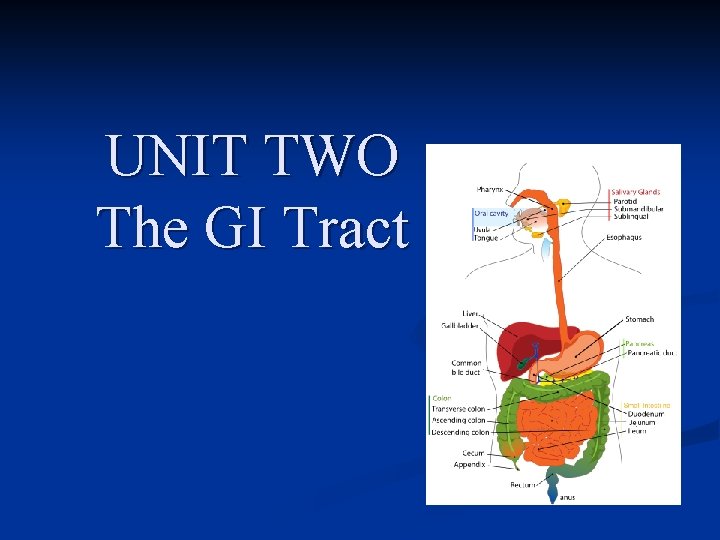
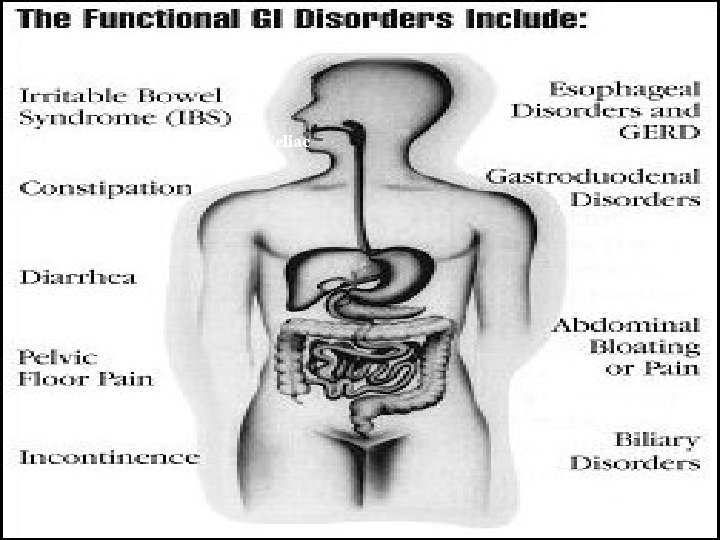
UNIT TWO The GI Tract GastroIntestinal Tract Disorders



- Slides: 121
UNIT TWO The GI Tract
Gastro-Intestinal Tract & Disorders
Objectives • • • Review the A&P of the GI system Discuss the significance of vitamins and our ability to absorb them Describe oral infections/inflammations and the nursing care. Discuss the pathophysiology of esophageal disorders and the treatment /nursing care (i. e. GERD, hiatal hernia) Discuss the pathophysiology of disorders of the stomach and upper small intestine (i. e. gastritis, upper GI bleed, peptic ulcer disease).
Selected Readings In Your text chapters 34, 35, 36, 37 n Readings from your syllabus n
Can you imagine: • • • Not to be able to eat anything with wheat in it? What condition? What it is like to live with an esophageal sphincter not closing? What condition? Living with part of your stomach in your esophagus? Being incontinent of stool or continuous diarrhea? Open Sores over your lips on most important occasions. . .
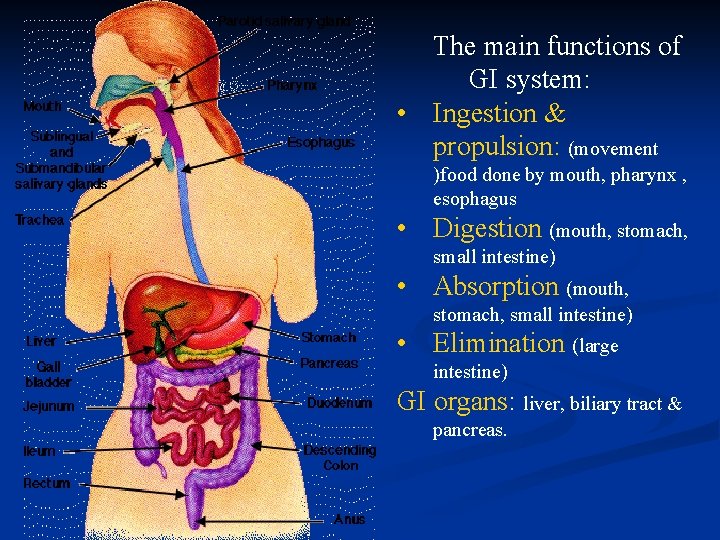
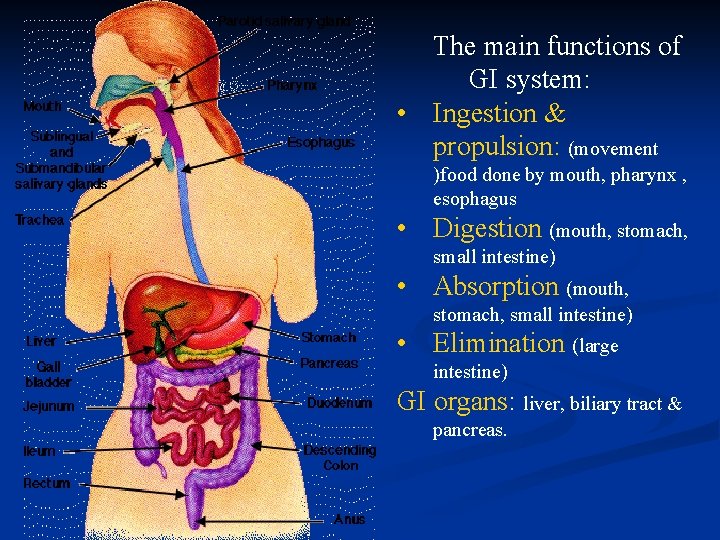
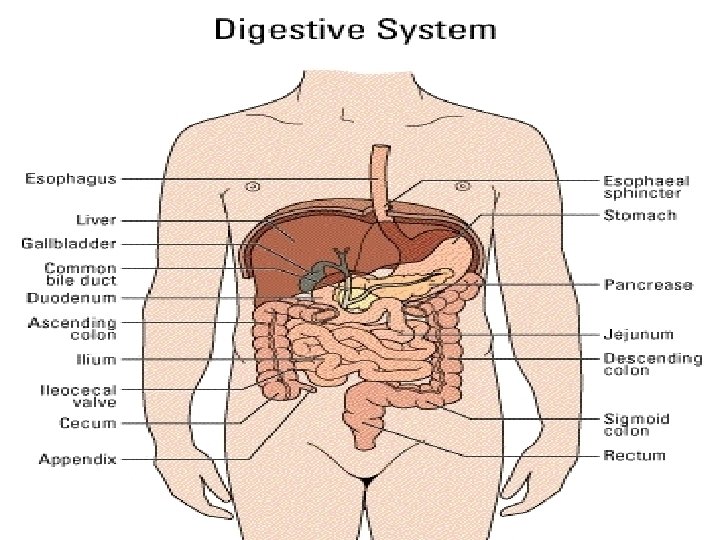
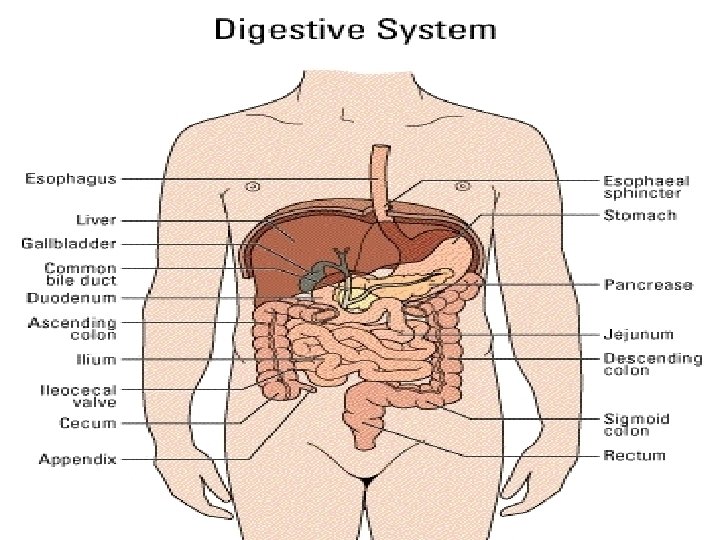
The main functions of GI system: • Ingestion & propulsion: (movement )food done by mouth, pharynx , esophagus • Digestion (mouth, stomach, small intestine) • Absorption (mouth, stomach, small intestine) • Elimination (large intestine) GI organs: liver, biliary tract & pancreas.
Mouth & Ulcerative Colitis /Crohn’s &Celiac
Food & GI System: Food generally takes about four hours to make it from the mouth to the end of the small intestine. The non-digested residue normally spends one to three days in the large intestine but can be there for seven days. Foods high in insoluble fiber (whole grains, wheat and corn brans, some vegetables) speedup intestinal transit. This is desirable because it prevents constipation, hemorrhoids, and diverticular disease.
Vitamins Fat Soluble (stored & need fat for absorption): • A: vision (fish, fruit, veg) • D: bone (dairy products esp calcium) • E: Antitoxins (dairy) • K: Blood clotting (milk, gr leafy veg) Water Soluble (not stored): • C: Connective tissue ascorbic acid, citrus, gr veg, tomatoes, broccoli • B 1, B 2, B 6, B 12: energy, lips, GI, RBC, heart, skin, gait, eyes synthesis DNA/RNA (meat veg, dairy products) NB: Vitamin B 12 needs intrinsic factor
Vitamin B 12 • • • Acts as antitoxidant Essential to formation of the protein collagen facilitates iron absorption facilitates cholesterol conversion to bile acids essential to serotonin synthesis
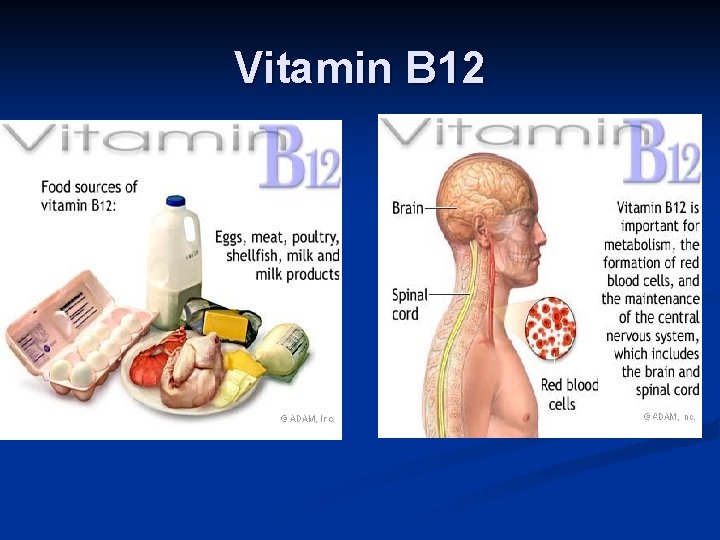
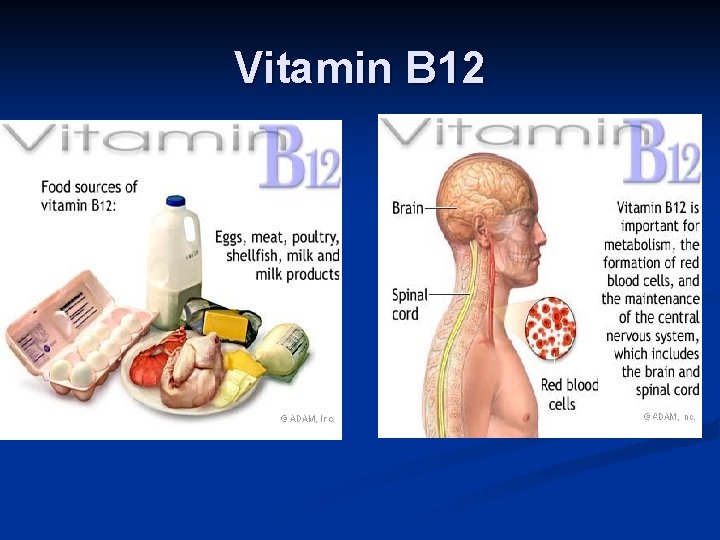
Vitamin B 12
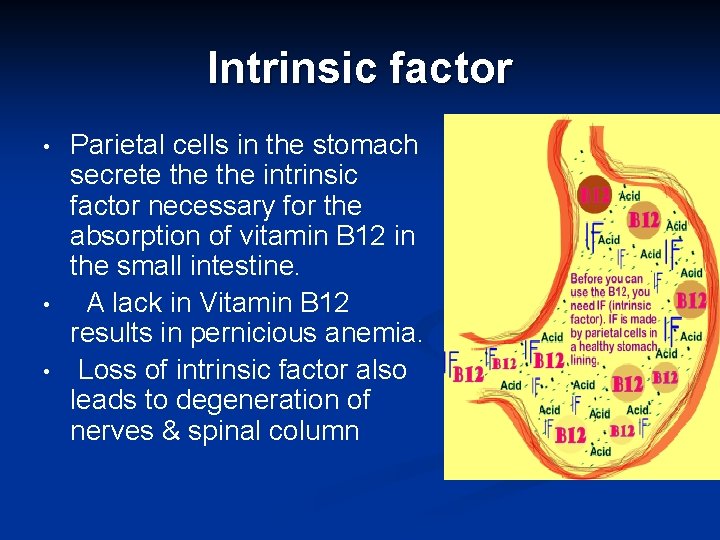
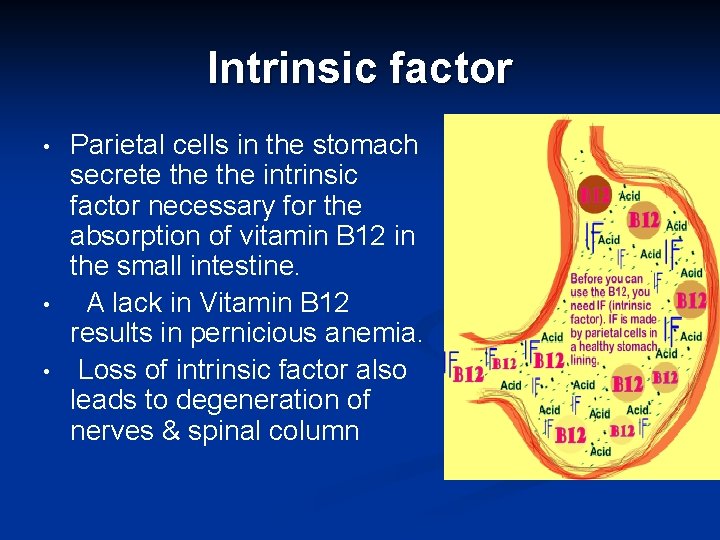
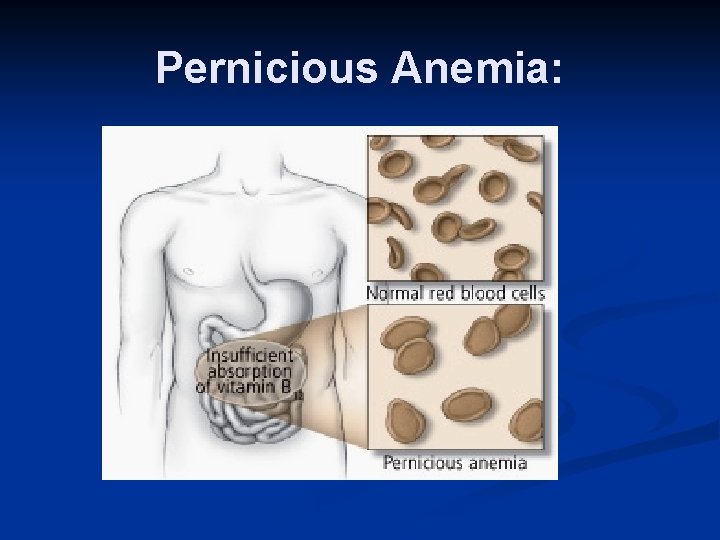
Intrinsic factor • • • Parietal cells in the stomach secrete the intrinsic factor necessary for the absorption of vitamin B 12 in the small intestine. A lack in Vitamin B 12 results in pernicious anemia. Loss of intrinsic factor also leads to degeneration of nerves & spinal column
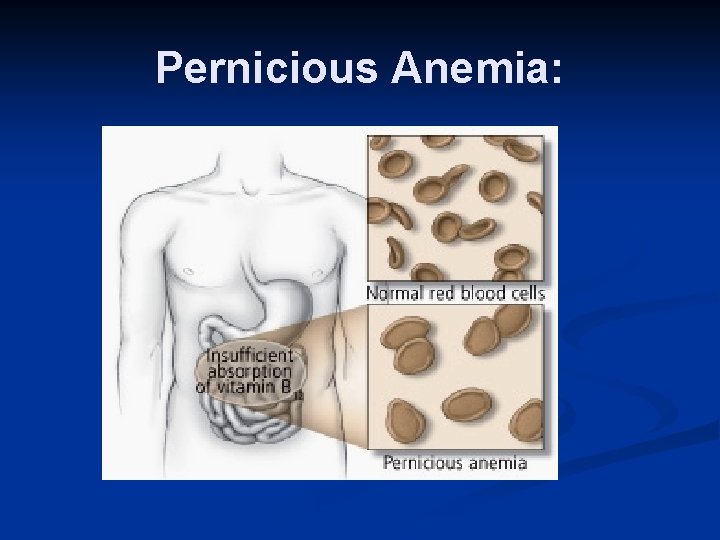
Pernicious Anemia:
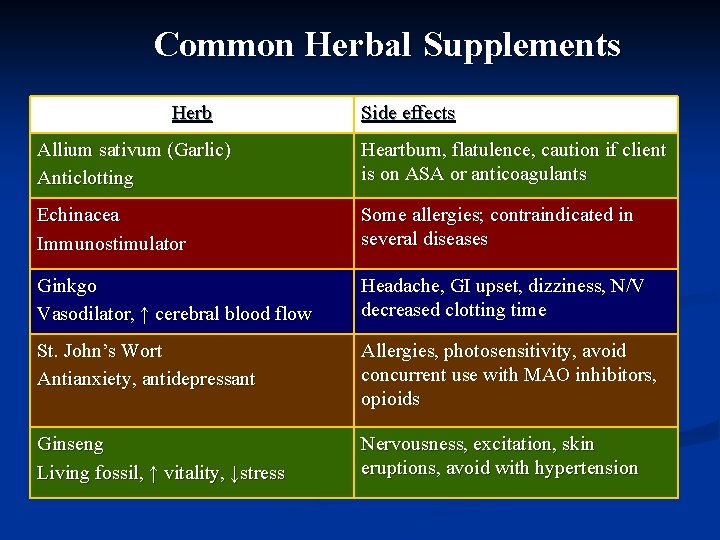
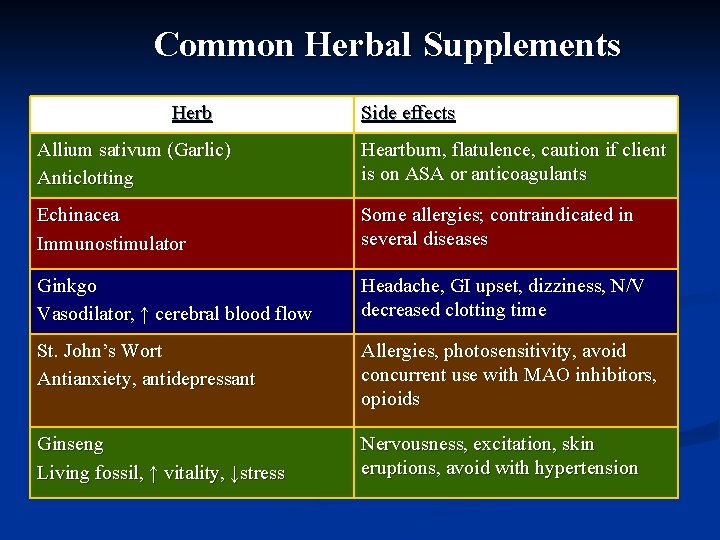
Common Herbal Supplements Herb Side effects Allium sativum (Garlic) Anticlotting Heartburn, flatulence, caution if client is on ASA or anticoagulants Echinacea Immunostimulator Some allergies; contraindicated in several diseases Ginkgo Vasodilator, ↑ cerebral blood flow Headache, GI upset, dizziness, N/V decreased clotting time St. John’s Wort Antianxiety, antidepressant Allergies, photosensitivity, avoid concurrent use with MAO inhibitors, opioids Ginseng Living fossil, ↑ vitality, ↓stress Nervousness, excitation, skin eruptions, avoid with hypertension
GI Tract: Oral Problems
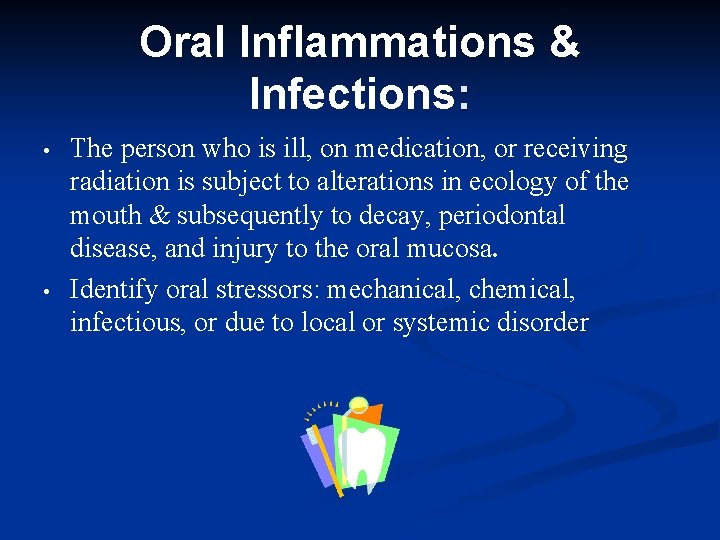
Oral Inflammations & Infections: • • The person who is ill, on medication, or receiving radiation is subject to alterations in ecology of the mouth & subsequently to decay, periodontal disease, and injury to the oral mucosa. Identify oral stressors: mechanical, chemical, infectious, or due to local or systemic disorder
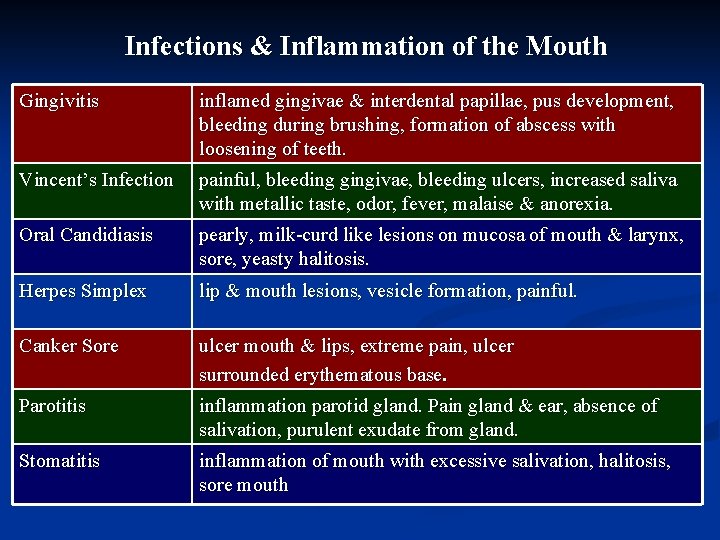
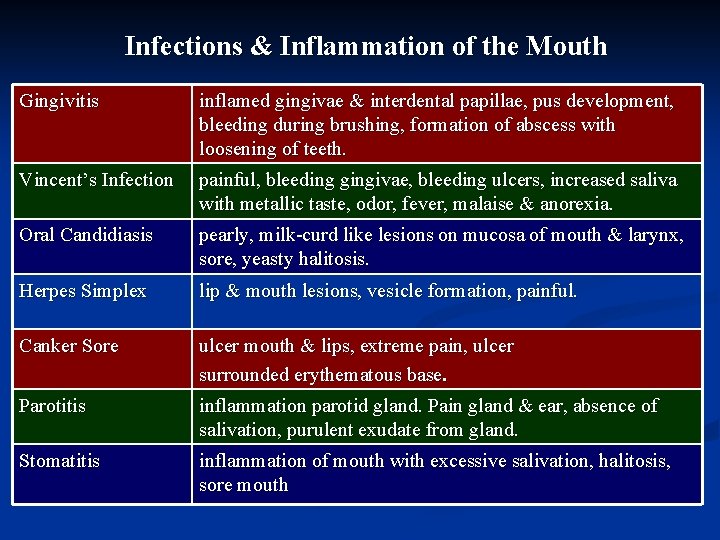
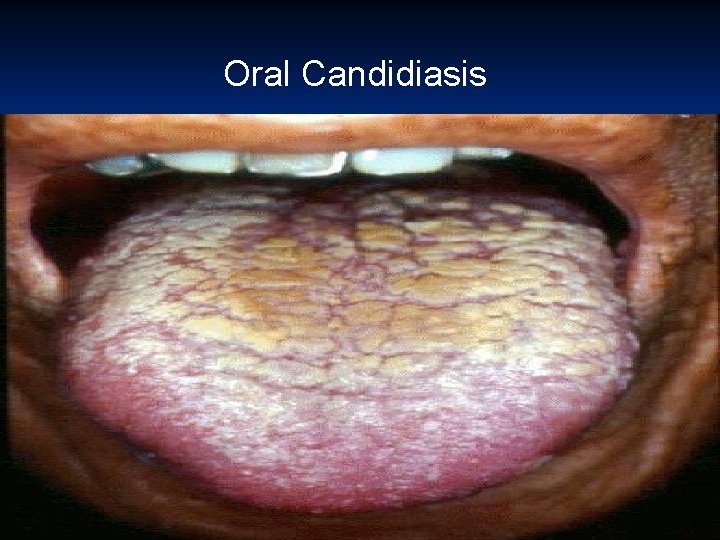
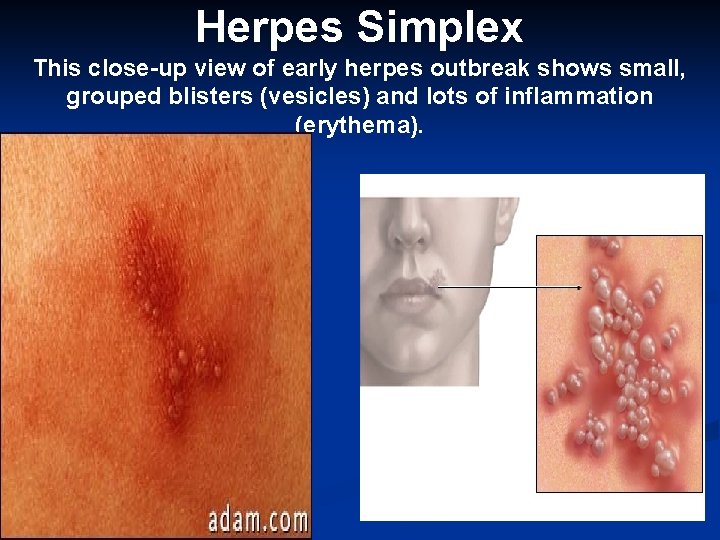
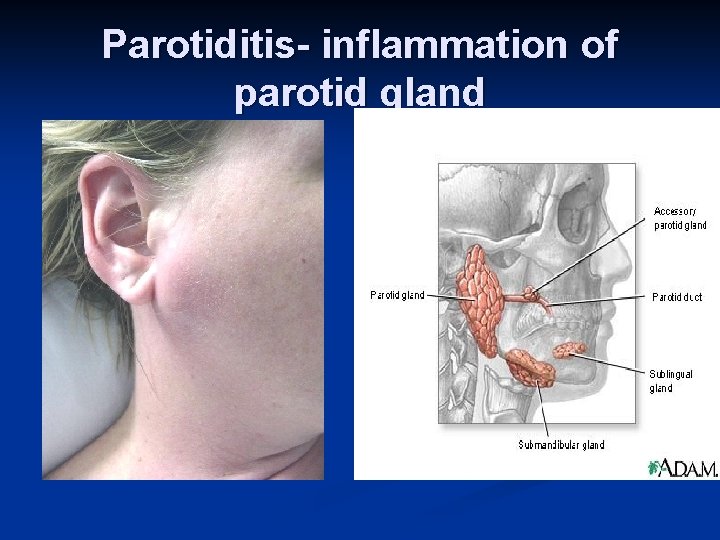
Infections & Inflammation of the Mouth Gingivitis inflamed gingivae & interdental papillae, pus development, bleeding during brushing, formation of abscess with loosening of teeth. Vincent’s Infection painful, bleeding gingivae, bleeding ulcers, increased saliva with metallic taste, odor, fever, malaise & anorexia. Oral Candidiasis pearly, milk-curd like lesions on mucosa of mouth & larynx, sore, yeasty halitosis. Herpes Simplex lip & mouth lesions, vesicle formation, painful. Canker Sore ulcer mouth & lips, extreme pain, ulcer surrounded erythematous base. Parotitis inflammation parotid gland. Pain gland & ear, absence of salivation, purulent exudate from gland. Stomatitis inflammation of mouth with excessive salivation, halitosis, sore mouth

St. Vincent’s Stomatitis Herpes Simplex I Cold Sore Gingivitis Oral Candidiasis Parotitis
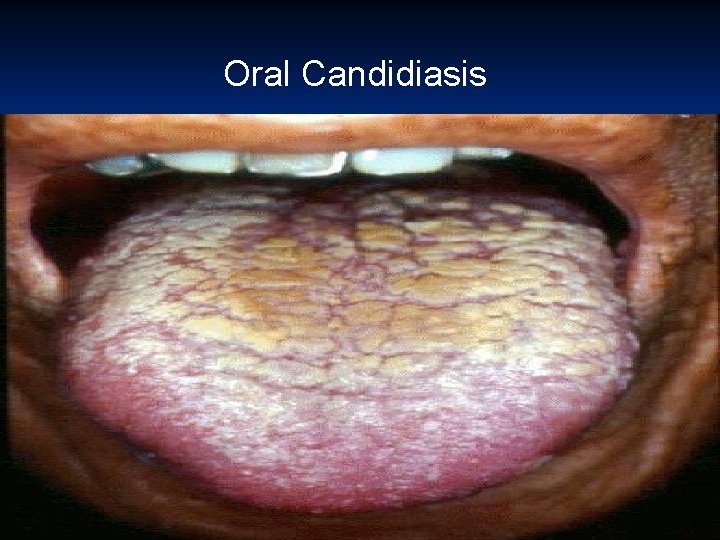
Oral Candidiasis .
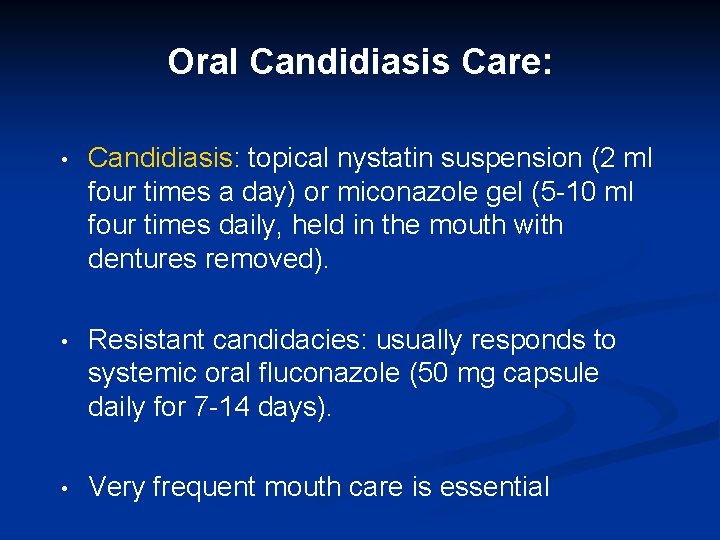
Oral Candidiasis Care: • Candidiasis: topical nystatin suspension (2 ml four times a day) or miconazole gel (5 -10 ml four times daily, held in the mouth with dentures removed). • Resistant candidacies: usually responds to systemic oral fluconazole (50 mg capsule daily for 7 -14 days). • Very frequent mouth care is essential
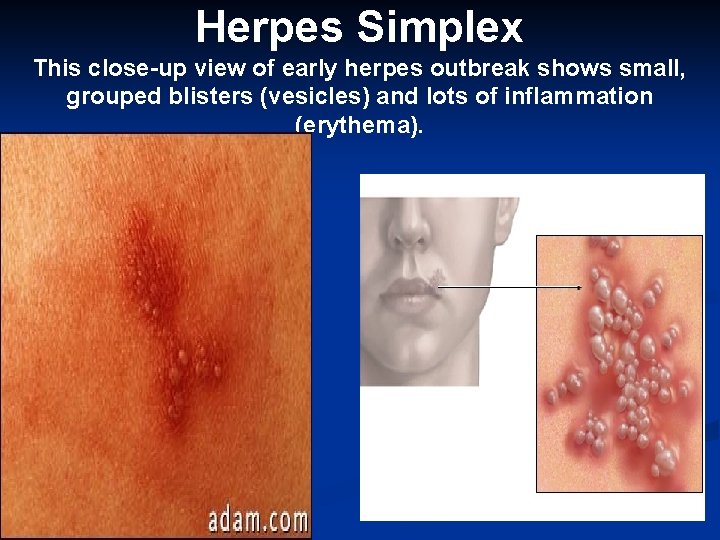
Herpes Simplex This close-up view of early herpes outbreak shows small, grouped blisters (vesicles) and lots of inflammation (erythema).
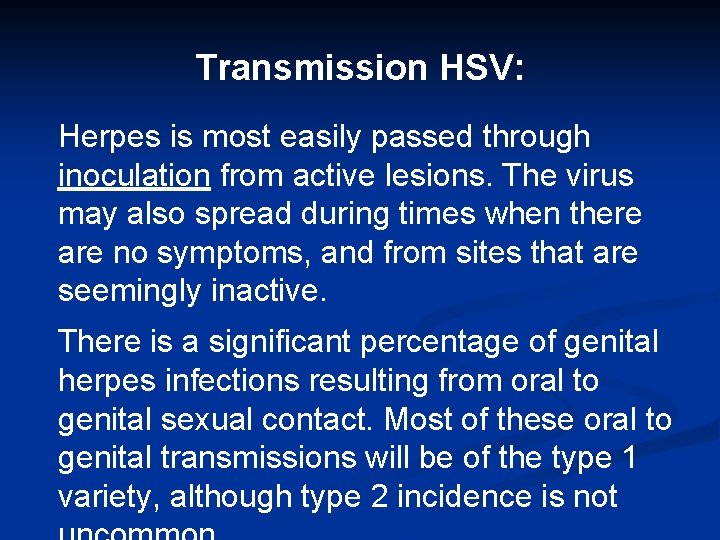
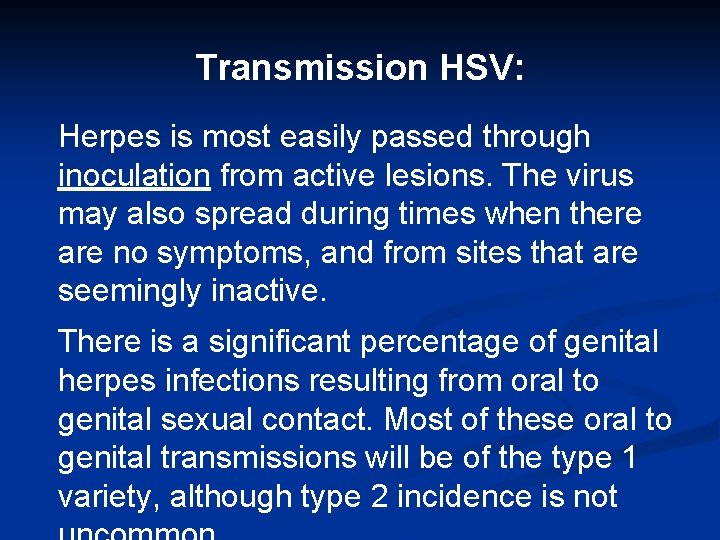
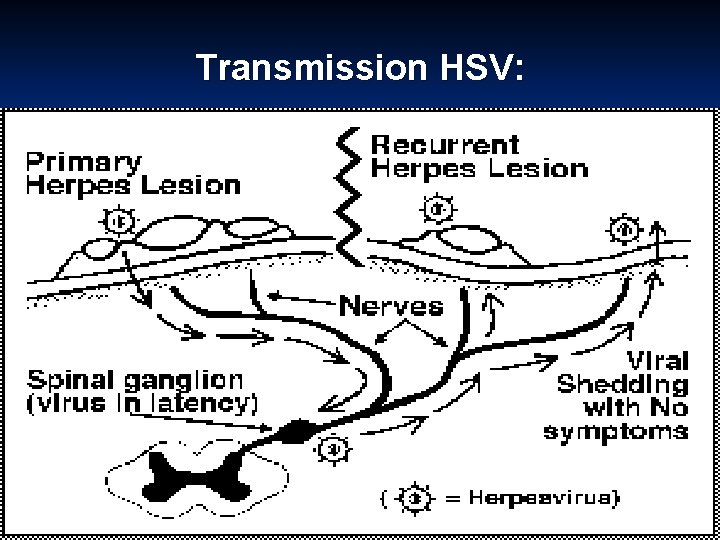
Transmission HSV: Herpes is most easily passed through inoculation from active lesions. The virus may also spread during times when there are no symptoms, and from sites that are seemingly inactive. There is a significant percentage of genital herpes infections resulting from oral to genital sexual contact. Most of these oral to genital transmissions will be of the type 1 variety, although type 2 incidence is not
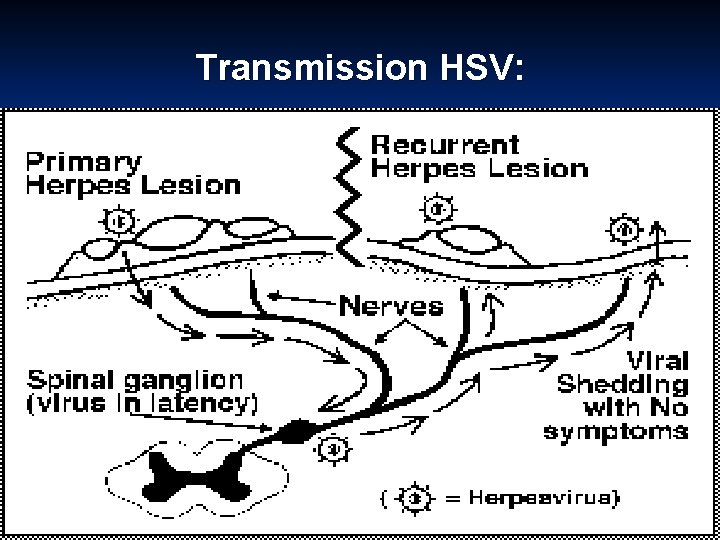
Transmission HSV:
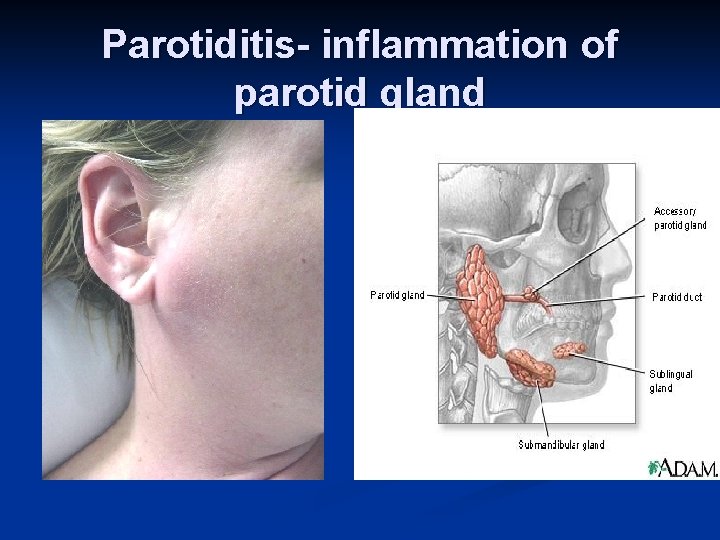
Parotiditis- inflammation of parotid gland
General Nursing Interventions for Oral Pain Relief: • • Careful, regular, frequent mouth care Oral agents such as Lidocaine 2% viscous, Benadryl elixir, Antacid, & Kaopectate, Acetaminophen Topical agents such as coating agents Swishing agents providing topical & anti-inflammatory action analgesia Iced water or a dish of crushed ice (with spoon). Mouth sprays - a small hand-held spray filled with iced fruit juice is simple and effective. It can be easily used by client or relative Artificial saliva - frequent sips of `artificial saliva' may help some patients. An artificial saliva aerosol spray such as An artificial saliva spray such as Moistir is also available.
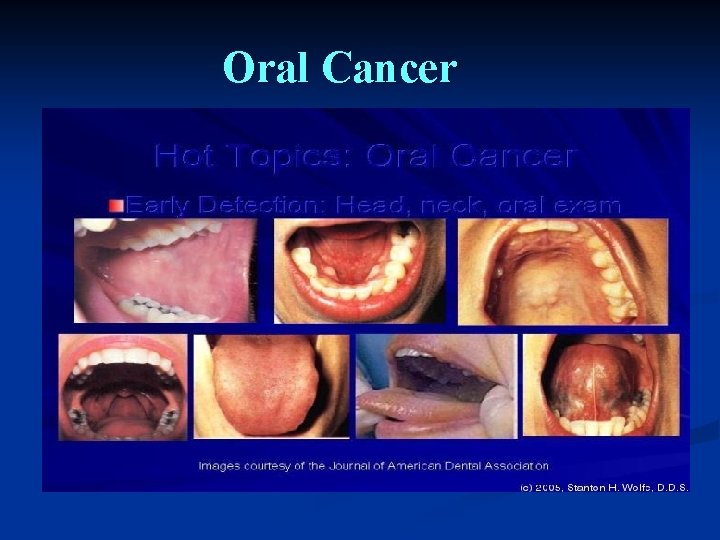
Oral Cancer • • • Occur lips or anywhere within the mouth. Smoking, excessive alcohol, chronic irritation from a jagged tooth, poor dental care, constant exposure to sun are predisposing factors Usually appears painless ulcer on lip Ca tongue ulcer or area of thickness, sore Biopsy to diagnose Treatment surgery, radiation, chemotherapy or combination.
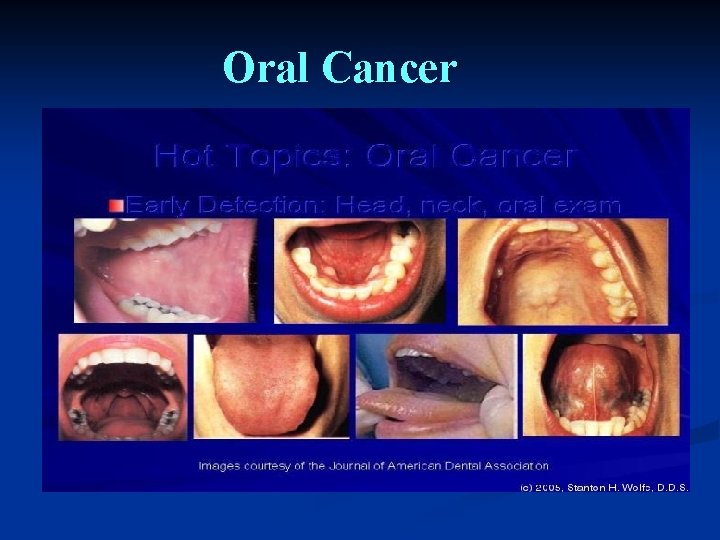
Oral Cancer
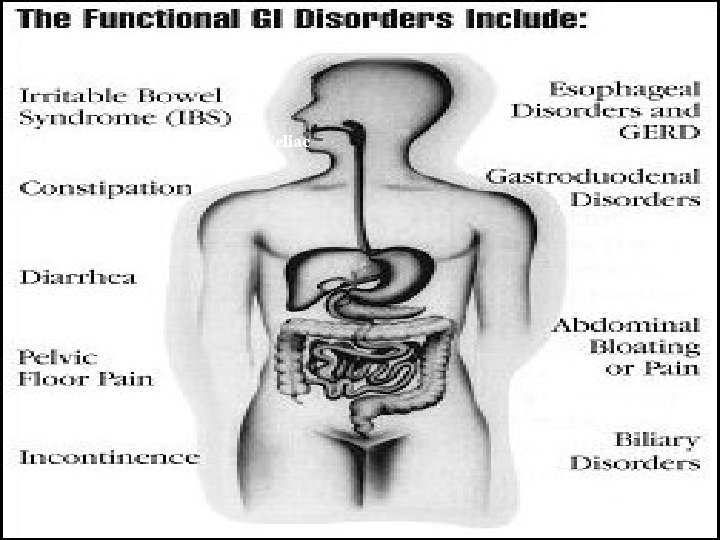
Esophageal Disorders • • • Mechanical : Tumor, Diverticulum, injury CV: aneurysm, varices Neurogenic: Neuro, CVA
Esophageal Disorders • • GERD (Gastroesophageal Reflux Disease) Hiatal Hernia Esophageal Cancer Esophageal Diverticula Esophageal Strictures Achalasia Esophageal Varices
Common Signs & Symptoms of Esophageal Disorders • • Problem swallowing * Pain * Hoarseness * Weight loss * Bleeding * Regurgitation (water brash) Heart burn Hiccups
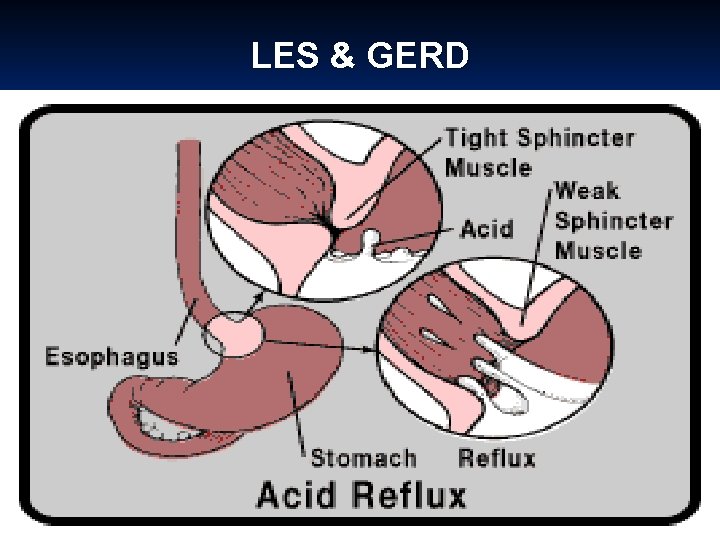
GERD • • Syndrome No one single cause Factors causing GERD: • Impaired esophageal mobility • Delayed gastric emptying • Defective mucosal defense • Reflux of gastric contents • Lower Esophageal Sphincter (LES) dysfunction –main factor.
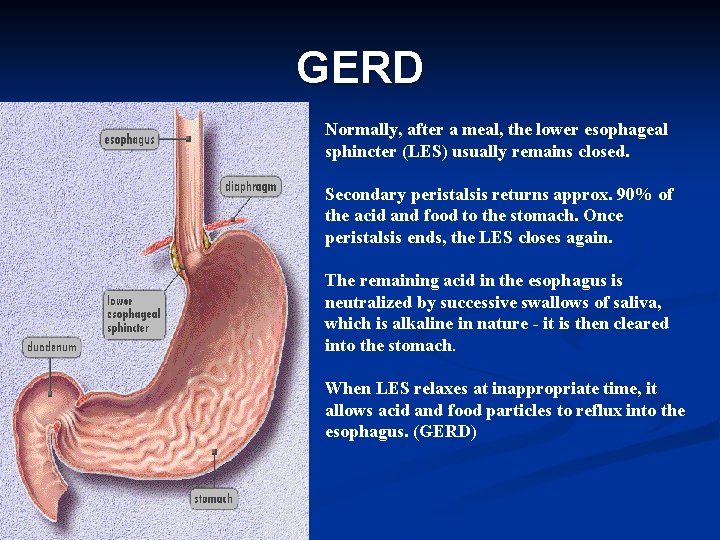
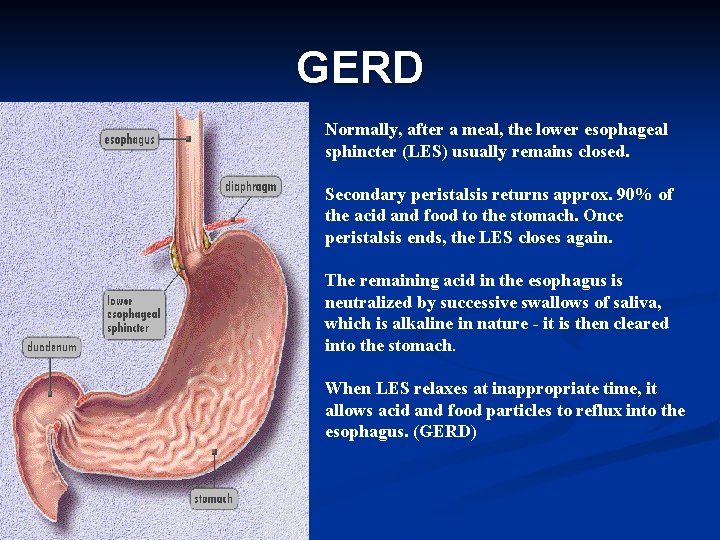
GERD Normally, after a meal, the lower esophageal sphincter (LES) usually remains closed. Secondary peristalsis returns approx. 90% of the acid and food to the stomach. Once peristalsis ends, the LES closes again. The remaining acid in the esophagus is neutralized by successive swallows of saliva, which is alkaline in nature - it is then cleared into the stomach. When LES relaxes at inappropriate time, it allows acid and food particles to reflux into the esophagus. (GERD)
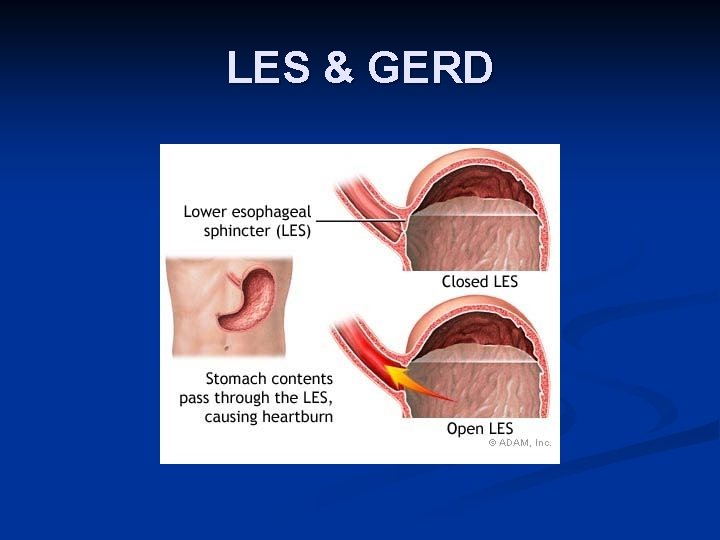
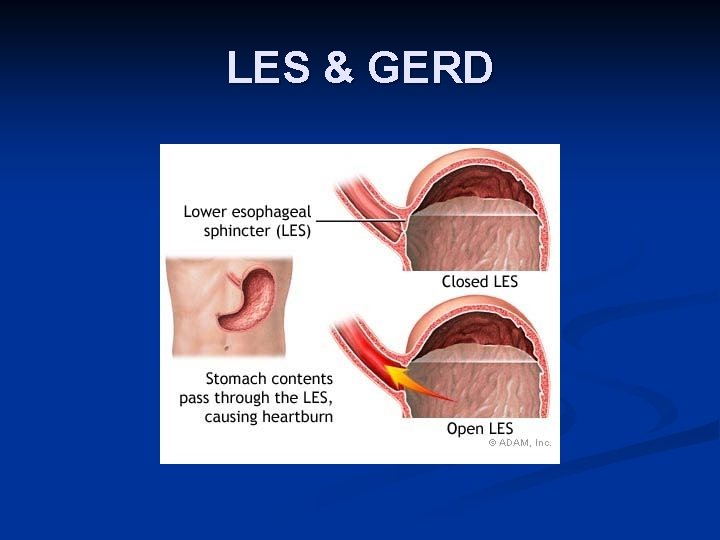
LES & GERD
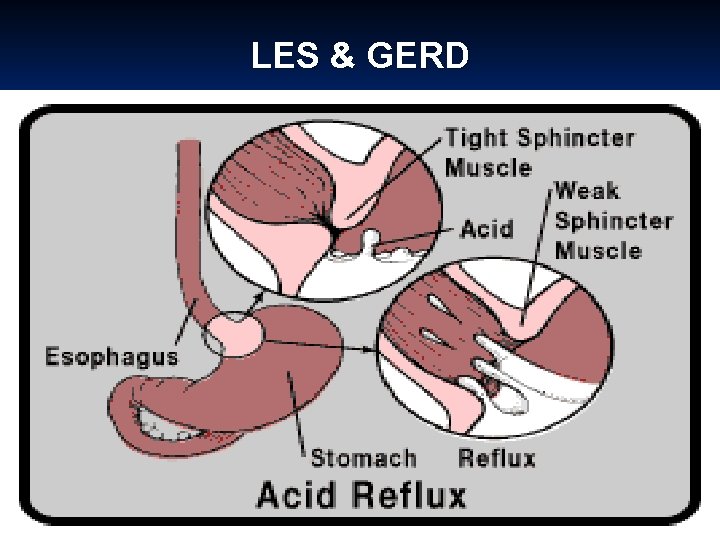
LES & GERD
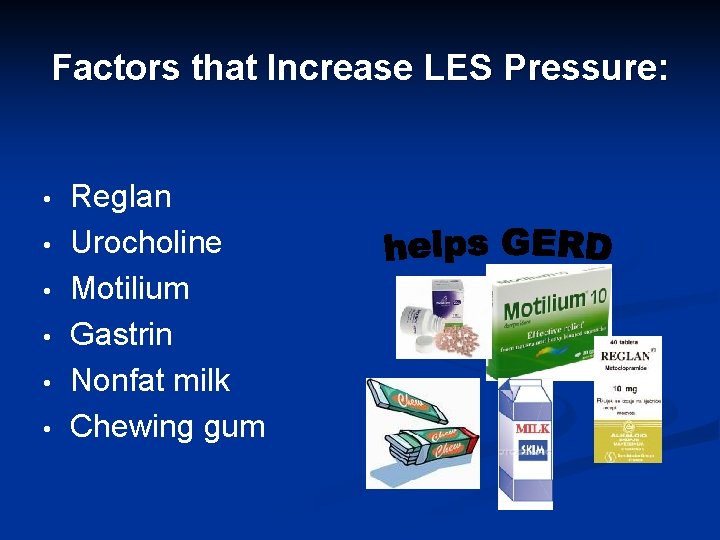
Factors that Increase LES Pressure: • • • Reglan Urocholine Motilium Gastrin Nonfat milk Chewing gum
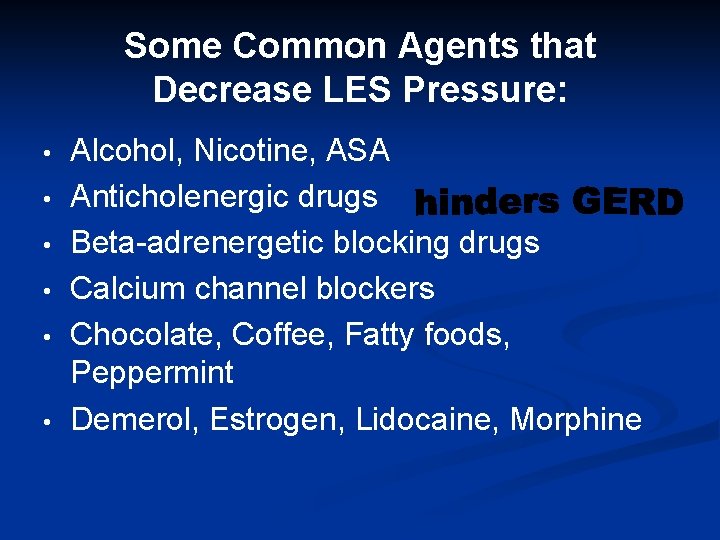
Some Common Agents that Decrease LES Pressure: • • • Alcohol, Nicotine, ASA Anticholenergic drugs Beta-adrenergetic blocking drugs Calcium channel blockers Chocolate, Coffee, Fatty foods, Peppermint Demerol, Estrogen, Lidocaine, Morphine
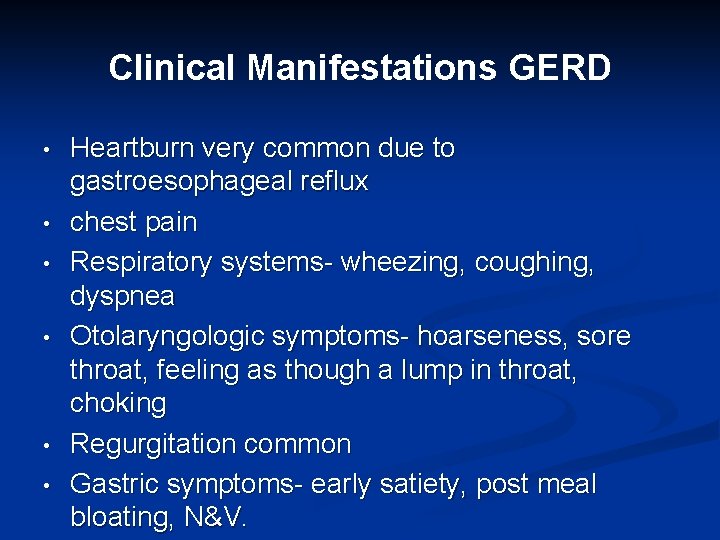
Clinical Manifestations GERD • • • Heartburn very common due to gastroesophageal reflux chest pain Respiratory systems- wheezing, coughing, dyspnea Otolaryngologic symptoms- hoarseness, sore throat, feeling as though a lump in throat, choking Regurgitation common Gastric symptoms- early satiety, post meal bloating, N&V.
Complications of GERD • • Esophagitis Barrett’s esophagus Respiratory complications: bronchospasms, laryngospasms, pneumonia Dental erosion
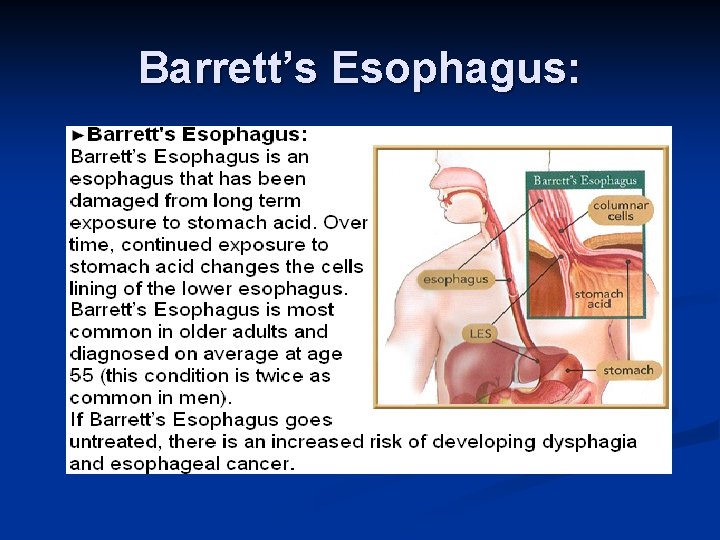
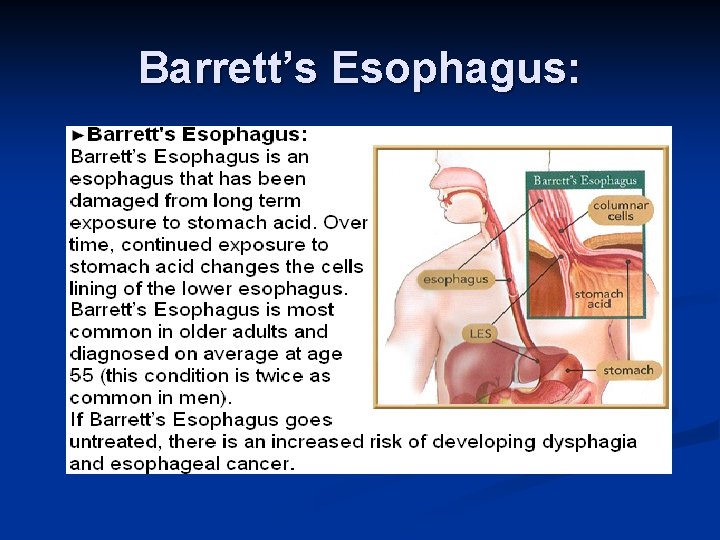
Barrett’s Esophagus:
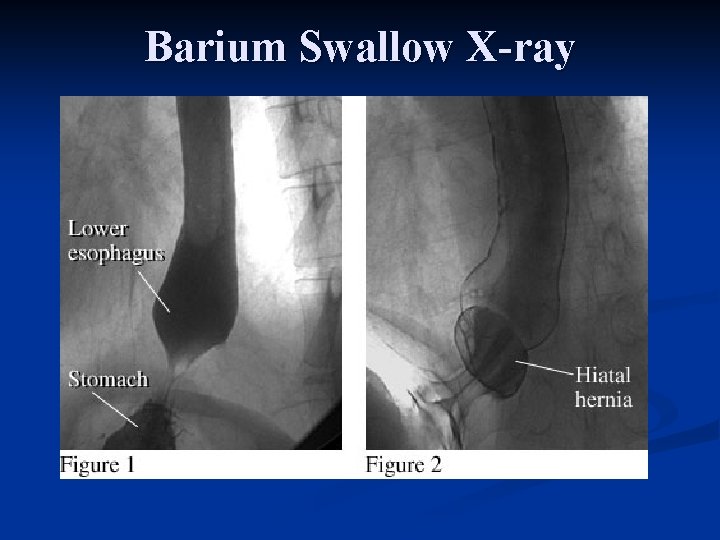
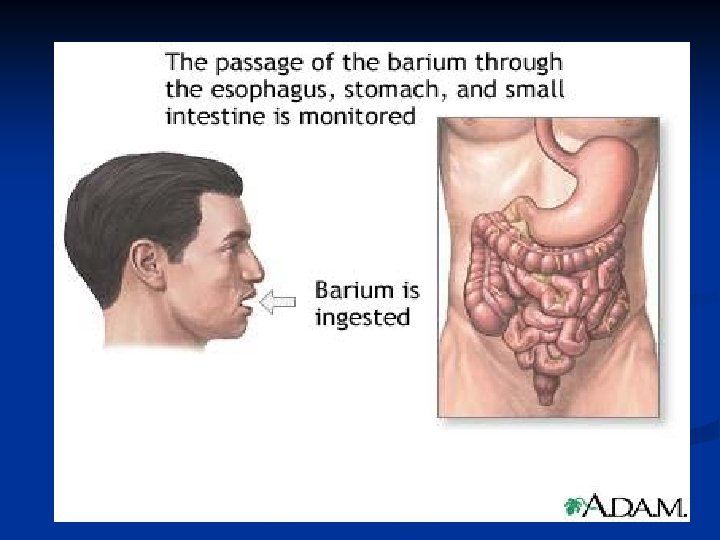
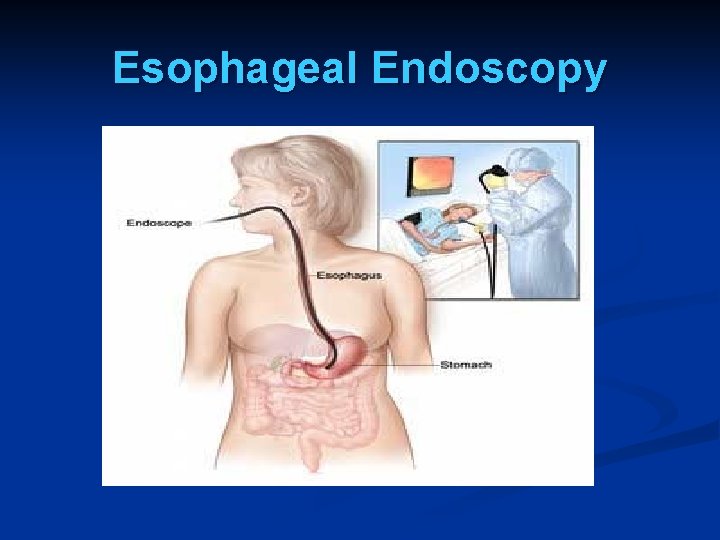
Diagnosing GERD • • • Barium swallow /X-ray if protrusion upper part of stomach Esophageal Endoscopy Biopsies to determine ca stomach or Barrett’s esophagus Esophageal manometric studies- measure pressure esophagus & LES PH measuring devices to determine if acid in esophagus High-dose proton pump inhibitor (PPI)
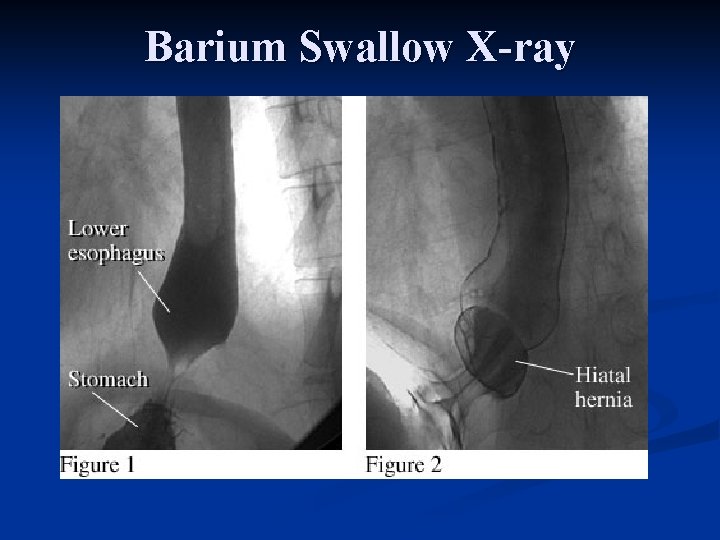
Barium Swallow X-ray
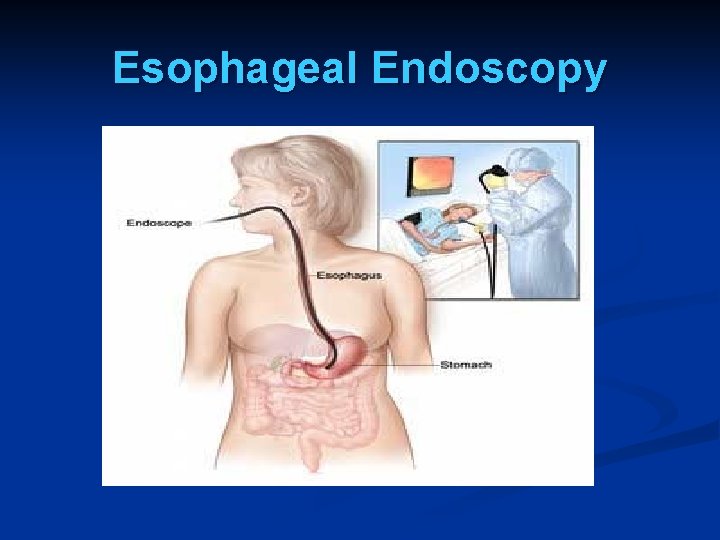
Esophageal Endoscopy
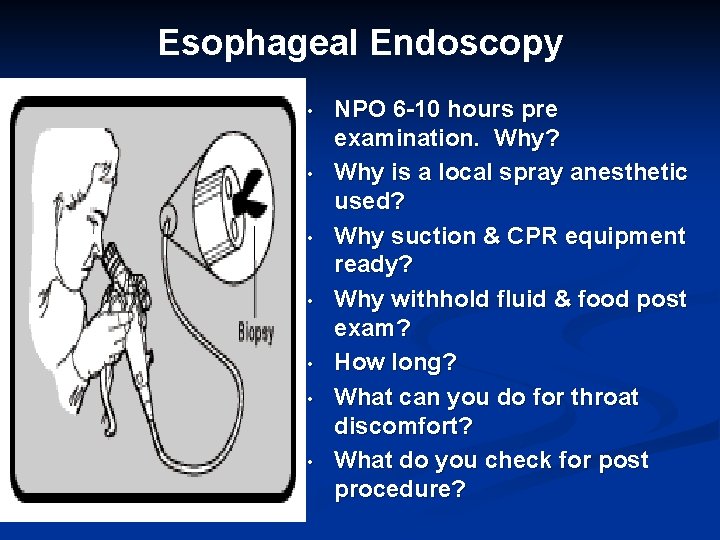
Esophageal Endoscopy • • NPO 6 -10 hours pre examination. Why? Why is a local spray anesthetic used? Why suction & CPR equipment ready? Why withhold fluid & food post exam? How long? What can you do for throat discomfort? What do you check for post procedure?
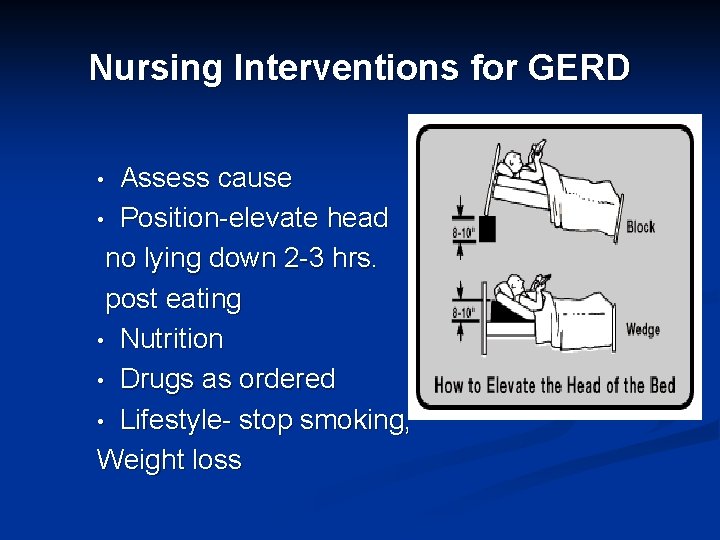
Nursing Interventions for GERD Assess cause • Position-elevate head no lying down 2 -3 hrs. post eating • Nutrition • Drugs as ordered • Lifestyle- stop smoking, Weight loss •
Drugs for GERD: Drugs for GERD focus on: n Improving LES function (urecholine) n Increasing esophageal clearance (metoclopramide) n Decreasing volume & acidity of reflux (H 2 receptor blockers, PPI, maalox, mylanta) n Protecting esophageal mucosa (gaviscon, carafate) n If they do not work surgery maybe required
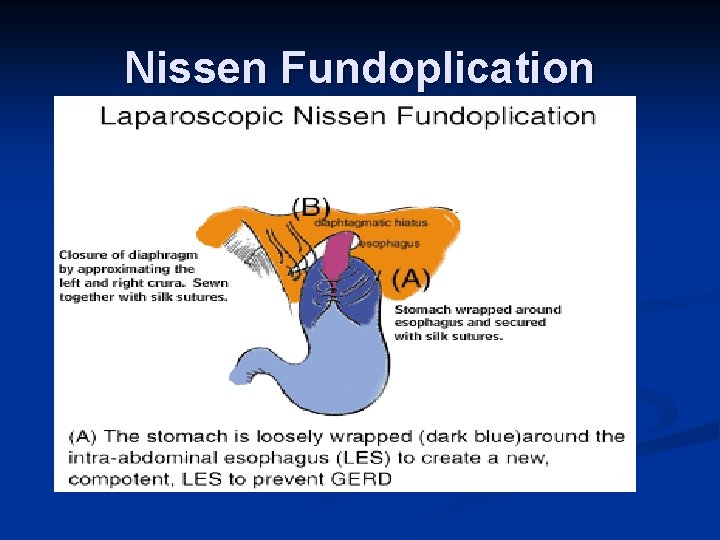
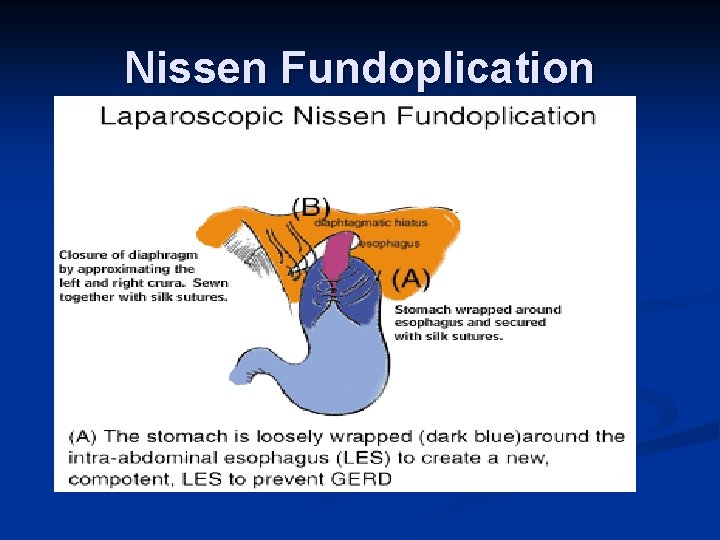
Nissen Fundoplication
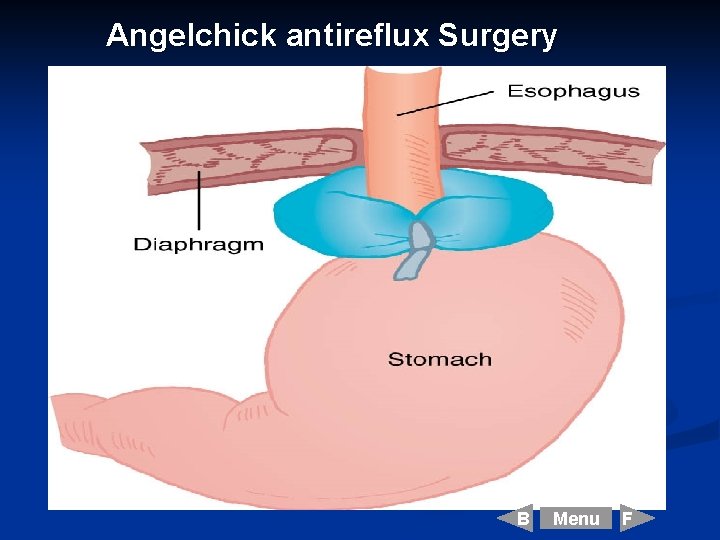
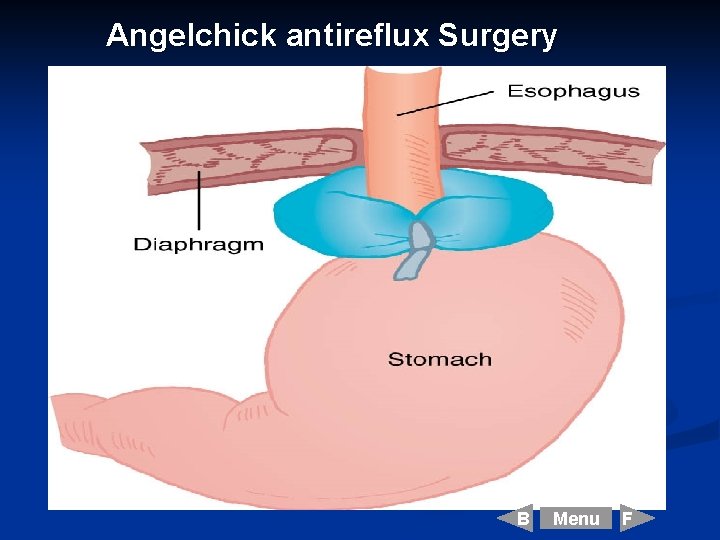
Angelchick antireflux Surgery B Menu F
Hiatal Hernia
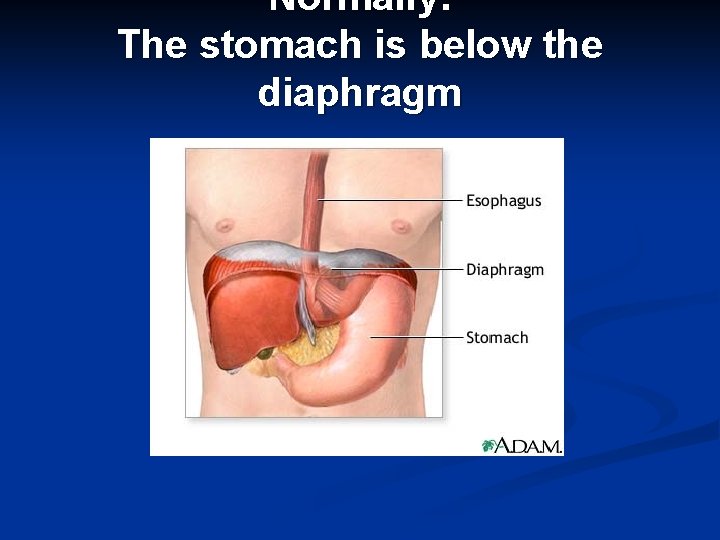
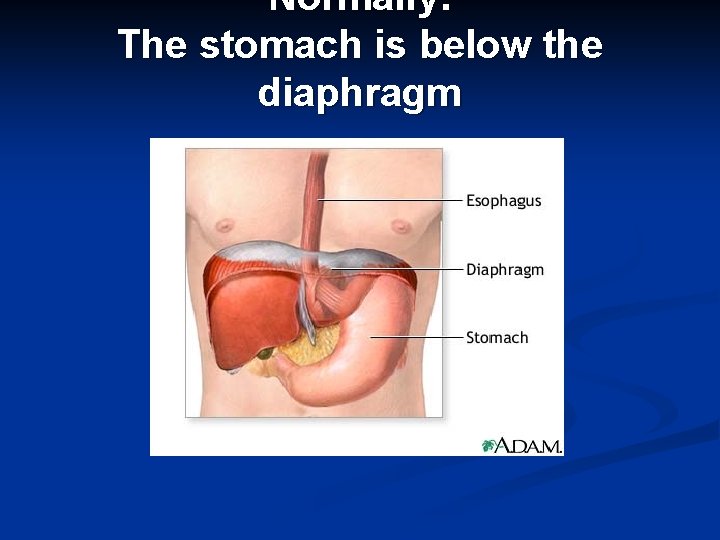
Normally: The stomach is below the diaphragm
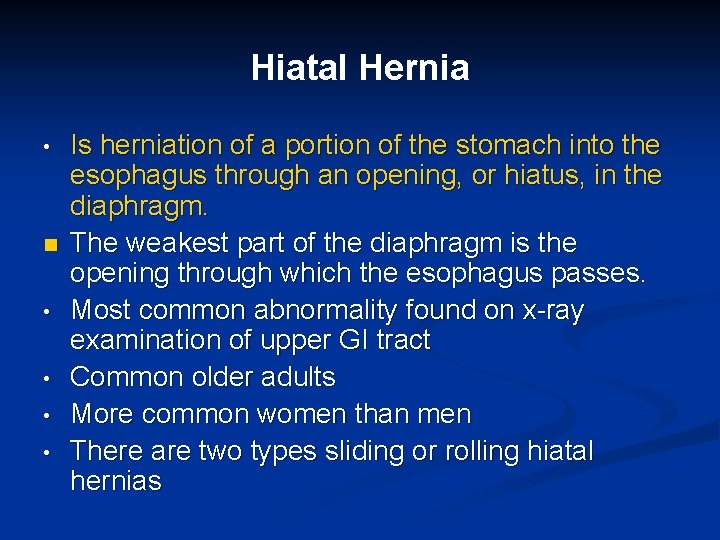
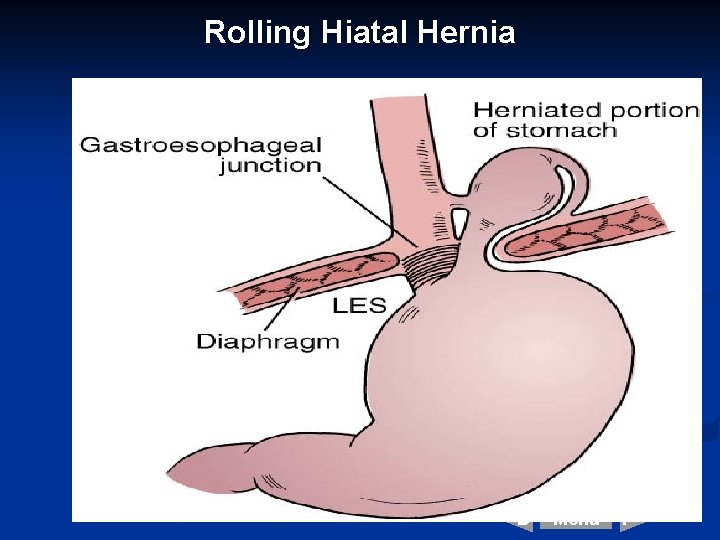
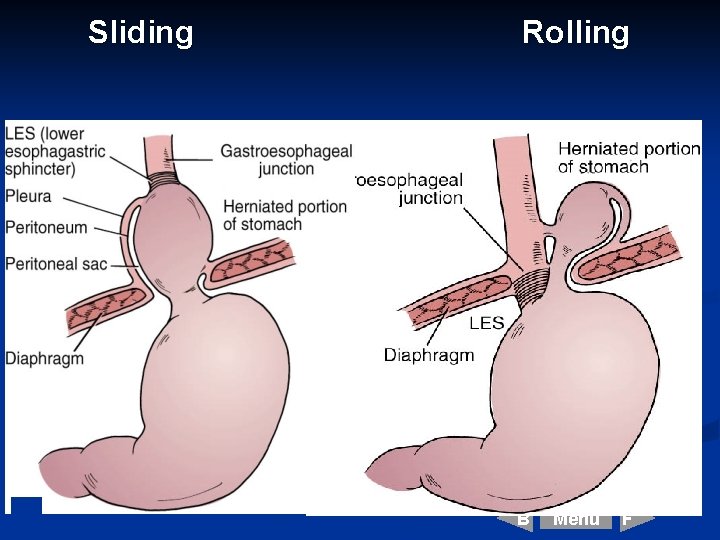
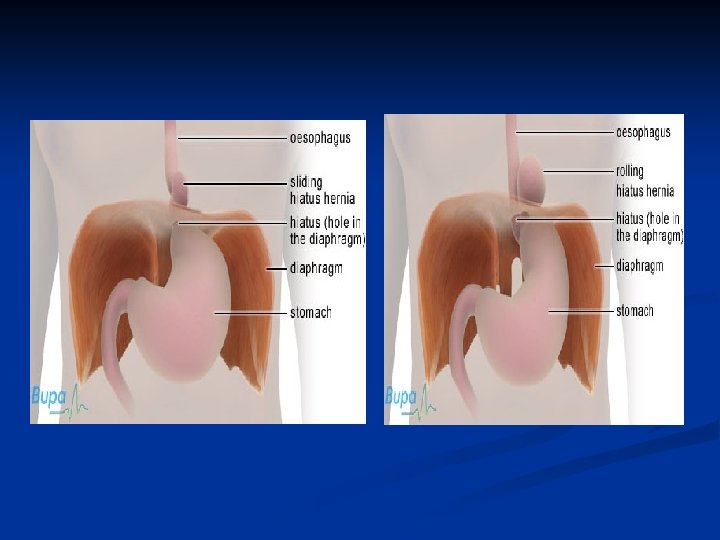
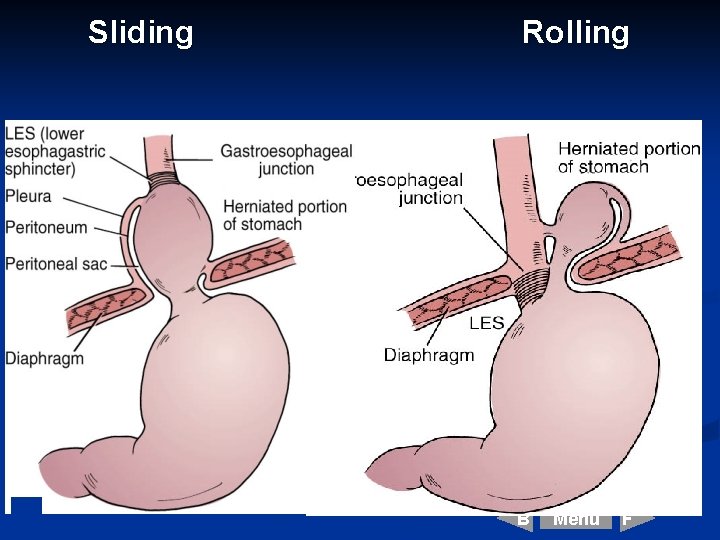
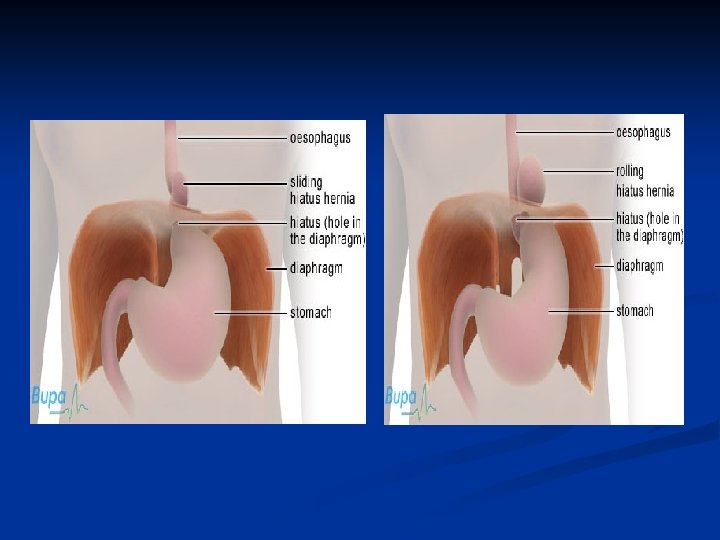
Hiatal Hernia • n • • Is herniation of a portion of the stomach into the esophagus through an opening, or hiatus, in the diaphragm. The weakest part of the diaphragm is the opening through which the esophagus passes. Most common abnormality found on x-ray examination of upper GI tract Common older adults More common women than men There are two types sliding or rolling hiatal hernias

Hiatal Hernia:
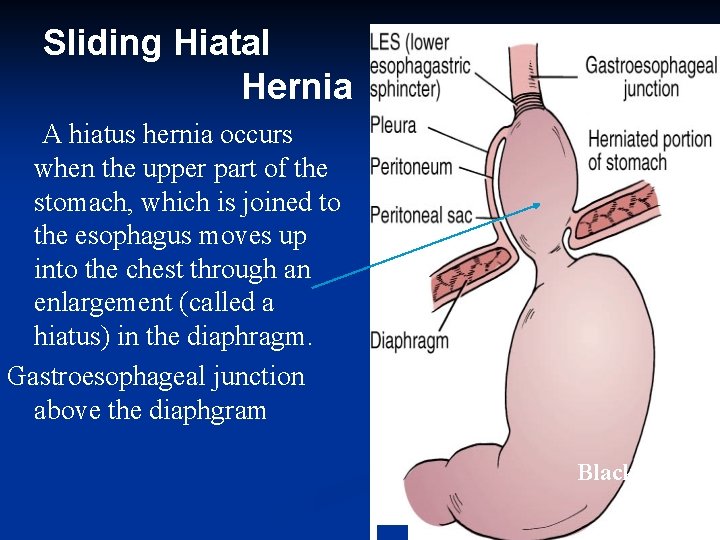
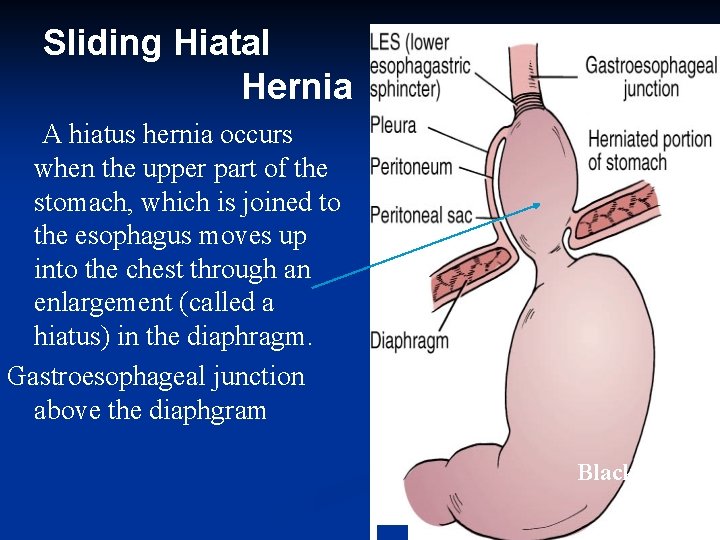
Sliding Hiatal Hernia A hiatus hernia occurs when the upper part of the stomach, which is joined to the esophagus moves up into the chest through an enlargement (called a hiatus) in the diaphragm. Gastroesophageal junction above the diaphgram Black, 2001 B Menu F

Sliding Hiatal Hernia/ Without Hernia
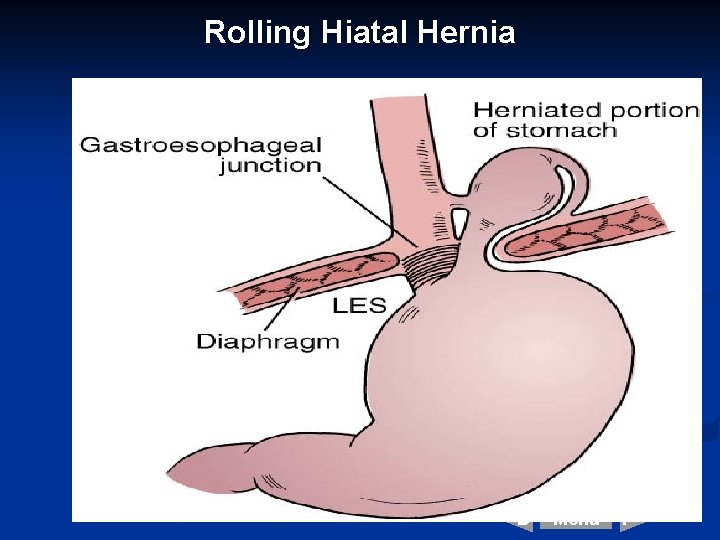
Rolling Hiatal Hernia B Menu F
Sliding Rolling B Menu F
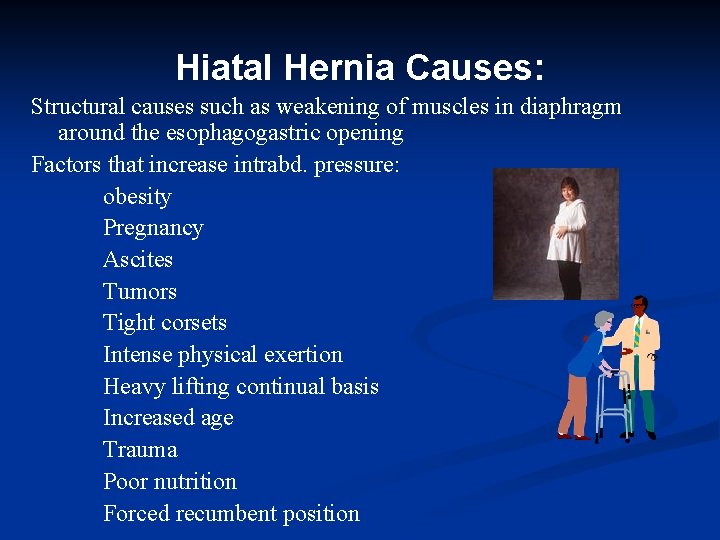
Hiatal Hernia Causes: Structural causes such as weakening of muscles in diaphragm around the esophagogastric opening Factors that increase intrabd. pressure: obesity Pregnancy Ascites Tumors Tight corsets Intense physical exertion Heavy lifting continual basis Increased age Trauma Poor nutrition Forced recumbent position
Clinical Manifestation Hiatal Hernia • • Maybe asymptomatic Heartburn after a meal or after lying supine Dysphagia Reflux & discomfort associated with position lying down Bending over may cause severe burning pain, relieved by standing Pain with large meals, alcohol, & smoking Heartburn at night common
Complications of Hiatal Hernia: • • GERD Hemorrhage from erosion Stenosis of esophagus Ulcerations of herniated portion of stomach Strangulation of the hernia Regurgitation with tracheal aspiration Increased risk for respiratory disease
Diagnosis of Hiatal Hernia • • • Barium swallow: may show protrusion of gastric mucosa through the esophagus X-rays Endoscopy: visualization of the lower esophagus provides info on the degree of mucosal inflammation or other abnormalities.
Conservative Treatment Hiatal Hernia • Keep to weight as ideal as possible • Avoid stooping • Avoid smoking • Reduce alcohol and coffee • Avoid tight clothing/under garments • Adjust bed - elevate HOB • Take antacid such as TUMS • Have small meals especially at supper • Avoid spicy food • Avoid hot drinks • Avoid gassy drinks
Other Esophageal Disorders • • • Esophageal Diverticula- saclike outpouchings of one or more layers of the esophagus Esophageal Strictures – narrowing of esophagus caused by acids or alkalis ingested and reflux of gastric juices Esophageal cancer-rare Achalasia- peristalsis of the lower two thirds of esophagus is absent. LES increased pressure & incomplete relaxation LES. Esophageal Varices- dilated veins occurring in lower portion of the esophagus as a result of portal hypertension. Common cirrhosis of liver.
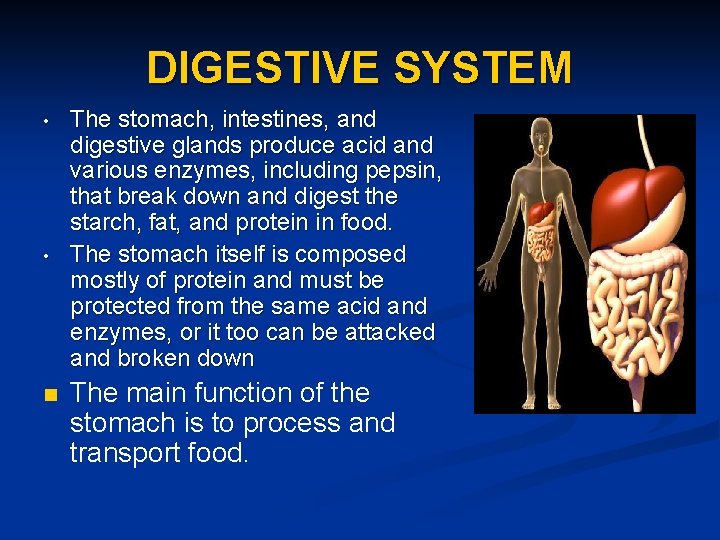
DIGESTIVE SYSTEM • • n The stomach, intestines, and digestive glands produce acid and various enzymes, including pepsin, that break down and digest the starch, fat, and protein in food. The stomach itself is composed mostly of protein and must be protected from the same acid and enzymes, or it too can be attacked and broken down The main function of the stomach is to process and transport food.
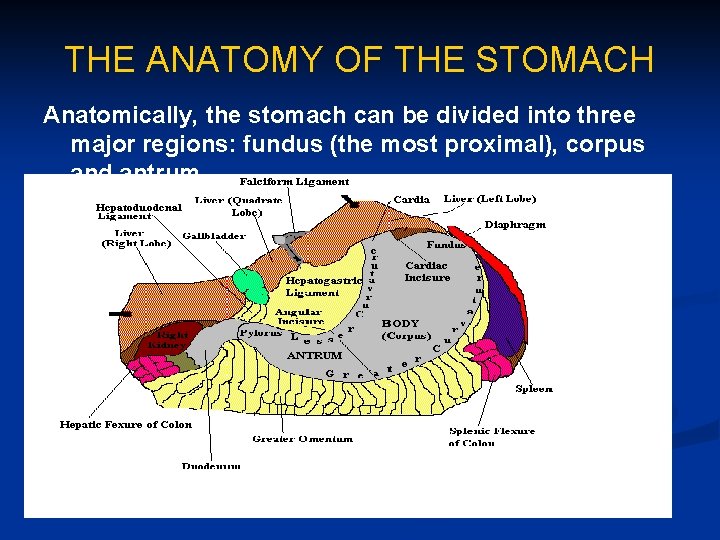
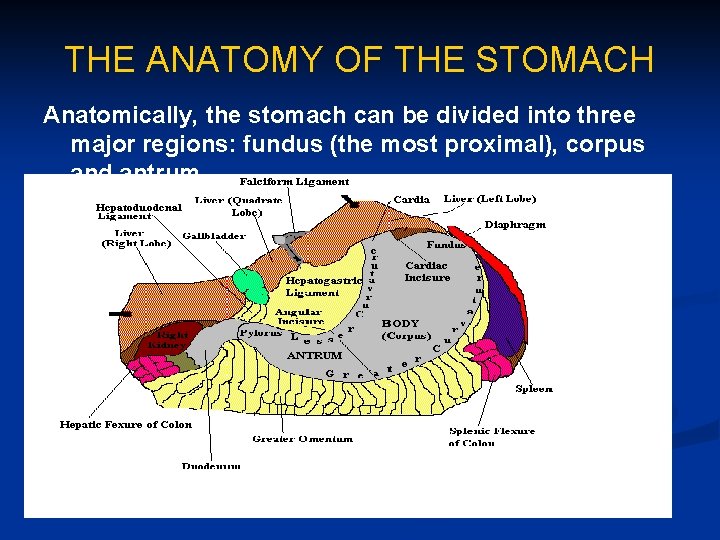
THE ANATOMY OF THE STOMACH Anatomically, the stomach can be divided into three major regions: fundus (the most proximal), corpus and antrum
Disorders of Stomach & Upper Small Intestine • • Gastritis Upper GI Bleeding Peptic Ulcer Disease Gastric Ulcers Duodenal Ulcers Gastric cancer Food Poisoning
Gastritis • • • Inflammation of gastric mucosa as a result of breakdown in normal gastric mucosal barrier. Most common problems affecting stomach Gastritis have tissue edema, disruption of capillary walls with loss of plasma into gastric lumen & possible hemorrhage. Broken mucosal barrier, autodigestion, HCL & pepsin cause gastritis. Can be acute or chronic (loss of intrinsic factor)
Causes of Gastritis • • • Drugs- aspirin, corticosteroids, NSAIDS, digitalis Diet-alcohol, spicy irritating foods Microorganisms-Helicobacter (H-Pylori), Salmonella, Staphylococcus organisms. Environmental-smoking, radiation Pathophysiologic Conditions- burns, lg. hiatal hernia, stress, reflux bile & pancreatic secretions, renal failure, sepsis, shock Other factors- endoscopic procedures, NG suction, psychologic stress
Clinical Manifestation Gastritis: • • Anoxeria N&V Epigastric tenderness Feeling of fullness Hemorrhage-common alcohol abuse Acute gastritis- self-limiting, lasts few hrs to few days, complete healing mucosa Chronic gastritis-loss of intrinsic factor
Diagnosis Gastritis • • Acute – based on history drugs & alcohol Chronic- non-specific symptoms: endoscopic examination with BX CBC-anemia/bld. Loss/lack intrinsic factor Stools Occult blood gastric analysis- HCL present serum tests antibodies tissue BX- R/O gastric cancer
Nursing Management Gastritis • Acute Gastritis: eliminate cause • • • Supportive care Vomiting-bedrest, npo, IV, antiemetics Severe V – NG Hemorrhage-V/S freq. check v blood Administer antacids (raise ph above 6), H 2 R blockers & PPI.
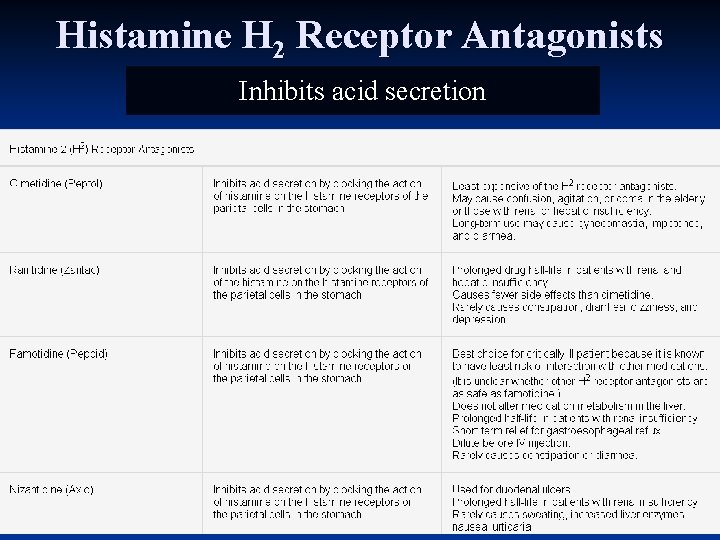
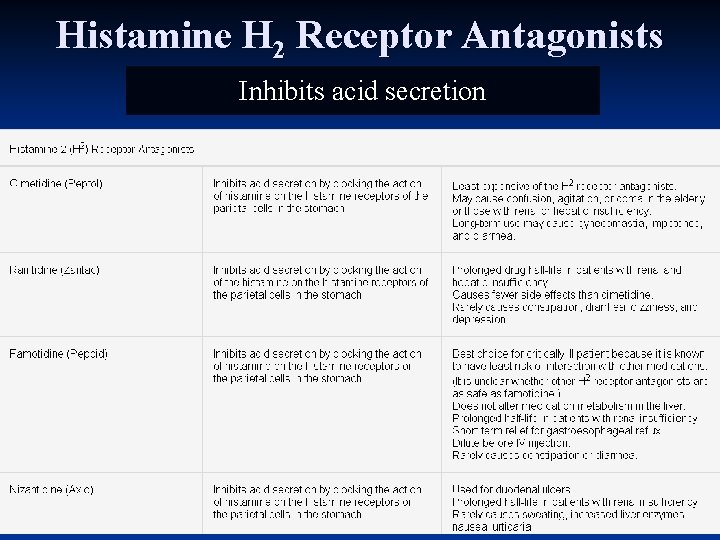
Histamine H 2 Receptor Antagonists Inhibits acid secretion
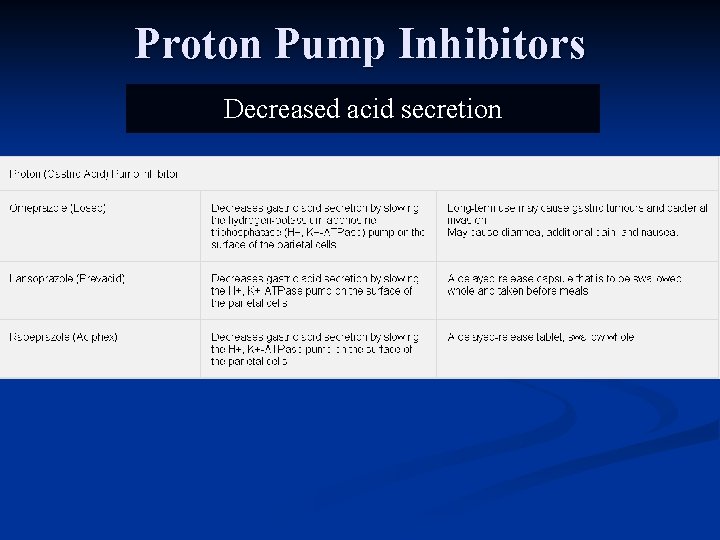
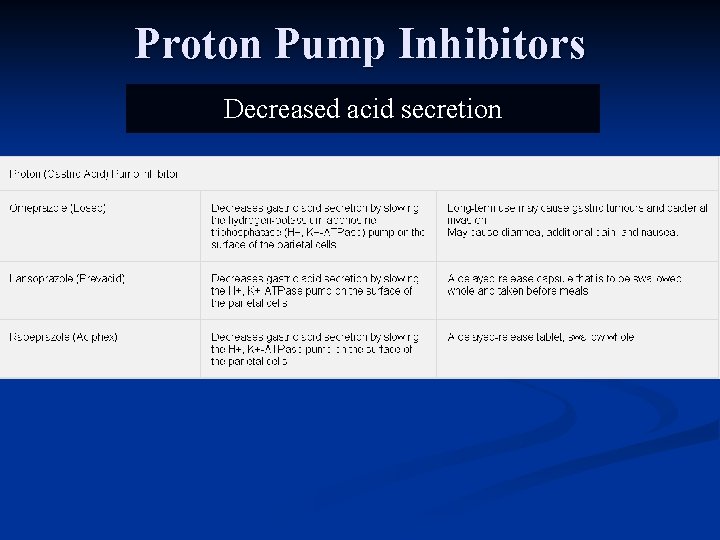
Proton Pump Inhibitors Decreased acid secretion
Nursing Management Gastritis • Chronic Gastritis: evaluation & eliminating cause (cessation alcohol, abstance from drugs, H. pylori eradication) • • • (Flagyl) Antibiotics & antisecretory agents –rid H-pylori Strict adherence drug regime Non-irritating diet Smoking cessation Close medical follow-up as increase incidence Gastric cancer
Upper GI Bleeding
Upper Tract GI Bleeding • • • Upper GI bleeding greater incidence older adults, esp. women using NSAID A sudden onset, insidious bleeding Can be venous, capillary or arterial Common sites esophagus, stomach & duodenum Types upper GI Beeding: • Hematemesis- bldy vomit bright red or coffeegrounds • Melena-black, tarry stools (foul smelling) • Occult Blding- sm. Amt bld in gastric secretions, vomitus or stool not apparent by appearance.
Common Causes Upper GI Bleeding • • Drugs- Corticosteriods, NSAIDS, Salicylates (stimulate acid production, suppress mucous production and cause local damage) Esophagus- Varices, esophagitis, Mallory. Weiss tear (complication of Bulemia) Stomach & duodenum- gastric Ca, hemorrhagic gastritis, peptic ulcers, polyps, stress ulcer Systemic diseases-leukemia, renal failure (increase secretion gastric acid)
Upper GI Bleed: Emergency Assessment & Management • • • Immediate physical exam VS Q 15 -30 mins. , capillary refill, check distension neck veins Abdominal exam (BS) & Resp assessment Labs- CBC, E+, PTT, liver enzymes, ABG’s Assess stool, vomit bld. UA & specific gravity Start 2 IV’s (Bld & fluid replacement R/L) O 2 & meds as ordred Foley indwelling (accurate measures urine ) May have Central line inserted (measure venous pressures) NG tube (mouth) removes bld from stomach & alleviates need to vomit & gastric lavage H 2 O or saline Some prefer endoscopy to NG
Diagnosis Upper GI Bleed • • • Endoscopy- identifies specific source bleeding. Angiography-when endoscopy not done. Invasive procedure catheter placed into gastric or superior mesenteric artery & advanced until site discovered. Barium Contrast- used after acute phase blding to detect lesion can’t verify blding source.
Nursing Management: Upper GI Bleeding • • Accurate & thorough assessment VS History drugs, ulcers, previous bleeds, varcies Approach calm manner acute phase bleed Start IV I/O measurements draw bloods Administer meds as ordered
Nursing Diagnosis Upper GI Bleed • • • Fluid volume deficit re: acute loss blood Ineffective tissue perfussion re: loss circulatory volume Anxiety re: upper GI bleed, uncertain outcome Risk of aspiration re: active blding & altered LOC Decreased cardiac output re: loss of blood
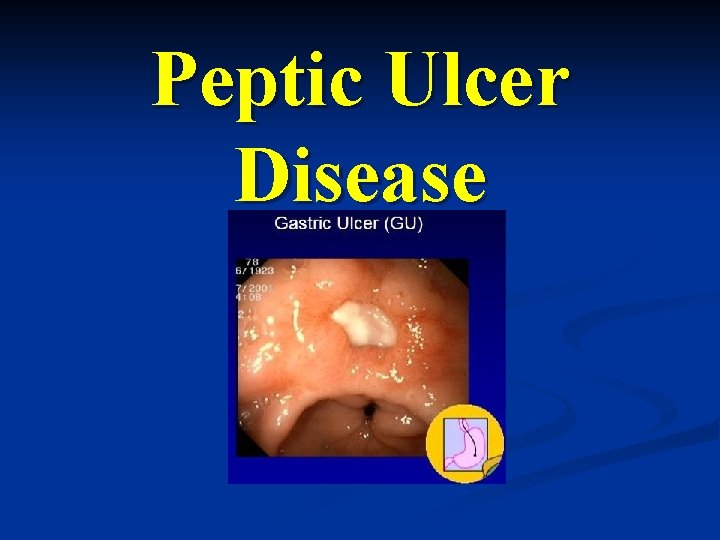
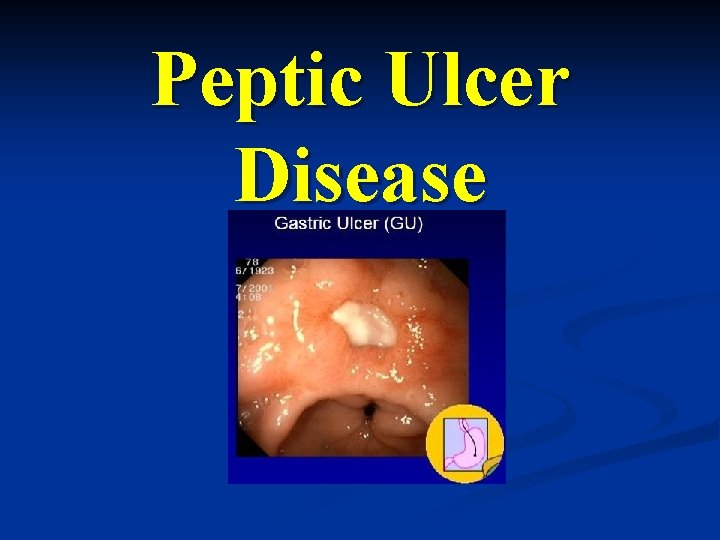
Peptic Ulcer Disease
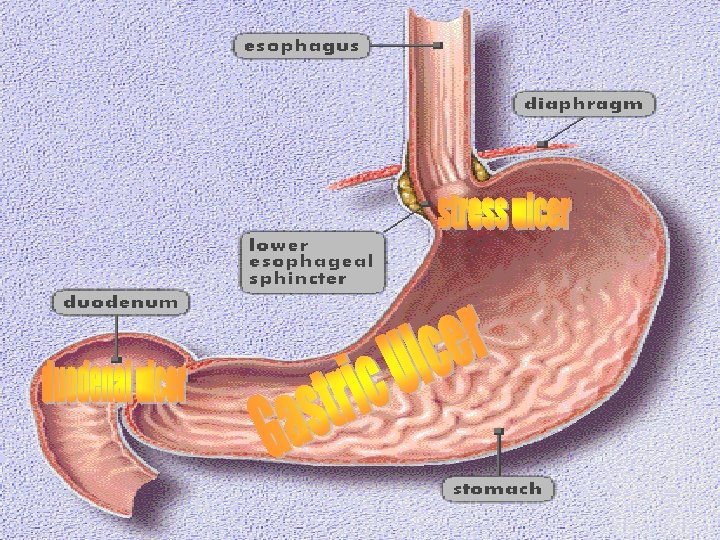
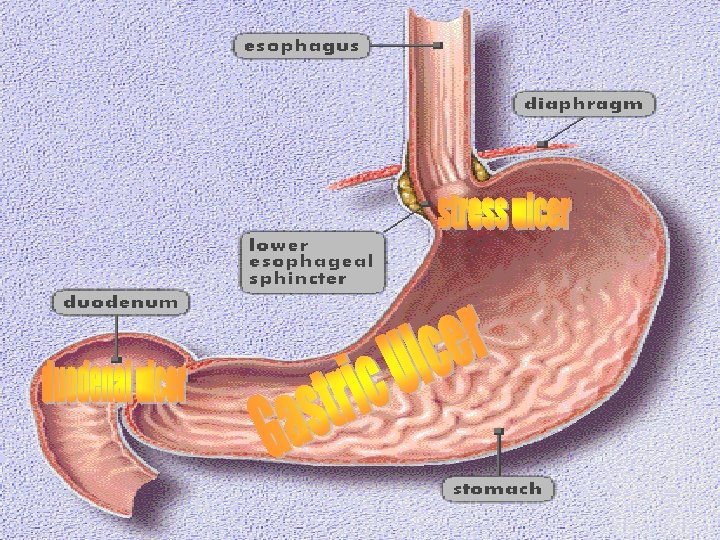
Peptic Ulcer Disease • • Condition characterized by erosion of GI mucosa resulting from the digestive action of HCL acid & pepsin. Can occur in any portion of GI tract comes in contact with gastric secretions Lower esophagus, stomach, duodenum, or jejunum after surgical procedure (gastroenterostomy) 10% males & 4% women will have ulcers during their lifetime
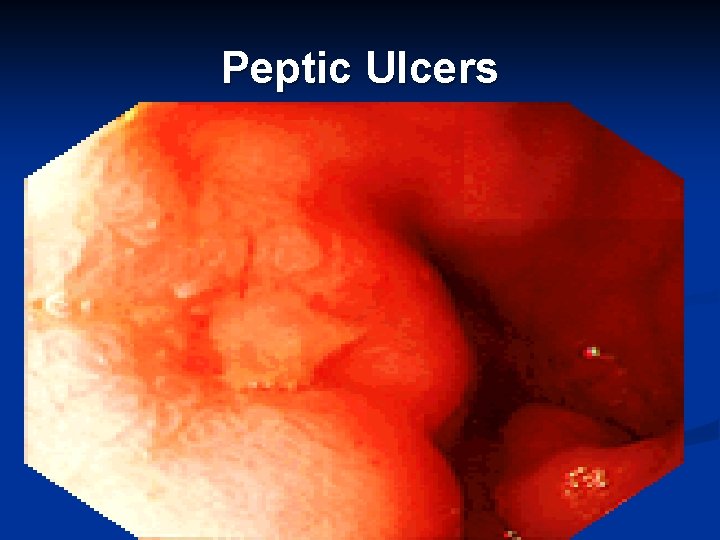
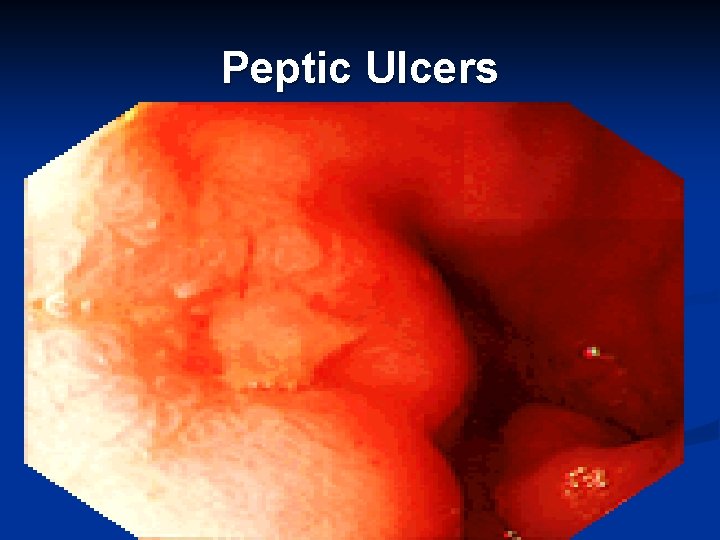
Peptic Ulcers
Facts Relating To Peptic Ulcers • • • Peptic ulcer Disease (PUD) is the most common stomach disorder. Peptic Ulcers are responsible for up to 50% of all upper GI bleeding episodes PUD is a chronic disorder
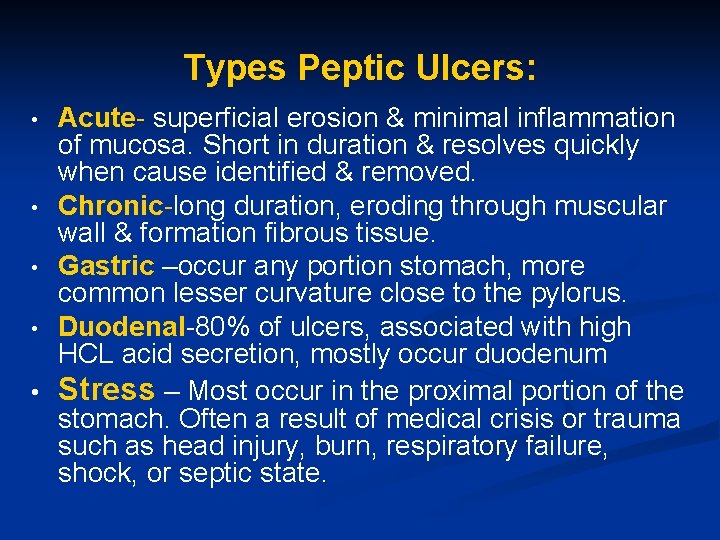
Types Peptic Ulcers: Acute- superficial erosion & minimal inflammation of mucosa. Short in duration & resolves quickly when cause identified & removed. • Chronic-long duration, eroding through muscular wall & formation fibrous tissue. • Gastric –occur any portion stomach, more common lesser curvature close to the pylorus. • Duodenal-80% of ulcers, associated with high HCL acid secretion, mostly occur duodenum • Stress – Most occur in the proximal portion of the stomach. Often a result of medical crisis or trauma such as head injury, burn, respiratory failure, shock, or septic state. •
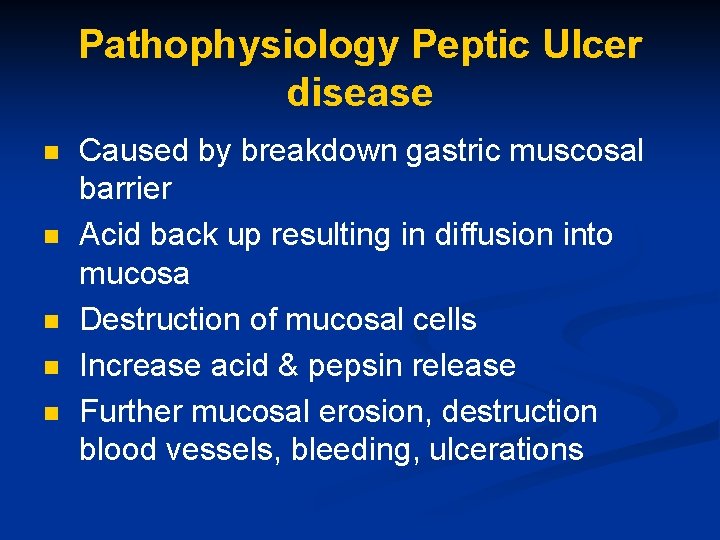
Pathophysiology Peptic Ulcer disease n n n Caused by breakdown gastric muscosal barrier Acid back up resulting in diffusion into mucosa Destruction of mucosal cells Increase acid & pepsin release Further mucosal erosion, destruction blood vessels, bleeding, ulcerations
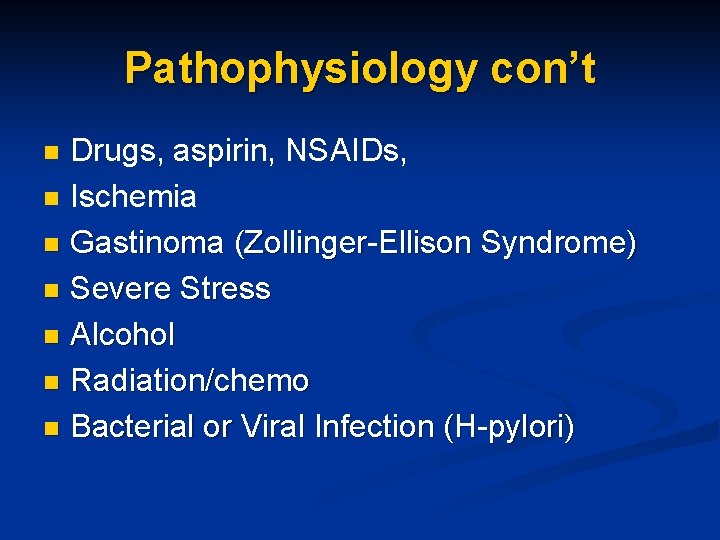
Pathophysiology con’t Drugs, aspirin, NSAIDs, n Ischemia n Gastinoma (Zollinger-Ellison Syndrome) n Severe Stress n Alcohol n Radiation/chemo n Bacterial or Viral Infection (H-pylori) n
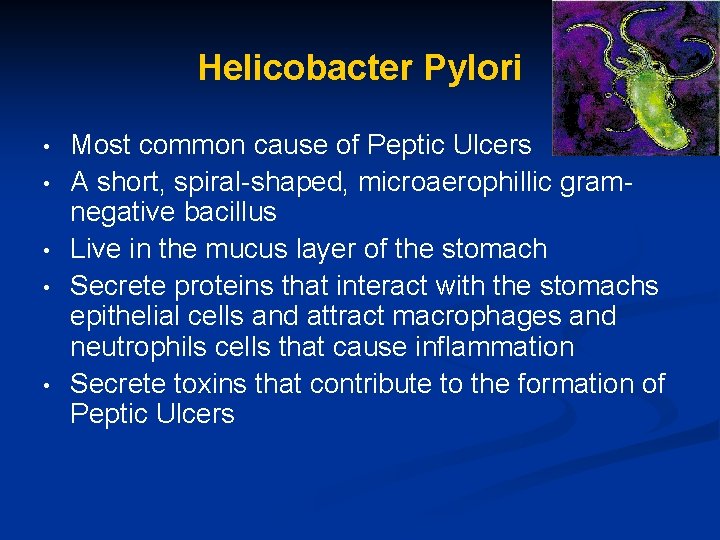
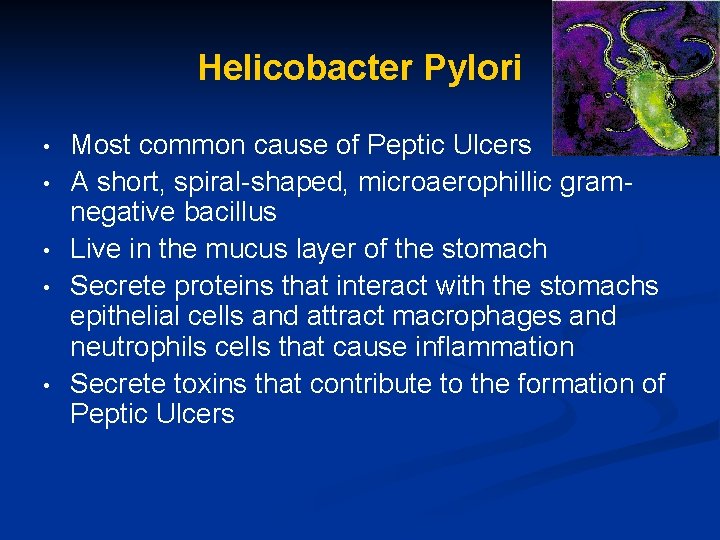
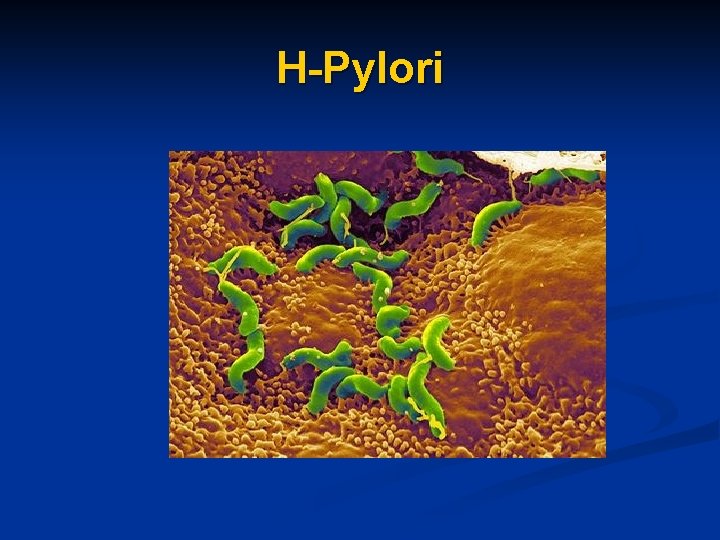
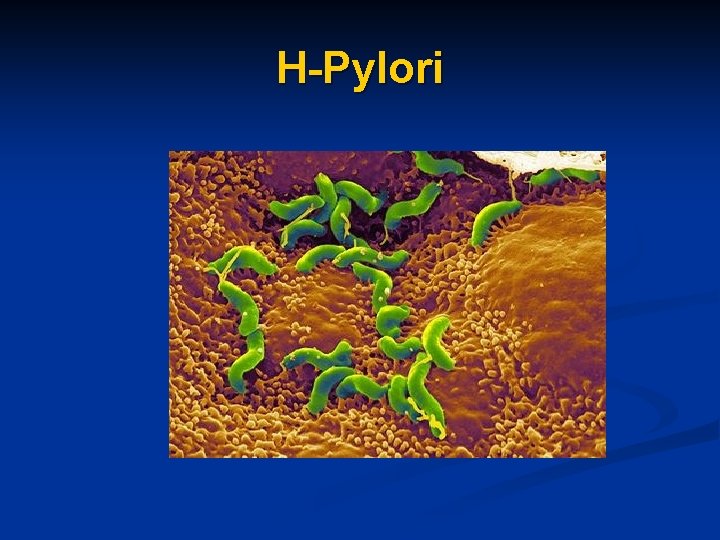
Helicobacter Pylori • • • Most common cause of Peptic Ulcers A short, spiral-shaped, microaerophillic gramnegative bacillus Live in the mucus layer of the stomach Secrete proteins that interact with the stomachs epithelial cells and attract macrophages and neutrophils cells that cause inflammation Secrete toxins that contribute to the formation of Peptic Ulcers
H-Pylori
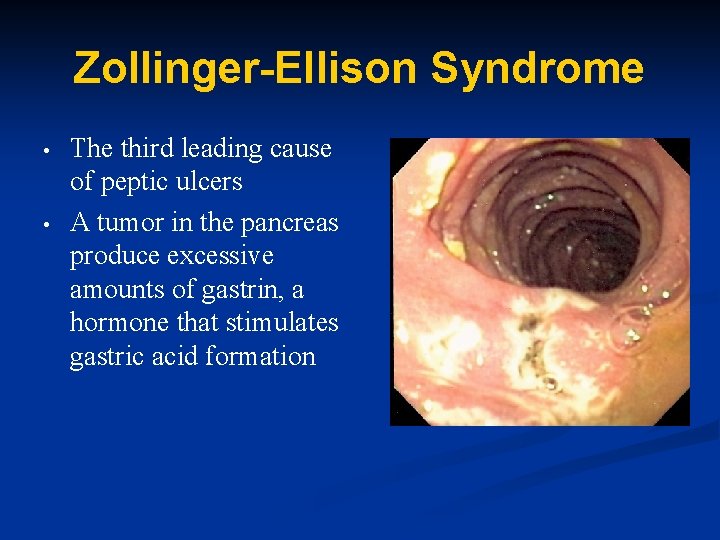
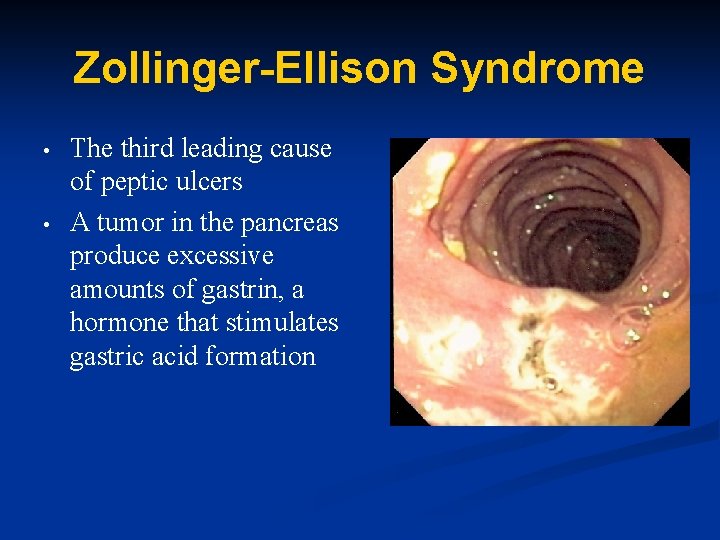
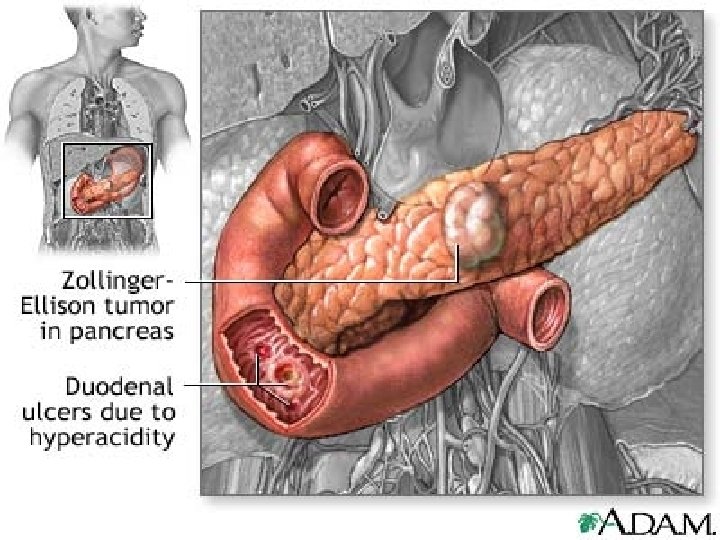
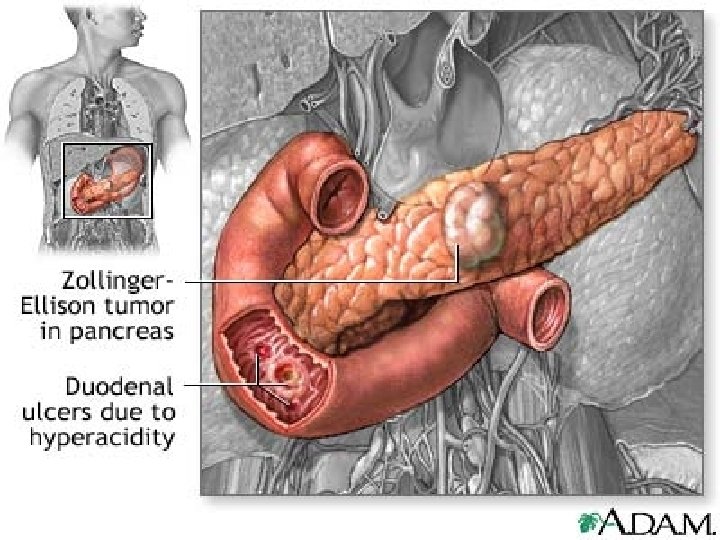
Zollinger-Ellison Syndrome • • The third leading cause of peptic ulcers A tumor in the pancreas produce excessive amounts of gastrin, a hormone that stimulates gastric acid formation
Signs & Symptoms: Peptic Ulcers Disease • • • Anemia (Fatique, dyspnea) GI bleeding Dyspepsia – encompasses a wide variety of problems in the upper abdomen/epigastric dysfunction after meals. Pain Discomfort Bloating Nausea Heartburn Regurgitation Belching
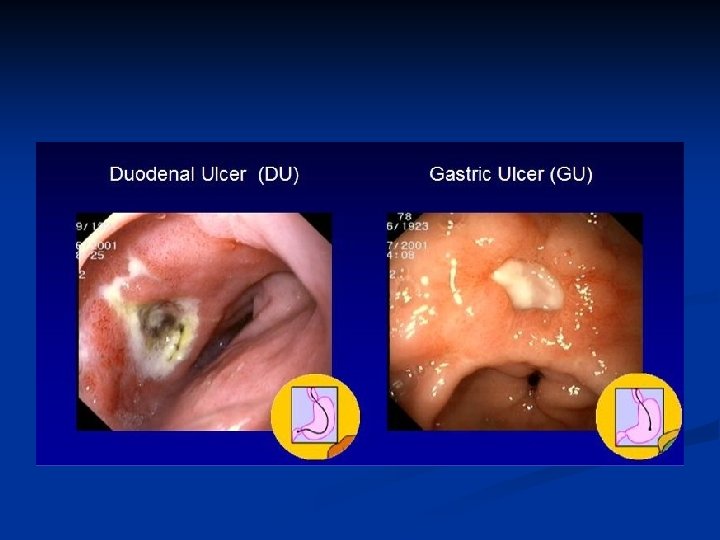
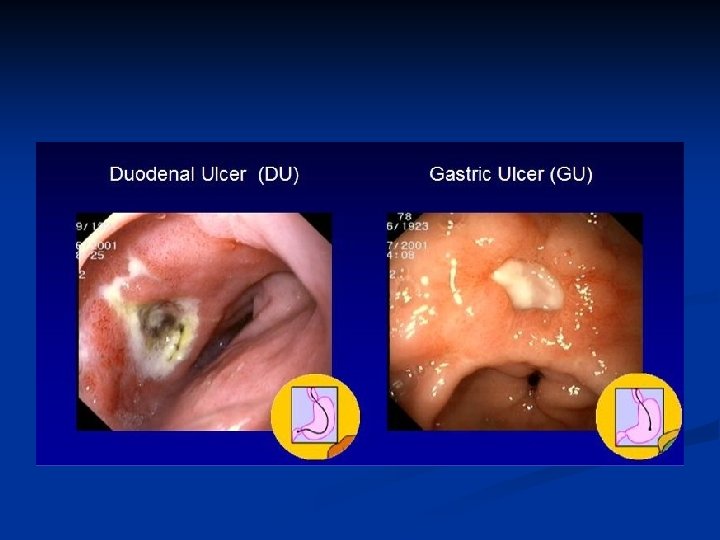
Gastric Ulcers • • • Commonly located lesser curvature close to pylorus Normal to low secretion gastric acids but back diffusion of acid is greater (than with duodenal ulcers) Can be acute or chronic H-pylori 50 -70% of patients NSAIDS, aspirin & corticosteroids cause acute gastric ulcers Chronic alcohol abuse, smoking
Duodenal Ulcers • • • Most common of all peptic ulcers Associated with high acid secretion Increased risk with COPD, cirrhosis, chronic pancreatitis, CRF, Zollinger-Ellison Syndrome, alcohol & heavy smoking. H-pylori identified 90 -95% Persons with blood type O have an increased incidence (genetic etiology)
Stress Ulcers • • • Acute ulcers Develop following major physiologic insult trauma or surgery Form of erosive gastritis Gastric muscosa undergoes a period of transient ischemia in association of hypotension, severe injury, extensive burns & complicated surgery multiple superficial erosions may bleed Risk factors for developing stress ulcers bleeding, resp failure & coagulopathy
Medications • • • Antacids ( Maalox, Mylanta) -Neutralizes gastric acidity H 2 Receptor Antagonists (Pepcid, Zantac) – Inhibits acid secretion Proton Pump Inhibitors (Prevacid) – Inhibits the mechanism that pumps acid into stomach Gastrointestinal Agents (Carafate) – Prevent relapse Prostaglandins (Cytotec) – Prevention in Pt’s taking NSAIDS and may be used with NSAIDS in Pt’s at a high risk of complications
QUESTION What factors do you think the nurse should consider when conducting a nursing assessment of a client suspected of a peptic ulcer?
Patient Assessment • • Age & Sex Occupation/daily stressors Diet- including caffeine and alcohol intake Use of Tobacco Medical and family History Medications History of when GI upset and pain occur
Three major Complications Peptic Ulcer Disease • • • Hemorrhage- most common complication. Erosion of granulation tissue at base of ulcer during healing or erosion through a major blood vessel- mostly duodenal Perforation- most lethal peptic ulcer. Large penetrating duodenal ulcers have not healed & posterior mucosal wall Gastric outlet obstruction- ulcers antrum & pyloric areas stomach & duodenum cause predisposition Narrowing pylorus due to edema, inflammation & spasms Long hx ulcer pain Relief from belching or self-induced vomiting (projectile)
Interventions Hemorrhage • • • Npo, IV Note changes in V/S NG maintain patency Assess abd distension infers blocked NG CBC- hgb & hct Administer meds as ordered IV
Interventions Perforation Assessment sudden severe, severe abd pain Rigid, boardlike abd, severe generalized abd & shoulder pain, drawing up knees • BS may diminish & become absent • Q 15 min V/S • Npo, IV • Patient allergies know • Initiate A/B • Prep for surgery •
Interventions for Outlet gastric Obstruction • • • Insert NG tube and prepare for iced saline lavage Prepare for surgery protocol Monitor vitals Arrange Hemoglobin and Hematocrit evaluation – determines blood loss status Withhold all oral foods and fluids – prepares bowel for surgery, decreases stimulus to the area
Diagnostic Tests • • • Endoscopy-view entire gastric & duodenal mucosa, determine degree healing after Rx, tissue specimens (H. pyloir, ca) Cytology (H-pylori, CBC, liver enzymes, serum amylase) U/A & stool specimens (blood) Urea breath test Upper GI Series ( Barium swallow)- beneficial Dx gastric outlet obstruction Gastric analysis
QUESTION • What are the main nursing diagnosis related to a client diagnosed with a peptic ulcer?
NURSING DIAGNOSIS • • Pain Potential for • hemorrhage • perforation • obstruction Constipation/ Diarrhea Potential altered health maintenance
Diagnosis cont’d • • Constipation/Diarrhea r/t effects of medication on bowel function Potential altered health maintenance r/t lack of knowledge of disease process, contraindications, S&S of complications, and treatment regimen
PAIN R/T GASTRIC & MUCOSAL INJURY • As manifested by : • • • Epigastric to left upper quadrant Frequently described as burning May radiate to the back Usually occurs 1 -5 hr after meals May be related by food, antacids (Duodenal), or vomiting (Gastric)
Intervention for Pain • • Administer antacids, anticholinergics, H 2 blockers as directed by physician Encourage lifestyle changes such as diet, exercise, stress, smoking, alcohol, caffeine, etc. Teach rationale avoiding OTC drugs (aspirin) Antibiotics for H-Pylori
Nutrition PUD • • • Have small and more frequent meals Avoid drinking liquids with meals Refrain from skipping meals Eliminate caffeine and alcohol Abstain from hot , spicy foods If a smoker, QUIT
Surgery • • Ulcer surgery is a procedure used to cure PUD when medications and other interventions have failed Used to relieve a present PUD and to prevent recurrence
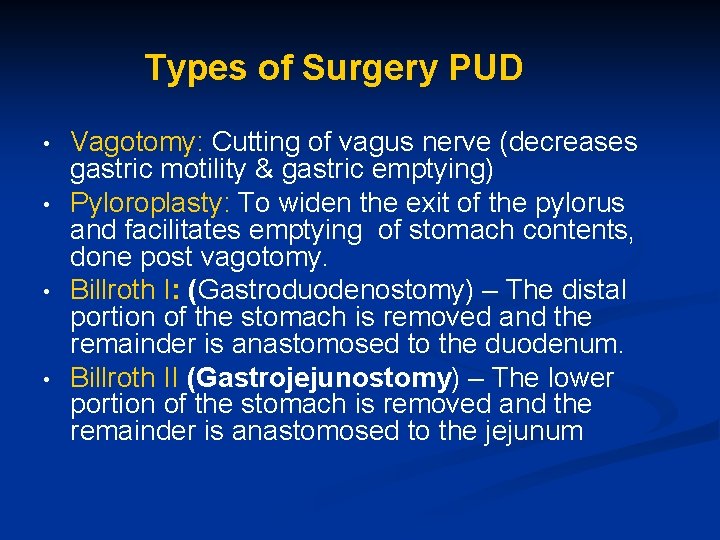
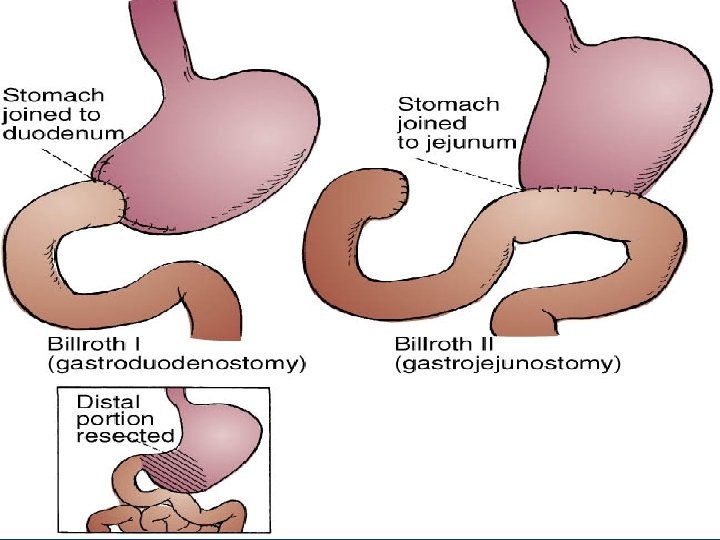
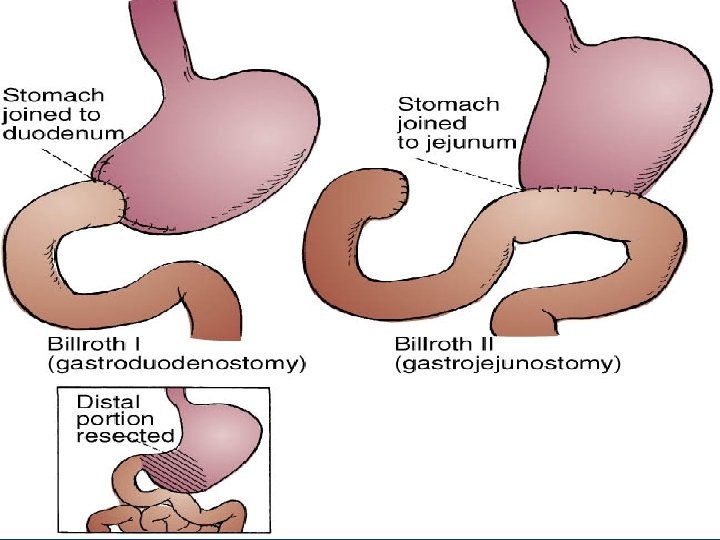
Types of Surgery PUD • • Vagotomy: Cutting of vagus nerve (decreases gastric motility & gastric emptying) Pyloroplasty: To widen the exit of the pylorus and facilitates emptying of stomach contents, done post vagotomy. Billroth I: (Gastroduodenostomy) – The distal portion of the stomach is removed and the remainder is anastomosed to the duodenum. Billroth II (Gastrojejunostomy) – The lower portion of the stomach is removed and the remainder is anastomosed to the jejunum
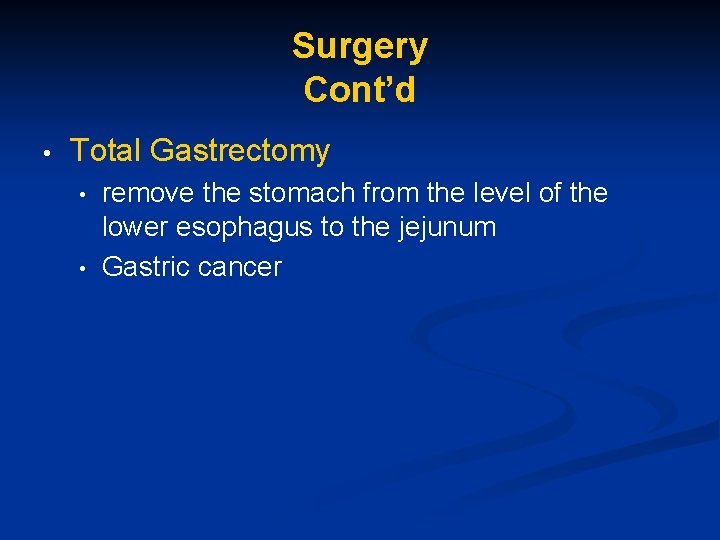
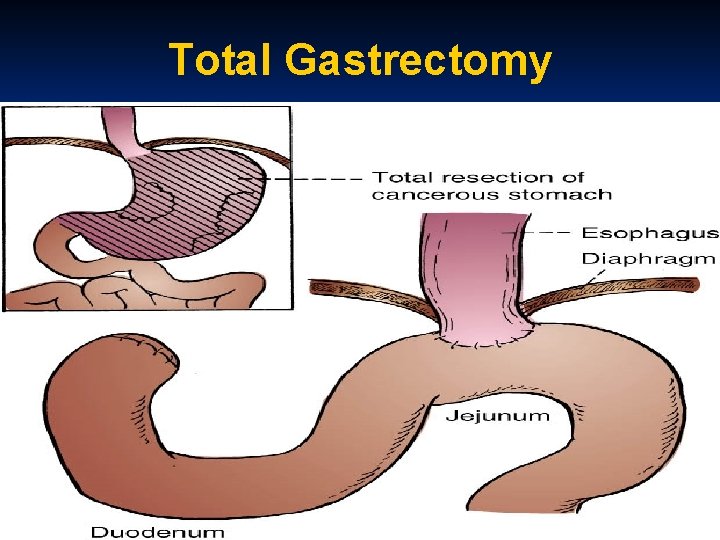
Surgery Cont’d • Total Gastrectomy • • remove the stomach from the level of the lower esophagus to the jejunum Gastric cancer
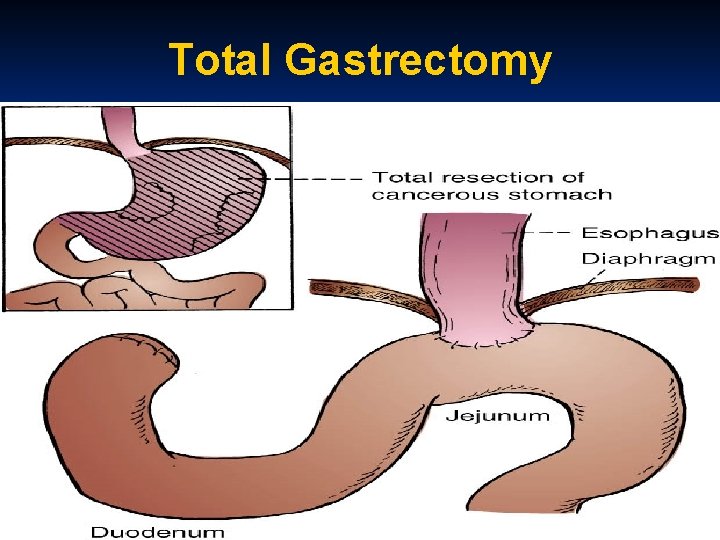
Total Gastrectomy
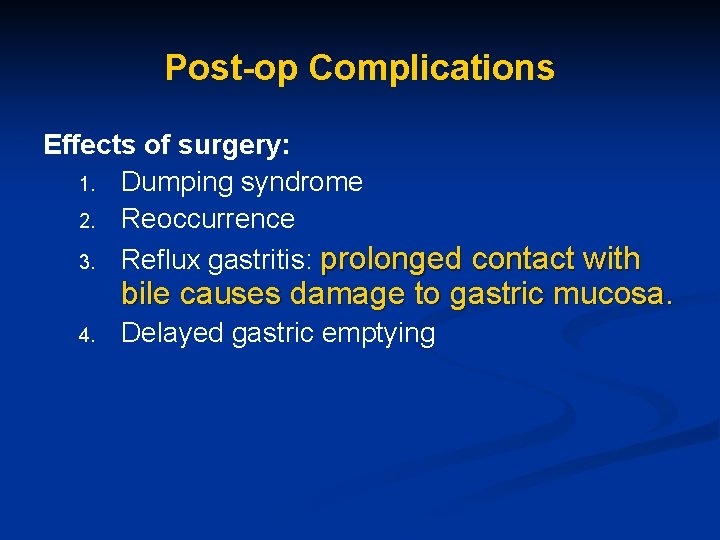
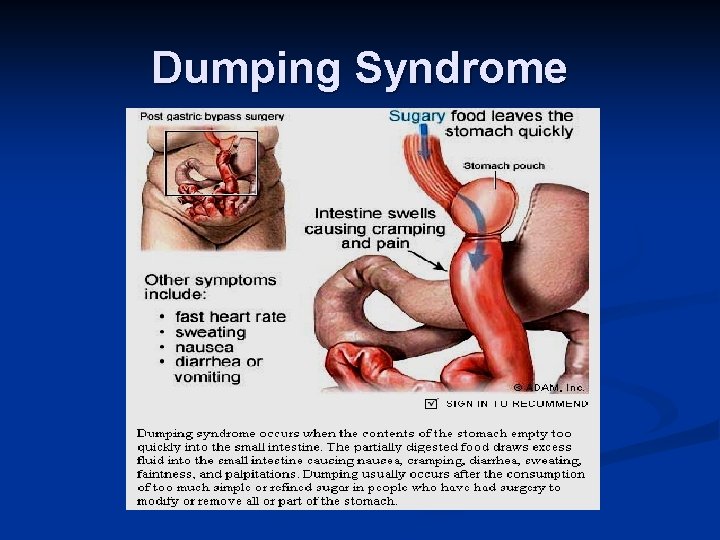
Post-op Complications Effects of surgery: 1. Dumping syndrome 2. Reoccurrence 3. Reflux gastritis: prolonged contact with bile causes damage to gastric mucosa. 4. Delayed gastric emptying
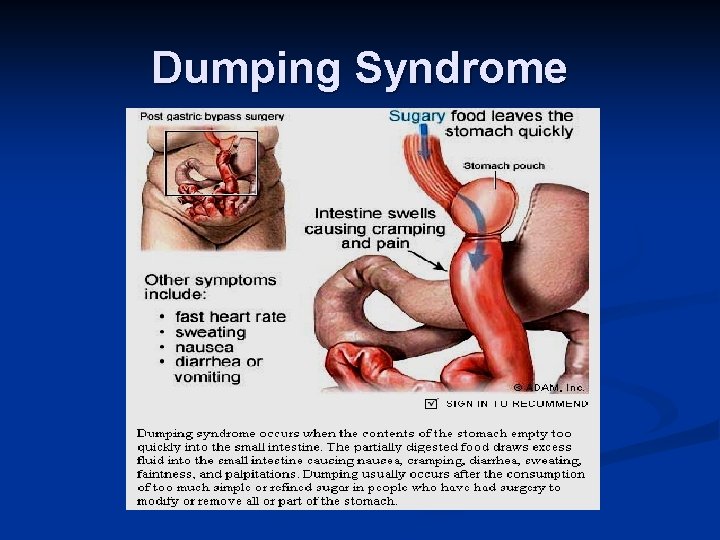
Dumping Syndrome
Read on Gastric cancers: Clinical manifestations Nursing care Food Poisoning Next Class: Lower GI