Unit III GeneticDevelopmental Childhood and Mental Health Diseases












- Slides: 66
Unit III Genetic/Developmental, Childhood, and Mental Health Diseases and Disorders Copyright © 2015 Cengage Learning®.
Chapter 19 Genetic and Developmental Diseases and Disorders Copyright © 2015 Cengage Learning®.
Anatomy and Physiology • Cell nucleus – 46 chromosomes – 23 pairs • Somatic cells reproduce through mitosis – Double then divide—produce identical cells • Germ cells (sex cells) reproduce through meiosis—result in each cell carrying only half the number of chromosomes. – Haploid cells carrying 23 chromosomes Copyright © 2015 Cengage Learning®.
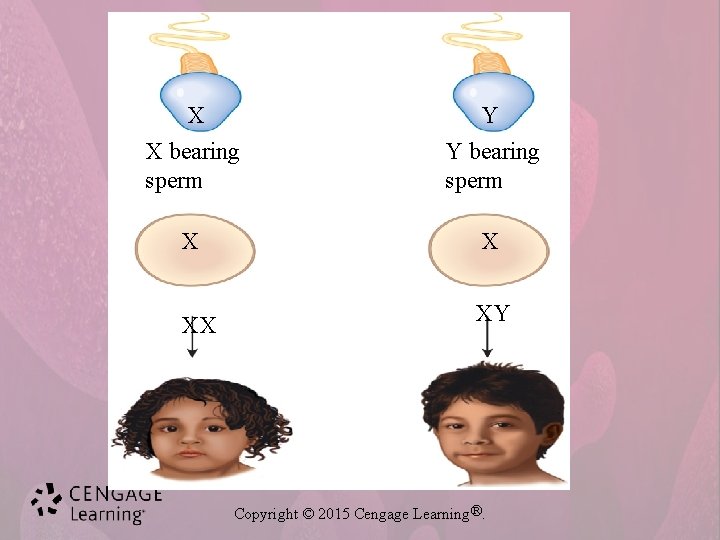
Anatomy and Physiology • Normal females – Sex chromosome is Xxthe ovum undergoes meiosis and divides into two separate X chromosomes • Normal male – Sex chromosomes is o spearate chromosomes, one X and one Y, so the male can give an X or Y – germ cells(sperm) undergo meiosis and divide into – Male sperm can be X or Y – male determines sex of child Chromosomes can be visualized by karyotyping Sex chromosomes can be evaluated by buccal smear Copyright © 2015 Cengage Learning®.
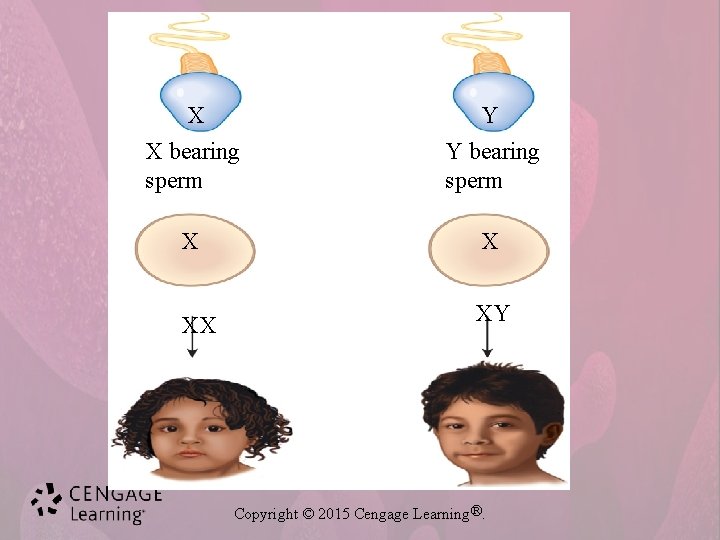
X Y X bearing sperm Y bearing sperm X X XX XY Copyright © 2015 Cengage Learning®.
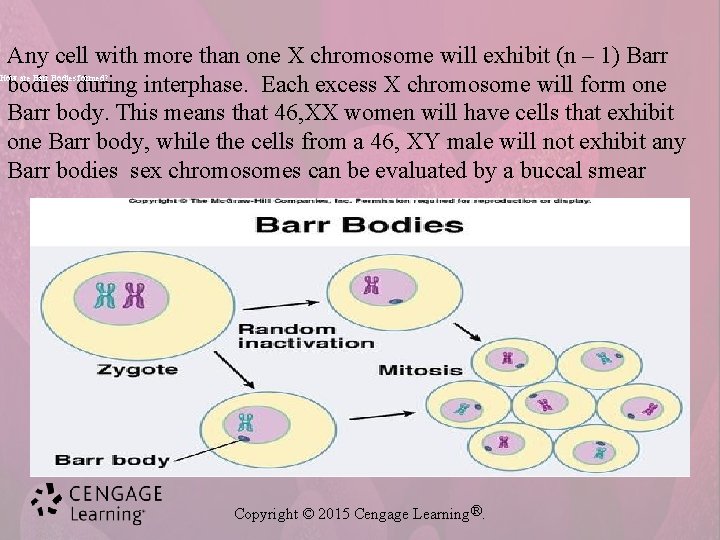
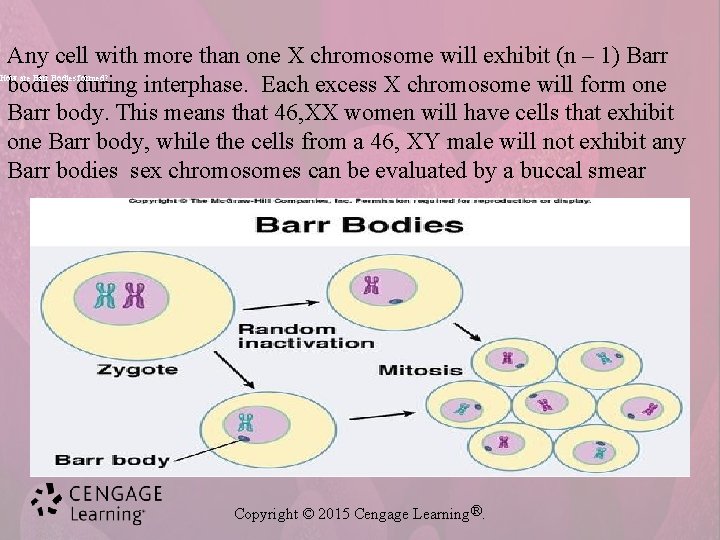
Any cell with more than one X chromosome will exhibit (n – 1) Barr bodies during interphase. Each excess X chromosome will form one Barr body. This means that 46, XX women will have cells that exhibit one Barr body, while the cells from a 46, XY male will not exhibit any Barr bodies sex chromosomes can be evaluated by a buccal smear How are Barr Bodies formed? Copyright © 2015 Cengage Learning®.
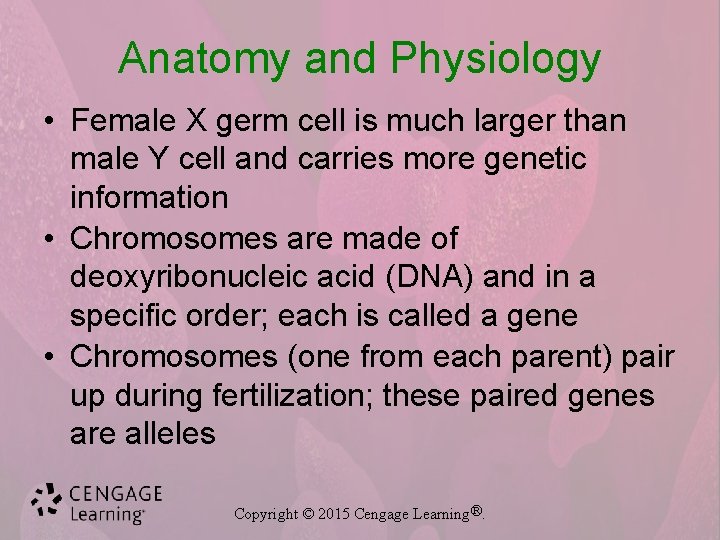
Anatomy and Physiology • Female X germ cell is much larger than male Y cell and carries more genetic information • Chromosomes are made of deoxyribonucleic acid (DNA) and in a specific order; each is called a gene • Chromosomes (one from each parent) pair up during fertilization; these paired genes are alleles Copyright © 2015 Cengage Learning®.
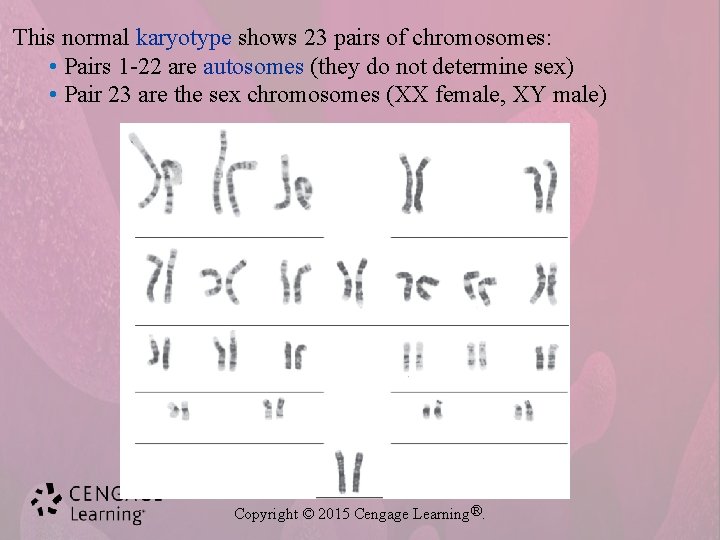
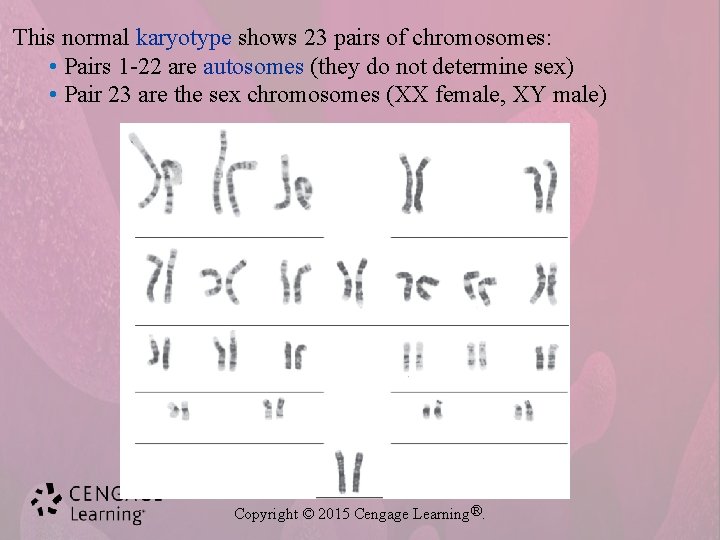
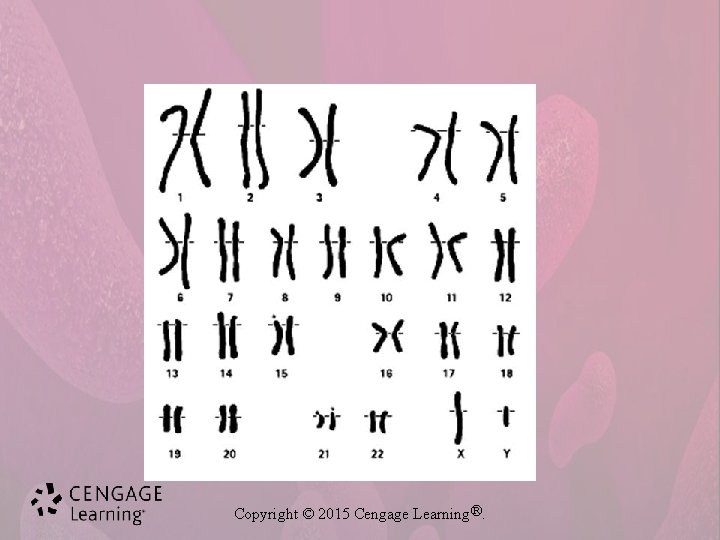
This normal karyotype shows 23 pairs of chromosomes: • Pairs 1 -22 are autosomes (they do not determine sex) • Pair 23 are the sex chromosomes (XX female, XY male) Copyright © 2015 Cengage Learning®.
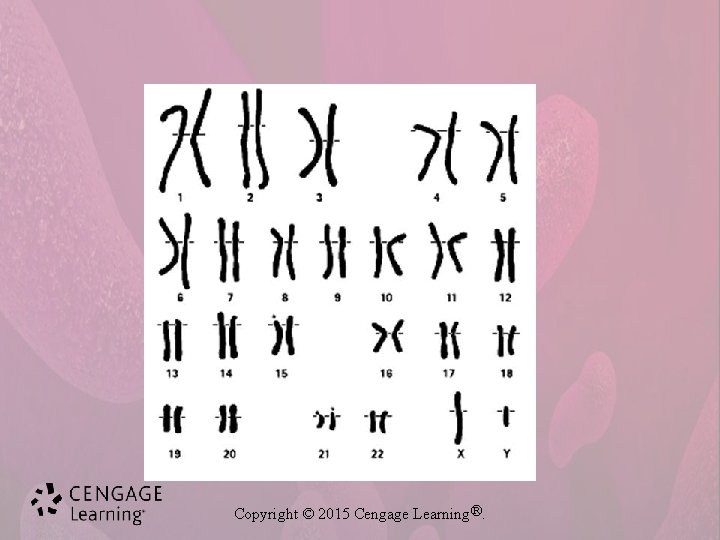
Copyright © 2015 Cengage Learning®.
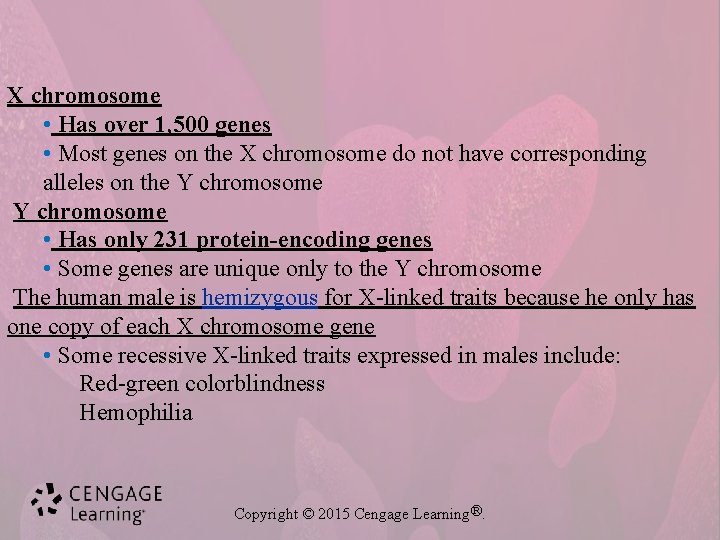
X chromosome • Has over 1, 500 genes • Most genes on the X chromosome do not have corresponding alleles on the Y chromosome • Has only 231 protein-encoding genes • Some genes are unique only to the Y chromosome The human male is hemizygous for X-linked traits because he only has one copy of each X chromosome gene • Some recessive X-linked traits expressed in males include: Red-green colorblindness Hemophilia Copyright © 2015 Cengage Learning®.
Anatomy and Physiology • Each gene in an allele can be dominant or recessive • Homozygous – matched alleles such as BB or bb • Heterozygous – unmatched alleles such as Bb • Expression of a physical trait is called phenotype Copyright © 2015 Cengage Learning®.

+ = wild type allele cf = cystic fibrosis allele Carrier parents For each child conceived 25% chance unaffected 50% chance unaffected carrier (cf noncarrier allele inherited from either parent) Copyright © 2015 Cengage Learning®. 25% chance affected
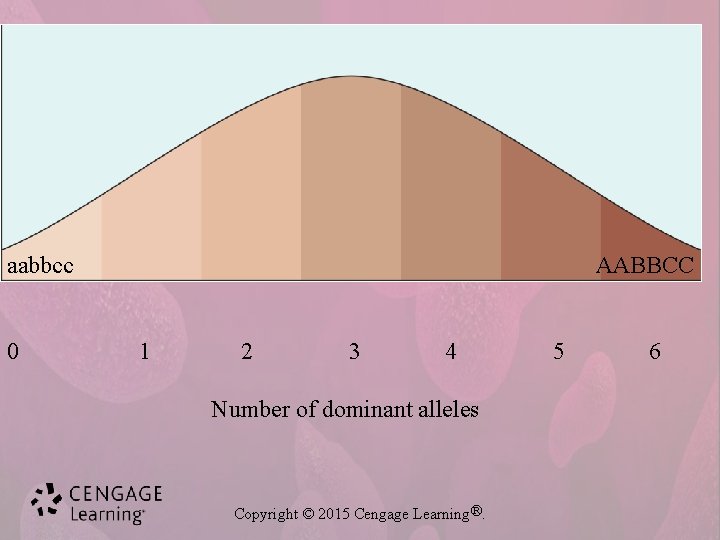
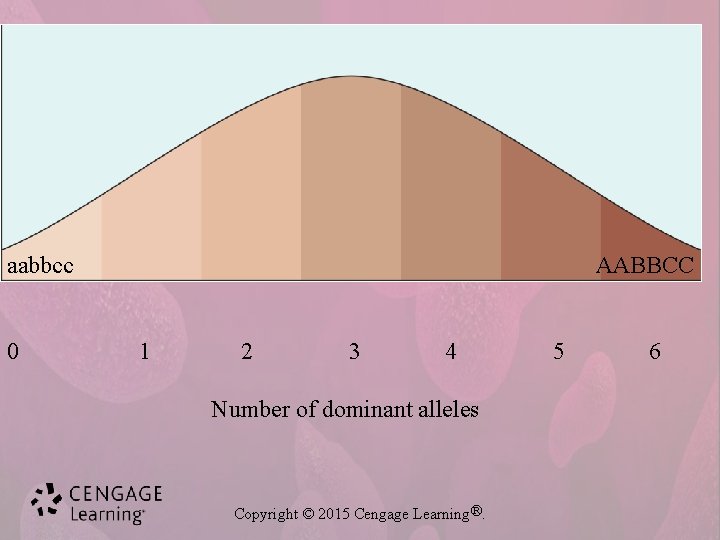
aabbcc 0 AABBCC 1 2 3 4 Number of dominant alleles Copyright © 2015 Cengage Learning®. 5 6

AABB aabb Copyright © 2015 Cengage Learning®.
Anatomy and Physiology p. 477 • Abnormalities can be due to: – – • Chromosomal disorder Genetic disorder Environmental factors Combination of above Individuals acquire abnormal genes in two ways: – Mutation of gene during meiosis – Passage of abnormal gene from parents (heredity) Copyright © 2015 Cengage Learning®.
Most if not all characteristics and disorders considered “inherited” actually reflect input from the environment as well as genes Polygenic traits • Determined by more than one gene • Examples include height, skin color, and eye color • Blood type O without genotype ii. Due to homozygous recessive expression of another gene, therefore blood types A and B are not possible – called Bombay phenotype Multifactorial traits • Traits molded by one or more genes plus environmental factors • Examples include height and skin color • Common diseases such as heart disease, diabetes mellitus, hypertension, and cancers are multifactorial Copyright © 2015 Cengage Learning®.
Deviations from the normal chromosome number of 46 produce syndromes because of the excess or deficit of genes Chromosome number abnormalities may involve single chromosomes or entire sets of chromosomes Euploid is a normal chromosome number Copyright © 2015 Cengage Learning®.
Anatomy and Physiology • Genetic disorders are passed to offspring in four ways: – Autosomal dominant – Autosomal recessive – Sex-linked dominant – Sex-linked recessive Copyright © 2015 Cengage Learning®.
Anatomy and Physiology p. 480 • Approximately 2% of newborns are born with congenital anomalies • Causes: – – 60% unknown cause 20% genetic 10% chromosomal 10% environmental Copyright © 2015 Cengage Learning®.
Diagnostic Tests • Fetal ultrasound – Detects malformations • Amniotic fluid – Reveals genetic and chromosomal disorders • Maternal blood – Reveals abnormal fetal substances Copyright © 2015 Cengage Learning®.

MD sex linked generally passed from mother to son the affected muscles are unable to store needed protein. Malnourished muscle fibers die and are replaced with fat and connective tissue. These fibers are unable to function as muscle fibers. Copyright © 2015 Cengage Learning®.
Musculoskeletal • Muscular dystrophy (MD)--– Genetic degeneration or weakening of muscles – Duchenne’s MD • Most common type – Cause: • Sex-linked disorder passes mother to son – Symptoms: • Onset between 2 and 5 years of age • Waddling gait, toe walking, lordosis, Gower’s maneuver p. 481 – Treatment: • No cure—usually in w/c by age 9. life expectancy late teens or early 20 s • Physical therapy, orthopedic devices, exercise helpful Copyright © 2015 Cengage Learning®.
Musculoskeletal p. 481 • Congenital hip dislocation (CHD) – Abnormal hip joint resulting in femoral head slipping out of normal position – Cause: • Improper positioning in uterus, maternal hormones – Symptoms: • Asymmetrical folds of affected thigh • Difference in leg length • Limited abduction – Ortolanti’s sign – Treatment: • Closed or surgical reduction of femoral head Copyright © 2015 Cengage Learning®.
Musculoskeletal • Clubfoot – Also known as talipes equinovarus – Common congenital abnormality of foot – Cause: • Unknown—thought to be due to genetic factors or fetal positioning – Symptoms: • Foot or feet turn inward with toes pointed downward and heel drawn upward – Treatment: • Gradual straightening • Cast • Splints Copyright © 2015 Cengage Learning®.
Musculoskeletal p. 483 • Most cases of osteogenesis imperfecta have an autosomal dominant pattern of inheritance, which means one copy of the altered gene in each cell is sufficient to cause the condition • Osteogenesis imperfecta – Abnormally brittle bones leading to fractures – Cause: • Inherited gene mutation – Symptoms: • Frequent bone fractures • Blue coloration of sclera of eyes – Treatment: • No cure • Tendency for bones to fracture often disappears by adulthood Copyright © 2015 Cengage Learning®.
Neurologic • Hydrocephalus – Abnormal accumulation of cerebrospinal fluid in brain due to obstruction – Cause: • Congenital defect, infection, tumor – Symptoms: • Rapid enlargement of infant head and bulging eyes • Tight scalp and prominent head veins • Shrill, high-pitched cry – Treatment: • Surgical correction with shunt placement page 483 Copyright © 2015 Cengage Learning®.

Neurologic • Cerebral palsy – Congenital bilateral paralysis – Cause: • Inadequate blood or oxygen supply to brain during fetal development, birthing process, or infancy – Symptoms: • Hyperactive reflexes and rapid muscle contraction • Muscle weakness with scissors gait Copyright © 2015 Cengage Learning®.
Neurologic • Cerebral palsy – Treatment: • • Physical and speech therapy Orthopedic cast, braces, and surgery Anticonvulsants Muscle relaxants – No cure Copyright © 2015 Cengage Learning®.
Neurologic • Spina bifida----- 483 -(484 look at image) – Congenital disorder • Opening in spinal column – Cause: • Unknown • Risk factors include maternal radiation, virus, genetic factors – Symptoms: • Differ with form of disease – Forms of spina bifida • Spina bifida occulta • Meningocele • Myelomeningocele—most serious – Treatment: Surgery Copyright © 2015 Cengage Learning®.
Neurologic p. 484 -485 • Huntington’s disease – Genetic defect of chromosome 4 – Cause: • Genetic – if one parent has disorder, 50% chance in offspring – Symptoms: • Behavioral changes • Unsteady gait • Increasing dementia – Treatment: • No cure • Medications reduce symptoms Copyright © 2015 Cengage Learning®.
Eventually, a person with Huntington's disease requires help with all activities of daily living and care. Late in the disease, he or she will likely be confined to a bed and unable to speak. However, he or she is generally able to understand language and has an awareness of family and friends. Common causes of death include: Pneumonia or other infections Injuries related to falls Complications related to the inability to swallow Copyright © 2015 Cengage Learning®.

Cardiovascular p. 485 • Congenital heart defects – Heart and related vessels are most common sites of congenital defects – Defects can range from small to quite large – Collectively, these malformations are called congenital heart defects Copyright © 2015 Cengage Learning®.
Cardiovascular • Congenital heart defects (continued) – Cause: • Unknown, but genetic tendency is strongly suspected – Symptoms: • Vary from mild (asymptomatic) to extreme with cyanosis, breathing difficulty, and heart murmurs – Diagnosis: • Electrocardiogram • Physical examination – Treatment: • Early diagnosis • Surgery to correct the defect Copyright © 2015 Cengage Learning®.
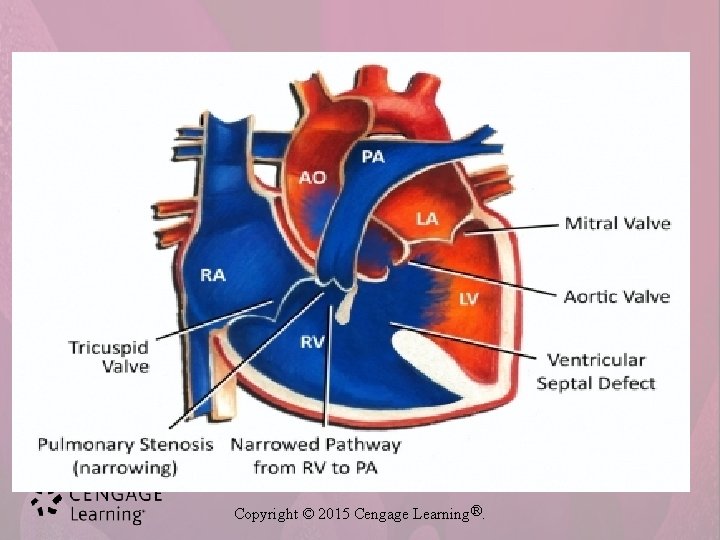
Cardiovascular • Congenital heart defects (continued) – Atrial septal defect • Opening between right and left atria • Commonly due to foramen ovale not closing at birth • Causes increased workload on right heart— blood from the left atria can go back through ovale to R atria to be pumped to lungs again—this repumping causes increased workload Copyright © 2015 Cengage Learning®.
Cont. Ventricular septal defect • Most common heart defect— 25% • Hole between right and left • Blood shunted from left to right • Causes increased workload on right heart The ductus arteriosus like the foramen ovale, normally closes off shortly after birth. If the structure does not close, or remains patent, the condition is called patent ductus arteriosus Copyright © 2015 Cengage Learning®.
Cardiovascular • Congenital heart defects (continued) – Patent ductus arteriosus--—occurs twice as frequently in girls as boys • Connection between pulmonary artery and aorta that does not close off after birth • Blood shunts from aorta to pulmonary artery • Causes increased workload on heart and pulmonary system – Coarctation of aorta • Stricture or narrowing of aorta • Causes increased blood pressure proximal to narrowingally— lower blood pressure dist • Causes increased workload on heart Copyright © 2015 Cengage Learning®.
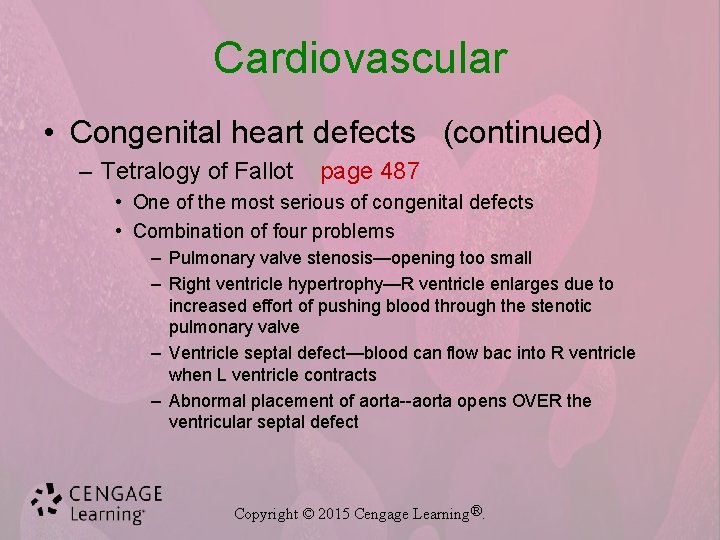
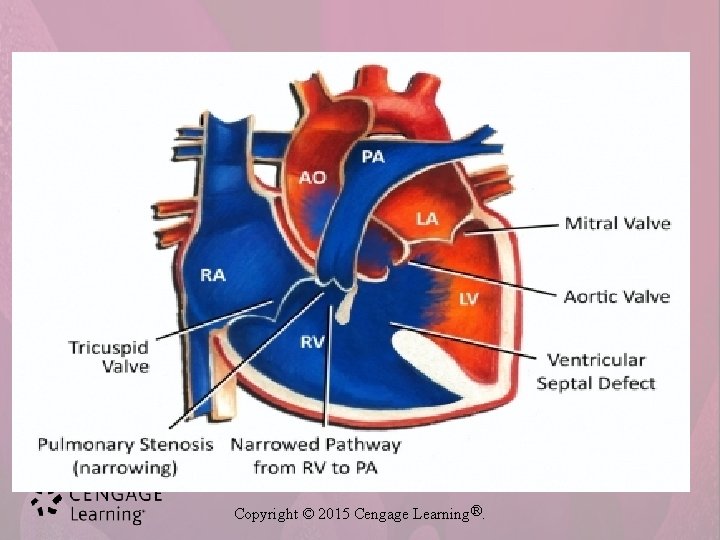
Cardiovascular • Congenital heart defects (continued) – Tetralogy of Fallot page 487 • One of the most serious of congenital defects • Combination of four problems – Pulmonary valve stenosis—opening too small – Right ventricle hypertrophy—R ventricle enlarges due to increased effort of pushing blood through the stenotic pulmonary valve – Ventricle septal defect—blood can flow bac into R ventricle when L ventricle contracts – Abnormal placement of aorta--aorta opens OVER the ventricular septal defect Copyright © 2015 Cengage Learning®.
Copyright © 2015 Cengage Learning®.
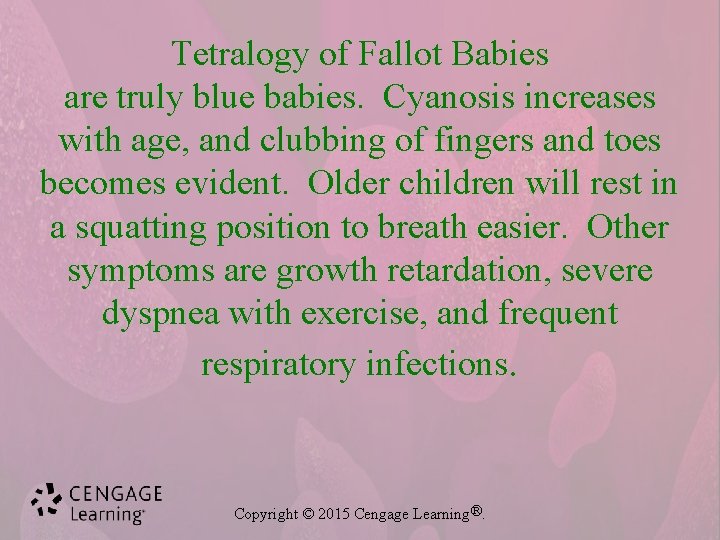
Tetralogy of Fallot Babies are truly blue babies. Cyanosis increases with age, and clubbing of fingers and toes becomes evident. Older children will rest in a squatting position to breath easier. Other symptoms are growth retardation, severe dyspnea with exercise, and frequent respiratory infections. Copyright © 2015 Cengage Learning®.

Blood • Sickle cell anemia – (discussed in detail in Chapter 7) – Chronic hereditary form of anemia – Predominantly affects black population • Hemophilia – (discussed in detail in Chapter 7) – X-linked hereditary disorder passed from mother to son Copyright © 2015 Cengage Learning®.
Digestive p. 488 • Digestive disorders both genetic and developmental range from mild to severe • Many are diagnosed at birth • Some are incompatible with life and must be corrected immediately Copyright © 2015 Cengage Learning®.
Digestive • Developmental malformations – Several developmental malformations occur in the digestive system – Cause: • Unknown • Might be related to genetic tendencies • Might be related to maternal risk factors – Maternal rubella – Poor maternal nutrition – Smoking – Alcoholism Copyright © 2015 Cengage Learning®.
Digestive Developmental malformations (continued) – Meckel’s diverticulum • Outpouching of diverticulum of the ileum—may be asymptomatic the entire life and only found on autopsy – Esophageal atresia • Abnormal esophagus • (atresia—is the congenital absence or closure of a normal opening or lumen in the body and can occur in a variety of areas) – Congenital diaphragmatic hernia • A hole in the diaphragm—abdominal organs might herniate through this opening Copyright © 2015 Cengage Learning®.
Digestive • Developmental malformations (continued) p. 489 – Imperforate anus • Failure of the anus to connect to the rectum—infant will not pass stool. Abdominal pain and cramping with vomiting. Must be surgical corrected – Cleft lip—affects nursing, speech, increases respiratory and middle ear infections • One or more splits in upper lip • Affects boys more frequently than girls • Treatment: – Surgical repair Copyright © 2015 Cengage Learning®.
Digestive • Developmental malformations (continued) – Cleft palate—hard palate (roof of mouth) does not close • More serious than cleft lip • Involves roof of mouth • Treatment: – Surgical repair – Again causes problems with feeding, speaking, increases respiratory infections and middle ear infections Copyright © 2015 Cengage Learning®.

Cleft Lip and Palate Photo courtesy Dr. Joseph Konzelman, School of Dentistry, Medical College of Georgia Copyright © 2015 Cengage Learning®.

Cleft Lip and Palate Photo courtesy Dr. Joseph Konzelman, School of Dentistry, Medical College of Georgia Copyright © 2015 Cengage Learning®.
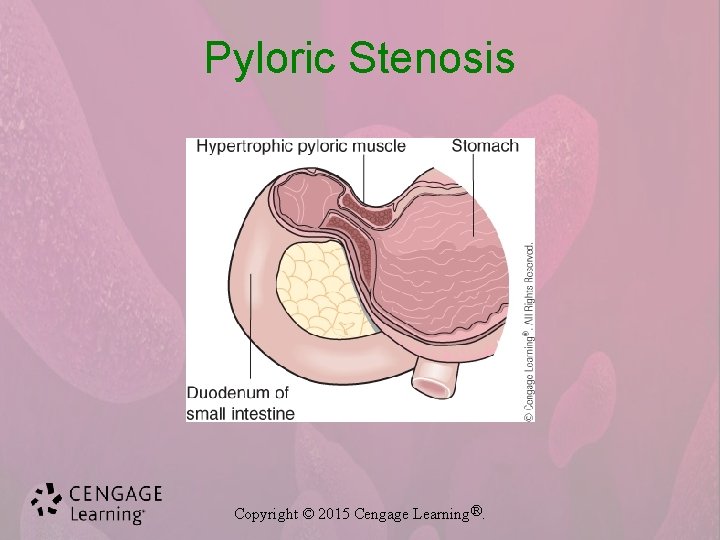
Digestive • Genetic digestive disorders p. 490 – Pyloric stenosis • Narrowing of lower end of stomach • Common anomaly of digestive tract • Symptoms: – Projectile vomiting • Treatment: – Pylorotomy—incising and suturing the pyloric sphincter muscle. Copyright © 2015 Cengage Learning®.
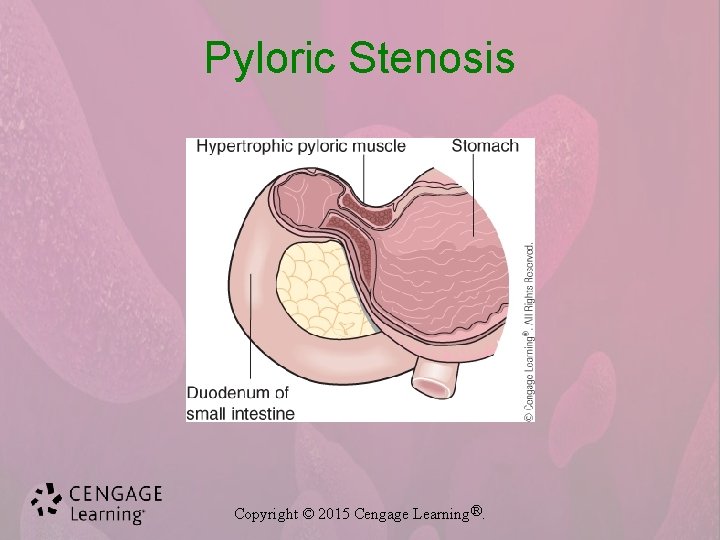
Pyloric Stenosis Copyright © 2015 Cengage Learning®.
Digestive • Genetic digestive disorders (continued) – Hirschsprung’s disease—seen more often in boys and those with Downs syndrom • Absence of nerves in segment of colon – Usually sigmoid colon—there is no peristalsis in this area. • Symptoms: – Chronic constipation – Abdominal distention—massive distention of the colon • Treatment: – Surgical removal of affected segment – Temporary colostomy may be necessary to allow adequate healing of colon Copyright © 2015 Cengage Learning®.
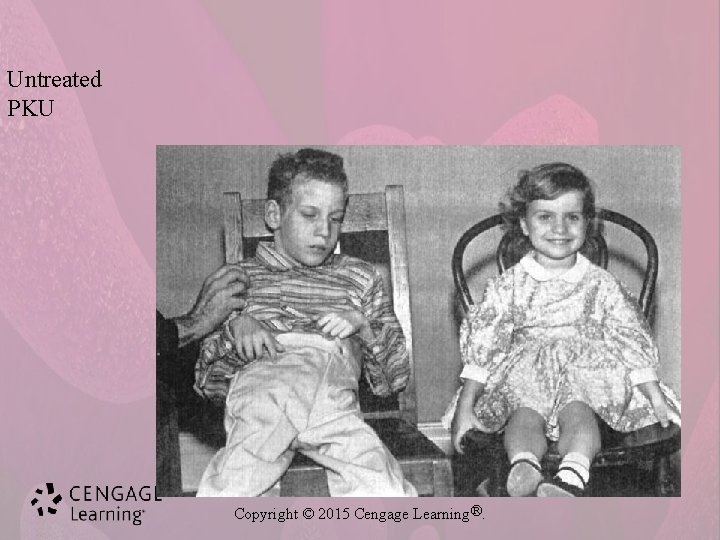
Digestive • Genetic digestive disorders (continued) – Phenylketonuria (PKU) • Genetic disorder involving faulty metabolism of protein phenylalanine • Diagnosis by blood test 72 hours after birth – Mandatory in United States • Lack of treatment can result in mental disability Copyright © 2015 Cengage Learning®.

Copyright © 2015 Cengage Learning®.
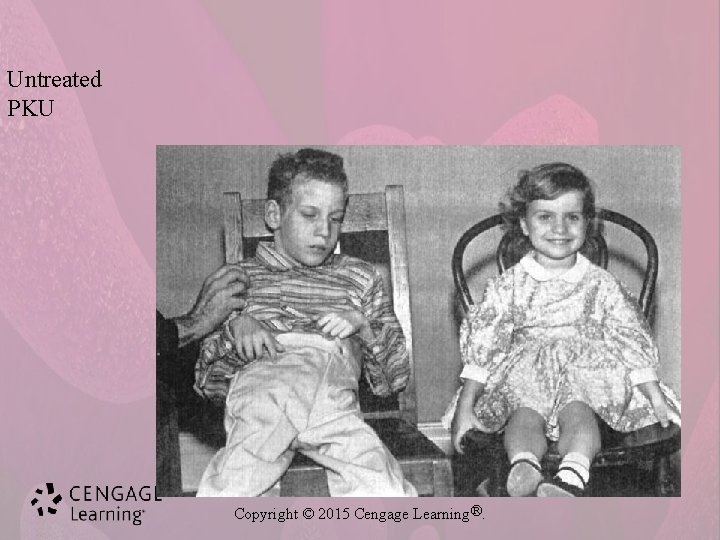
Untreated PKU Copyright © 2015 Cengage Learning®.
Urinary all can lead to problems with elimination of urine and can lead to difficulty with intecourse • Hypospadias – Abnormal congenital opening of male urinary meatus on under surface of penis—it can be severe with locations midshaft or near the scrotum. It occurs in 1 in 250 boys • Chordee – Abnormal fibrous band of tissue—abnormal downward curvature • Epispadias – Abnormal congenital opening of male urinary meatus on upper surface of penis – Cause of these conditions: • Unknown – Treatments: No treatment to surgical repair Copyright © 2015 Cengage Learning®.

Urinary • Wilms’ tumor – Most common solid tumor affecting children and infants – Cause: • Thought to be genetic • Highly malignant • Usually replaces one whole kidney – Symptoms: • Asymptomatic until large enough to feel in child’s stomach – Treatment: • Chemotherapy • Surgery Copyright © 2015 Cengage Learning®.
Reproductive • Cryptorchidism – Condition of undescended testes (discussed in Chapter 17) • Turner’s syndrome – Affects females; ovaries are abnormal or absent – Cause: • Chromosomal disorder • Females have only one X chromosome – Rather than two XX chromosomes – Symptoms: • Failure to develop normal secondary sex characteristics – Treatment: • Symptoms can be reduced with growth with hormones and estrogen therapy Copyright © 2015 Cengage Learning®.
Reproductive • Klinefelter’s syndrome—affects 1 in 1000 – Affects males; do not develop secondary sex characteristics – Cause: • Chromosomal disorder • Affected males have extra X chromosome—so XXY – Symptoms: • Not diagnosed until puberty due to abnormal male sexual development • Sterility, abnormally small penis and testes • General appearance of a eunuch – tall, slender body and long legs – Treatment: • Testosterone treatment and psychological counseling Copyright © 2015 Cengage Learning®.

Other Developmental Disorders • Autism – Developmental disorder characterized by difficulty communicating and in forming relationships – Cause: • Unknown – Symptoms: • Blank facial expression • Involved with self – inaccessible to others – Treatment • Behavioral therapy • Depends on severity and symptoms present Copyright © 2015 Cengage Learning®.
Other Developmental Disorders • Stuttering – – Also known as stammering Developmental speech disorder Cause: anxiety with addressing others Symptoms: • Hesitancy of starting and finishing words • Prolonged pauses between words – Treatment: • Behavior modification • Positive reinforcement Copyright © 2015 Cengage Learning®.
Multisystem Diseases and Disorders p. 494 • Cystic fibrosis – Hereditary disorder that affect all exocrine glands – Cause: • Hereditary recessive disorder – Symptoms: • Affects all exocrine glands leading to viscous secretions – Treatment: • • • Postural drainage Chest-clapping Antibiotics Bronchodilators Expectorants Oxygen Copyright © 2015 Cengage Learning®.
Multisystem Diseases and Disorders • Down syndrome—p. 494 – Also called trisomy 21 – a condition of having 3 chromosomes instead of the normal 2 in the 21 st position of the chromosome chain – Symptoms: • • • Mild to severe mental disability Flat nasal bridge Low-set ears Slanted eyes Epicanthus Thick, protruding tongue Abnormal extremities Organ defects – Treatment: • Highly individualized to maximize mental and physical abilities Copyright © 2015 Cengage Learning®.

Trauma • Failure to thrive—p. 495 – Lack of physical growth and development in infant or child – Cause: • Disturbance in mother–child relationship or failure to bond – Symptoms: • • Weight loss or failure to gain weight Anorexia, vomiting, diarrhea Irritability Rag-doll limpness Copyright © 2015 Cengage Learning®.
Trauma • Failure to thrive (continued) – Symptoms: • Unresponsiveness to affection • Avoidance of eye contact • Stiffening when cuddled – Treatment: • Teaching of mothering and nurturing behaviors to mother/parents • Promotion of self-esteem Copyright © 2015 Cengage Learning®.
Trauma • Fetal alcohol syndrome – A group of symptoms and birth defects in an infant born to a mother who consumed alcohol during pregnancy – Symptoms: • • • Varying degrees of mental disability Decreased physical development Irritability in infants Hyperactivity in older children Microcephaly Increased incidence of ventricular septal defects Copyright © 2015 Cengage Learning®.
Trauma • Congenital rubella syndrome – Transmission of rubella virus to unborn fetus – Can cause spontaneous abortion or major birth defects – The most common defects are: • • • Microcephaly Learning disorders Deafness Abnormal growth Heart defects Ocular lesions – Prevention: • Immunization – No pregnancy for 3 months after immunization Copyright © 2015 Cengage Learning®.
Rare Diseases • Anencephaly – Absence of brain or cranial vault – Not compatible with life • Achondroplasia – Decreased long bone growth leading to type of dwarfism—(what we think of as “little people” • Tay-Sachs disease – Genetic error in lipid metabolism resulting in accumulation of toxins in brain Copyright © 2015 Cengage Learning®.
 Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Chapter 32 childhood communicable diseases bioterrorism
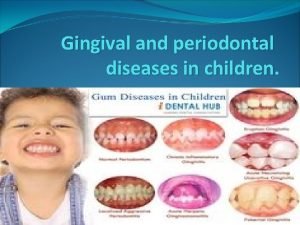
Chapter 32 childhood communicable diseases bioterrorism Retrocuspid papilla interdental clefts in primary teeth
Retrocuspid papilla interdental clefts in primary teeth Mental health and mental illness chapter 20
Mental health and mental illness chapter 20 Proximodistal development
Proximodistal development Mental health jeopardy
Mental health jeopardy Unit 2 mental and emotional health
Unit 2 mental and emotional health Hamlet act iii scene iii
Hamlet act iii scene iii Social development in adulthood
Social development in adulthood Chapter 3 achieving mental and emotional health answer key
Chapter 3 achieving mental and emotional health answer key Mental health and older adults
Mental health and older adults Lemhwa report to congress
Lemhwa report to congress Mental health and older adults
Mental health and older adults Mental health and citizenship
Mental health and citizenship Chapter 3 achieving mental and emotional health
Chapter 3 achieving mental and emotional health Glencoe health chapter 3 lesson 1 answers
Glencoe health chapter 3 lesson 1 answers Psychology, mental health and distress
Psychology, mental health and distress Mental health policy, plans and programmes michelle funk
Mental health policy, plans and programmes michelle funk Chapter 5 lesson 3 suicide prevention
Chapter 5 lesson 3 suicide prevention Chapter 3 mental and emotional health answer key
Chapter 3 mental and emotional health answer key Chapter 3 achieving mental and emotional health
Chapter 3 achieving mental and emotional health Chapter 15 achieving mental and emotional health answer key
Chapter 15 achieving mental and emotional health answer key Achieving mental and emotional health
Achieving mental and emotional health Mind map about mental health and wellbeing
Mind map about mental health and wellbeing Nice guidelines postnatal depression
Nice guidelines postnatal depression Chapter 3 mental and emotional health
Chapter 3 mental and emotional health Chapter 3 achieving mental and emotional health
Chapter 3 achieving mental and emotional health Chapter 3 achieving mental and emotional health
Chapter 3 achieving mental and emotional health Chapter 3 lesson 2 health
Chapter 3 lesson 2 health Chapter 3 achieving mental and emotional health
Chapter 3 achieving mental and emotional health Chapter 15 achieving mental and emotional health
Chapter 15 achieving mental and emotional health Unit 6 review questions
Unit 6 review questions Modern lifestyle and hypokinetic diseases
Modern lifestyle and hypokinetic diseases Communicable and noncommunicable diseases venn diagram
Communicable and noncommunicable diseases venn diagram Section 19-3 diseases caused by bacteria and viruses
Section 19-3 diseases caused by bacteria and viruses Define a primary skin lesion and list three types
Define a primary skin lesion and list three types Chapter 6 musculoskeletal system
Chapter 6 musculoskeletal system Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Chapter 22 genetics and genetically linked diseases
Chapter 22 genetics and genetically linked diseases Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Milady chapter 10
Milady chapter 10 Seborrheic keratoses
Seborrheic keratoses Chapter 10 nail disorders and diseases review questions
Chapter 10 nail disorders and diseases review questions Certain infectious and parasitic diseases
Certain infectious and parasitic diseases Chapter 8 cardiovascular system
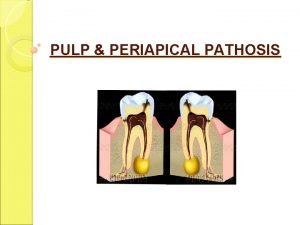
Chapter 8 cardiovascular system Pulp and periapical diseases
Pulp and periapical diseases Milady chapter 8 skin disorders and diseases
Milady chapter 8 skin disorders and diseases Venn diagram of communicable and non-communicable diseases
Venn diagram of communicable and non-communicable diseases Purulent diseases of lungs and pleura
Purulent diseases of lungs and pleura Tronsmo plant pathology and plant diseases download
Tronsmo plant pathology and plant diseases download Tronsmo plant pathology and plant diseases download
Tronsmo plant pathology and plant diseases download Albugo eye
Albugo eye Difference between communicable and noncommunicable
Difference between communicable and noncommunicable Vitamin name list
Vitamin name list Myths and fallacies about non communicable diseases
Myths and fallacies about non communicable diseases 10 diseases of lymphatic system
10 diseases of lymphatic system Health and social component 3
Health and social component 3 Frankston ccu
Frankston ccu Lenawee county cmh
Lenawee county cmh Van buren community mental health
Van buren community mental health Together for mental health
Together for mental health Mental health act 2007 made simple
Mental health act 2007 made simple Mental health triangle examples
Mental health triangle examples Introduction to mental health awareness presentation
Introduction to mental health awareness presentation Mental health committee
Mental health committee Kings fund
Kings fund