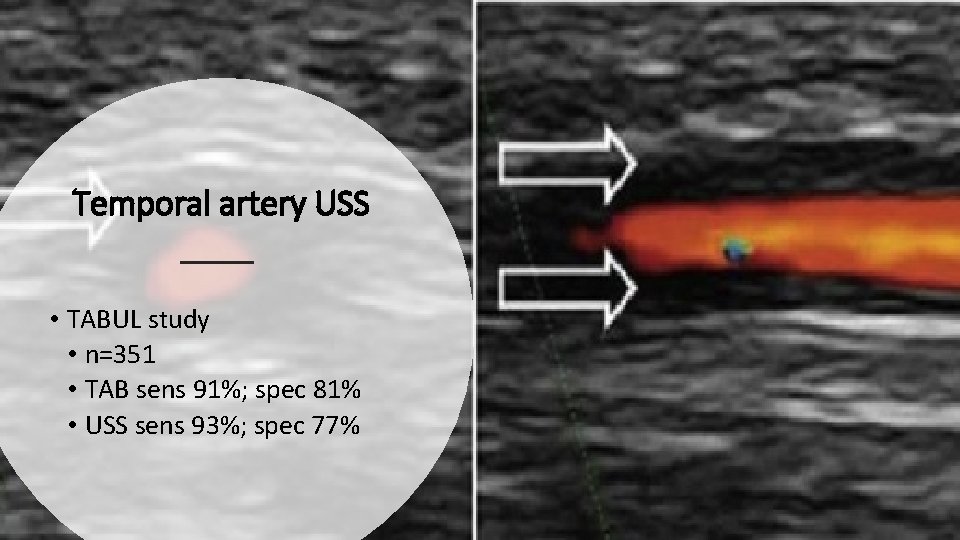
Temporal artery USS • TABUL study • n=351 • TAB sens 91%; spec 81% • USS sens 93%; spec 77%
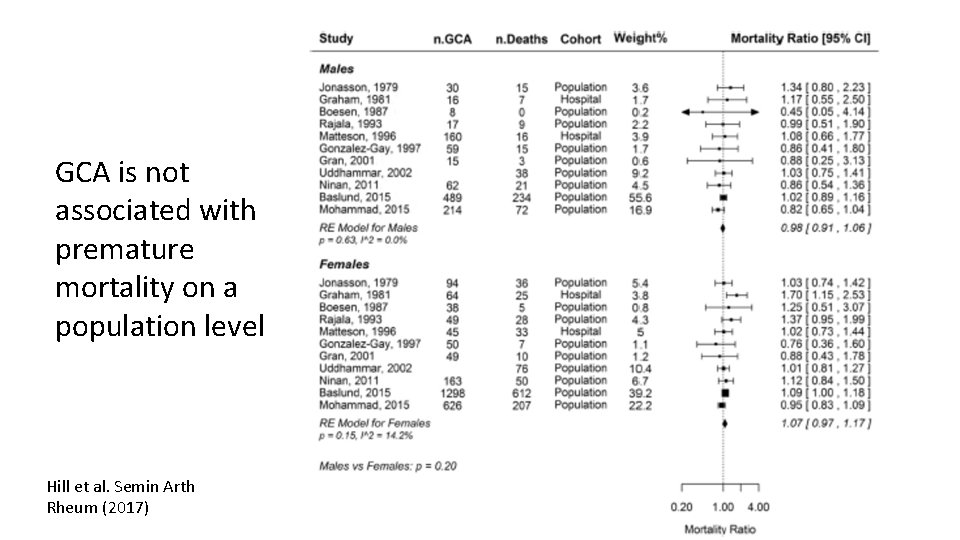
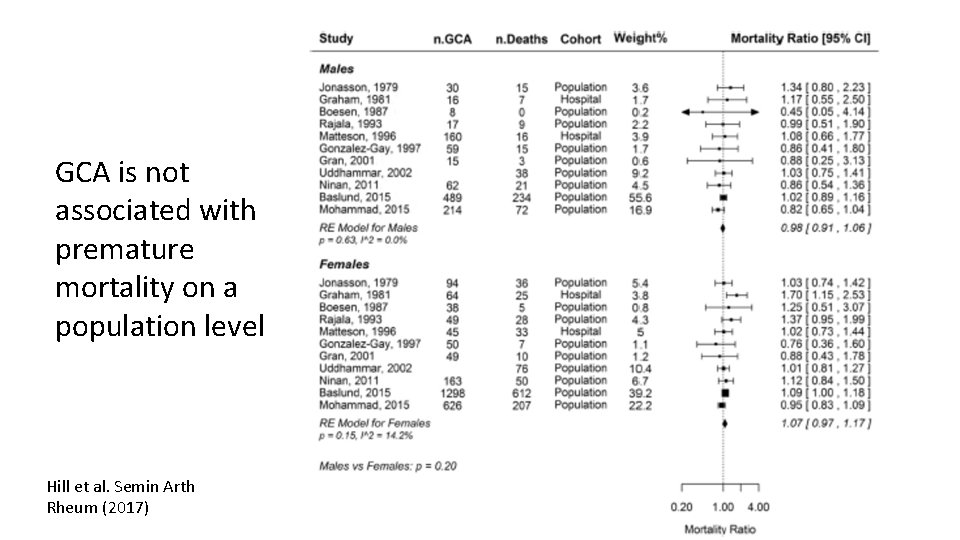
GCA is not associated with premature mortality on a population level Hill et al. Semin Arth Rheum (2017)
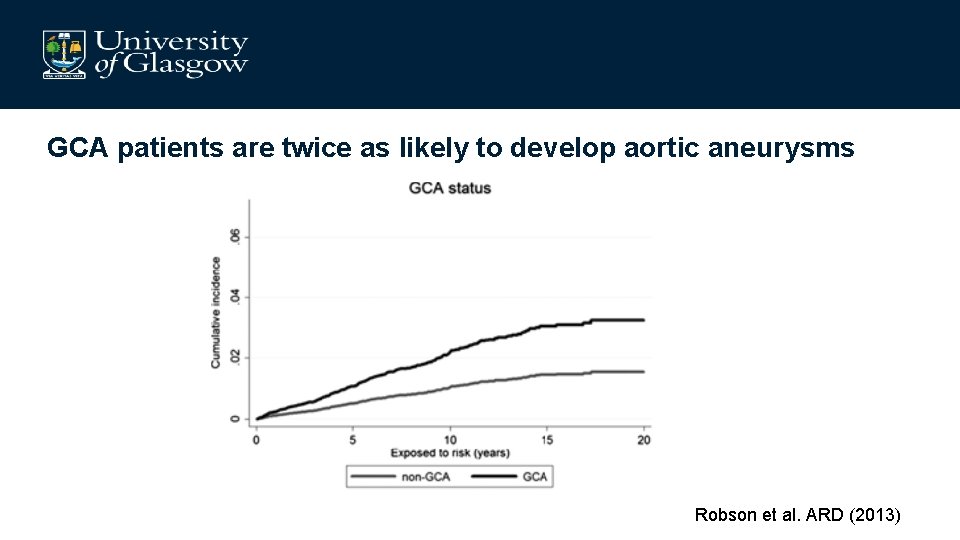
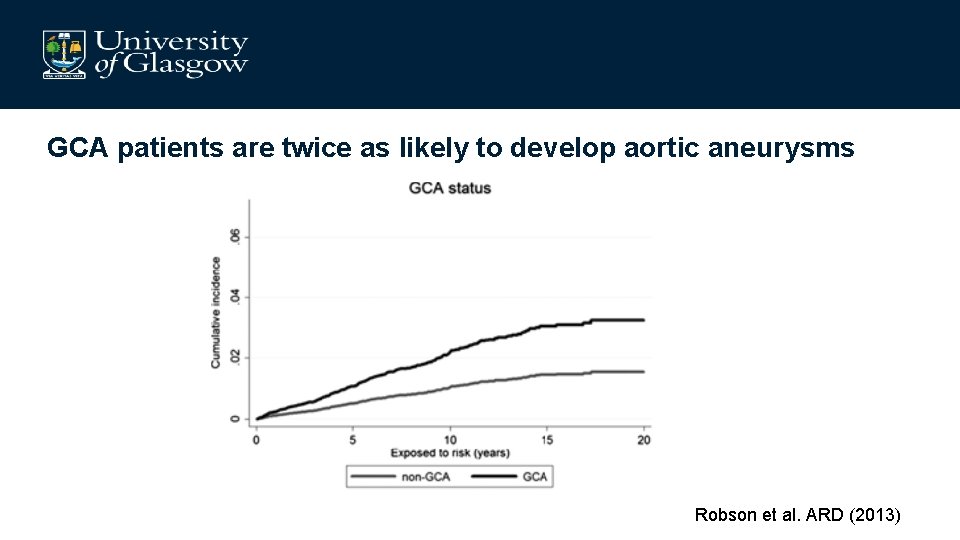
GCA patients are twice as likely to develop aortic aneurysms Robson et al. ARD (2013)
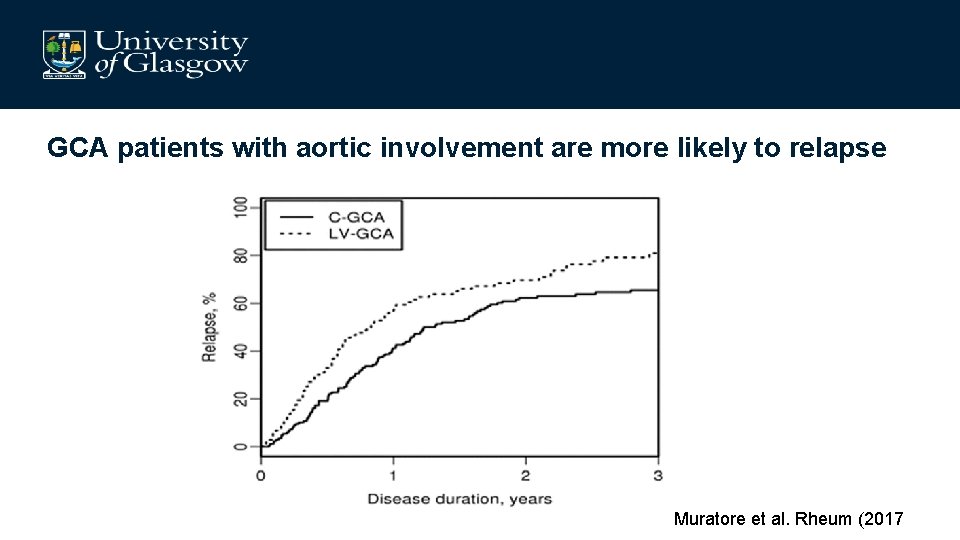
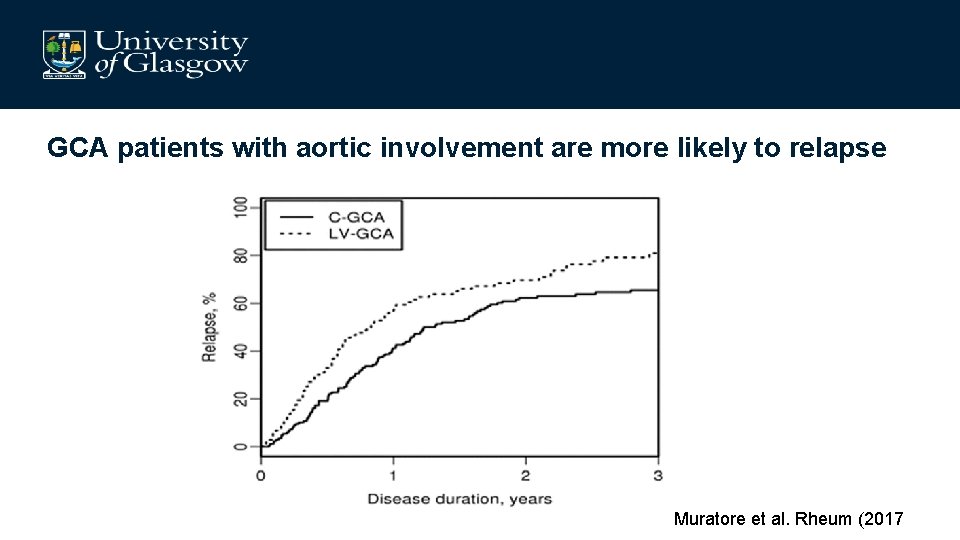
GCA patients with aortic involvement are more likely to relapse Muratore et al. Rheum (2017
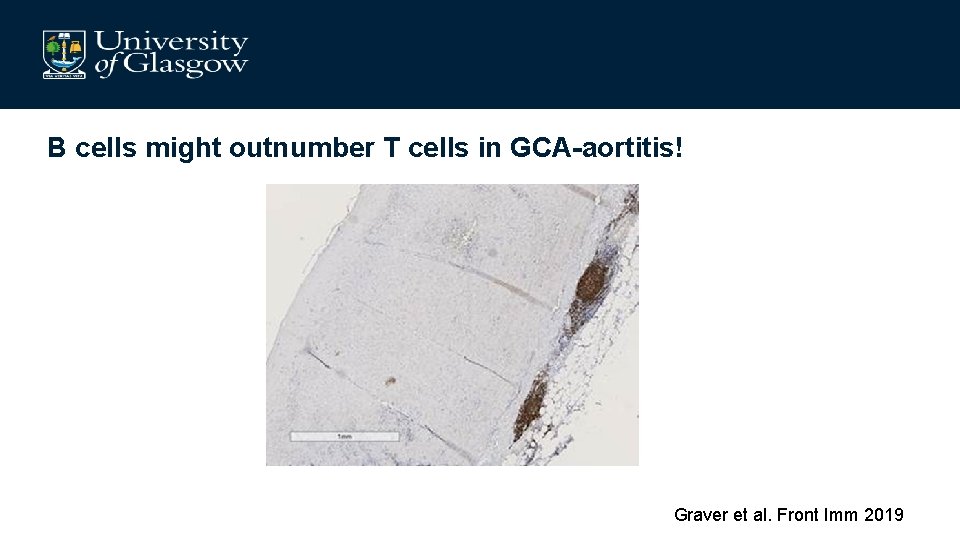
B cells might outnumber T cells in GCA-aortitis! Graver et al. Front Imm 2019
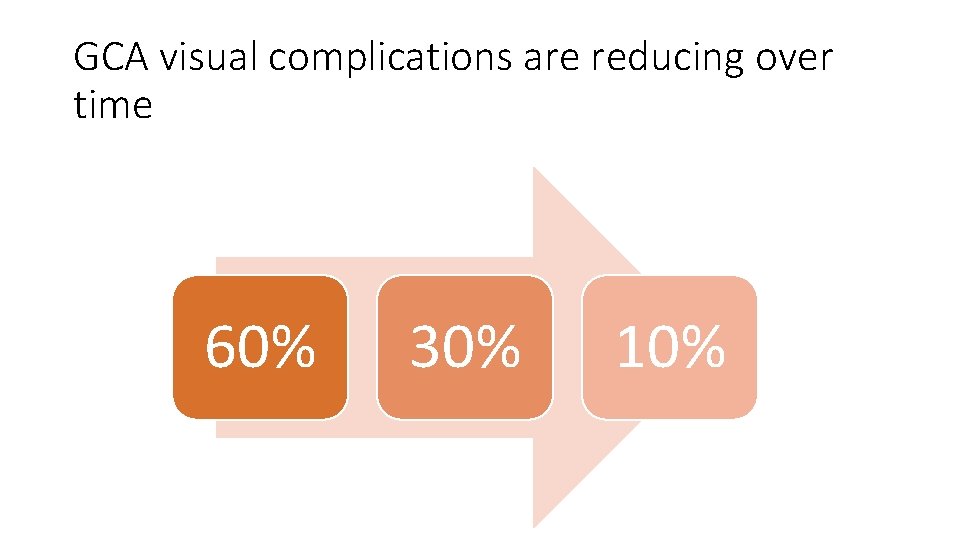
GCA visual complications are reducing over time 60% 30% 10%
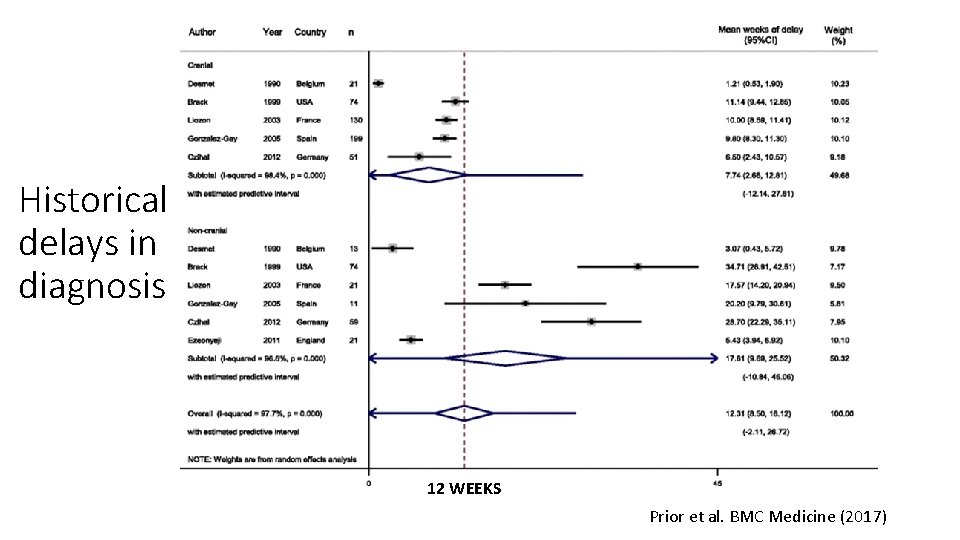
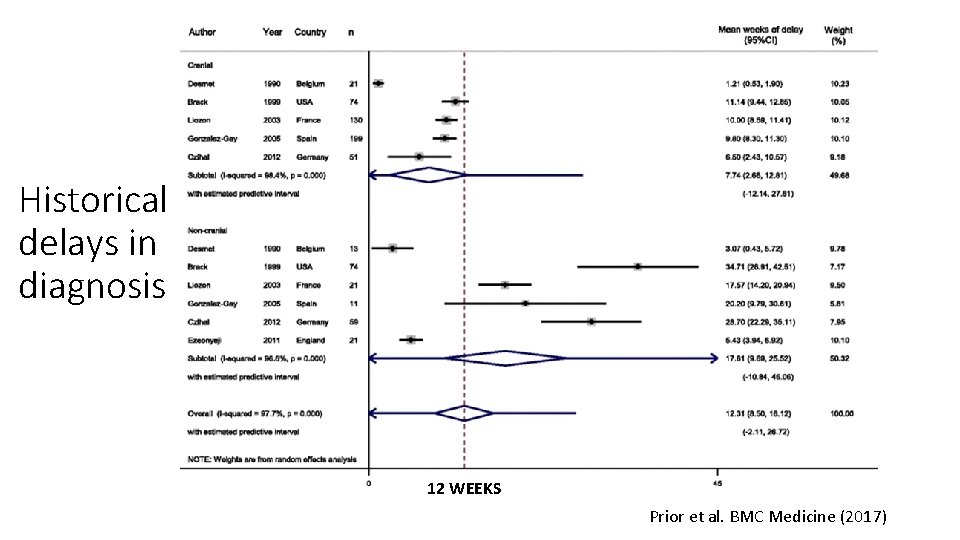
Historical delays in diagnosis 12 WEEKS Prior et al. BMC Medicine (2017)
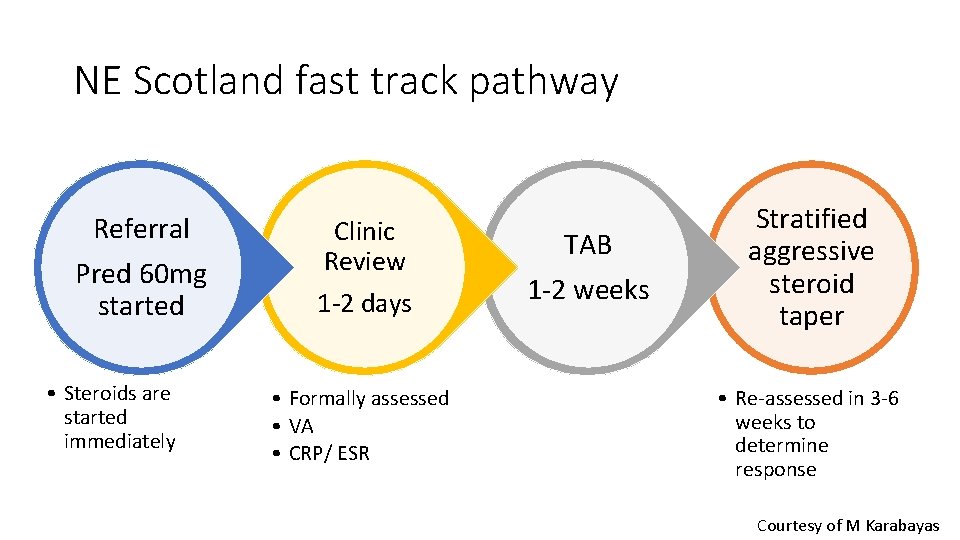
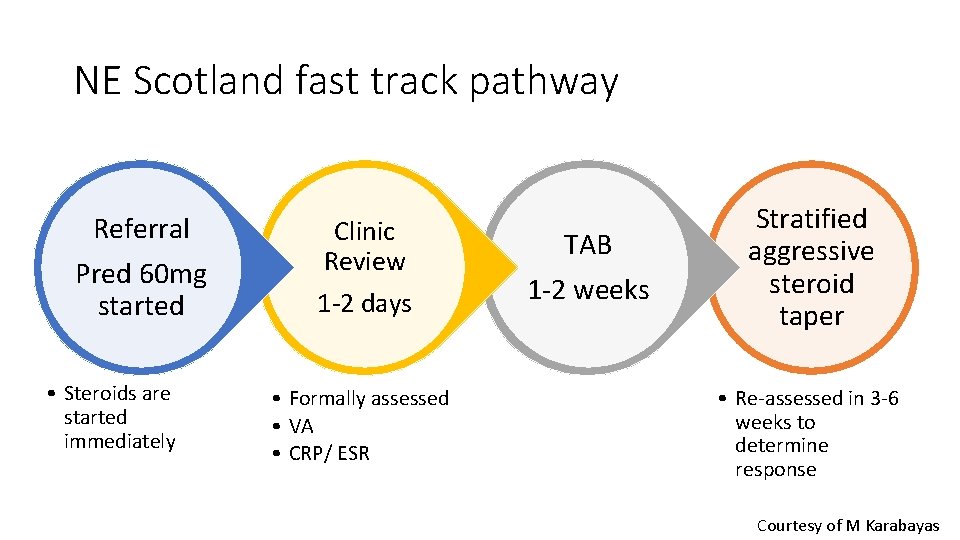
NE Scotland fast track pathway Referral Pred 60 mg started • Steroids are started immediately Clinic Review 1 -2 days • Formally assessed • VA • CRP/ ESR TAB 1 -2 weeks Stratified aggressive steroid taper • Re-assessed in 3 -6 weeks to determine response Courtesy of M Karabayas
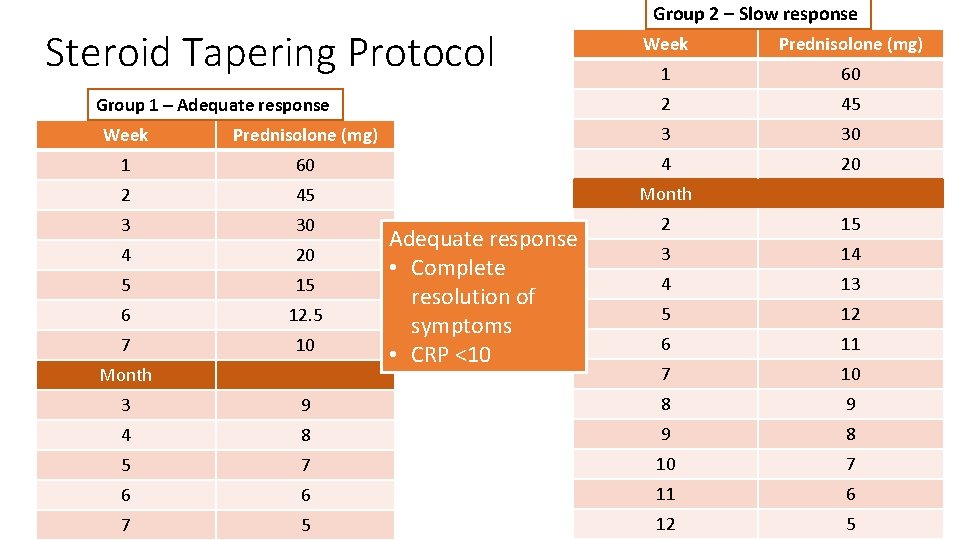
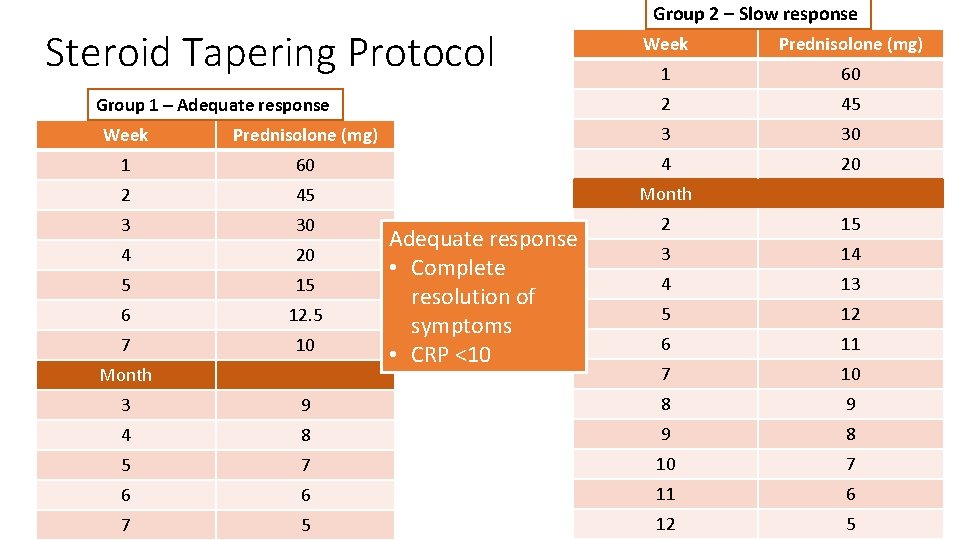
Steroid Tapering Protocol Group 1 – Adequate response Group 2 – Slow response Week Prednisolone (mg) 1 60 2 45 Week Prednisolone (mg) 3 30 1 60 4 20 2 45 Month 3 30 2 15 4 20 3 14 5 15 4 13 6 12. 5 5 12 7 10 6 11 7 10 Month Adequate response • Complete resolution of symptoms • CRP <10 3 9 8 9 4 8 9 8 5 7 10 7 6 6 11 6 7 5 12 5
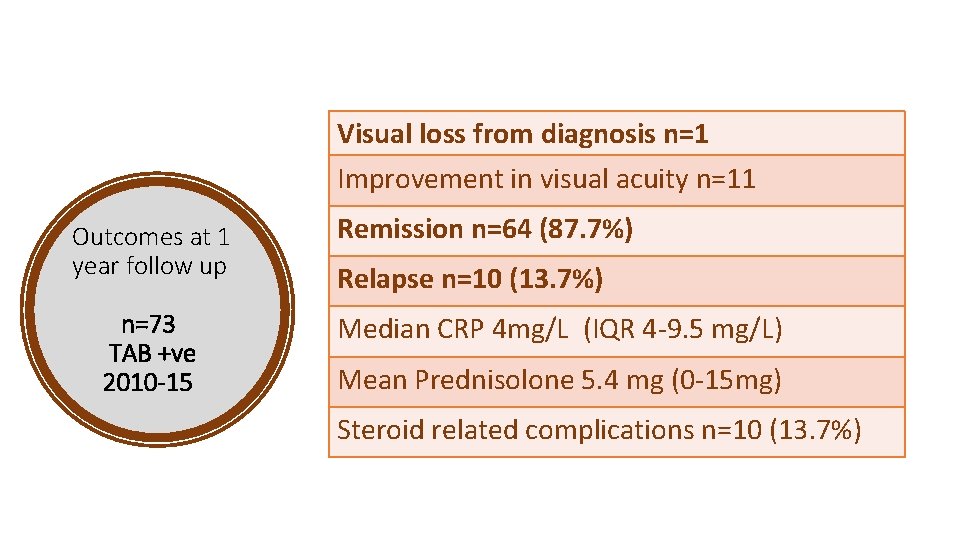
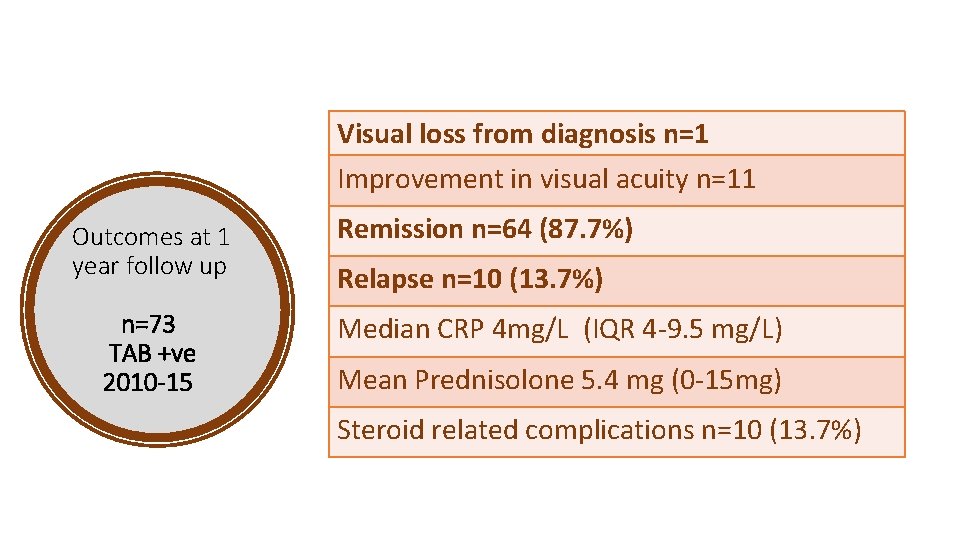
Visual loss from diagnosis n=1 Improvement in visual acuity n=11 Outcomes at 1 year follow up n=73 TAB +ve 2010 -15 Remission n=64 (87. 7%) Relapse n=10 (13. 7%) Median CRP 4 mg/L (IQR 4 -9. 5 mg/L) Mean Prednisolone 5. 4 mg (0 -15 mg) Steroid related complications n=10 (13. 7%)
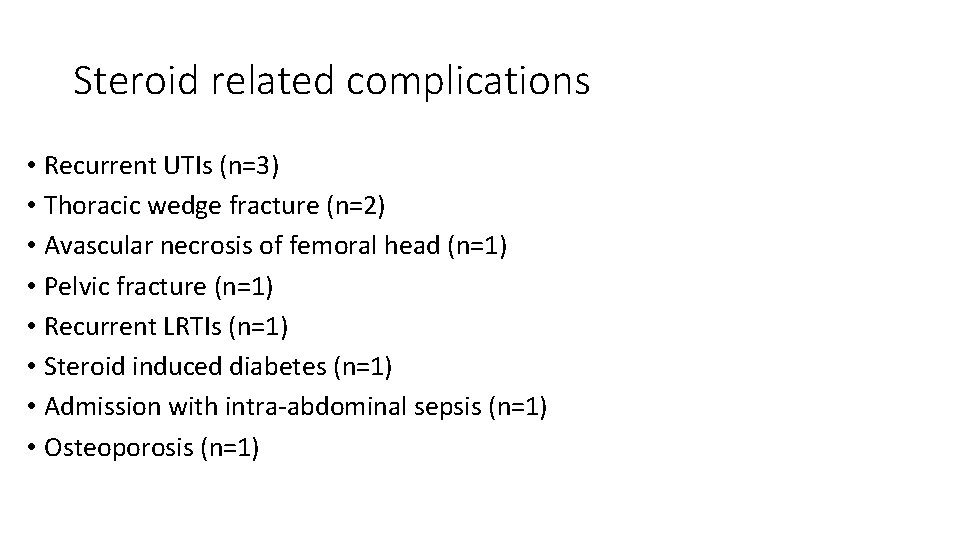
Steroid related complications • Recurrent UTIs (n=3) • Thoracic wedge fracture (n=2) • Avascular necrosis of femoral head (n=1) • Pelvic fracture (n=1) • Recurrent LRTIs (n=1) • Steroid induced diabetes (n=1) • Admission with intra-abdominal sepsis (n=1) • Osteoporosis (n=1)
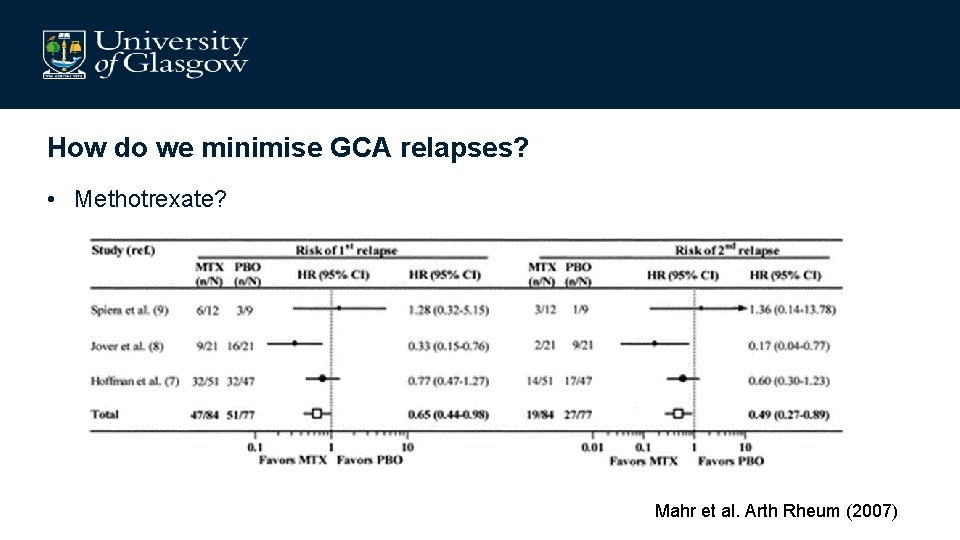
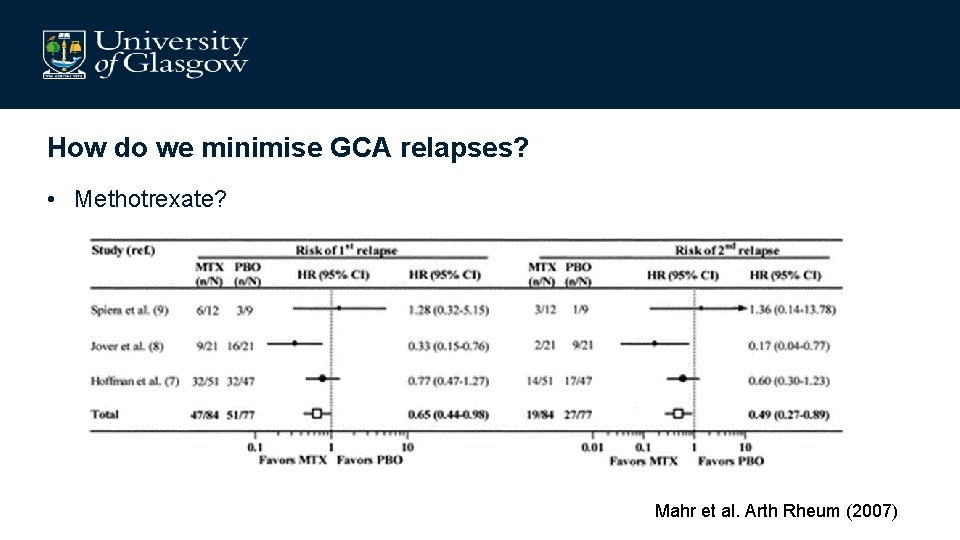
How do we minimise GCA relapses? • Methotrexate? Mahr et al. Arth Rheum (2007)
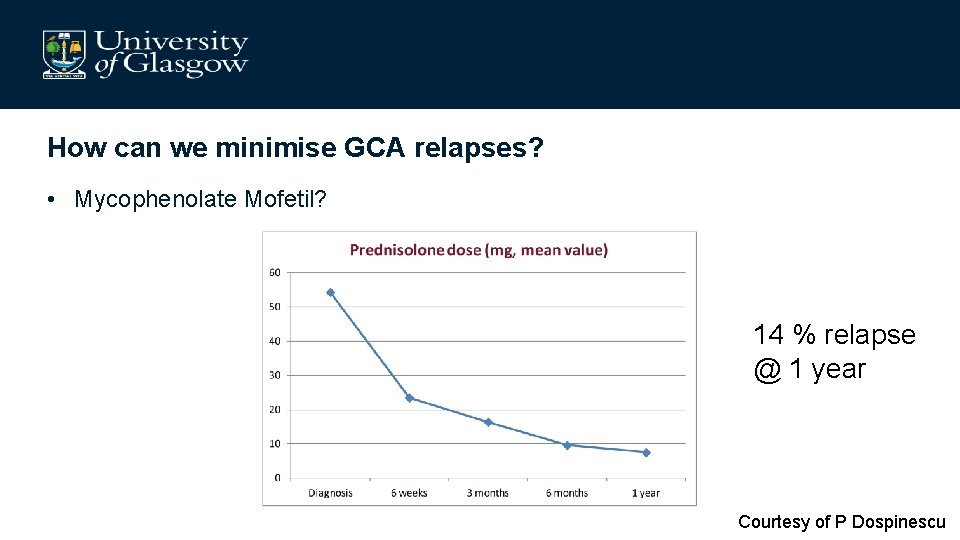
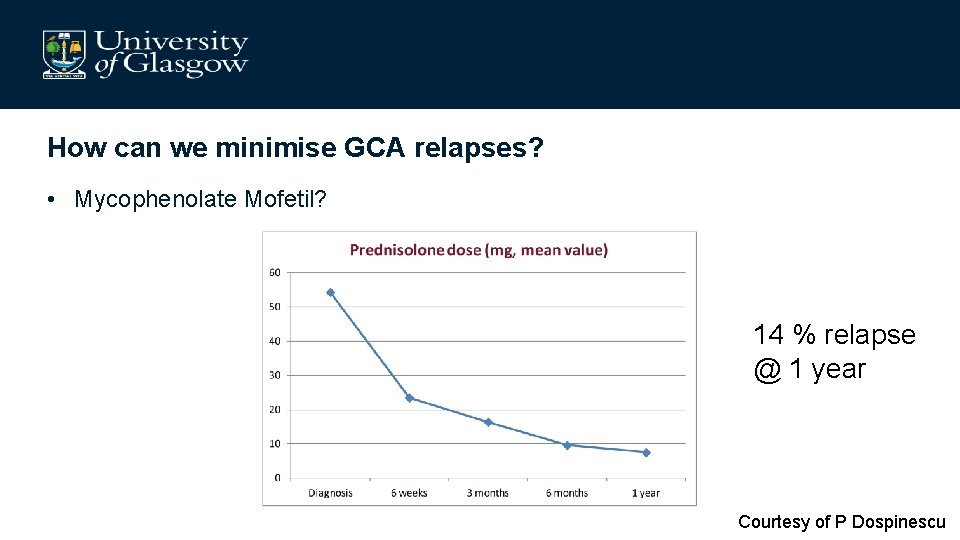
How can we minimise GCA relapses? • Mycophenolate Mofetil? 14 % relapse @ 1 year Courtesy of P Dospinescu
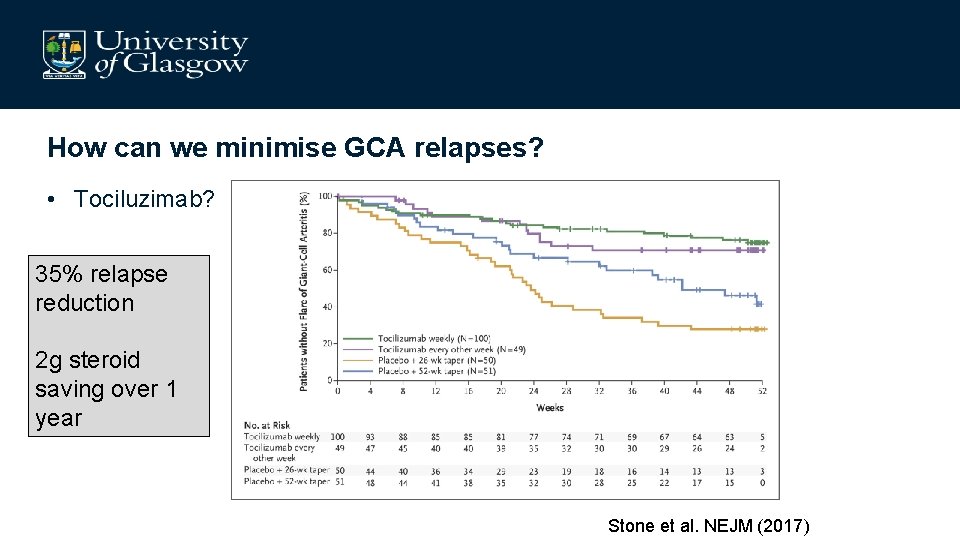
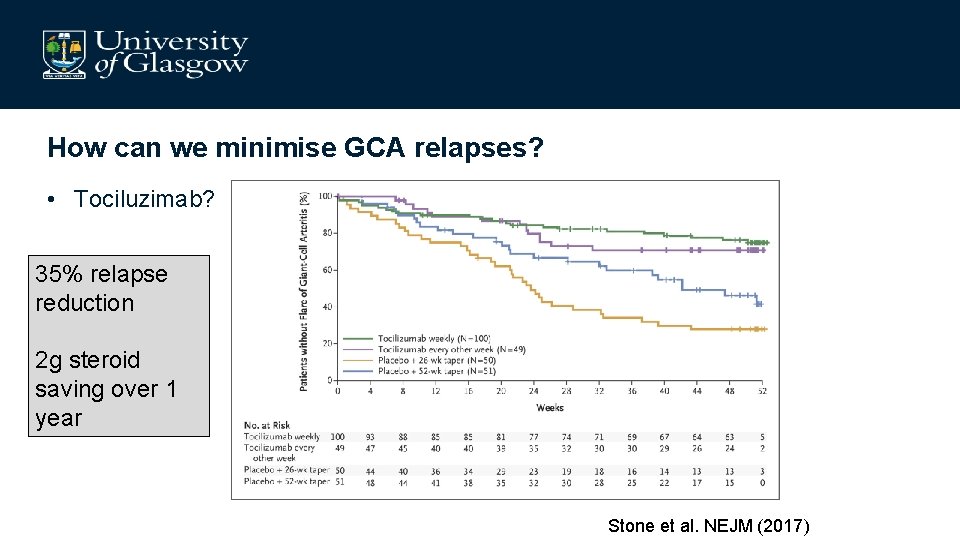
How can we minimise GCA relapses? • Tociluzimab? 35% relapse reduction 2 g steroid saving over 1 year Stone et al. NEJM (2017)
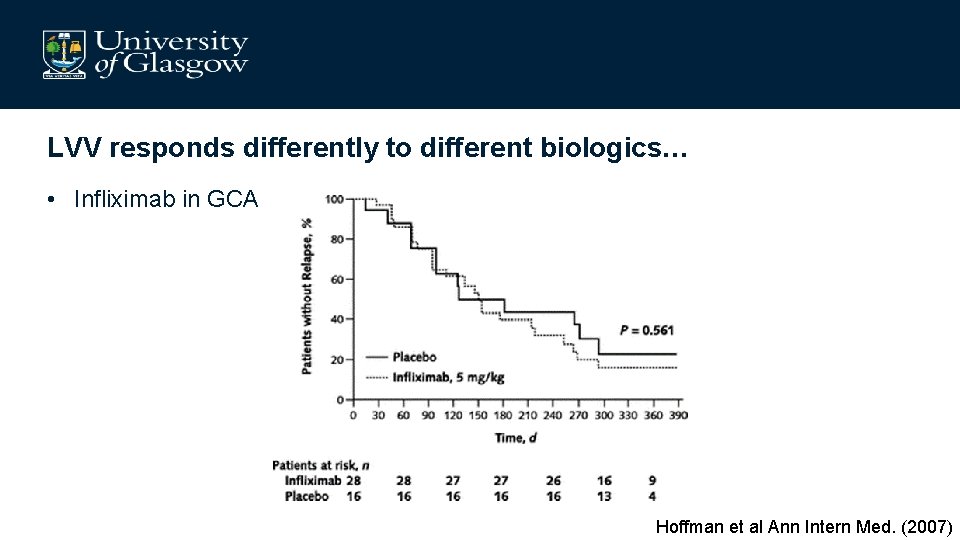
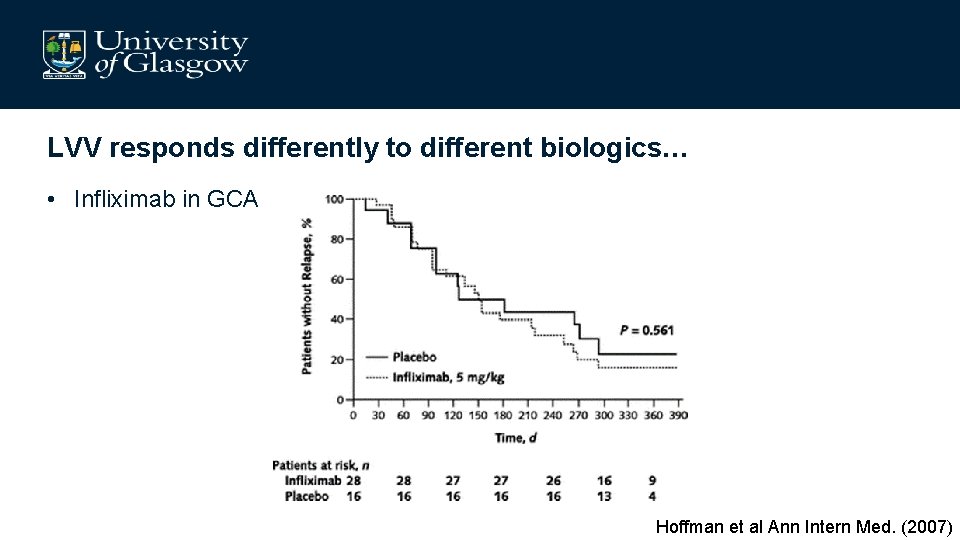
LVV responds differently to different biologics… • Infliximab in GCA Hoffman et al Ann Intern Med. (2007)
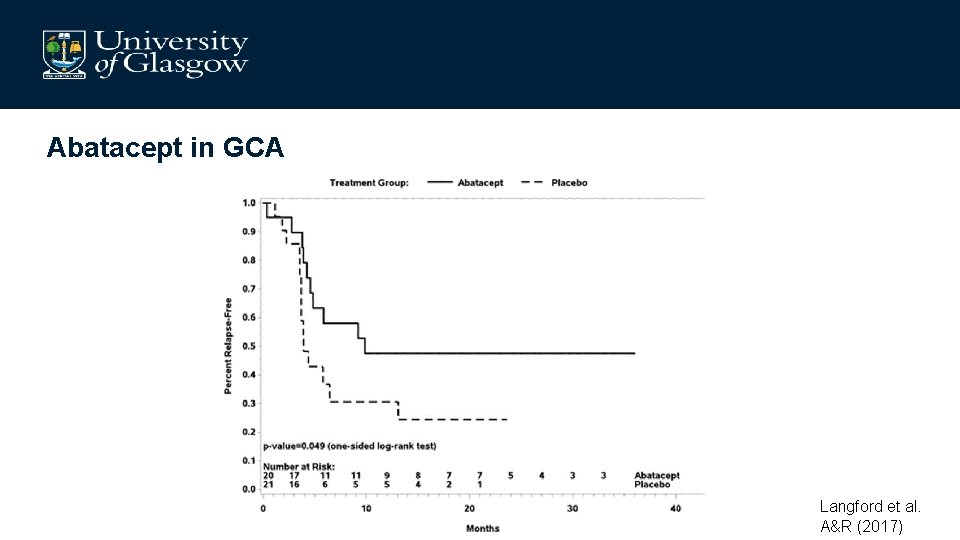
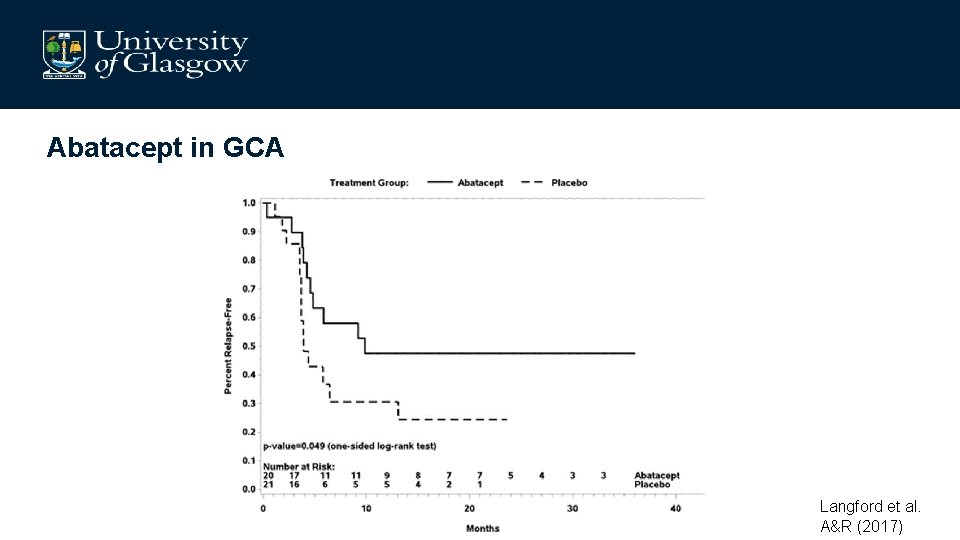
Abatacept in GCA Langford et al. A&R (2017)
Polarisation of T Helper Cells is critical to GCA pathogenesis
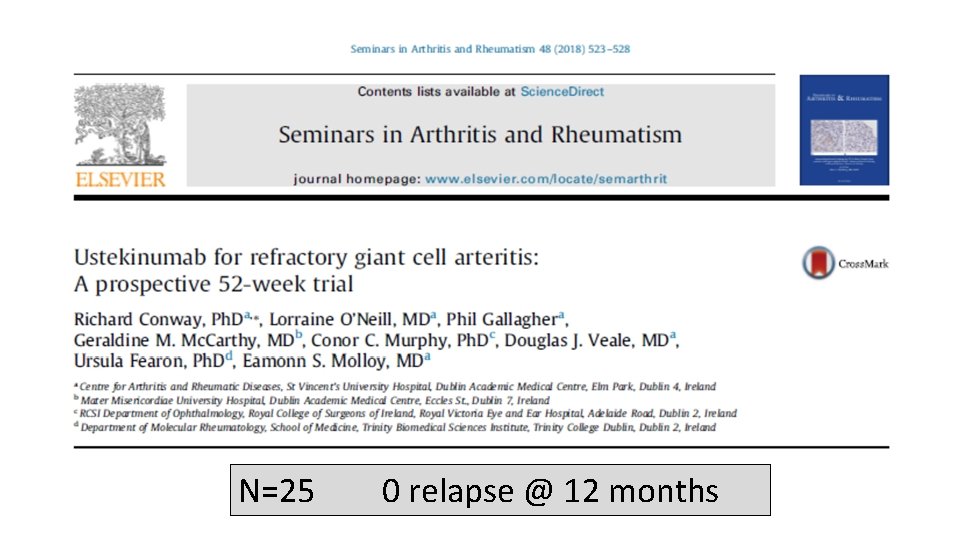
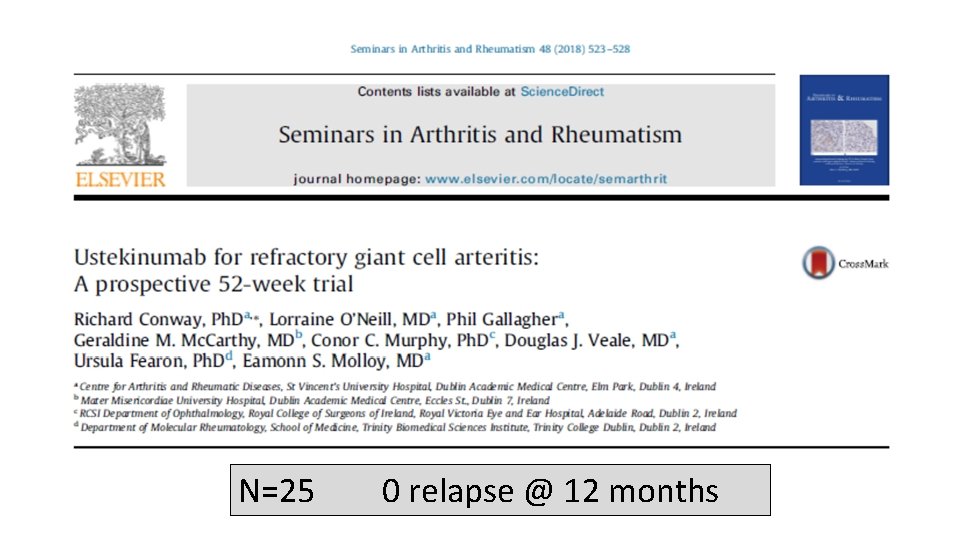
N=25 0 relapse @ 12 months
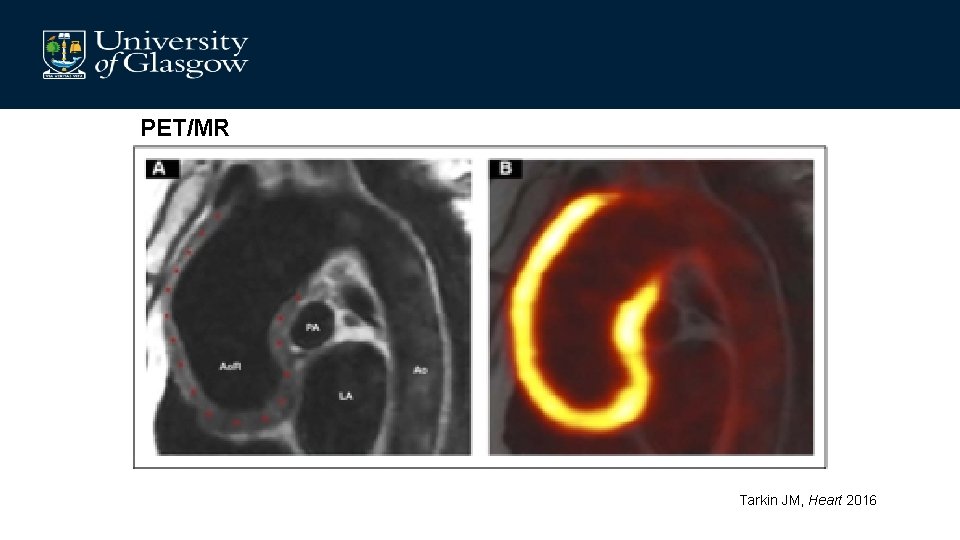
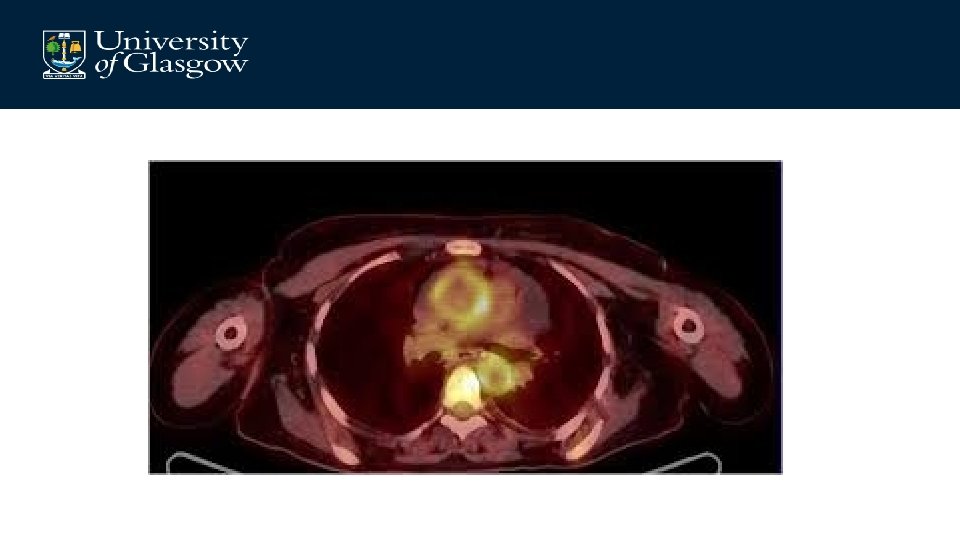
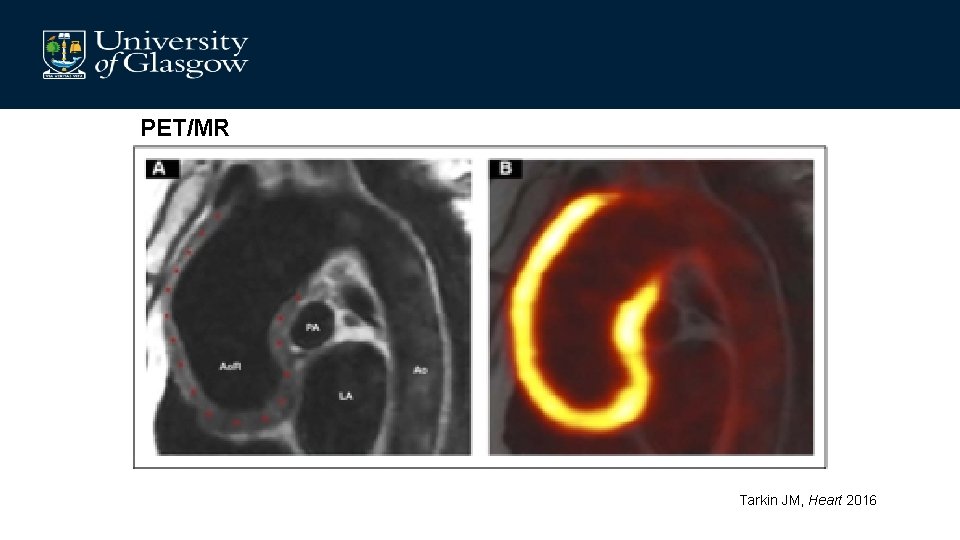
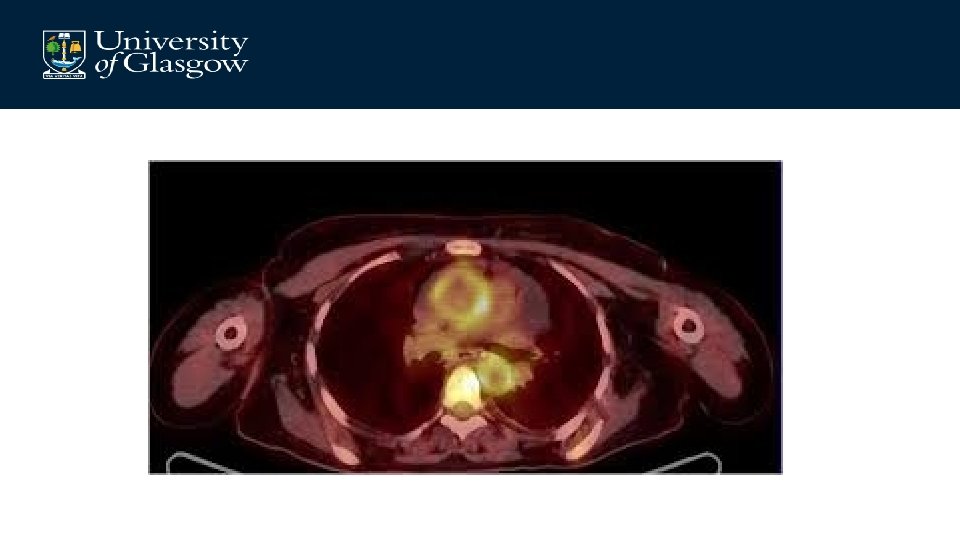
PET/MR Tarkin JM, Heart 2016
GCA take-aways • Th 1 based therapies require investigation to induce full remission • Diagnostic methods require optimisation • Monitoring biomarkers required • Biological differentiation of cranial v aortic GCA increasingly recognised – Towards therapeutic stratification?

Acknowledgements – – – Dr Shifa Sarcia Prof Corri Black Dr Angharad Mark Dr John Mc. Laren Dr Lucy Mc. Geoch Dr Jan Sznajd Dr Bean Dhaun Dr Eve Miller-Hodges Dr Nicole Amft Dr Vinod Kumar Prof Lars Erwig • Dr Dana Kidder • Dr Nick Fluck • Dr Paula Dospinescu • Dr Maira Karabayas • Mrs Gayle Hutcheon • Dr Dan Pugh • Dr Laura Mc. Gregor