UNIT III Nervous System Nervous system Epilepsy Parkinsons
- Slides: 22
UNIT III Nervous System
• Nervous system: – Epilepsy – Parkinson’s disease – stroke • Psychiatric Disorders: – Depression – Schizophrenia – Alzheimer’s diseases
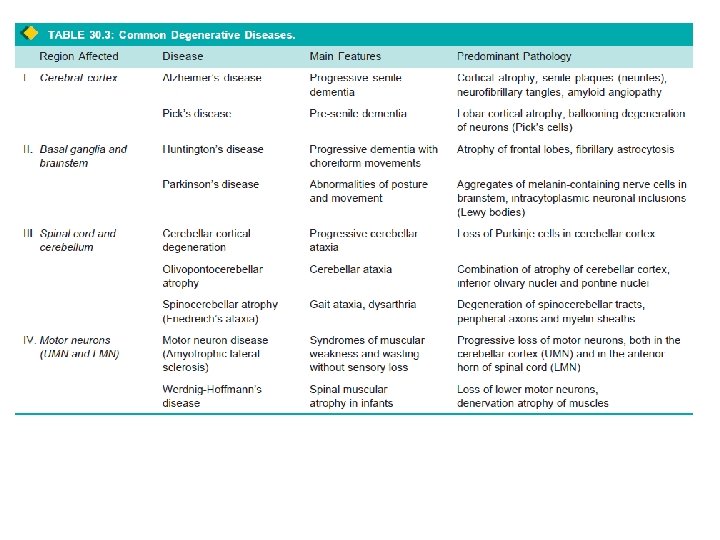
Degenerative Diseases • Disorders of unknown etiology and pathogenesis • Progressive loss of CNS neurons and their processes accompanied by fibrillary astrocytosis • Considerable proportion of degenerative disorders are genetic in origin, with either dominant or recessive inheritance; – others occur sporadically: Random • Family history is of great importance • Degenerative disorders usually begin insidiously and have a gradual progressive course over many years. • Lesions have characteristic bilaterally symmetric distribution. • Particular anatomic or physiologic system of neurons may be selectively affected, leaving others entirely intact
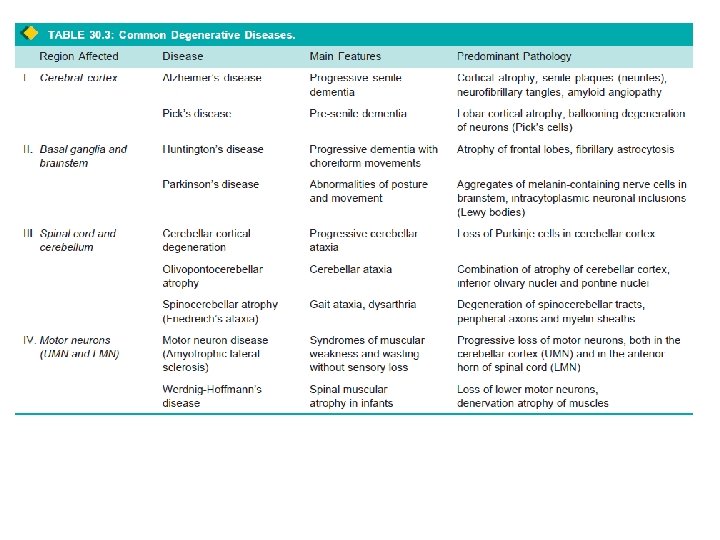
• Classification is based on clinical aspects and anatomic distribution of the lesions. • Common degenerative diseases: – Alzheimer’s disease – Parkinsonism
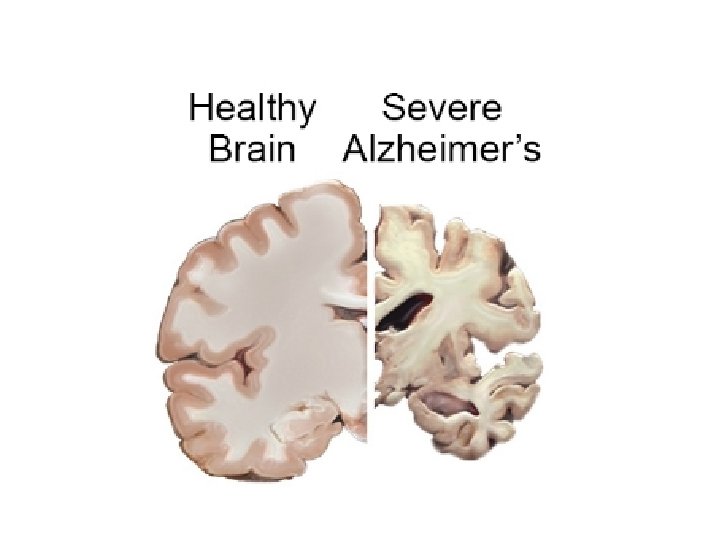
ALZHEIMER’S DISEASE • Characterised by loss of neurons and synapses in the cerebral cortex and certain subcortical regions. • loss results in gross atrophy of the affected regions, including degeneration in the temporal lobe and parietal lobe, and parts of the frontal cortex and cingulate gyrus • most common cause of dementia in the elderly • after 5 th decade of life • its incidence progressively increases with advancing age. • Unknown etiology • chronic neurodegenerative disease that usually starts slowly and gradually worsens over time.
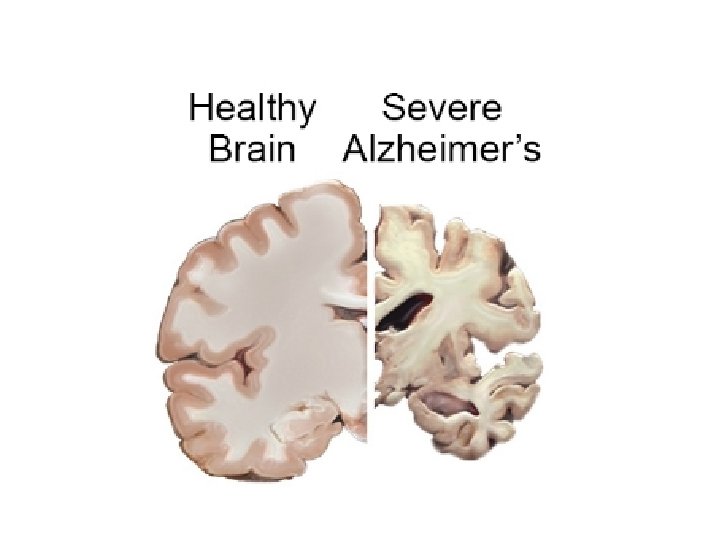
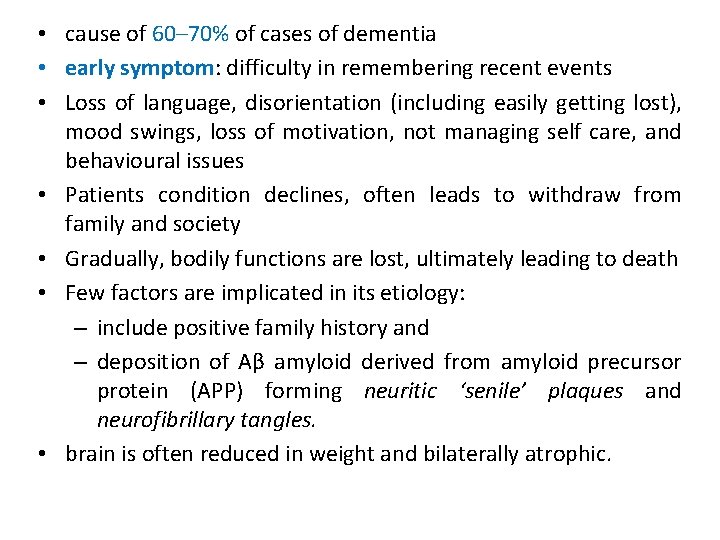
• cause of 60– 70% of cases of dementia • early symptom: difficulty in remembering recent events • Loss of language, disorientation (including easily getting lost), mood swings, loss of motivation, not managing self care, and behavioural issues • Patients condition declines, often leads to withdraw from family and society • Gradually, bodily functions are lost, ultimately leading to death • Few factors are implicated in its etiology: – include positive family history and – deposition of Aβ amyloid derived from amyloid precursor protein (APP) forming neuritic ‘senile’ plaques and neurofibrillary tangles. • brain is often reduced in weight and bilaterally atrophic.
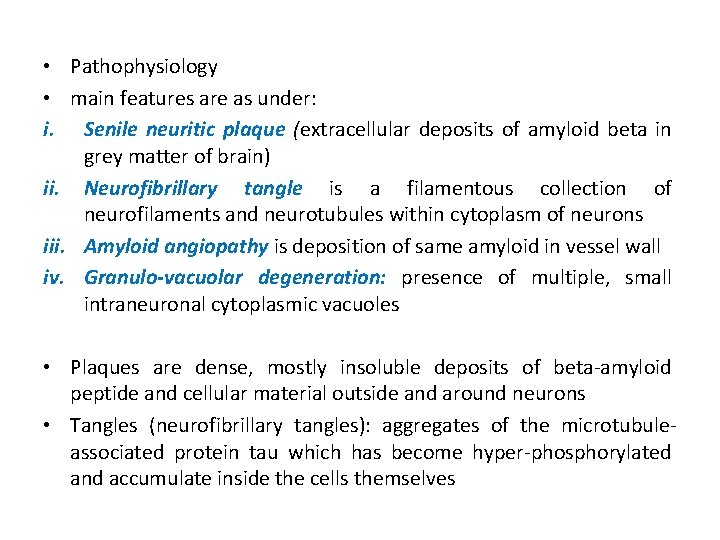
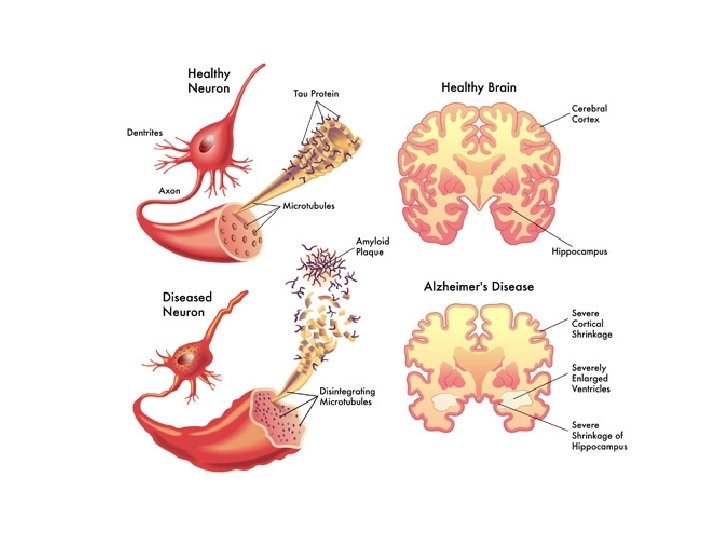
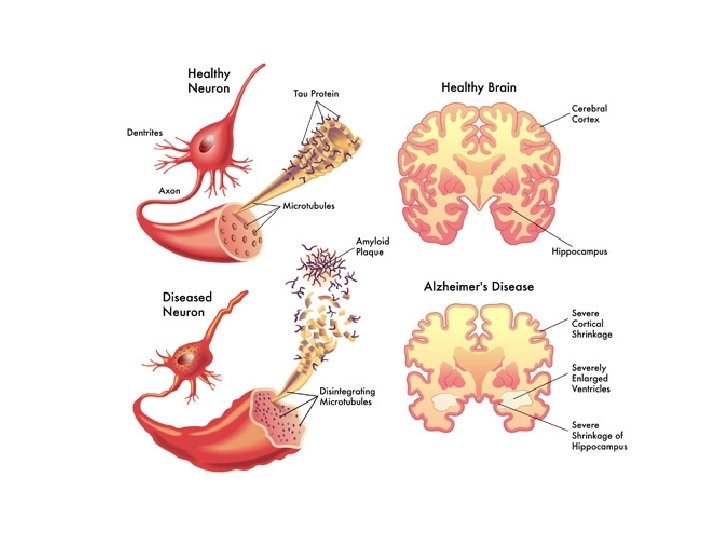
• Pathophysiology • main features are as under: i. Senile neuritic plaque (extracellular deposits of amyloid beta in grey matter of brain) ii. Neurofibrillary tangle is a filamentous collection of neurofilaments and neurotubules within cytoplasm of neurons iii. Amyloid angiopathy is deposition of same amyloid in vessel wall iv. Granulo-vacuolar degeneration: presence of multiple, small intraneuronal cytoplasmic vacuoles • Plaques are dense, mostly insoluble deposits of beta-amyloid peptide and cellular material outside and around neurons • Tangles (neurofibrillary tangles): aggregates of the microtubuleassociated protein tau which has become hyper-phosphorylated and accumulate inside the cells themselves
• protein misfolding disease (proteopathy), caused by plaque accumulation of abnormally folded in brain – amyloid beta protein – tau protein. • Plaques are made up of small peptides, 39– 43 amino acids in length, called amyloid beta (Aβ). • APP is critical to neuron growth, survival, and post-injury repair • In Alzheimer's disease, gamma secretase and beta secretase act together in a proteolytic process which causes APP to be divided into smaller fragments • One of these fragments, form clumps that deposit outside neurons in dense formations known as senile plaques
• tauopathy due to abnormal aggregation of tau protein • Neurons have microtubules, which act like tracks, guiding nutrients and molecules from body of cell to ends of the axon and back • Tau Protein stabilises microtubules when phosphorylated (called microtubule-associated protein) • In AD, tau undergoes chemical changes, becoming hyperphosphorylated • It then begins to pair with other threads, creating neurofibrillary tangles and disintegrating neuron's transport system • Pathogenic tau can also cause neuronal death through transposable element dysregulation
Disease mechanism • Etiology is not known • Amyloid toxic form of the protein responsible for disrupting cell's calcium ion homeostasis, induces programmed cell death (apoptosis) • Aβ selectively builds up in mitochondria in affected cells • It inhibits certain enzyme functions and utilisation of glucose by neurons • Various inflammatory processes and cytokines may have role • Neuro- immunological mechanisms in brain • Obesity and systemic inflammation may interfere with immunological processes which promote disease progression
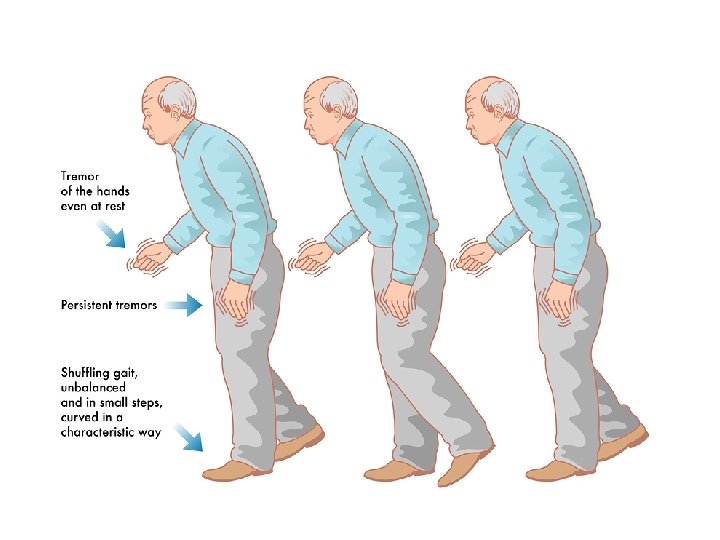
Parkinson's disease (PD) • Parkinsonism is a syndrome of chronic progressive disorder of motor function • Clinically characterised by tremors, most conspicuous at rest and worsen with emotional stress; • Other features are rigidity and disordered gait & posture. • Other causes of parkinsonism are trauma, toxic agents, and drugs (dopamine antagonists)
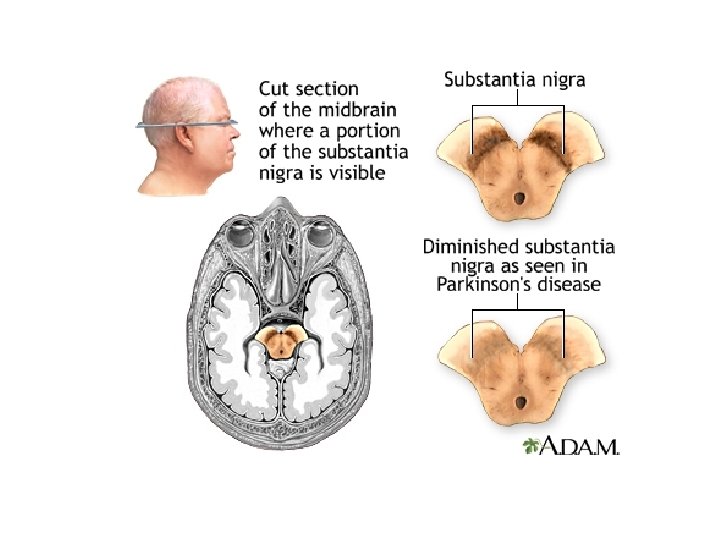
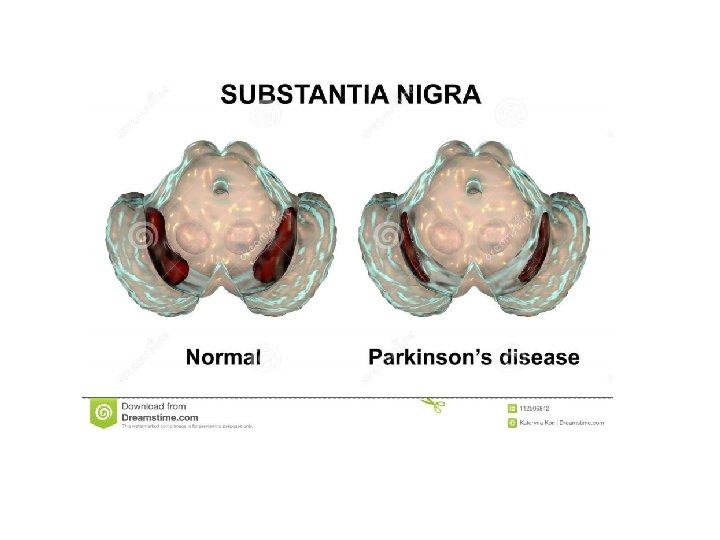
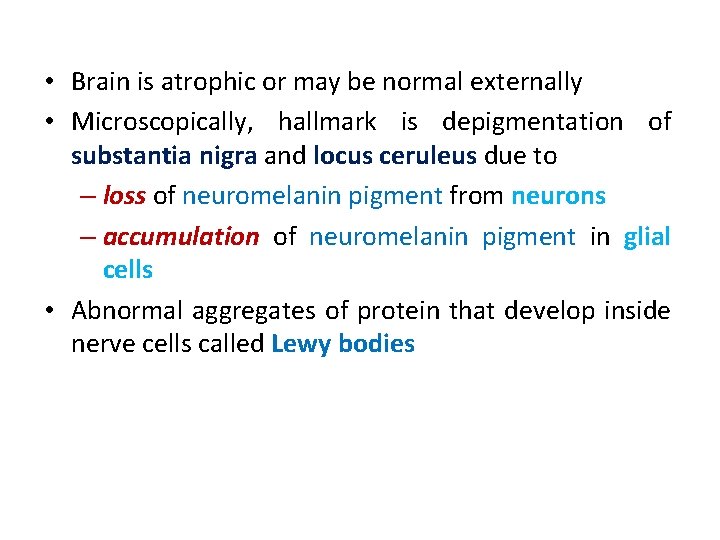
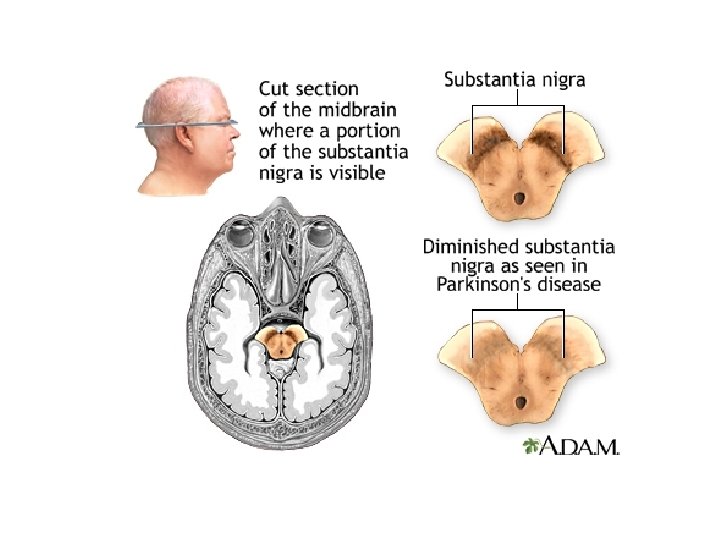
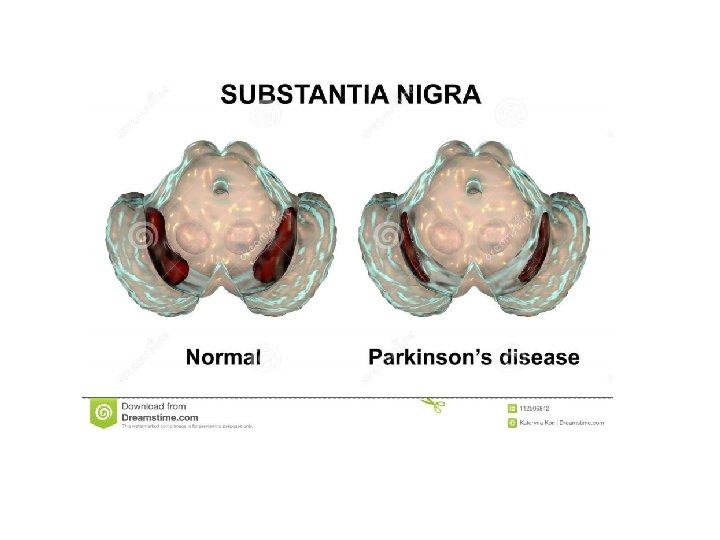
• Brain is atrophic or may be normal externally • Microscopically, hallmark is depigmentation of substantia nigra and locus ceruleus due to – loss of neuromelanin pigment from neurons – accumulation of neuromelanin pigment in glial cells • Abnormal aggregates of protein that develop inside nerve cells called Lewy bodies
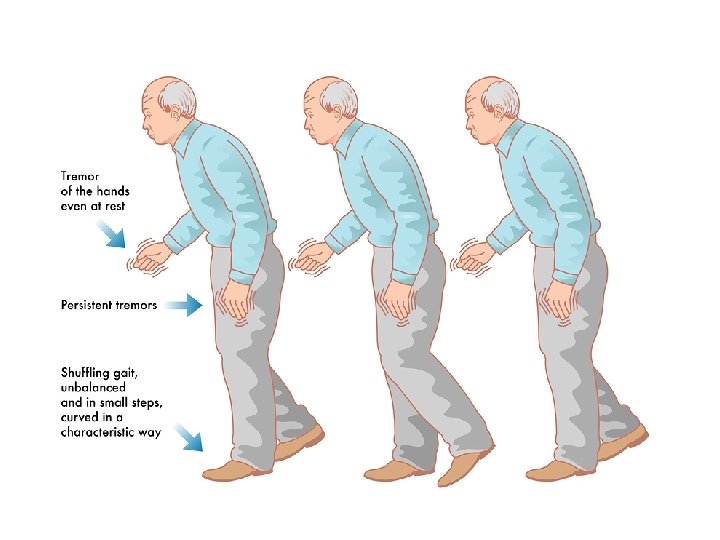
• As the disease worsens, non-motor symptoms become increasingly common. • Early symptoms, the most obvious are shaking, rigidity, slowness of movement, and difficulty with walking. • Late, thinking and behavioral problems, dementia, depression, anxiety • Sensory, sleep, and emotional problems • Cause: believed to involve both genetic and environmental factors • Motor symptoms of the disease result from death of cells in substantia nigra, a region of the midbrain – results in not enough dopamine in these areas • Diagnosis: based on symptoms • Cure: no cure
Pathogenesis • Sporadic and both autosomal dominant & recessive forms • Point mutations and duplications of gene encoding α-synuclein, a protein involved in synaptic transmission • Diagnostic feature of the disease—the Lewy body—is an inclusion containing α-synuclein • linkage between both is unclear • Two other causative genetic loci encode the proteins parkin, an E 3 ubiquitin ligase, and UCHL-1, an enzyme involved in recycling of ubiquitin from proteins targeted to the proteasome • suggesting that defects in protein degradation may have a pathogenic role • Another tantalizing clue comes from the association of PD with mutations in a protein kinase called LRRK 2 • Contribute in either Lewy bodies containing α-synuclein or tangles containing tau.
• Finally, some forms of familial PD are associated with mutations in the PARK 7 or PINK 1 genes, both of which appear to be important for normal mitochondrial function
• Reference: Textbook of Pathology, by Harsh Mohan (Author), JAYPEE Publication