UNIT II COMMON SIGNS SYMPTOMS TOPIC EDEMA Prepared
- Slides: 35
UNIT –II COMMON SIGNS & SYMPTOMS TOPIC: EDEMA Prepared by, Mrs. Anju Ullas Lecturer Dept. of Medical Surgical Nursing Yenepoya Nursing College
Learning objectives Students will be able to: Ø define edema Ø enlist and explain the types of edema. Ø explain causes, manifestations, pathophysiology, diagnostic clinical evaluation , complications and management in detail of hypokalemia and hyperkalemia.
Introduction • Edema, also spelled oedema is an abnormal accumulation of fluid in the interstitium, located beneath the skin and in the cavities of the body, which can cause severe pain. Clinically, edema manifests as swelling. The amount of interstitial fluid is determined by the balance of fluid homeostasis; and the increased secretion of fluid into the interstitium.
Meaning Edema is a excessive fluid trapped in the body's tissues or it is the abnormal accumulation of fluid in certain tissues within the body.
The accumulation of fluid may be under the skin • usually in dependent areas such as the legs (peripheral edema, or ankle edema) or arms • or it may accumulate in the lungs (pulmonary edema).
Causes • liver, kidney and thyroid diseases • Congestive heart failure • Being largely overweight or obese. • Standing or sitting for long periods of time • Diabetes • Peripheral vascular diseases • Pregnancy • High blood pressure
• Low protein levels • Menopause • Poor Circulation • Head Injuries • Eating food with a high salt content. • Spider & Insect Bites • Allergic reaction • Medications • Electrolyte imbalance
Types • Peripheral edema • Pedal edema • Lymphedema • Pulmonary edema • Cerebral edema • Macular edema • Peri-orbital edema
• Peripheral edema. This usually affects the legs, feet, ankles and arms. It could be a sign of problems of circulatory system, lymph nodes, or kidneys.
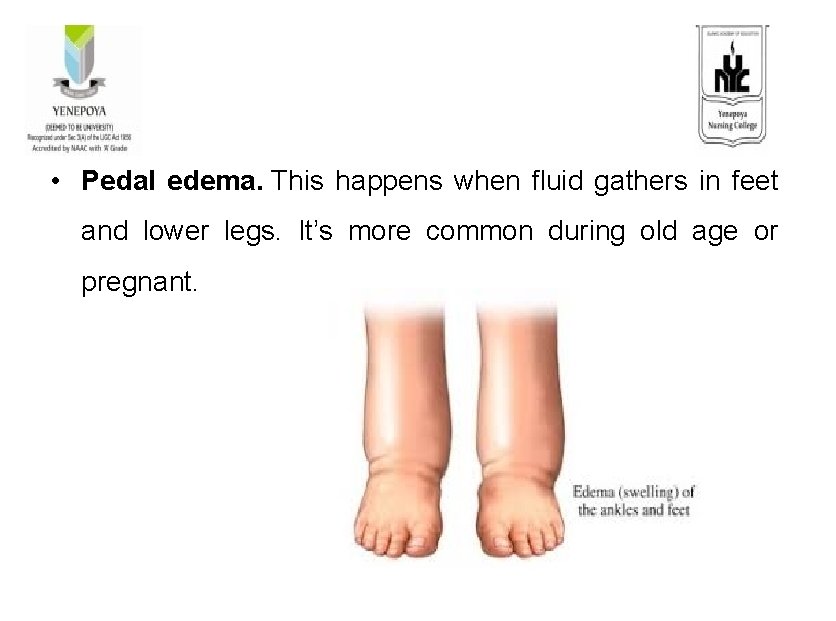
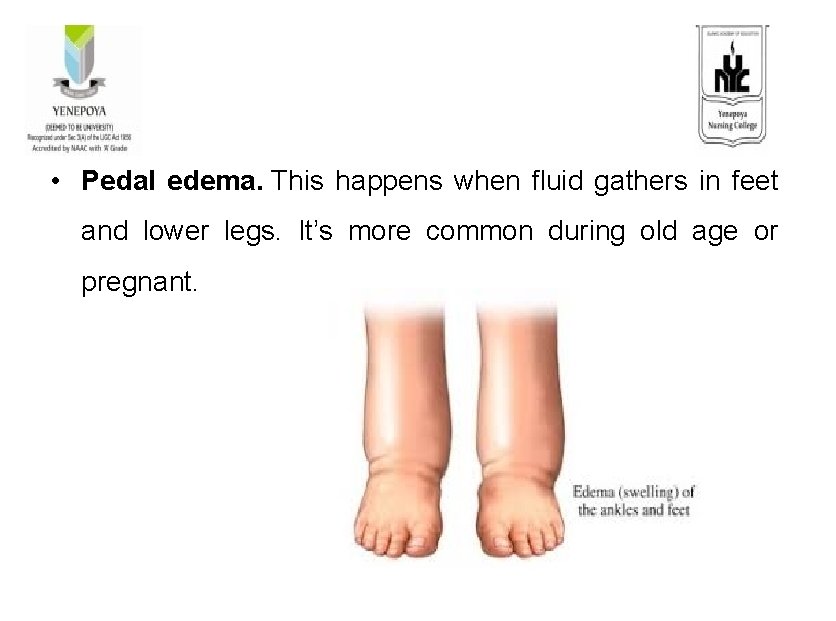
• Pedal edema. This happens when fluid gathers in feet and lower legs. It’s more common during old age or pregnant.
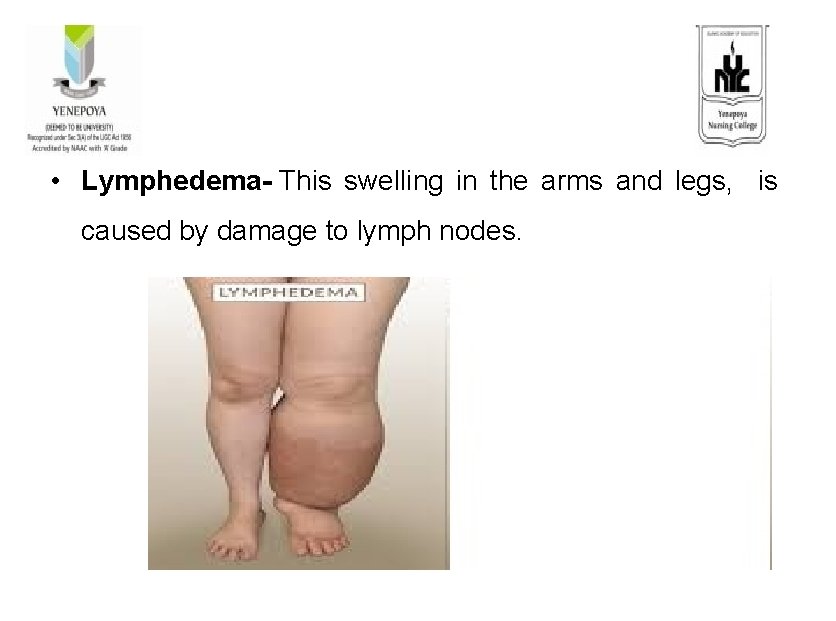
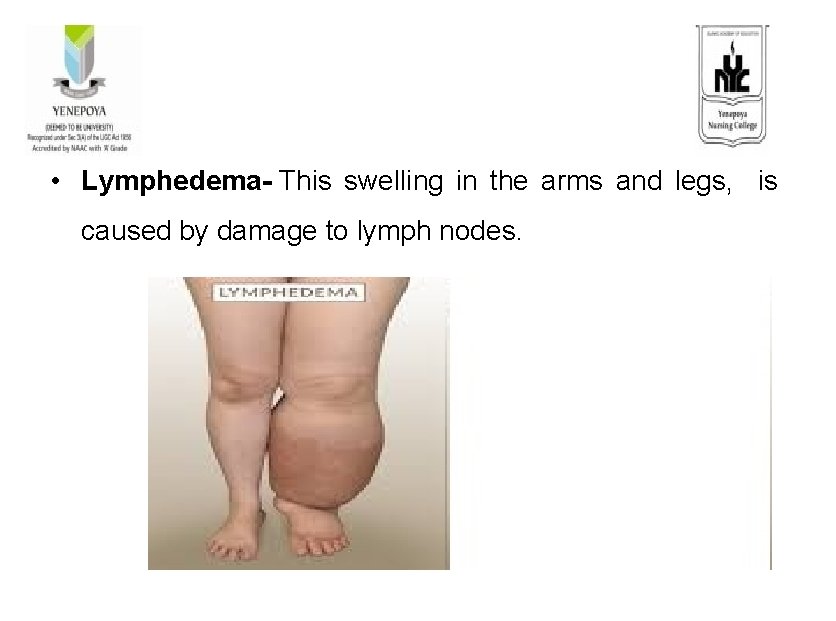
• Lymphedema- This swelling in the arms and legs, is caused by damage to lymph nodes.
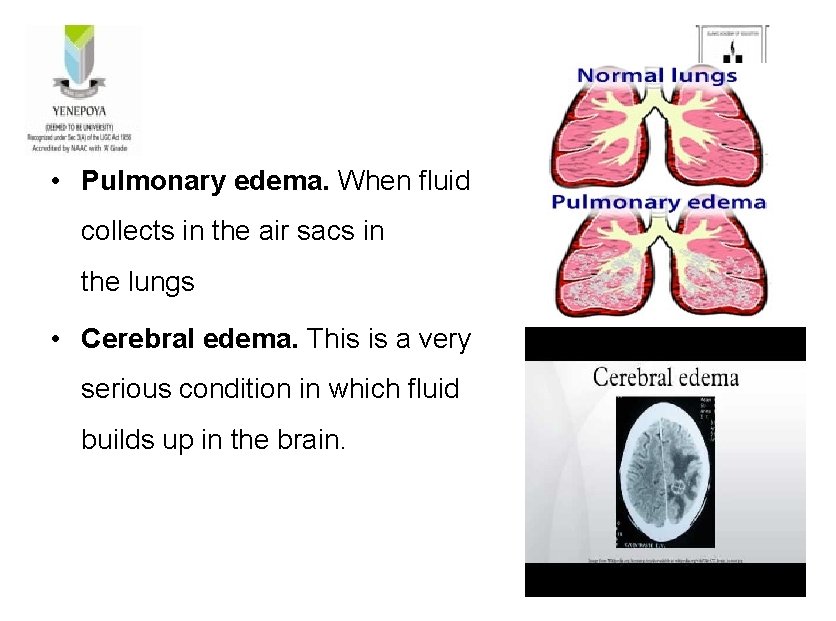
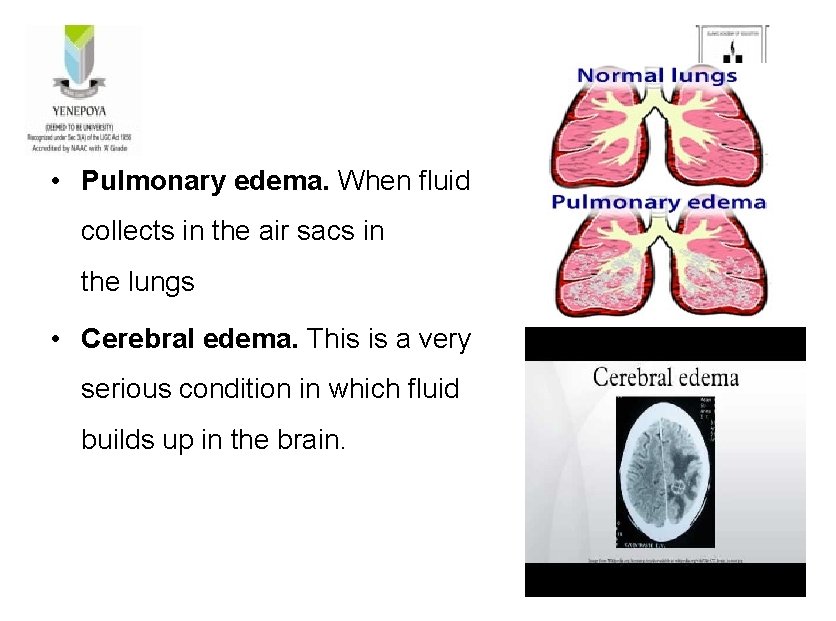
• Pulmonary edema. When fluid collects in the air sacs in the lungs • Cerebral edema. This is a very serious condition in which fluid builds up in the brain.
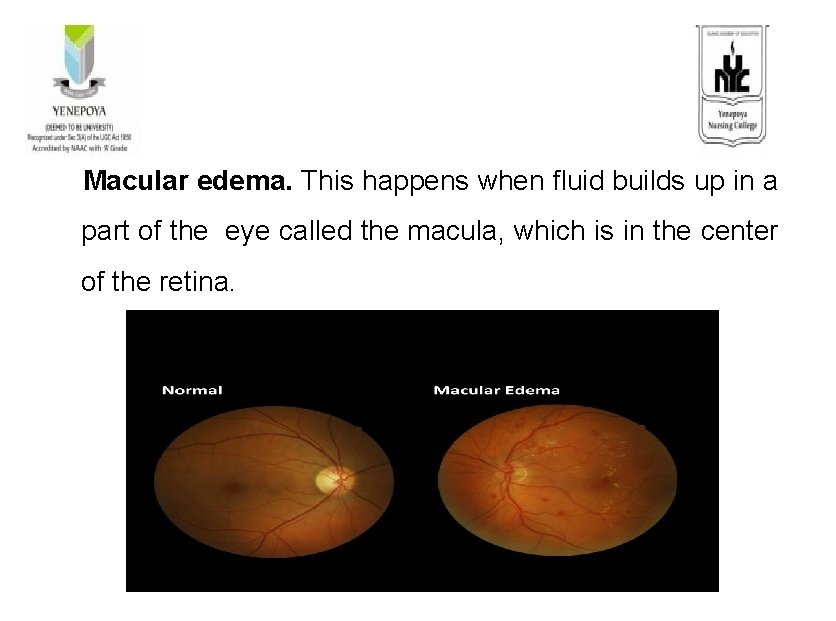
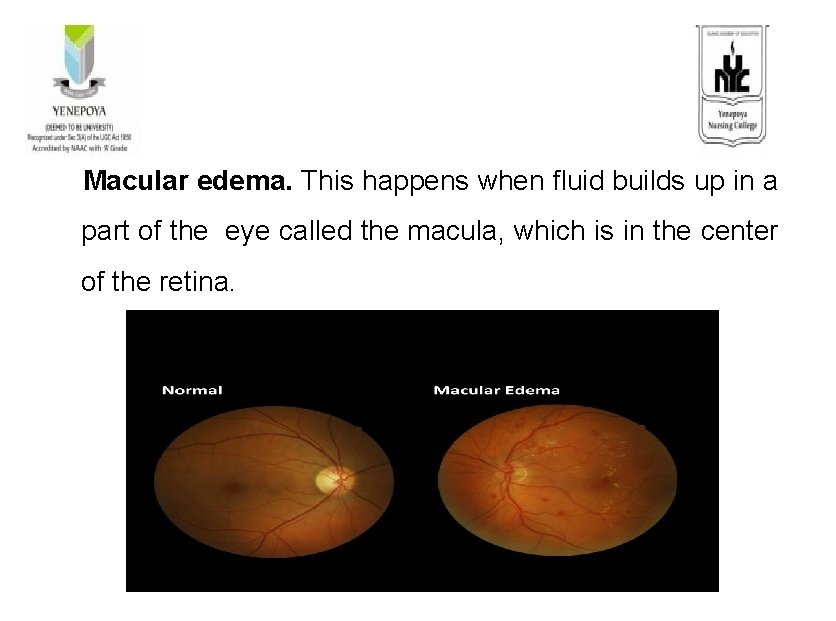
Macular edema. This happens when fluid builds up in a part of the eye called the macula, which is in the center of the retina.
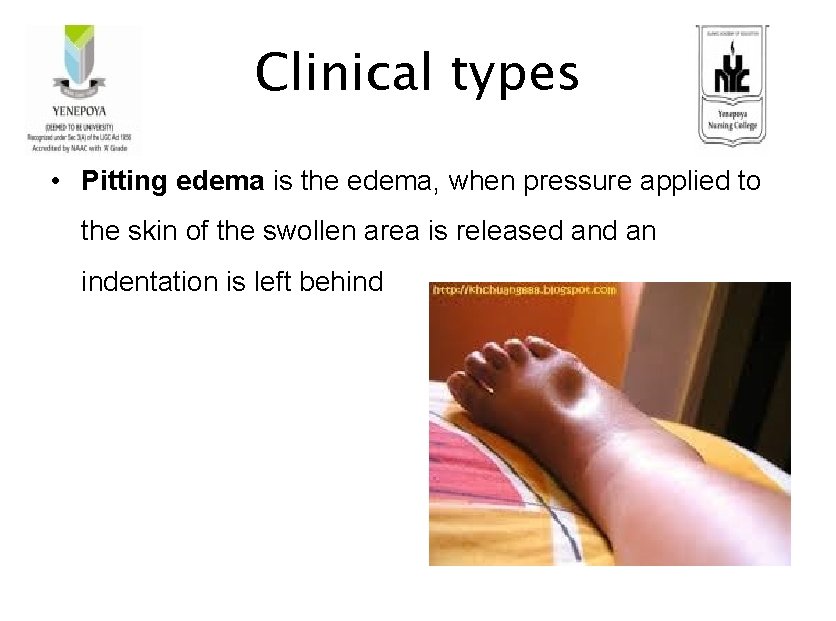
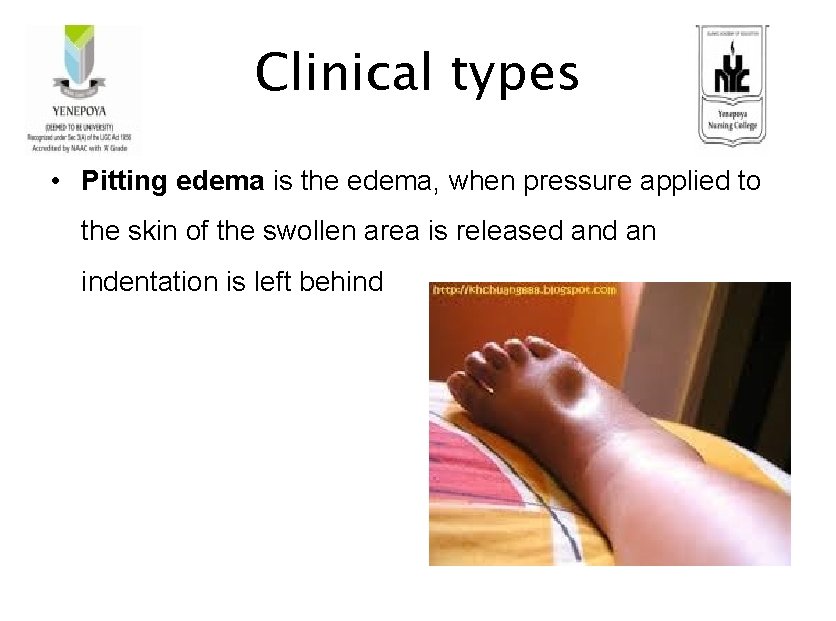
Clinical types • Pitting edema is the edema, when pressure applied to the skin of the swollen area is released an indentation is left behind
• Non-pitting edema is the term used to describe edema when this pressure-induced indentation does not occur.
Signs and symptoms • Puffiness of the tissue directly under your skin, especially in legs or arms • Stretched or shiny skin • Skin that retains a dimple (pits), after being pressed for • • • several seconds Increased abdominal girth ( size) Numbness Cramps Heaviness in affected part Visual disturbance
• Persistent indentation of the skin (Pitting) • Swollen feet, ankles and legs • Painful skin sensations such as burning, soreness, tingling • Puffiness • Abdominal bloating • Night sweats • Skin that is warm or hot to the touch
Diagnostic evaluation • History collection • physical examination • medical history. • X-ray • Ultrasound examination • Magnetic resonance imaging • Blood tests • Urine analysis
Management • Elevation of limb • Decrease Na intake • Decrease fluids • Increase proteins • Trendlenburg position • Decreasing or losing weight
• doing regular exercise • wearing supporting stockings • avoiding extremes of temperature, such as hot baths, showers. • dressing warmly in cold weather
• Underlying disease treatment – Hypertension – Liver disease – Kidney disease • Diuretics (eg: Furosemide and menital).
Nursing management Assessment • Review patient’s history to determine the probable cause of the fluid imbalance. • Monitor weight regularly. • Monitor intake and output chart. • Assess nutritional status. • Monitor and note BP and HR. • Assess urine output in response to diuretic therapy. • Note for presence of edema
• Assess for bounding peripheral pulses. • Check for distended neck veins and ascites. Monitor abdominal girth to follow any ascites accurately. • Review serum electrolytes, urine osmolality, and urine specific gravity. • Check for excessive response to diuretics.
Nursing diagnosis • Excess fluid volume related to sodium retention as evidenced by presence of edema in affected part • Risk for impaired skin integrity related to edema in affected part • Knowledge deficit related to edema as evidenced by frequent questioning.
Nursing interventions • Instruct patient, caregiver, and family members regarding fluid restrictions, as appropriate. • Limit sodium intake as prescribed. • Monitor fluid intake. • Take diuretics as prescribed. • Elevate edematous extremities
• Place the patient in a semi-Fowler’s or high-Fowler’s position. • Aid with repositioning every 2 hours if the patient is not mobile. • Educate patient and family members regarding fluid volume excess and its causes.
Complications • Increasingly painful swelling • Difficulty walking • Stiffness • Stretched skin, which can become itchy and uncomfortable • Increased risk of infection in the swollen area • Scarring between layers of tissue • Decreased blood circulation • Decreased elasticity of arteries, veins, joints and muscles • Increased risk of skin ulcers
Prevention • Follow a low salt diet • Avoid drinking more fluids • try to lose weight and reduce the pressure on lower limbs and joints • Elevate legs above the level of heart to keep swelling down and improve blood flow • If ankles and feet are swollen during pregnancy, keep legs elevated and lie on the side rather than back
• When lying down, place a pillow under legs • Wear support or compression stockings to improve the flow of blood through the veins • Avoid leg swelling on long trips by standing up and walking around often or get up every hour • Exercise feet and lower legs while sitting as this will help the veins move blood back toward the heart • Avoid smoking and drinking alcohol • Try massage therapy, which stimulates blood flow and improves circulation
Summary In this topic we have discussed about the definition, types causes, pathophysiology, clinical manifestation and management of patient with edema
Conclusion Edema can be generalized or localized in presentation. It can appear abruptly, or develop insidiously over time. It is generally seen as an underlying symptom to a worsening ailment or disease process. Treatment of edema is directly aligned with the organ or disease process creating it, such as decreasing sodium (Na+) intake, elevated lower extremities, or administration of cardiac medications.
Evaluation Ø define edema Ø enlist and explain the types of edema. Ø Management of patient with edema
References 1. Black MJ. Textbook of medical surgical nursing. 7 th ed. St. louis: Saunders 2. Brunner. Text book of medical surgical nursing. 6 th ed. Philadelphia: Saunders; 3. Lewis. Medical surgical nursing. 6 th ed. St louis: Mosby 4. Linda S Williams. Understanding Medical surgical nursing. 5 th ed. Jaypee publication